Abstract
Background
As the COVID-19 pandemic continues, there is a question of whether hospitals have adequate resources to manage patients. We aim to investigate global hospital bed (HB), acute care bed (ACB), and intensive care unit (ICU) bed capacity and determine any correlation between these hospital resources and COVID-19 mortality.
Method
Cross-sectional study utilizing data from the World Health Organization (WHO) and other official organizations regarding global HB, ACB, ICU bed capacity, and confirmed COVID-19 cases/mortality. Descriptive statistics and linear regression were performed.
Results
A total of 183 countries were included with a mean of 307.1 HBs, 413.9 ACBs, and 8.73 ICU beds/100,000 population. High-income regions had the highest mean number of ICU beds (12.79) and HBs (402.32) per 100,000 population whereas upper middle-income regions had the highest mean number of ACBs (424.75) per 100,000. A weakly positive significant association was discovered between the number of ICU beds/100,000 population and COVID-19 mortality. No significant associations exist between the number of HBs or ACBs per 100,000 population and COVID-19 mortality.
Conclusions
Global COVID-19 mortality rates are likely affected by multiple factors, including hospital resources, personnel, and bed capacity. Higher income regions of the world have greater ICU, acute care, and hospital bed capacities. Mandatory reporting of ICU, acute care, and hospital bed capacity/occupancy and information relating to coronavirus should be implemented. Adopting a tiered critical care approach and targeting the expansion of space, staff, and supplies may serve to maximize the quality of care during resurgences and future disasters.
Keywords: COVID-19, Bed capacity, Hospital resources, Global health
Background
As of October 11, 2020, 37,318,319 confirmed COVID-19 cases and 1,074,500 deaths (case fatality rate of 2.88%) have been reported across the globe. The United States (U.S.) accounts for 19.4% of global COVID-19 confirmed cases and 19.3% of deaths due to COVID-19.1 Many other countries around the world, including Brazil, the United Kingdom (U.K.), and India, are experiencing high disease burdens and deaths.1 Several factors likely contribute to the differing fatalities observed in each country. One of the largest factors implicated in the COVID-19 deaths is the surge of cases that deplete hospital resources.2, 3, 4 Many resources are required to adequately treat a critically ill patient with COVID-19, such as an ICU bed with a full-featured ventilator, personal protective equipment (e.g., isolation gowns, N95 respirators, gloves, etc.), and adequate hospital staffing.5, 6, 7 The rapid surge of cases has at times overwhelmed available resources and potentially comprised the ability to provide consistent, high-quality care, often forcing physicians to triage treatment among critically ill patients.8
Prior to the peak of the first wave of the outbreak in April, the Institute for Health Metrics and Evaluation (IHME) projected ICU bed shortages in many countries, including the U.S., U.K., and France, as the pandemic continues.9 These countries have experienced relatively high incidences of COVID-19 deaths amounting to 207,366 in the U.S., 42,317 in the U.K., and 31,969 in France as of October 4, 2020.10 Thus, an accurate report of the hospital supplies that continue to be exhausted is warranted in order to prioritize intervention and prevention strategies in anticipation of a second wave of COVID-19 cases that may occur once daily routines resume in full.
The relative shortage of hospital resources is a growing issue that can influence the practices of physicians and the subsequent care provided to their patients. The primary aim of this study is to investigate global hospital resources categorized as hospital beds (HBs), acute care beds (ACBs), and ICU beds. A secondary aim is to assess if there is any correlation between hospital resources and the number of confirmed COVID-19 deaths with the hypothesis that the number of COVID-19 deaths will be shown to decrease in areas with a greater concentration of hospital, acute care, and ICU beds.
