Abstract
Introduction.
Methamphetamine use is increasing in North America and is associated with numerous negative health effects and social harms. As drug-related harms are often gendered, this study sought to examine the differential impacts of gender on the trends, risk factors and health implications of crystal methamphetamine use among a Canadian cohort of people with high rates of injection polysubstance use.
Methods.
Data were collected from two prospective cohorts of people who inject drugs in Vancouver, Canada. We examined trends in reported crystal methamphetamine use from 2006–2017 using the Cochrane-Armitage test for trend. We used multivariable generalised estimating equations, stratified by gender, to determine independent risk factors and health outcomes associated with crystal methamphetamine use.
Results.
In total, 1984 participants were included in the study, including 694 (35%) women. The prevalence of reported crystal methamphetamine use within the previous 6 months rose from 19% in 2006 to 36% in 2017, with a rise seen in both genders (P < 0.001). Reported crystal methamphetamine use was associated with numerous risk behaviours and drug-related harms in both genders, and in women it was associated with an increase in experiences of sexual violence (adjusted odds ratio 1.64, 95% confidence interval 1.18, 2.27).
Conclusions.
These findings demonstrate the rising prevalence of reported crystal methamphetamine use in Vancouver in a cohort with high rates of polysubstance use. This work highlights drug and sex-related risk behaviours associated with crystal methamphetamine use for both genders, and underscores the need to develop strategies to address the growing use of crystal methamphetamine.
Keywords: methamphetamine, central nervous system stimulant, gender, HIV
Introduction
Methamphetamine is the most common illicit synthetic stimulant in the world, and its prevalence continues to rise in many settings [1]. Recent national survey data from the United States suggests that just over 5% of the US population has tried methamphetamine at least once in their lifetime, with past year use estimated at 0.7% [2]. In Australia, rates of methamphetamine use are among the highest in the world, with 1.4% of the population reporting use within the past year, and in a recent Australian survey specifically targeting people who inject drugs, 76% had injected crystal methamphetamine within the previous 6 months [3,4]. Canadian data estimate a prevalence rate of 3.7% lifetime use, with possession violations for methamphetamine rising 590% between 2010 and 2017, most notably in the western provinces of British Columbia and Alberta [5,6]. The rising prevalence of methamphetamine use is concerning not only because of its high addictive potential, but also because of the myriad of negative health effects and social consequences associated with its use, including HIV and hepatitis C virus transmission, cardiovascular effects and psychiatric harms [7]. Additionally, no effective pharmacotherapy currently exists for methamphetamine use disorder, and current evidence-based treatment strategies are limited to psychosocial interventions such as cognitive behavioural therapy and contingency management programs [8]. Taken together, it is unsurprising that hospitalisations and associated healthcare costs from methamphetamine use have risen sharply over the past decade [9].
Many important sociodemographic, social-structural and geographic variables shape the prevalence and patterns of illicit substance use. In North American settings, methamphetamine use in particular is more common in young adults, those of non-Hispanic white background, those located in the West or mid-West of the United States, and those in certain subgroups such as men who have sex with men (MSM) [10,11]. The role of gender specifically has been shown to have important implications for patterns of use, with methamphetamine use among women being associated with younger age of initiation, more rapid escalation of patterns of use, more underlying mood disorders and better response to treatment [12]. Conversely, among men, methamphetamine use is often associated with older age of initial use, higher rates of polysubstance use and more frequent engagement with the criminal justice system [12,13]. Since drug use is gendered, with marginalised women particularly impacted by intersecting factors that shape drug-related harms, exploring the role of gender may help inform effective service planning and delivery for individuals who use methamphetamine.
Previous work has shown increasing rates of injection crystal methamphetamine use in Western Canada, however, to our knowledge, no data have been published describing trends beyond the year 2004 [14]. Furthermore, there is a growing appreciation for the impact of methamphetamine on the overdose crisis in the US and Canada, yet current information on trends in methamphetamine use among those with polysubstance use is lacking [15]. Given the significant increases in prevalence seen elsewhere over the past decade, the present study sought to evaluate the prevalence of crystal methamphetamine use over the past decade among a cohort of people who inject drugs in Vancouver, Canada. Further, given the importance of understanding potentially modifiable factors that shape methamphetamine use and its health impacts, this study also examined risk factors and health outcomes associated with crystal methamphetamine use over the past decade, with special attention given to the role of gender. We hypothesized that the prevalence of crystal methamphetamine use is continuing to rise in both genders, as has been the overall trend in other parts of North America, with key differences in substance use patterns and experiences of violence between men and women.
Methods
Data for this study were obtained from two ongoing open prospective cohorts: the AIDS Care Cohort to Evaluate Exposure to Survival Services (ACCESS) and the Vancouver Injection Drug Users Study (VIDUS). Details for these cohorts have been well described in previous literature [16]. Briefly, these cohorts are from Vancouver, Canada, have been running since 1996 and are composed of HIV-positive and HIV-negative participants, respectively. Criteria for eligibility include being ≥18 years old, living within the Greater Vancouver Regional District and providing informed consent. Additionally, participants in ACCESS have to have used illicit drugs in addition to or other than cannabis (which was illegal during the study period) in the month prior to enrolment and be HIV-positive, while those in VIDUS have to have used injection drugs within the month before enrolment and be HIV-negative. Individuals in VIDUS who experience HIV seroconversion are transitioned to the ACCESS study. Participants are recruited through street outreach, word of mouth and self-referral. At the time of entry and on a semi-annual basis thereafter, participants complete an interviewer-administered questionnaire to elicit information on demographics, drug use behaviours and other exposures. Study procedures are harmonised to allow for pooled analysis when appropriate. Blood samples are also drawn to establish HIV and hepatitis C virus serostatus and to assess disease progression in those with HIV. All participants are offered referrals to addiction treatment services, and any that test positive for HIV are referred to an appropriate care provider. Participants are reimbursed with CAN$40 per visit for their time. The cohort studies receive annual ethics approval from the University of British of Columbia/Providence Health Care research ethics board.
