Abstract
The relationship between problems accessing medical care and depression is examined in a sample of older Hispanics (Puerto Rican, Dominican, and Other Hispanic) in Massachusetts and a comparison group of same-neighborhood non-Hispanic Whites. The research questions are: Do older Hispanics experience more problems with access to medical care than do older non-Hispanic Whites? What types of access problems do Hispanics encounter, and how do these relate to depression symptoms? The data come from the Massachusetts Hispanic Elders Study; descriptive and multivariate regression analysis procedures are used. Older Hispanics report more problems obtaining medical care than do older non-Hispanic Whites. Puerto Ricans report significantly more transportation problems to access medical care. For Dominicans and Puerto Ricans, being female, living alone, and lower education attainment are associated with depression. For Puerto Ricans, health problems, disability, and access problems are also significant.
Keywords: Hispanics, depression, access, transportation, Puerto Ricans
Depressive symptomatology is common among older Hispanics, and is more frequent among Puerto Ricans than other Hispanic subgroups (Falcon & Tucker, 2000; Gonzalez, Haan, & Hinton, 2001; Kemp, Staples, & Lopez-Aqueres, 1987; Lopez-Aqueres, Kemp, Plopper, Staples, & Brummel-Smith, 1984). Like their mainland counterparts, Puerto Ricans living on the island also experience high prevalence of depressive symptomatology (Vera et al., 1991). Several factors have been identified as associated with an increased likelihood of depression for aging Puerto Ricans on the mainland. Chief among them are financial strain, a high number of medical problems, social isolation, low acculturation, recent migration, younger age, being female, being separated or divorced, poor health status, functional limitations, limited emotional support, and a history of “ataque de nervios” (Kemp et al., 1987; Krause & Goldenhar, 1992; Meyler, Stimpson, & Peek, 2006; Ontiveros, Black, Jakobi, & Goodwin, 1999; Roberts, Kaplan, Shema, & Strawbridge, 1997; Robison et al., 2003; Rogler, Cortes, & Malgady, 1991; Weingartner, Robison, Fogel, & Gruman, 2002)
Puerto Ricans also present a more complicated health profile than other groups. Non-Puerto Rican Hispanic elderly (mainly those of Mexican origin) show relative high life expectancy and, despite socioeconomic disadvantage, low risk for a number of health conditions including cancer and heart disease—an intriguing phenomenon that has been described in the literature as the Hispanic epidemiological paradox (Markides & Coreil, 1986) or simply Hispanic paradox. This apparent counterintuitive phenomenon is observed mainly among recent immigrants of low socioeconomic status (SES), especially those of Mexican origin (Borrell, 2005). Much debate on the Hispanic paradox is still ongoing, but it has been argued that a selective healthy migrant factor, salmon effect, possible underreporting of deaths, and risk profile may contribute to but do not explain the paradox (Franzini, Ribble, & Keddie, 2001). It is hypothesized that some social and cultural characteristics of Hispanic communities might be protective, namely, diet, healthy behaviors, and strong social ties that tend to wane with increased acculturation (Chung, 2006).
The Hispanic paradox does not fit with the experience of aging Puerto Ricans. Instead, Puerto Ricans present a rather problematic health profile that includes lower life expectancy, lower self-rated health and significantly more disability than other Hispanics, African Americans, and non-Hispanic Whites (NCHS/CDC Public Affairs, 2000). When the demographic factors and the English-language disadvantage that distinguish Puerto Ricans from both Blacks and Whites are taken into account the effect of race and ethnicity on disability is reduced, but not eliminated. Indeed, older Puerto Ricans are at high risk for dependency, and within this population, those with limited English skills are at particular risk (Mahard O’Donnell, 1989). Puerto Rican elders with disabilities in the Northeast are more severely disabled, particularly in instrumental activities of daily living (ADL), and they have limited sources of informal care and use formal services minimally (Delgado & Tennstedt, 1997).
Dominican elders comprise another large segment of the elder population in Massachusetts. Puerto Ricans and Dominicans are among the most disadvantaged Hispanic groups in the United States (Falcon, Tucker, & Bermudez, 1997). Little is known about Dominican elders but existing research suggests that they fare comparably to Puerto Ricans on health outcomes, including depression. Dominicans in the Northeast experience similar rates of poverty, lack of participation in community programs, and extremely poor health (Falcon et al., 1997; Falcon & Tucker, 2000).
