ABSTRACT
We report the case of a 68-year-old woman who had abdominal pain and slightly elevated biliary enzymes. Magnetic resonance cholangiopancreatography detected biliary duct stenosis, while contrast-enhanced magnetic resonance imaging showed that the right hepatic artery transversed the extrahepatic bile duct at the level of bifurcation of the bile duct. We performed endoscopic retrograde cholangiopancreatography and peroral cholangioscopy with the SpyGlass DS™ system. Then, mild extrinsic pulsatile compression of the bile duct was observed at stricture level with an intact bile duct epithelium. Therefore, she was diagnosed with right hepatic artery syndrome and underwent cholecystectomy. Six months later, her biliary enzyme level decreased, and the recurrence of pain gradually decreased.
Keywords: diagnostic imaging, extrahepatic cholestasis
Anatomical characteristics of the hepatic portal are the concentration of luminal structures such as the bile duct, portal vein, and hepatic artery. In other organs (e.g. esophagus, duodenum, ureter), vessels compress the adjacent organ and disturb the flow of their contents. However, it has rarely been reported that the bile ducts are compressed by the right hepatic artery (RHA).1,2,3,4,5,6,7 In 1984, Tsuchiya reported the first case of jaundice and hepatolithiasis due to RHA compression on the common hepatic duct.1 Since then, this condition has been called RHA syndrome.
PATIENT REPORT
The patient was a 68-year-old woman who visited a nearby hospital with a chief complaint of right upper quadrant pain. She was diagnosed with biliary dyskinesia, and the administration of flopropione improved symptoms temporarily. Three years later, her body weight was reduced by 3 kg after an aortic valve replacement surgery for aortic valve stenosis, and the same symptoms presented. A laboratory examination revealed the following: alkaline phosphatase, 787 IU/L; gamma-glutamyl transpeptidase, 93 IU/L; aspartate aminotransferase, 23 U/L; alanine aminotransferase, 18 U/L; CEA, 3.3 ng/mL; CA19-9, 35.1 U/mL; Span-1, 24 U/mL; and DUPAN-2, < 25 U/mL. Her anti-mitochondrial antibody test was negative. Thus, she was referred to our hospital for further examination and treatment.
The preferred diagnostic procedure included the use of a contrast agent, however, a past allergic reaction prevented us from using it. An abdominal plain computed tomography (CT) was conducted instead, which did not show any abnormal findings. However, magnetic resonance cholangiopancreatography (MRCP) revealed a stricture in both right and left hepatic ducts (Fig. 1) and wall thickening of the gallbladder. Endoscopic ultrasonography (EUS) could not detect wall thickening or tumors in the strictures of the bile duct, but was able to visualize aberrant RHA and gallbladder wall thickening due to Rokitansky-Aschoff sinuses (RAS). Contrast-enhanced magnetic resonance imaging (MRI) showed RHA transversed the extra hepatic bile duct at the level of bifurcation of the bile duct (Fig. 2). At this point, we suspected RHA syndrome and planned further examination. Endoscopic retrograde cholangiopancreatography (ERCP) showed the pressure excursion of the bile duct, and intraductal ultrasonography (IDUS) confirmed that the blood vessel was adjacent to the compressed site (Fig. 3). Then we performed a peroral cholangioscopy (POCS) with the SpyGlass DSTM system (Boston Scientific Corp, Natick, MA) and observed a mild extrinsic pulsatile compression of the bile ducts at the stricture level (Fig. 4). There was no epithelial neoplasm at the site of pulsatile compression. Owing to stenosis of the bile duct, we considered malignant tumor in differential diagnosis during the initial examination; however, POCS revealed pulsatility stenosis, and we confirmed that the diagnosis of RHA syndrome. However, there were abdominal symptoms and hepatic dysfunction, and we contemplated that follow-up observation was not valid. Meanwhile, adenomyomatosis of the gallbladder was observed, and the patient was scheduled to undergo cholecystectomy; thus, we detected follow-up RHA syndrome after cholecystectomy. The biliary tree enzyme level decreased (alkaline phosphatase, 317 IU/L; gamma-glutamyl transpeptidase, 65 IU/L), and the frequency of pain gradually decreased 6 months after cholecystectomy.
Fig. 1.
MRCP; Both right and left hepatic ducts are constricted.
