Abstract
Childhood traumatic events are significant risk factors for psychopathology according to adult retrospective research; however, few studies examine trauma exposure and psychological symptoms in pre-adolescent children. Typically-developing children, aged 9–12 years (N = 114), were recruited from the community and selected from the Developmental Chronnecto-Genomics (Dev-CoG) study examining child development. Children completed questionnaires about traumatic life events, posttraumatic stress, anxiety, depression, dissociation, anger, and internalizing and externalizing behaviors. Parents also completed internalizing and externalizing measures. The number of traumatic events significantly correlated with symptom severity across all child-report psychological measures, but surprisingly, trauma was not correlated with any parent-report scores. Follow-up analyses revealed a significant trauma effect for internalizing and externalizing behaviors according to child self-report, but not for parent-report measures. Results indicate that childhood trauma may be a non-specific risk factor for sub-clinical psychopathology in otherwise typically-developing children. Moreover, children appear to be the most appropriate reporters of their own psychological distress.
Keywords: Trauma, Adverse childhood experiences, Psychopathology, Development, Internalizing and externalizing behaviors
Introduction
Half of all youth experience at least one traumatic event during childhood (Barzilay et al. 2018; Felitti et al. 1998). High rates of trauma exposure are concerning because childhood traumas are risk factors for a host of physical illnesses and psychological disorders (Briere et al. 2008; Edwards et al. 2003; Felitti et al. 1998; Graham-Bermann and Seng 2005; Green et al. 2010; Hughes et al. 2017; Seng et al. 2005; van Nierop et al. 2015). Specifically, meta-analyses indicate that trauma is a significant risk factor for depressive, psychotic, anxiety, and obsessive compulsive disorders (Fernandes and Osório 2015; Mandelli et al. 2015; Miller and Brock 2017; Varese et al. 2012). Importantly, the Adverse Childhood Experiences Study (ACEs) reports a cumulative trauma effect between the number of traumatic experiences and development of adult illnesses, with clearly increased odds ratios for additional difficulties in those experiencing four or more traumas (Felitti et al. 1998). However, most of these findings are based on adult patients’ recollections of traumatic events that occurred during their childhoods, and adult retrospective reports of adverse childhood experiences are subject to potential biases including false negatives and measurement error (Hardt and Rutter 2004).
Few studies address the impact of such adverse events on typically-developing youth. In fact, most recent literature focuses on child clinical or help-seeking populations (Hagan et al. 2016; Hodges et al. 2013). Data from the National Comorbidity Survey Replication Adolescent Supplement (NCS-A) found that childhood trauma was associated with adolescent psychopathology; however, as the title suggests, the youth included in this survey were at least 13 years old (Carliner et al. 2016, 2017). One important community-based epidemiological study by Barzilay et al. (2018) examined the number of adverse childhood experiences and current risk for psychopathology in a large sample of otherwise healthy youth aged 8–21. Barzilay et al. (2018) reported that greater exposure to traumatic events was associated with increased psychopathology across all assessed domains, including mood/anxiety symptoms, psychotic spectrum symptoms, externalizing behaviors, and fear. However, they did not examine their sample by smaller, age-based categories. Tremendous neurocognitive development occurs from 8 to 21 years old, especially in the prefrontal cortex (e.g., Diamond 2002). Thus, a more careful examination of the impact of trauma on childhood psychopathology should compare children within a narrow timeframe of development such as pre-adolescent children or post-pubertal adolescents rather than both of these age groups together.
To the best of our knowledge, no previous studies have exclusively examined the relationship between the experience of traumatic childhood events and psychological symptoms in typically-developing, pre-adolescent children. This is an important gap in the research because the prevalence rates for many psychological disorders increase during adolescence (Costello et al. 2002; Zahn-Waxler et al. 2008). The NCS-A (Merikangas et al. 2010) reported that the median age of onset was 11 for behavior disorders, 13 for mood disorders, and 15 for substance use disorders. Anxiety disorders tended to onset even earlier in childhood, and such fear-based disorders are the strongest predictors of subsequently developing comorbid disorders during adolescence (Kessler et al. 2012). Therefore, identifying risks that pre-date the emergence of psychological disorders is essential to prevention efforts and should offer clear targets for resilience building and therapeutic interventions (Meng et al. 2018).
The Developmental Chronnecto-Genomics (Dev-CoG) project, funded by the National Science Foundation (Award Number 1539067), is a collaborative effort between the Mind Research Network, the University of Nebraska Medical Center, Creighton University and Tulane University to advance the understanding of development in children. In the current study, we used data collected from the Dev-CoG cohort to examine the relationship between trauma exposure and symptom scores on various psychological measures. Our study is unique because it focuses on children aged 9–12 years to examine the potential association between trauma exposure and psychological symptoms before adolescence in healthy children. We hypothesized that the number of traumatic life events would be positively correlated with the severity of psychological symptoms including anxiety, depression, posttraumatic stress disorder (PTSD), dissociation, internalizing and externalizing behaviors in typically-developing children exposed to trauma.
