Abstract
This study uses national survey data to compare self-reported psychological distress among US adults in April and July 2020 by demographic and stressor type subgroups.
Serious psychological distress was reported by 13.6% of US adults in April 2020 vs 3.9% in 2018.1 How psychological distress has changed over the course of the coronavirus disease 2019 (COVID-19) pandemic is unknown.
Methods
We fielded wave 2 of the Johns Hopkins COVID-19 Civic Life and Public Health Survey from July 7 to July 22, 2020, among US adults aged 18 years and older who responded to wave 1, fielded April 7 to April 13, 2020. The sample was drawn from NORC’s AmeriSpeak panel of approximately 35 000 members sourced from NORC’s area probability sample and from a US Postal Service address-based sample covering 97% of US households.2 AmeriSpeak’s panel recruitment rate is 34%. The survey was administered online. The Johns Hopkins Bloomberg School of Public Health institutional review board deemed this study exempt and waived informed consent.
We measured psychological distress in the past 30 days using the Kessler 6 scale. A score of 13 or more on the 0- to 24-point scale indicated the validated measure of serious distress.3 We then asked, “During the past 30 days, have any of the following negatively impacted your mental health?” Respondents selected from a list of potential stressors affecting them or their family members, including concern about contracting COVID-19 or experiencing adverse effects related to COVID-19 on employment, finances, education, health insurance, and ability to obtain health care or childcare.
We compared prevalence of serious psychological distress overall and among demographic subgroups in July vs April, using the McNemar test to test for significant differences, defined as a 2-sided P < .05. We calculated the proportion of adults who reported serious distress in both April and July. χ2 Tests were used to compare the prevalence of each stressor among those with vs without serious distress. Analyses were conducted in Stata version 15 (StataCorp) and incorporated survey sampling weights to generate nationally representative estimates.
Results
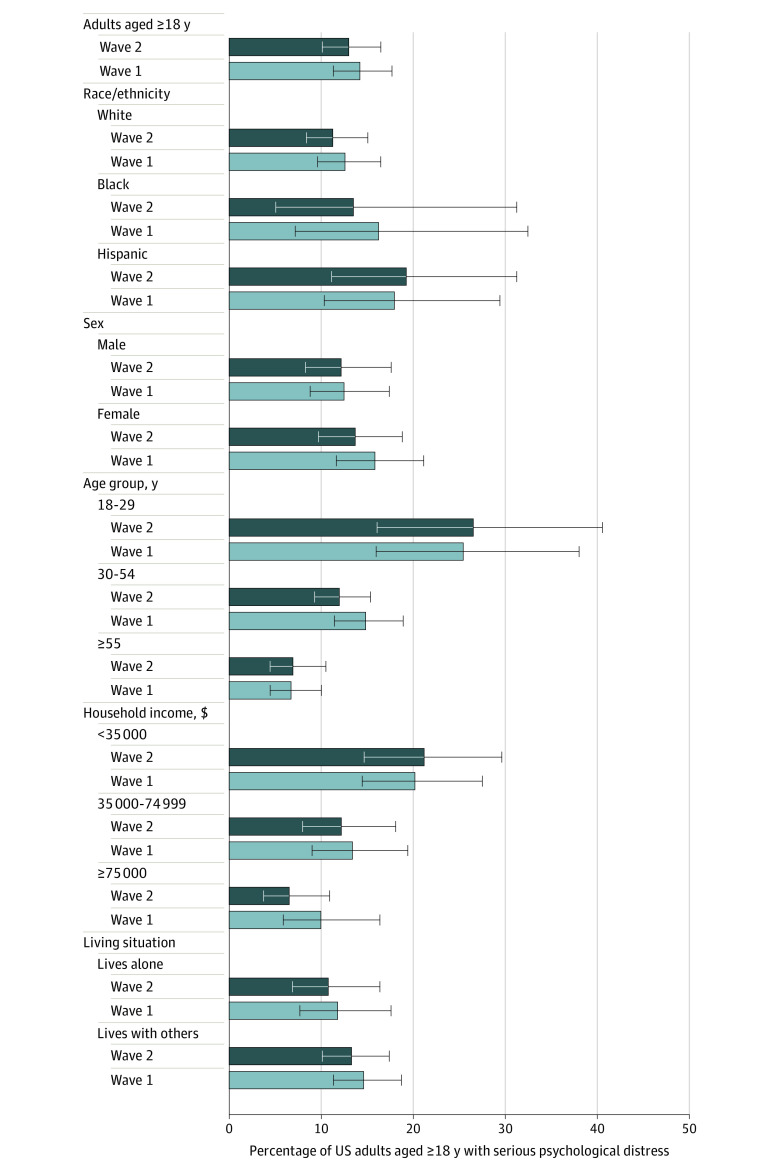