Overall, older Hispanics are at greater risk for several economic, social, mental health, and medical problems in comparison to other minority elders. Within Hispanic subgroups, Mexican Americans have the highest incidence of diabetes, whereas Puerto Ricans show greater psychological distress than other Hispanic groups (Burnette & Mui, 1999; Tucker, Bermudez, & Castaneda, 2000). Hispanics in general—as well as other underrepresented and underserved groups—have also been found to experience problems accessing health services. Some of the access problems experienced by older Hispanics include limited English proficiency, lack of bilingual staff at clinics, and lack of private or public health insurance (Andersen, Lewis, Giachello, Aday, & Chiu, 1981; Burnette & Mui, 1999; Derose & Baker, 2000; Haas et al., 2004; Hornberger et al., 1996; Kirby, Taliaferro, & Zuvekas, 2006; Solis, Marks, Garcia, & Shelton, 1990; Taira, 1999). Puerto Ricans use medical services more frequently than other Hispanics but are less likely to have a physician’s office as the primary source of care (Burnette & Mui, 1999). This inadequate access to medical care among older Hispanics is particularly troublesome, as access to medical care is instrumental in properly diagnosing and addressing health problems, including depression, and appropriately referring the client for treatment. Still, the existing literature has not yet tackled the question of how problems with access to medical care may be related to depression outcomes for older Hispanics and for older Puerto Ricans in particular. A growing number of studies suggest that experiencing depression may in itself hinder access to medical care, and thus result in lack of addressing problematic health conditions (Fitzpatrick, Powe, Cooper, Ives, & Robbins, 2004; Haviland, Pincus, & Morales, 2003; Miller, Druss, Dombrowski, & Rosenheck, 2003). For instance, people with chronic mental disorders may be at risk for substandard medical treatment and poor quality of care received (Miller et al., 2003); the psychological effect of negative perceptions of care may later cause future barriers for seeking health care (Fitzpatrick et al., 2004). Finally, depressed patients may be more pessimistic and less motivated to seek health care (Haviland et al., 2003). Because an elevated number of health problems is consistently and strongly associated with depression among older Puerto Ricans and Dominicans (Falcon & Tucker, 2000), this article examines how reported problems with access to medical care may contribute to increased depressive symptoms among aging Hispanics of Puerto Rican and Dominican origin in Massachusetts.
As U.S. citizens, Puerto Ricans are entitled to public health insurance, namely, Medicare and Medicaid programs, so insurance coverage among low-income Puerto Ricans may not be as problematic as it is for other aging Hispanics. Having U.S. citizenship since 1917, they also present a particular pattern of migration and settlement, which includes immigration, outmigration, and circular migration (Baer, 1992) and distinguishes them from other immigrant Hispanic groups.
Puerto Ricans have resided in Massachusetts in significant numbers since the 1960s and have grown at a steady pace since then. This Hispanic population growth coincides with an increase in poverty rates (Melendez, 1993). For the past three decades, Puerto Ricans and other Hispanics from the New York City area have engaged in a process of dispersion and Massachusetts has been one of their preferred destinations of secondary settlement (Melendez, 1993). Thus, the recent poverty-stricken and migratory character of Puerto Ricans and other Hispanic groups in Massachusetts makes this population uniquely different from others (Falcon & Tucker, 2000). We anticipate that access problems for Puerto Ricans in Massachusetts might be associated with sociodemographic characteristics of the group, such as the number of women living alone and health characteristics (number of health problems and disability) that set Puerto Ricans in Massachusetts apart from other Hispanic groups in the United States.
Healthy normal-functioning older adults are at no greater risk of depression than younger adults (Roberts et al., 1997). However, prevalence of depression tends to increase with age due to an increase in health-related disability. Depression is significantly more prevalent for older Hispanics compared to the general older population. In addition, it is higher for women in most populations. For instance, Roberts et al. found an overall prevalence of 6.6% for older American men and 10.1% for older American women. In contrast, research on older Hispanics has found a prevalence of depression of 25% and above, although this rate varies by Hispanic subgroup (Gonzalez et al., 2001; Kemp et al., 1987; Lopez-Aqueres et al., 1984; Ontiveros et al., 1999). Previous research reported a higher prevalence of depressive symptomatology than in previous studies among older Puerto Ricans (44%) and Dominicans (32%) aged 60 years or more (Falcon & Tucker, 2000).
In general, factors associated with depression among older adults include being female, lack of insurance, financial strain, chronic health conditions, and disability (Roberts et al., 1997). In addition to these, several sociocultural factors have been associated with the illness in older Hispanics: immigrant status, levels of acculturation and assimilation, health locus of control, and recency of immigration to the United States (Cuellar, Bastida, & Braccio, 2004; Gonzalez et al., 2001; Kemp et al., 1987). Moreover, a link between immigration and gender has also been shown with female immigrants found to be at higher risk for depression than males (Ontiveros et al., 1999).
Problems to Access Medical Care for Older Hispanics
For older adults, problems with access to medical care increase sharply with declining levels of family income and for those who lack private health care insurance. Residents of rural areas and poor areas are at a disadvantage in accessing care, whereas residents of neighborhoods that are homogeneous in ancestral heritage appear to have better access to care (Auchincloss, Van Nostrand, & Ronsaville, 2001). Hispanics as a whole are the most disadvantaged with regard to health care access, but Hispanics are comprised of heterogeneous groups that differ in their experiences with health care (Kirby et al., 2006). Kirby and colleagues maintain that because of the U.S. citizenship access, Puerto Ricans fare comparable to Blacks in the magnitude of disparities in access to medical care, except for language-related problems that impede access to ambulatory care for Hispanics in general (Kirby et al., 2006).
English proficiency appears to be a fundamental factor in explaining disparities in health and health care access among older adults, particularly older Hispanics. Older adults with limited English proficiency have been shown to have worse access to care and poorer health status than do English-proficient, older Puerto Ricans. They were also found to be more likely to report transportation-related problems with access to health care than other Hispanic groups (Becerra, 1984).
Objectives
The purpose of this study is to explore the relationship between reporting problems with access to medical care and depression symptoms among older Hispanics in Massachusetts and a neighborhood-based comparison group of non-Hispanic White elders. The study focuses on three main research questions:
Research question 1: Do older Hispanics experience more problems accessing health care than non-Hispanic Whites living in the same neighborhoods?