For this study, we used data gathered between December 2006 and June 2017. All study participants with a history of injection drug use at baseline were included. Our primary outcome was defined as any reported recent crystal methamphetamine use, defined as any use within the previous 6 months (yes vs. no). A number of explanatory variables were selected based on previously established or hypothesized relationships with crystal methamphetamine use: calendar year of interview, age (per 10 years older), ethnicity (white vs. non-white), employment (yes vs. no), homelessness (yes vs. no), residence in the Downtown Eastside (an urban Vancouver neighbourhood with a high concentration of substance use; yes vs. no), sex work involvement (yes vs. no), drug dealing (yes vs. no), at least daily injection heroin use (yes vs. no), at least daily injection cocaine use (yes vs. no), at least daily non-injection crack use (yes vs. no), methadone maintenance therapy (yes vs. no), HIV positive (yes vs. no), history of nonfatal overdose (yes vs. no), history of shared syringes (yes vs. no), history of unprotected vaginal/anal intercourse (yes vs. no), history of experiencing physical violence (yes vs. no), history of experiencing sexual violence (yes vs. no), and MSM (in men only, yes vs. no). All behavioural variables referred to activities within the previous 6 months.
Baseline sample characteristics stratified by reported crystal methamphetamine use within the previous 6 months were compared using Pearson chi-squared test for categorical variables and Mann–Whitney test for continuous variables. Baseline sample characteristics stratified by gender were also examined among individuals who reported crystal methamphetamine use within the previous 6 months.
To examine changes in prevalence of crystal methamphetamine use over time, we examined the proportion of participants reporting the following activities within the previous 6 months: (i) any crystal methamphetamine use; (ii) any intravenous crystal methamphetamine use; and (iii) at least daily crystal methamphetamine use. These trends were also stratified by gender and analysed by Cochran-Armitage test for trend.
Next, we used linear regression stratified by gender to evaluate for an association between yearly frequency of each of our individual variables and calendar year in order to illustrate changes in the composition of the overall cohort over time.
Finally, generalised estimating equations models, using an exchangeable correlation structure (assuming that the within subject observations are equally correlated) and the logit link function, were performed to identify factors independently associated with the primary outcome of reported crystal methamphetamine use within the previous 6 months, stratified by gender. Variance inflation factors were used to test for multicollinearity among variables. The multivariable models were fit using an a priori defined model including all variables that were found to be significant (P < 0.1) in bivariable analyses. All statistical models were performed using R version 3.5.0 (R Core Team, Vienna, Austria) and all P values were two-sided and considered significant if P < 0.05.
Results
This study included 2032 participants enrolled between the years of 2006 and 2017 and followed for an average of 6.9 years per participant (interquartile range 2.2, 9.7). Out of the sample 35% identified as female gender (n = 694) and 65% identified as male gender (n = 1290), while 1% of participants (n = 20) identified as transgender, two-spirited or other non-binary persons and were not included in these analyses due to low prevalence in the sample. A total of 28 participants did not state their gender and were also excluded. The median age of the 1984 included participants was 41.8 years (interquartile range 34.6, 48.1). The majority of participants identified as white (58%, n = 1151) or Indigenous ancestry (31%, n = 609). At the first available survey, 29% (n = 582) of participants reported crystal methamphetamine use within the previous 6 months. Of those 582 individuals, 188 (32%) reported daily injection heroin use and 49 (8%) reported daily injection cocaine use at first available survey. See Appendix S1 for baseline characteristics of the study sample, taken from each individual participant’s time of entry into the cohort, stratified by reported crystal methamphetamine use within the previous 6 months.
Crystal methamphetamine use was reported by 52% of all participants (n = 1030), 51% of women (n = 355) and 52% of men (n = 675), at some point during the study period. A comparison of baseline characteristics of 1030 participants who reported any crystal methamphetamine use during the study period (Table 1) found that men were more likely to be older, white and employed, and were less likely compared to women to reside in the Downtown Eastside, to be involved in sex work, to report at least daily injection heroin use, to report at least daily non-injection crack use, to be on methadone maintenance therapy, to have unprotected sex or to have experienced sexual violence (all P < 0.05).
Table 1.