Methods
Search strategy and selection criteria
This cross-sectional study utilized the data obtained through literature, government, Central Intelligence Agency (CIA), Center for Disease Control and Prevention (CDC), The World Bank, World Health Organization (WHO), and professional & official hospital sources (Supplementary File). A literature search for data regarding ICU bed capacity was necessary due to the lack of publicly available data regarding these figures. A total of 183 countries were included in this analysis. The countries chosen in this analysis were selected based on the availability of data, as many countries do not have information regarding the number of ICU beds and/or ACBs. Countries were then classified by income according to The World Bank definitions: low-income (gross net income [GNI] of ≤$1035/capita), lower middle-income (GNI $1036-4045/capita), upper middle-income (GNI $4046-12,535/capita), and high-income (GNI ≥$12,536/capita).11 , 12 ICU beds were defined as beds with critical care equipment (e.g., ventilator) that are adequately staffed by specialized nurses and physicians with critical care training.13 HBs were defined as beds regularly maintained, staffed, and available for use in public, private, general, and specialized hospitals and rehabilitation centers.14 ACBs were defined as beds accommodating patients for curative care with the intent to do at least one of the following: manage labor, perform surgery, cure illness/provide definitive treatment of injury, reduce the severity of illness/injury, protect against exacerbation/complications and perform diagnostic or therapeutic procedures.15
Data collection
The most recent reports detailing statistics relevant to the countries under study were utilized. Due to variability in the format statistics were reported in, data was uniformly converted to the number of beds/100,000 population utilizing epidemiological information from the CIA. Hospital resource data provided by news media articles, unofficial, or unreliable resources were excluded. Finally, the number of COVID-19 deaths as of October 4, 2020, were obtained from the WHO, Korean CDC, and Taiwan CDC.10 , 16, 17, 18
Statistical analysis
A descriptive statistical analysis was performed to evaluate the counts, means, and distribution of hospital, ICU, and ACBs in relation to the number of COVID-19 cases, deaths, and case-fatality rates (CFRs). Linear regression was also performed in order to test for any significant associations between bed capacity and confirmed COVID-19 deaths. IBM SPSS Statistics Version 26.0 (Armonk, NY) was used for statistical analyses. Significance was defined as P < 0.05. This study was conducted in compliance with ethical principles, was reviewed by our institutional review board, and was deemed exempt.
Results
Number of hospital beds per 100,000 population
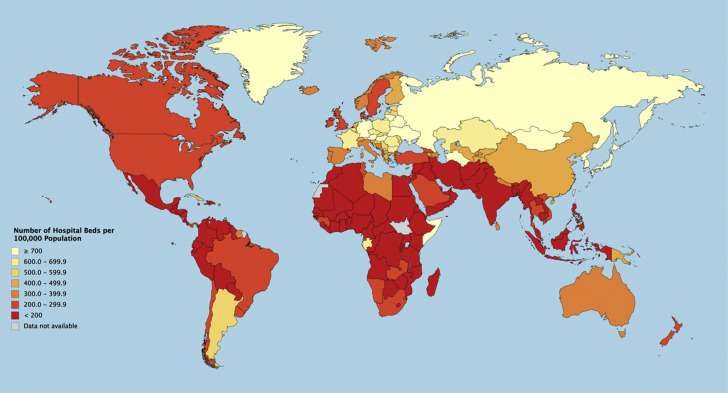
Data for total HBs were available for 183 countries with a mean of 307.1/100,000 in the population (Fig. 1 ). Monaco, Japan and North Korea reported the greatest amount of HBs/100,000 (1380, 1340, 1320, respectively).14 , 18 In contrast, all of the countries in Africa reported less than 200 HBs/100,000 population with the exception of Libya reporting 370, Somalia reporting 870, and Gabon reporting 630/100,000 population.14 Similarly, the majority of countries in North and South America, and Southern Asia reported <200 HBs/100,000 (Fig. 1).14 , 18 In regards to World Bank Income Regions, low-income regions had a mean of 231.79 HBs/100,000 (maximum = 880, minimum = 40, range = 840, standard deviation [SD] = 189.07), lower middle-income regions had a mean of 308.85 HBs/100,000 (maximum = 1,870, minimum = 30, range = 1,840, SD = 371.61), upper middle-income regions had a mean of 283.13 HBs/100,000 (maximum = 1,100, minimum = 10, range = 1,090, and high-income regions had a mean of 356.13 HBs/100,000 (maximum = 1,440, minimum = 20, range = 1,420, SD = 275.1). Linear regression analysis did not reveal any significant association between the number of HBs/100,000 and the number of confirmed COVID-19 deaths (Pearson coefficient = –0.006, R2 = 0.0004, P = 0.935, 95% CI: –0.003,0.003) nor CFR (Pearson coefficient = –0.098, R2 = 0.010, P = 0.186, 95% CI: –0.002,0.000).
Fig. 1.
Number of Hospital Beds per 100,000 Population. The majority of countries with hospital bed data reside in the 0-299 hospital beds/100,000 population range: 79 (43%) countries had <200 hospital beds/100,000 population whereas 37 (20%) countries reported 200-299 hospital beds/100,000 population. In contrast, only 13 (7.1%) countries reported ≥700 hospital beds/100,000 population. The number of hospital beds per 100,000 population ranged from 100 in Mali to 1870 in the Virgin Islands. Countries shaded in gray did not have data for the number of hospital beds. (Color version of the figure is available online.)
