Abstract
HIV testing rates remain low among youth ages 13–24 in the US, with only 55% of HIV-positive youth aware of their serostatus. We conducted a systematic review to assess the utility of technology-based interventions to increase point-of-care youth HIV testing and linkage to care. We searched PubMed, Embase, CINAHL, and Cochrane CENTRAL for randomized controlled trials of technology-based interventions aimed at increasing point-of-care youth HIV testing, published between 2008 and 2020. All identified citations were independently screened for inclusion by two authors, and the Cochrane Risk of Bias Tool for Randomized Controlled Trials was used to assess the quality of included studies. Three studies met all inclusion criteria. Two interventions were effective in increasing HIV testing, while one was effective at linkage to care. Technology-based interventions have the potential to increase youth HIV testing in clinical settings and facilitate linkage to care, possibly reducing undiagnosed HIV among adolescents and emerging adults.
Keywords: HIV testing, Youth, Point-of-care testing, Technology-based interventions, Clinical settings
Introduction
Youth aged 13–24 years accounted for 21% of all newly diagnosed HIV cases in the US in 2018 [1]. Youth in this age group are the least likely to have diagnosed HIV infections, with only 55% of those with HIV being aware of their serostatus [2], due to low HIV testing rates [1]. Evidence from various youth samples indicate that less than 50% of US youth have ever been tested for HIV [3–5]. Trend data from two behavior surveillance systems also indicate significant declines in HIV testing rates among youth in recent years [6, 7]. Undiagnosed HIV infections among youth facilitate transmission and propagate HIV within this population [1, 8, 9]. Low testing rates also lead to delayed diagnosis and worse prognosis among HIV-infected youth [10, 11]. Early diagnosis of all individuals infected with HIV is essential to curbing the HIV epidemic and, in fact, is the first of the four pillars of the plan to end the HIV epidemic in the US [12]. Increasing HIV testing among youth is therefore of the utmost importance [13].
Technology-based interventions present a valuable opportunity to increase HIV testing among youth and engage them in the HIV care continuum. Several technology-based interventions have been developed to increase HIV testing rates among youth. Most of these interventions specifically target youth at high risk of becoming HIV-infected, such as men who have sex with men (MSM) and transgender youth of color [14–18] who account for a large proportion of all new HIV diagnoses [1]. Research suggests that technology-based interventions may help address some of the barriers to testing faced by youth. For example, a recent telehealth intervention, was used to address concerns regarding stigma or discrimination (commonly cited barriers to testing among youth [3, 19, 20]) and other individual barriers to testing, among a sample of transgender youth [14]. Similarly, a social media campaign to increase HIV testing among adolescents emphasized that testing can be done confidentially and without the need for parental consent after youth highlighted this as a key barrier to testing during intervention development [21]. Other common barriers to HIV testing such as low perceived risk for HIV infection [20, 22–24] and low levels of HIV-related knowledge (particularly knowledge about HIV testing) [20, 25, 26] can also be addressed using technology-based interventions.
Point-of-care technology-based interventions may be especially useful for increasing HIV testing of youth in clinical settings. This is because newly diagnosed youth can be readily linked to care in such settings. Yet, despite recommendations for routine HIV testing for adolescents and young adults in all clinical settings [27, 28], research indicates that youth are often not tested for HIV [10, 29, 30]. For example, in a study of youth receiving care for acute sexually transmitted infections (STIs) in large urban primary care clinics only 55% of patients received an HIV test [31]. This is despite recommendations that all patients being tested and treated for STIs also be tested for HIV [32]. The low youth HIV testing rates observed in clinical settings are in part due to low levels of awareness among youth [26, 33] and healthcare providers [34, 35] of the need for youth to be routinely screened for HIV. There is a clear need for interventions or approaches that increase HIV testing as a routine part of health care provided to youth [13]. Point-of-care technology-based interventions may be particularly useful in meeting this need. They may also be particularly useful in facilitating HIV testing during the ongoing COVID-19 pandemic given the need to minimize contact between providers and patients.
In addition to testing, ensuring that youth with diagnosed HIV infections are linked to HIV treatment and care is critical to address individual-level health and reduce HIV transmission in the community [27]. Research suggests that youth are the least likely group in the US to be engaged in care or virally suppressed [2, 36]. However, recent data demonstrate that once youth are linked to and successfully engaged in care, they remain in care and achieve viral suppression [37]. Thus, it is imperative to identify ways to not only increase HIV testing, but also linkage to and retention in care among youth. This will help move youth through the relevant steps of the HIV care continuum and reduce further transmission of HIV [38]. The majority of youth-focused technology-based interventions are designed for use outside of clinical settings making it difficult to immediately get youth who test positive into HIV care. Research shows that youth whose HIV is diagnosed outside of the health care setting are less likely to be linked to care [23]. Point-of-care diagnosis may increase the likelihood of linkage to care [27, 39]. For example, a young person who is diagnosed with HIV while in a hospital can be linked to care before they are discharged [40]. The importance of linkage to care is highlighted by the second pillar of the plan to end the HIV epidemic in the US which is to “treat HIV infection rapidly and effectively to achieve sustained viral suppression” [12].
The goal of the current review was to identify technology-based interventions that were designed to increase HIV testing among youth aged 13–24 in the US in clinical settings and evaluated through randomized controlled trials (RCTs). The insights gained from the review, including examinations of key aspects that did or did not facilitate testing, will help inform future interventions to increase HIV testing among youth in clinical settings.
