Abstract
Schistosomiasis is a serious water-borne disease of public health importance in southern Africa and is characterised by high morbidity and negative socio-economic repercussions. Limited knowledge on the mode of transmission and treatment contribute towards increase in the risk of infection. This study assessed community knowledge levels, perceptions and the co-constructed realities of social actors with regards to schistosomiasis in rural resource-poor communities of Ndumo in South Africa and Ntalale in Zimbabwe. We hypothesised that there was association between community knowledge level on schistosomiasis and location of residency and socio-demographic factors. Two-hundred and eight questionnaires were used to gather quantitative data on socio-demographics and knowledge levels while 18 focus group discussions were used to collect qualitative data on perceptions and social constructs. The Fisher's exact and Chi-square tests were used to determine the differences in community knowledge levels based on localities, gender, religion and age. Results showed that awareness level of schistosomiasis was assessed as ‘good’ in both Ndumo (91%) and Ntalale (81%). Majority of the respondents identified schistosomiasis as a water-borne disease with significantly higher proportion in Ndumo (89%) compared to Ntalale (68%) (p = 0.005). A significant proportion of participants in both localities were aware of the symptoms of schistosomiasis especially the passing of urine with blood (82.5% in Ndumo and 77.0% in Ntalale; p = 0.039). However, presence of schistosomiasis eggs in human stool apart from urine as a sign of infection was highly acknowledged in Ntalale (57.4%) compared to Ndumo (11.7%; p < 0.001). Knowledge on the body parts affected by the infection was low in both localities with 36.9% in Ntalale compared to 1.0% in Ndumo (p < 0.001). In both study areas, local understanding of schistosomiasis was limited to passing urine with blood, a symptom only seen in cases of urinary schistosomiasis. All the participants associated schistosomiasis with being water-borne, but had divergent perceptions on the symptoms, lifecycle and treatment of the infection. Trends of schistosomiasis and at-risk populations were perceived differently in Ndumo and Ntalale. Although respondents from the two localities acknowledged schistosomiasis as water-borne disease, the study showed lack of in-depth knowledge on the life cycle of the diseases. We therefore recommend that health education be implemented together with other strategies such as improvement in access to water and sanitation in the two study areas to achieve effective control and prevention of the disease.
Keywords: Schistosomiasis, Knowledge level, Perceptions, South Africa, Zimbabwe
Highlights
-
•
Community awareness level of schistosomiasis as a water-borne disease was good
-
•
Knowledge levels of the cause and risk factors of schistosomiasis was relatively low
-
•
Communities from the two study localities were aware of the symptoms of Schistosoma haematobium and not the mode of transmission
-
•
Knowledge on S. mansoni was poor in both areas
-
•
In Ndumo, the understanding of schistosomiasis had changed over time
1. Background
Schistosomiasis is one of the most prevalent water-borne parasitic diseases in sub-Saharan Africa caused by trematode worms of the genus Schistosoma (Class: Trematoda, Family: Schistosomatidae) (Kabatereine et al., 2014; Dawaki et al., 2015). About 200 million people are infected with schistosomiasis, and over 90% infections are in sub-Saharan Africa (Dawaki et al., 2015). Transmission involves an intermediate host snail species of the genus Bulinus and Biomphalaria and takes place at human water-contact points where infected snails are present and shedding cercariae (Kloos et al., 1998; Chimbari, 2012; Midzi et al., 2014; Magaisa et al., 2015). Eggs are excreted by infected individuals, and after reaching a body of freshwater, eggs hatch to release miracidia that must infect the intermediate host snail for reproduction. Cercariae are subsequently shed by the snail into water and penetrate the intact skin of humans who get in contact with contaminated water to complete the life cycle.
In South Africa and Zimbabwe, schistosomiasis is endemic and poses public health challenges characterised by high morbidity, negative socio-economic repercussions and mortality (Chimbari, 2012; Midzi et al., 2014; Magaisa et al., 2015). In Zimbabwe, a nationwide schistosomiasis survey carried out in 2014 involving 280 primary schools showed that nearly 50% of surveyed schools had moderate prevalence while approximately 20% had high prevalence (Midzi et al., 2014). Another study in Ndumo, South Africa revealed an overall prevalence of 37.5% (120/320) of S. haematobium among school-going children aged 10–15 years (Muhubiri, et al., 2017). The high prevalence in most communities in affected areas is exacerbated by lack of- or limited knowledge on the mode of transmission and treatment of this disease which increases the risk of infection. Raising awareness in endemic communities is fundamental for schistosomiasis control, combined with other interventions like mass drug administration (MDA) to at-risk population groups, access to safe water, improved sanitation, health education and snail control (Gazzinelli et al., 2006; Fleming et al., 2009; Wang et al., 2009). Mostly, if the parents and/or household heads are knowledgeable of a disease in their local settings and in this case schistosomiasis, they may encourage their children or family members to participate in control programmes such as MDAs which will contribute to the success of these programmes. Because of limited awareness and lack of knowledge, some school children at-risk of contracting infection may not participate in these programmes and hence become sources of contamination at water contact sites used by communities.
