Abstract
Introduction:
The novel coronavirus has spread rapidly around the world with particularly high mortality in the elderly. Care and nursing homes have become the sites of greatest concentration of cases. We intended to review 30-day mortality of COVID-19 patients with hip fractures. This is relevant given the disease impact in this age group.
Methods:
Medline and Embase databases were searched for relevant studies linked to mortality and morbidity in COVID-19 patients who have undergone non-elective hip surgeries using the keywords “COVID-19”OR “SARS-cov-2”OR “Coronavirus Infections”; AND “Surgery”OR “Hip”OR “Fracture”OR “Orthopedics.” We included all patients with hip fractures, but excluded pathological fractures and other non-traumatic hip pathologies. Four-hundred and eighty-one articles were identified for screening, in addition to an unpublished case-series of 67 patients that have 3 cases turned positive for COVID 19, yielding a total of 50patients for the final review.
Results:
The study included 4 articles published until May 9th 2020 and a case-series: 26(52%) patients were females; the median age was 86years; hypertension(53.6%), diabetes mellitus type II(28.6%), and coronary artery heart disease(25%) were the most common comorbidities; 34(68%) patients had intertrochanteric hip fracture and 16(32%) patients had femoral neck fractures; 22(59.5%) patients underwent cephalomedullary nail fixation, 12(32.4%) patients had hemiarthroplasty, and for 3(8.1%) patients, the type of surgery was not documented; 20(40%) patients died(12patients died before the surgery and 8died after surgery at a median time of 3days), 29(76.3%) patients had an unremarkable course throughout hospitalization and were discharged including 1(2.6%) patient managed non-operatively, and 1(2.6%) patient was admitted to the ICU after the surgery but eventually discharged.
Conclusion:
COVID-19 infected elderly patients have a higher 30-days mortality rate compared to non-COVID-19 infected cases. Further studies are warranted to look at the morbidity and mortality rates in COVID-19 positive patients with hip fractures and to investigate how these outcomes can be improved.
Level of evidence:
Level IV
Keywords: COVID 19, SARS-cov-2, coronavirus infections, surgery, hip, fracture, orthopedics
Background
The outbreak of coronavirus disease 2019 (COVID-19) caused by the 2019 novel coronavirus (SARS-CoV-2) began in Wuhan, Hubei Province, China in December 2019, and has rapidly spread throughout the world forcing near total shut down of most countries.1-3 The pandemic has overwhelmed healthcare systems, especially intensive care units (ICU), in the world. To minimize the risk of coronavirus spread, and to conserve manpower and resources, elective orthopaedic procedures were suspended in most countries. Most guidelines recommended hospital admission only for those patients who needed it. They further recommended surgical treatment only where its results are superior to non-operative treatment.4-7 Existing literature suggests that COVID-19 affects most severely older patients and those with comorbidities.8 A group that has attracted little attention are those with hip fractures.9-12 Generally, hip fractures are associated with increased morbidity and a 30-day mortality rate of 7–10%.13 To date, there is a dearth of studies looking into the morbidity and mortality rates among COVID-19 patients with hip fractures. We, therefore, aim from the current review to investigate the 30-day mortality caused by COVID-19 in this group of patients.
Methods
Search Strategy
The research question and inclusion criteria for individual studies were established prior to searching databases. Online databases (Embase and Medline) were used to find literature related to mortality and morbidity in COVID-19 patients who have undergone urgent hip surgeries. PubMed was also screened but it added less relevant articles compared to other databases as MeSH terms were not established by the time of search date. Key words included were “COVID-19” OR “SARS-cov-2” OR “Coronavirus Infections”; AND “Surgery” OR “Hip” OR “Fracture” OR “Orthopedics.” The search was conducted on May 9th, 2020 and yielded a total of four-hundred and eighty-one articles from both databases, without any restriction on language or date of publication (Table 1).
Table 1.