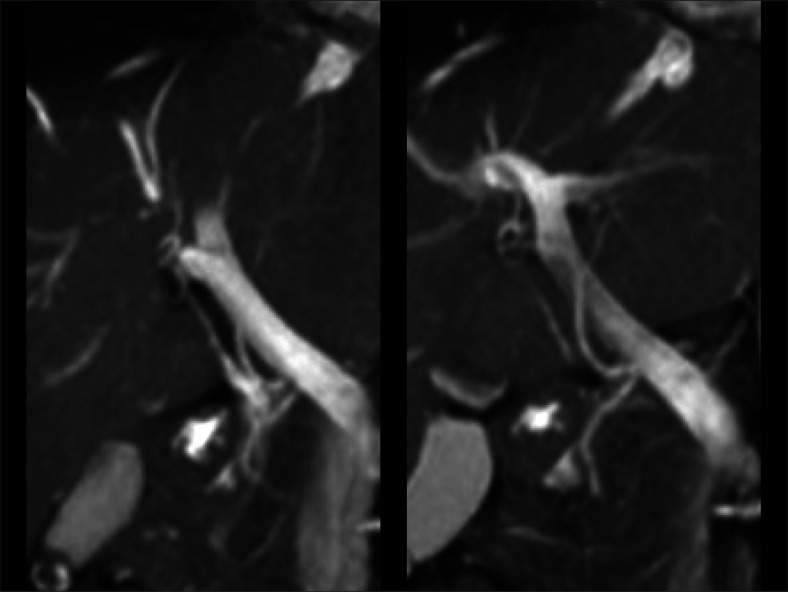
Fig. 2.
Contrast-enhanced MRI showing RHA transversed the extra hepatic bile duct at the level of bifurcation of the bile duct.
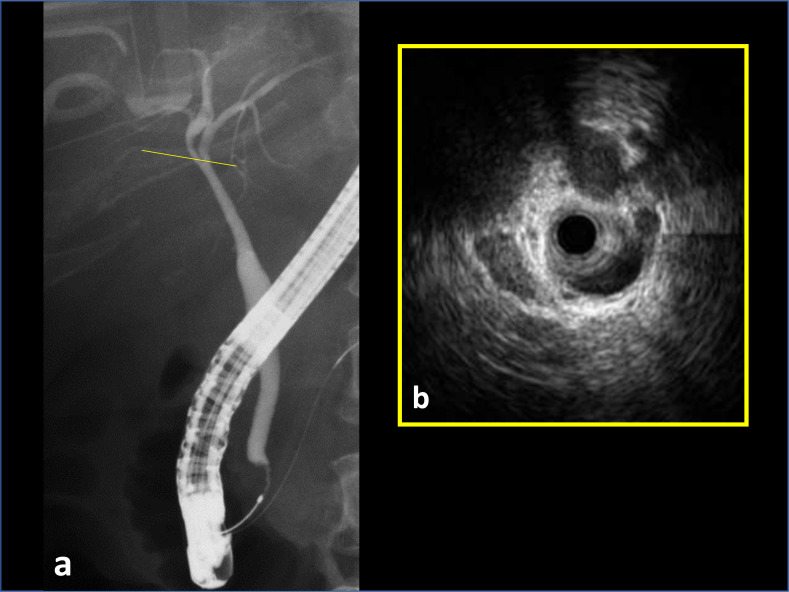
Fig. 3. a.
: ERCP showing the pressure excursion of the bile duct. b: IDUS showing that the blood vessel was adjacent to the same site.
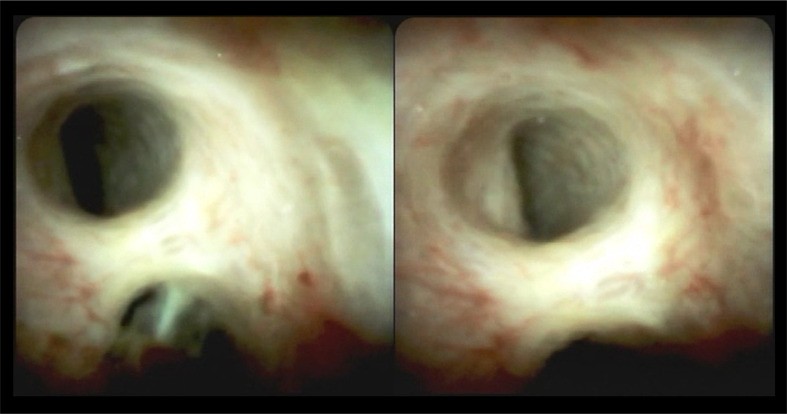
Fig. 4.