Social science studies on schistosomiasis have dominantly studied the effects of knowledge levels and perceptions on schistosomiasis risk, transmission and treatment. Limited knowledge on schistosomiasis and incorrect perceptions has potential to increase transmission and increase burden of the disease (Cline and Hewlett, 1996; Kloos et al., 1997; Aagaard-Hansen et al., 2009; Manyangadze et al., 2016). Incorrect perceptions towards schistosomiasis may lead to poor health care seeking behaviour. However, studies have shown that an individual's knowledge of a disease does not necessarily result in positive behavioural change that promotes disease prevention and control (Cline and Hewlett, 1996; Gazzinelli et al., 1998; Gazzinelli et al., 2006). Individual choice of where to receive treatment is not only determined by knowledge and perceptions, but by social constructs which afford a holistic understanding of reality within the cultural setting. Social constructs are defined as representations of specific attributes and behaviours of others used in perceiving and interpreting social events inferred from a culturally defined meaning (Stromquist et al., 1991; Huber and Gillaspy, 1998). Hence social constructs consider the context and differences in perceptions that are defined as one's point of view.
In southern Africa, some studies have demonstrated the contributions of socio-economic, demographic and level of development, in the transmission of schistosomiasis (Chimbari et al., 2004; Kapito-Tembo et al., 2009; Chimbari, 2012). The geo-political history of Ndumo (South Africa) and Ntalale (Zimbabwe) influence their political economic dynamics that shape community wealth levels, provision of health infrastructure and services, education structure and water, sanitation and hygiene (WASH), which are important in determining schistosomiasis prevention programmes, treatment and social construct of the disease. South Africa was colonised by the British and Afrikaners that formed an apartheid system. When the new democratic government took over, it adopted an affirmative policy to develop infrastructure in rural areas. Thus, the government constructed more roads, hospitals, schools and provided basic health care services in previously rural disadvantaged areas.
Although Zimbabwean (formerly a British colony), inherited a rich and stable economy in 1980, the initial gains in social protection policies were dismantled by the adoption of a liberal economic model called Economic Structural Adjustment programme (ESAP) that reversed the gains in health provision systems. Although significant progress has been made in the control and prevention of schistosomiasis through mass drug administration (MDA), further weaknesses in the governance system threatens to derail the progress as the national health system and infrastructure are currently in a dilapidated state. Hence, the country is heavily subsidised by international organisations that focus on other interests such as HIV and AIDS and malaria, and diseases such as schistosomiasis tend to be neglected. Limited research has been done in southern Africa to explore schistosomiasis knowledge levels, perceptions and social constructs in resource-poor endemic communities.
This study assessed the knowledge levels and explored perceptions and social constructs on schistosomiasis risk, transmission and treatment among the household heads in Ntalale ward in Gwanda district of Zimbabwe and Ndumo chieftaincy in uMkhanyakude district of South Africa. This was motivated by the view that communities in the similar climatic settings may have similar experiences and adaptive behaviour, however, due to a high level of health infrastructure development and coverage in South Africa compared to Zimbabwe, we expected schistosomiasis knowledge to be higher in Ndumo (South Africa) compared to Ntalale (Zimbabwe) and these knowledge levels were also expected to be associated with socio-demographic factors such as gender, age and religion. Higher knowledge levels and good perceptions of schistosomiasis lead to higher chances of adoption of disease prevention methods and improved treatment seeking behaviour.
2. Materials and methods
2.1. Study area
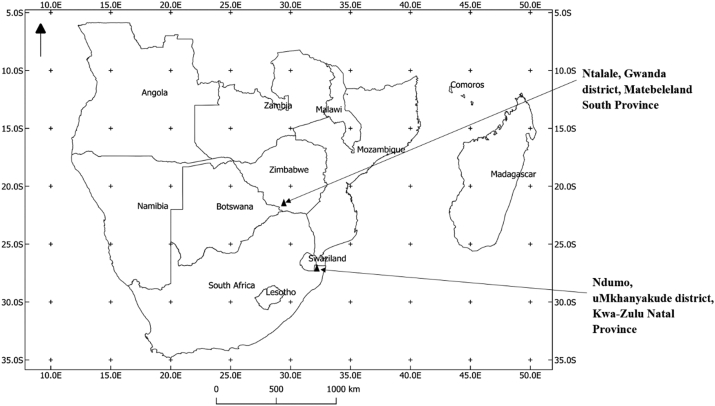
Ntalale in Zimbabwe and Ndumo in South Africa, (Fig. 1), were purposively selected as target geographical spaces for the study for the following reasons; i) the two areas are in the semi-arid sub-tropical region where they experience frequent droughts with changing rainfall patterns due to climate change. They rely more on ground water for domestic and productive uses ii) they are endemic to schistosomiasis (Appleton and Kvalsvig, 2006; Chimbari, 2012; Midzi et al., 2014; Muhubiri et al., 2017) iii) they were part of a larger WHO/TDR funded study on malaria, bilharzia (schistosomiasis) in southern Africa (MABISA). Finally, no study has been conducted on the knowledge levels and perceptions on schistosomiasis in communities residing in the two study areas. Given that the two areas are experiencing increasing temperatures which will exacerbate the risk of schistosomiasis in future, community awareness of the disease is an important factor in determining the transmission and burden of the disease.
Fig. 1.
Southern Africa showing the location of Ntalale in Zimbabwe and Ndumo in South Africa.
The geopolitical spaces in Zimbabwe and South Africa are defined differently, with Ntalale defined as a ward and Ndumo as a sub-chieftaincy area. The two areas share a number of similarities such as; Nguni tribes dominate the study areas; an elected councillor presides, they are the lowest geopolitical units recognised by their respective governments, and there are constituted by a number of villages headed by kraal heads. At least a clinic, shopping centre and primary and secondary schools service the areas. The shortest route between Ntalale and Ndumo by road is approximately 1045 km (Fig. 1).
