Abstract
The food environment has been shown to influence dietary patterns, which ultimately affects nutrition-related diseases such as diabetes, obesity, and cardiovascular disease (CVD). Measures of food accessibility and socioeconomics were combined to develop the Food Environment Index (FEI), characterizing all U.S. counties between 2008–2016. Multi-level regression models showed that this index is significantly negatively associated with CVD death rates across the two time periods studied (20082010 and 2013–2016). The FEI may be a useful proxy for identifying differences in the food environment to inform future interventions.
Keywords: Food environment, cardiovascular disease, mortality, U.S. counties
1. Introduction
The food environment is linked to a host of health outcomes and health behaviors primarily through its influence on food consumption 1–3. Its impact can best be understood when studying the disease risks of those living in poorer food environments – characterized by a greater availability of unhealthy food outlets relative to healthy food outlets near consumers’ homes. These individuals are more likely to have diabetes and be obese compared to those that live in better food environments regardless of community income 4. They are also subject to poorer dietary patterns, which contribute to increased risk for noncommunicable diseases including cardiovascular disease (CVD), diabetes, and cancer 5.
While current measures of the food environment exist, they have key limitations and very specific uses. For example, there is an increase use of Geographic Information Systems (GIS) coupled with data on retail food establishments to help investigate food access and consumption patterns. However, these analyses are limited crucially by their assumption in that dietary patterns are primarily determined by proximity to food outlets 6. Another commonly used measure of the food environment is the Nutrition Environment Measure Survey (NEMS) which assesses food availability and access through store audits 7. However, this tool was only evaluated in a single large metropolitan area and may not be valid for use in different geographic areas 7.
Previous indices that sought to measure the food environment are also limited because they generally focus on only a few environmental measures8. In particular, much of the current literature use the Retail Food Environment Index (RFEI), which represents the ratio of unhealthful food stores to healthful food stores8,9. The RFEI is limited in a number of ways, including its reliance on supermarkets or produce vendors which results in undefined values in small communities without these food stores10. The Physical Food Environment Index (PFEI) modifies the RFEI by adding counts of fast food outlets and convenience stores, but still results in undefined values in 13% of communities10. Additionally, the RFEI and its modified alternatives remain measures of proportion that do not provide context of affordability or transportation access. The County Health Rankings & Roadmaps (CHR) program’s food environment index is a good start for measures at the county level and over time, but weights access to healthy foods and food insecurity as its only two food environment indicators 11.
A more robust index that considers more aspects of the food environment such as food assistance program participation, the number of different food stores and restaurants, and transportation access will provide a better understanding of the relationship between the food environment, its dimensions, and health. This article utilizes these data, among others, from national sources to make changes and improvements to an index describing a community’s food environment. As a result, this study develops a composite Food Environment Index (FEI) with consideration for the criticisms and reflections of prior food environment measures.
A further goal was to demonstrate the FEI’s association with cardiovascular disease (CVD) outcomes and compare the FEI to the CHR food environment index in its spatial distribution and its strength in associations with CVD outcomes.
2. Materials and Methods
As mentioned earlier, the food environment is a complex concept composed of multiple dimensions, but can be thought of as the affordability, convenience, preferences, and availability of food which will serve as our conceptual framework1. The measures considered in the construction of the FEI are based on these specified dimensions. Through confirmatory factor analysis (CFA), observed measures from the aforementioned databases were combined where 3 latent factors ultimately emerged. The details of the measures, latent factors, and construction of the FEI are detailed in the following section.
2.1. Data sources
County-level data (identified by county FIPS codes) were integrated from multiple databases including the United States Department of Agriculture (USDA) Food Environment Atlas, Atlas of Heart Disease and Stroke from the Centers for Disease Control and Prevention (CDC), and Health Rankings from County Health Rankings & Roadmaps (CHR) 11–13.
Compiled by the Economic Research Service of the United States Department of Agriculture (USDA), the Food Environment Atlas contains community characteristics, indicators of health, and food access 12. Community characteristics include and components of the built environment like food stores, which were collected over various years. Store types were identified and classified by the North American Industry Classification System (NAICS). From these data, the analysis used: number of grocery stores per 1,000 population, number of convenience stores per 1,000 population, number of SNAP stores per 1,000 population, and number of full-service restaurants per 1,000 population. Number of stores were per unit population were converted to store count per 100,000 people to help interpret subsequent analyses.
The health indicators used as covariates in the model described below include adult obesity prevalence rate and adult diabetes prevalence rate which were also obtained from the USDA Food Environment Atlas 12. Adult obesity rate is the estimate of the age-adjusted percentage of persons 20 years and older who are considered obese 12. Obesity is defined as an individual having a Body Mass Index (BMI) greater than or equal to 30 kg/m2. Adult diabetes rate is the estimate of the age-adjusted percentage of persons of 20 years and older with diabetes but excluding gestational diabetes 12. These USDA Food Environment Atlas data were collected for 2008 and 2013. Food access variables from the USDA Food Atlas include proportion of the total population who are SNAP eligible, percent of population without a car and low access to store, and percent of households that are food insecure or have very low food security. SNAP participants are those that receive SNAP (Supplemental Nutrition Assistance Program, or previously the Food Stamp Program) benefits in an average month. Low access to a store without a car was defined as the percentage of the population living more than 1 mile from a supermarket or large grocery store 12. Vehicle access was measured from an American Community Survey question that asked if respondents whether the household had access to a car 12. Food security was assessed based on food-insecure conditions such as being unable to afford balanced meals, limiting the size of meals because of insufficient financial resources, or being hungry due to insufficient financial resources 12. Very low food security is defined when food intake of one or more members was reduced and eating patterns disrupted during the year due to insufficient food or financial resources 12.