Baseline characteristics of participants with any reported crystal methamphetamine use at any point during the study period, stratified by gender
| Characteristic | Total n = 1030 (100%) |
Men n = 675 (65.5%) |
Women n = 355 (34.5%) |
Odds ratio (95% CI) |
P value |
|---|---|---|---|---|---|
| Age (median, IQR) | 38.6 (32.2, 45.3) | 40.2 (33.6, 46.7) | 36.0 (30.4, 42.9) | 1.05 (1.04, 1.07) | <0.001 |
| White | |||||
| Yes | 612 (59.4) | 447 (66.2) | 165 (46.5) | 2.26 (1.74, 2.94) | <0.001 |
| No | 418 (40.6) | 228 (33.8) | 190 (53.5) | ||
| Employmenta | |||||
| Yes | 218 (21.2) | 174 (25.8) | 44 (12.4) | 2.46 (1.72, 3.52) | <0.001 |
| No | 811 (78.7) | 500 (74.1) | 311 (87.6) | ||
| Homelessnessa | |||||
| Yes | 478 (46.4) | 313 (46.4) | 165 (46.5) | 1.00 (0.77, 1.29) | 0.992 |
| No | 548 (53.2) | 359 (53.2) | 189 (53.2) | ||
| Reside in Downtown Eastsidea | |||||
| Yes | 781 (75.8) | 496 (73.5) | 285 (80.3) | 0.68 (0.50, 0.93) | 0.015 |
| No | 249 (24.2) | 179 (26.5) | 70 (19.7) | ||
| Sex work involvementa | |||||
| Yes | 200 (19.4) | 40 (5.9) | 160 (45.1) | 0.08 (0.05, 0.11) | <0.001 |
| No | 827 (80.3) | 634 (93.9) | 193 (54.4) | ||
| Drug dealinga | |||||
| Yes | 374 (36.3) | 250 (37.0) | 124 (34.9) | 1.10 (0.84, 1.43) | 0.504 |
| No | 656 (63.7) | 425 (63.0) | 231 (65.1) | ||
| Daily injection heroin usea | |||||
| Yes | 301 (29.2) | 167 (24.7) | 134 (37.7) | 0.54 (0.41, 0.71) | <0.001 |
| No | 726 (70.5) | 506 (75.0) | 220 (62.0) | ||
| Daily injection cocaine usea | |||||
| Yes | 95 (9.2) | 67 (9.9) | 28 (7.9) | 1.29 (0.81, 2.04) | 0.282 |
| No | 932 (90.5) | 606 (89.8) | 326 (91.8) | ||
| Daily non-injection crack usea | |||||
| Yes | 376 (36.5) | 210 (31.1) | 166 (46.8) | 0.51 (0.39, 0.67) | <0.001 |
| No | 653 (63.4) | 465 (68.9) | 188 (53.0) | ||
| Methadone maintenancea | |||||
| Yes | 434 (42.1) | 261 (38.7) | 173 (48.7) | 0.66 (0.51, 0.85) | 0.001 |
| No | 591 (57.4) | 412 (61.0) | 179 (50.4) | ||
| HIV | |||||
| Yes | 411 (39.9) | 278 (41.2) | 133 (37.5) | 1.17 (0.90, 1.52) | 0.247 |
| No | 619 (60.1) | 397 (58.8) | 222 (62.5) | ||
| History of overdosea | |||||
| Yes | 113 (11.0) | 76 (11.3) | 37 (10.4) | 1.09 (0.72, 1.65) | 0.699 |
| No | 914 (88.7) | 598 (88.6) | 316 (89.0) | ||
| Shared syringesa | |||||
| Yes | 119 (11.6) | 70 (10.4) | 49 (13.8) | 0.73 (0.49, 1.08) | 0.113 |
| No | 902 (87.6) | 597 (88.4) | 305 (85.9) | ||
| Unprotected sexa | |||||
| Yes | 422 (41.0) | 254 (37.6) | 168 (47.3) | 0.66 (0.50, 0.85) | 0.002 |
| No | 595 (57.8) | 415 (61.5) | 180 (50.7) | ||
| Experienced physical violencea | |||||
| Yes | 293 (28.4) | 191 (28.3) | 102 (28.7) | 0.98 (0.74, 1.30) | 0.897 |
| No | 727 (70.6) | 477 (70.7) | 250 (70.4) | ||
| Experienced sexual violencea | |||||
| Yes | 17 (1.7) | 4 (0.6) | 13 (3.7) | 0.16 (0.05, 0.48) | <0.001 |
| No | 1005 (97.6) | 666 (98.7) | 339 (95.5) |
Denotes activities or situations referring to the previous 6 months. CI, confidence interval; IQR, interquartile range.
Between 2006 and 2017, reported crystal methamphetamine use within the previous 6 months increased in all participants from 19% to 36% (P < 0.001; Figure 1a), in women from 14% to 36% (P < 0.001), and in men from 22% to 37% (P < 0.001). Similarly, reported daily crystal methamphetamine use over the previous 6 months rose in all participants from 1% to 12% % (P < 0.001; Figure 1b), in women from 0% to 11% (P < 0.001), and in men from 2% to 12% (P < 0.001). Lastly, reported injection crystal methamphetamine use within the previous 6 months increased in all participants from 18% to 28% (P < 0.001; Figure 1c), in women from 14% to 27% (P < 0.001), and in men from 20% to 29% (P < 0.001). There were no significant differences between men and women for any measurement of reported crystal methamphetamine use over time.
Figure 1.