Differences exists in the power balance; where in Ndumo (South Africa), the traditional leadership is more powerful and commands more respect than the councillor; while in Ntalale (Zimbabwe) the councillor is more powerful than traditional leadership. These power dynamics define the gatekeeper issues, community involvement in external programmes and decision locus.
2.2. Sampling procedure and data collection methods
The target population was the household heads (HH) in the respective study areas, since they are more involved in decision making and providing socio-economic support for families or household in most rural African settings. The views of HH and socio-economic conditions or status carries weight in terms of exposure, prevention and management of diseases at household and community level. Using the ward registers, we established that Ntalale had 371 households. In Ndumo of uMkhanyakude, there was no consolidated register for all the households under the sub-chief. With the assistance of traditional and local leaders, we estimated that the number of rural households were +/− 320. The sample size for the questionnaire survey was based on a confidence level of 95%, with a degree of precision or margin of error of 8%, 50% response distribution and the target population of 341 and 320 households in Ntalale and Ndumo respectively. This resulted in a sample size of 105 and 103 in Ntalale and Ndumo respectively. The sample size was adjusted for a 20% attrition rate or non-response and other errors.
Data collection was done in Zimbabwe in May 2015 and in South Africa in June 2015. The inclusion criteria for the study participants included; being either one of the household heads (wife or husband). Respondent had to be above 18 years and resident of either Ndumo or Ntalale area. A systematic sampling technique was used in both study areas to select the households. In cases where the potential respondent did not satisfy the criteria above and did not consent to be interviewed the next household was considered. The correct and valid questionnaires considered for the study were 122 and 103 for Ntalale and Ndumo, respectively and these were within the determined sample sizes. Questionnaires were administered by trained research assistants who were members of the respective communities.
The study adopted mixed methods combining qualitative and quantitative methods. Firstly, ten and eight focus group interviews (FGDs) were conducted in Ntalale (Zimbabwe) and Ndumo (South Africa), respectively. FGD participants were purposively sampled. Each headman was given a criteria and asked to select between 10 and 15 adult females and males who were above the age of 18 years. FGDs with males and females were done separately. A senior social scientist conducted the FGDs with the help of a local research assistant who was proficient in the native language (isiZulu and Ndebele in Ndumo and Ntalale respectively) and English. The FGDs were used to gather constructed understandings of schistosomiasis which included past indigenous and present knowledge systems, current behaviour in relation to schistosomiasis and perceptions. A voice recorder was used to record all the FGD sessions.
Secondly, questionnaires were administered by research assistants with the supervision of a senior scientist. The questionnaire had closed and open-ended questions. Questions solicited for awareness of schistosomiasis, knowledge level of schistosomiasis, household's experiences with schistosomiasis and on the community level impacts of schistosomiasis. In order to assess the respondents' knowledge level, a matrix of 8 questions was administered as part of the questionnaire. The knowledge level matrix had 8 questions that covered issues on transmission, symptoms, treatment and common misconceptions of schistosomiasis. Table 2 shows the questions and the choices of answers and the correct answers are in bold.
Table 2.
Questions on knowledge regarding schistosomiasis and the choices.
| Knowledge regarding schistosomiasis | Choices |
|---|---|
| Do you know the cause of schistosomiasis |
|
| How schistosomiasis is transmitted |
|
| Parts of the body affected by schistosomiasis infection |
|
| The intermediate host of schistosomiasis in the environment |
|
| Whether schistosomiasis is a waterborne disease |
|
| Passing urine with blood can be a sign of bilharzia |
|
| Schistosomiasis eggs can be found in human stool |
|
| Schistosomiasis can be treated |
|
Correct answers are in bold.
Researchers prepared the questionnaire used in this study guided by the variables considered important to form the knowledge matrix. A pilot survey was conducted in the nearby villages to test and validate the questionnaires before the survey in both Ndumo and Ntalale. Questionnaires which had faults in data captured and omission of some key questions were discarded.
2.3. Data analysis and interpretation
Quantitative data from the questionnaires was coded, entered and analysed in Statistical Package for Social Sciences (SPSS) version 20. Community knowledge of schistosomiasis based on eight (8) questions focusing on causes, symptoms and treatment of schistosomiasis (Table 2) was analysed and expressed as proportions. The Fisher's exact and Chi-square tests were used to determine the differences in community knowledge levels based on study areas, gender, religion and age.
FGDs were conducted in local languages i.e. isiNdebele in Ntalale and isiZulu in Ndumo. Verbatim transcription of qualitative data from the FGDs was conducted by professional translators proficient in both languages. The translation was checked for accuracy and consistency by back and forth translations of randomly selected sections of the recordings. Qualitative data was interpreted using thematic approach with the exception of vernacular names and conceptualisation for schistosomiasis where discourse analyses was employed. The qualitative data was cleaned and contextualised in the FGD settings. Data was grouped into themes and sub-themes before interpretation and linking of sub-themes.
