Abstract
Purpose:
Quantify changes in sleep during the middle-to-high school transition and determine if changes in sleep differ by socio-demographic characteristics.
Methods:
Adolescents were enrolled in 8th grade and followed into 9th grade (N=110; 2,470 nights observed). The outcomes were actigraphy-estimated sleep duration, sleep onset, sleep offset and sleep sufficiency (≥8 hours of sleep). The exposures were school grade (8th or 9th), school night status (school or non-school), sex (female or male) and race (White, Black or Other).
Results:
On school nights, sleep duration declined by 25.8 minutes per night (P<0.001) from 8th to 9th grade. There was no change in sleep duration on non-school nights. Timing of sleep onset was 22.2 minutes later on school nights (P<0.001) and 17.4 minutes later on non-school nights (P<0.001) in 9th grade. Timing of sleep offset did not change on school mornings, but was 22.2 minutes later on non-school mornings (P<0.001) in 9th grade. The proportion of school nights (and non-school nights) with sleep duration ≥8 hours was 9.4% (38.3%) in 8th grade and 5.7% (35.9%) in 9th grade. The odds of sleeping ≥8 hours per night was 42% lower in 9th grade, compared to 8th grade (OR=0.58; 95% CI: 0.37, 0.91). Males were 59% less likely to sleep ≥8 hours per night. Black adolescents were 51% less likely to sleep ≥8 hours per night.
Conclusion:
Insufficient sleep is highly prevalent, especially on school nights and among male and Black adolescents, and this problem worsens with the transition to high school.
Keywords: Sleep, Adolescence, Disparities, Sex Differences, Actigraphy, Longitudinal
Introduction
The American Academy of Sleep Medicine recommends that adolescents sleep for 8–10 hours per day (1). Obtaining sufficient sleep is associated with less risky behavior (2) and with traits needed to achieve academic potential (e.g., memory) (3), develop pro-socially (e.g., emotional regulation) (4) and achieve healthier growth (e.g., obesity prevention) (5). Indeed, given the linkages between sleep and multiple aspects of adolescent development, sleeping sufficiently is one of the single most important factors for positive adolescent functioning. Ironically, as our knowledge of the benefits of sufficient sleep has accumulated, the time youth spend sleeping has declined (6).
The middle-to-high school transition is a particularly vulnerable period for insufficient sleep (7–11). The pubertal progression that typically occurs in this age range is associated with a preference for later sleep onset and wake times (12). This conflicts with potentially earlier high school start times, as well and increasing extracurricular activities and homework demands in high school that could delay bedtimes. Indeed, in the U.S. 47% of middle school students in 8th grade sleep ≥8 hours per night, but only 35% of 9th grade high school students do so (13, 14). However, these estimates are based on adolescent self-report, which overestimates sleep duration (15). Actigraphy has been used in cross-sectional studies to objectively estimate sleep duration in adolescents (16–21), but there are no studies that have objectively quantified changes in sleep during adolescence.
In addition, insufficient sleep is more problematic among certain socio-demographic groups. Prior cross-sectional observations using actigraphy have observed that adolescent males sleep night) and timing on school and non-school nights from 8th to 9th grade. We hypothesized that sleep duration and sufficiency would decline from 8th to 9th grade; timing of sleep onset would occur later; and timing of sleep offset would occur earlier on school mornings and later on non-school mornings. We also aimed to determine if changes in sleep patterns differed by sex, race, parent education and household income groups. We hypothesized that the following socio-demographic groups would have greater decreases in sleep duration from 8th to 9th grade: males (vs. females) (16, 17, 21); Black adolescents (vs. White adolescents) (16); adolescents from households with lower incomes (vs. adolescents from households with higher incomes); and adolescents whose parents have a lower education level (vs. adolescents whose parents have a higher education level) (20).
Methods
Sample
We analyzed data from the Sleep and Growth Study (S-Grow), a 1-year prospective observational study. We enrolled 118 adolescents in 8th grade of middle school (2016–2018) and completed follow-up assessments one year later in 9th grade of high school (2017–2019). All follow-up visits occurred at 12 months (±1 month). Participants were recruited in collaboration with the Children’s Hospital of Philadelphia’s (CHOP) Recruitment Enhancement Core. This core sent email and letter invitations to families who had received care within the CHOP network that covers the southeastern Pennsylvania and southern New Jersey regions. Our study was also advertised on the CHOP campus. Interested families completed a screening questionnaire by phone. Adolescents diagnosed with a medical or behavioral health condition that could have affected their physical growth or sleep (e.g., cancers; clinical sleep disorders; anxiety; depression) were excluded. Study visits took place in the Nutrition Core Lab at CHOP’s Center for Human Phenomic Science where participants were provided with an actigraphy device to allow for the estimation of sleep patterns in the home setting. Parents/guardians provided written informed consent and all adolescents provided their assent. All measurements were obtained during the fall or spring school terms. The study protocol was approved by the CHOP Institutional Review Board (IRB number: 15–011988).
Actigraphy
Participants wore an Actiwatch-2 (Philips Respironics) on their non-dominant wrist for 14 days in 8th grade and for 14 days in 9th grade. The Actiwatch-2 has been validated for sleep estimation in adolescents (26). Devices were initialized to start collecting data in 1-minute epochs at 08:00 on the day of the study visits. All devices were returned by mail. Rest periods were automatically detected using Actiware (v.6.0.8) with the medium wake threshold (27). We excluded actigraphy data collected before the device was given to participants and data collected after the study period ended (e.g., while in transit). We also removed overnight sleep periods with zero night awakenings and 100% sleep efficiency, which indicates the device was not worn. Participants kept a sleep diary to report bed and wake times, consistent with guidelines for actigraphy scoring (26, 28, 29). We followed an a priori scoring rule to review the data and consider making manual adjustments to the start and/or end times of the rest period when automatically generated rest periods were ±15 minutes different from the self-reported sleep diary (29). To ensure consistency in scoring, all manual adjustments were checked by a second reviewer and any disagreements were resolved by a third reviewer. Sunday through Thursday nights were considered school nights, and Friday and Saturday nights were considered non-school nights. School night sleep periods that ended on the morning of a Federal holiday were recoded as non-school nights. We corrected sleep periods impacted by daylight saving time in the spring and fall.