Search Strategy of Embase and Medline Databases.
| Embase May 9th 2020 | Total articles |
|---|---|
| 1) “COVID 19” OR “SARS-cov-2” OR “Coronavirus Infections” | 10389 |
| 2) “Surgery” OR “Hip” OR “Fracture” OR “Orthopedics” | 3813393 |
| 3) 1 and 2 | 258 |
| Medline May 9th 2020 | 11806 |
| 1) “COVID 19” OR “SARS-cov-2” OR “Coronavirus Infections” | 2849777 |
| 2) “Surgery” OR “Hip” OR “Fracture” OR “Orthopedics” | 223 |
| 3) 1 and 2 | |
| Total from Embase and Medline | 481 |
The following inclusion criteria were used: (1) all levels of evidence irrespective of the study type, (2) male and female patients with no age limitation, and (3) all COVID-19 patients with hip fractures. We excluded patients with (1) pathological fractures, (2) non-hip fractures, and (3) non-traumatic hip pathologies.
Study Selection
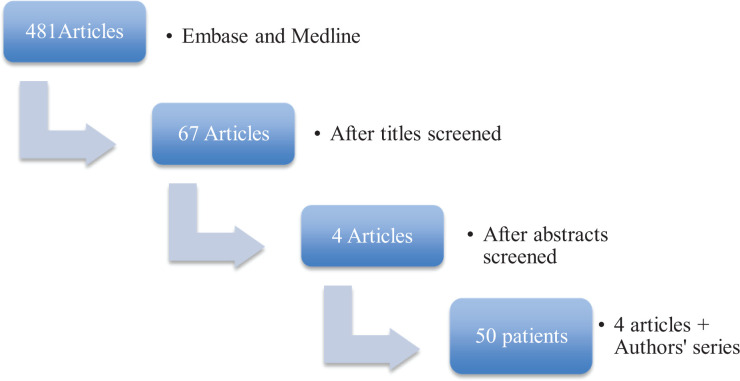
Combined results of all searches produced four-hundred and eighty-one articles. Titles and abstracts were screened, yielding a total of 4 studies that satisfied our inclusion and exclusion criteria. All reviewers performed a full-text review of the 4 eligible studies and case-series (Figure 1).
Figure 1.
Flow chart illustrating the article screening process.
Data Abstraction
One reviewer abstracted relevant study data from the final pool of the included studies and recorded them on a spreadsheet. These included study and publication information (author, year of publication, study design, level of evidence, and sample size), patients’ data (age, sex, comorbidities, and pathology), surgical details (type of fixation), outcomes (acute respiratory distress syndrome “ARDS,” respiratory failure, intensive care unit “ICU” admission, and death).
An unpublished case-series of 67 patients during COVID-19 outbreaks attended orthopaedic clinic at the University of Verona, Italy until May 14th, 2020 revealed 3 patients were COVID-19 infected with hip fracture who satisfy our inclusion criteria, and therefore, were added to the total number of patients included.
Results
A total of 50 patients were included in the final results. The age of the patients ranges from 50 to 100 years with a median age of 86 years. Female patients were 26 (52%). All the fractures were due to low energy injury except for 1 patient with traumatic brain injury who had a high-velocity (traffic) accident. Nearly 56% of patients had 1 or more comorbidities: hypertension (53.6%), diabetes mellitus type II (28.6%), and coronary artery heart disease (25%) were the most common comorbidities; the medical comorbidities were not reported in 22 patients. Thirty-four (68%) patients had intertrochanteric fracture and 16 (32%) patients had femoral neck fractures. Twenty-two (59.5%) patients underwent cephalomedullary nail fixation, 12 (32.4%) patients underwent hemiarthroplasty, and for 3 (8.1%) patients, the type of surgery was not documented. Twelve (24%) patients died before the surgery and 8 (16%) patients died after the surgery (total of 20 patients, 40%). The time from surgery to death ranged from 1 to 16 days, with a median of 3 days. Twenty-nine (76.3%) patients had an unremarkable course throughout hospitalization and were discharged including 1 (2.6%) patient managed non-operatively, and 1 (2.6%) patient was admitted to the ICU after the surgery but eventually discharged (Table 2).
Table 2.