Methods
Search Strategy
As a first step, a protocol was developed to guide the conduct of the systematic review. A librarian on the research team developed and conducted searches of PubMed, Embase, CINAHL, and Cochrane Central Register of Controlled Trials covering publication dates 2008 to April 2020. The search strategies combined keywords and controlled vocabulary related to four concepts: adolescent/young adult, HIV testing, point-of-care setting, and technology. No limits on publication type or language were included at this stage. A sample PubMed search strategy is presented in Table 3 in the Appendix. Initial searches were conducted on October 4, 2019, covering publication years 2008–2018 and were updated on April 17, 2020 to include more recent publications.
Table 3.
Initial PubMed search strategy (2008–2018)
| 1 | ("Young Adult"[mesh] OR “Adolescent”[mesh] OR adolescent[tiab] OR adolescents[tiab] OR “young adult”[tiab] OR “young adults”[tiab] OR teen[tw] OR teens[tiab] OR teenage[tiab] OR teenager[tiab] OR teenagers[tiab]) |
| 2 | ("AIDS Serodiagnosis"[mesh] OR "HIV Antibodies/analysis"[mesh] OR "HIV Antigens/analysis"[mesh] OR “HIV Infections/diagnosis”[mesh] OR “HIV Seropositivity/diagnosis”[mesh] OR "HIV Infections/prevention and control"[mesh] OR hiv test*[tiab]) |
| 3 | (“HIV"[mesh] OR “HIV Infections”[mesh] OR "Acquired Immunodeficiency Syndrome"[mesh] OR hiv[tw]) |
| 4 | (“Mass Screening”[mesh] OR "Serologic Tests"[mesh] OR "Diagnosis"[mesh] OR "diagnosis" [Subheading] OR "prevention and control" [Subheading] OR screening[tiab] OR test[tiab] OR tests[tiab] OR tested[tiab] OR testing[tiab]) |
| 5 | #3 and #4 |
| 6 | #2 or #5 |
| 7 | ("Ambulatory Care Facilities"[mesh] OR "Emergency Medical Services"[mesh:noexp] OR "Emergency Services, Psychiatric"[mesh] OR "Emergency Service, Hospital"[mesh] OR "Point-of-Care Systems"[mesh] OR "Ambulatory Care"[mesh] OR "Primary Health Care"[mesh] OR emergency department*[tiab] OR “emergency care”[tiab] OR “urgent care”[tiab] OR “point of care”[tiab] OR “general practice”[tiab] OR “primary care”[tiab] OR outpatient[tiab] OR clinic[tiab] OR clinics[tiab] OR clinical[tiab] OR "Hospitalization"[mesh] OR "Critical Care"[mesh] OR inpatient[tiab] OR "Community Health Services"[mesh] OR ambulatory[tiab] OR community setting*[tiab]) |
| 8 | (“Computer systems”[mesh] OR “Educational Technology”[mesh] OR “Text Messaging”[mesh] OR “Cell Phone”[mesh] OR “software”[mesh:noexp] OR “telemedicine”[mesh] OR “online systems”[mesh:noexp] OR “reminder systems”[mesh] OR “information systems”[mesh:noexp] OR “user-computer interface”[mesh] OR “mobile applications”[mesh] OR “video games”[mesh] OR “videotape recording”[mesh] OR “videodisc recording”[mesh] OR “computer-assisted instruction”[mesh] OR technology[tiab] OR technologies[tiab] OR computer*[tiab] OR smartphone*[tiab] OR ehealth[tiab] OR mhealth[tiab] OR telehealth[tiab] OR texting[tiab] OR text messag*[tiab] OR sms[tiab] OR cell phone*[tiab] OR mobile phone*[tiab] OR cellular phone*[tiab] OR mobile device*[tiab] OR ipad*[tiab] OR tablet[tiab] OR tablets[tiab] OR “mobile app”[tiab] OR "mobile apps"[tiab] OR mobile application*[tiab] OR “web based”[tiab] OR “network based”[tiab] OR audiovisual[tiab] OR multimedia[tiab] OR video[tiab] OR videos[tiab] OR videorecord*[tiab]) |
| 9 | ("2008/01/01"[PDAT]: "2018/12/31"[PDAT]) |
| 10 | #1 and #6 and #7 and #8 and #9 |
Eligibility Assessment
All identified citations were uploaded into a citation manager and duplicates were identified and removed. After deduplication, two members of the research team individually screened the title and abstracts of all identified results for relevance. Any disagreements were resolved by a third member of the team. Next the full texts of seemingly relevant articles were independently reviewed in detail by two team members. Studies were deemed eligible if: (1) they tested the effect of a technology-based intervention aimed at increasing HIV testing; (2) the intervention was aimed at increasing on-site HIV testing; (3) the study involved an RCT; and (4) the study sample included youth between the ages of 13 and 24 years.
Quality Assessment, Data Extraction and Analysis
All articles deemed relevant were then assessed for risk of bias using version 2 of the Cochrane Risk of Bias Tool for Randomized Controlled Trials (ROB2) [41]. The tool assessed the potential for bias in five domains including the randomization process, deviations in intervention implementation, and outcome measurement issues. Finally, relevant data including study sample characteristics, intervention characteristics and study findings were extracted using a standardized form. At each stage, discrepancies were discussed until consensus was reached. Findings from the relevant studies were qualitatively summarized. All components of the systematic review are reported in line with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) Statement [42].
