Abstract
Objectives
To investigate the role of ethnicity in COVID-19 outcome disparities in a cohort in Kuwait.
Methods
This is a retrospective analysis of 405 individuals infected with SARS-CoV-2 in Kuwait. Outcomes such as symptoms severity and mortality were considered. Multivariate logistic regression models were used to report the odds ratios (OR) for ICU admission and dying from COVID-19.
Results
The cohort included 290 Arabs and 115 South Asians. South Asians recorded significantly higher COVID-19 death rates compared to Arabs (33% vs. 7.6%, P value<0.001). When compared to Arabs, South Asians also had higher odds of being admitted to the ICU (OR = 6.28, 95% CI: 3.34–11.80, p < 0.001). South Asian patients showed 7.62 (95% CI: 3.62–16.02, p < 0.001) times the odds of dying from COVID-19.
Conclusion
COVID-19 patients with South Asians ethnicity in Kuwait are more likely to have worse prognosis and outcome when compared to patients with Arab ethnicity. This suggest a possible role for ethnicity in COVID-19 outcome disparities and this role is likely to be multifactorial.
Highlights
-
•
Kuwait is a multiethnic country with a population of 4.3 million made mostly by Arabs and South Asians.
-
•
South Asians were more likely to develop a severe form of the disease which also corresponded to a higher death rate compared to Arabs in Kuwait.
-
•
Results highlighted probable impact of ethnicity on COVID-19 outcome.
Introduction
Clinical manifestations of COVID-19 patients vary broadly, ranging from asymptomatic infection to acute respiratory failure and death (Alshukry et al., 2020). It is well established now that age, gender and certain pre-existing health conditions are considered as risk factors for a severe form of the disease (Alahmad et al. 2020; Apicella et al. 2020). However certain indications have suggested a possible implication for ethnicity and race as contributors to the wide disparity in COVID-19 outcomes. Recent findings in the United States and United Kingdom showed differences in COVID-19 related hospitalization and death rates by ethnicity (Garg et al. 2020; Patel et al. 2020). Black, Asian and Minority Ethnic (BAME) individuals have been shown to have an elevated risk of acquiring SARS-CoV2 infection and getting worse COVID-19 outcomes when compared to white individuals (Pan et al. 2020).
Ethnicity is influenced by genetic backgrounds, environmental factors, as well as cultural and behavioral norms. Others have linked ethnicity to socioeconomic status, living standards and occupations (Patel et al. 2020). These factors linked to ethnicity are likely to function interdependently and influence disease outcome. As COVID-19 continue to spread globally, understanding how ethnicity affects SARS-CoV2 susceptibility and disease outcome would surely improve disease management and outcome.
Kuwait is a multiethnic country with a population of 4.3 million. According to Central Statistical Bureau of Kuwait, Arabs make 59.2% of the population while South Asians make 37.8% . In here, we present and compare COVID-19 clinical outcomes in the Arabs and South Asians ethnic groups.
Material and methods
Cohort details.
Four hundred and five consecutive COVID-19 patients were recruited in this study. Patients were admitted to Jaber Al-Ahmad Hospital in Kuwait between February 24 and May 24, 2020. Hospitalization rate was 100%, subject to a positive PCR test regardless of disease severity. Cohort clinical characteristics were previously described by our group Alshukry et al., 2020 . The study was reviewed and granted an approval by the standing committee for coordination of health and medical research in the Ministry of Health in Kuwait (IRB 2020/1404). Patients were divided into two main groups; Arabs and South Asian. Disease severity was determined following criteria described previously (Alshukry et al., 2020)
Statistical analysis
Student t-test was used to examine continuous variables, results were reported as mean ± standard deviation. Nominal variables were determined by using χ2 test and categorical variables compared using Fisher-Exact test. We investigated the relationships between ethnicity as a categorical exposure and both (1) the death outcome from COVID-19 and (2) ICU admission. We used binary response variables and adjusted for age, gender, smoking status and other co-morbidities. A logistic regression model was used to report the odds ratios (OR) for dying from COVID-19 and for ICU admission for patients of South Asian ethnicity, with a baseline comparison to Arab ethnicity.
