Abstract
Digital therapeutics (DTx), like drugs or medical devices, 1) must prove their effectiveness and safety through clinical trials; 2) are provided to patients through prescriptions from doctors; and 3) may require the approval of regulatory agencies, though this might not be mandatory. Although DTx will play an important role in the medical field in the near future, some merits of DTx have been exaggerated at this crucial juncture. In the medical field, where safety and effectiveness are important, merely reducing the development time and costs of DTx is not advantageous. The adverse effects of DTx are not yet well-known, and will be identified eventually, with the passage of time. DTx is beneficial for the collection and analysis of real-world data (RWD); however, they require new and distinct work to collect and analyze high-quality RWD. Naturally, whether this is possible must be independently ascertained through scientific methods. Depending on the type of disease, it is not recommended that DTx be prescribed, even if the patient rejects conventional treatment. Prescription of conventional pharmacotherapy is often necessary, and if the prescription of DTx is inadequate, the critical time for initial treatment may be missed. There is no basis for continuing DTx use by patients. Rather, the rate of continuity of DTx use is extremely low. While many conventional pharmacotherapies have undergone numerous verification and safety tests over a long time, barriers to the application of DTx in the medical field are lower than those for conventional pharmacotherapies. Considering these reasons, except for certain special cases, an approach to DTx is needed that complements the prescription of conventional pharmacotherapy by the medical staff. When DTx are prescribed by doctors who clearly know their advantages and disadvantages, the doctors' expertise may undergo further refinement, and the quality of medical care is expected to improve.
Keywords: Devices, Medicine, Patients, Physicians, Prescriptions
Graphical Abstract
INTRODUCTION
Digital therapeutics (DTx) has emerged as an important issue in the medical field in recent times.1,2 DTx essentially means using digital devices or software to treat specific diseases. The use of mobile applications, Internet, games, virtual reality, and so on, to diagnose the symptoms of patients and consequently treat them, as against diagnosis and treatment with traditional drugs or injections, is one of the characteristics of DTx.3,4,5 The world's first DTx is the mobile application “reSET®” produced by Pear Therapeutics in the United States.6 reSET® is approved by the Food and Drug Administration (FDA) to provide Cognitive Behavioral Therapy (CBT) for patients who are 18 years and older with drug addiction. The “Nunap Vision,” which treats visual impairment after brain injury, was first approved by the Ministry of Food and Drug Safety in Korea.7 In addition, there are many cases of DTx targeting various chronic diseases such as diabetes mellitus, obesity, epilepsy, or Parkinson's disease; here, therapeutic effects are expected through behavioral changes induced by DTx.8,9
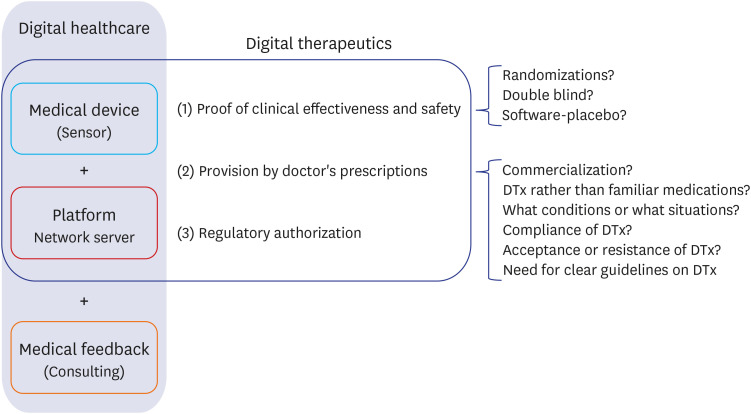
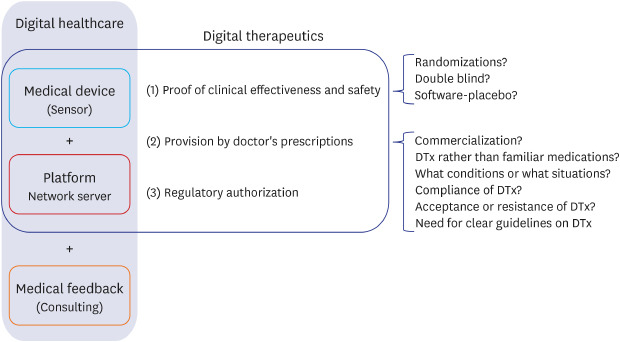
DTx, like traditional digital healthcare, can provide customized medical feedback based on medical data without the constraints of time and space.10 It is a smaller concept than traditional digital healthcare, focusing on clinical treatment based on clinical evidence. DTx, like drugs or other medical devices, must prove its effectiveness and safety through clinical trials.10 DTx is provided to patients through prescriptions from doctors.11 Due to this, DTx products require the approval of regulatory agencies, though this is not mandatory. DTx is transforming the wellness area of traditional digital healthcare into therapeutic areas of healthcare (Fig. 1).