Sleep Duration, Timing and Quality Outcomes
We operationalized nighttime sleep duration as hours per night and we generated a sleep sufficiency variable to register if nights of sleep were <8 hours or ≥8 hours (1). The sleep timing variables (onset and offset) were operationalized as hours from midnight (e.g., −0.5 = 23:30; and 6.5 = 06:30). We included sleep quality metrics for sensitivity analyses: night awakenings (number of awakenings during the sleep period); sleep efficiency (percentage of time asleep during the sleep period); wake after sleep onset (time spent awake after the onset of sleep during the sleep period); and sleep onset latency (time taken to fall asleep in a sleep period). The following sleep quality metrics were not normally distributed and were categorized: sleep efficiency (<85% and ≥85%) (21) and tertiles for wake after sleep onset and sleep onset latency.
Socio-Demographic Predictors
Participants self-reported their sex (male or female) and their race and ethnicity using standard NIH categories. From the available race and ethnicity data collected, we categorized participants as White, Black and Other. The vast majority of participants reported being non-Hispanic (93%); due to the limited numbers we were not able to investigate Hispanic and non-Hispanic ethnicity. Household income data were collected with participants asked to report on of the following income brackets: <$10,000, $10,000-to-$19,999, …, $90,000-to-$99,999, or ≥$100,000. From the available parental household income data, we categorized participants as: <$40K, $40–69K, $70–99K and >$99K. The education level attained by the parent/guardian who accompanied the adolescent to the study visit was captured using the following categories: Did not complete high school; completed high school; technical school certificate; associate degree; some college, but no degree; bachelor degree or GED; or graduate degree. Based on available education data, we categorized as: some college or less, college degree and graduate degree.
Statistical Analyses
We analyzed our data at the daily level using mixed effect models to account for the multiple observations per individual, with maximum likelihood estimation, random intercepts, robust standard errors and an unstructured correlation matrix (linear mixed models for continuous outcomes and logistic mixed models for categorical outcomes). We described changes in each sleep outcome (duration, sufficiency, onset and offset) from 8th to 9th grade on school and non-school nights by including grade (coded 0 for 8th and 1 for 9th), school status (0 for school night and 1 for non-school night) and grade x school night interaction terms. We then tested whether individual demographic factors were associated with each sleep outcome, and further tested if any demographic factor association differed by grade or weekday status through interaction terms (demographic factor x grade and demographic factor x school night status). We used an alpha level of 0.05 to determine main associations and for the interactions we used a Bonferroni corrected alpha threshold to account for the number of interactions performed (0.05/16=0.0031). We performed sensitivity analyses to determine if the demographic factors associated with sleep quality traits (awakenings, efficiency, wake after sleep onset and sleep onset latency). All analyses were completed using Stata 14.2 (StataCorp, College Station, TX).
Results
