Abstract
Objective
To systematically review, identify and report the screening tools used for early identification of developmental delay in low- and middle-income countries.
Design
Systematic review.
Data sources
Four bibliographic databases: Medline (1946 to 13 July 2020), Embase (1974 to 13 July 2020), Scopus (1823 to 11 July 2020) and PsycINFO (1987 to July week 1 2020).
Eligibility criteria
Peer-reviewed original articles published in English addressing validated culturally sensitive developmental screening tools among children aged <5 years were included in this review.
Data extraction and synthesis
One author (CK, medical librarian) developed the search strategy. Three authors conducted the database search (phase I: CK; phase II: IJ and MKI). Three authors (TF, IJ and MKI) independently screened the title and abstracts. TF, MKI and GK independently performed the full-text review of the screened articles. During each step of the study selection process, disagreements were resolved through discussion. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement was used to guide the systematic review. Data extraction and analysis were performed using MS Excel. Meta-analysis was not possible due to heterogeneity of the study findings.
Results
We identified 3349 articles, of which 18 studies from 10 countries, reporting 16 screening tools, were selected for qualitative synthesis. Six cultural contexts were explored. Twelve general, two motor and two speech-language tools were identified. Seven of them found to be parent-completed ones. Five screening tools (American Speech-Language and Hearing Association, Guide for Monitoring Child Development, Infant Neurological International Battery, New Delhi-Development Screening Questionnaire and Woodside Screening Technique) reported relatively higher sensitivity (82.5%–100%) and specificity (83%–98.93%).
Conclusions
Limited number of culturally sensitive developmental screening tools were validated for children aged <5 years in low- and middle-income countries. Revising existing screening tools in different ethnic and cultural settings and subsequent validation with normative value should be a research priority.
Keywords: developmental neurology & neurodisability, paediatric neurology, neonatal intensive & critical care, neurological injury, community child health, public health
Strengths and limitations of this study.
This review puts together extensive literature searches on original studies (both observational and experimental) conducted among under-5 children from low- and middle-income countries reporting standardisation, validity (in terms of sensitivity and specificity) of developmental screening tools in early diagnosis of developmental delay.
Meta-analysis was not possible due to the heterogeneity of the study setting and findings.
Critical evaluation of the available screening tools in terms of diagnostic accuracy was not possible to perform due to the unavailability of the necessary information.
Introduction
Developmental delay is a condition where children exhibit significant variation in achieving developmental milestones as expected for their actual or adjusted age.1–3 Complications at birth including premature birth; brain trauma and encephalitis; severe medical problems after birth; inborn metabolic errors; genetic or chromosomal abnormalities; inadequate stimulation; malnutrition; iron deficiency anaemia; chronic illness; adverse environmental, familiar and psychological states may lead to developmental delay.4–6 Although the condition itself may not be permanent, it can provide a foundation for recognising children who might have more severe and permanent health conditions, that is, developmental disabilities. Apart from developmental delay, developmental disability is considered as a severe, chronic disability originating at birth or during childhood, expected to continue indefinitely, and substantially restricts the individual’s functioning in several major life activities.2 7 Examples of developmental disabilities include autism spectrum disorder, behavioural disorders, cerebral palsy, Down syndrome, fetal alcohol syndrome, intellectual disability and so on. As a predictive of above-mentioned learning, movement and behavioural disorders, it is possible to identify developmental delay to a great extent during the preschool period (ie, before the age of 5 years) with the help of well-validated screening tools.8 9 There is a long-term financial impact on society in terms of healthcare, educational support and other special services related to developmental delay and/or disability. This is because the affected children require substantial resources and increased cost over their lifespan compared with those without such conditions.10 This further accentuates the significance of early identification to initiate appropriate interventions and/or rehabilitations with the intention of preventing further delays, stimulating emerging skills and creating a more encouraging and protective surroundings.5
In the last few decades, successful implementation of WHO’s key health services11 regarding ‘The Countdown to 2015 Initiatives’ resulted in the reduction of the neonatal mortality rate from 37 deaths per 1000 live births in 1990 to 19 per 1000 live births in 2016, worldwide with a projection of further future reductions.12 13 Among the survivors, >250 million under-5 children from low- and middle-income countries (LMICs) are not fulfilling their developmental potential in cognitive, motor and social-emotional domains due to poor nutrition, poverty and conflicts.4 14–16 In addition to them, there is an undetected number of surviving children suffering from various forms of developmental delay presumably due to brain injury during the fetal, perinatal and postneonatal period.17 We have discovered that, with time, while the neonatal mortality rate is reducing, the prevalence of developmental delay is gradually increasing (by analysing the data generated from two nation-wide population-based retrospective studies conducted in Taiwan) (see online supplemental figure S1).18 19
bmjopen-2020-038182supp001.pdf (281.9KB, pdf)
Monitoring, screening and surveillance have been found effective to track a child’s developmental progress. As a means of tracking a child’s developmental progress, developmental monitoring is the ordinary observation of child’s developmental advancement performed by parents/caregivers. On the contrary, developmental screening aims to identify specific developmental concern by doctors/healthcare professionals using brief questionnaire/checklist. When such activity is performed on a regular basis during routine health check-ups, it is termed as developmental surveillance.20 21 Among them, developmental screening is the first step of the comprehensive diagnostic procedure for secondary prevention and early identification of developmental delay.16 22 23 Thus, a well-validated developmental screening tool is very important. The standardised tools available from western countries provide well-validated assessment in their own settings. However, the transfer of such western-based tools to non-western countries is linked with substantial limitations in terms of score interpretation and feasibility of their use in resource-constrained settings such as in LMICs.24 In the high-income countries, early identification of developmental delay is considered as mandatory part of good healthcare practice, which is recommended by the American Academy of Paediatrics.16 In contrast, in LMICs, most teaching and training programmes of health professionals are still concentrated on acute illness and growth aspects of children rather than a developmental perspective, resulting in limited attention in developmental delay.16 Also, in these geographical areas, parents and caregivers with strong cultural beliefs and superstitions regarding health remain ignorant of the child’s developmental deficit and about the future impact of the condition.25 The combined effect of these two factors often results in overlooking or delaying of the diagnosis of developmental concerns.
The perspective on developmental disability varies from one culture to another. Along with economic, geographical, social factors, it often becomes a barrier to healthcare accessibility for children with disability.26 In Chinese culture, having children with disability is often considered shameful for the family. In Southeast Asian cultures, parents often face social deprivation due to the stigma related to developmental disability.27 Moreover, cultural believe often holds control over treatment approaches for developmental delay or disabilities, including: (1) whether to seek help or not; (2) which treatment option to choose; (3) parental expectations for their child; (4) interpersonal relationship between caregiver and healthcare professionals and so on.28 One of the biggest challenges in early identification of developmental delay or disability is providing culturally sensitive screening tools, which include cultural perception of delay and/or disability and easily adaptable across the various cultural/nation.24 Among the developmental domains, social development is culturally specific and difficult to adapt, whereas the gross motor domain is easier to adapt culturally.29
The purpose of this study was to look for the screening tools which have been used and validated for early identification of developmental delay in LMICs, to report how effective they are for early identification of developmental delay in terms of validity, and to identify areas for future research.
Materials and methods
Data sources and search strategy
To locate items on screening tools for early identification of developmental delay among children in LMICs, the search strategy was developed by an experienced medical librarian (CK). Literature search was conducted in two phases (phase I up to March 2018: CK; phase II up to July 2020: IJ and MKI) in four bibliographic databases. The databases searched were: OVID Medline (1946 to 13 July 2020), OVID Embase (1974 to 13 July 2020), Scopus (1823 to 11 July 2020) and PsycINFO (1987 to July week 1 2020). Search terms included database-specific thesaurus terms where available such as ‘Mass Screening’, ‘Diagnosis’, ‘Surveys and Questionnaires’, ‘Neurodevelopmental Disorders’, ‘Motor Disorders’, ‘Cerebral Palsy’, ‘Cognitive Dysfunction’ and ‘Communication Disorders’ as well as relevant associated text word terms. These were combined with LMIC terms and infant, child and adolescent terms. To minimise the introduction of bias, no publication date and language limits were used. The date of the latest search was 13 July 2020. The Medline search strategy could be found in online supplemental table S1.
In addition to bibliographic database searches, we manually checked the reference lists of recent systematic reviews30 31 as well as articles included in the full-text review. We also contacted experts in the relevant field to identify any additional studies or information.
Selection criteria
Study inclusion criteria were: (1) children aged <5 years who were at risk of developmental delay; (2) original studies (both observational and experimental); (3) study where single, as well as multiple developmental domains, were examined; (4) studies conducted only in LMICs. The exclusion criteria were: (1) studies conducted on diagnosed cases of developmental delay; (2) studies focusing on autism spectrum disorder and other behavioural disorders; (3) studies conducted among HIV exposed children; (4) studies on developmental delay among children aged >5 years; (5) interventional studies on developmental delay; (6) studies on developmental delay published before 1946; (7) article published in languages other than English; (8) conference papers, letter to the editor, protocols, systematic reviews and ongoing studies; (9) study conducted among children of eligible ethnic origin but in different country settings (ie, children adopted from LMICs but study conducted in high-income countries). List of key definitions regarding study selection are available in online supplemental table S2.