Fig. 1. Digital healthcare and digital therapeutics.
DTx = digital therapeutics.
GENERAL CHARACTERISTICS OF DIGITAL THERAPEUTICS
Proof of clinical effectiveness
Although DTx must demonstrate effectiveness and safety through clinical trials, there are many other considerations to analyze the clinical effectiveness of DTx using traditional clinical research methods, unlike conventional pharmacotherapy.11 Given the nature of DTx, is it possible to make randomizations that are not realistically biased? (If patients who participate voluntarily in clinical trials are assigned to the control group, patient compliance will often drop rapidly during the study period. This will be a serious bias for the study.) Is a double blind possible? (Due to the nature of DTx, the control group and experimental groups are apparently divided by users and researchers.) If double-blinding is possible, what kind of software-placebo can we make? Or how should we make a software placebo? Should the effectiveness of DTx be compared to a simple placebo group or a conventional pharmacotherapy group?
In the future, various types of clinical research will be proposed to supplement this study. At this point, DTx should be developed not to compete with and replace existing drugs but to complement the existing ones for a certain period of time.12,13 reSET® has also been approved for supplementary use in existing conventional forms of treatments, rather than as a new treatment.6
Provision by doctor's prescription
Even though the existing digital healthcare has proved itself at a clinical level14,15 and demonstrated clinical effectiveness and safety in clinical studies, it has not been commercialized; thus, prescribing DTx to patients in clinical settings is another challenge.16
Before having doctors use DTx, the following questions should be considered: When a patient visits the hospital, are medical professionals expected to prescribe DTx rather than familiar medications? When the effect of a patient's continued medication is less effective, what kind of choice does the doctor make between increasing the dose of the drug (or changing to a new drug) or prescribing DTx? Is there any possibility that the golden treatment time will be delayed by prescribing DTx instead of prescribing medication? In what conditions will physicians prefer conventional pharmacotherapy, and in what situations will DTx be prescribed? Will there be proper compliance of DTx? Since the actual use of DTx is quite low,17,18,19 do we expect patients who visit hospitals to be willing to accept prescriptions or recommendations of DTx rather than prescriptions for drugs? Do we expect that there will be no resistance from patients to prescriptions for DTx rather than medications? Given these situations, do we expect doctors to actively prescribe DTx?
This is not just a matter of choosing conventional pharmacotherapy or DTx. Even if the effectiveness and safety of DTx is clear, it is still difficult to ensure that this is the best medical practice. Therefore, there is a need for clear guidelines on DTx before simple digital literacy.20
Regulatory authorization
Apart from establishing evidence through clinical trials, an official approval of a digital therapeutic agent is required to be officially recognized. Obtaining FDA approval is not a compulsory requirement, but it is a necessary step to gain the trust of patients and practicing physicians. Moreover, due to the nature of DTx, even if the developer does not receive FDA approval, clinical trials may have evinced its benefits; therefore, the developer may suggest its use for disease diagnosis and treatment. However, it is difficult to claim that it is an effective treatment for patients. A typical example is Sleepio™, the American app that claims to help customers achieve a good sleep cycle.21 Sleepio™ has established evidence from clinical trials, but has not received FDA approval. It cannot be clearly identified as sleep therapy, but the effect of improving sleep is suggested.