Results
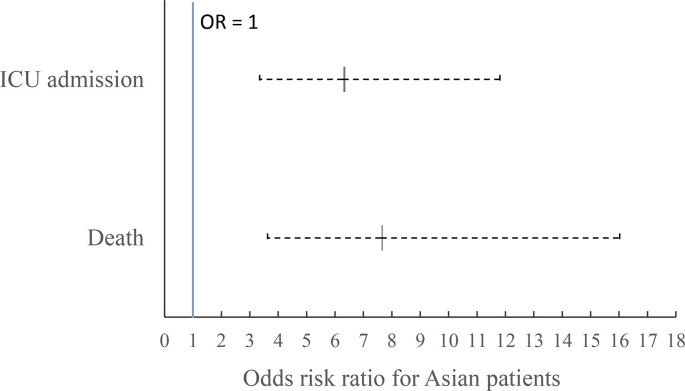
Arabs made the majority of the cohort (71.6%). Males were predominant in both ethnic groups which were also age matched. Mortality rate in Arabs groups was 7.5% while it reached 33% in the South Asians (p < 0.001). No significant differences were reported in comorbidities prevalence between both groups (Table.1 ). South Asians also had higher odds of being admitted to the ICU (OR = 6.28, 95% CI: 3.34–11.80, p < 0.001). (Fig. 1 ). They also showed 7.62 (95% CI: 3.62–16.02, p < 0.001) times the odds of dying from COVID-19 when compared to Arabs (Fig. 1).
Table 1.
Cohort characteristics.
| Arabs | South Asians | ||||
|---|---|---|---|---|---|
| count | % | count | % | P value | |
| 290 | 71.6 | 115 | 28.4 | ||
| Gender | |||||
| Male | 164 | 56.6 | 91 | 79.1 | <0.001 |
| Female | 126 | 43.4 | 24 | 20.9 | <0.001 |
| Age | (Mean years ± SD) | (Mean years ± SD) | 0.069 | ||
| 44.5 ± 18.2 | 47.6 ± 13.4 | ||||
| Disease spectrum | |||||
| Asymptomatic | 136 | 46.9 | 25 | 21.7 | <0.001 |
| Mild/Moderate | 119 | 41.0 | 43 | 37.4 | 0.499 |
| ICU | 35 | 12.1 | 49 | 42.6 | < 0.001 |
| Deaths | 22 | 7.6 | 38 | 33 | < 0.001 |
| Comorbidities | |||||
| Diabetes | 67 | 23.3 | 30 | 26.1 | 0.606 |
| Hypertension | 93 | 32.2 | 28 | 24.3 | 0.148 |
| Asthma | 31 | 10.8 | 9 | 7.9 | 0.462 |
| Cardiovascular disease | 31 | 10.7 | 8 | 7.0 | 0.350 |
| Chronic renal disease | 12 | 4.2 | 2 | 1.7 | 0.367 |
| Malignancy | 9 | 3.1 | 3 | 2.6 | 0.784 |
Fig. 1.
Odds ratios of dying and being admitted to ICU from COVID-19 if a patient is of South Asian ethnicity. Baseline is Arab ethnicity. ORs are adjusted for age, gender, smoking status and other co-morbidities.
Discussion
Results from our cohort, which provided good representation of the population in Kuwait, indicated that South Asians were more likely to develop a severe form of COVID-19 which also corresponded to a higher death rate compared to Arabs.
Our results suggested ethnicity as a possible risk factor for COVID-19 poor prognosis and outcome. The vast majority of South Asians in Kuwait are unskilled labor living in highly populated accommodations. Their living conditions and perhaps occupation can increase their exposure to SARS-CoV2. While this could have a major impact on infection dynamics, it may not explain the results entirely. Local laws grant each resident in Kuwait free access to governmental health care, hence rolling out healthcare access inequalities of such outcome disparity. Comorbidities are known as risk factors for severe and poor outcomes however our results indicated no significant differences in prevalence between the two ethnic groups and therefore do not provide a conclusive answer for the disparity in outcome. We certainly cannot overlook the role of genetic factors which might make people from certain ethnicity more prone to severe outcome (Al-Mulla et al., 2020) .
Our presented study has a number of limitations including relatively small sample size and unmatched gender distribution between ethnic groups. There is also a possibility of differential management of chronic health conditions prior to admission between the two ethnic groups which could impact the measured outcomes.
