Abstract
Background
The ongoing COVID-19 pandemic strains the medical system, limiting access to healthcare services. Many people use cannabis medically for chronic health conditions and as a substitute for other medications. As such, changes in cannabis access associated with COVID-19 may result in increased non-cannabis drug use.
Methods
We recruited N = 353 individuals through Amazon Mechanical Turk who reported current medical cannabis use in April and May of 2020. We assessed the effects of the COVID-19 pandemic on patterns of medication and substance use, as well as on cannabis use patterns.
Results
Over half of participants either started using or increased use of medications or substances because of the COVID-19 pandemic, most commonly alcohol and sleep aids. Over a third of participants increased cannabis use while 25% decreased cannabis use. Approximately 40% of participants who increased or started use of medications/substances (other than cannabis) reported doing so because of changed access to medical cannabis.
Conclusion
The reported increase in drug use among people using medical cannabis is concerning. Because the pandemic will likely continue for months (or even years), having a better understanding of why this is occurring is critical for developing effective harm-reduction strategies in this population.
Keywords: Medical cannabis, Alcohol, Drug use, Covid-19, Substitution
Introduction
Severe acute respiratory syndrome coronavirus 2 (hereafter COVID-19) has caused >9.4 million infections and >232,000 deaths in the US as of November 4th, 2020.(Times, 2020) State governments have enforced social distancing, quarantine, and shelter-in-place policies, thereby sequestering communities and limiting access to medical care. Although critical for protecting public health, such policies have psychological consequences, including fear, anxiety, depression, and post-traumatic stress symptoms.(Brooks et al., 2020; Gan et al., 2020) Further, inability to access healthcare may exacerbate chronic disease symptoms.
People using cannabis medically represent one potentially vulnerable population, as many use cannabis for chronic conditions such as chronic pain, cancer, and multiple sclerosis.(Boehnke, Gangopadhyay, Clauw & Haffajee, 2019) Although cannabis remains Schedule I under the Controlled Substances Act, use of cannabis medically has increased nationwide – even in states without legal cannabis.(Han, Compton, Blanco & Jones, 2018) Of thirty-three states allowing medical cannabis, only twenty-three have designated cannabis businesses as essential, allowing them to stay open during shelter-in-place orders.(Booker, 2020) This disruption in cannabis access may potentially cause negative health effects for people using cannabis medically through anxiety about cannabis access, symptom flares, and changes in substance use to compensate for the lack of cannabis. For example, some people intentionally substitute cannabis for other medications due to better symptom management and a favorable side effect profile,(Boehnke et al., 2019; Lucas, Baron & Jikomes, 2019) so some may re-initiate or increase use of other medications due to decreased cannabis access. Alternately, studies show that individuals using medical cannabis report greater use/misuse of prescription drugs and alcohol than those who do not.(Campbell et al., 2018; Caputi & Humphreys, 2018; Wall, Liu, Hasin, Blanco & Olfson, 2019) This population may thus be at particular risk of increasing substance use to cope with COVID-19-related stressors and lockdown/quarantine policies.
We sought to understand how people using cannabis medically are affected by COVID-19, with specific focus on cannabis access and use of other medications and substances (e.g., alcohol, tobacco). We hypothesized that concern about/decreased access to cannabis would be associated with increased use of medications and substances.
Methods
Participants and recruitment
We recruited US-based participants using Amazon Mechanical Turk via Cloud Research(Chandler, Rosenzweig, Moss, Robinson & Litman, 2019) in April-May 2020. All responses were anonymized. Participants first completed a screener survey (<1 min, $0.01 compensation) containing an attention check, distraction questions, and a query about current cannabis use (never used, recreationally only, medically only, combination of medically and recreationally). N = 2897 participants completed the screener. Those who passed the attention check and currently used cannabis medically or medically and recreationally were invited to participate in the full survey (~5 min, $0.50 compensation). After removing 135 responses that failed attention checks, indicated that they did not use cannabis medically, or were not >18 years, 353 eligible responses remained. All procedures were approved as an exempt study (HUM00180360) at the University of Michigan.