We enrolled 118 adolescents in 8th grade. One participant dropped-out before completing their 8th grade lab visit and so we provided an Actiwatch-2 to 117 (Figure 1). After removing siblings to avoid correlation within families (N=3), we captured 1,398 nights of data from 107 participants in 8th grade [90% wear compliance; average number of wear days: 13.5 (SD=2.1)] (Figure 1). In 9th grade, 90 participants returned for their follow-up lab visit and all were provided with an Actiwatch-2 (Figure 1). We captured 1,072 nights of data from 84 participants in 9th grade [82% wear compliance; average number of wear days 13.1 (SD=2.3)]. Three participants did not provide actigraphy data in 8th grade, but were retained and provided actigraphy data in 9th grade (Figure 1). Therefore, our sample includes 110 participants (i.e., 107 participants with at least 8th grade Actiwatch-2 data plus 3 participants with only 9th grade Actiwatch-2 data). Household income data were not available for two participants, so the analytical sample is N=108 when household income is included in the model.
Figure 1.
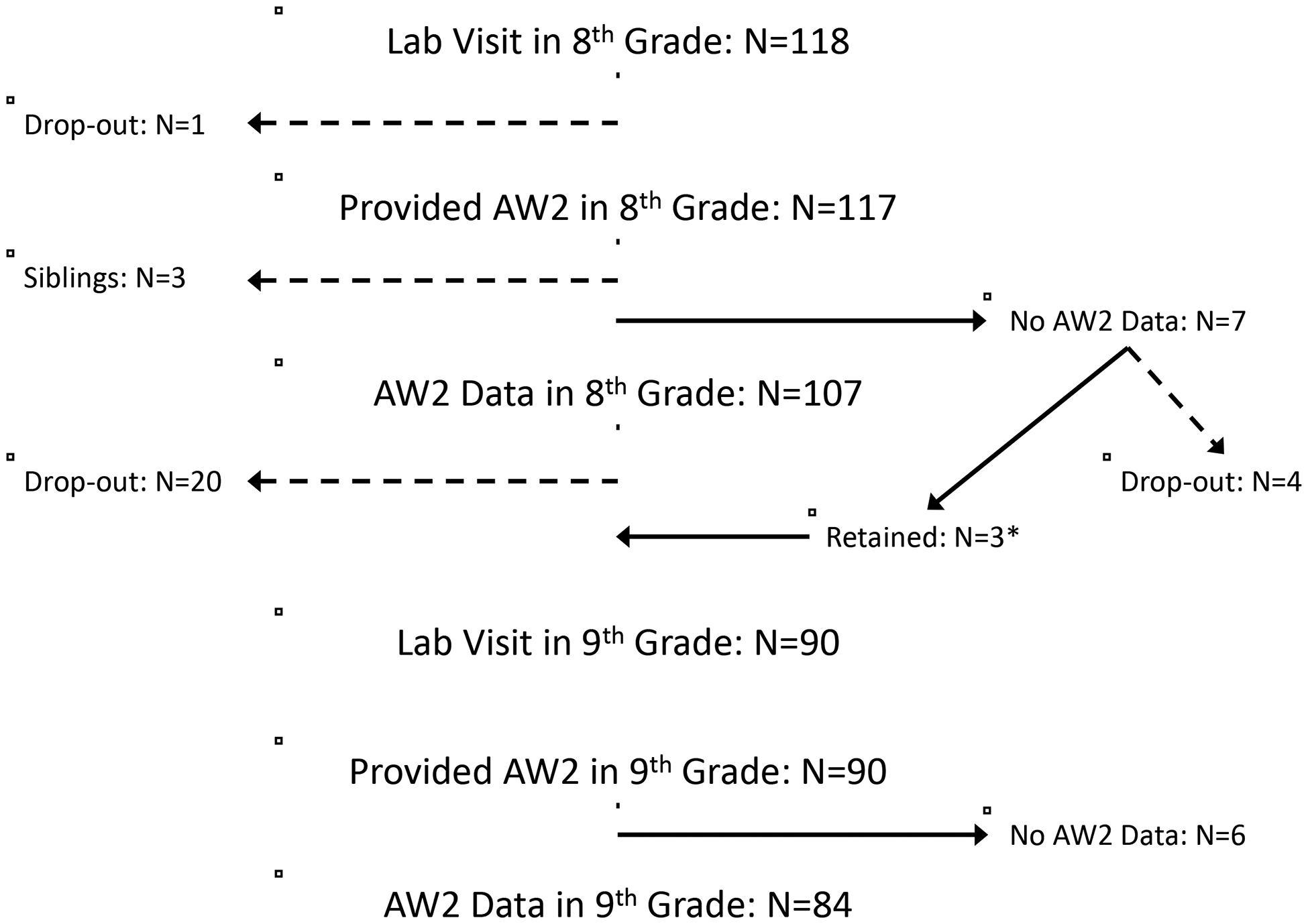
Enrollment, retention and actigraphy sleep data. Abbreviations: AW2, Actiwatch-2 (the actigraphy device used to objectively measure sleep patterns). *Three participants did not provide actigraphy data in 8th grade, but were retained and provided actigraphy data in 9th grade; therefore, the analytical sample includes 110 participants (i.e., 107 participants with at least 8th grade AW2 data plus 3 participants with only 9th grade AW2 data).
In 8th grade, approximately half the adolescents were female (53%), most were White (69%) and most lived in a household with an income ≥$99K per year (65%) (Table 1). The parents/guardians accompanying their adolescent had educational attainment that was approximately evenly distributed across the categories (Table 1). Black adolescents and adolescents from lower income households were more likely to have missing data (Supplementary Table 1) and be less compliant with the Actiwatch-2 protocol (Supplementary Table 2), so we adjusted for race and household income in all models. Descriptive statistics for sleep duration are provided by socio-demographic groups (Supplementary Table 3).
Table 1.
2013 Descriptive statistics for the analytical sample by study visit (8th and 9th grades)
| 8th Grade (N=107) | 9th Grade (N=84) | |
|---|---|---|
| Age, mean (SD), years | 13.9 (0.36) | 14.9 (0.36) |
| Female, N (%) | 57 (53.3) | 42 (50.0) |
| Male, N (%) | 50 (46.7) | 42 (50.0) |
| White, N (%) | 74 (69.2) | 65 (77.4) |
| Black, N (%) | 27 (25.2) | 14 (16.7) |
| Other, N (%) | 6 (5.6) | 5 (6.0) |
| Household Inc.: $<40,000, N (%) | 10 (9.5) | 5 (6.0) |
| Household Inc.: $40,000–69,999, N (%) | 16 (15.2) | 10 (11.9) |
| Household Inc.: $70,000–99,999, N (%) | 11 (10.5) | 11 (13.1) |
| Household Inc.: $>99,999, N (%) | 68 (64.8) | 58 (69.1) |
| Parent Educ.: Some College or Less, N (%) | 40 (37.4) | 27 (32.1) |
| Parent Educ.: College Degree, N (%) | 31 (29.0) | 29 (34.5) |
| Parent Educ.: Graduate Degree, N (%) | 36 (33.6) | 28 (33.3) |
| Leave for School, mean (SD), hours from 00:00 | 7.36 (0.41) | 7.01 (0.42) |
| Commute Time, mean (SD), minutes | 17.9 (18.0) | 21.3 (18.3) |
Abbreviations: Educ., education; Inc, income. Missing household income data in 8th grade (N=2).
In 8th grade, sleep duration averaged 6.72 hours on school nights and 7.50 hours on non-school nights (Figure 2). On school nights, sleep duration declined to 6.29 hours per night in 9th grade (25.8 minute decline; 95% CI: 17.4,34.2); on non-school nights there was no change in sleep duration (Figure 2). The percentage of school nights (and non-school nights) with sleep duration ≥8 hours was 9.4% (38.3%) in 8th grade and 5.7% (35.9%) in 9th grade. The odds of sleeping ≥8 hours per night was 7-fold higher on non-school nights compared to school nights (OR=7.68; 95% CI: 5.17,11.42), and was 42% lower in 9th grade, compared to 8th grade (OR=0.59; 95% CI: 0.37,0.93).
Figure 2.