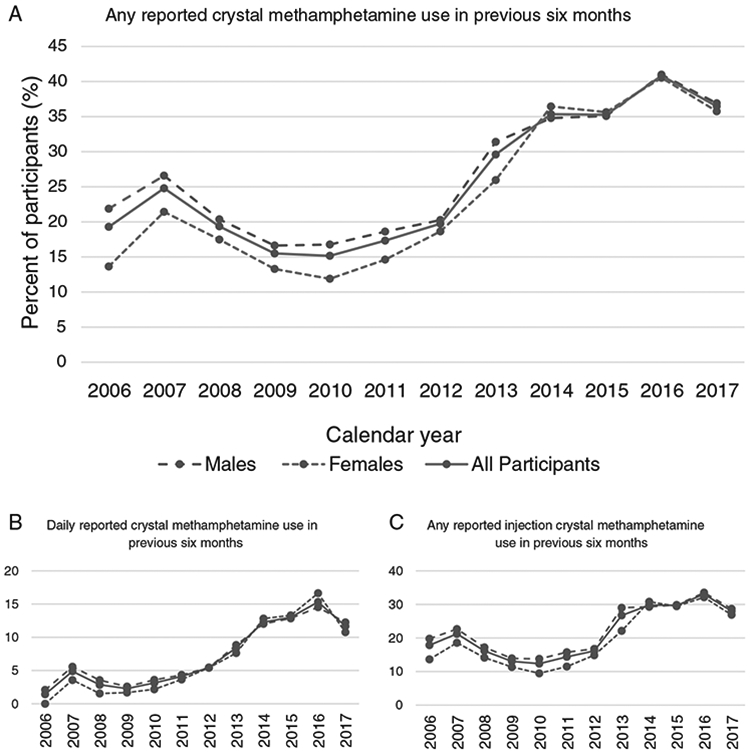
Trends in reported crystal methamphetamine use over time, stratified by gender. (a) Any reported crystal methamphetamine use in the previous 6 months (P < 0.001). (b) Daily reported crystal methamphetamine use in the previous 6 months (P < 0.001). (c) Any reported injection crystal methamphetamine use in the previous 6 months (P < 0.001).
Other sociodemographic factors, drug use patterns and health outcomes in our cohort were also changing over time. By examining the result of linear regression we saw that, in both women and men, there was a negative association between calendar year and the proportion of participants who were white, homeless, living in the Downtown Eastside, dealing drugs, reporting daily noninjection crack cocaine use and reporting experiences of physical violence. Conversely, in both genders there was a positive association between calendar year and the proportion of participants reporting HIV and nonfatal overdose. In women specifically, there was a negative association between year and sex work involvement, and a positive association with rates of employment. In men specifically, there was a negative association between year and rates of reported daily cocaine injection, shared injection equipment and unprotected sex, and a positive association with sex work involvement (all P < 0.05). See Appendix S2 for a complete list of associations between sociodemographic factors and drug use patterns with calendar year.
In multivariable generalised estimating equations analyses (Table 2), factors independently associated with reported crystal methamphetamine use in both genders included calendar year, involvement in sex work, drug dealing, nonfatal overdose, shared syringes, unprotected sex and having experienced physical violence. In women only, residing in the Downtown Eastside and having experienced sexual violence were associated with reported crystal methamphetamine use, while reported at least daily noninjection crack use was negatively associated. In men only, homelessness, reported at least daily injection heroin use, reported at least daily injection cocaine use, being HIV positive and MSM were also positively associated with reported crystal methamphetamine use, while older age and employment were negatively associated (all P < 0.05). Variance inflation factor testing showed no evidence of multicollinearity (variance inflation factor ranging from 1.03–1.33; Appendix 3).
Table 2.
Bivariable and multivariable GEE analysis of factors associated with reported crystal methamphetamine use, stratified by gender (n = 1984)
| Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
Unadjusted OR (95% CI) |
Adjusted OR (95% CI) |
|
|---|---|---|---|---|
| Characteristic | Men | Women | ||
| Year (by calendar year) | 1.07 (1.05, 1.09) | 1.18 (1.15, 1.21)* | 1.10 (1.08, 1.13) | 1.13 (1.10, 1.16)* |
| Age (per 10 years older) | 0.87 (0.78, 0.97) | 0.47 (0.41, 0.53)* | 0.99 (0.86, 1.14) | — |
| White | 1.10 (0.89, 1.35) | — | 1.06 (0.81, 1.38) | — |
| Employmenta | 0.90 (0.83, 0.98) | 0.90 (0.81, 0.99)* | 0.95 (0.83, 1.09) | — |
| Homelessnessa | 1.21 (1.09, 1.35) | 1.13 (1.00, 1.28)* | 1.07 (0.91, 1.25) | — |
| Reside in Downtown Eastsidea | 1.14 (1.02, 1.27) | 1.13 (1.00, 1.27) | 1.19 (1.02, 1.38) | 1.29 (1.09, 1.53)* |
| Sex work involvementa | 2.28 (1.67, 3.11) | 1.80 (1.25, 2.59)* | 1.77 (1.53, 2.04) | 2.06 (1.75, 2.42)* |
| Drug dealinga | 1.52 (1.38, 1.68) | 1.41 (1.26, 1.58)* | 1.42 (1.23, 1.63) | 1.55 (1.32, 1.82)* |
| Daily injection heroin usea | 1.57 (1.40, 1.77) | 1.37 (1.19, 1.57)* | 1.34 (1.14, 1.57) | 1.19 (1.00, 1.42) |
| Daily injection cocaine usea | 1.21 (1.03, 1.42) | 1.21 (1.00, 1.47)* | 1.13 (0.92, 1.39) | — |
| Daily non-injection crack usea | 0.86 (0.77, 0.98) | 0.88 (0.77, 1.01) | 0.72 (0.61, 0.84) | 0.70 (0.59, 0.82)* |
| Methadone maintenancea | 0.98 (0.87, 1.11) | — | 1.08 (0.93, 1.26) | — |
| HIV positive | 1.25 (1.02, 1.54) | 1.48 (1.18, 1.85)* | 0.78 (0.61, 1.01) | 1.08 (0.82, 1.42) |
| History of overdosea | 1.89 (1.63, 2.19) | 1.60 (1.35, 1.89)* | 1.82 (1.45, 2.30) | 1.44 (1.13, 1.84)* |
| Shared syringesa | 1.95 (1.59, 2.40) | 1.87 (1.47, 2.39)* | 1.83 (1.41, 2.38) | 1.85 (1.40, 2.45)* |
| Unprotected sexa | 1.32 (1.20, 1.46) | 1.29 (1.14, 1.45)* | 1.62 (1.44, 1.83) | 1.55 (1.36, 1.77)* |
| Experienced physical violencea | 1.39 (1.27, 1.52) | 1.38 (1.23, 1.53)* | 1.35 (1.16, 1.57) | 1.24 (1.05, 1.47)* |
| Experienced sexual violencea | 2.32 (1.22, 4.39) | 0.91 (0.46, 1.81) | 1.95 (1.43, 2.65) | 1.64 (1.18, 2.27)* |
| Men who have sex with mena | 1.95 (1.56, 2.45) | 1.72 (1.32, 2.25)* | N/A | N/A |
Note: Items found to be non-significant on univariate analysis were not included in the bivariate model.