Of the 1466 adults surveyed, 1337 responded (response rate, 91.2%). In this cohort of US adults, 13.0% (95% CI, 10.1%-16.5%) reported serious distress in July 2020 relative to 14.2% (95% CI, 11.3%-17.7%) in April 2020 (P = .73) (Figure 1). Reported prevalence of serious distress did not significantly differ in July vs April for any subgroups. At both time points, reported prevalence was highest among adults aged 18 to 29 years (25.4% [95% CI, 16.0%-38.0%] in April; 26.5% [95% CI, 16.1%-40.5%] in July), those with income less than $35 000 (20.2% [95% CI, 14.4%-27.5%] in April; 21.2% [95% CI, 14.7%-29.6%] in July), and Hispanic individuals (17.9% [95% CI, 10.3%-29.4%] in April; 19.2% [95% CI, 11.1%-31.2%] in July). Seventy-two percent (95% CI, 60.1%-81.3%) of adults reporting serious distress in July also reported serious distress in April.
Figure 1. Serious Psychological Distress Among a National Cohort of 1337 US Adults in April and July 2020.
Data are from waves 1 and 2 of the Johns Hopkins Civic Life and Public Health Survey. The 2 waves were fielded in a longitudinal cohort of 1337 US adults aged 18 years or older. Wave 1 was fielded from April 7 to 13, 2020. Wave 2 was fielded from July 7 to 22, 2020. The McNemar χ2 test was used to test for statistically significant differences in proportion of respondents reporting serious psychological distress in July vs April 2020. No differences were statistically significant at the P < .05 level. Psychological distress was measured using the Kessler 6 scale, with scores of 13 or older indicating serious psychological distress. Race/ethnicity was collected as part of the demographic profile in April 2020. The options were defined by the study investigators and participants classified their own race/ethnicity. The survey measured 3 race categories that are not reported due to small sample sizes: other race, non-Hispanic (n = 13); 2 or more races, non-Hispanic (n = 25); and Asian, non-Hispanic (n = 34). The error bars indicate 95% CIs.
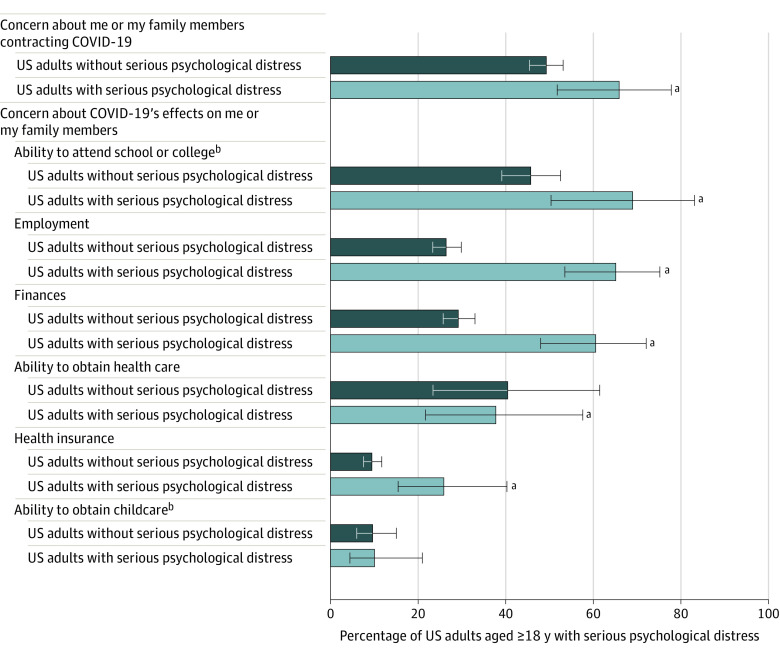
Adults with serious distress were statistically significantly more likely than those without serious distress to report all stressors except ability to obtain childcare (Figure 2). The most common stressors reported by the overall sample with serious distress (n = 132) were concerns about contracting COVID-19 (65.9% [95% CI, 51.8%-77.7%]) and pandemic effects on employment (65.1% [95% CI, 53.6%-75.1%]) and finances (60.6% [95% CI, 48.0%-72.0%]). Among the subgroup of adults with serious distress attending college and/or with school-aged children (n = 52), 69.0% (95% CI, 50.3%-83.1%) cited educational interruptions as a stressor.