Method
Participants and Procedures
All typically-developing children (N = 114; 58 female, 56 male) ages 9 to 12 (M = 10.88, SD = 1.73) were selected from a larger sample of 9–14 year olds (N = 183) enrolled in the Dev-CoG study. Participants were considered “typically-developing” if they did not have a previous diagnosis of a neurological, psychological or attention disorder, nor a history of serious head injury. Only 9–12 year old children whose parents completed all study questionnaires were included in data analysis, reducing the sample to 106 participants (53 female, 53 male). The average age of the sample was 10.88 years (SD = 1.10), with roughly a quarter of the sample assessed at each included age (9, 10, 11, and 12 years). In terms of race, the sample was predominately White (85%). The remainder of the sample included individuals who identified as Native American (5%), African American (3%), Pacific Islander (1%), Asian (1%), and Other (5%). In terms of ethnicity, 27% reported identifying as Hispanic or Latinx. The sample included children from a wide range of socioeconomic groups. Their parents had educational levels ranging from grade school to graduate degrees, and they held jobs ranging from labor to professional. Barratt Simplified Measure of Social Status (BSMSS; measure described below) scores can range from 8 to 66, and our sample ranged from 11 to 66. Our sample average (M = 43.58, SD = 12.56) is an average socioeconomic status score (Cirino et al. 2002).
The study was approved by the Institutional Review Boards (IRBs) for each respective member of the consortium, and all research was conducted according to ethical principles including obtaining fully informed and written parental permission and child assent. Computerized demographic and psychological questionnaires were completed by the children, while a parent/guardian completed socioeconomic and behavioral questionnaires about the child. Data collection occurred at the Mind Research Network in Albuquerque, New Mexico and the University of Nebraska Medical Center in Omaha, Nebraska.
Measures
Barratt Simplified Measure of Social Status (Barratt 2012)
We used the Barratt Simplified Measure of Social Status (BSMSS) to assess socioeconomic status (SES) using marital status, employment status, educational achievement, and occupational merit. The measure was administered to parents who reported their own and their parents’ marital status, occupation and highest level of education. A total score was calculated by adding the total education score with the total occupation score and taking family of origin and current marriage/partnership into account (Davis et al. 1991; Hollingshead 1957, 1975).
Child Behavior Checklist for Children (Achenbach and Rescorla 2001)
We used the Child Behavior Checklist for Children (CBCL) for ages 6–18 to assess child internalizing and externalizing behaviors according to parent report. The questionnaire consisted of 113 items, though we modified two items to eliminate specific statements about suicidality at the request of the research consortium. Each parent rated their child’s behaviors on a 3-point Likert scale ranging from 0 (not true) to 2 (very true or often true). Statements included externalizing items such as “Destroys his/her own things” and internalizing statements such as “Self-conscious or easily embarrassed.” The CBCL has strong content and criterion-related validity such that all items discriminated between referred and non-referred children (Achenbach and Rescorla 2001).
Modified UCLA Trauma History Profile (Steinberg et al. 2004)
We used a modified, self-report version of the UCLA Trauma History Profile to assess participants’ exposure to traumatic events. Children responded “yes” or “no” as to whether or not they had experienced each of 12 events. Sample events included the death of a loved one or being seriously hit, punched, or kicked. We shortened the original measure, using only 12 of the 15 items to reduce potential distress, especially with regard to sexual and/or physical abuse in the home. The UCLA Trauma History Profile is part of the UCLA PTSD Reaction Index, which is a psychometrically sound and frequently used measure of childhood trauma (Steinberg et al. 2013).
Mood and Feelings Questionnaire (Angold et al. 1995)
We used the child self-report version of the Mood and Feelings Questionnaire (MFQ) as an additional and unmodified measure of depression. We used the short form which included 13 phrases addressing participants’ emotions in the past two weeks. Participants read statements such as, “I cried a lot,” and “I felt lonely,” then responded to a Likert scale ranging from 0 (True) to 2 (Not true). The MFQ has shown strong internal consistency (Angold et al. 1995), and moderate to high criterion validity as a measure of depression (Daviss et al. 2006).
Strengths and Difficulties Questionnaire (Goodman 1997)
We used both the child (SDQ-C) and parent (SDQ-P) versions of the Strengths and Difficulties Questionnaire (SDQ). The externalizing score ranges from 0 to 20 and is the sum of the conduct problems and hyperactivity scale scores. The internalizing score ranges from 0 to 20 and is the sum of the emotional problems and peer problems scale scores. Both versions included all SDQ 25 items; however, we did not use the prosocial scale in this study. Child participants responded to statements such as, “I worry a lot” or “I get very angry and lose my temper” by selecting from a Likert scale ranging from 0 (Not True) to 2 (Certainly True) for each statement. Parents responded to similar statements about their child’s behavior using the same Likert scale. All participants were asked to respond based on their experiences over the last six months. The SDQ is a reliable and valid measure of internalizing and externalizing behaviors (Goodman 2001), correlating well with the CBCL scales (Warnick et al. 2008).