3. Results
3.1. Socio-demographic characteristics of the study participants
Table 1 summaries the demographic characteristics of the study participants in Ndumo (South Africa) and Ntalale (Zimbabwe). Majority of the study participants in both localities were females (61.2% in Ndumo and 80.3% in Ntalale) (Table 1). Both Ntalale and Ndumo had the highest number of participants in the 36–50 years' category. Largest proportion of the participants in both study areas were of the Christian faith (68% for Ndumo and 86.1% for Ntalale).
Table 1.
Socio-demographic characteristics of study participants by locality.
| Characteristic | Study area |
|
|---|---|---|
| Ndumo-South Africa (%) n = 103 |
Ntalale-Zimbabwe (%) n = 122 |
|
| Gender | ||
| Male | 40 (38.8) | 24 (19.7) |
| Female | 63 (61.2) | 98 (80.3) |
| Age (years) | ||
| 20–35 | 29 (28.2) | 25 (20.5) |
| 36–50 | 46 (44.7) | 48 (39.3) |
| 51–65 | 23 (22.3) | 16 (13.1) |
| >65 | 5 (4.9) | 33 (27.0) |
| Religion | ||
| None | 9 (8.7) | 8 (6.6) |
| Christian | 68 (66.0) | 105 (86.1) |
| Mixed | 19 (18.4) | 4 (3.3) |
| African Tradition | 7 (6.8) | 5 (4.1) |
3.2. Knowledge on schistosomiasis
The awareness level of schistosomiasis was good in both Ndumo and Ntalale. A high percentage of respondents (91%, n = 103) were aware of schistosomiasis in Ndumo (South Africa) than in Ntalale (Zimbabwe) (81%, n = 122). Table 3 summarizes, knowledge of causes, symptoms and treatment of schistosomiasis according to localities. The knowledge on the cause of schistosomiasis was low in both study areas (1.0% in Ndumo and 2.5% in Ntalale, p < 0.001). Majority of the respondents identified schistosomiasis as a waterborne disease with significantly higher proportion in Ndumo (89%) compared to Ntalale (68%) (p = 0.005). A significant proportion in both localities were aware that schistosomiasis is not a sexually transmitted disease (STD).
Table 3.
Knowledge of schistosomiasis according to localities (Ndumo in South Africa and Ntalale in Zimbabwe).
| Knowledge regarding schistosomiasis | Correct responses |
||
|---|---|---|---|
| Ndumo (%) n = 103 |
Ntalale (%) n = 122 |
p-value | |
| Cause of schistosomiasis | 1 (1.0) | 3 (2.5) | <0.001b |
| How schistosomiasis is transmitted | 66 (64.1) | 77 (63.1) | 0.399a |
| Parts of the body affected by schistosomiasis infection | 1 (1.0) | 45 (36.9) | <0.001b |
| The intermediate host of schistosomiasis in the environment | 64 (62.1) | 28 (23.0) | <0.001b |
| Whether schistosomiasis is a waterborne disease | 89 (86.4) | 83 (68.0) | 0.005a |
| Passing urine with blood can be a sign of bilharzia | 85 (82.5) | 94 (77.0) | 0.039b |
| Schistosomiasis eggs can be found in human stool | 12 (11.7) | 70 (57.4) | <0.001a |
| Schistosomiasis can be treated | 85 (82.5) | 96 (78.7) | 0.279b |
Significant p-values (<0.05) are in bold.
n: number of respondents; Fisher's exact was used when one of the cell values in the 2 × 2 contingency table was less than 5.
p-value based on chi-square test.
p-value based on Fisher's exact test.
A significant proportion of the participants in both localities were aware of the symptoms of schistosomiasis especially passing of urine with blood (82.5% in Ndumo and 77.0% in Ntalale; p = 0.039). However, knowledge that schistosome eggs can be passed in human stool was highly acknowledged in Ntalale (57.4%) compared to Ndumo (11.7%; p < 0.001). Most of the participants in both localities knew that schistosomiasis can be treated (Table 3) but majority of the participants in Ntalale were more aware (p < 0.001) of the body parts affected by infection (36.9%) compared to Ndumo (1.0%) with.
In Ndumo, there was association between gender and knowledge of schistosomiasis as a waterborne disease (p = 0.031) (Table 3). Religion was not significantly associated with knowledge of schistosomiasis, causes, symptoms and treatment in the two localities. There was correlation between gender and knowledge of schistosomiasis as a waterborne disease in Ndumo (Table 4). Age was associated with knowledge of schistosomiasis, causes, signs and symptoms. In South Africa there was a significant difference (p = 0.024) between proportions in different age groups who acknowledged that blood in urine is a symptom of schistosomiasis. Those below 65 years of age were more knowledgeable compared to those older.
Table 4.
Knowledge of schistosomiasis according to gender.