Measures
Demographics
We collected participant gender, age, education level, household income, state, and medical cannabis license status. Participants selected their primary condition/symptom for using cannabis. Participants rated their physical health and mental/emotional health (responses: poor through excellent).
COVID-19 related measures
Participants indicated whether they were currently under a shelter-in-place order (responses: yes, no, and don't know) and whether they thought cannabis businesses should be allowed to stay open during the pandemic (responses: yes/no).
Cannabis access
Participants selected their level of concern that COVID-19 might affect their access to cannabis (responses: not concerned at all to extremely concerned). We also asked where participants typically purchased cannabis, and whether participants had purchased more cannabis than usual in case of COVID-19-related lapses in access (responses: yes/no).
Cannabis use
Items assessed how frequently participants used cannabis, and whether use frequency had changed since COVID-19 (responses: stopped use through increased a lot). Those who changed use frequency were asked why, selecting all that apply from the following responses: anxiety, boredom, cannabis products less available, fewer responsibilities, increased symptom burden, financial concerns, less stressed or anxious, and other. We asked how participants’ ability to manage their condition/symptom with cannabis had changed due to COVID-19, (responses: very negatively impacted through very positively impacted).
Use of other medications and substances
We asked whether participants had started or increased use of medications/substances due to COVID-19, with a list including common prescription/over-the-counter medication classes, and substances (e.g., tobacco, alcohol). Those who indicated starting/increasing use were asked whether this was in response to changes in cannabis availability.
Statistical analyses
Descriptive analyses included frequencies and means, with selections of subgroups as appropriate. Chi-square tests examined differences in rationale for increasing or decreasing cannabis use. Independent samples t-tests examined whether starting/increasing drug use was related to cannabis access concerns, cannabis use frequency, physical health, and mental/emotional health.
Results
Participants (N = 353, Table 1 ) were from 44 states and Washington, DC, with the highest proportions from California (14%), Pennsylvania (8%), Florida (7%), and New York (7%). Ninety-two percent reported current shelter-in-place policies. Consistent with a nationally representative sample of people using medical cannabis,(Lin, Ilgen, Jannausch & Bohnert, 2016) approximately one-third of participants rated their emotional and physical health as poor/fair, one-third good, and one-third very good/excellent (Table 1). Most (75%) participants used cannabis both medically and recreationally, a proportion similar to that reported among people using cannabis medically vs. medically and recreationally in nationally representative data.(Wall et al., 2019) While there were no significant demographic differences between participants with and without legal access to cannabis, those using cannabis medically were significantly older, had more education, and reported worse physical health than those using medically and recreationally.
Table 1.
Participant Demographics (N = 353).