Number of acute care beds per 100,000 population
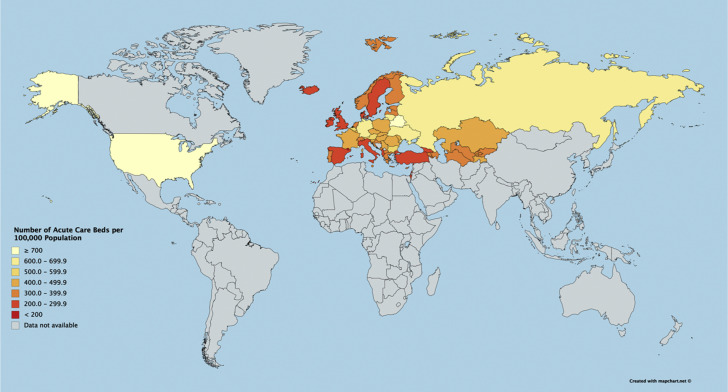
Data for ACBs were available for 52 countries with a mean of 413.87 ACBs/100,000 population. The U.S. and Belarus reported >700 ACBs/100,000 population (Fig. 2 ).15 In contrast, some European countries, including Turkey, Italy, Spain, Sweden, U.K., Iceland and Ireland reported <200 ACBs/100,000 population.15 Several Asian countries reported a moderate number of ACBs/100,000 population, including Tajikistan with 425, Kazakhstan 419, Kyrgyzstan 354, Uzbekistan 334, and Turkmenistan with 306/100,000 population.15 In regards to World Bank Income Regions, low-income regions had a mean of 425.00 ACBs/100,000 (maximum = 425, minimum = 425, range = 0, SD = 0), lower middle-income regions had a mean of 439 ACBs/100,000 (maximum = 613, minimum = 334, range = 279, SD = 127.52), upper middle-income regions had a mean of 424.75 ACBs/100,000 (maximum = 866, minimum = 210, range = 656, SD = 190.56) and high-income regions had a mean of 402.32 ACBs/100,000 (maximum = 1,119, minimum = 190, range = 929, SD = 179.58). Linear regression analysis did not reveal any significant association between the number of ACBs/100,000 and the number of deaths (Pearson coefficient = –0.078, R2 = 0.006, P = 0.585, 95% CI: –61.725,35.182) nor CFR (Pearson coefficient = –0.084, R2 = 0.007, P = 0.552, 95% CI: –0.004,0.002).
Fig. 2.
Number of Acute Care Beds per 100,000 Population. The number of acute care beds∗ per 100,000 population ranged from 190 in Andorra to 1119 in Monaco. Countries shaded in gray did not have data for the number of acute care beds. ∗Acute Care Beds were defined as hospital beds that are available for curative care. (Color version of the figure is available online.)
Number of ICU beds per 100,000 population
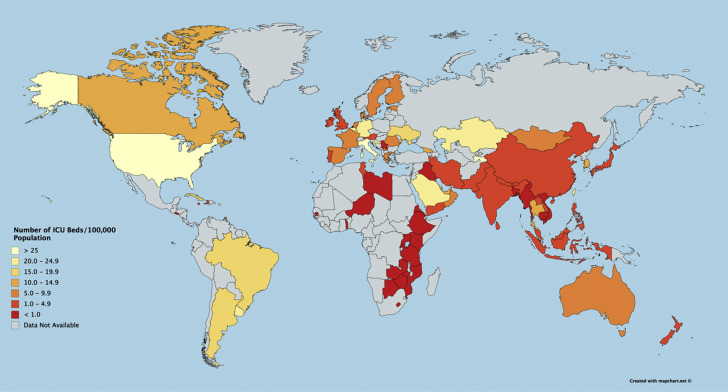
Data for ICU Beds/100,000 were available for 87 countries with a mean of 8.73 beds/100,000 population. The number of ICU beds differed considerably between countries. The U.S., Italy, and Tajikistan reported >25 ICU beds/100,000 population (Fig. 3 ).19 , 20 In contrast, many countries in Africa such as Libya, Niger, Ethiopia and Zambia reported a capacity of <1 ICU bed/100,000 population.21 Similarly, countries in Asia, including India, China, Vietnam, and Cambodia, among others, reported a similar ICU capacity (Fig. 3).22, 23, 24, 25, 26, 27, 28, 29 In regards to World Bank Income Regions, low-income regions had a mean of 6.44 ICU bed/100,000 (maximum = 65, minimum = 0.03, range = 64.97, SD = 19.45), lower middle-income regions had a mean of 2.05 ICU beds/100,000 (maximum = 15, minimum = 0.03, range = 14.97, SD = 3.54), upper middle-income regions had a mean of 9.23 ICU beds/100,000 (maximum = 57, minimum = 0.16, range = 56.84, SD = 13.60) and high-income regions had a mean of 12.79 ICU beds/100,000 (maximum = 86, minimum = 1.8, range = 84.2, SD = 14.57). Linear regression analysis counterintuitively revealed a significant association between the number of ICU beds/100,000 population and number of COVID-19 deaths (Pearson coefficient = 0.258, R2 = 0.067, P = 0.016, 95% CI: 62.298,602.402). However, there was no significant association between number of ICU beds/100,000 population and CFR (Pearson correlation = 0.169, R2 = 0.029, P = 0.119, 95% CI: –0.015, 0.126).