NOT WRONG, BUT EXAGGERATED CLAIMS
There is no doubt that DTx will play an important role in the medical field. However, from a healthcare practitioner's point of view, it needs to be approached more conservatively. This is because there are many impediments that must be addressed before a proper implementation of DTx in the medical field.16 Although there are both advantages and disadvantages compared to conventional pharmacotherapy, only the advantages have been highlighted in recent years. In order to make proper use of the new and unfamiliar DTx with patients, doctors must first understand its disadvantages (Table 1). Although DTx has advantages over conventional pharmacotherapy, this is limited to a few supportive roles.
Table 1. Refutations from the medical field against the advantages of digital therapeutics.
| Claims by some industries | Refutations from the medical field |
|---|---|
| DTx have significantly reduced development time and cost compared to conventional pharmacotherapy. | In the medical field where safety and effectiveness are important, just shortening the development time and cost is not an advantage. |
| DTx have few side-effects. | The adverse effects of DTx are not yet known and will be found out eventually. |
| DTx are capable of real-time collection and analysis of RWD. | While it is true that DTx are beneficial for the collection and analysis of RWD, they require new and distinct work for collecting and analyzing high-quality RWD. Naturally, this must be independently proved by scientific methods. |
| Patients are reluctant toward conventional pharmacotherapy. | Depending on the type of disease, it is not recommended to prescribe DTx even if the patient rejects conventional pharmacotherapy. Prescription of conventional pharmacotherapy is often necessary, and if the prescription of DTx is not adequate, the time for treatment may be missed. |
| In DTx, the patient collects and manages their data, so the patient is actively involved. | There is no basis for continuity of active participation. Rather, the continuity of DTx use is extremely low. |
| Once verified in clinical studies, DTx can be applied to the medical field and can be supplemented when problems arise. | While many conventional pharmacotherapies have undergone numerous verification and safety tests over a long period of time, barriers to the application of DTx in the medical field are relatively low. |
| Except for some cases, for the time being, an approach is needed that complements the prescription of conventional pharmacotherapy by medical staff. |
DTx = digital therapeutics, RWD = real-world data.
Patients are reluctant to be prescribed medications, so do they need digital therapeutics?
It is true that patients are hesitant to take medications or injections.22,23 In this case, of course, DTx will help as a therapeutic complement.12,13 However, the drug or medical intervention prescribed by doctors is the result of long, reliable clinical research, and is prescribed according to the standard guidelines. Should doctors prescribe DTx rather than drugs, simply because the patient resists taking medications? It is difficult to accept the simple claim that patients should be prescribed DTx only because they show resistance in taking medications.
For instance, suppose an obese patient comes to the hospital for a consultation. Generally, a patient visits a hospital for weight loss only when both diet and exercise have failed. For patients who want to be prescribed conventional pharmacotherapy, if the doctor prescribes DTx through diet/exercise-related applications instead, can we expect patients to be satisfied with the doctor's decision? It may be better for the patient to go to the local health gym and exercise rather than taking medicine. It is not preferable to expect that DTx will completely ensure patient compliance. In this case, the patient's resistance to the prescription of DTx will be more severe. If DTx helps patients diet/exercise well, coming to the hospital to get a prescription would seem redundant to the patients. However, it cannot be said that DTx is meaningless. The usage of DTx is an area that needs further knowledge. Exaggerated advertisement for DTx is a matter of concern. There is a belief in the medical industry that patients have high resistance to conventional pharmacotherapy than DTx. When a patient visits a hospital without a social consensus on DTx, the resistance to DTx prescriptions will also be high. Ultimately, if the timing of drug prescriptions is delayed, the appropriate treatment time may possibly be missed.
Do digital therapeutics have fewer side effects than conventional drugs?
As mentioned above, conventional pharmacotherapy is a reliable result of long-term, expensive and large-scale studies.24 The side-effects of DTx, due to its relatively short development time and low cost, are not yet known. Therefore, claims that there are few side-effects of DTx compared to conventional pharmacotherapy are, of course, unreliable.