| Correct responses |
|||
|---|---|---|---|
| Male (%) |
Female (%) |
p-valuea | |
| Ndumo-South Africa | n = 40 | n = 63 | |
| Cause of schistosomiasis | 1 (2.5) | 0 (0) | 0.141b |
| Body part attacked by schistosome parasite | 0 (0) | 1 (1.6) | 0.883b |
| Intermediate host of schistosomes in the environment | 26 (65.0) | 38 (38) | 0.446b |
| Knowledge of schistosomiasis as a waterborne disease | 39 (97.5) | 50 (79.4) | 0.031b |
| Blood in urine can be a sign of bilharzia | 36 (90.0) | 49 (77.8) | 0.340b |
| Schistosomiasis eggs can be found in human stool | 5 (12.5) | 7 (11.1) | 0.272b |
| Schistosomiasis can be treated | 35 (87.5) | 50 (79.4) | 0.670b |
| Bilharzia is a sexually transmitted disease | 3 (7.5) | 3 (4.8) | 0.625b |
| Ntalale–Zimbabwe | n = 24 | n = 98 | |
| Cause of schistosomiasis | 0 (0) | 3 (3.1) | 1.000b |
| Body part affected by schistosomiasis | 12 (50) | 33 (33.7) | 0.364b |
| Intermediate host of schistosomiasis in the environment | 5 (20.8) | 23 (23.5) | 0.674b |
| Know of schistosomiasis as a waterborne disease | 18 (75.0) | 65 (66.3) | 0.071b |
| Blood in urine can be a sign of bilharzia | 22 (91.7) | 72 (73.5) | 0.158b |
| Schistosomiasis can be found in human stool | 15 (62.5) | 55 (56.1) | 0.797b |
| Schistosomiasis can be treated | 22 (91.7) | 74 (75.5) | 0.323b |
| Bilharzia is a sexually transmitted disease | 3 (12.5) | 10 (10.2) | 0.786b |
Significant p-values (<0.05) are in bold.
n: number of respondents. Fisher's exact was used when one of the cell values in the 2 × 2 contingency table was less than 5.
p-value based on chi-square test.
p-value based on Fisher's exact test.
In Zimbabwe there was a significant difference between proportions in different age groups that correctly identified the cause of schistosomiasis (p < 0.05). The middle age range of 35–65 years had higher proportions of participants who managed to correctly identify the causes of schistosomiasis.
3.3. Perceptions and social actor's constructions
In Ntalale, the original local name for schistosomiasis is inkabalo. Literally inkabalo means the navel. Thus, schistosomiasis was constructed as a disease of the navel and acute stomach problems that result in one passing urine with blood. The reference to schistosomiasis as inkabalo was over time replaced by the term nxama-gazi, which is in use to date. Nxama literary means urinate and gazi means blood. Nxama-gazi describes the passing of urine with blood droplets towards the end of urination. The shift in the conceptualisation of schistosomiasis was influenced by the shift from relying on traditional medical knowledge to modern medicine. Inkabalo was considered to be misleading as there are various acute infections that affect the stomach especially in women. Nxama-gazi was socially constructed with the influence of the formal medical practitioners, since it directly singled out schistosomiasis. In Ndumo, schistosomiasis is referred to as isichenene or umkhazi. The two terms are used inter-changeably and they mean passing blood with urine. The indigenous terms used in both Ndumo and Ntalale express the aspect of passing urine with blood.
FGD's held in the Ntalale ward showed that some community members still rely on traditional herbs for the treatment or management of schistosomiasis. In an FGD it was explained as follows;
The elders in the past used to prevent and treat schistosomiasis so it was not as much as in the current times. The elders used herbs to prevent and treat schistosomiasis. Today, schistosomiasis appears to be more than in the past because the clinic is bringing it out [spoken of openly] … through health campaigns. Herbs were put in the mahewu (a fermented drink made from cereals) for prevention. One could get sick from schistosomiasis but they did not pass as much blood in urine as the case with the current infections (FGD interview Ntalale, Gwanda).
Based on this quote it can be deduced that the community still used traditional herbs to manage schistosomiasis. Furthermore, they noticed the increase in the amount of blood in the urine.
The use of traditional herbs in the management of schistosomiasis was subscribed to high levels of poverty, social stigma and their belief in them. Unlike in Ndumo (South Africa) which has better health delivery facility and system, the Ntalale system in Zimbabwe has a relatively poor health facility and system and usually located at far from where majority of the study communities live. It was also observed that the transport network system connecting communities to the business centre where the clinic is situated is better in Ndumo than in Ntalale. In Ndumo, there are open truck vehicles that carry people to and from the clinic at a fee. Furthermore, in Ndumo there are mobile clinics that frequently visit the area, while in Ntalale, there was one bus that serviced the area and people had to rely on animal drawn carts or walking to and from the clinic. The difficulties experienced in accessing the clinic is an important factor in the continued use of herbs in treating schistosomiasis. However, in both rural communities, praziquantel (the drug for treating schistosomiasis) was free of charge when available at the clinic.
The two communities held different responses from the sub-themes of FGD, highlighting different perceptions of the five different stages of schistosomiasis cycle. These perceptions demonstrate how schistosomiasis is conceptualised by the different participants of the FGDs. Although the participants associated schistosomiasis with water, they had divergent perceptions on the symptoms and life cycle of the parasite. Trends of schistosomiasis and at-risk populations were perceived differently in Ndumo and Ntalale. In Ntalale, schistosomiasis was perceived to be decreasing and fishermen were perceived to be the most at risk population. In Ndumo, schistosomiasis was perceived as having increased over time with women and children being at higher risk of the disease. Furthermore, FGD participants from Ntalale indicated that transmission of schistosomiasis takes place when one gets in contact with urine and dirty water. In Ndumo, varied incorrect perceptions on infection transmission patterns existed ranging from jumping a fire, stagnant water as high risk and the association of schistosomiasis to sexually transmitted disease (perhaps taken from its effects on reproductive organs).