All the under-5 children who were not previously diagnosed with any neurodevelopmental delay or disability, were considered as ‘at risk of developmental delay’. Studies where overall or categorised (based on different age group/cut-off score) sensitivity-specificity of screening tools were examined and clearly reported, were considered as validated. We did not discriminate among screening, monitoring and surveillance tools. If any of those tools were validated for screening developmental delay among under-5 children, considered eligible for inclusion. Tools which were declared as assessment tools by the developer themselves as well as studies where a tool was used for developmental assessment by the researchers, were excluded from the review.
When we had searched the keywords ‘Autism Spectrum Disorder’ and ‘Developmental Delay’ in the medical databases, the number of search items were as follows: (i) OVID Medline-9320: 12402; (ii) OVID Embase-21750: 7506; (iii) Scopus-20675: 7530 and (iv) PsycINFO-17130: 3067, respectively, which is a bit alarming. We have excluded autism and other behavioural disorders from the study to provide undivided attention to developmental delay. Apart from scientific community, parents and caregivers of LMICs are more familiar with the term autism spectrum disorder compared with developmental delay. Which is evident from growing concerns regarding speech-language and behavioural domains of child development compared with rest of the domains.32 We believe, to ensure successful developmental screening/surveillance programme in LMICs in the long run, and more importantly, to raise public awareness about developmental delay, we need to work more in this area than we used to.
LMICs consist of countries belonging to three World Bank income groups (low, lower-middle and upper-middle) of WHO’s Member States. The classification is based on the estimated per capita gross national income. We have used the World Bank’s country classifications by income level (2020–2021) in this review.33 34
Study selection, data extraction and quality appraisal
We carried out the following steps to decide on the studies: (1) searching the above-mentioned databases using similar search strategy (CK, IJ, MKI); (2) deduplicating and merging search results using the EndNote bibliographic software (TF); (3) examining titles and abstracts to remove obviously irrelevant reports (TF, IJ, MKI); (4) retrieving and examining the full-text reports of eligible studies (TF, MKI, GK); (5) applying the selection criteria on the shortlisted articles (TF, GK); (6) making final decisions on study inclusion and proceeding for data collection. Extracted information included: publication year, the country where the study was conducted, the name of the screening tool, the gold standard tool(s) against which the screening tool was validated, study design, study setting, sample size, sampling technique, the age of the participants, selection criteria and sensitivity-specificity of the screening tools. During each step of the study selection process, disagreements were resolved through discussion. We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement, including 27-item PRISMA checklist to guide the systematic review.35 The quality of the selected studies was assessed using the Quality Assessment Tool for Diagnostic Accuracy Studies-236 (see online supplemental table S3) and Newcastle-Ottawa Scale for cross-sectional studies37 (see online supplemental table S4).
Data analysis
Individual study findings were reported including the country, study design, study setting, sample size, sampling technique, proportions and age range of participants, sensitivity-specificity of the developmental screening tools, etc. Data extraction and analysis were performed using MS Excel. We were unable to perform a meta-analysis due to the heterogeneity of the study setting and findings.
Protocol registration
The protocol of this systematic review has been registered in PROSPERO (registration number: CRD42018095232).
Patient and public involvement
Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Results
Search results
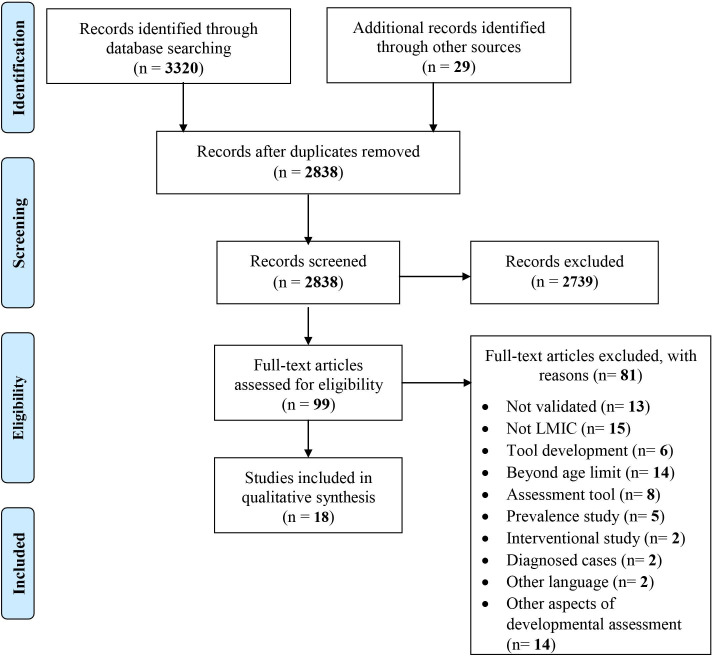
The initial search retrieved 3349 records. We have found 3320 records from four bibliographic databases (1555 from OVID Medline, 1317 from OVID Embase, 348 from Scopus and 100 from PsycINFO). Twenty-nine records were located by reviewing the reference lists of recent systematic reviews, fully extracted articles and consulting expert researchers in this area. There were 2838 records once duplicates were removed. Following the screening of title and abstracts for articles, which described the validation of tools to screen developmental delay among children, 99 articles were selected for further evaluation. After further review and application of selection criteria, 18 articles were selected for inclusion in study.38–55 A PRISMA flow diagram has been prepared to illustrate the study selection process (as shown in figure 1).
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram. LMIC, low- and middle-income countries.
Summary of the included studies
All of the 18 studies included for qualitative synthesis were original articles published in English, with a publication date range from 1991 to 2020 inclusive. Eight studies originated in ‘South Asia’,38 41 44 46 48 51 54 55 four from ‘East Asia and Pacific’,39 47 49 50 three from ‘sub-Saharan Africa’,45 52 53 one study each from the ‘Middle East and North Africa’,43 ‘Latin America and Caribbean’40 and ‘Europe and Central Asia’42 region of the World Bank. In total, 16 developmental screening tools were used in 10 countries. Among the 16 screening tools, American Speech-Language and Hearing Association (ASHA), Language Evaluation Scale Trivandrum for 0–3 years LEST (LEST 0–3) focus on language domain; Infant Neurological International Battery (INFANIB) and Little Developmental Coordination Disorder Questionnaire (Little DCDQ) work on motor domains. The remaining tools are for general developmental screening. A brief description of the selected screening tools has been provided in table 1.
Table 1.
Brief description of the selected screening tools
| Screening tool | Country of origin | Study country | Concerned age | Parent-reported version | Questionnaire type | Number of questionnaires | Number of items | Developmental domain | Validated against |
| General screening tools | |||||||||
| Ages and Stages Questionnaire (ASQ) | USA | India, China | 1–66 months | Yes | Q & A | 21 age sets | 30 items per set | Communication, gross motor, fine motor, problem solving, personal-social | Developmental Assessment Scales for Indian Infants (DASII)38 |
| Bayley Scales of Infant Development (BSID-III)39 | |||||||||
| Development Screening Questionnaire DSQ) | Bangladesh | Bangladesh | 0-24 months | No | Q & A | 24 age sets | 8 questions per set | Gross motor, fine motor, vision, hearing, cognition, socialisation, behaviour and speech | Rapid Neurodevelopmental Assessment (RNDA)41 |
| Guide for Monitoring Child Development (GMCD) | Turkey | Turkey | 0–3.5 years | Yes | Q & A | Single | 7 items | Expressive language and communication, receptive language, fine and gross motor, social-emotional, self-help | Bayley Scales of Infant Development (BSID-II)42 |
| Lucknow Developmental Screen (LDS) | India | India | 0-24 months | Yes | Chart | Single | 27 item | Motor, mental, language, social | Developmental Assessment Scales for Indian Infants (DASII)46 |
| Vineland Social Maturity Scale46 | |||||||||
| Mongolian Rapid Baby Scale (MORBAS) | Mongolia | Mongolia | 0–42 months | No | Written | Single | 161 item | Cognitive, receptive communication, expressive communication, fine motor, gross motor, social-emotional, adaptive behaviour | Bayley Scales of Infant and Toddler Development (BSID-III)47 |
| New Delhi-Development Screening Questionnaire (ND-DSQ) | India | India | 9–18 months | Yes | Q & A | 2 age sets | 20 items | General screening tool (domains not explicitly mentioned) | Developmental Assessment Scales for Indian Infants (DASII)48 |
| Parent Evaluation of Developmental Status (PEDS) | USA | Thailand | 0-8 years | Yes | Q & A | Single | 10 items | Global/cognitive, speech/expressive language, receptive language, behaviour, social-emotional, school, self-help, fine motor, gross motor, other | Parent Evaluation of Developmental Status: Developmental Milestones, Assessment Level49 |
| Mullen Scales of Early Learning50 | |||||||||
| Rapid Prescreening Denver Questionnaire (R-PDQ) | USA | India | 0–6 years | No | Q & A | 4 age sets | 25 items | Gross motor, fine motor activity, personal-social, language | Denver Developmental Screening Test (DDST)51 |
| Road to Health Booklet Developmental Checklist (RTHB-DC) | South Africa | South Africa | 14 weeks to 6 years | No | Checklist | Single | 21 items | Gross motor, fine motor, communication, vision, hearing | Parent Evaluation of Developmental Status (PEDS)52 |
| Parent Evaluation of Developmental Status: Developmental Milestones52 | |||||||||
| Ten Questions Screening Instrument (TQSI) | Multiple | Benin | 2–9 years | Yes | Q & A | Single | 10 items | Vision, hearing, seizure, cognition, motor | Mullen Scales of Early Learning53 |
| Trivandrum Developmental Screening Chart (TDSC) | India | India | 0–2 years | No | Chart | Single | 17 items | Mental, motor, vision, hearing | Denver Developmental Screening Test (DDST)54 |
| Woodside System Screening Technique (WSST) | Scotland | India | 0–4 years | No | Chart | Single | 70 items | Social, hearing and language, vision and fine motor, gross motor | Gesell’s Developmental Schedules (GDS)55 |
| Language screening tools | |||||||||
| American Speech-Language and Hearing Association (ASHA) | USA | Brazil | 0–5 years | No | Q & A | 7 age sets | 6–13 items | Language reception and expression | Child Language Test in Phonology, Vocabulary, Fluency and Pragmatics (ABFW*)40 |
| Language Evaluation Scale Trivandrum for 0–3 years (LEST 0-3) | India | India | 0–3 years | No | Chart | Single | 33 items | Speech and language | Receptive Expressive Emergent Language Scale (REELS)44 |
| Motor screening tools | |||||||||
| Infant Neurological International Battery (INFANIB) | USA | Iran | 0–18 months | No | Not found | Single | 20 items | Gross motor | Developmental Assessment by Paediatric Neurologist43 |
| Little Developmental Coordination Disorder Questionnaire (Little DCDQ) | Israel | South Africa | 3–5 years | Yes | Q & A | Single | 15 items | Gross motor, fine motor | Movement Assessment Battery for Children-2 (MABC-2)45 |
*ABFW: Child Language Test in Phonology, Vocabulary, Fluency and Pragmatics. Originally known as “Teste de Linguagem Infantil nas Áreas de Fonologia, Vocabulário, Fluência e Pragmática” (Portuguese Brazilian)
Participant characteristics
All the studies involved males and females; age ranged between 0 and 5 years. The smallest sample size was 53 and the largest was 1945. The studies explored the following cultural contexts: East Asia and Pacific (China, Mongolia and Thailand), Europe and Central Asia (Turkey), Latin America and the Caribbean (Brazil), Middle East and North Africa (Iran), South Asia (Bangladesh, India), sub-Saharan Africa (Benin, South Africa). Selection criteria used for participation in those studies are stated in online supplemental table S5.