Results
Search Results and Study Characteristics
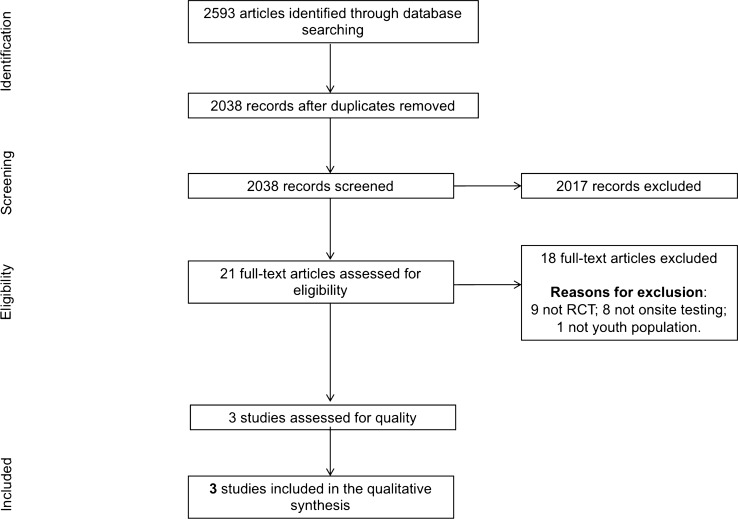
A total of 2593 citations were identified through the search strategy, with 555 being duplicates. Of the 2038 unique citations, only three articles met all inclusion criteria and were included in the analysis. Figure 1 shows the PRISMA flowchart delineating the number of citations involved in each step.
Fig. 1.
PRISMA flowchart of study selection
All three included studies involved interventions that were employed to increase HIV testing in an emergency department (Table 1). One study exclusively targeted youth aged 15–21 [43]; the requirement for parental consent for youth under age 18 years was waived to facilitate the participation of minors in the study. The remaining two studies included youth ages 18–24 as part of larger samples of adults within the recommended HIV testing age range [44, 45]. Two of the identified studies used videos to increase participants’ knowledge about HIV testing [43, 45]. Two interventions directly assessed participants’ HIV risk behaviors and provided personalized feedback based on participants’ self-reported risk behaviors [44, 45]. Detailed descriptions of the interventions are included in Table 1. All three studies had a low risk of bias (Table 2).
Table 1.
Summary and characteristics of studies included in the systematic review
| Calderon et al. 2011 [43] | Merchant et al. 2011 [44] | Kurth et al. 2013 [45] | |
|---|---|---|---|
| Study characteristics | |||
| Setting | Emergency department in urban area (New York City), July 2008–November 2008 |
Emergency department in urban area (New England), October 2007–September 2008 |
Emergency department in urban area (Pacific Northwest), during a period when the ED only provided HIV testing if clinically indicated or in the event of occupational blood exposure |
| Sample size | 200 | 571 | 517 |
| Age range | 15–21 years |
18–64 years (25% of participants < 22 years) |
18 years and older (Inta: 3% < 20, 31% 20–29) Ctrlb: 6% < 20, 26% 20–29) |
| Sex |
Female: 47.5% Male: 52.5% |
Female: 62.2% Male: 37.8% |
Female: 41% (Int); 38% (Ctrl) Male: 59% (Int); 62% (Ctrl) |
| Intervention | A 4-minute pre-test HIV educational video covering the seven essential elements required by New York State law for HIV pretest counseling which included information on HIV transmission, HIV infection and AIDS, the HIV test, benefits of testing, voluntary and mandatory testing, results reporting requirements and partner notification | An audio, computer-assisted, interview system-based HIV risk questionnaire (described below) plus tailored feedback messages to participants’ reported HIV risk behaviors. Feedback messages were provided immediately after each question and were directed to the participant (i.e. “you”) both verbally (via audio recording) and written on the computer screen. The feedback messages did not mention HIV testing | The Computer Assessment and Risk-reduction Education (CARE) tool is a theory-based (Integrative Model of Change and Social Cognitive Theory) intervention which includes a risk assessment, a rapid HIV test video, HIV test consent, personalized feedback on reported risks, tailored behavioral skill-building videos, and development of a specific HIV risk-reduction plan which was printed out at the end of the session. Chart review was also conducted after the visit similar to the control group |
| Control condition | An in-person HIV counseling session of unspecified duration from a counselor trained to provide age-appropriate, culturally-sensitive HIV education and counseling | An audio, computer-assisted, interview system-based HIV risk questionnaire which asked participants about their self-perceived HIV risk twice–before and after they reported their sexual and injection drug use-related HIV risk behaviors. Participants completed the questionnaire on a tablet personal computer with headphones | Standard care–an emergency department visit and chart review to assess risk behaviors and HIV/STI test referrals |
| Results | |||
| Willingness to test and HIV testing uptake | Intervention group participants were more willing to be tested for HIV [51% (Int) vs. 22% (Ctrl); p < 0.01] and more likely to get an HIV test [aOR:3.6; 95% CI 1.8–7.2; p < 0.001] |
Overall, HIV testing uptake was greater in the control group than in the intervention group [55.5% (Ctrl) vs. 54.1% (Int); Δ = − 0.01%; 95% CI 0.09% to 0.07%)] More women in the intervention group were willing to be tested regardless of the effect of the intervention on their self-perceived HIV risk (80% vs. 52.8% with decreased risk perception; 51% vs 33% with no change in risk perception; 73% vs 68% with increased risk perception). Among men, those in the control group were more willing to test (36% vs 89% decreased; 50% vs 54% no change; 59% vs 80% increased) |
97% of intervention group participants were HIV tested, one participant who was not tested as part of the study was tested by ED clinicians. No one in the control group was HIV tested, but two participants were referred elsewhere for an HIV test |
| HIV diagnosis and linkage to care | No one tested HIV positive | There was one true positive and two false positive HIV test results (0.4% seroprevalence; 95% CI 0.01–2.2). The HIV positive person was linked to care in the hospital-based HIV clinic | |
| Acceptability of intervention and satisfaction with testing experience | Intervention group participants reported more satisfaction with the testing experience [Mean satisfaction score: 28.6 out of 30 (Int) vs. 25.4 (Ctrl); p < 0.0001] |
Acceptability of the intervention was high in terms of ease of use (97%), privacy (96%), helpfulness compared to face-to-face counseling (91%), and duration (86%); 55% would choose computer-based HIV counseling in the future. In verbal exit interviews, participants reported that the CARE tool was more private (83%), convenient (77%), more comfortable (76%), safer (72%), and more helpful (54%) compared to staff-delivered counseling Intervention group was more likely to be “very satisfied” with their visit (54% vs. 46%) |
|
