Abstract
Inflammatory myofibroblastic tumor (IMT) is a rare mesenchymal tumor usually seen within the first and second decade. They are extremely rare in adults, constituting less than 1% of adult lung tumors. It's usually benign, but it had a tendency for local recurrence.
We report a case of asymptomatic inflammatory myofibroblastic tumor of lung in a 46-year-old non-smoker woman.
Keywords: Inflammatory myofibroblastic tumor, Inflammatory pseudotumor, Mesenchym.al neoplasms, Lung tumor, Surgery, Wedge resection
1. Introduction
Inflammatory myofibroblastic tumor (IMT) is a rare mesenchymal tumor usually seen within the first and second decade [1,2].They are extremely rare in adults, constituting less than 1% of adult lung tumors [1]. This tumor also known as plasma cell granuloma or inflammatory pseudotumor, used to be classified as a benign tumor [2,3]. However, it had a tendency for local recurrence.
Therefore, many recent study classified this tumor as an « intermediate malignancy » tumor [4]. IMT has been reported to occur in multiples anatomic sides which most commonly are lung, mesentery and omentum [5]. The treatment of choice is a complete surgical resection to exclude malignancy and to achieve a good prognosis [1]. We report a case of pulmonary inflammatory myofibroblastic tumor and review the literature related to demographical, clinical, biological characteristics as well as treatment efficacy of this tumor.
2. Case report
46-year-old non-smoker woman presented to chest department for incidental discovery of a suspected radiological opacity.
The patient had a history of systemic lupus erythematosus with joint and skin manifestations stabilized by plaquenil for 2 years. She had also a history of allergic asthma controlled by inhaled corticosteroid low doses.
The patient was asymptomatic. The clinical examination was normal.
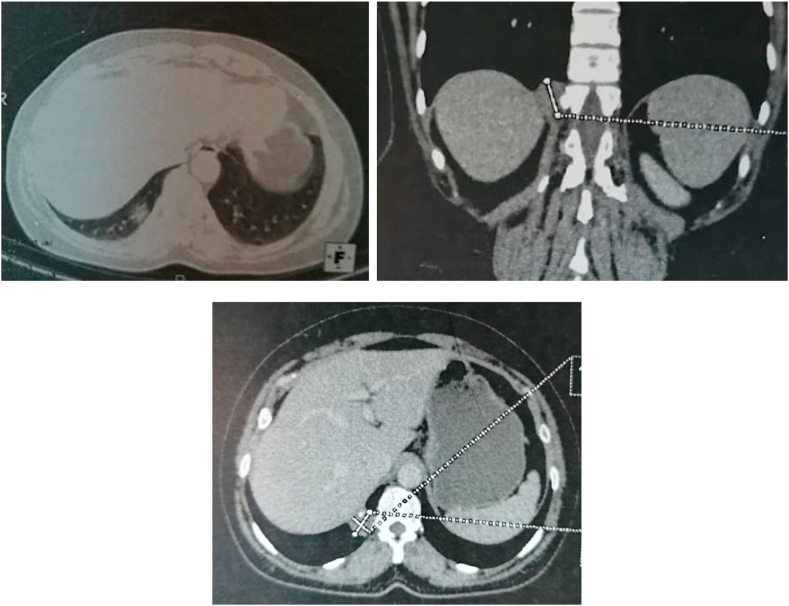
Chest computed tomography (CT) showed a solitary nodule of right posterobasal segment, measuring 2 cm long axis with eccentric calcifications and without lymph node (Fig. 1). This nodule was highly suspicious of malignancy.
Fig. 1.
CT chest scan: A solitary nodule of posterobasal segment of the right lower lobe measuring 2 cm long axis with eccentric calcifications.
Pet Scan was not performed for unavailability.
Bronchoscopy did not objectify a suspicious lesion and microscopy, culture and cytological examination of bronchial fluid were almost normal.