| Descriptive | Total | Recreational Use? | Legal Access? | ||
|---|---|---|---|---|---|
| Yes | No | Yes | No | ||
| Gender (n = 353) | |||||
| Women | 55.5% | 53.4% | 62.9% | 54.5% | 57.6% |
| Men | 43.9% | 45.9% | 37.9% | 45.1% | 41.5% |
| Other | 0.6% | 0.8% | 0% | 0.4% | 0.8% |
| Age in years (Mean, SD, range)* | 37, 11, 20–78 | 35, 10, 20–78 | 43, 12, 22–78 | 37, 12, 20–78 | 37, 10, 20–63 |
| Education (n = 353)* | |||||
| High school graduate, GED, or less | 10.0% | 11.0% | 6.9% | 8.4% | 10.6% |
| Some college or associate's degree | 39.4% | 42.9% | 28.7% | 45.8% | 36.2% |
| Bachelor's Degree | 36.3% | 34.6% | 41.4% | 34.7% | 37.0% |
| Master's, Doctorate or Professional Degree | 12.5% | 10.2% | 19.5% | 10.2% | 13.7% |
| Other | 2.0% | 1.5% | 3.4% | 0.8% | 2.6% |
| Currently a student (n = 47) | 13.3% | 13.9% | 11.5% | 13.2% | 13.6% |
| Annual household income in 2019 (n = 352) | |||||
| $50,000 or less | 50.6% | 50.3% | 51.1% | 50.6% | 50.4% |
| $50,001-$100,000 | 35.0% | 37.2% | 27.9% | 34.1% | 36.8% |
| $100,001-$150,000 | 9.4% | 8.3% | 12.8% | 9.8% | 8.5% |
| More than $150,000 | 5.1% | 4.1% | 8.1% | 5.5% | 4.3% |
| Races/ethnicities (inclusive) (n = 353) | |||||
| White | 80.2% | 80.1% | 80.5% | 77.0% | 86.4% |
| Asian | 7.6% | 8.3% | 5.7% | 8.9% | 5.1% |
| Hispanic/Latino | 7.4% | 8.6% | 3.4% | 8.1% | 5.9% |
| Black/African American | 7.1% | 6.4% | 9.2% | 7.2% | 6.8% |
| American Indian or Alaska Native | 3.7% | 4.1% | 2.3% | 3.4% | 4.2% |
| Native Hawaiian/Pacific Islander | 0.6% | 0.4% | 1.1% | 0.9% | 0% |
| Other | 0.6% | 0.8% | 0% | 0.9% | 0% |
| Physical Health (n = 353)* | |||||
| Poor | 5.9% | 6.0% | 5.7% | 6.8% | 4.2% |
| Fair | 25.2% | 21.1% | 37.9% | 24.3% | 27.1% |
| Good | 34.8% | 36.1% | 31.0% | 34.9% | 34.7% |
| Very good | 26.9% | 28.6% | 21.8% | 27.2% | 26.3% |
| Excellent | 7.1% | 8.3% | 3.4% | 6.8% | 7.6% |
| Mental or emotional health (n = 353) | |||||
| Poor | 10.5% | 11.7% | 6.9% | 9.4% | 12.7% |
| Fair | 28.6% | 27.4% | 32.2% | 28.1% | 29.7% |
| Good | 35.1% | 34.6% | 36.8% | 37.0% | 31.4% |
| Very good | 17.6% | 16.9% | 19.5% | 18.3% | 16.1% |
| Excellent | 8.2% | 9.4% | 4.6% | 7.2% | 10.2% |
Indicates significant differences (p<0.05) between participants using medically only and those using a combination of medically and recreationally.
Congruent with other studies,(Lucas et al., 2019) cannabis was most commonly used for mood/stress symptoms (38%) and chronic pain (32%). Forty-nine percent used cannabis daily or more frequently. Two-thirds had access to legal cannabis, and 48% had medical cannabis licenses. Most (84%) participants with legal access obtained cannabis through state-licensed dispensaries. Participants without legal access (33%) typically obtained cannabis from a friend (83%). Most participants (95%) thought cannabis dispensaries should be allowed to remain open during the pandemic.
Effects of COVID-19 on medical cannabis access and use
Nearly half (49%) of participants were moderately, very, or extremely concerned that the COVID-19 pandemic would affect medical cannabis access. Despite concerns about decreased access, only 25% decreased use, whereas 35% increased use and 40% had no change. This may be due to 56% of overall participants purchasing more cannabis than usual in case of a lapse in cannabis access. Participants without access to legal cannabis were more likely to report decreased cannabis availability, t(351)=3.19, p = 0.002, d = 0.36 as well as decreased frequency of cannabis use (t(351)=2.16, p = 0.032, d = 0.24) than those with legal cannabis access.
Those who decreased cannabis use did so because cannabis products were less available (67%), anxiety about COVID-19 (26%), and fewer responsibilities (18%). Those who increased cannabis use did so because of anxiety about COVID-19 (68%), boredom (47%), and increased symptom burden (42%). Thirty percent reported that COVID-19 had negatively affected their ability to manage their medical condition vs. 16% reporting positive effects and 54% no change.