| Post-intervention HIV knowledge or risk perception | Intervention group participants reported higher HIV knowledge scores [78.5% (Int) vs. 66.3% (Ctrl); p < 0.0] | The intervention and control groups did not significantly differ on change in self-perceived HIV risk | Two-thirds of participants in the intervention group thought it was “very important” to change their behaviors to reduce their risk for HIV infection |
| Unmet need potentially addressed by intervention | More HIV risk was identified through the intervention than in the control condition (risk from sexual contact 59% vs 1%; injection drug use 26% vs 2%) and more HIV risk reduction plans were made (98% vs 1%). Most (84%) of participants who made risk reduction plans felt very confident about their ability to change their behaviors | ||
aInt intervention
bCtrl control
Table 2.
Risk of bias of included studies
Effect of the Interventions on HIV Testing
In the one study targeting youth exclusively, a video-based HIV intervention was more effective than in-person counseling at increasing HIV testing, with intervention participants being almost four times more likely than control participants to get an HIV test [43]. Similarly, in a study of an intervention combining videos with personalized feedback and risk-reduction planning, 97% of participants in the intervention group were tested for HIV during their emergency department visit compared to none in the control group (two control group participants were referred elsewhere for HIV testing) [45]. Conversely, an intervention that combined a risk assessment questionnaire with personalized feedback on reported risk behaviors did not increase HIV testing compared to the control condition which involved only the risk assessment questionnaire [44].
HIV Diagnosis and Linkage to Care
Only two of the included studies reported information on HIV diagnosis [43, 45]. In one study, no participants tested HIV positive [43]. In the second study, the one person with a confirmed HIV diagnosis was linked to care in a hospital-based HIV clinic [45].
Effect on HIV Risk Perception
Merchant et al. reported similar levels of change in HIV risk perception among participants in both the intervention and control groups in their study. In the study, participants’ perceived risk of being HIV infected was measured before and after they self-reported HIV risk behaviors in both study groups. Although the intervention group also received personalized feedback on each risk behavior reported, the feedback did not appear to have much effect on participants. The researchers posited that the feedback “may have been too limited in scope or depth” to effectively increase HIV risk perception and testing [44]. Kurth et al., reported that several participants in the intervention group of their study thought it was “very important” to change their behaviors to reduce their risk for HIV infection after the intervention [45].
Other Findings
The two studies that provided information on acceptability of and/or satisfaction with the interventions indicated that more participants in the intervention group reported being satisfied with their testing experience than control group participants [43, 45]. One study reported greater HIV knowledge among intervention group members after receiving the intervention [43]. One study identified more HIV risk behaviors among intervention group participants compared to those in the control group who received standard care, indicating high rates of unmet need for HIV testing that would have gone unaddressed without the intervention [45].
Discussion
Our review of the literature indicates that the use of technology-based interventions may be an effective way of increasing HIV testing among youth in clinical settings. Two of the three included interventions resulted in increased HIV testing. A common characteristic of the interventions that increased HIV testing uptake was the use of videos [43, 45]. Video-based interventions may be particularly effective in addressing literacy issues and may help make the information more accessible and relatable to participants [46]. It is unclear how effective the use of personalized feedback is on HIV testing uptake. The one study that combined personalized feedback with a risk assessment questionnaire, videos and a risk-reduction plan reported an increase in HIV testing [45]. However, the second intervention that used personalized feedback in combination with a risk assessment questionnaire only did not increase HIV testing. This may be due to the fact that control group participants also received the risk assessment questionnaire; the similarity in conditions may have led to the lack of an effect [44]. However, research has shown that risk assessment questionnaires on their own may not be enough to increase demand for testing [47]. Future studies that test technology-based intervention components individually may help shed some light on which components are most effective at increasing HIV testing.
All three identified interventions were used in the emergency department. The emergency department may provide an ideal location to increase HIV testing among youth for several reasons. Patients often spend a lot of time waiting for care in the emergency department; the average time from arrival to discharge is well over three hours [48]. Technology-based interventions that do not require a high degree of staff resources can be administered to patients while they wait, increasing their demand for HIV testing. The convenience of being able to get tested for HIV while waiting in the emergency department and being asked were the most commonly cited reasons for accepting HIV testing in the study by Merchant and colleagues [44]. Furthermore, research indicates that a sizeable proportion of at-risk youth may seek care in the emergency department due to lack of health insurance coverage [3, 49]. Research also suggests that integrating testing into the triage routine in emergency departments may help increase HIV testing and facilitate linkage to care [50, 51]. Moreover, routine opt-out testing increases HIV testing rates [52]. Therefore, HIV testing rates among youth may be further increased by integrating technology-based testing interventions into the patient care routine in emergency departments.