Additional health indicators used as covariates include physical inactivity, socioeconomic data, and healthcare access were obtained from County Health Rankings 11. Physical inactivity is the percentage of persons 20 years and older that report no leisure-time physical activity 11. Socioeconomic data include the percentage of the population that is unemployed and race-ethnicity data for the percentage of African-Americans, American Indians and Alaskan Natives, Asians, Native Hawaiians and other Pacific Islanders, Hispanics, and Non-Hispanic Whites in the population. Healthcare access indicators of uninsured rate, defined as the percentage of people under age 65 without insurance, and primary care physicians (PCP) rate, defined as the ratio of PCP to per 100,000 population. CHR data are compiled using county-level measures from a range of publicly available data sources to measure the health of all counties in the nation 11.
To study the association between CVD mortality and the food environment, CVD death rates were obtained from the Division for Heart Disease and Stroke of the CDC as the outcome measure of interest 13. The online mapping tool provided county-level visualization and data on heart disease over a 3-year time period. These county-level rates were generated only after 4 criteria were met: 1) At least 20 events occurred within the county and its adjacent neighbors OR at least 16 events occurred within the county OR at least 5,000 population years within the county; 2) At least 6 population years for each age group used for age adjustment if that age group had 1 or more events; 3) The number of population years in an age group was greater than the number of events; and, 4) At least 100 population years within the county 13. Total CVD death rate data was obtained for all ages for the 2008–2010 time range and the 2013–2015 time range to best match the variables from the Food Atlas because data was not uniformly available. Rates are reported as CVD deaths per 100,000 population.
After merging these data with corresponding timespans of Time Period 1 (2008–2010) or Time Period 2 (2013–2016), the complete variable list was finalized and is presented in Table 1, organized into measures of health outcomes, built environment, store access, and demographic characteristics.
Table 1.
Description of data and summary statistics.
| Variable | Time Period 1 (2008–2010) Mean (SD) |
Time Period 2 (2013–2016) Mean (SD) |
Data Source |
|---|---|---|---|
| CVD deaths per 100,000 population | 256.53 (75.07) | 239.20 (71.40) | CDC |
| Health outcomes | |||
| Obesity rate prevalence (%) | 28.9 (3.7) | 31.0 (4.5) | USDA Food Atlas |
| Diabetes rate prevalence (%) | 9.9 (2.1) | 11.2 (2.5) | USDA Food Atlas |
| Physical inactivity (%) | 28 (5) | 28 (5) | CHR |
| Built Environment (per 10,000) | |||
| Full-service restaurants | 7.8 (5.8) | 7.8 (5.9) | USDA Food Atlas |
| Grocery stores | 2.7 (2.3) | 2.5 (2.2) | USDA Food Atlas |
| Convenience stores | 6.0 (3.1) | 6.0 (3.1) | USDA Food Atlas |
| Farmers’ markets | 0.4 (0.7) | 0.6 (1.0) | USDA Food Atlas |
| SNAP-authorized stores | 8.8 (3.9) | 10.2 (4.5) | USDA Food Atlas |
| Access | |||
| No car and low access to store (%) | 3.2 (3.2) | 3.3 (3.2) | USDA Food Atlas |
| Household food insecurity (%) | 15.0 (2.4) | 14.3 (2.5) | USDA Food Atlas |
| Household very low food security (%) | 5.8 (0.9) | 5.7 (1.0) | USDA Food Atlas |
| Economic characteristics | |||
| SNAP participants (% of pop.) | 15.2 (3.6) | 13.3 (3.2) | USDA Food Atlas |
| Unemployment (%) | 9 (3) | 7 (2) | CHR |
| Race/ethnic composition | |||
| African-American (%) | 9.2 (14.4) | 8.9 (12.8) | CHR |
| American-Indian (%) | 2.1 (7.6) | 2.20 (6.4) | CHR |
| Asian (%) | 1.1 (2.4) | 1.4 (2.3) | CHR |
| Native Hawaiian/Other Pacific Islander (%) | 0.1 (0.9) | 0.1 (0.7) | CHR |
| Hispanic (%) | 8.0 (12.9) | 9.0 (11.9) | CHR |
| Non-Hispanic White (%) | 79.6 (19.8) | 77.1 (17.4) | CHR |
| Healthcare access | |||
| Uninsured rate (%) | 18 (6) | 18 (5) | CHR |
| PCP rate | 58 (45) | 55 (34) | CHR |
2.2. Constructing a Food Environment Index (FEI)
We used factor analysis to construct a Food Environment Index (FEI). Specifically, confirmatory factor analysis (CFA) was used over other data reduction methods because it is a top-down strategy that is driven by theory and is able to identify and confirm latent factors 14. CFA is a more appropriate method to validate the relationship strength between latent factors and observed measures because the acceptability of a specified CFA model is evaluated by goodness of fit 14,15.
In creating the FEI, observed measures were first used in a first order CFA to create latent factors of access (“Healthy Access” and “Unhealthy Access” in Figure 1) or socioeconomics (“Socioeconomics” in Figure 1). Second order CFA was then used to create the FEI itself which is composed of the latent factors created 16. Progressive model refinement was then used to achieve an acceptable fit, defined as having all factors that loaded significantly (p ≤ 0.05). Measures that did not load significantly were dropped from the model, including fast-food outlets.
Figure 1.