Denotes activities or situations referring to the previous 6 months.
P < 0.05.
CI, confidence interval; GEE, generalised estimating equations; N/A, not applicable; OR, odds ratio.
Discussion
In this prospective cohort study of participants with high rates of injection polysubstance use situated in Vancouver, Canada, we observed a significant rise in the use of crystal methamphetamine between 2007 and 2018, with over half of our participants reporting its use at some point during the study period. We found that, in this population, overall prevalence of reported crystal methamphetamine use was similar between men and women. Furthermore, we found that many of the harms associated with reported crystal methamphetamine use were common to both genders, including drug-related exposures such as drug dealing, sharing syringes and recent non-fatal overdose, as well as sexual risk exposures, such as sex work and unprotected sex. Experiences of sexual violence, however, were associated with reported crystal methamphetamine use in women only.
Our observation of steadily increasing rates of reported crystal methamphetamine use is consistent with many other reports from North America and globally [1,2]. Reliable estimates of the global burden of methamphetamine use are challenging to obtain, but reported seizure rates of amphetamine-type substances over the past 5 years have been steadily rising, and methamphetamine makes up the majority of these seized drugs [1]. Furthermore, rates of amphetamine-related hospitalisations in the US are rising dramatically [9]. While data from elsewhere in Canada is scarce, within the US other studies involving people who inject drugs (PWID) suggest comparable increases over time to what we have described, with the prevalence of methamphetamine use reaching as high as 65% in a cohort of PWID in Washington State [17,18]. Interestingly, rising rates of the co-injection of methamphetamine and opioids together may be at least partially responsible for the increase seen in these specific populations over the past few years, as this appears to be a relatively new phenomenon [17,18].
The majority of the literature on crystal methamphetamine use, response to treatment and associated health outcomes has been focused on high-risk subpopulations including MSM, PWID and youth. There is less of an emphasis on the specific risks and consequences of crystal methamphetamine use in women, despite the fact that it is well established that women frequently exhibit different patterns of substance use, different co-morbidities and different responses to treatment [10]. The existing literature focusing on methamphetamine use in women does, however, demonstrate some relatively consistent distinctions compared to men. Unlike most substances, the overall prevalence of methamphetamine use is similar across genders, though women often begin to use methamphetamine at a younger age and show a quicker progression to dependence [12,13,19-21]. Women also demonstrate a higher incidence of psychiatric co-morbidities, more history of physical and/or sexual trauma, higher levels of unemployment and fewer legal issues [12,19,20,22]. While treatment was not a focus of this study, women also frequently demonstrate delayed access to treatment for methamphetamine use disorder compared to men, though may have better retention and improved outcomes once engaged [13,22,23].
It is important to interpret our results in the broader context of the population included in this particular cohort and its changing composition over time. Much of the current published data describes trends in crystal methamphetamine use in populations with significantly less polysubstance use than the cohort described in this study. This is particularly true when referring to women, where overall lower rates of polysubstance use have been described in those who use methamphetamine as compared to men [12,13]. In contrast, the women in our population reported higher rates of heroin use and daily noninjection crack use than men did at entry into the cohort. In this regard, this represents a unique cohort of women, yet the association between reported crystal methamphetamine use and experiences of sexual violence is consistent with previous work [20,24]. In particular, one past survey of patients in treatment for methamphetamine use disorder found that 58% of the women had experienced lifetime sexual abuse and violence, in contrast to only 16% of men [25]. Another local study of women who engage in sex work found that experiencing physical or sexual violence was associated with initiation into injection crystal methamphetamine use [26]. The social-structural factors that produce gendered violence among substance-using women have been previously explored, and understanding the gendered mechanisms and contexts that produce vulnerability to sexual violence among women PWID and the association between methamphetamine use and experiences of sexual violence is imperative to understanding barriers to health and/or harm reduction services for women who inject crystal methamphetamine [27-30].