Study characteristics
All the included studies were cross-sectional in nature. Among the 18 studies, one study was conducted in the community and tertiary hospital simultaneously,54 8 were conducted in the tertiary hospital,38 42 43 46–50 5 were conducted in the community39 40 44 51 55 and 1 study each was conducted in a nursery school setting45 and primary healthcare clinic setting.52 In the remaining two studies, screening was done in the community followed by a hospital-based detailed assessment in one41 and primary healthcare clinic-based assessment in another.53
Validated screening tools
The Ages and Stages Questionnaire
This is a parent-completed questionnaire that could be used as a general developmental screening tool. The Ages and Stages Questionnaire (ASQ) was designed and developed by J. Squires and D. Bricker, at the University of Oregon and can be completed in 12–18 min.56 The questionnaire has 30 items focusing on five domains of child development, named gross motor, fine motor, problem-solving, communication and personal-social. Obtaining lower scores than the cut-off in any domain is considered as ‘screen positive’. The latest version of ASQ, ASQ-III, has 21 sets of questionnaires, appropriate for children aged 1–66 months.57 In the study by Juneja et al, a Hindi adaptation of an older version of ASQ, (ASQ-II, which had 19 sets of questionnaires for 4–60 months aged children) was used in a convenience sample of 200 children divided into four age groups: 4, 10, 18 and 24 months, in a tertiary hospital setting.38 Each age group consisted of 30 low-risk and 20 high-risk children. High-risk status was determined by the presence of any of the following risk factors: prematurity, low birth weight, history of neonatal hospitalisation, history of central nervous system infection, history of afebrile seizure, diagnosed cases of developmental disorder and chromosomal abnormalities. Children without these risk factors were treated as being in the low-risk group. Eventually, 4, 10, 18 and 24 months questionnaires of ASQ-II were validated against ‘Developmental Assessment Scales for Indian Infants (DASII)’, considered as a gold standard for developmental assessment tool among Indian children.38 The overall sensitivity and specificity of ASQ-II for Indian children were found to be 83.3% and 75.4%, respectively.
In the study by Yue et al, Chinese adaptation of ASQ-3 was used among 1831 children aged 5–24 months in a cluster random sample from rural China. Eventually, the tool was validated against the Bayley Scales of Infant and Toddler Development-III. Overall sensitivity and specificity of ASQ-III found to be 76.52% and 40.97%, respectively. The authors suggested to avoid using ASQ-III for children lower than 13 months of age as well as children whose primary caregiver are not their mother, due to poor performance in those group of children.39
American Speech-Language and Hearing Association Screening Tool
The ASHA was designed and developed to screen out under-5 children for language delay in receptive and expressive language domain. There are seven age sets consisting of 6–13 questions per age set. Cut-off score for screen positive result varies from one age set to another. In general, if a child gets more than two negative answers in any domain will be considered as ‘screen positive’. In the study conducted by Dias et al, 1000 under-5 children were screened for language delay during a polio vaccination campaign in São Paulo, Brazil by using the tool. Later detailed assessment was conducted using the Child Language Test in Phonology, Vocabulary, Fluency and Pragmatics (ABFW). ASHA found to have excellent sensitivity and specificity (82.5% and 98.93%, respectively) against ABFW Child Language Test.40 The authors recommended to adapt the instrument for bilingual children as well as validating it in larger sample size.
Development Screening Questionnaire
The Development Screening Questionnaire (DSQ) was designed and developed in Bangladesh, to be administered to mothers of children from birth to 24 months of age to screen their child’s neurodevelopmental status. The DSQ has 24 age sets with 8 questions per set related to eight functional domains, named: gross motor, fine motor, vision. hearing, cognition, socialisation, behaviour and speech.41 Any child found to be positive on one or more functional domain is considered ‘screen positive’. In a study conducted in urban Bangladesh, a random sample of 197 children aged 0–24 months was screened in the community with DSQ, and then a detailed developmental assessment was done in a tertiary hospital with the help of the ‘Rapid Neurodevelopmental Assessment’ tool as the gold standard. Overall sensitivity and specificity of DSQ for Bangladeshi children under 2 years was found to be 47.1% and 97.2%, respectively.41 Despite moderate sensitivity, the DSQ might be advantageous for resource-poor settings due to its high specificity.
Guide for Monitoring Child Development
The Guide for Monitoring Child Development (GMCD) was designed and developed in Turkey to monitor development of children aged 0–3.5 years in LMICs. The tool consists of 7 open-ended questions focusing on the following domains: expressive language and communication, receptive language, fine and gross motor, social-emotional, self-help. Children declared screened positive if they failed to demonstrate one or more age-appropriate milestones. In a study conducted by Ertem et al, GMCD was validated against Bayley Scales of Infant Development (BSID-II) in a random sample 79 Turkish children of 1–24 months of age. The overall sensitivity and specificity of GMCD were found to be 88% and 93%, respectively.42
Infant Neurological International Battery
The INFANIB was established by Ellison and Browning in 1985 to assess the gross motor function of children aged 0–18 months. The tool contains 20 items focusing on spasticity, vestibular function, head and trunk, French angles and legs.58 In the study by Soleimani and Dadkhah, a consecutive sample of 6150 children were screened using INFANIB and classified as normal, transiently abnormal and abnormal. To validate the tool, a random sample of 153 children from the above-mentioned groups were assessed by paediatric neurologists. It was found that overall sensitivity and specificity of INFANIB for Iranian children were 90% and 83%, respectively.43
Language Evaluation Scale Trivandrum
Designed and developed at the Child Development Centre of the Trivandrum Government Medical College, India, Language Evaluation Scale Trivandrum (LEST 0–3) is a 33 items screening tool to screen out language delay among children aged 0–3 years.44 The LEST 0–3 was validated against the ‘Receptive-Expressive Emergent Language Scale’ tool as a gold standard in a community sample of 643 Indian children aged 0–36 months. To decide on the best possible combination, researchers considered both ‘one item delay’ and ‘two items delay’ as screen positive. When one item delay considered as screen positive, sensitivity and specificity of LEST 0–3 found to be 95.8% and 77.5%, respectively. Similarly, when two items delay measured as screen positive, the sensitivity and specificity obtained as 66.7% and 94.8%, respectively.44 It should be noted that the original version of Receptive-Expressive Emergent Language Scale (1971) was used in this study for validation due to the lack of age-appropriate language assessment tool for language delay.