Use of technology-based interventions can also potentially address various types of stigma and privacy issues that have been identified as key barriers to HIV testing and engagement of youth at all stages of the HIV care continuum [53]. Youth in need of HIV testing and related health services are frequently discouraged by provider discomfort, which can at times stem from prejudice against racial or sexual minorities [54, 55]. Research indicates that concerns about stigma can be so powerful that some African American youth will refuse to even discuss HIV prevention, much less accept testing when available [56]. Moreover, sexual and racial minority youth may experience negative judgements from staff that discourage them from seeking out or accepting testing and available treatment when needed [55]. Technology-based interventions can be particularly helpful in addressing these types of stigma because young people are often more comfortable disclosing behavioral risk and discussing sensitive issues, such as HIV testing, via computer because they do not expect a device to judge them the way a person might [57]. Moreover, because people in emergency departments are often treated within earshot of other patients, the increased privacy afforded by technology (e.g., the ability to discretely disclose risk factors including substance use and sexual behaviors, or to listen to the dialogue of an educational video via headphones) allows staff to implement interventions in high volume settings without compromising confidentiality. Also, young patients who arrive in the emergency department accompanied by a parent may be more comfortable reporting risk behaviors and learning about HIV prevention via tablet computer because they do not need to discuss their sexual activity or other risk behaviors in front of older family members [58]. Technology-based interventions may facilitate confidential HIV testing opportunities for youth, especially in states or jurisdictions that allow minors to access HIV testing and prevention services without parental consent [59].
Technology-based HIV testing interventions may also be helpful in persuading patients who have previously declined testing of the importance of or need for testing. Felsen et al., found that almost half of patients who had initially declined testing during an emergency department visit ultimately agreed to be tested when asked later after being hospitalized. This was facilitated by an electronic medical record alert that informed clinicians that the person had not yet been tested [60]. Unfortunately, most patients who decline testing are not given a second chance to test before leaving the emergency department or other clinical settings. An intervention that provides patients with additional information about HIV and the need for routine testing may further increase the number of patients who are tested in clinical settings, as research has shown that both access to and knowledge of HIV testing are needed to increase uptake among youth [38]. This combination of access and information on HIV may account for the increased HIV testing of the two effective interventions included in this review [43, 45]. However, current standards of care do not include HIV prevention education for emergency department patients, even for those who test negative for HIV but report risk behaviors that greatly increase their likelihood of future exposure. Technology-based interventions have the potential to fill this gap in care by being deployed to provide post-test counseling and risk-reduction planning (as was done in one of the included studies [45]) and provide information on potential HIV prevention options such as pre-exposure prophylaxis (PrEP) [14].
A main benefit of employing technology-based HIV testing interventions in clinical settings is the greater opportunity to link newly diagnosed individuals to care immediately. The one included study with a participant who tested HIV-positive reported successfully linking the participant to care [45]. Although the interventions included in this review were all tested in the emergency department, such interventions may be relevant or adaptable to other clinical settings. There is a need for studies testing the efficacy of technology-based HIV testing interventions in other health care settings. Research indicates that integrating routine HIV testing into family planning clinics that serve youth may increase HIV testing rates [30]. HIV testing is also feasible in non-traditional clinical settings such as dental offices [61]. These and other clinical settings represent avenues to address missed opportunities for HIV testing. A recent study on missed opportunities for testing in clinical settings found that participants at high-risk for HIV had visited several healthcare settings in the previous 12 months including visits to dentists, eye doctors, psychologists, substance use treatment facilities and chiropractors among others [29]. Technology-based interventions have the potential to facilitate HIV testing in such settings to increase HIV diagnosis and linkage to care among youth.
Limitations
The findings of this review should be viewed in light of a few limitations. First, our search was limited to four databases and did not include grey literature. Thus, there is a possibility that our search strategy might not have captured all relevant interventions. Furthermore, since we only included published studies, there is the possibility of reporting and publishing bias, as studies of ineffective interventions are less likely to be published. By limiting the current review to only the most rigorously evaluated interventions (i.e., RCTs), we excluded several technology-based interventions that have been developed to increase point-of-care HIV testing. Such interventions may also provide useful insights to guide the development and implementation of future point-of-care HIV testing interventions.
Conclusions
The current review indicates that technology-based interventions may be effective in increasing HIV testing among youth in point-of-care settings in the US. Such interventions could also be used to educate patients who test negative on ways to minimize their risk for HIV such as through the use of PrEP. There is a need to test such interventions in other clinical settings beyond the emergency department. With the ongoing COVID-19 pandemic, technology-based interventions may prove particularly important in clinical settings as they allow providers to continue to address HIV risk among patients while minimizing direct contact as dictated by current social distancing protocols.
Acknowledgements
This research was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (Grant No. R42 HD088325), and the National Institute of Drug Abuse (Grant Nos. P30 DA029926 and P30 DA011041), both components of the US National Institutes of Health.
Appendix
See Table 3.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Centers for Disease Control and Prevention. HIV among youth. https://www.cdc.gov/hiv/group/age/youth/index.html. Accessed May 13, 2020.