With regards to other stimulants, in both genders there was a significant decrease noted in rates of reported non-injection crack use seen over time, which may correspond with the increasing uptake of crystal methamphetamine as the most commonly used form of stimulant in this population. In men only, however, did we see a comparable decrease in rates of reported injection cocaine use, despite no differences between genders noted at baseline. This emphasizes once more the severity of the polysubstance use disorder in our woman participants. Overdose rates were increasing in both genders over time, though it was interesting to note that methadone maintenance therapy was also more common in women at baseline and did not have any significant associations noted with calendar year in either gender. This is in contrast with the usual trend seen in the literature, where women often experience decreased access to methadone, and has been explored in detail in a previous publication from these same cohorts [31].
Our study clearly observed a number of risky behaviours and negative health outcomes associated with reported crystal methamphetamine use in both genders, including high-risk HIV behaviours such as syringe sharing and unprotected sex. This adds to a significant body of literature highlighting the relationship between methamphetamine use, HIV risk and worse overall HIV outcomes. Indeed, it has been well described that people with a history of methamphetamine use are at an increased risk of HIV infection through unsafe injection practices and/or unsafe sex [32,33]. Our results are consistent with previous observations that methamphetamine use is not only associated with sexual risk behaviours among MSM but also in male and female heterosexual encounters [33]. Despite the similarities in risk behaviours between genders in this sample, however, in men only was reported crystal methamphetamine use associated with increased rates of HIV, even after controlling for specific risk factors including MSM. Which factors might explain this association are not entirely clear, especially given comparable HIV rates between genders at baseline and a positive association noted between HIV rates and calendar year in both groups.
We also observed an independent relationship between reported crystal methamphetamine use and the likelihood of non-fatal overdose among both women and men. This relationship has previously been noted in multiple studies, though it remains unclear whether the effects of methamphetamine itself are directly responsible for the increased risk, or whether this is a marker for other risky behaviours that may carry with them a higher risk of overdose, such as higher frequency of substance use or polysubstance use [17,34-38]. Our analysis did attempt to adjust for other substances by including variables for at least daily heroin injection, at least daily cocaine injection, at least daily non-injection crack use and methadone maintenance therapy, yet the association between reported crystal methamphetamine use and non-fatal overdose remained significant. This is worth noting in light of the current opioid overdose crisis in the United States and Canada, especially given the increasing appreciation for the role of stimulant use in many of these deaths [15]. It highlights the importance of addressing polysubstance use in our overall response to the epidemic.
Another association worth highlighting is that, in men only, our data demonstrated a negative association between employment and rates of reported crystal methamphetamine use, as well as a positive association between homelessness and reported use. While we cannot make inferences on the direction of these relationships, similar findings have been shown with methamphetamine use elsewhere in the past but there were no noted gender differences [39,40]. At the very least, these findings suggest that in men employment and housing may represent modifiable risk factors for crystal methamphetamine use.
This study has several limitations that are important to note. First is the observational nature of the study and while our multivariable model accounts for a number of key confounding variables, it is not possible to establish causal relationships. Second, though follow-up rates are generally higher than average in our cohort, given the length of the study period these data may be subject to attrition bias. Third, we are not able to determine the directionality of the associations reported above. Fourth, we relied on the self-reporting of sensitive data by our participants, including information on substance use patterns and sexual practices. We cannot rule out the presence of a response bias, though self-reporting of similar variables has previously been shown to be valid for gathering data in comparable studies [41]. Fifth, recruitment for our cohort is not random, and there is the possibility that our sample is not generalisable to other PWID or groups of younger PWID. Finally, we have conducted an analysis using self-reported gender, and did not include participants who identified as transgender, two-spirit or other non-binary persons due to low counts. Based on previous literature, this is a population with higher rates of substance use including use of methamphetamine, and one disproportionately impacted by socio-structural (e.g. gender norms, criminalisation) and interpersonal factors (e.g. gendered violence) [42-44]. Further epidemiological study that goes beyond the use of a gender binary is an important area of future investigation.
Conclusions
This study observed a significant rise in the prevalence of reported crystal methamphetamine use in both men and women PWID in two Canadian prospective cohort studies with high rates of polysubstance use. Women in particular were more likely to report experiences of sexual violence, while a number of negative health outcomes were associated with its use in both genders, including the increased likelihoods of non-fatal overdose and both drug-related and sexual risk factors for HIV. These rising rates of crystal methamphetamine use among a population with high levels of polysubstance use are consistent with reports of the increasing role stimulants are playing in the North American overdose crisis, and highlight some of the particular risk factors and consequences of crystal methamphetamine use in this population. The need for gender-inclusive health services planning and research for PWID who use crystal methamphetamine is paramount.
Supplementary Material
Appendix S1. Baseline characteristics of all study participants, stratified by reported crystal methamphetamine use.
Appendix S2a. Percentage of women reporting each variable by year and results of linear regression between individual variables and calendar year.
Appendix S2b. Percentage of men reporting each variable by year and results of linear regression between individual variables and calendar year
Appendix S3. Variance inflation factor testing for multicollinearity at baseline entry into cohort and in all cohort observations.