Figure 2. Coronavirus Disease 2019 (COVID-19)–Related Concerns Reported as Negatively Influencing Mental Health Among US Adults in July 2020.
Measures are from wave 2 of the Johns Hopkins Civic Life and Public Health Survey, fielded from July 7 to 22, 2020, with 1337 total respondents and 132 respondents with serious psychological distress. Psychological distress was measured using the Kessler 6 scale, with scores of 13 or higher indicating serious distress. The error bars indicate 95% CIs.
aStatistically significant difference at the P < .05 level between those with vs without serious psychological distress. Pearson χ2 test was used to test for significant differences. Exact P values for each comparison were P = .03 (contracting COVID-19); P = .02 (school); P < .001 (employment); P < .001 (finances); P < .001 (health care); P < .001 (health insurance); and P = .95 (childcare).
bStressor measured in a subset of the overall sample. Concern about the effects of COVID-19 on the ability to attend school, college, or other education was measured among US adults aged 18 years or older who reported having children aged 0 to 17 years in their household and/or reported that they themselves were currently attending or planning to attend college in 2020. This subgroup included 436 adults overall, including 52 with serious psychological distress and 384 without serious psychological distress. Concern about COVID-19’s effects on the ability to obtain childcare was measured among the 365 US adults aged 18 years or older who reported having children aged 0 to 17 years in their household.
Discussion
Reported prevalence of serious psychological distress among US adults was 13.6% in April 2020 and 13% in July 2020. Persistent distress increases risk of psychiatric disorders, which the Kessler 6 scale predicts.3 High prevalence at both time points suggests that the pandemic’s longer-term disruptions are important drivers of distress. More than 60% of adults with serious distress reported that pandemic-related disruptions to education, employment, and finances negatively affected their mental health. These stressors may be particularly salient to young adults, about a quarter of whom reported serious distress in both April and July. Thirty-five percent of adults with serious distress cited inability to obtain health care as a contributing factor, highlighting the need to facilitate safe and affordable health care access during the pandemic and beyond.4,5
Limitations of the study include potential sampling and response biases. AmeriSpeak uses best-practice probability-based recruitment to minimize sampling bias,6 and survey weights incorporated nonresponse adjustments.
Section Editor: Jody W. Zylke, MD, Deputy Editor.
References
- 1.McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324(1):93-94. doi: 10.1001/jama.2020.9740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.NORC at the University of Chicago Technical overview of the AmeriSpeak panel NORC's probability-based household panel. Updated June 18, 2020. Accessed October 7, 2020. https://amerispeak.norc.org/Documents/Research/AmeriSpeak%20Technical%20Overview%202019%2002%2018.pdf
- 3.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184-189. doi: 10.1001/archpsyc.60.2.184 [DOI] [PubMed] [Google Scholar]
- 4.Slavitt A. The COVID-19 pandemic underscores the need to address structural challenges of the US health care system. JAMA Health Forum. 2020; 1(7):e200839-e200839. doi: 10.1001/jamahealthforum.2020.0839 [DOI] [PubMed] [Google Scholar]
- 5.Butler SM. After COVID-19—thinking differently about running the health care system. JAMA Health Forum. 2020;1(4):e200478-e200478. doi: 10.1001/jamahealthforum.2020.0478 [DOI] [PubMed] [Google Scholar]
- 6.American Association for Public Opinion Research Report on online panels. Accessed May 14, 2020. https://www.aapor.org/Education-Resources/Reports/Report-on-Online-Panels.aspx