Increases in medication and substance use
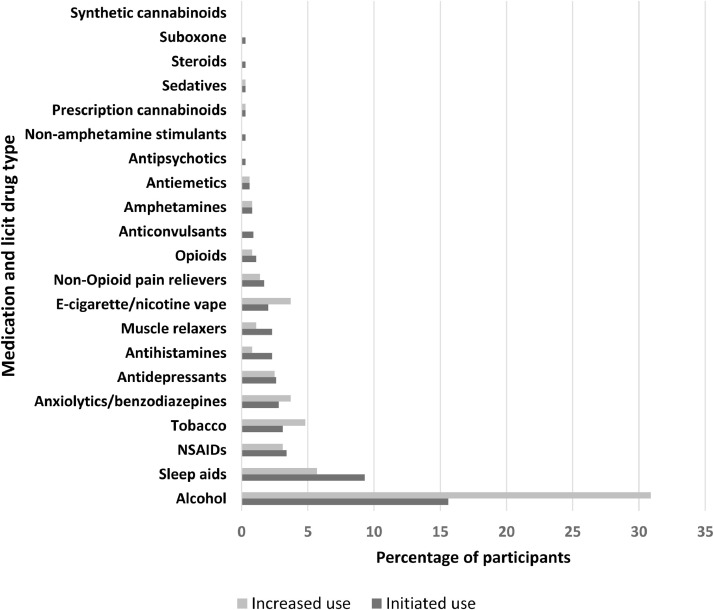
Overall, 52% (n = 185) of participants reported increasing or starting use of a medication/substance, with 28% (n = 97) both increasing/starting use. Thirty-two percent (n = 114) reported starting use of a medication/substance, and 12% reported started using multiple medications/substances. Similarly, 48% (n = 168) of participants increased use of medications/substances because of COVID-19, with 11% increased use of multiple medications/substances. Alcohol was the substance most commonly started (16%, n = 55) or increased (31%, n = 109) (Fig. 1 ). Those starting medications/substances had a higher level of education, t(351)=3.73, p<0.001, d = 0.43 were younger, t(351)=2.02, p = 0.044, d = 0.22, and reported worse mental/emotional health, t(351)= 2.2, p = 0.025, d = 0.24. No differences in increased/started substance use were seen between individuals using cannabis medically alone vs. medically and recreationally, nor between those in states with and without legal cannabis.
Fig. 1.
Percentage of participants who indicated that they had started or started use of medications (prescription or over the counter) and substances as a result of the COVID-19 pandemic. Overall, 32.3% started use of a drug, and 47.5% increased their use of a drug.
Consistent with our hypothesis, 44% of new and 43% of increased medication/substance use was attributed to changed cannabis access. Those starting medications/substances were more likely to report reduced cannabis use frequency because of COVID-19, t(351)=2.8, p = 0.005, d = 0.32, greater concern that COVID-19 would affect cannabis access, t(351)=5.9, p<0.001, d = 0.67, and lower current frequency of cannabis use, t(350)=3.1, p = 0.002, d = 0.35. Greater concern that COVID-19 would affect cannabis access was also associated with increasing medication/substance use, t(351)=2.3, p = 0.023, d = 0.24.
Discussion
Our results highlight a troubling trend: in response to the COVID-19 pandemic, >50% of people using cannabis medically report initiation or increased use of medications/substances – most commonly alcohol. Consistent with our hypotheses, some individuals (~40%) who started using or increased medication/substance use attributed those behaviors to lack of access to cannabis products. However, despite access concerns, 35% of participants increased their cannabis use (vs. 25% who decreased) to cope with anxiety, symptom flares, or boredom. Although our cross-sectional design precludes us from determining causality, several factors may be influencing these results.