Little Developmental Coordination Disorder Questionnaire
The Little Developmental Coordination Disorder Questionnaire (Little DCDQ) was developed by Rithman et al in Israel to assess gross motor and fine motor function of children between 3 and 5 years of age. It is a parent-reported questionnaire with 15 items under three main components, control during execution, fine motor execution and overall coordination.45 The Little DCDQ was validated against the Movement Assessment Battery for Children-2 as a gold standard in a group of 53 South African preschoolers between 3 and 5 years of age, with Afrikaans, Tswana or English-speaking parents.45 With 57.14% sensitivity and 81.25% specificity, Little DCDQ had the potential to be used in South African culture, however, some adjustments would be required.
Lucknow Development Screen
The Lucknow Development Screen (LDS) was developed in CSM Medical University, Lucknow, India, using selected milestones from Baroda Development Screening Test. It is a 27 items chart format tool, covering four domains namely motor, mental, language and social. Suitable for children aged 0–24 months. The LDS is said to be easily administrable by interviewing parents or caregiver.46 In a study conducted in India, the LDS tool was validated against the DASII and the Vineland Social Maturity Scale. They administered the tool to mothers of a sample of 142 children, aged between 6 and 24 months, attending Paediatric Outpatients or Neurology Clinic of CSM Medical University, Lucknow, India. The screening tool was translated into Hindi for easy understanding and administration. For three children among the sample size of 142, Vineland Social Maturity scale was used as a gold standard, as DASII could not be applied to them. It is claimed that the LDS has a great potential to be used as a community screening tool among Indian children, with an overall sensitivity of 95.9% and specificity 73.1%.46
Mongolian Rapid Baby Scale
The Mongolian Rapid Baby Scale (MORBAS) is a written developmental screening test, designed and developed in Mongolia. It has 161 items arranged under seven developmental domains, namely gross motor, fine motor, cognitive, expressive language, receptive language, social-emotional and adaptive behaviour. The tool is suitable for children aged 0–42 months.47 In a study conducted in Mongolia, MORBAS was administered in a convenience sample of 150 Mongolian children aged 0–42 months and thus validated against the Bayley Scales of Infant and Toddler Development-III (BSID-III). With sensitivity 81.8% and specificity 52.3%,47 MORBAS could be useful in the long run to screen out children for early intervention and rehabilitation.
New Delhi-Development Screening Questionnaire
The New Delhi-Development Screening Questionnaire (ND-DSQ) was developed by Jain et al, at Chacha Nehru Bal Chikitsalaya, a tertiary hospital of northern India. ND-DSQ has 20 items, two age sets (9 and 18 months) and applicable for children aged 9–18 months.48 The items mentioned were milestone specific. Thus, no explicit mention of the developmental domains was found. In the study by Jain et al, ND-DSQ was validated against DASII in a convenience sample of 200 children aged 9 and 18 months (with 100 children per age group). It was established that the 9-month questionnaire was 100% sensitive and 87.2% specific for Indian children. Correspondingly, the 18 months questionnaire was validated with 91.4% sensitivity and 88.7% specificity.48 As a newly developed tool, the ND-DSQ is promising to be useful for Indian and similar cultural settings.
Parent Evaluation of Developmental Status
This tool was developed in 1997 by F. P. Glascoe at Tennessee, USA.59 It is the only screening tool available to date that addresses parent’s concern about children’s development in the following domains: gross motor, fine motor, cognitive, expressive language, receptive language, behaviour, social-emotional, self-help, school and other.60 It has ten open-ended questions under 10 areas of parental concerns, applicable for children aged 0–8 years. The other category allows parents to express concerns not already addressed under previous categories. This unique property makes Parent Evaluation of Developmental Status (PEDS) unique as a developmental screening tool. In PEDS, parental concerns are labelled as ‘predictive’ (significant) and ‘non-predictive’ (non-significant). Thus, children are screened as low-risk, moderate-risk and high-risk group if they have no or non-predictive concerns, one predictive concern and two predictive concerns, respectively.49
In the study by Chunusuwan et al, the PEDS-Thai was validated against the ‘Parent Evaluation of Developmental Status: Developmental Milestones, Assessment Level’ in a tertiary hospital. A convenience sample of 266 children of 9, 18 and 30 months of age was selected. Screen positive children were assembled as ‘high-risk’ (≥2 significant concerns) and ‘moderate-risk or high-risk’ (≥1 significant concern) group. Sensitivity and specificity of PEDS against Parent Evaluation of Developmental Status: Developmental Milestones, Assessment Level for the high-risk group was established as 27.7% and 93.0%, respectively. For moderate-risk or high-risk group, the tool was 67.7% sensitive and 60.7% specific.49 In order to avoid unnecessary/over-referral, the authors suggested to practice second stage evaluation (using Parent Evaluation of Developmental Status: Developmental Milestones, ASQ, Denver-II etc.) alongside/after PEDS screening.
In another study by Wantanakorn et al, they validated the PEDS-Thai against the Mullen Scales of Early Learning tool as a gold standard in a convenience sample of 137 children aged 18–36 months in another tertiary hospital. It was found that the PEDS-Thai is a promising tool for Thai cultural backgrounds with overall sensitivity of 92.8% and specificity 49.2%.50 According to the authors, ‘the relatively low specificity of PEDS seen here may be because of the excessive concern of parents regarding their child’s development, especially who are in relatively high socioeconomic status’. The selection bias of participants was mentioned as the major limitation of the study. Thus, they advised further evaluation of the diagnostic performances of the tool using a representative sample of the population.
Rapid Prescreening Denver Questionnaire
The Rapid Prescreening Denver Questionnaire (R-PDQ) is a general developmental screening tool covering four developmental domains: gross motor, fine motor activity, personal-social and language.51 It has four age sets applicable for children aged 0–6 years: 0–9 months, 9–24 months, 2–4 years and 4–6 years. Each questionnaire contained 25 items. To score a child, the responding person had to keep answering the questions until there were three negative responses under a specific domain. In the study by Awasthi et al, the 2–4 years questionnaire of R-PDQ was validated against the Denver Developmental Screening Test. The study participants were randomly selected 126 children living in urban slums of Lucknow, India. To validate the tool, when a delay in more than one domain was considered as the cut-off, the tool was revealed to be 100% sensitive and 7.8% specific. Similarly, when a delay in more than two domains was considered as the cut-off, the sensitivity and specificity were found to be 18.2% and 42.6%, respectively.51 Inconvenient validity and high referral rate compared with US children were explained by the presence of various ‘difficult to interpret’ questions and Denver Developmental Screening Test being an unsuitable gold standard for R-PDQ.
Road to Health Booklet Developmental Checklist
The Road to Health Booklet Developmental Checklist (RTHB-DC) was prepared as an integrated part of The Road to Health Booklet, the revised version of which was introduced in October 2010. RTHB-DC is the only developmental surveillance and screening tool, currently implemented nationally in South Africa. The tool consists of 21 questions covering gross motor, fine motor, communication, vision and hearing domains. The checklist is applicable for children aged 14 weeks to 6 years.61 In the study by van der Linde et al, RTHB-DC was validated against PEDS and Parent Evaluation of Developmental Status: Developmental Milestones tools. The sample size was 201, consisting of children aged 6–12 months. In a primary healthcare clinic setting in South Africa, the sensitivity of the tool was found to be very low, that is, 25% compared with reasonably high specificity of 91%.52 Further development of the tool has been suggested by the authors incorporating consistent age gaps and inclusion of all developmental domains.
Ten Questions Screening Instrument
The Ten Questions Screening Instrument (TQSI) was developed in 1984 as part of a pilot study conducted by the University of Columbia, USA, for use in resource-poor countries.62 63 TQSI is a parent-reported tool comprising 10 questions addressing motor, cognitive, vision, hearing and seizure status. A child is considered screen positive if any of the questions are found to be positive. The tool is appropriate for children aged 2–9 years. In a study by Koura et al, the TQSI was validated against the Mullen Scales of Early Learning in a sample of 357 children aged 12 months.53 The participants were the offspring of the mothers who were enrolled in the ‘Malaria in Pregnancy Preventive Alternative Drugs’ trial. To adjust the tool for that age group, researchers had excluded the language domain which is applicable for children above 2 years. In that study, screening was done in the community followed by a detailed assessment done in the health centre. It was found that the overall tool had reasonably high sensitivity (81%) but poor specificity (31%) for children of Benin. This is compared with the 76.5% sensitivity and 75.7% specificity where only the motor domain was considered.53 Mullen Scales of Early Learning was used due to lack of a gold standard assessment tool for the Beninese population. The result suggests that the TQSI tool might be useful for resource-poor settings to screen out moderate to severe delay in motor function.
Trivandrum Developmental Screening Chart
The Trivandrum Developmental Screening Chart (TDSC) was designed and developed by Nair et al in 1991 in Child Development Center, Kerala, India. The chart contains 17 items under four developmental domains—mental, motor, vision and hearing; applicable for children under 2 years od age.54 If a child fails to achieve any item appropriate for his chronological age, considered as screened positive. In a study conducted by Nair et al, TDSC was validated against Denver Developmental Screening Test (DDST) simultaneously in community as well as hospital settings in a cluster random sample of 1945 Indian children aged <2 years. Overall sensitivity and specificity of TDSC found to be 66.7% and 78.8%, respectively.54 The authors recommended to use the chart for mass screening of developmental delay among under-2 children in resource-poor settings.