In some cases, smoking cessation applications are provided to aid smoking cessation. Furthermore, to encourage continuous use, various fun elements are introduced. However, it is noted that this causes mobile phone addiction among smokers. To combat this problem, some companies offer mobile-phone-addiction-evasion applications to help patients escape from their addiction. These are misguided examples or attempts to independently treat only one part of healthcare without understanding the overall context. Conventional pharmacotherapy provides the appropriate dosage regimen obtained by numerous clinical trials, but there is no such guide regarding DTx. This is, of course, the reason why active participation by medical staff is necessary.25
Do digital therapeutics have the advantage of short development period and low cost compared to conventional pharmacotherapy?
In some industries, DTx are software-based, and they continue to emphasize that it is possible to develop a variety of DTx at relatively short time and low cost. However, it is worth considering more carefully whether the short production time and low cost are advantages of DTx. While many drugs or medical devices have undergone numerous validation and stability tests over time, it is true that the barriers to approval for DTx are perceived as relatively low compared to traditional drugs or medical devices.26 The reason for the long development period of traditional drugs and medical devices is, of course, to ensure safety.27 It can be said that for the sake of patient safety, detailed time and money should be invested in DTx development. It is irresponsible to think that a long development time and significant expenses are due to institutional shortcomings. It is a dangerous idea to first implement DTx within the medical field and then address problems should they arise. It has been pointed out that the overall propensity to allow DTx in medical fields can threaten the safety of some patients.28,29
Do digital therapeutics induce active participation of patients as compared to conventional drugs?
DTx emphasize the advantage of collecting and managing medical data in real time, but in reality, this is difficult to obtain. It also cannot be conclusively said that patients are actively involved in DTx, and are passive in conventional pharmacotherapy. In medical lore, simply taking the prescribed medication properly is an active act of the patient. Based on past digital healthcare experiences, it is difficult to ascertain the active participation of the patient. In fact, many studies have found negative trends regarding the sustainability of digital healthcare.30,31 The continued usage rate of specific DTx products has not exceeded 50% for more than a year. In terms of patient compliance, the intake of medicines appears to be higher than the use of DTx. After all, whether the patient's participation is active or passive depends on the kind of disease the patient has and the purpose of the treatment. Thus, it is an exaggeration to say that DTx can increase patient compliance and actively cure diseases.
CONCLUSIONS
It can be safely assumed that DTx will play an important role in medical fields eventually. The medical staff should accept this fact unequivocally. After all, DTx are tools used by healthcare professionals in medical practice. If this tool is accurate, useful, and has scientific evidence, it can be a powerful instrument for the healthcare industry. More detailed and precise medical practice will be possible if there is information on the specific tool to be used for particular diseases. It would be desirable to introduce DTx in the medical field as a complementary method to conventional pharmacotherapy.13 If there are limitations to existing conventional pharmacotherapy methods, or when rehabilitation is needed, or there is an unmet need for medical treatment, DTx can be an efficient instrument for the medical industry.
From the medical staff's point of view, there is still concern about the usage of DTx in the distant future. Science and medicine are both in stages of development, and the development of science will ultimately lead to the development of medicine. Eventually, the development of science and medicine will immensely contribute to the subspecialty of medicine. As DTx become more active in medical practice, the role of skilled medical staff must also change.
Medical practitioners should supervise the purpose of medical treatment by DTx, its process, and results. The reasonability and appropriateness of DTx should be considered based on its medical value. Depending on the nature of the medical practice, the physician must simultaneously supervise the usage of DTx, so that the medical practice using DTx can be applied realistically in the right direction.
Footnotes
Funding: This work was supported by the Technology Development Program (S2726209) funded by the Ministry of SMEs and Startups (MSS, Korea).
Disclosure: The author has no potential conflicts of interest to disclose.