Research question 2: Do older Puerto Ricans report different problems with access to medical care than other Hispanic groups and non-Hispanic Whites?
Research question 3: After controlling for various sociodemographic and health variables, do problems with access to medical care relate to depressive symptomatology in older Puerto Ricans and Dominicans?
There are two central hypotheses driving the analysis. Based on the literature, we anticipate that older Hispanics in general will be more likely to report problems accessing medical care than non-Hispanic Whites living in the same neighborhoods. We also believe that there will be some differences across Hispanic groups in the types of problems reported. Further, because of the implications of limitations in access to medical care, especially for those with high numbers of health problems, we expect that problems related to medical care access will be associated with higher levels of depressive symptomatology among older Puerto Ricans.
Methods and Variables
The data used for this study are from the Massachusetts Hispanic Elders Study (MAHES)—a representative sample of Hispanics, aged 60 years or more, in the state of Massachusetts, and a neighborhood-based comparison group of non-Hispanic White elders. The data collection started in 1992 and ended in 1997. A two-stage cluster sample was used to identify subjects, with sampling proportionate to size by county for Hispanics aged 60 years and older within counties in Massachusetts. Counties and census blocks served as the two levels of the hierarchy. Sample clusters (30) were randomly assigned to counties based on the proportional representation of Hispanics aged 55 years and older (in 1990) in the county (Levy & Lemeshow, 1980). After cluster samples were allocated to counties, samples of 25 subject blocks were selected, with proportionate probability of selection of a block to the number of eligible Hispanics in the block. Blocks drawn into the sample were enumerated and respondents were selected randomly. There were 1,033 face-to-face interviews completed, which include 475 Puerto Ricans, 146 Dominicans, 160 other Hispanics, and 252 neighborhood non-Hispanic Whites (NHWs). The comparison group of non-Hispanic Whites is comprised of subjects living in the same neighborhoods with Hispanics. The respondents were asked to complete comprehensive questionnaires, including modules on social and economic background, migration history, health history, physical functioning, depression, cognitive function, dietary intake, and prescription drug use. In addition, body measurements of weight, height, blood pressure, and blood samples were also collected. Bilingual interviewers trained in the administration of questionnaires conducted the interviews. The vast majority of respondents answered the questionnaire in Spanish.
Dependent Variables
Depressive symptomatology.
The number of symptoms of depression was measured with the Center for Epidemiologic Studies Depression scale (CES-D), which has been widely used in epidemiological studies. In addition, this scale has been validated for use with Hispanics, and with Hispanic elders in particular (Mahard, 1988; Robison, Gruman, Gaztambide, & Blank, 2002). Participants are asked to indicate whether they have experienced—and how frequently they have experienced—a number of indicators of depressive symptoms within the past 2 weeks. A score of 16 through 40 is generally interpreted as an indication of symptoms of depression.
Problems with access to medical care.
We created a dichotomous variable from subjects’ responses to the following question: “Sometimes people have problems in getting medical care. Have you had any problems getting medical care?” The value 1 was assigned to those who answered yes, and value 0 to those who responded no, they had had no problems obtaining care.
Independent Variables
The independent variables selected from the MAHES survey include the following broad categorizations: ethnicity, sociodemographics, and health-related variables.
Ethnicity.
Ethnic groups included Puerto Rican, Dominican, Other Hispanic and non-Hispanic Whites living in the same neighborhoods in the Boston Metro area. Indicator variables for each of the three Hispanic subgroups were included in the analysis, with non-Hispanic Whites as the reference category.
Sociodemographics.
Sociodemographic variables included sex (female = 1), age, household income above the poverty threshold (below threshold = 1), total years of education (number of education years), and living alone (living alone = 1). Age was included as number of years in the linear regressions, with CES-D score as the dependent variable. We also created a three-category age variable (ages 60–64, 65–74, and 75 years or older) to examine potential age cohort differences in depression symptomatology.
Acculturation.
The acculturation variable, language inclusion, was created from a set of variables that asked the respondents which language they used in daily activities such as talking to friends in their neighborhood, reading, and listening to the radio. Respondents were categorized into three groups that correspond to the frequency of use of English in these activities. Thus, respondents who are frequent users of English are seen as being language included, whereas those who are low-frequency users are seen as being language excluded or isolated.
Health Variables
Health variables included (a) a count of the number of chronic health problems (excluding depression) reported by the respondent at the time of the survey; (b) the CES-D depression score at the time of the survey; and (c) disability, which is the sum of the responses to the ADL and the instrumental activities of daily living (IADL) scales.
Problems with access to medical care.
Participants who indicated having problems with access to medical care were asked the follow-up question, “Why did you have a problem?” and were provided a list of common problems from which to choose up to three. The multiple response options were the following: Because care was not available when you needed it? “Because of how much it cost? Because you did not know where to go?” “Because you did not have a way to get there?” “Because the hours were not convenient?” “Because you had to wait too long to get an appointment?” “Because you would lose pay from work?” “Because you had to wait too long in the office or clinic?” “Because the staff at the office or clinic was disrespectful?” “Because you had no confidence in the staff?” “Because they did not speak Spanish/Others?” “Because there were no (Hispanic) staff members at the office or clinic?” and an option to indicate Other.
In analyzing the pattern of responses, we arrived at four categories of problems—transportation problems, cost problems, language problems, and staff trust problems. Dichotomous variables for transportation, cost, language, and staff trust problems were created, with values 1 (if they had the problem) and 0 (if they had not had that problem).