Woodside Screening Technique
The Woodside Screening Technique (WSST) was designed and developed in Glasgow, Scotland in the year 1976. The tool consists of 70 items covering social, hearing and language, vision and fine motor and gross motor domains, suitable for children under 4 years of age.55 In a study conducted by Gupta and Patel, WSST was validated against Gesell’s Developmental Schedules (GDS) in a random sample of 619 children aged 6 weeks–2 years from Jabalpur, India. Overall sensitivity and specificity of WSST found to be 83% and 88%, respectively.55
The major findings of this systematic review are presented in table 2. We have classified the eligible tools into two broad categories—‘Parents/Caregiver Reported Tools’ and ‘Direct Child Testing/Observation Tools’. The tools/studies which were not included in this review as they did not meet the selection criteria, are enlisted along with the reasons for rejection in online supplemental table S6.
Table 2.
Major findings from the selected studies used in this review
| Ref. | Country | Screening tool | Gold standard | Study | Participants | Key findings | |
| Parents/Caregiver reported tools | |||||||
| General screening tools | |||||||
| 38 | India | Ages and Stages Questionnaire II (ASQ-II) | Developmental Assessment Scales for Indian Infants (DASII) | Design: cross-sectional | Sample: 200 | Overall | Sensitivity 83.3% |
| Lower-middle income | Setting: hospital | Age: 4, 10, 18 and 24 months | Specificity 75.4% | ||||
| Convenience sample | |||||||
| 39 | China | Ages and Stages Questionnaire III (ASQ-III) | Bayley Scales of Infant Development (BSID-III) | Design: cross-sectional | Sample: 1831 | Overall | Sensitivity 76.52% |
| Upper-middle income | Setting: community | Age: 5–24 months | Specificity 40.97% | ||||
| Cluster random sample | |||||||
| 42 | Turkey | Guide for Monitoring Child Development (GMCD) | Bayley Scales of Infant Development (BSID-II) | Design: cross-sectional | Sample: 79 | Overall | Sensitivity 88% |
| Upper-Middle income | Setting: hospital | Age: 1–24 months | Specificity 93% | ||||
| Random sample | |||||||
| 46 | India | Lucknow Development ScreenDevelopmental Assessment Scales for Indian Infants (DASII) | Developmental Assessment Scales for Indian Infants (DASII) | Design: cross-sectional | Sample: 142 | Overall | Sensitivity 95.9% |
| Lower-Middle income | Setting: hospital | Age: 6–24 months | Specificity 73.1% | ||||
| Vineland Social Maturity Scale | Convenience sample | ||||||
| 48 | India | New Delhi-Development Screening Questionnaire (ND-DSQ) | Developmental Assessment Scales for Indian Infants (DASII) | Design: cross-sectional | Sample: 200 | 9 months | Sensitivity 100% |
| Lower-Middle income | Setting: hospital | Age: 9 and 18 months | Specificity 87.2% | ||||
| Convenience sample | 18 months | Sensitivity 91.4% | |||||
| Specificity 88.7% | |||||||
| 49 | Thailand | Parent Evaluation of Developmental Status (PEDS) | Parent Evaluation of Developmental Status: Developmental Milestones, Assessment Level | Design: cross-sectional | Sample: 266 | ≥1 significant concern | Sensitivity 67.7% |
| Upper-Middle income | Setting: hospital | Age: 9, 18 and 30 months | Specificity 60.7% | ||||
| Convenience sample | ≥2 significant concerns | Sensitivity 27.7% | |||||
| Specificity 93.0% | |||||||
| 50 | Thailand | Parent Evaluation of Developmental Status (PEDS- Thai) | Mullen Scales of Early Learning | Design: cross-sectional | Sample: 137 | Overall | Sensitivity 92.8% |
| Upper-Middle income | Setting: hospital | Age: 18–30 months | Specificity 49.2% | ||||
| Convenience sample | |||||||
| 53 | Benin | Ten Questions Screening Instrument (TQSI) | Mullen Scales of Early Learning | Design: cross-sectional | Sample: 357 | Motor | Sensitivity 76.5% |
| Lower-Middle income | Setting | Age: 12 months | Specificity 75.7% | ||||
| Screening: household | Random sample | ||||||
| Assessment: health centre | Overall | Sensitivity 81% | |||||
| Specificity 31% | |||||||
| Motor screening tools | |||||||
| 45 | South Africa | Little Developmental Coordination Disorder Questionnaire (Litttle DCDQ) | Movement Assessment Battery for Children-2 (MABC-2) | Design: cross-sectional | Sample: 53 | Overall | Sensitivity 57.14% |
| Upper-Middle income | Setting: nursery schools | Age: 3–5 years | Specificity 81.25% | ||||
| Convenience sample | |||||||
| Direct child testing/observation tools | |||||||
| General screening tools | |||||||
| 41 | Bangladesh | Development Screening Questionnaire (DSQ) | Rapid Neurodevelopmental Assessment (RNDA) | Design: cross-sectional | Sample: 197 | Overall | Sensitivity 47.1% |
| Lower-Middle income | Setting: screening- household | Age: 0–2 years | Specificity 97.2% | ||||
| Assessment: hospital | Random sample | ||||||
| 47 | Mongolia | Mongolian Rapid Baby Scale (MORBAS) | Bayley Scales of Infant and Toddler Development-III (BSID-III) | Design: cross-sectional | Sample: 150 | Overall | Sensitivity 81.8% |
| Lower-Middle income | Setting: hospital | Age: 0 month 16 days–42 months 15 days | Specificity 52.3% | ||||
| Convenience sample | |||||||
| 51 | India | Revised Prescreening Denver Questionnaire (R-PDQ) | Denver Developmental Screening Test (DDST) | Design: cross-sectional | Sample: 126 | Delay in ≥1 domain | Sensitivity 100% |
| Lower-Middle income | Setting: community | Age: 2–4 years | Specificity 7.8% | ||||
| Cluster random sample | Delay in ≥2 domains | Sensitivity 18.2% | |||||
| Specificity 42.6% | |||||||
| 52 | South Africa | Road to Health Booklet Developmental Checklist (RTHB-DC) | Parent Evaluation of Developmental Status (PEDS) | Design: comparative cross-sectional within-subject | Sample: 201 | Overall | Sensitivity 25% |
| Upper-Middle income | Setting: Primary Health Centre clinics | Age: 6–12 months | Specificity 91% | ||||
| Parent Evaluation of Developmental Status: Developmental Milestones | Convenience sample | ||||||
| 54 | India | Trivandrum Developmental Screening Chart (TDSC) | Denver Developmental Screening Test (DDST) | Design: cross-sectional | Sample: 1945 | Overall | Sensitivity 66.7% |
| Lower-Middle income | Setting: hospital+community | Age: 0–2 years | Specificity 78.8% | ||||
| Cluster random sample | |||||||
| 55 | India | Woodside Screening Technique (WSST) | Gesell’s Developmental Schedules (GDS) | Design: cross-sectional | Sample: 619 | Overall | Sensitivity 83% |
| Lower-Middle income | Setting: community | Age: 6 weeks–2 years | Specificity 88% | ||||
| Random sample | |||||||
| Language screening tools | |||||||
| 40 | Brazil | American Speech-Language and Hearing Association (ASHA) | Child Language Test in Phonology, Vocabulary, Fluency and Pragmatics (ABFW) | Design: cross-sectional | Sample: 1000 | Overall | Sensitivity 82.5% |
| Upper-Middle income | Setting: community | Age: 0–5 years | Specificity 98.93% | ||||
| Random sample | |||||||
| 44 | India | Language Evaluation Scale Trivandrum for 0–3 years (LEST 0-3) | Receptive Expressive Emergent Language Scale (REELS) | Design: cross-sectional | Sample: 643 | One item delay | Sensitivity 95.8% |
| Lower-Middle income | Setting: community | Age: 0–3 years | Specificity 77.5% | ||||
| Cluster random sample | Two item delay | Sensitivity 66.7% | |||||
| Specificity 94.8% | |||||||
| Motor screening tools | |||||||
| 43 | Iran | Infant Neurological International Battery (INFANIB) | Developmental Assessment by Paediatric Neurologist | Design: cross-sectional | Sample: 153 | Overall | Sensitivity 90% |
| Upper-Middle income | Setting: hospital | Age: 4–18 months | Specificity 83% | ||||
| Random sample | |||||||
Discussion
To the best of our knowledge, this is the first systematic review which attempts to find the available screening tools for early identification of children with developmental delay in LMICs. Although some systematic reviews were found who considered developmental assessment tools requiring professional experts with a special office setup,64 screening neurodevelopmental disability irrespective of age limit and diagnosis (eg, developmental delay, global developmental delay, cerebral palsy, autism spectrum disorder, attention deficit hyperactivity disorder, epilepsy and so on),65 or reflected high-income country context.8 We have also observed a study in which both screening and assessment tools have been systematically rated for accuracy and feasibility to use in LMICs,30 where information was significantly dependent on World Bank’s toolkit and inventory on early child development tools,66 rather than being obtained from systematic search through databases. In contrast, the purpose of this review was to systematically look for the available studies where screening tools were used exclusively for early identification (limited to children under 5 years of age) of developmental delay in the LMICs region where all types of study settings (ie, from household to health facilities) were addressed in order to go for early intervention and rehabilitation of the screened cases. Therefore, the unique contribution of this review is to be able to report those screening tools exclusively designed for screening of developmental delay at the earliest possible time in both single and multiple domains.