Trauma Symptom Checklist for Children (Briere 1996)
The Trauma Symptom Checklist for Children (TSCC) is a self-report measure for children ages 8–16 who have experienced traumatic life events. We used the alternative version, referred to as TSCC-A, which has five clinical scales assessing anxiety, depression, anger, posttraumatic stress, and dissociation, but does not address sexual concerns, per the request of the Dev-CoG consortium. Similarly, we modified the depression scale to eliminate specific questions about suicidality. The TSCC-A included statements such as, “Remembering things I don’t want to remember,” and “Getting into fights,” followed by a Likert scale assessing frequency of symptoms from 0 (Never) to 3 (Almost all of the time). The TSCC demonstrates convergent validity with measures of child symptomatology (Briere and Lanktree 1995) and shows solid internal consistency for each clinical scale (Briere 1996).
Statistics
First we calculated Pearson correlations between the number of traumatic life events experienced and all child-report measures (TSCC-A anxiety, anger, PTSD, dissociation, depression, MFQ total score, and SDQ-C internalizing and externalizing scores) and parent-report measures of internalizing and externalizing symptoms (SDQ-P and CBCL). This set of correlations between trauma history and each of the 12 psychological variables is the primary focus of our study. Accordingly, we used a Bonferroni correction of α = .05 divided by 12 correlations; such that the corrected significance level for this set of analyses became α = .004. Then to explore follow-up questions driven by our primary analysis, we looked at all correlations among child and parent measures of internalizing and externalizing symptoms to explore these relationships using a Bonferroni correction of α = .05 divided by 8 correlations; such that the corrected significance level for these analyses became α = .006.
Finally, we conducted multivariate analyses of covariance (MANCOVAs) exploring the effect of trauma level (high, low) on each set of parent or child measures of internalizing and externalizing behaviors while controlling for SES, as well as follow-up analyses of covariance ANCOVAs for each scale separately controlling for SES. We included SES as a covariate in these analyses because low SES and financial hardship are associated with increased exposure to childhood adversities like maltreatment and witnessing family violence (Turner et al. 2006), and first onset of various mood, anxiety, behavior, and substance use disorders (McLaughlin et al. 2011). For these analyses we selected a matched sample (by age and sex) of children with 4 or more traumatic events for the “high trauma” group (n = 22; 8 female, 14 male), and 0 or 1 traumatic events for the “low trauma” group (n = 19; 7 female, 12 male). We dichotomized the sample into high and low trauma based on previous research comparing those with 4 or more traumas to those without trauma (Anda et al. 2006; Felitti et al. 1998; Hughes et al. 2017). The average age in the high trauma group was 10.55 years (SD = 1.17), the average age in the low trauma group was 10.45 years (SD = 1.11).
Results
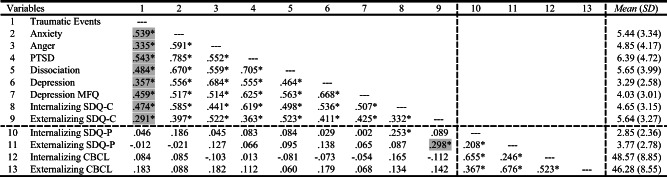
Consistent with our primary hypothesis, the number of self-reported traumatic life events (see Table 1) significantly correlated with symptom severity scores across all child self-report measures, even after conducting a Bonferroni correction for multiple tests (all p values < .004). Correlations between trauma and all child self-report symptom measures survived Bonferroni correction (see shading in Table 2 column 1, rows 2–9), and ranged from a high of r = 0.543 for trauma and PTSD to a low of r = 0.291 for trauma and externalizing behaviors. Surprisingly, the number of traumatic life events did not correlate significantly with severity of symptom scores on any of the parent-reported measures (all ps ≥ .061; see Table 2, column 1 rows 10–13). Moreover, the only correlation surviving Bonferroni correction between child-reported measures of internalizing and externalizing symptoms with parent-reported measures of those variables (see columns 8 and 9; rows 10–13) was for externalizing SDQ-C with externalizing SDQ-P (r = .298, p = .002), and this significant cell is shaded in column 9. Internalizing SDQ-C and SDQ-P were correlated (r = .253, p = .009) in the uncorrected matrix, but this relationship did not survive correction for multiple tests. The complete uncorrected correlation matrix is presented in Table 2.
Table 1.
Percent of Children Experiencing Specific Traumatic Events
| Event | % |
|---|---|
| Death of a loved one | 65.1 |
| Being seriously hit, punched or kicked very hard | 28.3 |
| Seeing or hearing about violence to a loved one | 27.4 |
| Seeing a family member hit, punched or kicked very hard | 14.2 |
| Being in a fire, flood or natural disaster | 12.3 |
| Being beaten up, shot at or threatened in the community | 11.3 |
| Seeing someone who was beaten up, shot at or killed | 10.4 |
| Having a painful or scary medical procedure | 10.4 |
| Being in a bad accident | 7.5 |
| Seeing a dead body not at a funeral | 4.7 |
| Being surrounded by war | 0 |
| Having anything else scary or upsetting happen | 36.8 |
The average number of traumatic events experienced by children in this sample was 2.28 (SD = 1.73) out of 12 possible events. Some respondents had multiple traumas
Table 2.