- 2.Harris NS, Johnson AS, Huang YLA, Kern D, Fulton P, Smith DK, et al. Vital signs: status of human immunodeficiency virus testing, viral suppression, and HIV preexposure prophylaxis – United States, 2013–2018. MMWR Morb Mortal Wkly Rep. 2019;68:1117–1123. doi: 10.15585/mmwr.mm6848e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.The Henry J. Kaiser Family Foundation. National Survey of Young Adults on HIV/AIDS. 2017. http://files.kff.org/attachment/Report-National-Survey-of-Young-Adults-on-HIV/AIDS.
- 4.Olakunde BO, Pharr JR, Adeyinka DA, Danquah P. HIV-related risk behaviors and testing among adolescent gay and bisexual boys in the United States. AIDS. 2019;33:2107–2109. doi: 10.1097/QAD.0000000000002333. [DOI] [PubMed] [Google Scholar]
- 5.Pitasi MA, Delaney KP, Brooks JT, DiNenno EA, Johnson SD, Prejean J. HIV testing in 50 local jurisdictions accounting for the majority of new HIV diagnoses and seven states with disproportionate occurrence of HIV in rural areas, 2016–2017. MMWR Morb Mortal Wkly Rep. 2019;68:561–567. doi: 10.15585/mmwr.mm6825a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, et al. Youth risk behavior surveillance – United States, 2017. MMWR Surveill Summ. 2018;67:1–114. doi: 10.15585/mmwr.ss6708a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Patel D, Johnson CH, Krueger A, Maciak B, Belcher L, Harris N, et al. Trends in HIV testing among US adults, aged 18–64 years, 2011–2017. AIDS Behav. 2020;24:532–539. doi: 10.1007/s10461-019-02689-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. AIDS. 2006;20:1447–1450. doi: 10.1097/01.aids.0000233579.79714.8d. [DOI] [PubMed] [Google Scholar]
- 9.Irene Hall H, Holtgrave DR, Maulsby C. HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS. 2012;26:893–896. doi: 10.1097/QAD.0b013e328351f73f. [DOI] [PubMed] [Google Scholar]
- 10.Dailey AF, Hoots BE, Hall H, Song R, Hayes D, Fulton P, et al. Vital signs: human immunodeficiency virus testing and diagnosis delays –United States. MMWR Morb Mortal Wkly Rep. 2017;66:1300–1306. doi: 10.15585/mmwr.mm6647e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gutman CK, Middlebrooks LS, Zmitrovich A, Camacho-Gonzalez A, Morris CR. Characteristics of children and adolescents diagnosed with HIV by targeted and diagnostic testing in a children’s hospital network. Acad Emerg Med. 2018;25:1306–1309. doi: 10.1111/acem.13491. [DOI] [PubMed] [Google Scholar]
- 12.Fauci AS, Redfield RR, Sigounas G, Weahkee MD, Giroir BP. Ending the HIV epidemic: a plan for the United States. J Am Med Assoc. 2019;321:844–845. doi: 10.1001/jama.2019.1343. [DOI] [PubMed] [Google Scholar]
- 13.Stein R, Song W, Marano M, Patel H, Rao S, Morris E. HIV testing, linkage to HIV medical care, and interviews for partner services among youths – 61 health department jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. MMWR Morb Mortal Wkly Rep. 2017;66:629–635. doi: 10.15585/mmwr.mm6624a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stephenson R, Todd K, Kahle E, Sullivan SP, Miller-Perusse M, Sharma A, et al. Project Moxie: results of a feasibility study of a telehealth intervention to increase HIV testing among binary and nonbinary transgender youth. AIDS Behav. 2020;24:1517–1530. doi: 10.1007/s10461-019-02741-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stephenson R, Metheny N, Sharma A, Sullivan S, Riley E. Providing home-based HIV testing and counseling for transgender youth (Project Moxie): protocol for a pilot randomized controlled trial. JMIR Res Protoc. 2017;6:e237. doi: 10.2196/resprot.8562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosengren AL, Huang E, Daniels J, Young SD, Marlin RW, Klausner JD. Feasibility of using GrindrTM to distribute HIV self-test kits to men who have sex with men in Los Angeles California. Sex Health. 2016;13:389–392. doi: 10.1071/SH15236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bauermeister JA, Golinkoff JM, Horvath KJ, Hightow-Weidman LB, Sullivan PS, Stephenson R. A multilevel tailored web app-based intervention for linking young men who have sex with men to quality care (Get Connected): protocol for a randomized controlled trial. JMIR Res Protoc. 2018;7:e10444. doi: 10.2196/10444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hightow-Weidman LB, Bauermeister JA. Engagement in mHealth behavioral interventions for HIV prevention and care: making sense of the metrics. mHealth. 2020;6:7. doi: 10.21037/mhealth.2019.10.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gamarel KE, Nelson KM, Stephenson R, Santiago Rivera OJ, Chiaramonte D, Miller RL. Anticipated HIV stigma and delays in regular HIV testing behaviors among sexually-active young gay, bisexual, and other men who have sex with men and transgender women. AIDS Behav. 2018;22:522–530. doi: 10.1007/s10461-017-2005-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Evangeli M, Pady K, Wroe AL. Which psychological factors are related to HIV testing? A quantitative systematic review of global studies. AIDS Behav. 2016;20:880–918. doi: 10.1007/s10461-015-1246-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dowshen N, Lee S, Matty Lehman B, Castillo M, Mollen C. IknowUshould2: feasibility of a youth-driven social media campaign to promote STI and HIV testing among adolescents in Philadelphia. AIDS Behav. 