Research gaps and future directions
Several research gaps have been identified in the reported studies. Primarily, there was a lack of standard terminologies to indicate the developmental domains. The examples of synonymous domain names are as follows: (i) cognitive: cognition, cognitive, global, mental, problem solving and so on38 39 41 46 47 49 50 53 54; (ii) language: communication, expressive communication, expressive language, language, receptive communication, receptive language, speech, speech and language and so on38–42 44 46 47 49–51; (iii) psychosocial: adaptive behaviour, behaviour, personal-social, self-help, social, social-emotional, socialisation and so on.38 39 41 42 46 47 49–51 55 Apart from those, few researchers incorporated unconventional developmental domains in their tools, such as: hearing, school, seizure, vision and so on.49 50 52–55 Secondarily, there was a lack of standard proxy measures to define the screen-positive cases. Currently available examples of proxy measures are as follows: overall scores,38 39 number of negative answers,40 number of milestones,42 number of items,44 54 number of functional domains,51 number of significant concerns49 50 and so on. These two factors together, often make the screening results incomprehensible to health professionals who are not familiar with the tool in question. Moreover, it is neither possible to convert nor compare the test scores between separate screening tools, for better understanding. Many of the tools developed in English-speaking countries might not be suitable for non-English-speaking countries due to different sociocultural backgrounds and problematic translation.67–69 These issues might become a barrier for early identification and rehabilitation of developmental delay from the service providers’ end. Lastly, several studies reported that the expected sensitivity-specificity was not achieved due to the lack of validated gold standard assessment tool for the particular culture in question.44 51 53 To the best of our knowledge, there is a lack of WHO’s centralised initiatives, as well as no global regulatory body is currently working in this regard. Majority of the developmental assessment tools found in this review were established for high-income countries (BSID, DDST, REELS, GDS, MABC-2 and so on). Only three of them were designed and developed in LMICs (ABFW, DAASII and RNDA). None of the studies using assessment tools designed for high-income counties, provided information on cultural adaptation. However, Parveen et al, took the initiative to culturally adapt Bayley Scales of Infant Development- Second Edition (BSID-II) items for Bangladeshi infants.70 Example of culture-sensitive BSID-II items for Bangladeshi infants are presented in online supplemental table S7. Future research work should focus on developing or adapting developmental assessment tools to be efficiently used as gold standard for LMICs.
In this systematic review, we had observed East Asian and Pacific, European and Central Asian, Latin American and the Caribbean, Middle East and North African, South Asian and sub-Saharan cultural contexts among the eligible studies, although the number of countries engaged in similar studies are alarmingly low compared with the number of LMICs in total.34 This reveals the urgent need for valid and culturally sensitive screening tools for the rest of the LMICs. Among the 16 eligible screening tools, half of them were developed in LMICs (DSQ, GMCD, LEST 0–3, LDS, MORBAS, ND-DSQ, RTHB-DC and TDSC) and another half were developed in high-income countries (ASHA, ASQ, INFANIB, Little DCDQ, PEDS, R-PDQ, TQSI and WSST). We have found the majority of the culturally sensitive tools translated in their native language. Still, for multilingual countries like Benin, Ethiopia, India and so on, the necessity of translating the tools in regional languages remains high. None of the LMICs has been found to be engaged in collecting nationally representative longitudinal data on the prevalence of developmental delay, which is vital for disease projection. The gathering of nationally representative prevalence data in linguistic, social, ethnic and cultural subgroups would allow the validation of customised developmental screening tools according to disease burden. Greater customisation to respect the diverse cultural norms71 of a particular community, will also most likely result in greater acceptance72 73 of the screening process, which is crucial for the success of a large-scale surveillance programme.
While planning surveillance programme for resource-poor settings, additional factors should be kept in mind. According to Gupta and Patel, lack of furniture as well as staircase at home often results in exhibition of delayed gross motor skills due to lack of practice. Similarly, being heavily dependent on recall method is also problematic, as it is burdensome for parents with no or minimal education.55 To overcome these issues, Ertem et al suggested to target very young children for developmental screening/surveillance. As earlier we can screen the children, higher the chances of attaining similar milestones at similar ages despite cultural differences.42
Promising quasi-validated tool
We have found quite a few promising screening tools suitable for early identification of developmental delay. Unfortunately, could not include them as the studies did not fulfil our selection criteria. One of the quasi-validated tools is Neonatal Oral Motor Assessment Scale (NOMAS). NOMAS is a commonly used neonatal feeding evaluation which is developed by Marjorie Meyer Palmer in 1985. The NOMAS is the only available neonatal feeding evaluation that can be used for the term or preterm infants and for breast or bottle-fed infants. This is a 28-items observational checklist for tongue and jaw movement. Following the observation of non-nutritive sucking, oral feeding for the first 2 min are evaluated.74 In a study conducted in Taiwan by Tsai et al, 2010, the predictive validity of NOMAS was assessed against BSID-II in a group of 27 preterm infants without brain lesion to demonstrate neurodevelopmental outcome at 6 months and 12 months of corrected age.75
Suitable screening tools for primary healthcare setting
Out of the 16 eligible screening tools, we would recommend two screening tools feasible enough to be used for developmental surveillance at the primary healthcare setting. They are ASQ and PEDS. Both are parent-completed screening tools. Their strong points are: PEDS requires bare minimum additional materials and for ASQ, it provides 21 sets of questionnaires for 21 age groups. Besides, both are very easy to administer. We can easily build up a surveillance system using these tools. Where health workers can carry out screening at households using single PEDS questionnaire for all, then screened positive cases can be referred to the primary healthcare centres to conduct secondary screening with age-specific ASQ questionnaire. Basic properties of ASQ and PEDS are stated in the online supplemental table S8.76
Limitations
Despite our best efforts, there were several limitations to this study. This study was limited to articles published in the English language only due to constraints in resources and time. In this study, we exclude children who had developmental delay due to HIV exposure or autism spectrum disorder or other behavioural disorders. Although these children also suffer from varying degrees of developmental delay, the pathogenesis behind those delays is closely related to the diseases.77 78 Moreover, conventionally it takes >2 years of age to diagnose a child with autism spectrum disorder and hence the age range of currently available autism screening tools starts later than general developmental screening tools (eg, Modified Checklist for Autism in Toddlers: 16–30 months; where ASQ-III: 1–66 months). This conflicts with the objectives of our study to ensure early diagnosis of developmental delay. So, with respect to other neurodevelopmental disorders, we preferred to focus exclusively on developmental delay in our study. Although it is very difficult to rule out the possibility of undiagnosed cases of autism being included among all the developmentally delayed children, as none of the studies reported so. Moreover, we were unable to critically appraise the available screening tools in terms of diagnostic accuracy due to the unavailability of the necessary information, which is quite reasonable as Boggs et al also reported that authors tend to provide validity information very briefly and evidence on accuracy are most difficult to obtain.30 We are hopeful to conduct subsequent systematic review and meta-analysis on geographical region/country/domain-specific screening tools and their psychometric properties based on the information obtained from this study.
Recommendations
A global regulatory body should be formed to standardise the terminologies and cut-off scores of available and future screening tools to improve comprehensiveness and interpretation of test results, simultaneously ensuring better correlation between results obtained from different screening tools.
Future research work should focus on revising existing screening as well as assessment tools in different ethnic and cultural perspectives and validate them in the respective normative sample as well as conducting systematic reviews based on individual screening tools in different cultural settings.
We also recommend ensuring nationwide routine developmental surveillance programmes in LMICs using culturally sensitive tools to identify and treat developmental delay as early as possible. Developmental screening at the time of routine immunisation schedule could be a possible way to integrate this with an existing successful public health programme in LMICs. This timing would be both cost-effective and maximise response rates.
Conclusions
Developmental screening is required for early diagnosis of developmental delays in infants and young children in LMICs to enable early intervention and rehabilitation. In order to do this, culturally sensitive, easy-to-administer screening tools with good psychometric properties are needed. We observed that there is a lack of culturally sensitive developmental screening tools validated among under-5 children in LMICs. However, we have found eight screening tools with relatively high sensitivity and specificity. We also identified key research gaps and consequently proposed a few recommendations for overcoming those gaps. These include (but not limited to) global standardisation of terminologies and cut-off scores for screening tools, revising existing tools according to diverse cultural norms and validating them in the respective normative sample and finally ensuring nationwide routine developmental surveillance programmes in LMICs using culturally sensitive tools. To execute so, we have suggested a health worker-centred screening system consisting of ASQ and PEDS. Therefore, future research should focus on enabling the caregivers, health workers and therapists to assist in children with developmental delays in LMICs to reach their full developmental potential.
Supplementary Material
Acknowledgments
The authors acknowledge the wise feedback and invaluable suggestions received from Professor Dr M. Shafiqur Rahman, Institute of Statistical Research and Training, University of Dhaka and Professor Dr Naila Zaman Khan, Department of Paediatric Neuroscience, Dhaka Shishu (Children’s) Hospital, Bangladesh Institute of Child Health.