The FGD participants indicated symptoms associated with urinary schistosomiasis such as passing of urine with blood and discomforts/pains associated with passing the urine. Some individuals from Ndumo associated passing urine with blood to maturity and the body's preparedness for sexual intercourse. Just like the questionnaire respondents, FGD participants did not allude to Schistosoma mansoni, the cause of intestinal schistosomiasis, in their responses. The FGD participants in both study areas perceived that schistosomiasis was treatable and they preferred modern medicine. However, in Ndumo traditional medicine seemed to be still valued while in Ntalale it was used in the past. Study participants from Ndumo use traditional herbal treatment before going to a clinic or hospital. Traditional herbs were perceived to be effective in the management of schistosomiasis and the distance to the clinic was another factor that contributed to the use of traditional medicines in managing schistosomiasis. In Zimbabwe, traditional herbalists were scorned and participants preferred conventional or western treatment. Communities distrusted the traditional practitioners and blamed them for exacerbating schistosomiasis through the healing rituals performed in rivers and streams. Fishermen were perceived to be the high-risk group in Ntalale as they risk contracting schistosomiasis when they immerse in water for long periods while fishing. The fishermen perceived that some rituals can save them from contracting schistosomiasis.
4. Discussion
This study assessed the knowledge level, perceptions and actor constructions of schistosomiasis in two semi-arid endemic areas in southern African namely; Ndumo in South Africa and Ntalale in Zimbabwe. The high levels of awareness found in this study suggest that schistosomiasis is endemic in the two study areas (Chimbari, 2012; Magaisa et al., 2015). A large proportion of respondents in Ndumo, who had stayed in the area for more than 41 years were aware of schistosomiasis. The FGD data shows that the disease has affected their communities since the colonial period. The first schistosomiasis case was reported in 1863 and using data collected in surveys between 1860 and 1932, the first schistosomiasis map was produced for South Africa (Magaisa et al., 2015). Porter in 1938, Appleton and Stiles (1976) and Gear et al. (1980) produced schistosomiasis maps that demonstrate high prevalence of schistosomiasis in uMkhanyakude district, which our study area is part of (Appleton and Stiles, 1976; Magaisa et al., 2015). In Ntalale, respondents who had stayed in the area for a period between 20 and 50 years had higher proportion of people aware of schistosomiasis. In Zimbabwe, early cases of schistosomiasis were detected in the early 1940s (Gelfand and Osburn, 1943). Three surveys conducted since 1982 show that Gwanda had a high prevalence of schistosomiasis, of which Ntalale is part of (Chimbari, 2012). The high schistosomiasis awareness levels in both study areas might be due to the individuals' experiences on the health and social effects of schistosomiasis for decades.
We observed that higher proportions of respondents from Ndumo were aware of schistosomiasis than Ntalale in most of the aspects probed in this study. Ntalale is one of the areas included in the MDA programme being supported by WHO in Zimbabwe. The lack of knowledge on some key aspects of schistosomiasis transmission demonstrates the neglect of the health education component in the morbidity control strategy in Zimbabwe. In Ndumo, the score demonstrates weaknesses in the health education structures in the area as well. In KwaZulu-Natal, regular treatment of children with praziquantel reduced egg excretion by 95.3% three weeks after treatment (Appleton and Kvalsvig, 2006; Kabuyaya et al., 2017a). The rate of new infections remained high partly due to a weak schistosomiasis education component to the programme (Magaisa et al., 2015; Kabuyaya et al., 2017b). The regular praziquantel treatment were too expensive and lacked financial support leading to the collapse of the programme (Magaisa et al., 2015). In cases where schistosomiasis health education contributed to the successful control of the disease, continuous assessments of the programme, and evaluating change in infection patterns have been key (Curtale et al., 1998).
Findings from the FGDs and questionnaire survey indicate that the community associates schistosomiasis with passing urine with blood and abdominal pains especially when passing urine, which are symptoms of S. haematobium. This shows weaknesses in the communities' acknowledgement of S. mansoni. Although the life cycles for both forms of the disease are similar, it should be noted that unlike urinary, intestinal schistosomiasis has clinical symptoms which are not easily noticeable by infected individuals (Cline and Hewlett, 1996). More respondents from Ntalale, Zimbabwe (57%) had knowledge of intestinal schistosomiasis than in Ndumo. In Ndumo, negative perceptions associated passing bloody urine with sexuality and sex. Despite 64% of the respondents knowing that schistosomiasis is not a sexually transmitted disease, it was perceived as embarrassing to pass blood through your genitals. Other studies have documented that such misinformation has negative implications on individual choices in seeking schistosomiasis treatment (Takougang et al., 2004; Odhiambo et al., 2014).
High proportions of respondents were aware that schistosomiasis was treatable, however, the mode of treatment preferences differed from individual to individual or household to household. In Ndumo, both western and traditional medicines were used in the treatment of schistosomiasis. Study participants from Ndumo use traditional herbal treatment before going to a clinic or hospital as this was perceived to be effective in the management of schistosomiasis. Koffi et al. (2018) also noted that cultural conceptions of schistosomiasis influence health-seeking behaviours and in their study in northern Côte d'Ivoire and southern Mauritania participants also highlighted that the “mystic form of schistosomiasis” can only be treated by traditional healers through prayers and medicinal plants. A study conducted in the Magu district of Tanzania also observed that in endemic areas, patients consult traditional healers (Mwanga et al., 2004). The knowledge of the disease and the social construction around it influences people's care-seeking choices and leads to people using methods that are in contrast to those advocated by biomedical sciences and which may result in a delay in effective healthcare (Koffi et al., 2018). In the current study, in Zimbabwe, traditional herbalists were scorned and participants preferred western treatment. The communities distrusted the traditional practitioners and blamed them for exacerbating schistosomiasis through the healing rituals performed in rivers or streams. This is contrary to many other previous studies as mentioned above. It indicates the existence of good care practices in communities in Zimbabwe as they know and trust medical means to manage the disease thereby reducing the burden of the disease. de Silva et al. (2001) noted that care-seeking behaviours of mothers and maternal knowledge of symptoms of the disease contributed to reducing childhood disease in Sri Lanka.