Acknowledgements
The authors thank the study participants for their contribution to the research, as well as current and past researchers and staff. The study was supported by the US National Institutes of Health (U01-DA038886, U01-DA0251525). This research was undertaken, in part, thanks to funding from the Canada Research Chairs program through a Tier 1 Canada Research Chair in Inner City Medicine which supports EW, and the Canadian Institutes of Health Research (CIHR) Canadian Research Initiative on Substance Misuse (SMN–139148). PB is supported by the Michael Smith Foundation for Health Research and was a participant in the National Institute on Drug Abuse-funded Research in Addiction Medicine Scholars Program for the duration of this work (R25DA037756 and R25DA033211). M-JM, the Canopy Growth professor of cannabis science, is supported in part by the United States National Institutes of Health (U01-DA021525), a New Investigator Award from CIHR and a Scholar Award from the Michael Smith Foundation for Health Research. His institution has received an unstructured gift to support him from NG Biomed, Ltd., a private firm applying for a government license to produce cannabis. The Canopy Growth professorship in cannabis science was established through unstructured gifts to the University of British Columbia from Canopy Growth, a licensed producer of cannabis, and the Ministry of Mental Health and Addictions of the Government of British Columbia. KH is supported by a CIHR New Investigator Award (MSH-141971), a Michael Smith Foundation for Health Research Scholar Award and the St. Paul’s Foundation. NF is supported by a Michael Smith Foundation for Health Research/St. Paul’s Foundation Scholar Award.
Footnotes
Conflict of Interest
The authors report no conflicts of interest.
Supporting Information
Additional Supporting Information may be found in the online version of this article at the publisher’s website:
References
- [1].World Drug Report 2018. United Nations publication, sales no. E18XI9. [Google Scholar]
- [2].Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. Results from the 2018 National Survey on drug use and health: detailed tables. Rockyville: Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality, 2019. [Google Scholar]
- [3].Peacock A, Uporova J, Karlsson A et al. Australian drug trends 2019: key findings from the National Illicit Drug Reporting System (IDRS) interviews. Sydney: National Drug and Alcohol Research Centre, UNSW Sydney, 2019. [Google Scholar]
- [4].Australian Institute of Health and Welfare National drug strategy house-hold survey 2016. Canberra: Australian Institute of Health and Welfare. [Google Scholar]
- [5].Statistics Canada. Canadian tobacco, alcohol and drugs survey (CTADS): Summary of results for 2017. Ottawa: Statistics Canada. [Google Scholar]
- [6].Canadian Centre on Substance Use and Addiction. Canadian drug summary Methamphetamine. Canadian Centre on Substance Use and Addiction, 2018. [Google Scholar]
- [7].Vearrier D, Greenberg MI, Miller SN, Okaneku JT, Haggerty DA. Methamphetamine: history, pathophysiology, adverse health effects, current trends, and hazards associated with the clandestine manufacture of methamphetamine. Dis Mon 2012;58:38–89. [DOI] [PubMed] [Google Scholar]
- [8].Morley KC, Cornish JL, Faingold A, Wood K, Haber PS. Pharmacotherapeutic agents in the treatment of methamphetamine dependence. Expert Opin Investig Drugs 2017;26:563–78. [DOI] [PubMed] [Google Scholar]
- [9].Winkelman TNA, Admon LK, Jennings L, Shippee ND, Richardson CR, Bart G. Evaluation of amphetamine-related hospitalizations and associated clinical outcomes and costs in the United States. JAMA Netw Open 2018;1:e183758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Ait-Daoud N, Blevins D, Khanna S, Sharma S, Holstege CP. Women and addiction. Psychiatr Clin North Am 2017;40:285–97. [DOI] [PubMed] [Google Scholar]
- [11].Courtney KE, Ray LA. Methamphetamine: an update on epidemiology, pharmacology, clinical phenomenology, and treatment literature. Drug Alcohol Depend 2014;143:11–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Dluzen DE, Liu B. Gender differences in methamphetamine use and responses: a review. Gend Med 2008;5:24–35. [DOI] [PubMed] [Google Scholar]
- [13].Brecht ML, O’Brien A, von Mayrhauser C, Anglin MD. Methamphetamine use behaviors and gender differences. Addict Behav 2004;29:89–106. [DOI] [PubMed] [Google Scholar]
- [14].Fairbairn N, Kerr T, Buxton JA, Li K, Montaner JS, Wood E. Increasing use and associated harms of crystal methamphetamine injection in a Canadian setting. Drug Alcohol Depend 2007;88:313–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Kariisa M, Scholl L, Wilson N, Seth P, Hoots B. Drug overdose deaths involving cocaine and psychostimulants with abuse potential—United States, 2003–2017. MMWR Morb Mortal Wkly Rep 2019;68:388–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Strathdee SA, Patrick DM, Currie SL et al. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS 1997;11:F59–65. [DOI] [PubMed] [Google Scholar]
- [17].Al-Tayyib A, Koester S, Langegger S, Raville L. Heroin and methamphetamine injection: an emerging drug use pattern. Subst Use Misuse 2017;52:1051–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Glick SN, Burt R, Kummer K, Tinsley J, Banta-Green CJ, Golden MR. Increasing methamphetamine injection among non-MSM who inject drugs in King County, Washington. Drug Alcohol Depend 2018;182:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hser YI, Evans E, Huang YC. Treatment outcomes among women and men methamphetamine abusers in California. J Subst Abuse Treat 2005;28:77–85. [DOI] [PubMed] [Google Scholar]
- [20].Kittirattanapaiboon P, Srikosai S, Wittayanookulluk A. Methamphetamine use and dependence in vulnerable female populations. Curr Opin Psychiatry 2017;30:247–52. [DOI] [PubMed] [Google Scholar]