Footnotes
Contributors: This study was conceived and designed by GK and TF. CK developed the search strategy. Three authors conducted the database search (phase I up to March 2018: CK; phase II up to July 2020: IJ and MKI). Three authors (TF, IJ and MKI) independently screened the title and abstracts. TF, MKI and GK independently performed the full-text review of the screened articles. During each step of the study selection process, disagreements were resolved through discussion. TF and MKI wrote the first draft with input from GK, NB, KuB and MM. All authors reviewed all drafts and approved the final submitted manuscript.
Funding: This project was not externally funded. Study activities were supported by the Asian Institute of Disability and Development (AIDD), University of South Asia, Bangladesh.
Competing interests: None declared.
Patient and public involvement statement: Patients or the public were not involved in the design, or conduct, or reporting, or dissemination plans of our research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
No data are available. No original data were generated for this study.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
As this systematic review did not directly involve human or animal subjects, or access to medical records, ethical approval was not required.
References
- 1. University of Michigan . Developmental delay [online], 2010. Available: http://www.med.umich.edu/yourchild/topics/devdel.htm [Accessed 5 Jul 2018].
- 2. WHO . International classification of functioning, disability and health. Geneva: World Health Organization, 2001. [Google Scholar]
- 3. Fernald L, Kariger P, Engle P, et al. Examining early child development in low-income countries: a toolkit for the assessment of children in the first five years of life [online]. The World Bank, 2009. Available: https://openknowledge.worldbank.org/bitstream/handle/10986/28107/NonAsciiFileName0.pdf?sequence=1 [Accessed 1 Jan 2019].
- 4. Walker SP, Wachs TD, Gardner JM, et al. Child development: risk factors for adverse outcomes in developing countries. Lancet 2007;369:145–57. 10.1016/S0140-6736(07)60076-2 [DOI] [PubMed] [Google Scholar]
- 5. WHO . Early childhood development and disability: a discussion paper [online], 2012. Available: https://apps.who.int/iris/bitstream/handle/10665/75355/9789241504065_eng.pdf;sequence=1 [Accessed 13 Feb 2019].
- 6. House with No Steps . What is a developmental delay? [online], 2018. Available: https://www.hwns.com.au/disability-services/childrens-services/early-childhood-intervention/what-is-a-developmental-delay-or-disability/ [Accessed 15 May 2019].
- 7. Institute of Community Integration, University of Minnesota . About developmental disabilities [online], 2019. Available: https://ici.umn.edu/welcome/definition.html [Accessed 15 May 2019].
- 8. Warren R, Kenny M, Bennett T, et al. Screening for developmental delay among children aged 1-4 years: a systematic review. CMAJ Open 2016;4:E20–7. 10.9778/cmajo.20140121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Sim F, Thompson L, Marryat L, et al. Predictive validity of preschool screening tools for language and behavioural difficulties: a PRISMA systematic review. PLoS One 2019;14:e0211409. 10.1371/journal.pone.0211409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sices L. Developmental screening in primary care: the effectiveness of current practice and recommendations for improvement [online], 2007. Available: https://core.ac.uk/download/pdf/71350769.pdf [Accessed 15 May 2018].
- 11. WHO . Newborn death and illness [online], 2011. Available: https://www.who.int/pmnch/media/press_materials/fs/fs_newborndealth_illness/en [Accessed 5 Jul 2018].
- 12. UNICEF . Neonatal mortality - UNICEF Data [online], 2018. Available: https://data.unicef.org/topic/child-survival/neonatal-mortality/ [Accessed 10 Jul 2018].
- 13. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006;3:e442. 10.1371/journal.pmed.0030442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Grantham-McGregor S, Cheung YB, Cueto S, et al. Developmental potential in the first 5 years for children in developing countries. Lancet 2007;369:60–70. 10.1016/S0140-6736(07)60032-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hasan A, Leslie R, Nakajima N. How community-based early childhood programs can impact child development [online]. World Bank Blogs, 2017. Available: http://blogs.worldbank.org/education/how-community-based-early-childhood-programs-can-impact-child-development [Accessed 10 Jul 2018].
- 16. Scherzer AL, Chhagan M, Kauchali S, et al. Global perspective on early diagnosis and intervention for children with developmental delays and disabilities. Dev Med Child Neurol 2012;54:1079–84. 10.1111/j.1469-8749.2012.04348.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Ofek-Shlomai N, Berger I. Inflammatory injury to the neonatal brain - what can we do? Front Pediatr 2014;2:30. 10.3389/fped.2014.00030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuo H-T, Muo C-H, Chang Y-T, et al. Change in prevalence status for children with developmental delay in Taiwan: a nationwide population-based retrospective study. Neuropsychiatr Dis Treat 2015;11:1541–7. 10.2147/NDT.S84088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Wang S-Y, Hsu SH, Chen L-K. The impact on neonatal mortality of shifting childbirth services among levels of hospitals: Taiwan’s experience. BMC Health Serv Res 2009;9:94. 10.1186/1472-6963-9-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Centers for Disease Control and Prevention . Developmental monitoring and screening [online], 2020. Available: https://www.cdc.gov/ncbddd/childdevelopment/screening.html [Accessed 12 Oct 2020].
- 21. Committee on Children with Disabilities . Developmental surveillance and screening of infants and young children. Pediatrics 2001;108:192–5. [DOI] [PubMed] [Google Scholar]
- 22. Sabanathan S, Wills B, Gladstone M. Child development assessment tools in low-income and middle-income countries: how can we use them more appropriately? Arch Dis Child 2015;100:482–8. 10.1136/archdischild-2014-308114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Glascoe F, Cairney J. Best practices in test construction for developmental-behavioral measures: quality standards for reviewers and researchers. follow-up for NICU graduates. Springer 2018:255–79. [Google Scholar]
- 24. Fischer VJ, Servili C, Morris JE, et al. Developmental screening tools: feasibility of use at primary health level in low and middle-income settings. Neuropsychiatr Enfance Adolesc 2012;60:S304. 10.1016/j.neurenf.2012.04.881 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Scherzer AL. Experience in Cambodia with the use of a culturally relevant developmental milestone chart for children in low- and middle-income countries. J Policy Pract Intellect Disabil 2009;6:287–92. 10.1111/j.1741-1130.2009.00234.x [DOI] [Google Scholar]
- 26. Soltani S, Takian A, Akbari Sari A, Sari A, et al. Cultural barriers in access to healthcare services for people with disability in Iran: a qualitative study. Med J Islam Repub Iran 2017;31:293–9. 10.14196/mjiri.31.51 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Baker DL, Miller E, Dang MT, et al. Developing culturally responsive approaches with Southeast Asian American families experiencing developmental disabilities. Pediatrics 2010;126:S146–50. 10.1542/peds.2010-1466I [DOI] [PubMed] [Google Scholar]
- 28. Baxter C, Mahoney W. Developmental disability across cultures [online]. Caring for kids new to canada, 2018. Available: https://www.kidsnewtocanada.ca/mental-health/developmental-disability/ [Accessed 15 May 2019].
- 29. Gladstone MJ, Lancaster GA, Jones AP, et al. Can Western developmental screening tools be modified for use in a rural Malawian setting? Arch Dis Child 2008;93:23–9. 10.1136/adc.2006.095471 [DOI] [PubMed] [Google Scholar]
- 30. Boggs D, Milner KM, Chandna J, et al. Rating early child development outcome measurement tools for routine health programme use. Arch Dis Child 2019;104:S22–33. 10.1136/archdischild-2018-315431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Marlow M, Servili C, Tomlinson M. A review of screening tools for the identification of autism spectrum disorders and developmental delay in infants and young children: recommendations for use in low- and middle-income countries. Autism Res 2019;12:176–99. 10.1002/aur.2033 [DOI] [PubMed] [Google Scholar]
- 32. Richards M, Mossey J, Robins DL. Parentsʼ concerns as they relate to their child's development and later diagnosis of autism spectrum disorder. J Dev Behav Pediatr 2016;37:532–40. 10.1097/DBP.0000000000000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. World Bank Blogs . New world bank country classifications by income level: 2020-2021, 2020. Available: https://blogs.worldbank.org/opendata/new-world-bank-country-classifications-income-level-2020-2021 [Accessed 13 Jul 2020].
- 34. World Bank Country and Lending Groups . World bank data help desk. Datahelpdesk.worldbank.org, 2020. Available: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups [Accessed 13 Jul 2020].