Analysis Plan
We used the SPSS software (Version 16.0) to manage and analyze the data. Mean comparisons are presented first to highlight differences in socioeconomic and health indicators for each of the ethnic groups. Cross-tabulation analyses of frequencies with the problems to access medical care variables by ethnicity and type of problem are then presented to show differences in both the magnitude and the type of access problems across the groups. To examine the impact of access problems on depression symptoms, net of other key variables, we used linear regression models. Variables were added sequentially, in clusters of related variables, to the model. First, we entered the ethnicity variables to show disparities in depression symptoms by group. Second, we added sociodemographics (income, sex, age, marital status proxy). A third set includes cultural capital- type variables—education and language inclusion—because these variables have been shown in prior studies to explain disparities in depression in many Hispanic samples. The fourth model includes the health variables (health problems and disability). Finally, the last model added the access problems variable to examine its effect independent of other sociodemographic and health variables.
Results
Table 1 presents general descriptive statistics for the respondents by ethnicity. Puerto Ricans and Dominicans were the most disadvantaged groups, as highlighted by several indicators. On average, the income of Puerto Ricans was only 9.4% above the poverty threshold, compared to 92% above it for non-Hispanic Whites. Average income for Dominicans was even lower, at 5.2% below the poverty threshold. Average education among Puerto Ricans and Dominicans in the sample fell in the elementary school category, at 4.8 years, whereas non-Hispanic Whites had an average of 11.3 years. Puerto Ricans reported the greatest number of health problems (2.3), whereas the Other Hispanic group reported the fewest (1.7). Puerto Ricans also report higher number of disabilities (2.86) followed by Dominicans (2.11) and Other Hispanics (1.92), whereas non-Hispanic Whites show the lowest number (1.51). In addition, Puerto Ricans showed the highest average CES-D score (16.17)—at a level that is above the standard cutoff for depressive symptomatology in the CES-D scale. In comparison, non-Hispanic Whites had the lowest depressive symptomatology scores. Dominicans were particularly disadvantaged. In addition to the lowest average income and education, they reported less language inclusion than the rest of the groups (1.83) and were second to Puerto Ricans in the number of health problems (2.08), number of disabilities (2.11), and symptoms of depression (13.24).
Table 1.
Descriptive Characteristics by Ethnicity
| Variables | Puerto Rican | Dominican | Other Hispanic | Non-Hispanic White | Total |
|---|---|---|---|---|---|
| Age (60–93; years, mean) | 69.7 | 69.2 | 70.9 | 72.9 | 70.6 |
| Above poverty (threshold = 1; income, mean) | +9% | −5% | +74% | +92% | +38% |
| Education (0–17; years, mean) | 4.86 | 4.86 | 7.43 | 11.3 | 6.67 |
| Language inclusion (1–3; mean level)a | 2.12 | 1.83 | 2.29 | 2.99 | 2.32 |
| Health problems (0–12; mean, number) | 2.32 | 2.08 | 1.68 | 1.90 | 2.08 |
| Disability (0–17; mean, number) | 2.86 | 2.11 | 1.92 | 1.51 | 2.10 |
| CES-D score (mean)b | 16.2 | 13.2 | 11.7 | 10.0 | 13.5 |
| Total (%) | 46 | 14 | 16 | 24 | 100 |
Note: CES-D = Center for Epidemiologic Studies on Depression.
Language inclusion: 1 = isolated; 2 = partial inclusion, 3 = inclusion.
CES-D-Score ≥16 = symptomatic of depression.
Figure 1 shows the distribution of having problems with access to medical care by group. There are marked differences between Hispanics and non-Hispanic Whites in the reporting of problems with access. Hispanics are more than twice as likely as NHW to report access problems. Among Hispanics, Puerto Ricans stand out with about 1 in 4 Puerto Ricans reporting having experienced at least one problem accessing care. This is in contrast to Dominicans among who 1 in 5 reported a problem or NHW where 1 in 10 reported a problem.
Figure 1.