Our study shows lack of in-depth knowledge on the schistosomiasis lifecycle and hence we recommend that health education be implemented together with other strategies in the two study areas for the control and prevention of schistosomiasis. High levels of knowledge of the disease have been documented to determine the successes of schistosomiasis control programmes worldwide especially in China, Brazil, Uganda and Egypt (Magaisa et al., 2015). Knowledge and perceptions are key drivers of behaviour change and having the correct knowledge and perception in a community enhances success of control and intervention programmes since the interventions are tailored to suit the local context.
Ethical issues
The study received ethical clearance from the Biomedical Research Ethics Committee (BREC) BE 182/13, University of KwaZulu-Natal and the Medical Research Council of Zimbabwe (MRCZ) MRCZ/A/1737.
Funding
The project was supported by the College of Health Sciences scholarship programme at the University of KwaZulu-Natal and the MABISA project funded by the WHO Special Programme for Research and Training in Tropical Diseases (TDR) and the Canadian International Development Research Centre (IDRC).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
We would like to acknowledge the following institutions for their contributions to the study: The Jozini Municipality and Gwanda Rural District Council for granting access to the two communities; University of KwaZulu-Natal and Biomedical Research and Training Institute for facilitating the administration of the research grant. We would like to finally thank the communities especially the research respondents and participants.
References
- Appleton C., Kvalsvig J. A school-based helminth control programme successfully implemented in KwaZulu-Natal. South Afr. J. Epidemiol. Infect. 2006;21(2):55–67. [Google Scholar]
- Appleton C., Stiles G. Geology and geomorphology in relation to the distribution of snail intermediate hosts of bilharzia in South Africa. Ann. Trop. Med. PH. 1976;70(2):189–198. doi: 10.1080/00034983.1976.11687111. [DOI] [PubMed] [Google Scholar]
- Chimbari M.J. Enhancing schistosomiasis control strategy for Zimbabwe: building on past experiences. J. Parasitol. Res. 2012;2012 doi: 10.1155/2012/353768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chimbari M.J., Chirebvu E., Ndlela B. Malaria and schistosomiasis risks associated with surface and sprinkler irrigation systems in Zimbabwe. Acta Trop. 2004;89(2):205–213. doi: 10.1016/j.actatropica.2003.09.015. [DOI] [PubMed] [Google Scholar]
- Cline B.L., Hewlett B.S. Community-based approach to schistosomiasis control. Acta Trop. 1996;61(2):107–119. doi: 10.1016/0001-706x(95)00118-x. [DOI] [PubMed] [Google Scholar]
- Curtale F., Pezzotti P., Sharbini A.L., Al Maadat H., Ingrosso P., SobhySaad Y., Babille M. Knowledge, perceptions and behaviour of mothers toward intestinal helminths in Upper Egypt: implications for control. Health Policy Plann. 1998;13(4):423–432. doi: 10.1093/heapol/13.4.423. [DOI] [PubMed] [Google Scholar]
- Dawaki S., Al-Mekhlafi H.M., Ithoi I., Ibrahim J., Abdulsalam A.M., Ahmed A., Sady H., Nasr N.A., Atroosh W.M. The menace of schistosomiasis in Nigeria: knowledge, attitude, and practices regarding schistosomiasis among rural communities in Kano State. PLoS One. 2015;10(11) doi: 10.1371/journal.pone.0143667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Silva M.A., Wijekoon A., Hornik R., Martines J. Care seeking in Sri Lanka: one possible explanation for low childhood mortality. Soc. Sci. Med. 2001;53:1363–1372. doi: 10.1016/s0277-9536(00)00425-1. [DOI] [PubMed] [Google Scholar]
- Fleming F., Fenwick A., Tukahebwa E., Lubanga R., Namwangye H., Zaramba S., Kabatereine N. Process evaluation of schistosomiasis control in Uganda, 2003 to 2006: perceptions, attitudes and constraints of a national programme. Parasitol. 2009;136(13):1759–1769. doi: 10.1017/S0031182009990709. [DOI] [PubMed] [Google Scholar]
- Gazzinelli A., Gazzinelli M.F., Cadete M.M., Pena Filho S., Sá I.R., Kloos H. Socio-cultural aspects of Schistosomiasis mansoni in an endemic area in Minas Gerais, Brazil. Cadernos de Saudepublica. 1998;14(4):841–849. doi: 10.1590/s0102-311x1998000400026. [DOI] [PubMed] [Google Scholar]
- Gazzinelli M.F., Reis D.C., Kloos H., Velásquez-Melendez G., Dutra I.R., Gazzinelli A. The impact of two education methods on knowledge of schistosomiasis transmission and prevention among schoolchildren in a rural community in northern Minas Gerais, Brazil. Mem. Inst. Oswaldo Cruz. 2006;101:45–53. doi: 10.1590/s0074-02762006000900008. [DOI] [PubMed] [Google Scholar]