First, many people report substituting cannabis for medications and substances (e.g., opioids, alcohol) due to better symptom management and fewer side effects.(Boehnke et al., 2019; Lucas et al., 2019) As some participants were more likely to report decreased cannabis use and increased substance/medication use due to access concerns, these results may indicate that people who previously substituted cannabis could no longer do so effectively and subsequently increased/re-initiated use of other substances. If true, such changes are concerning, as cannabis substitution is often done for harm-reduction reasons and cannabis has substantially lower lethal overdose risk than other substances.(Lachenmeier & Rehm, 2015) Second, medical or combined medical/recreational cannabis use has been associated with worse overall health and risky health behaviors. One recent nationally representative study showed that combined medical/recreational cannabis use (the predominant use pattern among our participants) was associated with higher rates of anxiety disorders compared to the general public.(Wall et al., 2019) This finding is congruent both with our participants using cannabis for mood/stress and also increasing cannabis use typically due to anxiety. Others have shown that people using cannabis medically report high rates of prescription drug use/misuse.(Caputi & Humphreys, 2018) Similarly, a longitudinal cohort study of individuals with chronic pain associated cannabis use with more severe clinical pain and pain interference.(Campbell et al., 2018) As such, our data may reflect polysubstance use and/or increasing substance use to cope with medical burdens. Third, it is possible that as with other populations, people using medical cannabis are subject to stressors of COVID-19 (e.g., disrupted daily routines, anxiety, lockdown(Brooks et al., 2020)), resulting in coping through medications/substances. Indeed, health research firms reported increased benzodiazepine (10–34%) and antidepressant (9.2%) prescriptions in February and March 2020.(Petersen, 2020) This increase also may be because people confined to their residence are typically in closer proximity to substances than they would be otherwise, leading to greater use. Whether these effects are magnified among people using medical cannabis remains uncertain.
Policy implications
Our cross-sectional design limits us from making definitive policy recommendations. However, our results suggest that there may be subgroups who may respond differently to COVID-19-related changes. Policies that limit access to medical cannabis products may negatively affect people using cannabis as a substitute in the harm-reduction context, pointing to the importance of maintaining a standardized and safe medical cannabis supply chain. The increase in substance use – predominantly cannabis and alcohol – highlights the need for enhanced availability of counseling services, especially in the mental health and addiction/substance abuse context. Indeed, although many people do report using cannabis for anxiety,(Boehnke et al., 2019; Lucas et al., 2019) there is limited evidence suggesting that medical cannabis (especially Δ−9-tetrahydrocannabinol-dominant products) is actually useful for anxiety,(Boehnke et al., 2019) highlighting the importance of providing other more helpful treatment options.
Limitations
Our cross-sectional design prevents us from determining causality. The majority White study population may not generalize as other populations have been disparately affected by COVID-19, both economically and physically/emotionally. We had no objective measures (e.g., urine drug screens) confirming that increased drug use had occurred. Similarly, we did not investigate whether participants had previously substituted cannabis for other substances or had substance use disorders. Finally, our US-specific findings and use of MTurk as a recruitment platform may limit the generalizability of our results to other populations.
Conclusions
The majority of people using cannabis medically reported starting or increasing substance use (most commonly alcohol) due to the COVID-19 pandemic. Approximately 40% of those who increased or started using medications/substances reported doing so because of changed access to cannabis. Whether these concerning increases are unique to people using medical cannabis or affect other populations is unknown. Better understanding why and among whom these increases are occurring is critical for developing effective harm-reduction strategies.
Declarations of Interest
Drs. McAfee, Ackerman, and Kruger declare no conflicts of interest. Dr. Boehnke currently sits on a data safety monitoring board for an ongoing study with Vireo Health (unpaid). The cost of this research was covered by discretionary funds from the Chronic Pain and Fatigue Research Center.
Footnotes
Ethics statement: All surveys and procedures were approved as an exempt study as study HUM00180360 under IRBHSBS at the University of Michigan.