CFA structural model for creating the FEI with standardized factor loadings. Observed measures (rectangles) were used in first order CFA to create unobserved latent factors (circles), which were then taken to create the FEI (diamond) by second order CFA. εn represent error values associated with each observation.
First order factors were created by taking the mean of associated observed measures for each factor. As a result, the observable measures that make up each factor were equally weighted together. In total, three first order factors were created: Healthy Access, Unhealthy Access, and Socioeconomics. Unhealthy Access is composed of the number of SNAP stores per 10,000 population, the number of convenience stores per 10,000 population, and percentage of people with no car and low access. Healthy Access is composed of the number of grocery stores, farmer’s markets, and full-service restaurants per 10,000 population. Socioeconomics is composed of household food insecurity and very low food security, SNAP participants as a percentage of the total population, and the percentage of the population that is unemployed. These factors represent some of the underlying observations, or latent factors, that make up the food environment.
To address the varying scales of resulting factors, each factor was standardized to place them all on the same scale, or in terms of units of standard deviation. The scales of Unhealthy access and Socioeconomic were adjusted by transforming the range of values and changing their directionality for consistency across all factors. Interpretation for the resulting scales for all factors is that a higher value represents a better score, or a better food environment for a county to provide for simpler analysis.
The Pearson correlation between the three factors are as follows: Unhealthy Access and Healthy Access = −0.11; Healthy Access and Socioeconomics = 0.30; Unhealthy Access and Socioeconomics = 0.24, which show weak correlation between the factors.
Figure 1 shows the first and second order CFA models used to create the FEI. Standardized factor loadings, or regression coefficients, are shown on arrows connecting the FEI, latent factors, and observed measures to indicate correlation. Stronger relationships are indicated by a higher factor loading. The Food Environment Index factor variance was set to 1.000 to then estimate the factor loadings and residual variances in Figure 1.
Finally, the FEI was created by taking the mean of each first order factor (Healthy Access, Unhealthy Access, and Socioeconomics) with equal weights. The resulting FEI was transformed onto a 0 – 100 scale where 0 represents the poorest food environment and 100 represents the best food environment.
2.3. Data analysis
We used multilevel models to estimate the association between our developed FEI and CVD death rate in U.S. adults from 2008 to 2016, controlling for relevant confounders. FEI for each county-period was then used as the key exposure variable with CVD deaths per 100,000 population in 2008–2010 and 2013–2016 as a dependent variable. CVD poses the greatest public health burden in the U.S. as the leading cause of death, and this link between CVD and the food environment can help establish the validity of the FEI in its ability to predict CVD mortality rates17. Multilevel modeling (MLM) via mixed effects was used in Stata 15.1 to analyze how the FEI for each county affects CVD deaths per 100,000 population.
Three separate models were run for this analysis: a crude model, the fully adjusted model, and the fully adjusted model with state clustering. The hypothesis was that there will be an inverse relationship where a poor FEI score indicates a poorer food environment and thus a higher CVD mortality rate. The crude model was first run to provide a baseline for comparison before controlling for other variables. For the fully adjusted model, key covariates added include health indicators (rates of obesity, diabetes, and physical inactivity), race/ethnicity, and healthcare access indicators (uninsured rate and PCP rate). State clustering was considered for the final adjusted model to determine if there may be spatial dependence. In particular, this model aims to control for the potential relationship between the county and state. The overall goal of each model is to accurately predict the association between the FEI and CVD death rate.
An additional model was run in which each latent factor was used as covariates instead of FEI to determine the validity of each factor used. It was expected that as each factor increases, indicating an improving food environment, then CVD mortality rates would decrease. Resulting coefficients will therefore show how each latent factor is associated with CVD mortality rate while holding other confounders and latent factors constant. Therefore, results do not consider how these factors interact together and instead only show the crude association between each latent factor and CVD mortality rate.
3. Results
3.1. Comparisons with the CHR Food Environment Index
As mentioned earlier, the CHR food environment index uses only two indicators of the food environment: limited access to healthy foods and food insecurity. To compare our FEI to the CHR index, we scaled the CHR index by multiplying by 10 to convert the index from a 0–10 scale to a 0–100 scale. This change in scale is used to simplify the comparisons made between the two indices and will not impact the association trend that we are interested in.
Next, we conduct pairwise tests of correlation between the FEI at Time Period 2 and the CHR indices to determine how well aligned they are. The Pearson correlation coefficient of 0.431 (Table 2) between the two indices is statistically significant and indicates a positive, moderate linear relationship. The Spearman rho value of 0.4670 shows that there is a moderate monotonic relationship between the two indices, which is also statistically significant (Table 2). Finally, Kendall’s tau value of 0.3271 is statistically significant and indicates that the strength of dependence between the two indices is weak (Table 2).
Table 2.