Number of Traumatic Events and Psychological Symptoms Correlations (N = 106)
*Correlation is significant at uncorrected α = .05
Shading in column 1 indicates correlation is significant after Bonferroni correction for 12 variables correlated with trauma exposure; α = .004
Shading in column 9 indicates correlation is significant after Bonferroni correction for 8 correlations among parent/child measures of internalizing/externalizing; α = .006
Then, to explore the discrepancy in correlations between traumatic experiences with child-report symptom measures and child-experienced trauma with parent-report measures of the child’s symptoms, we conducted additional analyses for internalizing and externalizing symptoms because we had both child and parent reports of these difficulties. We conducted separate MANCOVAs exploring the effect of trauma level (high, low) on each set of parent or child measures of internalizing and externalizing behaviors while controlling for social status because of the known relationship between SES and trauma exposure (e.g. McLaughlin et al. 2011; Turner et al. 2006) (Table 3). Follow-up ANCOVAs were also conducted for each scale separately while controlling for SES. Interestingly, SES was not a significant covariate in any of these analyses; however, trauma level was significant for both internalizing (F(2,37) = 17.544, p < .001, η2partial = .316) and externalizing (F(2,37) = 8.599, p = .006, η2partial = .185) behaviors on the child-report SDQ-C measure with higher scores in the high trauma group (Table 4). No significant trauma level effects were found for internalizing (F(2,38) = .692, p = .410, η2partial = .017) or externalizing (F(2,38) = .106, p = .747, η2partial = .003) behaviors using the parent-report SDQ-P. Furthermore, trauma level was not significant for internalizing (F(2,38) = 1.434, p = .238, η2partial = .035) behaviors and only trends toward significance for externalizing (F(2,38) = 3.901, p = .055, η2partial = .185) behaviors using the CBCL parent reports.
Table 3.
MANCOVAs of Internalizing and Externalizing Measures by Trauma Level Controlling for SES
| Dependent Variable | Effect | Wilks’ Lambda | F | p |
|---|---|---|---|---|
| SDQ-Child | Intercept | .540 | 15.746 | < .001 |
| SES | .924 | 1.520 | .232 | |
| Trauma | .650 | 9.976 | < .001 | |
| SDQ-Parent | Intercept | .582 | 13.637 | < .001 |
| SES | .900 | 2.113 | .135 | |
| Trauma | .982 | .347 | .709 | |
| CBCL-Parent | Intercept | .155 | 103.395 | < .001 |
| SES | .965 | .679 | .513 | |
| Trauma | .906 | 1.964 | .154 |
Table 4.
Strengths and Difficulties Questionnaire Descriptive Statistics
| Variable | Low Trauma | High Trauma | ||||
|---|---|---|---|---|---|---|
| n | M | SD | n | M | SD | |
| Child SDQ | ||||||
| Internalizing | 19 | 3.11 | 2.355 | 22 | 7.23 | 3.491 |
| Externalizing | 19 | 4.32 | 2.562 | 22 | 7.32 | 3.524 |
| Parent SDQ | ||||||
| Internalizing | 20 | 2.15 | 1.899 | 22 | 2.77 | 1.950 |
| Externalizing | 20 | 3.80 | 2.526 | 22 | 4.32 | 3.198 |
Discussion
As hypothesized, trauma consistently correlated with psychological symptoms (Barzilay et al. 2018; Merikangas et al. 2010) as measured by child-report in our community sample of typically-developing, pre-adolescent children. Correlation coefficients revealed all child-report symptom measures were positively associated with number of traumas experienced, even after correction for multiple tests. Moderately strong correlations were noted between number of traumas and all types of emotional symptoms assessed. Not surprisingly, the highest correlation coefficient linked was between trauma and PTSD offering a small validity check for the utility of the child response measures. Taken as a whole these findings suggest that childhood exposure to traumatic events may be a substantial predictor of subclinical psychopathology in normally developing children. Notably, none of the children in this study had previously identified psychiatric diagnoses by parent report, and very few children endorsed psychological symptoms above clinical thresholds (~10%) on the study measures.
The current findings have important practical applications. Child-reported trauma appears to be a risk factor for developing psychopathology even before psychological symptoms may be obvious to parents, teachers, or other observers. Of concern, people who self-report traumatic events—as opposed to data obtained from other sources (e.g., parents) —seem to be at particularly elevated risk for psychopathology (Newbury et al. 2018). Previous research and meta-analyses suggest that subthreshold symptoms of specific disorders may predict eventual clinical diagnoses (Kaymaz et al. 2012; Linscott and van Os 2012; Pietrzak et al. 2013; Wesselhoeft et al. 2013). We found that self-reported symptoms were positively correlated among themselves likely reflecting diffuse trauma-related distress that may not be easily observed by others, but these symptoms are all reliably linked to level of trauma exposure.