Studies Included for Review.
| Study | LOE | Sample Size | COVID Positive | Patients | Age | Sex | Comorbidities | Pathology | Type of Surgery | Outcome | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Mi et al. 2020 6 | IV | 10 | 3 | 1 | 50 | F | HTN, DM | Intertrochanteric fracture | CMN | ICU admission(ARDS/RF), discharged |
| 2 | 79 | F | Osteoporosis | Femoral neck fracture | HA | Unremarkable | |||||
| 3 | 76 | M | Cirrhosis, Alzheimer disease | Intertrochanteric fracture | CMN | Death | |||||
| 4 | 80 | F | HTN, DM, CAHD | Intertrochanteric fracture | x | ICU admission (ARDS/RF), Death | |||||
| 5 | 84 | F | HTN, Osteoporosis | Intertrochanteric fracture | x | Death | |||||
| 6 | 85 | M | Brain injury | Intertrochanteric fracture | x | Death | |||||
| 2 | Lei et al. 2020 7 | III | 34 | 2 | 1 | 83 | M | HTN, CAHD, CVD | Femoral neck fracture | HA | ICU admission (ARDS/RF), Death |
| 2 | 84 | F | CAHD | Femoral neck fracture | HA | Unremarkable | |||||
| 3 | Catellani et al. 2020 8 | IV | 16 | 13 | 1 | 89 | F | HTN, DM, MR | Intertrochanteric fracture | CMN | Unremarkable |
| 2 | 89 | F | HTN, DM, HypoT4, DAS | Femoral neck fracture | HA | Unremarkable | |||||
| 3 | 84 | M | HTN, CAHD | Femoral neck fracture | HA | Unremarkable | |||||
| 4 | 84 | M | HTN, Hepatitis C | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 5 | 90 | M | HTN, CAHD, CHF | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 6 | 90 | F | HTN, remote CVA, VD, CHF | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 7 | 74 | M | HTN, DAS, Obesity | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 8 | 82 | M | CKD, BPH | Intertrochanteric fracture | CMN | Death | |||||
| 9 | 86 | M | HTN, HypoT4 | Intertrochanteric fracture | HA | Death | |||||
| 10 | 88 | M | DM, CAHD, BPH | Femoral neck fracture | HA | Death | |||||
| 11 | 85 | M | CAHD, BPH | Intertrochanteric fracture | HA | Unremarkable | |||||
| 12 | 82 | M | HTN, remote CVA | Femoral neck fracture | CMN | Unremarkable | |||||
| 13 | 85 | F | DAS | Femoral neck fracture | CMN | Death | |||||
| 14 | 79 | F | HTN, HypoT4, Obesity | Intertrochanteric fracture | x | Death | |||||
| 14 | 80 | F | DM | Intertrochanteric fracture | x | Death | |||||
| 16 | 82 | M | DM, CKD | Intertrochanteric fracture | x | Death | |||||
| 4 | Muñoz-Vives et al. 2020 9 | IV | 136 | 23 | 1 | 89 | M | NR | Intertrochanteric fracture | CMN | Death |
| 2 | 93 | M | NR | Intertrochanteric fracture | CMN | Death | |||||
| 3 | 85 | F | NR | Intertrochanteric fracture | x | Death | |||||
| 4 | 100 | M | NR | Intertrochanteric fracture | x | Death | |||||
| 5 | 89 | F | NR | Intertrochanteric fracture | x | Death | |||||
| 6 | 95 | F | NR | Intertrochanteric fracture | x | Death | |||||
| 7 | 88 | F | NR | Femoral neck fracture | x | Death | |||||
| 8 | 85 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 9 | 90 | M | NR | Intertrochanteric fracture | NR | Unremarkable | |||||
| 10 | 95 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 11 | 89 | F | NR | Femoral neck fracture | NR | Unremarkable | |||||
| 12 | 87 | M | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 13 | 77 | F | NR | Femoral neck fracture | HA | Unremarkable | |||||
| 14 | 92 | M | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 15 | 86 | M | NR | Femoral neck fracture | NR | Unremarkable | |||||
| 16 | 91 | M | OSAHS | Femoral neck fracture | HA | Unremarkable | |||||
| 17 | 94 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 18 | 85 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 19 | 88 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 20 | 97 | M | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 21 | 84 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| 22 | 72 | M | NR | Femoral neck fracture | HA | Unremarkable | |||||
| 23 | 89 | F | NR | Intertrochanteric fracture | CMN | Unremarkable | |||||
| Authors’ case series | IV | 67 | 3 | 1 | 100 | F | Dementia | Intertrochanteric fracture | CM | Unremarkable | |
| 2 | 91 | M | HTN, DM, AF, CHF, AS, CKD, BPH | Femoral neck fracture | x | Death | |||||
| 3 | 89 | F | DAS | Femoral neck fracture | HA | Unremarkable | |||||
HTN: Hypertension; DM: Diabetes Mellitus type II; CAHD: Coronary Artery Heart Disease; MR: Mitral Regurgitation; HypoT4: Hypothyroidism; DAS: Depression and Anxiety Syndrome; CHF: Congestive Heart Failure; CVA: Cerebrovascular Accident; VD: Vascular Dementia; BPH: Benign Prostatic Hyperplasia; CKD: Chronic Kidney Disease; OSAHS: Obstructive Sleep Apnoea Hypopnoea Syndrome; AF: Atrial Fibrillation; AS: Aortic Stenosis; CMN: Cephalomedullary Nail; HA: Hemiarthroplasty; ARDS: Acute Respiratory Distress Syndrome; RF: Respiratory Failure; NR: Not Reported, X: No Surgery, CM: Conservative Management.