FEI and CHR summary statistics and comparison tests
| Summary statistics | Mean | Standard deviation | 25th percentile | 50th percentile | 75th percentile | Interquartile range |
|---|---|---|---|---|---|---|
| FEI 1 (2008 – 2010) | 38.79 | 6.12 | 34.89 | 38.72 | 42.72 | 7.83 |
| FEI 2 (2013 – 2016) | 40.33 | 6.08 | 36.60 | 40.45 | 44.14 | 7.54 |
| CHR (2014 – 2016) | 71.32 | 12.43 | 65.24 | 73.42 | 79.57 | 14.33 |
| Correlation tests* | Coeff. | p-value | ||||
| Pearson’s r | 0.4341 | 0.0000 | ||||
| Spearman’s rho | 0.4670 | 0.0000 | ||||
| Kendall’s tau | 0.3271 | 0.0000 | ||||
Note:
denotes tests conducted between FEI Time Period 2 and CHR data
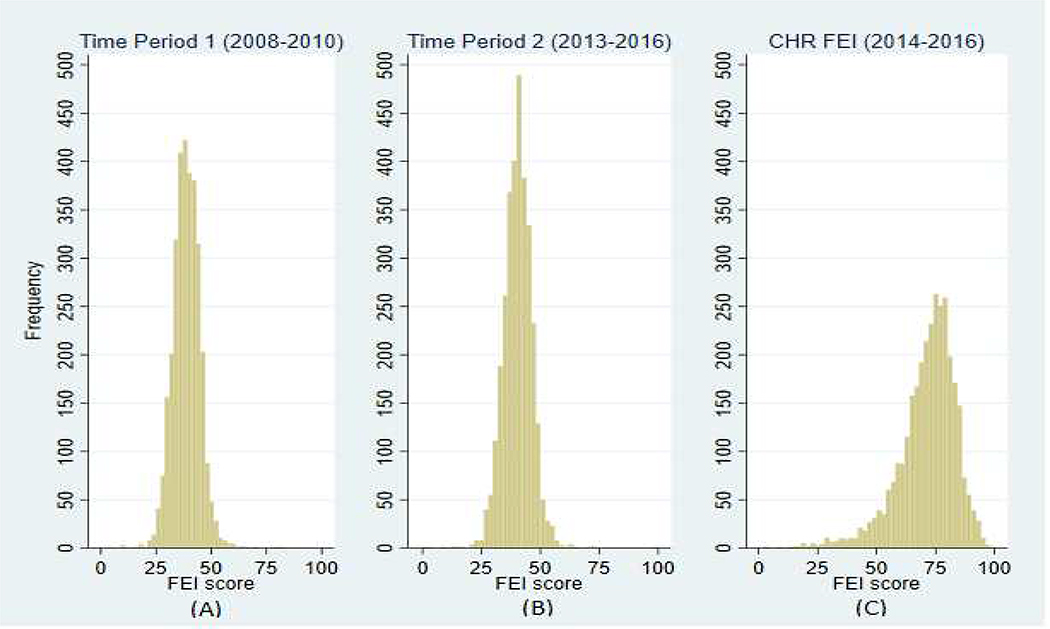
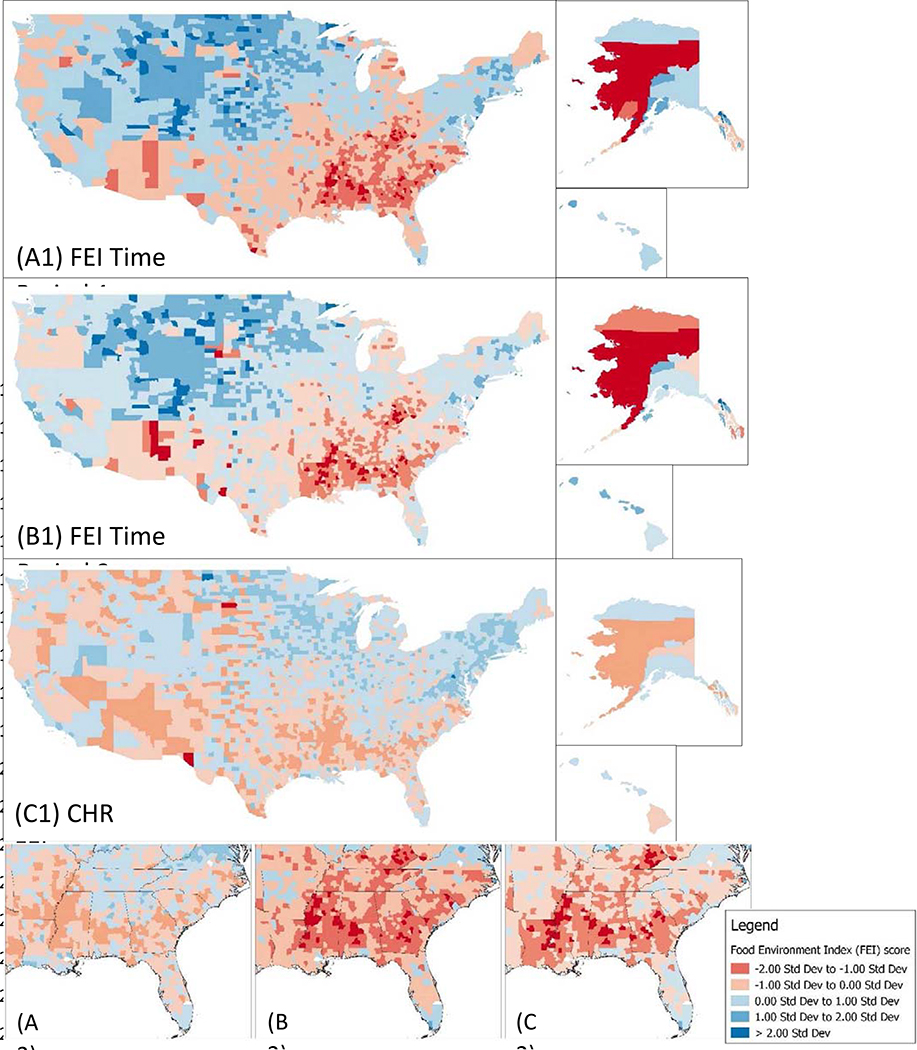
Table 2 shows that the mean for CHR data is higher than the means of both FEIs (out of a scale ranging from 0–100). Figure 2 shows the more normal distribution of FEI values for both time periods to reinforce that the CHR scores seem to be positively skewed. Figure 3 shows FEI values mapped for all U.S. counties which depict evident patterns in poor food environments in the southeast compared to the better food environments in the west and northeast. The skewed nature of the CHR data is also reflected on the map in Figure 3 which suggests that the newly developed FEI is better able to discern food environment conditions across the country when compared to the CHR measure. All maps were created using QGIS Version 2.18.23.