Fig. 3.
Number of ICU beds per 100,000 Population. The number of ICU beds per 100,000 population ranged from <1 in many African countries to >25 in the United States, Tajikistan, and Italy. The majority of countries reported ICU beds/100,000 in the 0-4.9 range: 23 (26.1%) countries reported <1 ICU beds/100,000 population, whereas 27 (30.7%) countries reported ICU beds/100,000 in the 1.0-4.9 range. In contrast, countries with >5 ICU beds/100,000 comprised a smaller percentage of countries, including 15 countries (17.0%) with 5-9.9 ICU beds/100,000, 8 countries (9.1%) with 10-14.9 ICU beds/100,000, 5 countries (5.7%) reporting 15-19.9 ICU beds/100,000, 7 countries (8.0%) with 20-24.9 ICU beds/100,000, and 3 countries (3.4%) reporting >25 ICU beds/100,000. Countries shaded in gray did not have data for the number of ICU beds. (Color version of the figure is available online.)
COVID-19 deaths as of July 15, 2020
Data for the number of COVID-19 deaths were available for the 183 countries analyzed in this study as of October 4, 2020. The ten countries with the highest number of COVID-19 deaths include the U.S. (207,366), Brazil (145,388), India (101,782), Mexico (78,492), U.K. (42,317), Italy (35,968), Peru (32,609), Spain (32,086), France (31,969), and Iran (26,746). In contrast, 12 of the 183 countries with confirmed COVID-19 cases have reported zero COVID-19 deaths, including Cambodia, Eritrea, Greenland, and Mongolia, among others.10 COVID-19 cases, deaths, and CFRs for each World Bank Income Region are listed in Table .
Table.
COVID-19 cases, deaths, and case:fatality ratios by World Health Bank Income Region.
| Low-income regions |
Lower middle-income regions |
Higher middle-income regions |
High-income regions |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cases | Deaths | CFR | Cases | Deaths | CFR | Cases | Deaths | CFR | Cases | Deaths | CFR | |
| Mean | 73,600.57 | 2174.75 | 2.49 | 58,957.31 | 1487.12 | 2.15 | 215,549.67 | 6745.85 | 2.40 | 305,775.65 | 9004.52 | 2.94 |
| Median | 9006.50 | 85.00 | 2.25 | 12,560.00 | 228.00 | 1.87 | 32,951.00 | 672.50 | 1.87 | 16,529.00 | 258.00 | 2.07 |
| Mode | 10,751.00 | 85.00 | 2.55 | 19.00 | 0.00 | 0.00 | 28.00 | 0.00 | 0.00 | 14.00 | 0.00 | 0.00 |
| Std. Deviation | 192,588.185 | 6702.40 | 1.71 | 98,193.30 | 2671.00 | 1.57 | 718,657.38 | 21,790.53 | 1.91 | 1,203,583.05 | 30,431.04 | 4.02 |
| Range | 789,423.00 | 32,085.00 | 6.97 | 367,546.00 | 11,055.00 | 6.25 | 4,880,495.00 | 145,388.00 | 8.26 | 7,256,220.00 | 207,366.00 | 28.85 |
| Minimum | 509.00 | 1.00 | 0.05 | 19.00 | 0.00 | 0.00 | 28.00 | 0.00 | 0.00 | 14.00 | 0.00 | 0.00 |
| Maximum | 789,932.00 | 32,086.00 | 7.02 | 367,565.00 | 11,055.00 | 6.25 | 4,880,523.00 | 145,388.00 | 8.26 | 7,256,234.00 | 207,366.00 | 28.85 |
Shown are the mean, median, mode, standard deviation, range, minimum, and maximum for COVID-19 cases, deaths, and case:fatality ratios stratified by income regions according to The World Bank definitions.
CFR = Case:Fatality Ratio, Std. = Standard.
Discussion
Our study revealed a weakly positive significant association between the number of ICU beds/100,000 population and COVID-19 deaths. While counterintuitive, our interpretation is that areas of high population density likely have a higher number of ICU beds to accommodate the needs of the population. However, densely populated areas are also those, which propagate the spread of the coronavirus and ultimately yield a higher death count. Therefore, the positive association discovered is likely affected by population size as a modifying variable. Additionally, patients with COVID-19 who are admitted into the ICU are in more critical condition and are in greater need of extreme supportive treatment, such as mechanical ventilation, compared to patients in other hospital locations.30 Recent literature has shown dramatic variation in the global mortality rate of COVID-19 patients admitted to the ICU, ranging from 2.7% to 65.4%, whereas hospitalized patients in non-ICU wards experienced a mortality rate of 14%.30, 31, 32, 33, 34 Moreover, another study concluded that the majority of ICU admissions occur in geriatric patients ≥65 y of age and account for 80% of all COVID-19 deaths.35 These findings suggest that the significant association discovered between ICU beds/100,000 population and COVID mortality rates is likely influenced by multiple patient factors, including age, underlying comorbidities, disease severity, and population size. Therefore, the collection and utilization of this clinical data from hospitalized patients represent one way in which future analyses could adjust for these variables to examine the association between ICU beds/100,000 population and COVID-19 mortality in greater detail.