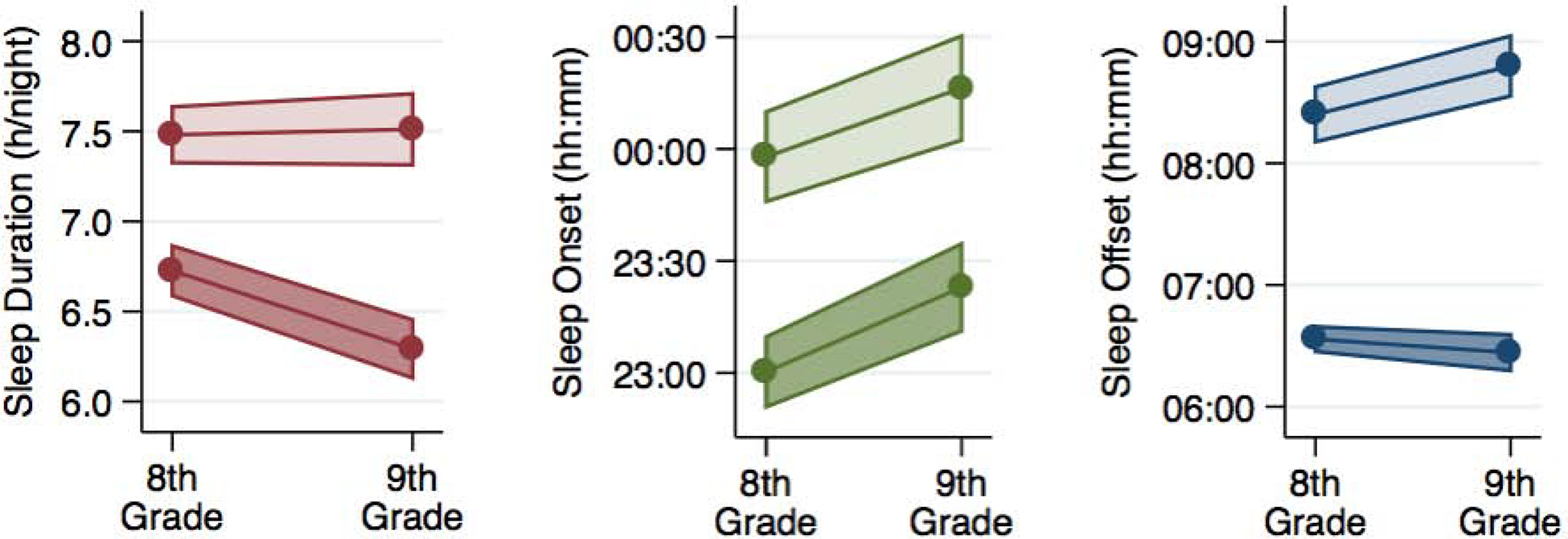
Sleep duration, onset and offset changes during the middle-to-high school transition (8th to 9th grade). The light shading represents non-school nights and the dark shading represents school nights.
In 8th grade, timing of sleep onset averaged 23:01 on school nights and 23:58 on non-school nights (Figure 2). Timing of sleep onset changed on school and non-school nights to be 22.2 minutes (95% CI: 12.6,31.8) and 17.4 minutes (95% CI: 4.8,30.0) later in 9th grade, respectively (Figure 2). In 8th grade, sleep offset averaged 6:34 on school mornings and 8:25 on non-school mornings (Figure 2). Change in sleep offset on school mornings was not statistically significant from 8th to 9th grade, but on non-school mornings sleep offset changed to occur 22.2 minutes later in 9th grade (95% CI: 9.6, 34.8; Figure 2).
Compared to females, males had shorter sleep duration [beta=−0.21(12 mins); 95% CI: −0.41,−0.02;] and were 59% less likely to sleep ≥8 hours per night (OR=0.41; 95% CI: 0.28,0.62) (Figure 3, panels A and B). We observed a sex by school night status interaction for sleep duration (Supplementary Figure 1); specifically, males slept for 0.69 fewer hours on non-school nights (41 mins; 95% CI: −1.00,−0.39) than females (Figure 3, panel E). There were no major sleep timing differences observed between males and females (Figure 3, panels C and D). Furthermore, the sex differences we observed were consistent in 8th and 9th grade (i.e., we did not detect sex by visit interactions, Supplementary Figure 1).
Figure 3.
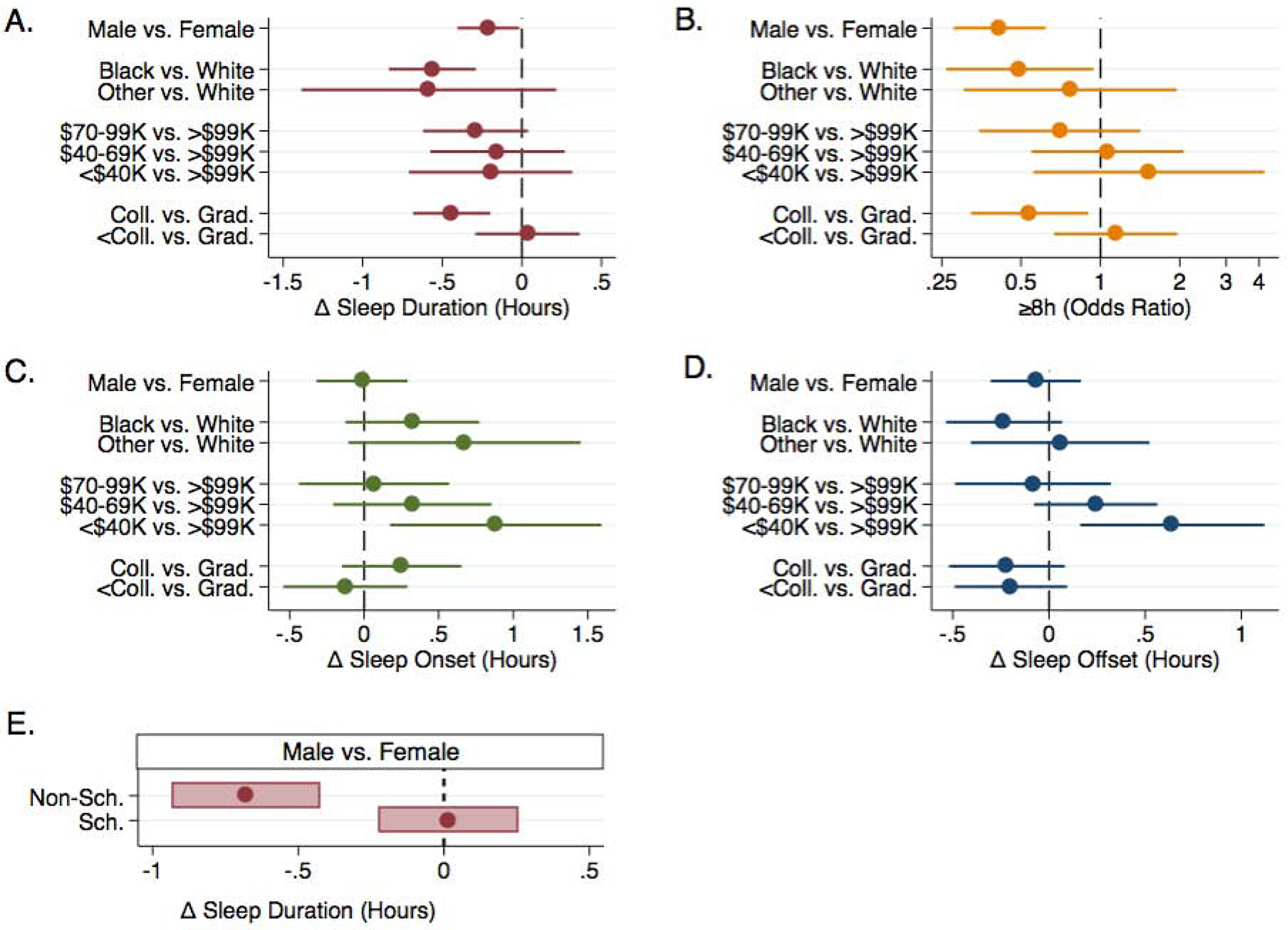
Demographic factor associations with the sleep outcomes. Main associations are presented in panels A (sleep duration), B (sleep sufficiency), C (sleep onset) and D (sleep offset). Delta (Δ): difference from the referent group for each demographic factor. Sex specific sleep duration associations on school and non-school nights are in panel E (based on significant sex x school night status interaction). The log-scale is used to present the odds ratios in panel B.