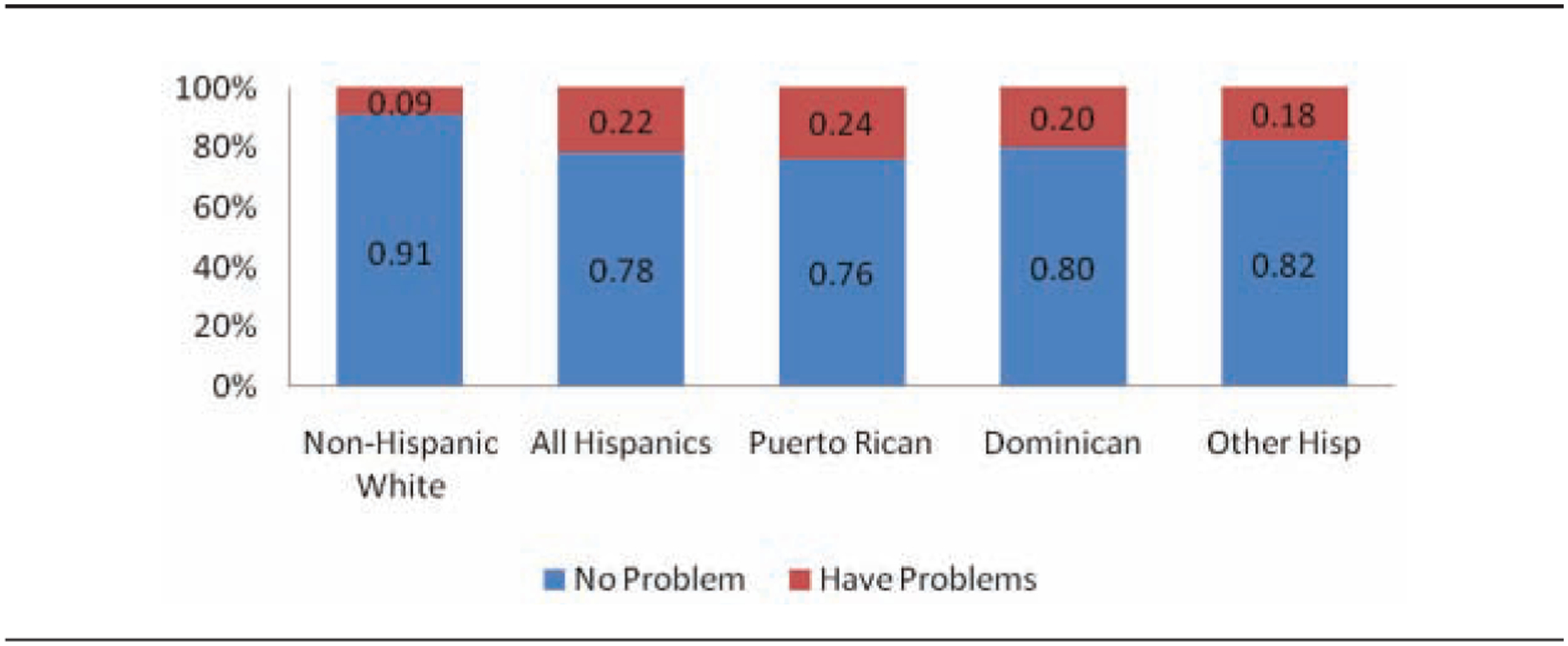
Problems With Access to Medical Care by Group
Table 2 presents the most frequently cited source of access problem by group. A larger number of Hispanics reported significantly more access problems (23.9%, p = .00) than non-Hispanic Whites (9.3%). Puerto Ricans reported more transportation problems and language problems than other groups. Although only a small percentage of the Dominicans (2.8%) and the Other Hispanics (3.7%) reported problems with transportation, almost 12% of Puerto Ricans reported having transportation problems. In addition, 6.2% of Puerto Ricans (p = .002) reported language problems in obtaining medical care. The latter is also a problem for the Dominicans, lesser so for Other Hispanics, and not a problem for non-Hispanic Whites.
Table 2.
Percentage of Respondents Who Reported Problems Obtaining Care by Ethnicity and Type of Problem
| Variable | Puerto Rican | Dominican | Other Hispanic | Hispanics | Non-Hispanic Whites | Total |
|---|---|---|---|---|---|---|
| Transportation | 11.6*** | 2.8* | 3.7 | 8.3*** | 2.4 | 6.9 |
| Language | 6.1** | 5.6 | 3.1 | 5.4*** | 0.0 | 4.1 |
| Cost | 1.9 | 4.2 | 3.7 | 2.7 | 2.8 | 2.7 |
| Staff trust | 1.5 | 0.0 | 1.2 | 1.2 | 1.6 | 1.3 |
| Other | 2.8 | 7.7 | 6.1 | 4.4 | 2.5 | 3.9 |
| Problems total | 23.9*** | 20.3 | 17.8 | 22.0*** | 9.3 | 18.9 |
p < .05.
p < .01.
p < .001.
Table 3 presents results from a linear regression model with the CES-D scores as the dependent variable. Prior research has shown (Falcon & Tucker, 2000) that Puerto Ricans and Dominicans experience a higher prevalence of depression than other Hispanic groups or non-Hispanic Whites. After controlling for sociodemographics (Model 3), only Puerto Ricans remained significantly different from non-Hispanic Whites in CES-D scores (b = .16, p = .002) suggesting that there are other factors not included in the model that account for the differences. Females showed significantly higher CES-D scores (b = .09, p = .002), as well as those living alone (b = .19***, p = .000), whereas having more years of education is inversely associated with depression scores (b = −.17***, p = .000). Indeed, in this model, education explained away the differences in depressive symptomatology between Dominicans and non-Hispanic Whites.
Table 3.
Variables Associated With Depressive Symptomatology
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| b | b | b | b | b | |
| Puerto Ricana | 0.26*** | 0.29*** | 0.16** | 0.12** | 0.10* |
| Dominicana | 0.09** | 0.13*** | 0.03 | 0.02 | 0.01 |
| Other Hispanica | 0.05 | 0.08* | 0.02 | 0.02 | 0.01 |
| Sex (female = 1) | 0.08** | 0.09** | 0.07** | 0.07** | |
| Lives alone | 0.13*** | 0.19*** | 0.11** | 0.09** | |
| Age | −0.03 | −0.06 | −0.09** | −0.07* | |
| Education | −0.17*** | −0.11** | −0.11** | ||
| Health problems | 0.23*** | 0.21*** | |||
| Disability | 0.15*** | 0.14*** | |||
| Access problems | 0.19*** | ||||
| R2 | 0.05 | 0.07 | 0.09 | 0.20 | 0.23 |
| Adjusted R2 | 0.05 | 0.06 | 0.08 | 0.19 | 0.22 |
| N | 1,030 | 1,030 | 1,030 | 1,030 | 1,030 |
Note: Analysis controlled for language inclusion and income above the poverty threshold.