However, our findings of low-income countries having a low reported COVID-19 mortality rate despite having a lower number of ICU beds, ACBs, and HBs per 100,000 population compared to high-income countries is worth discussing. Patient access to care is dependent on individual factors (e.g., insurance status, income/ability to afford healthcare, ability to travel to the hospital, etc.), as well the type of healthcare system utilized in their country (public, private, or mixed public/private). While patients in a public healthcare system have the cost of healthcare services paid by their government, those in a country with a mixed or private healthcare system may be less likely to seek care due to an inability to pay for services.36 Previous literature has shown that those with health insurance are more likely to seek care, with income serving as an important determinant in the decision to seek treatment, implying that those without insurance/adequate income are more likely to not seek care.36 In the context of our findings, the low reported mortality rates for COVID-19 patients in low-income regions may be attributed to these patients not traveling to hospitals to seek care due to an inability to afford care, consequently causing severely ill patients to die at home rather than in a hospital, which would confirm both their case and mortality due to COVID-19.36 Therefore, the greater mortality rate observed in high-income countries may be due to an increased patient ability to travel to and unfortunately succumb to COVID-19 in the hospital setting despite high-quality care.
Our study revealed no significant association between the number of hospital beds/100,000 and COVID-19 deaths, nor the number of ACBs/100,000 and COVID-19 deaths. This may imply that there are other factors that have a greater influence on the mortality of COVID-19 patients, such as available supplies and personnel. For example, full-feature ventilators may be needed to treat critically ill patients in the course of this disease and can significantly affect the prognosis of the patient.5 , 37 Furthermore, a relative deficit of PPE can compound the effects of healthcare personnel shortages and can have a dramatic effect on the survival of COVID-19 patients.6 , 7 , 38 , In particular, previous studies have deemed an insufficient number of respiratory therapists as a main limiting factor affecting the ability to deliver care in this large-scale pandemic.5
However, the true impact of COVID-19 on hospital systems is likely to be underestimated without considering the burden of other patient populations. As it has been shown that COVID-19 can profoundly exhaust hospital resources, many countries have been projected to experience a shortage of critical care supplies due to the rapid influx of COVID-19 patients.9 , 34 Therefore, it is important to consider the additional strain that non-COVID patients can place on already deficient hospital resources and the implications this has for treating patients. For example, many patients present to emergency departments due to traumatic injuries. Since the onset of the pandemic and the encouragement of social distancing and stay-at-home orders, patterns of traumatic injury have been shown to change.39, 40, 41, 42, 43 For example, the U.S. has observed a decrease in vehicle-related injuries and a paradoxical increase in gun violence in certain major cities.39, 40, 41, 42, 43 With an increased number of HBs, ACBs, and ICU beds being dedicated to COVID-19 patients, there is a question of whether patients with traumatic injuries can still receive a high quality of care and vice-versa, particularly as countries begin to lift restrictions and move toward restoring normalcy.
In addition to changing patterns of traumatic injury, recent studies have discovered altered patterns of mortality in non-COVID related categories.44 In particular, areas that have been heavily burdened with COVID-19 related deaths have also experienced large increases in deaths from other etiologies, including diabetes, heart disease, and cerebrovascular disease.44 This may imply that patients with underlying comorbidities are not seeking treatment due to fear and further highlights the need for hospitals to maintain adequate resources and minimize the risk of virus transmission in order to allow for those who require emergency medical treatment to feel comfortable doing so.
Many countries are currently experiencing a “second-wave” of COVID-19.1 , 45 As we enter the second half of 2020, the effects of seasonal influenza viruses can further complicate the situation and could potentially cause many areas of the world to reach bed capacity.46, 47 Therefore, urgent action is needed by hospital administration, official organizations such as the Centers for Disease Control and Prevention (CDC), and government to implement strategies that can encourage sufficient hospital bed capacity/resources and minimize the effects these limiting factors can have on patient care.