Figure 2.
Distribution of FEI values for (A) Time Period 1 (2008 – 2010), (B) Time Period 2 (2013 – 2016), (C) and CHR values (2014 – 2016).
Figure 3.
FEI scores of continental U.S., Alaska, and Hawaii (n = 3,141 counties) mapped for: (A1) Time Period 1 (2008 – 2010), (B1) Time Period 2 (2013 – 2016), (C1) and CHR values (2014 – 2016). A larger positive standard deviation implies a better food environment. Each of (A2), (B2), and (C2) show zoomed view of the American South to compare changes for each respective food environment index.
3.2. Association between FEI and CVD mortality
The results of the multi-level modeling (MLM) via mixed effects analysis are provided in Table 3. Analyses on the correlation between the FEI and CVD deaths per 100,000 population were conducted for all counties with available CVD data (n = 6,006). Overall, Table 2 shows that as the FEI score increases for a county, a decrease in CVD deaths per 100,000 population is predicted. The crude unadjusted model showed that a unit increase in FEI is associated with a decrease of 6.05 (z ≤ 0.05) CVD deaths per 100,000 population without any control variables. With the full adjustment set model, a one-point increase in FEI is associated with a decrease of 2.57 (z ≤ 0.05) CVD deaths per 100,000 population while holding time, race, health outcomes, and healthcare access constant. Likelihood ratio tests for both models were found to be significant (Prob>chibar2<0.05) to reaffirm the need for MLM.
Table 3.
Multilevel regression model via mixed effects estimating association between FEI and CVD by U.S. county (n = 6,006)
| Variable | Crude unadjusted model | Full adjusted model | Fully adjusted model with state clustering | Full model between latent factors |
|---|---|---|---|---|
| Coeff (Std Error) | Coeff (Std Error) | Coeff (Std Error) | Coeff (Std Error) | |
| FEI | −6.05 (0.12)*** | −2.57 (0.15)*** | −2.02 (0.19)*** | |
| Healthy Access | −5.15 (0.91)*** | |||
| Unhealthy Access ⫧ | −7.67 (0.86)*** | |||
| Socioeconomic | −5.66 (1.28)*** | |||
| Time | −15.21 (0.95)*** | −15.97 (0.98)*** | −16.71 (1.28)*** | |
| Diabetes (%) | 0.80 (0.40)* | 0.36 (0.42) | 0.22 (0.42) | |
| Obesity (%) | 0.13 (0.20) | 0.35 (0.21) | 0.44 (0.22)* | |
| Physically inactive (%) | 5.10 (0.20)*** | 5.07 (0.25)*** | 4.98 (0.25)*** | |
| African-American (%) | 0.52 (0.06)*** | 0.43 (0.07)*** | 0.42 (0.07)*** | |
| American Indian (%) | − 0.02 (0.10) | 0.19 (0.11) | 0.16 (0.11) | |
| Asian (%) | −0.56 (0.39) | −1.70 (0.41)*** | −1.56 (0.41)*** | |
| Pacific Islander (%) | 4.77 (2.15)* | 7.19 (2.49)*** | 6.88 (2.51)* | |
| Hispanic (%) Non-Hispanic White (%) | Referent | −0.10 (0.06) | −0.20 (0.07)*** | −0.20 (0.07)* |
| Uninsured rate (%) | 0.08 (0.12) | −0.29 (0.14)* | −0.35 (0.14)* | |
| PCP rate (%) | −0.00 (0.02) | 0.01 (0.02) | 0.01 (0.02) | |
| Constant | 493.99 (4.87)*** | 206.31 (10.48)*** | 190.40 (12.64)*** | 244.64 (17.18)*** |
| Variance of FIPS constant | 1448.51 (48.40)* | 1047.75 (37.04)* | 892.75 (33.32)* | 887.73 (33.35)* |
| Variance of State constant | --- | --- | 233.84 (56.16)* | 250.43 (60.63)* |
| Variance of residual | 771.73 (19.94)* | 637.95 (16.88)* | 634.03 (16.79)* | 635.04 (16.87)* |
| LR test statistic | 1645.39*** | 1343.28*** | 1623.66*** | 1613.57*** |
Notes:
denotes p-value < 0.05; * denotes 95% Confidence Interval does not contain null value 0
denotes p-value < 0.001. Negative values mean that a higher Health Access, Unhealthy Access, or Socioeconomic factor score is related to a better food environment.
Rescaled so that higher unhealthy access score denotes lower unhealthy access.
Because spatial dependence was shown for FIPS (Table 3), an additional model was also included to control for potential spatial dependence by state because neighboring groups (e.g. counties) tend to be more similar to each other than it otherwise would be. The “fully adjusted model with state clustering” therefore controls for spatial dependence by state as was also shown to be significant (Table 3). In this model, a unit increase in the FEI is associated with a 2.02 decrease in CVD deaths per 100,000 population while holding time, race, health outcomes, and healthcare access constant.