Compared to White adolescents, Black adolescents had shorter sleep duration [beta=−0.56 (33.6 mins); 95% CI: −0.84,−0.29] and were 51% less likely to sleep ≥8 hours per night (OR=0.49, 95% CI: 0.26,0.94) (Figure 3, panels A and B). There were no major sleep timing differences observed between White and Black adolescents, but the Black adolescents showed (non-significant) later timing of sleep onset and earlier timing of sleep offset (Figure 3, panels C and D). We did not observe sleep duration or timing differences between White adolescents and adolescents in the “Other” race group (Figure 3, panels A-D). We also did not observe any race interactions with grade or school night status (Supplementary Figure 1).
Adolescents living in households with <$40K annual income had later timing of both sleep onset [beta=0.88 (52.8 min); 95% CI: 0.17,1.59] and sleep offset [beta=0.64 (38.4 min); 95% CI: 0.16,1.12], compared to households with annual incomes >$99K (Figure 3, panel C and D). Compared to adolescents whose accompanying parent had a graduate degree, those accompanied by a parent with a college degree had shorter sleep duration [beta=−0.44 (26.4 mins); 95% CI: −0.68,−0.20] and were 46% less likely to sleep ≥8 hours per night (OR=0.54; 95% CI: 0.32,0.90) (Figure 3, panels A and B). There were no visit or school night interactions involving household income and parent education with respect to sleep duration or timing outcomes (Supplementary Figure 1).
In sensitivity analyses, males had more night awakenings (beta=2.66; 95% CI: 0.58,4.74), were less likely to have ≥85% sleep efficiency (OR=0.33; 95% CI: 0.21,0.54) and were more likely to have be higher wake after sleep onset (OR=2.66, 95% CI: 1.50,4.69), compared to females (Figure 4, panels A-C). We observed a sex x school night status interaction for night awakenings (Supplementary Figure 1); the awakenings sex difference was stronger on school nights (Figure 4, panel E). Adolescents from households with an income between $70–99K, compared to those from >$99K income households, were less likely to have ≥85% sleep efficiency (OR=0.29; 95% CI: 0.14,0.60) (Figure 4, panel B). We observed no differences in the sleep quality metrics across race and parental education groups (Figure 4).
Figure 4.
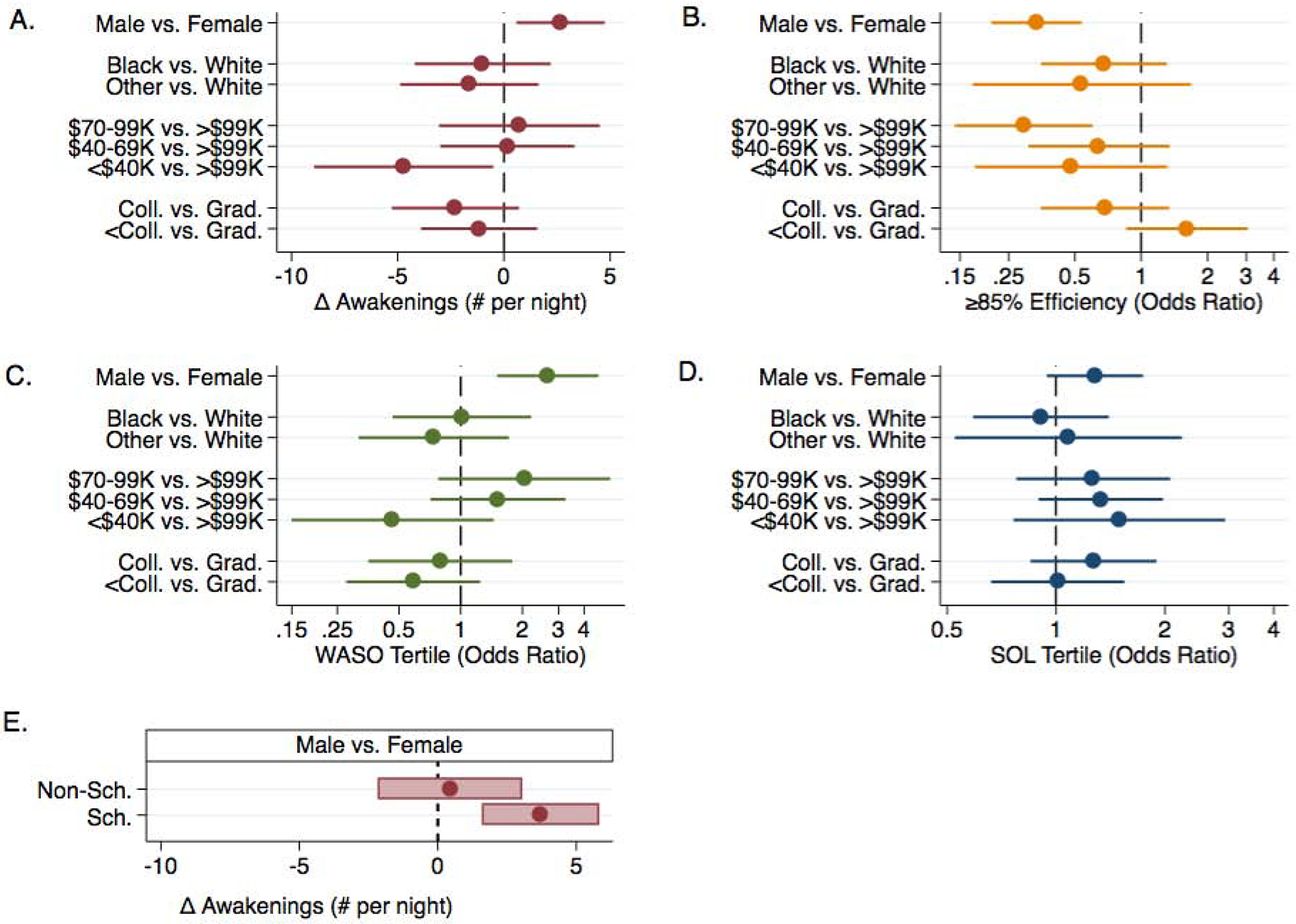
Demographic factor associations with the sleep quality outcomes. Main associations are presented in panels A (awakenings), B (efficiency), C (wake after sleep onset) and D (sleep onset latency). Delta (Δ): difference from the referent group for each demographic factor. Sex specific night awakenings associations on school and non-school nights are in panel E (based on significant sex x school night status interaction). The log-scale is used to present the odds ratios in panel B, C and D.
Discussion
Actigraphy estimated sleep duration and timing changed significantly during a key adolescent period: the middle-to-high school transition. In this one-year period, we observed a 25.8 minute per night reduction in average sleep duration on school nights (6.72 to 6.29 hours per night), largely due to a 22.2 minute later timing of sleep onset (23:01 to 23:24). We did not observe a reduction in average sleep duration on non-school nights because later timing of onset was compensated by later timing of sleep offset. The percentage of school nights (and non-school nights) with sleep duration ≥8 hours was 9.4% (and 38.3%) in 8th grade and 5.7% (and 35.9%) in 9th grade. Overall, the odds of sleeping ≥8 hours per night was reduced by 42% after transitioning to high school. In summary, our longitudinal study revealed that actigraphy-estimated insufficient sleep is highly prevalent in adolescence, especially on school nights, and this problem worsens as adolescents transition from middle-to-high school.