2015;19:106–111. doi: 10.1007/s10461-014-0991-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brown J, Kuo I, Bellows J, Barry R, Bui P, Wohlgemuth J, et al. Patient perceptions and acceptance of routine emergency department HIV testing. Public Health Rep. 2008;123(Suppl 3):21–26. doi: 10.1177/00333549081230S304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Frye V, Wilton L, Hirshfied S, Chiasson MA, Usher D, Lucy D, et al. “Just because it’s out there, people aren’t going to use it.” HIV self-testing among young, black MSM, and transgender women. AIDS Pat Care STDS. 2015;29:617–624. doi: 10.1089/apc.2015.0100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merchant RC, Seage GR, Mayer KH, Clark MA, DeGruttola VG, Becker BM. Emergency department patient acceptance of opt-in, universal, rapid HIV screening. Public Health Rep. 2008;123:27–40. doi: 10.1177/00333549081230S305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Swenson RR, Rizzo CJ, Brown LK, Vanable PA, Carey MP, Valois RF, et al. HIV knowledge and its contribution to sexual health behaviors of low-income African American adolescents. J Natl Med Assoc. 2010;102:1173–1182. doi: 10.1016/s0027-9684(15)30772-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arya M, Amspoker AB, Lalani N, Patuwo B, Kallen M, Street R, et al. HIV testing beliefs in a predominantly hispanic community health center during the routine HIV testing era: does English language ability matter? AIDS Pat Care STDS. 2013;27:38–44. doi: 10.1089/apc.2012.0230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Branson BM, Handsfield HH, Lampe MA, Janssen RS, Taylor AW, Lyss SB, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep. 2006;55:1–17. [PubMed] [Google Scholar]
- 28.US Preventive Services Task Force Screening for HIV infection US Preventive Services Task Force recommendation statement. J Am Med Assoc. 2019;321:2326–2336. doi: 10.1001/jama.2019.6587. [DOI] [Google Scholar]
- 29.Traynor SM, Rosen-Metsch L, Feaster DJ. Missed opportunities for HIV testing among STD clinic patients. J Commun Health. 2018;43:1128–1136. doi: 10.1007/s10900-018-0531-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Buzi RS, Madanay FL, Smith PB. Integrating routine HIV testing into family planning clinics that treat adolescents and young adults. Public Health Rep. 2016;131:130–138. doi: 10.1177/00333549161310S115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Petsis D, Min J, Huang Y-SV, Akers AY, Wood S. HIV testing among adolescents with acute sexually transmitted infections. Paediatrics. 2020;145:e20192265. doi: 10.1542/peds.2019-2265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Centers for Disease Control and Prevention. 2015 Sexually Transmitted Diseases Treatment Guidelines. Screening recommendations and considerations referenced in Treatment Guidelines and Original Sources. https://www.cdc.gov/std/tg2015/screening-recommendations.htm. Accessed 13 May 2020.
- 33.Arya M, Kallen MA, Williams LT, Street RL, Viswanath K, Giordano TP. Beliefs about who should be tested for HIV among African American individuals attending a family practice clinic. AIDS Pat Care STDS. 2012;26:1–4. doi: 10.1089/apc.2011.0053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arya M, Zheng MY, Amspoker AB, Kallen MA, Street RL, Viswanath K, et al. In the routine HIV testing era, primary care physicians in community health centers remain unaware of HIV testing recommendations. J Int Assoc Provid AIDS Care. 2014;13:296–299. doi: 10.1177/2325957413517140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mehta AS, Goyal MK, Dowshen N, Mistry RD. Practices, beliefs, and perceived barriers to adolescent human immunodeficiency virus screening in the emergency department. Pediatr Emerg Care. 2015;31:621–626. doi: 10.1097/PEC.0000000000000370. [DOI] [PubMed] [Google Scholar]
- 36.Kapogiannis BG, Koenig LJ, Xu J, Mayer KH, Loeb J, Greenberg L, et al. The HIV continuum of care for adolescents and young adults attending 13 urban US HIV care centers of the NICHD-ATN-CDC-HRSA SMILE Collaborative. J Acquir Immune Defic Syndr. 2020;84:92–100. doi: 10.1097/QAI.0000000000002308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lally MA, van den Berg JJ, Westfall AO, Rudy BJ, Hosek SG, Fortenberry JD, et al. HIV continuum of care for youth in the United States. J Acquir Immune Defic Syndr. 2018;77:110–117. doi: 10.1097/QAI.0000000000001563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Pat Care STDS. 2014;28:128–135. doi: 10.1089/apc.2013.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bhatt SR, Eckerle MD, Reed JL, Robinson V, Brown A, Lippe J, et al. Implementation of targeted point of care HIV testing in a pediatric emergency department. Pediatr Qual Saf. 2020;5:e248. doi: 10.1097/pq9.0000000000000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lubelchek R, Kroc K, Hota B, Sharief R, Muppudi U, Pulvirenti J, et al. The role of rapid vs conventional human immunodeficiency virus testing for inpatients: effects on quality of care. Arch Intern Med. 2005;165:1956–1960. doi: 10.1001/archinte.165.17.1956. [DOI] [PubMed] [Google Scholar]
- 41.Sterne J, Savović J, Page M, Elbers R, Blencowe N, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898. doi: 10.1136/bmj.l4898. [DOI] [PubMed] [Google Scholar]