Relative to non-Hispanic Whites.
p < .05.
p < .01.
p < .001.
In Model 4 the health variables (health problems and disability) were entered. The two health variables were the strongest predictors of depression for older Puerto Ricans: number of health problems (b = .23, p = .000) and disability (b = .15, p = .000). Interestingly, the age variable becomes significant in this model (b = −.09, p = .04), suggesting that after controlling for health problems and disability, the young old do tend to experience higher symptoms of depression. Despite the importance of the health variables in the model, the gap in CES-D scores between Puerto Ricans and non-Hispanic Whites remains.
In Model 5, the access problems variable is entered into the equation. Despite a number of strong predictors already in the model, reporting problems with access to medical care is independently and very strongly associated with depression symptoms (b = .19***, p = .000). As suspected, having access problems is an important factor in explaining the high symptoms of depression among Puerto Ricans. Although the Puerto Rican ethnicity variable remains significant in the final model, it has been weakened by the inclusion of the access to medical care variable (b = .10, p = .03).
Discussion
This study aimed to examine the connection between reporting problems with access to medical care and depressive symptoms among Hispanic elders in Massachusetts and a comparison group of non-Hispanic Whites living in the same neighborhoods. To our knowledge, this is the first study to have addressed this question within the research literature on aging. Both hypotheses were supported. Older Hispanics in Massachusetts reported more problems with access to medical care than did non-Hispanic Whites. There were also differences in the frequency and the type of problems reported by Hispanic subgroup. Puerto Ricans experience more access problems than any other group, particularly transportation problems. In addition, problems with access to medical care were strongly associated with depressive symptomatology. Although there is prior empirical evidence of transportation and language problems to access medical care among older Puerto Ricans, our study is the first—to our knowledge—to have found an association between these problems and elevated depression symptoms.
Other factors associated with depression symptoms among Puerto Ricans were health problems, lower education, disability, living alone, being female, and of younger age. These correlates have also been found in different studies on older Puerto Rican populations (Kemp et al., 1987; Krause & Goldenhar, 1992; Meyler et al., 2006; Ontiveros et al., 1999; Roberts et al., 1997; Robison et al., 2003; Rogler et al., 1991; Weingartner et al., 2002). Education in particular helped to explain disparities in depression symptoms between Dominicans and non-Hispanic Whites, which suggest that possessing lower education or cultural capital—more broadly—may impede adequate education on how to address mental health issues. Some studies with Hispanic populations and Puerto Rican populations in particular found a significant association between lower acculturation, immigrant status, and recency in the United States and depression. However, when we tested those variables with our sample we found no significant effect. It is possible that contextual factors are at play here, such as the existence of established social networks in the Boston area. For example, in our current survey of Puerto Ricans in Boston, we conducted ethnographic interviews with 40 Puerto Ricans aged 50 years and older and found that those who migrated in recent years were likely to have done so to join family members and other existing networks who serve as facilitators for the newcomers. Therefore, the strong disruption of social ties experienced by many recent Hispanic immigrants may not fit the experiences of older Puerto Ricans in Boston.
In this study, we also identified transportation problems as the major barrier to access medical care among Puerto Ricans in our sample. This finding also differs from other studies on access to medical care among Hispanics, which have shown that limited English proficiency and other communication barriers were the most prevalent problems. Prior research on access to medical care with Hispanics has focused on language barriers between medical care providers and Hispanic clients (Derose & Baker, 2000; Hornberger et al., 1996; Morales, Cunningham, Brown, Liu, & Hays, 1999; Ponce, Hays, & Cunningham, 2006; Solis et al., 1990). Certainly, language and communication barriers are a major problem for many Spanish-speaking elders, especially if they live in areas where there are few Spanish-speaking providers. This study has shown that although Hispanics in Massachusetts do report language problems, transportation is the most common problem encountered by Puerto Ricans (the largest Hispanic group in Massachusetts) in the Boston area. An examination of interactions between the transportation problems variable and other variables in the model did not yield any significant findings.
There are several implications of these findings for policy and for future research. We need to further investigate transportation problems and access problems in general in other samples and regions of the United States to provide more evidence of this problem at the national level. We also need to explore different empirical models to understand the pattern of problems with transportation. For example, future research might need to look at the effects of neighborhood characteristics, such as services offered and location, and access to medical facilities.
Finally, these findings highlight the importance of reaching out to older Puerto Rican women who are at greater risk for depression, health problems, and disability, and who simultaneously experience more transportation problems to access medical care. Many of these women may have never learned to drive, and language limitations may limit their ability to navigate the public transportation system.
Massachusetts offers two different transportation services for seniors, the TP1 is offered free of charge to MassHealth (Massachusetts’s Medicaid program) recipients but it requires that a doctor approves that the service is needed. The other service called the “Ride”-which is an affordable transportation service for seniors within the Boston area—charges US $4 each way within the city limits. One limitation of this service is the need for scheduling ahead and the scarcity of Spanish-speaking drivers relative to the existing or potential clients for those services. Appropriate interventions are needed to educate aging Hispanics on how to comfortably use transportation services to access medical care and to ensure that these services remain not only affordable but also welcoming.