POCS using SpyGlass DS™ system: Mild extrinsic pulsatile compression of the bile ducts at the stricture level with an intact bile duct epithelium.
DISCUSSION
Normally, the hepatic artery courses between the extrahepatic bile duct and the portal vein. Aberrant and replaced RHAs are well-known variants. Koops reported that normal anatomy of the hepatic artery was found in 79.1% patients and the anomalous arterial patterns in the remaining patients.8 Tsuchiya reported that 11 (14%) among 79 patients who underwent angiographies or operations due to intrahepatic stone showed the RHA anteriorly crossing to the bile duct.1 He defined RHA syndrome as a variety of hepatobiliary symptoms caused by compression of the bile duct by the RHA. We searched PubMed with the keyword “right hepatic artery syndrome” and selected a report that was published in an English journal, met the definition of RHA syndrome, and could identify age, gender, and symptoms of the case. As a result, eight case reports were found in seven literature. (Table 1). Five cases were associated with gallstones, of which 3 cases were proximal to the compression site, 1 case was distal to the compression site, and 1 case was in the gallbladder. In RHA syndrome, the formation of gallstone is attributed to the bile stasis caused by compression of the common bile duct,1 and later by the bacterial proliferation.9 In the other 3 cases, although gallstone was not present, patients suffered from some symptoms (2 cases, abdominal pain; 1 case, fever). It is not known exactly why the congenital anomalies cause symptoms only during adulthood in RHA syndrome. Chung et al. considered that the cystic artery, which commonly branches from RHA, had tension and played some role, because the RHA became longer after cholecystectomy.2 Some studies described that post-cholecystectomy patients have significantly wider common bile duct diameters.10, 11 Tanaka et al. investigated the coordination of the gallbladder and sphincter of Oddi and the effect of cholecystectomy on biliary pressure physiology in 7 patients using an indwelling micro transducer catheter placed in the bile duct.12 They considered that the spasm of the sphincter of Oddi readily leads to a pressure rise if the gallbladder is absent, which may partly explain the change in common bile duct diameter and internal pressure after cholecystectomy. In our case, the expansion of the common bile duct diameter was unrecognized after cholecystectomy, but the symptoms and examination data improved.
Table 1. Details of 8 reported cases of RHA syndrome.
| Author | Age | Sex | Symptons | Gall stone | Pprocedures | Observation Period | Clinical Course |
|
| 1984 | Tsuchiya et al. |
59 | F | Fever, Abdominal pain |
Bile duct | Hepaticojejunostomy | − | Uneventful |
| 1984 | Tsuchiya et al. |
57 | F | Abdominal pain | Bile duct | Left partial hepatectomy + hepatico-jejunostomy |
53 days | Dead |
| 1994 | Chung et al. |
39 | F | Fever, Jaudice |
− | Cholecystectomy | 6 months | Abdominal pain |
| 2005 | Izushi et al. |
51 | M | Abdominal pain | − | Cholecystectomy | 3 years | Uneventful |
| 2005 | Miyashita et al. |
55 | M | Fever, Weight loss |
Gallbladder | Hepaticojejunostomy | 1 year | Uneventful |
| 2012 | Estiaghpour et al. |
54 | M | Abdominal pain, Jaudice |
Bile duct | Endoscopic lithotripsy | − | Uneventful |
| 2012 | Tas et al. | 74 | F | Abdominal pain | − | − | − | Uneventful |
| 2014 | Mendes et al. |
52 | F | Abdominal pain, Jaudice |
Bile duct | Hepaticojejunostomy | 2 years | Uneventful |
F, female; M, male.
There was no dilation of the upstream bile duct, but pulsatile stenosis that caused cholestasis was present. Making differential diagnosis from cholangiocarcinoma was difficult with static images such as CT and MR images; however, diagnosis was possible by observing dynamically. Both IDUS and POCS are capable of being observed dynamically. While IDUS dynamically observes a cross-sectional image of the bile duct, POCS has the advantage of being able to simultaneously be observed a specific area of the bile duct on the same screen. In addition, since IDUS sometimes cannot diagnose the intraepithelial extension of the bile duct,13 direct observation by POCS was performed to confirm the diagnosis.