Surprisingly, parent-report measures of internalizing and externalizing behaviors did not correlate with trauma histories or any of the psychological and behavioral symptoms their children reported, which would be expected given the literature (Briggs-Gowan et al. 2012; Evans et al. 2008; Hunt et al. 2017; Vu et al. 2016). Children in our study reported objectively more symptoms than their parents did, and this was especially true for children in the high trauma group. We found that trauma level accounted for 31.6% of the variance in childrens’ internalizing behaviors as reported on the child SDQ, consistent with the literature linking childhood adverse events and internalizing symptoms (Heleniak et al. 2016; McLaughlin and Hatzenbuehler 2009; McLaughlin et al. 2009). Of concern, trauma accounted for less than 3.5% of the variance for internalizing behaviors on both the SDQ-P and CBCL parent measures. Even for readily observable externalizing behaviors that children may be reluctant to report, trauma still accounted for 18.5% of the variance for externalizing behaviors on the SDQ child measure, but the effect was only half that for parent report measures of externalizing behaviors. Notably trauma-related psychological risk does not covary with SES, counter to commonly held assumptions about at-risk youth being synonomous with low income youth.
Regarding our study limitations, we recognize that correlations between child-reported trauma and child-reported symptoms have respondent-based shared variance that is not present in correlations of child-reported trauma and parent-reported behaviors; however, child reports of trauma coincided most strongly with known trauma-related symptoms including PTSD, anxiety, depression and dissociation, reducing concern about shared variance. Second, despite collecting data in two urban clinics, our sample lacks racial diversity. Future research should include typically-developing children from racially diverse communities, as exposure to specific types of traumatic events has been shown to vary across race/ethnic groups (Roberts et al. 2011). Finally, we were not able to ask directly about physical or sexual abuse, so it is possible that these particular traumas were left out by some children. A complete trauma screen would be preferable; however, our results were significant despite the potential omission of an additional trauma by some children, which suggests that these findings are robust.
Given that traumatic life events are associated with diverse psychological symptoms in typically-developing children as young as 9 years old, our findings have clear, real-world implications. General subclinical psychological distress often predicts future pathology (McGorry and van Os 2013; Wigman et al. 2013), so we conclude that children who outwardly appear to be resilient to trauma may still have subclinical symptoms that would benefit from early intervention. This is a key practical application of our findings, because research has shown that early intervention protects against the effects of trauma (Roberts et al. 2009) and may be effective in preventing future diagnosable clinical disorders (Lenz and Hollenbaugh 2015). However, our findings also suggest that referring traumatized children to potentially beneficial early interventions may be difficult. According to our results, children, especially children who have experienced multiple traumas, have more psychological symptoms than their parents are aware of, so we cannot depend on parents to see the need for therapeutic services for their seemingly typically-developing children.
In conclusion, we propose that a brief trauma screen administered directly to children could help identify those children who are at risk for general mental health concerns and who could benefit from early therapeutic services. We show that trauma exposure is an efficient and effective marker of general psychological risk in preadolescent children; therefore, trauma screens, such as the one used in this study, could be implemented during physican visits or in schools. Then children with notable trauma histories could be referred and effectively linked to appropriate interventions (Garg et al. 2016) in hopes of reducing psychological issues before they reach diagnostic thresholds.
Funding
This work was supported by At Ease USA and the National Science Foundation [#1539067].
Compliance with Ethical Standards
Conflict of Interest
Mackenzie S. Mills—Reports no disclosures, Christine M. Embury—Reports no disclosures, Alicia K. Klanecky—Reports no disclosures, Maya M. Khanna—Reports no disclosures, Vince C. Calhoun—Reports no disclosures, Julia M. Stephen—Reports no disclosures, Yu-Ping Wong—Reports no disclosures, Tony W. Wilson—Reports no disclosures, Amy S. Badura-Brack—Reports no disclosures.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mackenzie S. Mills, Email: mackenziemills@creighton.edu
Christine M. Embury, Email: christine.embury@unmc.edu
Alicia K. Klanecky, Email: aliciaklanecky@creighton.edu
Maya M. Khanna, Email: mayakhanna@creighton.edu
Vince D. Calhoun, Email: vcalhoun@mrn.org
Julia M. Stephen, Email: jstephen@mrn.org
Yu-Ping Wang, Email: wyp@tulane.edu.