Discussion
Many national guidelines have recommended that patients with hip fractures undergo surgery within 48 hours of admission long before the appearance of COVID-19.14,15 Various guidelines set during COVID-19 pandemic have, also, identified patients with hip fractures among those requiring urgent surgical intervention.4-7 Pre-COVID-19 studies have reported a 30-day mortality rate of 7-10% and postoperative pulmonary complications rate of 4.9%.12,16
In the present review of 50 patients from 4 studies and case series, the overall death rate is 40% in COVID-19 positive patients. The death rate was mainly observed among elderly patients in their seventh and eighth decades of life. This finding is consistent with the trend of hip fracture in non COVID-19 elderly patients.17 One study reported only 14-days follow-up which may underestimate the 30-day mortality rate.13
It is clear from this small group that the mortality rate is much higher than in the non-COVID-19 patients with hip fractures. The virus’s predilection to target the lungs combined with the severe discomfort resulting from hip fractures leading to poor respiratory effort seem to be a plausible explanation for these patients’ poor condition on admission to hospital and high preoperative mortality rate. The comparatively lower postoperative mortality rate may reflect the positive pain relieving effect of surgical treatment of the fractures allowing for early rehabilitation and postural drainage of the lungs. What is not clear are the reasons why so many patients are admitted in such poor condition with such high preoperative mortality rate. It is noteworthy that Do Not Resuscitate (DNR) status was not documented, and therefore, these patients were to be denied ICU treatment, ventilator support, and cardiopulmonary resuscitation (CPR) when becoming seriously-ill. Not only being symptomatic with COVID-19, but also asymptomatic positive testing and, even simply, coming from a high COVID-19 environment (like a nursing home) seems to increase the mortality rate in patients with hip fractures.10,13 One possible explanation is that these patients may have had a false negative test.
This review has a number of limitations. The sample size is small. It included level 3 and 4 retrospective studies that are prone to selection, recall or misclassification bias, subject to confounding and cannot determine causation, only association. Moreover, the studies have some missing data and the reported number of COVID-19 positive patients with hip fractures since this pandemic has started is low to run any subgroup analysis. The authors were contacted for the missing data but, unfortunately, because of the retrospective nature of these studies most of the requested data were not available. In addition, one of the included studies was published in a non-peer review journal, however, only 2 COVID-19 positive patients with hip fractures were included in that study.
In summary, the review revealed that the combination of COVID-19 positive and hip fracture carries a particularly high 30-days mortality rate compared to the non-COVID-19 patients with hip fracture. Clearly, greater protective measures from both COVID-19 exposure and hip fractures need to be instituted for this vulnerable group of patients. Given the evolving nature of the COVID-19 pandemic and its vast and rapid spread among population, especially nursing homes, it is important to report all data together so that a greater understanding of the disease in this group of patients is attained. Further studies are warranted to look at the morbidity and mortality rates in COVID-19 positive patients with hip fractures and to investigate how these outcomes can be improved.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: We disclose that the authors of this study have no commercial or financial association with regards to this project and, therefore, have no affiliation that may pose a conflict of interest with the manuscript enclosed. We had full access to all the data in the study and take responsibility for the integrity and accuracy of the data, as well as the decision to submit for publication.