References
- Boehnke K.F., Gangopadhyay S., Clauw D.J., Haffajee R.L. Qualifying conditions of medical cannabis license holders in the United States. Health Affairs (Project Hope) 2019;38(2):295–302. doi: 10.1377/hlthaff.2018.05266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boehnke K.F., Scott J.R., Litinas E., Sisley S., Williams D.A., Clauw D.J. Pills to pot: Observational analyses of cannabis substitution among medical cannabis users with chronic pain. The Journal of Pain : Official Journal of the American Pain Society. 2019;20(7):830–841. doi: 10.1016/j.jpain.2019.01.010. [DOI] [PubMed] [Google Scholar]
- Booker, B. (2020). 'Illegal to essential': How the coronavirus is boosting the legal cannabis industry. Retrieved from https://www.npr.org/2020/04/20/831861961/illegal-to-essential-how-coronavirus-is-boosting-the-legal-cannabis-industry.
- Brooks S.K., Webster R.K., Smith L.E., Woodland L., Wessely S., Greenberg N., & Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. The Lancet. 2020;395(10227):912–920. doi: 10.1016/s0140-6736(20)30460-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell G., Hall W.D., Peacock A., Lintzeris N., Bruno R., Larance B. Effect of cannabis use in people with chronic non-cancer pain prescribed opioids: Findings from a 4-year prospective cohort study. The Lancet Public Health. 2018;3(7):e341–e350. doi: 10.1016/s2468-2667(18)30110-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caputi T.L., Humphreys K. Medical marijuana users are more likely to use prescription drugs medically and nonmedically. Journal of Addiction Medicine. 2018;12(4):295–299. doi: 10.1097/ADM.0000000000000405. [DOI] [PubMed] [Google Scholar]
- Chandler J., Rosenzweig C., Moss A.J., Robinson J., Litman L. Online panels in social science research: Expanding sampling methods beyond Mechanical Turk. Behavior Research Methods. 2019;51(5):2022–2038. doi: 10.3758/s13428-019-01273-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gan Y., Ma J., Wu J., Chen Y., Zhu H., Hall B.J. Immediate and delayed psychological effects of province-wide lockdown and personal quarantine during the COVID-19 outbreak in China. Psychological Medicine. 2020:1–12. doi: 10.1017/S0033291720003116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han B., Compton W.M., Blanco C., Jones C.M. Trends in and correlates of medical marijuana use among adults in the United States. Drug and Alcohol Dependence. 2018;186(January):120–129. doi: 10.1016/j.drugalcdep.2018.01.022. [DOI] [PubMed] [Google Scholar]
- Lachenmeier D.W., Rehm J. Comparative risk assessment of alcohol, tobacco, cannabis and other illicit drugs using the margin of exposure approach. Scientific Reports. 2015;5:8126. doi: 10.1038/srep08126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin L.A., Ilgen M.A., Jannausch M., Bohnert K.M. Comparing adults who use cannabis medically with those who use recreationally: Results from a national sample. Addictive Behaviors. 2016;61:99–103. doi: 10.1016/j.addbeh.2016.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lucas P., Baron E.P., Jikomes N. Medical cannabis patterns of use and substitution for opioids & other pharmaceutical drugs, alcohol, tobacco, and illicit substances; results from a cross-sectional survey of authorized patients. Harm Reduction Journal. 2019;16(1):9. doi: 10.1186/s12954-019-0278-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petersen, A. (2020). More people are taking drugs for anxiety and insomnia, and doctors are worried. Retrieved from https://www.wsj.com/articles/more-people-are-taking-drugs-for-anxiety-and-insomnia-and-doctors-are-worried-11590411600.
- Times, T.N.Y. (Producer). (2020 , Nov 4, 2020). Coronavirus in the U.S.: Latest Map and Case Count. Retrieved from https://www.nytimes.com/interactive/2020/us/coronavirus-us-cases.html.
- Wall M.M., Liu J., Hasin D.S., Blanco C., Olfson M. Use of marijuana exclusively for medical purposes. Drug Alcohol Depend. 2019;195:13–15. doi: 10.1016/j.drugalcdep.2018.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]