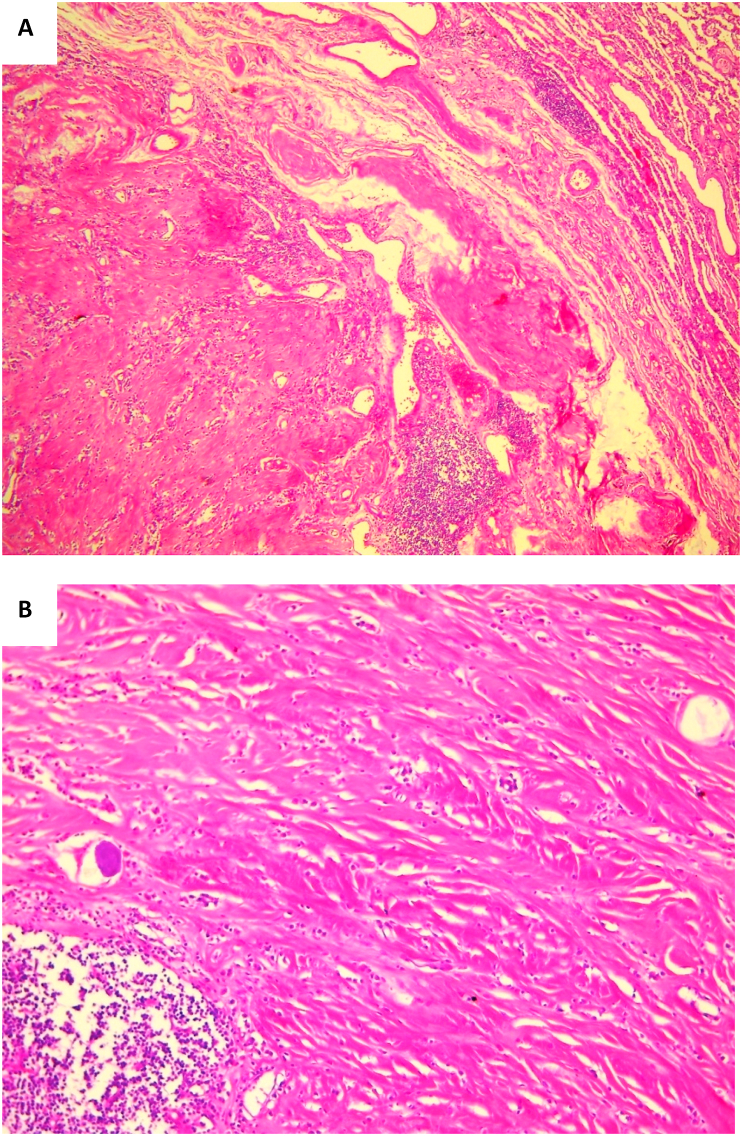
Surgery was carried out to obtain a diagnosis and achieve cure. Wedge resection was performed, and histological examination revealed the diagnosis of an inflammatory myofibroblastic tumor of the lung (Fig. 2).
Fig. 2.
Lung tissue shows a pauci-cellular tumor on a fibrous background with calcification. Spindle cells show minimal cytological atypia admixed with chronic inflammatory infiltrate composed of lymphocytes and plasma cells. (A: HEx40, B: HEx100).
At the follow-up (14 months after operation), the patient was symptoms free and there was no evidence of tumor recurrence on chest CT scan.
3. Discussion
IMT of the lung are rare. Its exact incidence is unknown. In the literature, the incidence reported is <1% of all lung tumors [4,6]. There were first described in 1939 [2]. IMT occur at any age, but have a predilection for children and young adults [7].
They are not limited to the lung, but any site can be involved, such as the brain, liver, spleen, lymph nodes, salivary glands, breast, soft tissues and skin [2]. The most common locations are lung, abdominopelvic region and retro peritoneum. This tumor usually affects a single organ, but multiple locations are possible [3].
Diverse nomenclature has been applied to describe these lesions, including plasma cell granuloma, xanthogranuloma, inflammatory myofibroblastic proliferation, inflammatory pseudotumor, fibrous histiocytoma, plasma cell histiocytoma complex and inflammatory fibrosarcoma [3,8]. All these entities reflect the uncertainty of the true origin of IMTs [2].