In conclusion, the role of ethnicity in COVID-19 outcome disparities is likely to be multifactorial in nature. Understanding why certain ethnic groups are prone to severe COVID-19 outcome is important to improve outcomes and develop effective mitigation strategies.
Authors contribution
HA was involved in data analysis, drafted the article and had the final approval of the version to be submitted. AA1, YA, MB, AA2, YB and MD are involved in acquisition of the data. SM, MA and AA3 are involved in data analysis. MA and JA involved in data interpretation. FA revised the article critically for important intellectual content.
Ethical approval
The study was reviewed and granted an approval by the standing committee for coordination of health and medical research in the Ministry of Health in Kuwait (IRB 2020/1404).
Funding
No funding was obtained for the presented work.
Authors contribution
HA was involved in data analysis, drafted the article and had the final approval of the version to be submitted. AA1, YA, MB, AA2, YB and MD are involved in acquisition of the data. SM, MA and AA3 are involved in data analysis. MA and JA involved in data interpretation. FA revised the article critically for important intellectual content.
Declaration of interests
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Declaration of competing interest
The authors have no conflicts of interest to declare. All co-authors have seen and agree with the contents of the manuscript and there is no financial interest to report.
References
- Alahmad B., Al-Shammari A.A., Bennakhi A., Al-Mulla F., Ali H. Fasting blood glucose and COVID-19 severity: nonlinearity matters. Diabetes Care. 2020;34:3113–3116. doi: 10.2337/dc20-1941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mulla F., Mohammad A., Al Madhoun A., Haddad D., Ali H., Eaaswarkhanth M., John S.E., Nizam R., Channanath A., Abu-Farha M., Ahmad R., Abubaker J., Thanaraj T.A. A comprehensive germline variant and expression analyses of ACE2, TMPRSS2 and SARS-CoV-2 activator FURIN genes from the Middle East: Combating SARS-CoV-2 with precision medicine. bioRxiv. 2020 2020.2005.2016.099176. [Google Scholar]
- Alshukry A., Ali H., Ali Y., Al-Taweel T., Abu-farha M., AbuBaker J., Devarajan S., Dashti A.A., Bandar A., Taleb H., Al Bader A., Aly N.Y., Al-Ozairi E., Al-Mulla F., Bu Abbas M. Clinical characteristics of Coronavirus Disease 2019 (COVID-19) patients in Kuwait. PLoS One. 2020;15 doi: 10.1371/journal.pone.0242768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apicella M., Campopiano M.C., Mantuano M., Mazoni L., Coppelli A., Del Prato S. COVID-19 in people with diabetes: understanding the reasons for worse outcomes. Lancet Diabetes Endocrinol. 2020;8:782–792. doi: 10.1016/S2213-8587(20)30238-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garg, S., Kim, L., Whitaker, M., O'Halloran, A., Cummings, C., Holstein, R., Prill, M., Chai, S.J., Kirley, P.D., Alden, N.B., Kawasaki, B., Yousey-Hindes, K., Niccolai, L., Anderson, E.J., Openo, K.P., Weigel, A., Monroe, M.L., Ryan, P., Henderson, J., Kim, S., Como-Sabetti, K., Lynfield, R., Sosin, D., Torres, S., Muse, A., Bennett, N.M., Billing, L., Sutton, M., West, N., Schaffner, W., Talbot, H.K., Aquino, C., George, A., Budd, A., Brammer, L., Langley, G., Hall, A.J., Fry, A., 2020. Hospitalization Rates and Characteristics of Patients Hospitalized with Laboratory-Confirmed Coronavirus Disease 2019 - COVID-NET, 14 States, March 1–30, 2020. MMWR Morb Mortal Wkly Rep 69, 458–464. [DOI] [PMC free article] [PubMed]
- Pan D., Sze S., Minhas J.S., Bangash M.N., Pareek N., Divall P., Williams C.M., Oggioni M.R., Squire I.B., Nellums L.B., Hanif W., Khunti K., Pareek M. The impact of ethnicity on clinical outcomes in COVID-19: a systematic review. EClinicalMedicine. 2020;23:100404. doi: 10.1016/j.eclinm.2020.100404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel P., Hiam L., Sowemimo A., Devakumar D., McKee M. Ethnicity and covid-19. BMJ. 2020;369:m2282. doi: 10.1136/bmj.m2282. [DOI] [PubMed] [Google Scholar]