Tony W. Wilson, Email: tony.w.wilson@gmail.com
Amy S. Badura-Brack, Email: AmyBaduraBrack@creighton.edu
References
- Achenbach TM, Rescorla LA. Manual for the ASEBA School-age Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, Dube SR, Giles WH. The enduring effects of abuse and related adverse experiences in childhood: A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience. 2006;256(3):174–186. doi: 10.1007/s00406-005-0624-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A, Costello EJ, Messer SC, Pickles A, Winder F, Silver D. The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research. 1995;5:237–249. [Google Scholar]
- Barratt, W. (2012, June 14). The Barratt simplified measure of social status (BSMSS). [blog post]. Retrieved from http://socialclassoncampus.blogspot.com/2012/06/barratt-simplified-measure-of-social.html
- Barzilay, R., Calkins, M.E., Moore, T.M., Wolf, D.H., Satterthwaite, T.D., Scott, J.C Cobb Scott J., Jones J. D., Benton T. D., Gur R. C. Gur, R.E. (2018). Association between traumatic stress load, psychopathology, and cognition in the Philadelphia neurodevelopmental cohort. Psychological Medicine, 1–10. doi:10.1017/S0033291718000880, 49. [DOI] [PubMed]
- Briere J. Trauma symptom checklist for children: Professional manual. Odessa, FL: Psychological Assessment Resources, Inc.; 1996. [Google Scholar]
- Briere, J., & Lanktree, C.B. (1995) The Trauma Symptom Checklist for Children (TSCC): Preliminary psychometric characteristics. Unpublished manuscript, Dept. of psychiatry, University of Southern California School of Medicine, Los Angeles, California.
- Briere J, Kaltman S, Green BL. Accumulated childhood trauma and symptom complexity. Journal of Traumatic Stress. 2008;21(2):223–226. doi: 10.1002/jts.20317. [DOI] [PubMed] [Google Scholar]
- Briggs-Gowan MJ, Carter AS, Ford JD. Parsing the effects violence exposure in early childhood: Modeling developmental pathways. Journal of Pediatric Psychology. 2012;37(1):11–22. doi: 10.1093/jpepsy/jsr063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H, Keyes KM, McLaughlin KA, Meyers JL, Dunn EC, Martins SS. Childhood trauma and illicit drug use in adolescence: A population-based National Comorbidity Survey Replication-Adolescent Supplement Study. Journal of the American Academy of Child and Adolescent Psychiatry. 2016;55(8):701–708. doi: 10.1016/j.jaac.2016.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carliner H, Gary D, McLaughlin KA, Keyes KM. Trauma exposure and externalizing disorders in adolescents: Results from the National Comorbidity Survey Adolescent Supplement. Journal of the American Academy of Child & Adolescent Psychiatry. 2017;56(9):755–764. doi: 10.1016/j.jaac.2017.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cirino P, Sevcik R, Wolf M, Lovett M, Morris R. Measuring socioeconomic status: Reliability and preliminary validity of different approaches. Assessment. 2002;9(2):145–155. doi: 10.1177/10791102009002005. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Erkanli A, Fairbank JA, Angold A. The prevalence of potentially traumatic events in childhood and adolescence. Journal of Traumatic Stress. 2002;15(2):99–112. doi: 10.1023/A:1014851823163. [DOI] [PubMed] [Google Scholar]
- Davis J, Smith T, Hodge R, Nakao K, Treas J. Occupational prestige ratings from the 1989 general social survey. Ann Arbor MI: Inter-university Consortium for Political and Social Research; 1991. [Google Scholar]
- Daviss WB, Birmaher B, Melhem NA, Axelson DA, Michaels SM, Brent DA. Criterion validity of the mood and feelings questionnaire for depressive episodes in clinic and non-clinic subjects. The Journal of Child Psychology and Psychiatry. 2006;47(9):927–934. doi: 10.1111/j.1469-7610.2006.01646.x. [DOI] [PubMed] [Google Scholar]
- Diamond A. Normal development of prefrontal cortex from birth to young adulthood: Cognitive functions, anatomy, and biochemistry. In: Stuss DT, Knight RT, editors. Principles of frontal lobe function. London, UK: Oxford University Press; 2002. pp. 466–503. [Google Scholar]
- Edwards V, Holden G, Felitti V, Anda R. Relationship between multiple forms of childhood maltreatment and adult mental health in community respondents: Results from the adverse childhood experiences study. American Journal of Psychiatry. 2003;160(8):1453–1460. doi: 10.1176/appi.ajp.160.8.1453. [DOI] [PubMed] [Google Scholar]
- Evans SE, Davies C, DiLillo D. Exposure to domestic violence: A meta-analysis of child and adolescent outcomes. Aggression and Violent Behavior. 2008;13(2):131–140. doi: 10.1016/j.avb.2008.02.005. [DOI] [Google Scholar]
- Felitti V, Anda R, Nordenberg D, Williamson D, Spitz A, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults the adverse childhood experiences (ACE) study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/S0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Fernandes V, Osório FL. Are there associations between early emotional trauma and anxiety disorders? Evidence from a systematic literature review and meta-analysis. European Psychiatry. 2015;30(6):756–764. doi: 10.1016/j.eurpsy.2015.06.004. [DOI] [PubMed] [Google Scholar]