An additional model was run with each latent factor as covariates to compare how they perform against each other, which is shown in Table 3. Unhealthy Access (higher score denotes less unhealthy access) had the strongest association at a predicted decrease of 7.67 CVD deaths per 100,000 population. The associations between Healthy Access and Socioeconomic trended similarly where a one unit increase in these factors were associated with a 5.15 and 5.66 decrease in CVD deaths per 100,000, respectively. All associations were found to be statistically significant. These associations follow the FEI in that a better score or food environment factor is associated with decreased CVD mortality rates. We also conducted Ordinary Least Squares regression, which when compared to MLM, showed a much smaller association and thus reinforces the appropriateness of MLM for this analysis (results available upon request).
4. Discussion
Multilevel modeling was used to examine the relationship between the developed FEI value and CVD deaths per 100,000 population while controlling for time-county clustering, county-state clustering, race/ethnicity, health status, and healthcare access. In all of our models, a higher (better) FEI was found to be significantly negatively associated with CVD deaths. These findings follow previous research that has demonstrated how each component of the FEI is related to CVD or CVD risk factors. These include the positive associations between SNAP stores and limited food variety 18 and obesity 19, low access and poor diet quality 20, convenience stores and diabetes 21, low income and BMI 22 and negative associations between farmers’ markets and obesity23, full-service restaurants and diabetes rates 24, food insecurity and diet quality 25, and grocery stores and diabetes 24.
To provide context for the FEI and its association with CVD mortality rate, it should be emphasized that the standard deviation of FEI is about 6 units (Table 2). Therefore, a county that is one standard deviation below the average FEI is predicted to have about 12.12 more CVD deaths per 100,000 population. To provide an illustration, we can consider the state of North Carolina, where Vance county was shown to have one of the poorest food environments with a FEI score of 31.33 and an associated CVD death rate of 252.9 deaths per 100,000 population in Time Period 2. In contrast, Wake county was shown to have one of the best food environments with a FEI score of 42.99 and an associated CVD death rate of 177.2 deaths per 100,000 population in the same time frame. If Vance county’s FEI score increased by one standard deviation to 37.33, its CVD mortality rate would be predicted to decrease to 240.78 deaths per 100,000 population. Additionally, if Vance county’s FEI matched that of Wake, the predicted number of CVD deaths would further drop to 229.35 deaths per 100,000 population. The model therefore provides an estimate of the expected population health benefits that could occur by improving counties’ food environments, assuming all other relevant variables remain unchanged.
The final model run in Table 3 shows the varying strengths of associations among the latent factors: Unhealthy Access, Healthy Access, and Socioeconomic. The Unhealthy Access factor showed the strongest association with CVD mortality rate as it was associated with the largest decrease of 7.67 CVD deaths per 100,000 for a single unit increase in the factor. Overall, these results are consistent with the fully adjusted model with state clustering and suggests that future interventions to improve the food environment or CVD outcomes should prioritize limiting or restricting unhealthy food access (e.g., via zoning regulations). In other words, interventions should seek to decrease food outlets related to unhealthy access to affect the most change. However, it is important to remember that the food environment is made up of all the latent factors together and a county may be better served to focus on the other factors to improve the food environment. For example, the county of Chattahoochee has an FEI score lower than the average U.S. county, but its Unhealthy Access is above average. Its Healthy Access and Socioeconomic factors rank far below the average and should instead be the focus of future interventions. The FEI is necessary to identify areas of need while understanding the impact of each factor can help focus efforts in improving the food environment.
While the covariates used in the adjusted models are not our primary focus, they do provide some insights. For example, we see that the coefficient for time is large and negative, indicating a general time trend of lowering CVD mortality over time across the United States. However, the coefficients for proportion of African-Americans are consistently positive given other covariates in the model suggest that there are factors that contribute to CVD mortality in communities with higher African-American populations. A growing body of evidence suggest that chronic stress due to discrimination experienced by African-Americans and their communities may be a key factor which we are unable to account for in our models26. Additionally, even when the socioeconomic status of African-Americans are comparable to that of non-Hispanic whites, health outcomes are still poorer among African-Americans which further suggest deeper underlying factors. Some of these factors may include other aspects of the built environment such as advertisements for high-calorie foods or perceived safety of spaces for physical activity27.
Limitations of this study are noted as follows. Components used in the makeup of the FEI were equally weighted with each other under the assumption that each component contributes equally to the food environment. However, using a more empirically- or theory-driven justification for weighting may improve characterization of the food environment 28. Also, there may be important health-related differences in the food environment within counties. Therefore, using counties as the geographic unit for analysis may not be precise enough to accurately detect differences in the food environment related to CVD 29. The use of aggregate level data and a composite measure may also create ambiguity because associations cannot distinguish the cause for differences across areas 28,29. Food price measures, or other measures of affordability, were also not available consistently over time.
Despite these limitations, the study has a number of strengths, such as its use of a composite index which may help identify associations previously undetected when analyzing only its components 28. Another important strength of the study comes from the use of multilevel modeling via mixed effects, which considers spatial dependence to examine effects of geographical distribution 30. Neighboring geographic regions may have greater similarities to each other, which multilevel modeling can control for to provide a more accurate analysis of the associations among counties 31.
Studies of the food environment have commonly used geographical information system (GIS) software to predict consumption patterns based on the built environment 6. However, this approach is limited by its assumption that an individual’s proximity to food outlets are strong predictors of consumption patterns 6. Other key aspects of the food environment that are excluded in GIS-based analyses include food store type, transportation access, and affordability 1,6. The developed FEI improves upon other indices because it acknowledges the aforementioned deficits and supplements distance information with measures of accessibility and socioeconomics to better assess the food environment 32. Our index is shown here to be a stronger predictor of CVD mortality rate where the fully adjusted model with state clustering shows that 2.02 CVD deaths per 100,000 are associated with a one unit increase in FEI compared to the 0.74 for the CHR FEI.