Our study has several advantages over the existing literature. While researchers have previously investigated ICU bed capacity in 182 countries around the world, our study includes a greater number of countries, as well as the incorporation of HBs and ACBs and capacity in relation to COVID-19 morality.34 , 47 Additionally, in contrast to other studies, we only utilized data published by reputable government and healthcare organizations.34 However, there are several limitations to our study. First, as there is no globally accepted consensus of the definitions for different categories of hospital beds evaluated in this study, countries may differ in their interpretation and reporting. For example, although the U.K. has a clear definition of ICU beds describing level three care with advanced respiratory support or at least two organ systems involved, the U.S. definition is less clear.11 Therefore, this lack of standardization in terminology may cause certain trends observed in this study to be overreported or underreported. Second, our study utilized global data that was reliant on countries submitting accurate reports of COVID cases and mortality to organizations such as WHO. Therefore, variation in reporting practices between countries may cause our analysis to be overestimated or underestimated. Finally, due to lack of available information, adjusting for potential ICU, ACB, and HB capacity expansion that many countries, including the U.S. and Spain, have resorted to during the COVID-19 pandemic was not possible and should be accounted for in future analyses.48
We offer several recommendations for moving forward. Bed capacity data for all categories evaluated in this analysis was not publicly available for all countries; we recommend the implementation of mandatory bed capacity and occupancy reporting to organizations such as WHO. Similarly, we recommend for hospitals to collect and synthesize information regarding coronavirus patient clinical and demographic variables in order to allow for these factors to be controlled for in future analyses that examine bed capacity in relation to patient outcomes. Additionally, it is of paramount importance that physicians, hospital administration, official health organizations, and government bodies cooperate and implement interventional strategies aimed at expanding hospital bed capacity and critical resources as countries experience a resurgence of coronavirus cases. Implementation of a tiered critical care surge strategy may have the potential to compensate for obstacles that bottleneck the ability of healthcare workers to deliver care. For example, the expansion of ICU bed capacity by transferring floor patients to alternate locations (e.g.., university dorms, hotels, etc.) may serve to increase the capacity to accommodate additional patients in a critical state.49 Additionally, increasing the ventilator/respiratory therapist (RT) ratio may maximize healthcare delivery. With a shortage of RTs implicated as a major concern in the future, it is important to have their expertise.5 , 49 Adherence to these strategies in combination with an adequate supply of healthcare resources may serve to maximize hospital capabilities and quality of care provided to COVID and non-COVID patients alike.
Conclusion
Global COVID-19 mortality rates are likely affected by numerous factors, including ICU, acute care, and hospital bed capacity, critical care resources, and personnel, among others. Higher income regions of the world have been shown to have a greater number of acute care, ICU, and hospital bed capacities compared to lower income regions. Mandatory reporting of ICU, acute care, and hospital bed capacity/occupancy, as well as accurate coronavirus cases/mortality, should be implemented on a global scale and made publicly available in order to rapidly identify areas for intervention. Additionally, implementation of a tiered critical care staffing could maximize healthcare delivery in spite of healthcare staffing shortages and minimize the burden a resurgence in COVID-19 cases can have on hospital resources and provide the highest quality patient care possible.
Acknowledgment
Authors’ contribution: Study design and conception: Elkbuli, Data collection, analysis, and interpretation: Sen-Crowe, Sutherland, Elkbuli, Drafting of the manuscript: Sen-Crowe, Sutherland, Elkbuli, Critical revisions of the manuscript: Elkbuli, Sutherland, Sen-Crowe, McKenney, All authors approve the final version.
Funding: None.
Conflict of interests: authors declare no competing interests.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jss.2020.11.062.