- [21].Smith K Gender differences in primary substance of abuse across age groups The CBHSQ report. Rockville: Center for Behavioural Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2014. [PubMed] [Google Scholar]
- [22].Cohen JB, Greenberg R, Uri J, Halpin M, Zweben JE. Women with methamphetamine dependence: research on etiology and treatment. J Psychoactive Drugs 2007;39:347–51. [DOI] [PubMed] [Google Scholar]
- [23].Rusch ML, Lozada R, Pollini RA et al. Polydrug use among IDUs in Tijuana, Mexico: correlates of methamphetamine use and route of administration by gender. J Urban Health 2009;86:760–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Hayashi HD, Patterson TL, Semple SJ, Fujimoto K, Stockman JK. Risk factors for recent intimate partner violence among methamphetamine-using men and women. J Psychoactive Drugs 2016;48:135–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Cohen JB, Dickow A, Horner K et al. Abuse and violence history of men and women in treatment for methamphetamine dependence. Am J Addict 2003;12:377–85. [PubMed] [Google Scholar]
- [26].Argento E, Strathdee SA, Goldenberg S, Braschel M, Montaner J, Shannon K. Violence, trauma and living with HIV: longitudinal predictors of initiating crystal methamphetamine injection among sex workers. Drug Alcohol Depend 2017;175:198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Boyd J, Collins AB, Mayer S, Maher L, Kerr T, McNeil R. Gendered violence and overdose prevention sites: a rapid ethnographic study during an overdose epidemic in Vancouver, Canada. Addiction 2018;113:2261–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Iversen J, Page K, Madden A, Maher L. HIV, HCV, and health-related harms among women who inject drugs: implications for prevention and treatment. J Acquir Immune Defic Syndr 2015;69:S176–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Marshall BD, Fairbairn N, Li K, Wood E, Kerr T. Physical violence among a prospective cohort of injection drug users: a gender-focused approach. Drug Alcohol Depend 2008;97:237–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].McNeil R, Shannon K, Shaver L, Kerr T, Small W. Negotiating place and gendered violence in Canada’s largest open drug scene. Int J Drug Policy 2014;25:608–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Bach P, Milloy MJ, Nguyen P et al. Gender differences in access to methadone maintenance therapy in a Canadian setting. Drug Alcohol Rev 2015;34:503–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Marshall BD, Shoveller JA, Wood E, Patterson TL, Kerr T. Difficulty accessing syringes mediates the relationship between methamphetamine use and syringe sharing among young injection drug users. AIDS Behav 2011;15:1546–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Passaro RC, Pandhare J, Qian HZ, Dash C. The complex interaction between methamphetamine abuse and HIV-1 pathogenesis. J Neuroimmune Pharmacol 2015;10:477–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Mitra G, Wood E, Nguyen P, Kerr T, DeBeck K. Drug use patterns predict risk of non-fatal overdose among street-involved youth in a Canadian setting. Drug Alcohol Depend 2015;153:135–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Meacham MC, Strathdee SA, Rangel G, Armenta RF, Gaines TL, Garfein RS. Prevalence and correlates of heroin-methamphetamine co-injection among persons who inject drugs in San Diego, California, and Tijuana, Baja California, Mexico. J Stud Alcohol Drugs 2016;77: 774–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Kinner SA, Milloy MJ, Wood E, Qi J, Zhang R, Kerr T. Incidence and risk factors for non-fatal overdose among a cohort of recently incarcerated illicit drug users. Addict Behav 2012;37:691–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Darke S, Marel C, Mills KL et al. Patterns and correlates of non-fatal heroin overdose at 11-year follow-up: findings from the Australian treatment outcome study. Drug Alcohol Depend 2014;144:148–52. [DOI] [PubMed] [Google Scholar]
- [38].Bazazi AR, Zelenev A, Fu JJ, Yee I, Kamarulzaman A, Altice FL. High prevalence of non-fatal overdose among people who inject drugs in Malaysia: correlates of overdose and implications for overdose prevention from a cross-sectional study. Int J Drug Policy 2015;26: 675–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Brecht ML, Greenwell L, von Mayrhauser C, Anglin MD. Two-year outcomes of treatment for methamphetamine use. J Psychoactive Drugs 2006;38:415–26. [DOI] [PubMed] [Google Scholar]
- [40].Das-Douglas M, Colfax G, Moss AR, Bangsberg DR, Hahn JA. Tripling of methamphetamine/amphetamine use among homeless and marginally housed persons, 1996-2003. J Urban Health 2008;85:239–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Darke S Self-report among injecting drug users: a review. Drug Alcohol Depend 1998;51:253–63 discussion 67-8. [DOI] [PubMed] [Google Scholar]
- [42].Collins AB, Bardwell G, McNeil R, Boyd J. Gender and the overdose crisis in North America: moving past gender-neutral approaches in the public health response. Int J Drug Policy 2019;69:43–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Pinkham S, Malinowska-Sempruch K. Women, harm reduction and HIV. Reprod Health Matters 2008;16:168–81. [DOI] [PubMed] [Google Scholar]
- [44].Reback CJ, Fletcher JB. HIV prevalence, substance use, and sexual risk behaviors among transgender women recruited through outreach. AIDS Behav 2014;18:1359–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Baseline characteristics of all study participants, stratified by reported crystal methamphetamine use.
Appendix S2a. Percentage of women reporting each variable by year and results of linear regression between individual variables and calendar year.
Appendix S2b. Percentage of men reporting each variable by year and results of linear regression between individual variables and calendar year
Appendix S3. Variance inflation factor testing for multicollinearity at baseline entry into cohort and in all cohort observations.