Limitations of the Study
There are some limitations to this study. First, the small sample of the non-Puerto Rican subgroups—particularly Dominicans—suggests that caution should be exercised when interpreting some of the results. Whereas this is one of the first studies to include a subset of Dominican respondents, it is important that these findings be validated in subsequent studies with larger samples. In this same vein, we used the more general access problems variable in the regression analysis, instead of focusing only on the transportation and language problems experienced by Puerto Ricans. The rationale for doing this was that problems in general might have an effect on symptoms of depression. However, this question deserves further examination with a larger sample of older Puerto Ricans. Second, the sample includes younger older adults aged 60 to 65 years. Part of the rationale for including this younger group was the lower life expectancy and younger age distribution of Puerto Ricans and other Hispanics in Massachusetts. However, there might be differences in health insurance coverage due to age, such as not yet being able to qualify for Medicare. Although health insurance coverage is not a major issue in this Massachusetts sample, future studies may need to look at differences in reported problems of access to medical care by age group and type of insurance coverage (Medicaid, Medicare, private health insurance, etc.). Finally, the authors caution that this study uses an urban population sample and that some of the findings may not be generalizable to the experiences of Hispanic elders in rural areas throughout Massachusetts or more generally in other areas of the Northeastern United States.
Acknowledgments
This study was supported by the National Institute of Aging grants R01 AG10425 and P01 AG023394, and by the Farnsworth Trust Fellowship in Aging Policy Research program (2006-2007). We appreciate the suggestions and comments received from the editor, anonymous reviewers, and Dr. Katherine Tucker.
Contributor Information
Marta B. Rodriguez-Galan, Transylvania University, Lexington, Kentucky.
Luis M. Falcón, Northeastern University, Boston, Massachusetts.
References
- Andersen R, Lewis SZ, Giachello AL, Aday LA, & Chiu G (1981). Access to Medical Care among the Hispanic Population of the Southwestern United States. Journal of Health and Social Behavior, 22, 78–89. [PubMed] [Google Scholar]
- Auchincloss AH, Van Nostrand JF, & Ronsaville D (2001). Access to health care for older persons in the United States: Personal, structural, and neighborhood characteristics. Journal of Aging and Health, 13, 329–354. [DOI] [PubMed] [Google Scholar]
- Baer W (1992). The Puerto Rican economy and the United States economic fluctuations. Rio Piedras: Social Science Research Center, University of Puerto Rico. [Google Scholar]
- Becerra R (1984). The Hispanic elderly: A research reference guide. University Press of America; Lanham, MD: University Press of America. [Google Scholar]
- Borrell L (2005). Racial identity among Hispanics: Implications for health and well-being. American Journal of Public Health, 95, 379–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burnette D, & Mui AC (1999). Physician utilization by Hispanic elderly persons. Medical Care, 37, 362–374. [DOI] [PubMed] [Google Scholar]
- Chung J (2006, August 28). Healthier than you might expect. Los Angeles Times, p. B1. [Google Scholar]
- Cuellar I, Bastida E, & Braccio SM (2004). Residency in the United States, subjective well-being, and depression in an older Mexican-origin sample. Journal of Aging and Health, 16, 447–466. [DOI] [PubMed] [Google Scholar]
- Derose KP, & Baker DW (2000). Limited English proficiency and Latinos’ use of physician services. Medical Care Research and Review, 57, 76–91. [DOI] [PubMed] [Google Scholar]
- Falcon LM, & Tucker KL (2000). Prevalence and correlates of depressive symptoms among Hispanic elders in Massachusetts. Journals of Gerontology Series B-Psychological Sciences and Social Sciences, 55, S108–S116. [DOI] [PubMed] [Google Scholar]
- Falcon LM, Tucker K, & Bermudez O (1997). Correlates of poverty and participation in food assistance programs among Hispanic elders in Massachusetts (Discussion Papers DP#1121–97). Madison: Institute for Research on Poverty, University of Wisconsin. [Google Scholar]
- Fitzpatrick AL, Powe NR, Cooper LS, Ives DG, & Robbins JA (2004). Barriers to health care access among the elderly and who perceives them. American Journal of Public Health, 94, 1788–1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franzini L, Ribble JC, & Keddie AM (2001). Understanding the Hispanic paradox. Ethnicity and Disease, 11, 496–518. [PubMed] [Google Scholar]
- Gonzalez HM, Haan MN, & Hinton L (2001). Acculturation and the prevalence of depression in older Mexican Americans: Baseline results of the Sacramento area Latino study on aging. Journal of the American Geriatrics Society, 49, 948–953. [DOI] [PubMed] [Google Scholar]
- Haas JS, Phillips KA, Sonneborn D, McCulloch CE, Baker LC, Kaplan CP, et al. (2004). Variation in access to health care for different racial/ethnic groups by the racial/ethnic composition of an individual’s county of residence. Medical Care, 42, 707–714. [DOI] [PubMed] [Google Scholar]