The Youth Risk Behavior Surveillance System (YRBSS) reported that 47% of 8th grade and 35% of 9th grade adolescents in the U.S. obtain sufficient sleep on school nights (13, 14). Our sample was recruited from the greater Philadelphia region and the YRBSS reported that the prevalence of sufficient sleep on school nights in Pennsylvania was 21.3% across all high school grades (and 16.6% within Philadelphia) (13). It is known that self-reported sleep duration estimates tend to be higher than actigraphy estimates (15), and this likely explains why we observed a lower percentage of sufficient sleep nights. Our estimated average sleep durations are similar to adolescent actigraphy data reported in other studies (16–21), but these studies did not report actigraphy-estimated sleep sufficiency for direct comparison. However, a study of younger children (10–11y) found that actigraphy estimates of sleep sufficiency were substantially lower than self-report estimates (2.5% vs. 51.3%) (30). Future surveillance studies using actigraphy will provide more accurate estimates of sleep duration. Current prevalence estimates are concerning, but the extent of insufficient sleep is likely more severe. Effective sleep extension strategies are urgently needed.
Delaying school start times to 08:30 can help address insufficient sleep among adolescents (31). Adolescents attending high schools with later start times sleep longer and have later timing of sleep offset (17). A delayed high school start time policy in Seattle, WA, from 07:50 to 08:45, increased actigraphy-estimated median sleep duration by 34 minutes per night (6.8–7.4 hours) as a consequence of a 44 minute later median timing of sleep offset (32). Delaying school start times is highly advantageous because it can reach almost all adolescents in a school district and the logistical changes are surmountable. However, delaying start times does not resolve insufficient sleep, nor does it result in earlier timing of sleep onset or target sleep duration on non-school nights. School education programs could additionally help, but sleep focused education programs show limited effectiveness and may be a necessary, but insufficient, component of a broader strategy (33–35). For example, school-based education programs for adolescent sleep promotion could be paired with both a delay in school start times and more intensive health behavior change efforts. This could include establishing family-school partnerships with pediatric healthcare providers to support bedtime routine regularity, reduction of bedroom electronics, and limiting caffeine intake.
The pediatric healthcare setting has a key role in helping to resolve insufficient sleep during adolescence. Pediatric sleep specialists already manage clinical and behavioral sleep disorders, including insufficient sleep, and increasing the number of providers and the quality of their training to promote sleep should be a priority (36, 37). A feasibility study found that families with an insufficient sleeping adolescent were open to meeting with a research team to set goals, problem solve, develop routines, learn about sleep hygiene best practices and receive positive feedback geared towards sleep promotion (38, 39). After two weeks, this approach increased actigraphy-estimated sleep duration by approximately 1 hour as a consequence of an approximate 1 hour earlier timing of sleep onset (39). The challenge is to translate this strategy into an intervention that remains effective, but is also scalable.