References
- 1.Sverdlov O, van Dam J, Hannesdottir K, Thornton-Wells T. Digital therapeutics: an integral component of digital innovation in drug development. Clin Pharmacol Ther. 2018;104(1):72–80. doi: 10.1002/cpt.1036. [DOI] [PubMed] [Google Scholar]
- 2.Palanica A, Docktor MJ, Lieberman M, Fossat Y. The need for artificial intelligence in digital therapeutics. Digit Biomark. 2020;4(1):21–25. doi: 10.1159/000506861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nordyke RJ, Appelbaum K, Berman MA. Estimating the impact of novel digital therapeutics in type 2 diabetes and hypertension: health economic analysis. J Med Internet Res. 2019;21(10):e15814. doi: 10.2196/15814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dorsey ER, Okun MS, Bloem BR. Care, convenience, comfort, confidentiality, and contagion: the 5 C's that will shape the future of telemedicine. J Parkinsons Dis. 2020;10(3):893–897. doi: 10.3233/JPD-202109. [DOI] [PubMed] [Google Scholar]
- 5.Cho CH, Lee HJ. Could digital therapeutics be a game changer in psychiatry? Psychiatry Investig. 2019;16(2):97–98. doi: 10.30773/pi.2019.01.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirschtritt ME, Insel TR. Digital technologies in psychiatry: present and future. Focus Am Psychiatr Publ. 2018;16(3):251–258. doi: 10.1176/appi.focus.20180001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Choi MJ, Kim H, Nah HW, Kang DW. Digital therapeutics: emerging new therapy for neurologic deficits after stroke. J Stroke. 2019;21(3):242–258. doi: 10.5853/jos.2019.01963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaufman N. Digital therapeutics: leading the way to improved outcomes for people with diabetes. Diabetes Spectr. 2019;32(4):301–303. doi: 10.2337/ds19-0012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Afra P, Bruggers CS, Sweney M, Fagatele L, Alavi F, Greenwald M, et al. Mobile software as a medical device (SaMD) for the treatment of epilepsy: development of digital therapeutics comprising behavioral and music-based interventions for neurological disorders. Front Hum Neurosci. 2018;12:171. doi: 10.3389/fnhum.2018.00171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lougheed T. How “digital therapeutics” differ from traditional health and wellness apps. CMAJ. 2019;191(43):E1200–1. doi: 10.1503/cmaj.1095801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sharma A, Harrington RA, McClellan MB, Turakhia MP, Eapen ZJ, Steinhubl S, et al. Using digital health technology to better generate evidence and deliver evidence-based care. J Am Coll Cardiol. 2018;71(23):2680–2690. doi: 10.1016/j.jacc.2018.03.523. [DOI] [PubMed] [Google Scholar]
- 12.Powell J. Trust me, I'm a chatbot: how artificial intelligence in health care fails the turing test. J Med Internet Res. 2019;21(10):e16222. doi: 10.2196/16222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim HS. Decision-making in artificial intelligence: is it always correct? J Korean Med Sci. 2020;35(1):e1. doi: 10.3346/jkms.2020.35.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim HS, Sun C, Yang SJ, Sun L, Li F, Choi IY, et al. Randomized, open-label, parallel group study to evaluate the effect of internet-based glucose management system on subject with diabetes in China. Telemed J E Health. 2016;22(8):666–674. doi: 10.1089/tmj.2015.0170. [DOI] [PubMed] [Google Scholar]
- 15.Kim HS, Yang SJ, Jeong YJ, Kim YE, Hong SW, Cho JH. Satisfaction survey on information technology-based glucose monitoring system targeting diabetes mellitus in private local clinics in Korea. Diabetes Metab J. 2017;41(3):213–222. doi: 10.4093/dmj.2017.41.3.213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim HS, Kim H, Lee S, Lee KH, Kim JH. Current clinical status of telehealth in Korea: categories, scientific basis, and obstacles. Healthc Inform Res. 2015;21(4):244–250. doi: 10.4258/hir.2015.21.4.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Maeder A, Poultney N, Morgan G, Lippiatt R. Patient compliance in home-based self-care telehealth projects. J Telemed Telecare. 2015;21(8):439–442. doi: 10.1177/1357633X15612382. [DOI] [PubMed] [Google Scholar]