While the usefulness of the FEI has been demonstrated through its association with CVD mortality rate, it is may be important to understand the potential mechanisms that may underlying this association. A community with a lower FEI score, or a poorer food environment, may have one or more of the following: higher availability of unhealthy foods, lower availability of healthy foods, less financial means to purchase higher quality foods, and limited transportation access. Together, these factors contribute to increased consumption of foods with excess salt, sugars, fat, and flavor additives which lead to obesity33. In the case of CVD risk, obesity plays a central role in the development of metabolic syndrome which includes diseases such as dyslipidemia, hypertension, and atherosclerosis34,35.
In terms of feasibility, the FEI is an important step towards characterizing and identifying food environments as it allows for universal comparisons of counties to each other, as if on a continuum. Our index improves upon previous indices by capturing more aspects of the food environment to provide a more robust understanding. Urban planners and policy makers alike could use the index to identify high-risk counties to direct intervention efforts for improving CVD-related outcomes 36. The development of the FEI can also initiate a larger discussion about how the food environment impacts health outcomes. Change in the FEI over time can also provide insight into how local policies may or may not be addressing highlighted issues. Additionally, its use of public access data that are periodically updated allows for the index to remain up to date and able to address changing environments. However, as a whole, our index only represents a broad measure of the food environment, but individual factors of the FEI can offer more precise measure. Another weakness that remains in using the FEI is the lack of data available for some counties, which makes it unable to accurately identify some areas of need.
Building upon these findings, future research must continue to explore what drives these associations between the food environment and CVD outcomes to better understand causal relationships and ultimately inform future interventions and policies 36. Although we only demonstrated the FEI’s association with CVD mortality here, there is also further room to investigate associations with other food environment-related health outcomes.
Highlights.
The Food Environment Index (FEI) characterizes food environments of U.S. counties
Our FEI improves prior indices by including additional food environment measures
We found higher association between our FEI and CVD mortality than prior indices
Our FEI may better identify counties with poor food environments for CVD prevention
Acknowledgments
Funding: NIH P2C HD050924 to CPC for center/facilities support, otherwise this research did not receive any specific grant for this research.
Footnotes
Declarations of interest: All authors have no declaration of interests to declare.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Herforth A, Ahmed S. The food environment, its effects on dietary consumption, and potential for measurement within agriculture-nutrition interventions. Food Secur. 2015;7(3):505–520. doi: 10.1007/s12571-015-0455-8 [DOI] [Google Scholar]
- 2.Powell LM, Zhao Z, Wang Y. Food prices and fruit and vegetable consumption among young American adults. Heal Place. 2009;15(4):1064–1070. doi: 10.1016/j.healthplace.2009.05.002 [DOI] [PubMed] [Google Scholar]
- 3.Zenk SN, Lachance LL, Schulz AJ, Mentz G, Kannan S, Ridella W. Neighborhood Retail Food Environment and Fruit and Vegetable Intake in a Multiethnic Urban Population. Am J Heal Promot. 2009;23(4):255–264. doi: 10.4278/ajhp.071204127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Babey SH, Diamant AL, Hastert TA, Harvey S. Designed for Disease: The Link Between Local Food Environmentsand Obesity and Diabetes. UCLA Cent Heal Policy Res. 2008. https://escholarship.org/uc/item/7sf9t5wx. [Google Scholar]
- 5.Cena H, Calder PC. Defining a Healthy Diet: Evidence for The Role of Contemporary Dietary Patterns in Health and Disease. Nutrients. 2020;12(2). doi: 10.3390/nu12020334 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lytle LA, Sokol RL. Measures of the food environment: A systematic review of the field, 2007–2015. Health Place. 2017;44:18–34. doi: 10.1016/j.healthplace.2016.12.007 [DOI] [PubMed] [Google Scholar]
- 7.Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in Stores (NEMS-S): Development and Evaluation. Am J Prev Med. 2007;32(4):282–289. doi: 10.1016/j.amepre.2006.12.019 [DOI] [PubMed] [Google Scholar]
- 8.Paquet C, Coffee NT, Haren MT, et al. Food environment, walkability, and public open spaces are associated with incident development of cardio-metabolic risk factors in a biomedical cohort. Health Place. 2014;28:173–176. [DOI] [PubMed] [Google Scholar]
- 9.Koleilat M, Whaley SE, Afifi AA, Estrada L, Harrison GG. Understanding the Relationship Between the Retail Food Environment Index and Early Childhood Obesity Among WIC Participants in Los Angeles County Using GeoDa. Online J Public Health Inform. 2012;4(1):ojphi.v4i1.3936. doi: 10.5210/ojphi.v4i1.3936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shier V, An R, Sturm R. Is there a robust relationship between neighbourhood food environment and childhood obesity in the USA? Public Health. 2012;126(9):723–730. doi: 10.1016/j.puhe.2012.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.County Health Rankings & Roadmaps. Health Rankings. http://www.countyhealthrankings.org/explore-health-rankings/rankings-data-documentation Published 2018.
- 12.USDA. Food Environment Atlas. https://www.ers.usda.gov/data-products/food-environment-atlas/go-to-the-atlas/ Published 2017. Accessed April 12, 2018.
- 13.CDC. Interactive Atlas of Heart Disease and Stroke. https://nccd.cdc.gov/DHDSPAtlas/?state=County&ol=[10] Published 2018.