Although IMTs show typically benign clinical behavior, malignant evolution has been described in the literature, including recurrent (between 2 and 25% of cases) and metastatic disease (less than 5% of cases) [4,6].
The clinical symptomatology of pulmonary IMTs is various and nonspecific [8]. In approximately 70% of cases, the disease is discovered coincidentally on imaging exams requested for other reasons [1]. Patients may manifest some symptoms such as cough, chest pain, and shortness of breath, hemoptysis, fever and fatigue. These manifestations depend on the size and location of the tumor [4,9].
Radiographic findings showed in approximately 90% of cases a solitary peripheral lung nodule. There is a predilection for lower lobes, peripheral lung parenchyma and subpleural locations [4]. On computed tomography, the lesion appears as a heterogeneous mass with variable contrast enhancement. Calcifications -such as seen in our patient-, cavitations and lymphadenopathy are rare [3]. In 5% of cases, lung IMTs can extend towards mediastinum, diaphragm, pleura or chest wall [8]. PET can be useful to distinguish benign IMT from malignant lesions [3].
The diagnosis of IMT is difficult to establish, and histologic examination of tissue is always required [10]. Fine needle aspiration biopsy and bronchoscopic samples are typically too small and insufficient for confident diagnosis [3]. Therefore, surgical excision of the lesion is the preferred diagnostic method [2].
Histologic examination showed a varying proportions of myofibroblastic cells, arranged in a myxoîd, fibrous or calcificated stroma associated to a chronic inflammation component including lymphocytes, plasma cells and eosinophils distributed to a variable degree throughout the tumor [11,12]. Three histological patterns have been described [4,13]. The first is myxoid and richly vascularized that has the appearance of nodular fasciitis or granulation tissue. The second pattern is a more densely spindle cell proliferation with focal nodular lymphoid hyperplasic resembling fibromatosis. The third type is that of a very sclera-hyalinized, slightly cellular stroma [4,13]. In this case, the histological pattern was hypocellular, densely collagenised and reminiscent of a fibrous scar.
Approximately, 50% of patients presents a cytogenetic translocation of the band chromosome 2p23 resulting in overexpression of ALK protein [4,14]. Recent studies demonstrated that these chromosomal abnormalities are correlated with tumor aggressiveness and local recurrence, and concluded that IMT is a true neoplasm rather than an inflammatory reactive lesion [12,15].
Complete surgical resection of the tumor is the treatment of choice [2,4]. Medical therapy such as chemotherapy, radiation and even corticosteroid therapy are recommended for patients with incomplete resection, multifocal disease, not resecable tumor or when surgery is contraindicated [3,16].
The prognosis depends on the quality of surgical resection and the tumor size [4,14]. After radical resection the prognosis is excellent [2,11]. Recurrent disease can occur even many years after the initial diagnosis. For this reason, patients should be followed closely after resection to detect local or distant recurrence [6].
4. Conclusion
Pulmonary inflammatory myofibroblastic tumor is a rare benign tumor. Clinical and radiological manifestations are non specific. Only histologic examination can confirm the diagnosis.
Despite the benign origin of IMTs, the risk of recurrence and distant metastasis require a complete surgical resection and prolonged follow-up.
Declaration of competing interest
The authors declare no conflict of interest.