- 18.Kim HS, Choi W, Baek EK, Kim YA, Yang SJ, Choi IY, et al. Efficacy of the smartphone-based glucose management application stratified by user satisfaction. Diabetes Metab J. 2014;38(3):204–210. doi: 10.4093/dmj.2014.38.3.204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Blakey JD, Bender BG, Dima AL, Weinman J, Safioti G, Costello RW. Digital technologies and adherence in respiratory diseases: the road ahead. Eur Respir J. 2018;52(5):1801147. doi: 10.1183/13993003.01147-2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dunn P, Hazzard E. Technology approaches to digital health literacy. Int J Cardiol. 2019;293:294–296. doi: 10.1016/j.ijcard.2019.06.039. [DOI] [PubMed] [Google Scholar]
- 21.Elison S, Ward J, Williams C, Espie C, Davies G, Dugdale S, et al. Feasibility of a UK community-based, eTherapy mental health service in Greater Manchester: repeated-measures and between-groups study of ‘Living Life to the Full Interactive’, ‘Sleepio’ and ‘Breaking Free Online’ at ‘Self Help Services’. BMJ Open. 2017;7(7):e016392. doi: 10.1136/bmjopen-2017-016392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Villalva CM, Alvarez-Muiño XL, Mondelo TG, Fachado AA, Fernández JC. Adherence to treatment in hypertension. Adv Exp Med Biol. 2017;956:129–147. doi: 10.1007/5584_2016_77. [DOI] [PubMed] [Google Scholar]
- 23.Shahiwala A. Formulation approaches in enhancement of patient compliance to oral drug therapy. Expert Opin Drug Deliv. 2011;8(11):1521–1529. doi: 10.1517/17425247.2011.628311. [DOI] [PubMed] [Google Scholar]
- 24.Paul SM, Mytelka DS, Dunwiddie CT, Persinger CC, Munos BH, Lindborg SR, et al. How to improve R&D productivity: the pharmaceutical industry's grand challenge. Nat Rev Drug Discov. 2010;9(3):203–214. doi: 10.1038/nrd3078. [DOI] [PubMed] [Google Scholar]
- 25.Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab (Seoul) 2019;34(4):349–354. doi: 10.3803/EnM.2019.34.4.349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Park SH, Han K. Methodologic guide for evaluating clinical performance and effect of artificial intelligence technology for medical diagnosis and prediction. Radiology. 2018;286(3):800–809. doi: 10.1148/radiol.2017171920. [DOI] [PubMed] [Google Scholar]
- 27.Wax PM. Elixirs, diluents, and the passage of the 1938 Federal Food, Drug and Cosmetic Act. Ann Intern Med. 1995;122(6):456–461. doi: 10.7326/0003-4819-122-6-199503150-00009. [DOI] [PubMed] [Google Scholar]
- 28.Park SH, Do KH, Choi JI, Sim JS, Yang DM, Eo H, et al. Principles for evaluating the clinical implementation of novel digital healthcare devices. J Korean Med Assoc. 2018;61(12):765–775. [Google Scholar]
- 29.Park SH, Kressel HY. Connecting technological innovation in artificial intelligence to real-world medical practice through rigorous clinical validation: what peer-reviewed medical journals could do. J Korean Med Sci. 2018;33(22):e152. doi: 10.3346/jkms.2018.33.e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hermsen S, Moons J, Kerkhof P, Wiekens C, De Groot M. Determinants for sustained use of an activity tracker: observational study. JMIR Mhealth Uhealth. 2017;5(10):e164. doi: 10.2196/mhealth.7311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thorup C, Hansen J, Grønkjær M, Andreasen JJ, Nielsen G, Sørensen EE, et al. Cardiac patients' walking activity determined by a step counter in cardiac telerehabilitation: data from the intervention arm of a randomized controlled trial. J Med Internet Res. 2016;18(4):e69. doi: 10.2196/jmir.5191. [DOI] [PMC free article] [PubMed] [Google Scholar]