- Gelfand M., Osburn H. Clinical Proceedings. Cape Town. 1943. Katayama in southern Rhodesia; pp. 169–173. 1943. [Google Scholar]
- Kabatereine N., Fleming F., Thuo W., Tinkitina B., Tukahebwa E.M., Fenwick A. Community perceptions, attitude, practices and treatment seeking behaviour for schistosomiasis in L. Victoria islands in Uganda. BMC Research Notes. 2014;7(1):900–910. doi: 10.1186/1756-0500-7-900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabuyaya M., Chimbari M.J., Manyangadze T., Mukaratirwa S. Efficacy of praziquantel on Schistosoma haematobium and re-infection rates among school-going children in the Ndumo area of uMkhanyakude district, KwaZulu-Natal, South Africa. Infect. Dis. Poverty. 2017;6(1):83–91. doi: 10.1186/s40249-017-0293-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabuyaya M., Chimbari M.J., Manyangadze T., Mukaratirwa S. Schistosomiasis risk factors based on the infection status among school-going children in the Ndumo area, uMkhanyakude district, South Africa. S. Afr. J. Infect. Dis. 2017;32(2):67–72. [Google Scholar]
- Kapito-Tembo A.P., Mwapasa V., Meshnick S.R., Samanyika Y., Banda D., Bowie C., Radke S. Prevalence distribution and risk factors for Schistosoma hematobium infection among school children in Blantyre, Malawi. PLOS Neglect. Trop. Dis. 2009;3(1):e361. doi: 10.1371/journal.pntd.0000361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kloos H., Fulford A., Butterworth A., Sturrock R., Ouma J., Kariuki H., Thiongo F., Dalton P., Klumpp R. Spatial patterns of human water contact and Schistosoma mansoni transmission and infection in four rural areas in Machakos District, Kenya. Soc. Sci. Med. 1997;44(7):949–968. doi: 10.1016/s0277-9536(96)00218-3. [DOI] [PubMed] [Google Scholar]
- Kloos H., Gazzinelli A., Van Zuyle P. Microgeographical patterns of schistosomiasis and water contact behavior; examples from Africa and Brazil. Mem. Inst. Oswaldo Cruz. 1998;93:37–50. doi: 10.1590/s0074-02761998000700006. [DOI] [PubMed] [Google Scholar]
- Koffi A.J., Doumbia M., Fokou G., Keita K., Koné B., Abé N.N. Community knowledge, attitudes and practices related to schistosomiasis and associated healthcare-seeking behaviours in northern Côte d'Ivoire and southern Mauritania. Infect. Dis. Poverty. 2018;7(70) doi: 10.1186/s40249-018-0453-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magaisa K., Taylor M., Kjetland E.F., Naidoo P.J. A review of the control of schistosomiasis in South Africa. S. Afr. J. Sci. 2015;111:1–6. [Google Scholar]
- Manyangadze T., Chimbari M.J., Gebreslasie M., Mukaratirwa S. Risk factors and micro-geographical heterogeneity of Schistosoma haematobium in Ndumo area, uMkhanyakude district, KwaZulu-Natal, South Africa. Acta Trop. 2016;159:176–184. doi: 10.1016/j.actatropica.2016.03.028. [DOI] [PubMed] [Google Scholar]
- Midzi N., Mduluza T., Chimbari M.J., Tshuma C., Charimari L., Mhlanga G., Manangazira P., Munyati S.M., Phiri I., Mutambu S.L. Distribution of schistosomiasis and soil transmitted helminthiasis in Zimbabwe: towards a national plan of action for control and elimination. Plos Neglect. Trop. Dis. 2014;8(8) doi: 10.1371/journal.pntd.0003014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mwanga J.R., Magnussen P., Mugashe C.L., Gabone R.M., Aagaard-Hansen J. Schistosomiasis-related perceptions, attitudes and treatment-seeking practices in Magu district, Tanzania: public health implications. J. Biosoc. Sci. 2004;36:63–81. doi: 10.1017/s0021932003006114. [DOI] [PubMed] [Google Scholar]
- Odhiambo G.O., Musuva R.M., Atuncha V.O., Mutete E.T., Odiere M.R., Onyango R.O., Alaii J.A., Mwinzi P.N. Low levels of awareness despite high prevalence of schistosomiasis among communities in Nyalenda informal settlement, Kisumu City, Western Kenya. Plos Neglect. Trop. Dis. 2014;8(4) doi: 10.1371/journal.pntd.0002784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takougang I., Meli J., Fotso S., Angwafo F., Kamajeu R., Ndumbe P.M. Some social determinants of urinary schistosomiasis in Northern Cameroon: implications for schistosomiasis control. Afr. J. Health Sci. 2004;11(3):111–120. doi: 10.4314/ajhs.v11i3.30788. [DOI] [PubMed] [Google Scholar]
- Wang L.D., Guo J.G., Wu X.H., Chen H.G., Wang T.P., Zhu S.P., Zhang Z.H., Steinmann P., Yang G.J., Wang S.P. China's new strategy to block Schistosoma japonicum transmission: experiences and impact beyond schistosomiasis. Tropical Med. Int. Health. 2009;14(12):1475–1483. doi: 10.1111/j.1365-3156.2009.02403.x. [DOI] [PubMed] [Google Scholar]