Disclosure
The authors reported no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Supplementary data
References
- 1.COVID-19 map. Johns Hopkins Coronavirus Resource Center. 2020. https://coronavirus.jhu.edu/map.html Available at:
- 2.Shoukat A., Wells C.R., Langley J.M., Singer B.H., Galvani A.P., Moghadas S.M. Projecting demand for critical care beds during COVID-19 outbreaks in Canada. CMAJ. 2020;192:E489–E496. doi: 10.1503/cmaj.200457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li R., Rivers C., Tan Q., Murray M.B., Toner E., Lipsitch M. Estimated demand for US hospital inpatient and intensive care unit beds for patients with COVID-19 based on comparisons with Wuhan and Guangzhou, China. JAMA Netw Open. 2020;3:e208297. doi: 10.1001/jamanetworkopen.2020.8297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barrett K., Khan Y.A., Mac S., Ximenes R., Naimark D.M.J., Sander B. Estimation of COVID-19-induced depletion of hospital resources in Ontario, Canada. CMAJ. 2020;192:E640–E646. doi: 10.1503/cmaj.200715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ventilator Stockpiling and availability in the US. Johns Hopkins Center for Health Security; 2020. https://www.centerforhealthsecurity.org/resources/COVID-19/COVID-19-fact-sheets/200214-VentilatorAvailability-factsheet.pdf Available at: [Google Scholar]
- 6.Strategies to mitigate healthcare personnel staffing shortages. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/mitigating-staff-shortages.html Available at: [Google Scholar]
- 7.Strategies to optimize the supply of PPE and equipment. Centers for Disease Control and Prevention; 2020. https://www.cdc.gov/coronavirus/2019-ncov/hcp/ppe-strategy/index.html Available at: [Google Scholar]
- 8.Maves R.C., Downar J., Dichter J.R. Triage of scarce critical care resources in COVID-19 an implementation Guide for regional allocation: an expert panel report of the Task force for mass critical care and the American college of chest physicians. Chest. 2020;158:212–225. doi: 10.1016/j.chest.2020.03.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.COVID-19 projections. Institute for Health and Evaluation. https://covid19.healthdata.org/united-states-of-america Available at:
- 10.Coronavirus disease (COVID-19). World Health Organization. https://www.who.int/docs/default-source/coronaviruse/situation-reports/20201005-weekly-epi-update-8.pdf Available at:
- 11.The World Bank The World by Income and Region. https://datatopics.worldbank.org/world-development-indicators/the-world-by-income-and-region.html Available at:
- 12.The World Bank World Bank Country and Lending Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups Available at:
- 13.Wunsch H. Chapter 76: ICU Bed Utilization. In: Critical Care. McGraw-Hill Education. Available at: https://accessanesthesiology.mhmedical.com/content.aspx?bookid=1944§ionid=143521546. Accessed 11 October 2020.
- 14.Hospital Bed Density. Central Intelligence Agency. https://www.cia.gov/library/publications/the-world-factbook/fields/360.html Available at:
- 15.Acute care hospital beds per 100,000. World Health Organization – Europe. https://gateway.euro.who.int/en/indicators/hfa_478-5060-acute-care-hospital-beds-per-100-000/visualizations/#id=20057&tab=table Available at:
- 16.Updates on COVID-19 in Republic of Korea 4 October 2020. Korean Centers for Disease Control and Prevention; 2020. https://www.cdc.go.kr/board/board.es?mid=a30402000000&bid=0030 Available at: [Google Scholar]
- 17.CECC confirms 1 more COVID-19 case; female found to have COVID-19 after returning to Taiwan from Philippines. Taiwan Centers Dis Control. 2020 https://www.cdc.gov.tw/En/Bulletin/Detail/ddTptredDOWgUmWIismXaw?typeid=158 Available at: [Google Scholar]
- 18.Hospital Beds The World Bank. https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?end=2015&start=2015&view=bar Available at:
- 19.Halpern N., Tan K.U.S. 2020. ICU resource availability for COVID-19. Society of critical care medicine.https://sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-US Available at: [Google Scholar]
- 20.Mandeville K. 2020. Tajikistan emergency COVID-19 project.http://documents.worldbank.org/curated/en/274761585067722387/pdf/Project-Information-Document-Tajikistan-Emergency-COVID-19-Project-P173765.pdf Available at: [Google Scholar]
- 21.Murthy S., Leligdowicz A., Adhikari N.K. Intensive care unit capacity in low-income countries: a systematic review. PLoS One. 2015;10:e0116949. doi: 10.1371/journal.pone.0116949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jayaram R., Ramakrishnan N. Cost of intensive care in India. Indian J Crit Care Med. 2008;12:55–61. doi: 10.4103/0972-5229.42558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Prin M., Wunsch H. International comparisons of intensive care: informing outcomes and improving standards. Curr Opin Crit Care. 2012;18:700–706. doi: 10.1097/MCC.0b013e32835914d5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Phu V.D., Wertheim H.F., Larsson M. Burden of hospital acquired infections and antimicrobial use in Vietnamese adult intensive care units. PLoS One. 2016;11:e0147544. doi: 10.1371/journal.pone.0147544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Caring for Cambodia - Royal phnom penh hospital. Bangkok Hosp. 2017. https://www.bangkokhospital.com/en/royal-phnom-penh-hospital Available at:
- 26.Fabre-Teste B., Sokha O. Hôpital Calmette, Phnom Penh, Cambodge. Bilan de la mise en place du système d’information médicale (SIM). Analyse globale des données de 1998. Cah d’études Rech Francoph Santé. 2000;9:367–375. [PubMed] [Google Scholar]
- 27.Morestin S., Lesbre J.P., Grinda J.M., Deloche A. Bilan de 17 mois d'activité chirurgicale au Centre de cardiologie de Phnom-Penh [Results of 17 months' surgical experience in the Cardiological Centre of Phnom-Penh (CCPP). The challenge of sanitation in a developing country] Arch Mal Coeur Vaiss. 2004;97:285–290. [PubMed] [Google Scholar]
- 28.Çeliker M.Y., Pagnarith Y., Akao K., Sophearin D., Sorn S. Pediatric palliative care initiative in Cambodia. Front Public Health. 2017;5:185. doi: 10.3389/fpubh.2017.00185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Central hospital. 2020. http://www.central-hospital.com/ch/aboutus Available at: [Google Scholar]
- 30.Argenziano M.G., Bruce S.L., Slater C.L. Characterization and clinical course of 1000 Patients with COVID-19 in New York: retrospective case series. Medrxiv. 2020:2020. doi: 10.1136/bmj.m1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Outcomes from intensive care in patients with COVID-19: a systematic review and meta-analysis of observational studies. Anaesthesia. 2020;75:1340–1349. doi: 10.1111/anae.15201. [DOI] [PubMed] [Google Scholar]
- 32.Grasselli G., Greco M., Zanella A. Risk factors associated with mortality among patients with COVID-19 in intensive care units in lombardy, Italy. JAMA Intern Med. 2020;180:1–11. doi: 10.1001/jamainternmed.2020.3539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wang Y., Lu X., Li Y. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430–1434. doi: 10.1164/rccm.202003-0736LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moiseev S., Avdeev S., Brovko M., Bulanov N., Tao E., Fomin V. Outcomes of intensive care unit patients with COVID-19: a nationwide analysis in Russia. Anaesthesia. 2020;75:1–2. doi: 10.1111/anae.15265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Severe outcomes among patients with coronavirus disease 2019 (COVID-19) – United States, february 12-march16,2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Peters D.H., Garg A., Bloom G., Walker D.G., Brieger W.R., Rahman M.H. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136:161–171. doi: 10.1196/annals.1425.011. [DOI] [PubMed] [Google Scholar]
- 37.Ma X., Vervoort D. Critical care capacity during the COVID-19 pandemic: global availability of intensive care beds. J Crit Care. 2020;58:96–97. doi: 10.1016/j.jcrc.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ranney M.L., Griffeth V., Jha A.K. Critical supply shortages - the need for ventilators and personal protective equipment during the covid-19 pandemic. N Engl J Med. 2020;382:e41. doi: 10.1056/NEJMp2006141. [DOI] [PubMed] [Google Scholar]
- 39.Shilling F. Road Ecology Center – University of California Davis; 2020. Special Report 3: Impact of COVID19 Mitigation on Traffic, Fuel Use, and Climate Change.https://roadecology.ucdavis.edu/files/content/projects/COVID_CHIPs_Impacts_updated_430_1.pdf Available at: [Google Scholar]
- 40.Sutherland M., McKenney M., Elkbuli A. Vehicle related injury patterns during the COVID-19 pandemic: what has changed? Am J Emerg Med. 2020;38:1710–1714. doi: 10.1016/j.ajem.2020.06.006. [DOI] [PubMed] [Google Scholar]
- 41.NYPD announces citywide crime statistics for March 2020. New York Police Department; 2020. https://www1.nyc.gov/site/nypd/news/p0402b/nypd-citywide-crime-statistics-march-2020 Available at: [Google Scholar]
- 42.Report covering Week of 23-Mar-20 through 29-Mar-20. Chicago Police Department; 2020. https://www.civicfed.org/sites/default/files/cpd_crime_statistics_march_23-29.pdf Available at: [Google Scholar]
- 43.Sutherland M., McKenney M., Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York city, chicago, los angeles and Baltimore [published online ahead of print, 2020 may 7] Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Woolf S.H., Chapman D.A., Sabo R.T., Weinberger D.M., Hill L. Excess deaths from COVID-19 and other causes, march-april 2020. JAMA. 2020;217:15–17. doi: 10.1001/jama.2020.11787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xu S., Li Y. Beware of the second wave of COVID-19. Lancet. 2020;395:1321–1322. doi: 10.1016/S0140-6736(20)30845-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The flu season. Cent Dis Prev Control. 2018. https://www.cdc.gov/flu/about/season/flu-season.htm Available at:
- 47.Bloom J.A., Foroutanjazi S., Chatterjee A. The impact of hospital bed density on the COVID-19 case fatality rate in the United States. Am Surg. 2020:1–2. doi: 10.1177/0003134820939909. [DOI] [PubMed] [Google Scholar]
- 48.Arango C. Lessons learned from the coronavirus health crisis in madrid, Spain: How COVID-19 has changed our lives in the last 2 weeks [published online ahead of print, 2020 apr 8] Biol Psychiatry. 2020;88:e33–e34. doi: 10.1016/j.biopsych.2020.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chan W., Al-Ibrahim H., Cutter C., Patel K., Bogart A. RAND Corporation; 2020. Critical care surge response strategies for the 2020 COVID-19 outbreak in the United States.https://www.rand.org/pubs/research_reports/RRA164-1.html Available at: [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.