We observed sex, race and household income differences that suggest a need for tailored sleep promotion intervention approaches. Males slept less than females and had lower sleep quality, specifically on non-school nights. Whereas Black adolescents slept less that White adolescents, but sleep quality was similar across race groups. Additionally, adolescents from <$40K income households had later timing of sleep onset and offset compared to those from >$99K income households. These observations align with findings from prior studies that used actigraphy to estimate sleep in adolescents (16, 17, 21). Accordingly, it will be important to test if intervention strategies are equally effective for different sex, race and income groups. Indeed, delaying school start times, which provides longer opportunities for sleep on school nights, may have little impact on resolving the sex difference in sleep sufficiency, based on our observation that the sex differences were driven by non-school night sleep. In contrast, school start time delays could be effective for addressing the race difference in sleep sufficiency, if this school policy is adopted equally across all school districts. We also need to determine why these differences exist to help identify key targets for intervention (40). For example, lines of inquiry could investigate if social factors (e.g. parenting structure and family chaos) (22, 23), the bedroom environment (e.g., screen time in bed) (24, 25) or school level factors (e.g. homework) differ by sex, race and income groups to impact sleep patterns. We did not observe extensive differences in sleep patterns by parental education groups, but we only captured the education level of the parent accompanying their adolescent to their study visit.
Our study has strengths and limitations. We collected actigraphy data over 14 days in 8th and 9th grades and analyzed our data at the daily level. Comparable studies used cross-sectional designs, collected data over 7 days, and analyzed aggregated data (16). Our sample was predominantly White, non-Hispanic and most adolescents lived in higher-income households; we had limited ability to fully investigate race/ethnicity differences and differences across household incomes. We captured data in the final year of middle school and the first year of high school; we did not describe changes in sleep patterns throughout middle and high school. We also conducted our study at a single site in the U.S., in a region with a higher than average prevalence of insufficient sleep. Replication of our findings in other regions is needed. We excluded adolescents with clinical diagnoses that may impact sleep and/or growth, but it is possible that adolescents with undiagnosed disorders or subclinical symptoms were enrolled.
Conclusion
In conclusion, insufficient sleep is highly prevalent in adolescence, especially on school nights, and this problem worsens as adolescents transition from middle-to-high school. Male and Black adolescents are particularly susceptible to insufficient sleep. There is an urgent need for effective sleep health promotion interventions in addition to delaying school start times.
Supplementary Material
Supplemental Figure 1. Demographic factor interaction P-values with visit (top row) and weeknight status (bottom row). Panel A: Sleep duration and timing outcomes (red: sleep duration; orange: sleep sufficiency; green: sleep onset; blue: sleep offset). Panel B: Sleep quality outcomes (red: awakenings; orange: efficiency; green: wake after sleep onset; blue: sleep onset latency). The horizontal reference line represents the Bonferroni corrected P-value for a statistically significant interaction (0.05/16 = 0.0031).
Implications and Contribution.
Sleep is essential for adolescent development. This study used objective tracking of sleep to reveal that the extent of insufficient sleep in adolescence is more severe than previously indicated via self-report, especially among males and among Black adolescents. Interventions to promote sleep during the middle-to-high school transition are urgently needed.
Acknowledgements
We thank the families for volunteering to take part in this study. We appreciate the dedication of the research staff who helped to collect and manage the data. The study was supported by an NIH/NHLBI Career Development Award K01HL123612 and the following NIH/NCATS awards: UL1TR000003 and UL1TR001878. Ariel A. Williamson is supported by Eunice Kennedy Shriver National Institute of Child Health and Human Development Career Development Award K23HD094905 and by the Sleep Research Society Foundation. Struan Grant is supported by the Daniel B. Burke Endowed Chair for Diabetes Research.
Abbrivation:
- S-Grow
Sleep and Growth Study
- CHOP
Children’s Hospital of Philadelphia
- WASO
Wake After Sleep Onset
- SOL
Sleep Onset Latency
- YRBSS
Youth Risk Behavior Surveillance System
- Coll.
College
- Sch.
School
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest:
The authors have no conflicts of interests relevant to this article to disclose.
References
- [1].Paruthi S, Brooks LJ, D’Ambrosio C, et al. Consensus Statement of the American Academy of Sleep Medicine on the Recommended Amount of Sleep for Healthy Children: Methodology and Discussion. J Clin Sleep Med 2016;12:1549–1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Weaver MD, Barger LK, Malone SK, et al. Dose-Dependent Associations Between Sleep Duration and Unsafe Behaviors Among US High School Students. JAMA Pediatr 2018;172:1187–1189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Beebe DW, Field J, Milller MM, et al. Impact of Multi-Night Experimentally Induced Short Sleep on Adolescent Performance in a Simulated Classroom. Sleep 2017;40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Reddy R, Palmer CA, Jackson C, et al. Impact of sleep restriction versus idealized sleep on emotional experience, reactivity and regulation in healthy adolescents. J Sleep Res 2017;26:516–525. [DOI] [PubMed] [Google Scholar]
- [5].Miller MA, Kruisbrink M, Wallace J, et al. Sleep duration and incidence of obesity in infants, children, and adolescents: a systematic review and meta-analysis of prospective studies. Sleep 2018;41. [DOI] [PubMed] [Google Scholar]
- [6].Keyes KM, Maslowsky J, Hamilton A, et al. The great sleep recession: changes in sleep duration among US adolescents, 1991–2012. Pediatrics 2015;135:460–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Iglowstein I, Jenni OG, Molinari L, et al. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 2003;111:302–307. [DOI] [PubMed] [Google Scholar]