- Haviland MG, Pincus HA, & Morales LS (2003). Depression and satisfaction with health coverage and medical care in the 1998 NRC Healthcare Market Guide survey. Administration and Policy in Mental Health, 30, 511–522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hornberger JC, Gibson CD, Wood W, Dequeldre C, Corso I, Palla B, et al. (1996). Eliminating language barriers for non-English-speaking patients. Medical Care, 34, 845–856. [DOI] [PubMed] [Google Scholar]
- Kemp BJ, Staples F, & Lopez-Aqueres W (1987). Epidemiology of depression and dysphoria in an elderly Hispanic population. Prevalence and correlates. Journal of the American Geriatrics Society, 35, 920–926. [DOI] [PubMed] [Google Scholar]
- Kirby JB, Taliaferro G, & Zuvekas SH (2006). Explaining racial differences and ethnic disparities in health care. Medical Care, 44, I64–I72. [DOI] [PubMed] [Google Scholar]
- Krause N, & Goldenhar LM (1992). Acculturation and psychological distress in three groups of Hispanics. Journal of Gerontology: Social Sciences, 47, S279–S288.. [DOI] [PubMed] [Google Scholar]
- Levy PS, & Lemeshow S (1980). Sampling for health professionals. New York: Van Nostrand Reinhold. [Google Scholar]
- Lopez-Aqueres W, Kemp B, Plopper M, Staples FR, & Brummel-Smith K (1984). Health needs of the Hispanic elderly. Journal of the American Geriatrics Society, 32, 191–198. [DOI] [PubMed] [Google Scholar]
- Mahard O’Donnell R (1989). Functional disability among the Puerto Rican elderly. Journal of Aging and Health, 1, 244–264. [Google Scholar]
- Mahard RE (1988). The CES-D as a measure of depressive mood in the elderly Puerto Rican population. Journal of Gerontology, 43, P24–P25. [DOI] [PubMed] [Google Scholar]
- Markides KS, & Coreil J (1986). The health of Hispanics in the southwestern United States: An epidemiological paradox. Public Health Report, 101, 253–265. [PMC free article] [PubMed] [Google Scholar]
- Melendez E (1993). Latino poverty and the economic development in Massachusetts In Melendez E & Uriarte M. Latino poverty and economic development in Massachusetts (pp. 15–37). Boston: University of Massachusetts Press. [Google Scholar]
- Meyler D, Stimpson JP, & Peek MK (2006). Acculturation and self-esteem among older Mexican Americans. Aging & Mental Health, 10, 182–186. [DOI] [PubMed] [Google Scholar]
- Miller CL, Druss BG, Dombrowski EA, & Rosenheck RA (2003). Barriers to primary medical care among patients at a community mental health center. Psychiatric Services, 54, 1158–1160. [DOI] [PubMed] [Google Scholar]
- Morales LS, Cunningham WE, Brown JA, Liu HH, & Hays RD (1999). Are Latinos less satisfied with communication by health care providers? Journal of General Internal Medicine, 14, 409–417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCHS/CDC Public Affairs. (2000). Health outcomes among Hispanic subgroups: Data from the National Health Interview Survey, 1992–1995. Advance Data No. 310.15 (PHS; pp. 2000–1250). [PubMed] [Google Scholar]
- Ontiveros JA, Black SA, Jakobi PL, & Goodwin JS (1999). Ethnic variation in attitudes toward hypertension in adults ages 75 and older. Preventive Medicine, 29, 443–449. [DOI] [PubMed] [Google Scholar]
- Ponce NA, Hays RD, & Cunningham WE (2006). Linguistic disparities in health care access and health status among older adults. Journal of General Internal Medicine, 21, 786–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts RE, Kaplan GA, Shema SJ, & Strawbridge WJ (1997). Prevalence and correlates of depression in an aging cohort: The Alameda County Study. Journals of Gerontology Series B: Psychological Sciences and Social Sciences, 52, S252–S258. [DOI] [PubMed] [Google Scholar]
- Robison J, Curry L, Gruman C, Covington T, Gaztambide S, & Blank S (2003). Depression in later-life Puerto Rican primary care patients: The role of illness, stress, social integration, and religiosity. International Psychogeriatrics, 15, 239–251. [DOI] [PubMed] [Google Scholar]
- Robison J, Gruman C, Gaztambide S, & Blank K (2002). Screening for depression in middle-aged and older Puerto Rican primary care patients. Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 57, M308–M314. [DOI] [PubMed] [Google Scholar]
- Rogler LH, Cortes DE, & Malgady RG (1991). Acculturation and mental health status among Hispanics: Convergence and new directions for research. American Psychologist, 46, 585. [DOI] [PubMed] [Google Scholar]
- Solis JM, Marks G, Garcia M, & Shelton D (1990). Acculturation, access to care, and use of preventive services by Hispanics: Findings from HHANES 1982–84 (Hispanic Health and Nutrition Examination Survey). American Journal of Public Health, 80, pS11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taira DA (1999). Improving the health and health care of non-English-speaking patients. Journal of General Internal Medicine, 14, 322–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker K, Bermudez O, & Castaneda C (2000). Type 2 diabetes is prevalent and poorly controlled among Hispanic elder of Caribbean origin. American Journal of Public Health, 90, 1288–1293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vera M, Alegria M, Freeman D, Robles RR, Rios R, & Rios CF (1991). Depressive Symptoms among Puerto Ricans: Island Poor Compared with Residents of the New York City Area. American Journal of Epidemiology, 134, 502–510. [DOI] [PubMed] [Google Scholar]
- Weingartner K; Robison J, Fogel D, & Gruman C (2002). Depression and substance use in a middle aged and older Puerto Rican population. Journal of Cross-Cultural Gerontology, 17, 173–193. [DOI] [PubMed] [Google Scholar]