- 42.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Calderon Y, Cowan E, Nickerson J, Mathew S, Fettig J, Rosenberg M, et al. Educational effectiveness of an HIV pretest video for adolescents: a randomized controlled trial. Pediatrics. 2011;127:911–916. doi: 10.1542/peds.2010-1443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Merchant RC, Clark MA, Langan TJ, IV, Mayer KH, Seage GR, Degruttola VG. Can computer-based feedback improve emergency department patient uptake of rapid HIV screening? Ann Emerg Med. 2011;58:S114–S119. doi: 10.1016/j.annemergmed.2011.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kurth AE, Severynen A, Spielberg F. Addressing unmet need for HIV testing in emergency care settings: a role for computer-facilitated rapid HIV testing? AIDS Educ Prev. 2013;25:287–301. doi: 10.1521/aeap.2013.25.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Aronson ID, Freeman R, Taylor T, Bennett AS. Developing digital media to destigmatize emergency department human immunodeficiency virus testing among sexual and racial minority youth: a hyper-iterative methodology. Cureus. 2020;12:e7209. doi: 10.7759/cureus.7209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Swenson RR, Hadley WS, Houck CD, Dance SK, Brown LK. Who accepts a rapid HIV antibody test? The role of race/ethnicity and HIV risk behavior among community adolescents. J Adolesc Health. 2011;48:527–529. doi: 10.1016/j.jadohealth.2010.08.013. [DOI] [PubMed] [Google Scholar]
- 48.Gillespie GL, Yap TL, Singleton M, Elam M. A summative evaluation of an EMS partnership aimed at reducing ED length of stay. J Emerg Nurs. 2009;35:5–10. [DOI] [PubMed]
- 49.Rothman RE. Current Centers for Disease Control and Prevention guidelines for HIV counseling, testing, and referral: Critical role of and a call to action for emergency physicians. Ann Emerg Med. 2004;44:31–42. doi: 10.1016/j.annemergmed.2004.01.016. [DOI] [PubMed] [Google Scholar]
- 50.Hankin A, Freiman H, Copeland B, Travis N, Shah B. A comparison of parallel and integrated models for implementation of routine HIV screening in a large, urban emergency department. Public Health Rep. 2016;131(Suppl):90–95. doi: 10.1177/00333549161310S111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Signer D, Peterson S, Hsieh Y-H, Haider S, Saheed M, Neira P, et al. Scaling up HIV testing in an academic emergency department: an integrated testing model with rapid fourth-generation and point-of-care testing. Public Health Rep. 2016;131(Suppl):82–89. doi: 10.1177/00333549161310S110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Carlos J, Montoy C, Dow WH, Kaplan BC. Patient choice in opt-in, active choice, and opt-out HIV screening: randomized clinical trial. BMJ. 2016;352:h6895. doi: 10.1136/bmj.h6895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kurth AE, Lally MA, Choko AT, Inwani IW, Fortenberry JD. HIV testing and linkage to services for youth. J Int AIDS Soc. 2015;18:23–28. doi: 10.7448/IAS.18.2.19433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Bauermeister JA, Pingel ES, Jadwin-Cakmak L, Harper GW, Horvath K, Weiss G, et al. Acceptability and preliminary efficacy of a tailored online HIV/STI testing intervention for young men who have sex with men: the Get Connected! program. AIDS Behav. 2015;19:1860–1874. doi: 10.1007/s10461-015-1009-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Winter S, Diamond M, Green J, Karasic D, Reed T, Whittle S, et al. Transgender people: health at the margins of society. Lancet. 2016;388:390–400. doi: 10.1016/S0140-6736(16)00683-8. [DOI] [PubMed] [Google Scholar]
- 56.Dorell CG, Sutton MY, Oster AM, Hardnett F, Thomas PE, Gaul ZJ, et al. Missed opportunities for HIV testing in health care settings among young African American men who have sex with men: implications for the HIV epidemic. AIDS Pat Care STDS. 2011;25:657–664. doi: 10.1089/apc.2011.0203. [DOI] [PubMed] [Google Scholar]
- 57.Mackenzie SLC, Kurth AE, Spielberg F, Severynen A, Malotte CK, St. Lawrence J, et al. Patient and staff perspectives on the use of a computer counseling tool for HIV and sexually transmitted infection risk reduction. J Adolesc Health. 2007;40:572. doi: 10.1016/j.jadohealth.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 58.Aronson ID, Guarino H, Bennett AS, Marsch LA, Gwadz M, Cleland CM, et al. Staff perspectives on a tablet-based intervention to increase HIV testing in a high volume, urban emergency department. Front Public Health. 2017;5:170. doi: 10.3389/fpubh.2017.00170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Nelson KM, Underhill K, Carey MP. Consent for HIV testing among adolescent sexual minority males: legal status, youth perceptions, and associations with actual testing and sexual risk behavior. AIDS Behav. 2020;24:373–378. doi: 10.1007/s10461-019-02424-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Felsen UR, Cunningham CO, Zingman BS. Increased HIV testing among hospitalized patients who declined testing in the emergency department. AIDS Care. 2016;28:591–597. doi: 10.1080/09540121.2015.1120268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hutchinson MK, VanDevanter N, Phelan J, Malamud D, Vernillo A, Combellick J, et al. Feasibility of implementing rapid oral fluid HIV testing in an urban university dental clinic: a qualitative study. BMC Oral Health. 2012;12:11. doi: 10.1186/1472-6831-12-11. [DOI] [PMC free article] [PubMed] [Google Scholar]