- 35. Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 2009;151:264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 36. Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 37. Modesti PA, Reboldi G, Cappuccio FP, et al. Panethnic differences in blood pressure in Europe: a systematic review and meta-analysis. PLoS One 2016;11:e0147601. 10.1371/journal.pone.0147601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Juneja M, Mohanty M, Jain R, et al. Ages and stages questionnaire as a screening tool for developmental delay in Indian children. Indian Pediatr 2012;49:457–61. 10.1007/s13312-012-0074-9 [DOI] [PubMed] [Google Scholar]
- 39. Yue A, Jiang Q, Wang B, et al. Concurrent validity of the ages and stages questionnaire and the Bayley scales of infant development III in China. PLoS One 2019;14:e0221675. 10.1371/journal.pone.0221675 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dias DC, Rondon-Melo S, Molini-Avejonas DR. Sensitivity and specificity of a low-cost screening protocol for identifying children at risk for language disorders. Clinics 2020;75:e1426. 10.6061/clinics/2020/e1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Khan NZ, Muslima H, Shilpi AB, et al. Validation of a home-based neurodevelopmental screening tool for under 2-year-old children in Bangladesh. Child Care Health Dev 2013;39:643–50. 10.1111/j.1365-2214.2012.01393.x [DOI] [PubMed] [Google Scholar]
- 42. Ertem IO, Dogan DG, Gok CG, et al. A guide for monitoring child development in low- and middle-income countries. Pediatrics 2008;121:e581–9. 10.1542/peds.2007-1771 [DOI] [PubMed] [Google Scholar]
- 43. Soleimani F, Dadkhah A. Validity and reliability of infant neurological international battery for detection of gross motor developmental delay in Iran. Child Care Health Dev 2007;33:262–5. 10.1111/j.1365-2214.2006.00704.x [DOI] [PubMed] [Google Scholar]
- 44. Nair MK, Nair GH, Mini AO, et al. Development and validation of language evaluation scale Trivandrum for children aged 0-3 years--LEST (0-3). Indian Pediatr 2013;50:463–7. 10.1007/s13312-013-0154-5 [DOI] [PubMed] [Google Scholar]
- 45. Venter A, Pienaar AE, Coetzee D. Suitability of the ‘Little DCDQ’ for the identification of DCD in a selected group of 3–5-year-old South African children. Early Child Dev Care 2015;185:1359–71. 10.1080/03004430.2014.1000887 [DOI] [Google Scholar]
- 46. Bhave A, Bhargava R, Kumar R. Development and validation of a new Lucknow development screen for Indian children aged 6 months to 2 years. J Child Neurol 2010;25:57–60. 10.1177/0883073809336121 [DOI] [PubMed] [Google Scholar]
- 47. Dagvadorj A, Takehara K, Bavuusuren B, et al. The quick and easy Mongolian rapid baby scale shows good concurrent validity and sensitivity. Acta Paediatr 2015;104:e94–9. 10.1111/apa.12884 [DOI] [PubMed] [Google Scholar]
- 48. Jain R, Arora A, Anand R, et al. Designing and validation of a Hindi-language parent self-report developmental screening tool. Indian Pediatr 2017;54:550–5. 10.1007/s13312-017-1066-6 [DOI] [PubMed] [Google Scholar]
- 49. Chunsuwan I, Hansakunachai T, Pornsamrit S. Parent evaluation of developmental status (PEDS) in screening: the Thai experience. Pediatr Int 2016;58:1277–83. 10.1111/ped.13055 [DOI] [PubMed] [Google Scholar]
- 50. Wantanakorn P, Sawangworachart K, Roongpraiwan R, et al. Parents’ evaluation of developmental status (PEDS) in screening for developmental delay in Thai children aged 18-30 months. Indian Pediatr 2016;53:1110–3. [PubMed] [Google Scholar]
- 51. Awasthi S, Pande VK. Validation of revised prescreening denver questionnaire in preschool children of urban slums. Indian Pediatr 1997;34:919–22. [PubMed] [Google Scholar]
- 52. van der Linde J, Swanepoel DW, Glascoe FP, et al. Developmental screening in South Africa: comparing the National developmental checklist to a standardized tool. Afr Health Sci 2015;15:188–96. 10.4314/ahs.v15i1.25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Koura KG, Boivin MJ, Davidson LL, et al. Usefulness of child development assessments for low-resource settings in francophone Africa. J Dev Behav Pediatr 2013;34:486–93. 10.1097/DBP.0b013e31829d211c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Nair MK, George B, Philip E, et al. Trivandrum developmental screening chart. Indian Pediatr 1991;28:869–72. [PubMed] [Google Scholar]
- 55. Gupta R, Patel NV. Trial of a screening technique of the developmental assessment of infants and young children (6 weeks-2 years). Indian Pediatr 1991;28:859–67. [PubMed] [Google Scholar]
- 56. Singh A, Yeh C, Blanchard S. Ages and stages questionnaire: una escala de evaluación global. Bol Med Hosp Infant Mex 2017;74:5–12. [DOI] [PubMed] [Google Scholar]
- 57. Squires J, Bricker D. Ages & stages questionnaires. Available: https://brookespublishing.com/product/asq-3/ [Accessed 10 Aug 2018].
- 58. Liao W, Wen E-yi, Li C, et al. Predicting neurodevelopmental outcomes for at-risk infants: reliability and predictive validity using a Chinese version of the INFANIB at 3, 7 and 10 months. BMC Pediatr 2012;12:27. 10.1186/1471-2431-12-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Page FP, Glascoe FP. Parents evaluation of developmental status (PEDS). Indian Pediatr 2003;40:439–40. [PubMed] [Google Scholar]
- 60. Woolfenden S, Eapen V, Williams K, et al. A systematic review of the prevalence of parental concerns measured by the parents’ evaluation of developmental status (PEDS) indicating developmental risk. BMC Pediatr 2014;14:231. 10.1186/1471-2431-14-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Plessis L, Koornhof H, Marais M, et al. Implementation of the road-to-health-booklet health promotion messages at primary health care facilities, Western Cape Province, South Africa. SAJCH 2017;11:164–9. [Google Scholar]
- 62. Krishnamurthy V, Srinivasan R. Childhood disability screening tools : the south east Asian perspective a review for the who office of the south east Asian region. Mumbai: WHO, 2011. [Google Scholar]
- 63. Landers C, Kagitcibasi C. Measuring the psychosocial development of young children: the innocent technical workshop. Consultative Group on Early Childhood Care Development, 1990. [Google Scholar]
- 64. Mukherjee SB, Aneja S, Krishnamurthy V, et al. Incorporating developmental screening and surveillance of young children in office practice. Indian Pediatr 2014;51:627–35. 10.1007/s13312-014-0465-1 [DOI] [PubMed] [Google Scholar]
- 65. Maulik PK, Darmstadt GL. Childhood disability in low- and middle-income countries: overview of screening, prevention, services, legislation, and epidemiology. Pediatrics 2007;120:S1–55. 10.1542/peds.2007-0043B [DOI] [PubMed] [Google Scholar]
- 66. Fernald L, Prado E, Kariger P, et al. A toolkit for measuring early childhood development in low and middle-income countries. The World Bank, 2017. [Google Scholar]
- 67. Sarmiento Campos JA, Squires J, Ponte J. Universal developmental screening: preliminary studies in galicia, Spain. Early Child Dev Care 2011;181:475–85. 10.1080/03004430903458007 [DOI] [Google Scholar]
- 68. Pomés M, Squires J, Yovanoff P. Psychometric examination of a Spanish translation of a developmental screening instrument. J Early Child Res 2016;14:132–45. 10.1177/1476718X14529279 [DOI] [Google Scholar]
- 69. Kiing JSH, Rajgor D, Toh T-H. Topical review: mind your language—translation matters (a narrative review of translation challenges). J Pediatr Psychol 2016;41:1110–9. 10.1093/jpepsy/jsw036 [DOI] [PubMed] [Google Scholar]
- 70. Parveen M, Rahman ST, Islam S, et al. Adaptation of items of bayley scales of infant development-II (BSID-II) suitable for Bangladeshi infants. Dhaka Univ J Biol Sci 2014;23:187–95. 10.3329/dujbs.v23i2.20099 [DOI] [Google Scholar]
- 71. Revel M. Article 12: Respect for cultural diversity and pluralism. In: ten Have H, Stanton-Jean M, eds. The UNESCO universal declaration on bioethics and human rights. UNESCO Publishing, 2019: 199–209. [Google Scholar]
- 72. Levine R, Levine S, Dixon S, et al. Child care and culture. Cambridge: Cambridge University Press, 1994. [Google Scholar]
- 73. Brooks E, Novins DK, Noe T, et al. Reaching rural communities with culturally appropriate care: a model for adapting remote monitoring to American Indian veterans with posttraumatic stress disorder. Telemed e-Health 2013;19:272–7. 10.1089/tmj.2012.0117 [DOI] [PubMed] [Google Scholar]
- 74. Zarem C, Crapnell T, Tiltges L, et al. Neonatal nurses’ and therapists’ perceptions of positioning for preterm infants in the neonatal intensive care unit. Neonatal Netw 2013;32:110–6. 10.1891/0730-0832.32.2.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Tsai S-W, Chen C-H, Lin M-C. Prediction for developmental delay on neonatal oral motor assessment scale in preterm infants without brain lesion. Pediatr Int 2010;52:65–8. 10.1111/j.1442-200X.2009.02882.x [DOI] [PubMed] [Google Scholar]
- 76. Garg P, Ha MT, Eastwood J, et al. Health professional perceptions regarding screening tools for developmental surveillance for children in a multicultural part of Sydney, Australia. BMC Fam Pract 2018;19:42. 10.1186/s12875-018-0728-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Lowry F. Brain chemistry differs in autism vs developmental delay [online]. Medscape, 2013. Available: https://www.medscape.com/viewarticle/808794 [Accessed 5 Jul 2018].
- 78. Ngoma MS MSOC. The effect of HIV on developmental milestones in children. J AIDS Clin Res 2015;06:482. 10.4172/2155-6113.1000482 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-038182supp001.pdf (281.9KB, pdf)
Data Availability Statement
No data are available. No original data were generated for this study.