- Garg A, Boynton-Jarrett R, Dworkin PH. Avoiding the unintended consequences of screening for social determinants of health. JAMA. 2016;316(8):813–814. doi: 10.1001/jama.2016.9282. [DOI] [PubMed] [Google Scholar]
- Goodman R. The strengths and difficulties questionnaire: A research note. Journal of Child Psychology and Psychiatry. 1997;38:581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Goodman R. Psychometric properties of the strengths and difficulties questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2001;40(11):1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- Graham-Bermann SA, Seng J. Violence exposure and traumatic stress symptoms as additional predictors of health problems in high-risk children. The Journal of Pediatrics. 2005;146(3):349–354. doi: 10.1016/j.jpeds.2004.10.065. [DOI] [PubMed] [Google Scholar]
- Green J, McLaughlin K, Berglund P, Gruber M, Sampson N, Zaslavsky A, Kessler R. Childhood adversities and adult psychiatric disorders in the National Comorbidity Survey Replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagan MJ, Sulik MJ, Lieberman AF. Traumatic life events and psychopathology in a high risk, ethnically diverse sample of young children: A person-centered approach. Journal of Abnormal Child Psychology. 2016;44(5):833–844. doi: 10.1007/s10802-015-0078-8. [DOI] [PubMed] [Google Scholar]
- Hardt J, Rutter M. Validity of adult retrospective reports of adverse childhood experiences: Review of the evidence. Journal of Child Psychology and Psychiatry. 2004;45(2):260–273. doi: 10.1111/j.1469-7610.2004.00218.x. [DOI] [PubMed] [Google Scholar]
- Heleniak C, Jenness JL, Stoep AV, McCauley E, McLaughlin KA. Childhood maltreatment exposure and disruptions in emotion regulation: A Transdiagnostic pathway to adolescent internalizing and externalizing psychopathology. Cognitive Therapy and Research. 2016;40(3):394–415. doi: 10.1007/s10608-015-9735-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodges M, Godbout N, Briere J, Lanktree C, Gilbert A, Kletzka NT. Cumulative trauma and symptom complexity in children: A path analysis. Child Abuse & Neglect. 2013;37:891–898. doi: 10.1016/j.chiabu.2013.04.001. [DOI] [PubMed] [Google Scholar]
- Hollingshead, August B. (1957). Two factor index of social position. Unpublished manuscript, Department of Sociology, Yale University, New Haven, Connecticut
- Hollingshead AB. Four factor index of social status. Department of Sociology, Yale University, New Haven, CT: Unpublished manuscript; 1975. [Google Scholar]
- Hughes K, Bellis M, Hardcastle K, Sethi D, Butchart A, Mikton C, et al. The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health. 2017;2(8):e356–e366. doi: 10.1016/S2468-2667(17)30118-4. [DOI] [PubMed] [Google Scholar]
- Hunt T, Slack K, Berger L. Adverse childhood experiences and behavioral problems in middle childhood. Child Abuse & Neglect. 2017;67:391–402. doi: 10.1016/j.chiabu.2016.11.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N, Weiser M, Lataster T, van Os J. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychological Medicine. 2012;42(11):2239–2253. doi: 10.1017/S0033291711002911. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Avenevoli S, McLaughlin KA, Green JG, Lakoma MD, Petukhova M, Pine DS, Sampson NA, Zaslavsky AM, Merikangas KR. Lifetime comorbidity of DSM-IV disorders in the NCS-R adolescent supplement (NCS-A) Psychological Medicine. 2012;42(9):1997–2010. doi: 10.1017/S0033291712000025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lenz AS, Hollenbaugh KM. Meta-analysis of trauma-focused cognitive behavioral therapy for treating PTSD and co-occurring depression among children and adolescents. Counseling Outcome Research and Evaluation. 2015;6(1):18–32. doi: 10.1177/2150137815573790. [DOI] [Google Scholar]
- Linscott R, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: On the pathway from proneness to persistence to dimensional expression across mental disorders. Psychological Medicine. 2012;43(6):1–17. doi: 10.1017/S0033291712001626. [DOI] [PubMed] [Google Scholar]
- Mandelli L, Petrelli C, Serretti A. The role of specific early trauma in adult depression: A meta-analysis of published literature. Childhood trauma and adult depression. European Psychiatry. 2015;30(6):665–680. doi: 10.1016/j.eurpsy.2015.04.007. [DOI] [PubMed] [Google Scholar]