ORCID iD: Humaid Al Farii, MD, MRCS (Ir)  https://orcid.org/0000-0001-8813-1686
https://orcid.org/0000-0001-8813-1686
Salim Al Rawahi, MD  https://orcid.org/0000-0002-1521-906X
https://orcid.org/0000-0002-1521-906X
References
- 1. Jernigan DB. Update: public health response to the coronavirus disease 2019 outbreak—United States, February 24, 2020 MMWR Morb Mortal Wkly Rep. 2020;69(8):216–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Holshue ML, DeBolt C, Lindquist S, et al. First case of 2019 novel coronavirus in the United States. N Engl J Med. 2020;382(10):929–936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Silverstein WK, Stroud L, Cleghorn GE, et al. First imported case of 2019 novel coronavirus in Canada, presenting as mild pneumonia. Lancet. 2020;395(10225):734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Centers for Medicare and Medicaid Services. CMS adult elective surgery and procedure recommendations: limit all non-essential planned surgeries and procedures, including dental, until further notice. Published March 15, 2020. Accessed July, 2020 https://www.cms.gov/files/document/31820-cms-adult-elective-surgery-and-procedures-recommendations.pdf
- 5. American College of Surgeons. ACS recommendations for management of elective surgical procedures. Published March 13, 2020. Accessed April 7, 2020 https://www.facs.org/covid-19/clinical-guidance/elective-surgery
- 6. Prada C, Yaping C, Poolman R, et al. COVID-19 evidence-based scoping review, a unifying report of global recommendations. Orthoevidence. 2020;1:37–45. [Google Scholar]
- 7. British Orthopaedic Association. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Published 2020. Accessed April 17, 2020 https://www.boa.ac.uk/resources/covid-19-boasts-combined.html
- 8. Abbatecola AM, Antonelli-Incalzi R. COVID-19 spiraling of frailty in older Italian patients. J Nutr Health Aging. 2020;24(5):453–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mi B, Chen L, Xiong Y, Xue H, Zhou W, Liu G. Characteristics and early prognosis of COVID-19 infection in fracture patients. J Bone Joint Surg Am. 2020;102(9):750–758. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. E Clin Med. 2020;23:100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Catellani F, Coscione A, D’Ambrosi R, Usai L, Roscitano C, Fiorentino G. Treatment of proximal femoral fragility fractures in patients with COVID-19 during the SARS-CoV-2 outbreak in Northern Italy. J Bone Joint Surg Am. 2020;102(12):e58 (online ahead of print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Daugaard CL, Jørgensen HL, Riis T, Lauritzen JB, Duus BR, Mark SV. Is mortality after hip fracture associated with surgical delay or admission during weekends and public holidays? A retrospective study of 38, 020 patients. Acta Orthopaedica. 2012;83(6):609–613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Muñoz Vives JM, Jornet-Gibert M, C´amara-Cabrera J, et al. Mortality rates of patients with proximal femoral fracture in a worldwide pandemic. J Bone Joint Surg Am. 2020;102(13):e69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. National Clinical Guideline Centre. The management of hip fracture in adults. NICE. Published 2011. Accessed May 8, 2020 https://www.nice.org.uk/guidance/cg124/evidence/full-guideline-183081997
- 15. American academy of orthopaedic surgeons: management of hip fractures in the elderly: evidence-based clinical practice guideline. J Am Acad Orthop Sur. Published September 2014. Accessed May 8, 2020 https://aaos.org/globalassets/quality-and-practice-resources/hip-fractures-in-theelderly/management_of_hip_fractures_in_the_elderly-7-24-19
- 16. Lv H, Yin P, Long A, et al. Clinical characteristics and risk factors of postoperative pneumonia after hip fracture surgery: a prospective cohort study. Osteoporos Int. 2016;27(10):3001–3009. [DOI] [PubMed] [Google Scholar]
- 17. Jean S, O/Donnell S, Lagace C, et al. Trends in hip fracture rates in Canada: an age-period-cohort analysis. J Bone Miner Res. 2013;28(6):1283–1289. [DOI] [PMC free article] [PubMed] [Google Scholar]