- 14.Moore MT. Hoyle CFA Chapter - Final Running head : CONFIRMATORY FACTOR ANALYSIS Confirmatory Factor Analysis Brown Timothy A. and Moore Michael T. Correspondence concerning this chapter should be addressed to Timothy A. Brown, Center for Anxiety & Related Disor; 2014;(July 2012). [Google Scholar]
- 15.Brown TA. Confirmatory Factor Analysis for Applied Research. Guilford Publications; 2014. [Google Scholar]
- 16.Muthén LK, Muthén BO. Mplus: Statistical Analysis with Latent Variables: User’s Guide. Muthén & Muthén; Los Angeles; 2005. [Google Scholar]
- 17.Hunter DJ, Reddy KS. Noncommunicable Diseases. N Engl J Med. 2013;369(14):1336–1343. doi: 10.1056/NEJMra1109345 [DOI] [PubMed] [Google Scholar]
- 18.Racine EF, Delmelle E, Major E, Solomon CA. Accessibility Landscapes of Supplemental Nutrition Assistance Program−Authorized Stores. J Acad Nutr Diet. 2018;118(5):836–848. doi: 10.1016/j.jand.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 19.Leung CW, Villamor E. Is participation in food and income assistance programmes associated with obesity in California adults? Results from a state-wide survey. Public Health Nutr. 2011;14(4):645–652. doi:DOI: 10.1017/S1368980010002090 [DOI] [PubMed] [Google Scholar]
- 20.Bodor JN, Rose D, Farley TA, Swalm C, Scott SK. Neighbourhood fruit and vegetable availability and consumption: the role of small food stores in an urban environment. Public Health Nutr. 2008;11(4):413–420. doi:DOI: 10.1017/S1368980007000493 [DOI] [PubMed] [Google Scholar]
- 21.Alhasan DM, Eberth JM. An ecological analysis of food outlet density and prevalence of type II diabetes in South Carolina counties Biostatistics and methods. BMC Public Health. 2016;16(1). doi: 10.1186/s12889-015-2681-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Beydoun MA, Powell LM, Wang Y. The association of fast food, fruit and vegetable prices with dietary intakes among US adults: Is there modification by family income? Soc Sci Med. 2008;66(11):2218–2229. doi: 10.1016/j.socscimed.2008.01.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rahman T, Cushing RA, Jackson RJ. Contributions of Built Environment to Childhood Obesity. Mt Sinai J Med A J Transl Pers Med. 2011;78(1):49–57. doi: 10.1002/msj.20235 [DOI] [PubMed] [Google Scholar]
- 24.Frankenfeld CL, Leslie TF, Makara MA. Diabetes, obesity, and recommended fruit and vegetable consumption in relation to food environment sub-types: a cross-sectional analysis of Behavioral Risk Factor Surveillance System, United States Census, and food establishment data. BMC Public Health. 2015;15:491. doi: 10.1186/s12889-015-1819-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nackers LM, Appelhans BM. Food Insecurity Is Linked to a Food Environment Promoting Obesity in Households With Children. J Nutr Educ Behav. 2013;45(6):780–784. doi: 10.1016/j.jneb.2013.08.001 [DOI] [PubMed] [Google Scholar]
- 26.Brewer LC, Cooper LA. Race, discrimination, and cardiovascular disease. Virtual Mentor. 2014;16(6):270–274. doi: 10.1001/virtualmentor.2014.16.06.stas2-1406 [DOI] [PubMed] [Google Scholar]
- 27.CM R, Jia P, George H, et al. Cardiovascular Health in African Americans: A Scientific Statement From the American Heart Association. Circulation. 2017;136(21):e393–e423. doi: 10.1161/CIR.0000000000000534 [DOI] [PubMed] [Google Scholar]
- 28.Cebrecos A, Escobar F, Borrell LN, et al. A multicomponent method assessing healthy cardiovascular urban environments: The Heart Healthy Hoods Index. Health Place. 2019;55:111–119. doi: 10.1016/j.healthplace.2018.11.010 [DOI] [PubMed] [Google Scholar]
- 29.Diez Roux AV Investigating Neighborhood and Area Effects on Health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/AJPH.91.11.1783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Corrado L, Fingleton B. WHERE IS THE ECONOMICS IN SPATIAL ECONOMETRICS?*. J Reg Sci. 2012;52(2):210–239. doi: 10.1111/j.1467-9787.2011.00726.x [DOI] [Google Scholar]
- 31.Corrado L, Fingleton B. Multilevel modelling with spatial effects. Discuss Pap Econ No 11–05. 2011. [Google Scholar]
- 32.Caspi CE, Sorensen G, Subramanian SV, Kawachi I. The local food environment and diet: A systematic review. Health Place. 2012;18(5):1172–1187. doi: 10.1016/j.healthplace.2012.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hall KD. Did the Food Environment Cause the Obesity Epidemic? Obesity (Silver Spring). 2018;26(1):11–13. doi: 10.1002/oby.22073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cercato C, Fonseca FA. Cardiovascular risk and obesity. Diabetol Metab Syndr. 2019;11:74. doi: 10.1186/s13098-019-0468-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bruce KD, Hanson MA. The Developmental Origins, Mechanisms, and Implications of Metabolic Syndrome. J Nutr. 2010;140(3):648–652. doi: 10.3945/jn.109.111179 [DOI] [PubMed] [Google Scholar]
- 36.Green MA, Daras K, Davies A, Barr B, Singleton A. Developing an openly accessible multi-dimensional small area index of ‘Access to Healthy Assets and Hazards’ for Great Britain, 2016. Health Place. 2018;54:11–19. doi: 10.1016/j.healthplace.2018.08.019 [DOI] [PubMed] [Google Scholar]