In conclusion, arterial compression should be considered in the differential diagnosis of extrahepatic biliary obstruction. POCS with SpyGlass DSTM system is useful for the diagnosis of RHA syndrome.
Acknowledgments
Acknowledgments: I wish to thank Dr. Kenichi Harada, medical director of gastroenterology in Yonago Medical Center, for advice on differentiated diagnosis.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Tsuchiya R,Eto T,Harada N,Yamamoto K,Matsumoto T,Tsunoda T,et al. . Compression of the common hepatic duct by the right hepatic artery in intrahepatic gallstones. World J Surg. 1984;8:321-6. 10.1007/BF01655064 [DOI] [PubMed] [Google Scholar]
- 2.Chung JP,Kim KW,Chi HS,Lee SI,Shin ET,Cho JH,et al. . Obstructive jaundice due to compression of the common hepatic duct by right hepatic artery: a case associated with the absence of the lateral segment of the left hepatic lobe. Yonsei Med J. 1994;35:231-8. 10.3349/ymj.1994.35.2.231 [DOI] [PubMed] [Google Scholar]
- 3.Izuishi K,Toyama Y,Wakabayashi H,Usuki H,Maeta H. Compression of the common hepatic duct by the right hepatic artery. Clin Imaging. 2005;29:342-4. 10.1016/j.clinimag.2005.01.023 [DOI] [PubMed] [Google Scholar]
- 4.Miyashita K,Shiraki K,Ito T,Taoka H,Nakano T. The right hepatic artery syndrome. World J Gastroenterol. 2005;11:3008-9. 10.3748/wjg.v11.i19.3008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Eshtiaghpour D,Eysselein VE,Reicher S. Hepatic artery compression of the common hepatic duct: direct visualization by single-operator peroral cholangioscopy. Clin Gastroenterol Hepatol. 2012;10:e45. 10.1016/j.cgh.2011.11.015 [DOI] [PubMed] [Google Scholar]
- 6.Tas A,Koklu S. Unusual cause of common bile duct dilatation in asymptomatic elderly patient: right hepatic artery syndrome. Ann Hepatol. 2012;11:150-1. 10.1016/S1665-2681(19)31503-0 [DOI] [PubMed] [Google Scholar]
- 7.Mendes VM,Nasser HA,Bou Nassif G,Choukr A. Prebiliary right hepatic artery resulting in common hepatic duct compression and subsequent intrahepatic stone formation: myth or reality? Case Rep Med. 2014;2014:1-3. 10.1155/2014/403104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Koops A,Wojciechowski B,Broering DC,Adam G,Krupski-Berdien G. Anatomic variations of the hepatic arteries in 604 selective celiac and superior mesenteric angiographies. Surg Radiol Anat. 2004;26:239-44. 10.1007/s00276-004-0229-z [DOI] [PubMed] [Google Scholar]
- 9.Beger HG,Schwarz A. Review article: spectrum of biliary infections in the West and in the East. HPB Surg. 1995;8:215-22. 10.1155/1995/74384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park SM,Kim WS,Bae IH,Kim JH,Ryu DH,Jang LC,et al. . Common bile duct dilatation after cholecystectomy: a one-year prospective study. J Korean Surg Soc. 2012;83:97-101. 10.4174/jkss.2012.83.2.97 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chawla S,Trick WE,Gilkey S,Attar BM. Does cholecystectomy status influence the common bile duct diameter? A matched-pair analysis. Dig Dis Sci. 2010;55:1155-60. 10.1007/s10620-009-0836-y [DOI] [PubMed] [Google Scholar]
- 12.Tanaka M,Ikeda S,Nakayama F. Change in bile duct pressure responses after cholecystectomy: loss of gallbladder as a pressure reservoir. Gastroenterology. 1984;87:1154-9. 10.1016/S0016-5085(84)80078-5 [DOI] [PubMed] [Google Scholar]
- 13.Noda Y,Fujita N,Kobayashi G,Ito K,Horaguchi J,Takazawa O,et al. . Intraductal ultrasonography before biliary drainage and transpapillary biopsy in assessment of the longitudinal extent of bile duct cancer. Dig Endosc. 2008;20:73-8. 10.1111/j.1443-1661.2008.00779.x [DOI] [Google Scholar]