References
- 1.Al-Obaidi A., Buess C., Mogire J., Reddy P.S. Inflammatory myofibroblastic tumor of the lung: an extremely rare condition in adults. Cureus. 2019;11(12):6432. doi: 10.7759/cureus.6432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marwah N., Bhutani N., Dahiya S., Sen R. Inflammatory pseudotumour: a rare tumor of lung. Ann Med Surg. 2018;36:106–109. doi: 10.1016/j.amsu.2018.10.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Na Y., Park S. Inflammatory myofibroblastic tumor of the pleura with adjacent chest wall invasion and metastasis to the kidney: a case report. J. Med. Case Rep. 2018;12 doi: 10.1186/s13256-018-1796-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sagar A.E.S., Jimenez C.A., Shannon V.R. Clinical and histopathologic correlates and management strategies for inflammatory myofibroblastic tumor of the lung. A case series and review of the literature. Med. Oncol. 2018;35 doi: 10.1007/s12032-018-1161-0. [DOI] [PubMed] [Google Scholar]
- 5.Mai S., Xiong G., Diao D., Wang W., Zhou Y., Cai R. Case report: crizotinib is effective in a patient with ROS1-rearranged pulmonary inflammatory myofibroblastic tumor. Lung Canc. 2019;128:101–104. doi: 10.1016/j.lungcan.2018.12.016. [DOI] [PubMed] [Google Scholar]
- 6.Tsuchiya T., Tanaka M. Pulmonary inflammatory myofibroblastic tumor: a case report. Asian Cardiovasc. Thorac. Ann. 2018;26:317–319. doi: 10.1177/0218492318770845. [DOI] [PubMed] [Google Scholar]
- 7.Surabhi V.R., Chua S., Patel R.P., Takahashi N., Lalwani N., Prasad S.R. Inflammatory myofibroblastic tumors. Radiol. Clin. 2016;54:553–563. doi: 10.1016/j.rcl.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Surabhi V.R., Chua S., Patel R.P., Takahashi N., Lalwani N., Prasad S.R. Inflammatory myofibroblastic tumors. Radiol. Clin. 2016;54:553–563. doi: 10.1016/j.rcl.2015.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Elmadi A., Rami M., Khattala K., Chater L., Harmouch T., Atmani S. Pseudotumeur inflammatoire pulmonaire chez un enfant. J. Pediatr. Pueric. 2011;24:69–71. [Google Scholar]
- 10.Sachdev R., Mohapatra I., Goel S., Ahlawat K., Sharma N. Core biopsy diagnosis of alk positive inflammatory myofibroblastic tumor of lung: an interesting case. Turk. J. Pathol. 2018;36:173–177. doi: 10.5146/tjpath.2018.01446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chauhan R., Sodhi K., Nada R., Virk R., Mathew J. Pediatric inflammatory myofibroblastic tumor of the trachea: imaging spectrum and review of literature. Lung India. 2018;35:516. doi: 10.4103/lungindia.lungindia_405_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vázquez I., Sánchez-Font A., Curull V., Pijuan L. Inflammatory myofibroblastic tumor diagnosed by transbronchial needle aspiration. Arch. Bronconeumol. 2018;54:43–44. doi: 10.1016/j.arbres.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 13.Dermarkarian C.R., Patel K.R., Fuller M.Y., Bernini J.C., Chévez-Barrios P., Allen R.C. Inflammatory myofibroblastic tumor of the orbit in an 8-month old. Ophthalmic Plast. Reconstr. Surg. 2019:1. doi: 10.1097/IOP.0000000000001575. [DOI] [PubMed] [Google Scholar]
- 14.Peretti M., Radu D.M., Pfeuty K., Dujon A., Riquet M., Martinod E. Surgical resection of pulmonary inflammatory pseudotumors: long-term outcome. Asian Cardiovasc. Thorac. Ann. 2017;25:440–445. doi: 10.1177/0218492317716587. [DOI] [PubMed] [Google Scholar]
- 15.Ogata M., Hatachi Y., Ogata T., Satake H., Imai Y., Yasui H. Effectiveness of crizotinib for inflammatory myofibroblastic tumor with ALK mutation. Intern. Med. 2019;58:1029–1032. doi: 10.2169/internalmedicine.1640-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nair V.V., Singh K.K., Kathayanat J.T., Radhakrishnan R., Babu A., Thanathu Krishnan Nair J. Inflammatory myofibroblastic lung tumor with dysphagia in a 4-year-old child. Asian Cardiovasc. Thorac. Ann. 2017;25:653–655. doi: 10.1177/0218492317738672. [DOI] [PubMed] [Google Scholar]