- [8].Leger D, Beck F, Richard JB, et al. Total sleep time severely drops during adolescence. PloS one 2012;7:e45204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Williams JA, Zimmerman FJ, Bell JF. Norms and trends of sleep time among US children and adolescents. JAMA Pediatr 2013;167:55–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Buxton OM, Chang AM, Spilsbury JC, et al. Sleep in the modern family: protective family routines for child and adolescent sleep. Sleep Health 2015;1:15–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Knell G, Durand CP, Kohl HW 3rd, et al. Prevalence and Likelihood of Meeting Sleep, Physical Activity, and Screen-Time Guidelines Among US Youth. JAMA Pediatr 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Carskadon MA, Acebo C, Jenni OG. Regulation of adolescent sleep: implications for behavior. Ann N Y Acad Sci 2004;1021:276–291. [DOI] [PubMed] [Google Scholar]
- [13].Wheaton AG, Jones SE, Cooper AC, et al. Short Sleep Duration Among Middle School and High School Students - United States, 2015. MMWR Morb Mortal Wkly Rep 2018;67:85–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Wheaton AG, Olsen EO, Miller GF, et al. Sleep Duration and Injury-Related Risk Behaviors Among High School Students--United States, 2007–2013. MMWR Morb Mortal Wkly Rep 2016;65:337–341. [DOI] [PubMed] [Google Scholar]
- [15].Nascimento-Ferreira MV, Collese TS, de Moraes AC, et al. Validity and reliability of sleep time questionnaires in children and adolescents: A systematic review and meta-analysis. Sleep Med Rev 2016;30:85–96. [DOI] [PubMed] [Google Scholar]
- [16].Matthews KA, Hall M, Dahl RE. Sleep in healthy black and white adolescents. Pediatrics 2014;133:e1189–1196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Nahmod NG, Lee S, Master L, et al. Later high school start times associated with longer actigraphic sleep duration in adolescents. Sleep 2019;42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Fobian AD, Avis K, Schwebel DC. Impact of Media Use on Adolescent Sleep Efficiency. J Dev Behav Pediatr 2016;37:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Harbard E, Allen NB, Trinder J, et al. What’s Keeping Teenagers Up? Prebedtime Behaviors and Actigraphy-Assessed Sleep Over School and Vacation. J Adolesc Health 2016;58:426–432. [DOI] [PubMed] [Google Scholar]
- [20].Marco CA, Wolfson AR, Sparling M, et al. Family socioeconomic status and sleep patterns of young adolescents. Behav Sleep Med 2011;10:70–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Cespedes Feliciano EM, Quante M, Rifas-Shiman SL, et al. Objective Sleep Characteristics and Cardiometabolic Health in Young Adolescents. Pediatrics 2018;142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Troxel WM, Lee L, Hall M, et al. Single-parent family structure and sleep problems in black and white adolescents. Sleep Med 2014;15:255–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Spilsbury JC, Patel SR, Morris N, et al. Household chaos and sleep-disturbing behavior of family members: results of a pilot study of African American early adolescents. Sleep Health 2017;3:84–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Falbe J, Davison KK, Franckle RL, et al. Sleep duration, restfulness, and screens in the sleep environment. Pediatrics 2015;135:e367–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Carter B, Rees P, Hale L, et al. Association Between Portable Screen-Based Media Device Access or Use and Sleep Outcomes: A Systematic Review and Meta-analysis. JAMA Pediatr 2016;170:1202–1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Meltzer LJ, Wong P, Biggs SN, et al. Validation of Actigraphy in Middle Childhood. Sleep 2016;39:1219–1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Meltzer LJ, Walsh CM, Traylor J, et al. Direct comparison of two new actigraphs and polysomnography in children and adolescents. Sleep 2012;35:159–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Acebo C, LeBourgeois MK. Actigraphy. Respir Care Clin N Am 2006;12:23–30, viii. [DOI] [PubMed] [Google Scholar]
- [29].Meltzer LJ, Westin AM. A comparison of actigraphy scoring rules used in pediatric research. Sleep Med 2011;12:793–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Gruber R, Somerville G, Wells S, et al. An actigraphic study of the sleep patterns of younger and older school-age children. Sleep Med 2018;47:117–125. [DOI] [PubMed] [Google Scholar]
- [31].Minges KE, Redeker NS. Delayed school start times and adolescent sleep: A systematic review of the experimental evidence. Sleep Med Rev 2016;28:86–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Dunster GP, de la Iglesia L, Ben-Hamo M, et al. Sleepmore in Seattle: Later school start times are associated with more sleep and better performance in high school students. Sci Adv 2018;4:eaau6200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Wing YK, Chan NY, Man Yu MW, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics 2015;135:e635–643. [DOI] [PubMed] [Google Scholar]
- [34].Rigney G, Blunden S, Maher C, et al. Can a school-based sleep education programme improve sleep knowledge, hygiene and behaviours using a randomised controlled trial. Sleep Med 2015;16:736–745. [DOI] [PubMed] [Google Scholar]
- [35].Gruber R, Somerville G, Finn C. School-based sleep health education in Canada. Sleep Med 2019;56:9–15. [DOI] [PubMed] [Google Scholar]
- [36].Faruqui F, Khubchandani J, Price JH, et al. Sleep disorders in children: a national assessment of primary care pediatrician practices and perceptions. Pediatrics 2011;128:539–546. [DOI] [PubMed] [Google Scholar]
- [37].Honaker SM, Meltzer LJ. Sleep in pediatric primary care: A review of the literature. Sleep Med Rev 2016;25:31–39. [DOI] [PubMed] [Google Scholar]
- [38].Hart CN, Hawley NL, Wing RR. Development of a Behavioral Sleep Intervention as a Novel Approach for Pediatric Obesity in School-aged Children. Sleep Med Clin 2016;11:515–523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Van Dyk TR, Zhang N, Catlin PA, et al. Feasibility and Emotional Impact of Experimentally Extending Sleep in Short-Sleeping Adolescents. Sleep 2017;40. [DOI] [PubMed] [Google Scholar]
- [40].Guglielmo D, Gazmararian JA, Chung J, et al. Racial/ethnic sleep disparities in US school-aged children and adolescents: a review of the literature. Sleep Health 2018;4:68–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure 1. Demographic factor interaction P-values with visit (top row) and weeknight status (bottom row). Panel A: Sleep duration and timing outcomes (red: sleep duration; orange: sleep sufficiency; green: sleep onset; blue: sleep offset). Panel B: Sleep quality outcomes (red: awakenings; orange: efficiency; green: wake after sleep onset; blue: sleep onset latency). The horizontal reference line represents the Bonferroni corrected P-value for a statistically significant interaction (0.05/16 = 0.0031).