- McGorry P, van Os J. Redeeming diagnosis in psychiatry: Timing versus specificity. The Lancet. 2013;381(9863):343–345. doi: 10.1016/S0140-6736(12)61268-9. [DOI] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML. Mechanisms linking stressful life events and mental health problems in a prospective, community-based sample of adolescents. Journal of Adolescent Health. 2009;44:153–160. doi: 10.1016/j.jadohealth.2008.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Hatzenbuehler ML, Hilt LM. Emotion dysregulation as a mechanism linking peer victimization to the development of internalizing symptoms among youth. Journal of Consulting and Clinical Psychology. 2009;77:894–904. doi: 10.1037/a0015760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Breslau J, Green JG, Lakoma MD, Sampson NA, Zaslavsky AM, Kessler RC. Childhood socio-economic status and the onset, persistence, and severity of DSM-IV mental disorders in a US national sample. Social Science & Medicine (1982) 2011;73(7):1088–1096. doi: 10.1016/j.socscimed.2011.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meng X, Fleury M-J, Xiang Y-T, Li M, D’Arcy C. Resilience and protective factors among people with a history of childhood maltreatment: A systematic review. Social Psychiatry and Psychiatric Epidemiology. 2018;53(5):453–475. doi: 10.1007/s00127-018-1485-2. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He J-PP, Burstein M, Swanson SA, Avenevoli S, Cui L, et al. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication--Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(10):980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller M, Brock R. The effect of trauma on the severity of obsessive-compulsive spectrum symptoms: A meta-analysis. Journal of Anxiety Disorders. 2017;47:29–44. doi: 10.1016/j.janxdis.2017.02.005. [DOI] [PubMed] [Google Scholar]
- Newbury JB, Arseneault L, Moffitt TE, Caspi A, Danese A, Baldwin JR, Fisher HL. Measuring childhood maltreatment to predict early-adult psychopathology: Comparison of prospective informant-reports and retrospective self-reports. Journal of Psychiatric Research. 2018;96:57–64. doi: 10.1016/j.jpsychires.2017.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Nierop M, Viechtbauer W, Gunther N, van Zelst C, de Graaf Ten Have M, et al. Childhood trauma is associated with a specific admixture of affective, anxiety, and psychosis symptoms cutting across traditional diagnostic boundaries. Psychological Medicine. 2015;45(6):1277–1288. doi: 10.1017/S0033291714002372. [DOI] [PubMed] [Google Scholar]
- Pietrzak R, Kinley J, Afifi T, Enns M, Fawcett J, Sareen J. Subsyndromal depression in the United States: Prevalence, course, and risk for incident psychiatric outcomes. Psychological Medicine. 2013;43(7):1401–1414. doi: 10.1017/S0033291712002309. [DOI] [PubMed] [Google Scholar]
- Roberts NP, Kitchiner NJ, Kenardy J, Bisson JI. Systematic review and meta-analysis of multiple-session early interventions following traumatic events. American Journal of Psychiatry. 2009;166(3):293–301. doi: 10.1176/appi.ajp.2008.08040590. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41(1):71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seng JS, Graham-Bermann SA, Clark KM, McCarthy A, Ronis DL. Posttraumatic stress disorder and physical comorbidity among female children and adolescents: Results from service-use data. Pediatrics. 2005;116(6):e767–e776. doi: 10.1542/peds.2005-0608. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Decker KB, Pynoos RS. The University of California at Los Angeles post-traumatic stress disorder reaction index. Current Psychiatry Reports. 2004;6(2):96–100. doi: 10.1007/s11920-004-0048-2. [DOI] [PubMed] [Google Scholar]
- Steinberg AM, Brymer MJ, Kim S, Ghosh C, Ostrowski SA, Gulley K, Briggs EC, Pynoos RS. Psychometric properties of the UCLA PTSD reaction index: Part I. Journal of Traumatic Stress. 2013;26:1–9. doi: 10.1002/jts.21780. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, Ormrod R. The effect of lifetime victimization on the mental health of children and adolescents. Social Science & Medicine. 2006;62:13–27. doi: 10.1016/j.socscimed.2005.05.030. [DOI] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse T, Lataster T, Viechtbauer W, et al. Childhood adversities increase risk of psychosis: A meta-analysis of patient-control, prospective- and cross-section cohort studies. Schizophrenia Bulletin. 2012;38(4):661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vu N, Jouriles EN, McDonald R, Rosenfield D. Children's exposure to intimate partner violence: A meta-analysis of longitudinal associations with child adjustment problems. Clinical Psychology Review. 2016;46:25–33. doi: 10.1016/j.cpr.2016.04.003. [DOI] [PubMed] [Google Scholar]
- Warnick EM, Bracken MB, Kasl S. Screening efficiency of the child behavior checklist and strengths and difficulties questionnaire: A systematic review. Child and Adolescent Mental Health. 2008;13(3):140–147. doi: 10.1111/j.1475-3588.2007.00461.x. [DOI] [PubMed] [Google Scholar]
- Wesselhoeft R, Sorensen MJ, Heiervang ER, Bilenberg N. Subthreshold depression in children and adolescent- a systemic review. Journal of Affective Disorders. 2013;151(1):7–22. doi: 10.1016/j.jad.2013.06.010. [DOI] [PubMed] [Google Scholar]
- Wigman JTW, van Os J, Thiery E, Derom C, Collip D, Jacobs N, Wichers M. Psychiatric diagnosis revisited: Towards a system of staging and profiling combining nomothetic and idiographic parameters of momentary mental states. PLoS One. 2013;8(3):1–8. doi: 10.1371/journal.pone.0059559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annual Review of Clinical Psychology. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]