ABSTRACT
Objective:
To provide dentists and dental team with insights concerning risk and precautions during COVID-19 outbreak crisis as it would help in decision making among dental community.
Materials and Methods:
A comprehensive review of all English and non-English articles was carried out using the available CORD-19 dataset with MEDLINE via PubMed, Cochrane library, Google Scholar and ScienceDirect databases. The study included all articles that matched the search terms.
Results:
A total of 353 were retrieved, of which 13 articles were reviewed comprehensively. Studies included in this systematic review emphasized on reinforcing strict infection control measures and minimizing human-to-human contact during COVID-19 outbreak. All surfaces in operatory room including waiting area need adequate ventilation and disinfection. Dental patients need to be screened using COVID-19 targeted questions as well as measuring their body temperature. Restricting dental treatments to only emergency cases and rescheduling all routine visits is advised with careful attention to minimize aerosol generation and following highest level of personal protection when treating COVID-19 confirmed cases. Dental offices need to establish a standard protocol of case reporting and referral to other well-prepared facilities. Lastly, online platforms are beneficial tools in providing psychological support to distressed dentists, dental team and dental patients and educating public during COVID-19 crisis.
Conclusion:
Dental team need to follow strict infection control measures and minimize aerosol generation during COVID-19 outbreak. It is the responsibility of dental care workers to keep themselves informed and ensure safety and control transmission within dental facilities. Further research is required.
KEYWORDS: Dental practice management, dentist, disease outbreaks, infection control, public health dentistry
INTRODUCTION
Rationale
In December 2019, Chinese authorities announced an emergence of severe pneumonia of unknown origin in Wuhan. This was later named COVID-19, which stands for coronavirus disease-2019.[1] This infection is caused by a virus called SARS-CoV-2 from the coronavirus family similar to Middle East respiratory syndrome coronavirus (MERS-CoV) and severe acute respiratory syndrome coronavirus (SARS-CoV), but with a higher transmissibility rate.[2] Patients with SARS-CoV-2 infection show symptoms of fever, coughing sneezing, fatigue, vomiting, and severe pneumonia.[3] Studies reported person-to-person, droplet, and aerosol transmission of 2019-nCoV.[2] In January 31, 2020, the World Health Organization (WHO) announced COVID-19 crisis as a “public health emergency of international concern.”[4] In March 11, 2020, the WHO declared the coronavirus outbreak a pandemic, with a total of (118,319) confirmed cases worldwide.[5] In the month of June 20, 2020 to be precise, the submission date of this review, the infection has affected (8,385,440) cases globally with the highest cases reported in the United States (2,149,166) followed by Brazil (955,377) with a total number of (450,686) reported deaths worldwide.[6]
This COVID-19 outbreak epidemic crisis has placed a substantial strain on the healthcare system in numerous countries.[7] Healthcare providers are struggling with the rising number of infected patients demanding hospitalization.[8] Studies are increasingly reporting 2019-nCoV cross-transmission to healthcare providers exceeding 3,387 cases with 22 confirmed deaths.[8,9] The nature of dental settings requires proximity between dentist and patient during operational work.[10] This could violate the recommended one-meter safe distance between individuals during the COVID-19 outbreak.[11] The incubation period of 2019-nCoV is up to 14 days, during which, the virus is still contagious.[12] This rings the alarm bell about possibility of asymptomatic patients visiting general dental clinic and spreading infection. Moreover, it has been reported that COVID-19 was found in silent carriers and children,[13] amongst the majority of patients in pediatric and orthodontic clinics that puts orthodontists and pediatric dentists at a great risk.
Considering the recent inception of COVID-19, the literature concerned with risk and precautions within the dental setting is limited. Furthermore, high transmissibility and pandemic nature of the disease amplifies the importance of formulating a consensus within dental community to fight this emerging threat.
OBJECTIVE
The aim of this systematic review was to provide dentists and dental auxiliary with insights regarding risk and precautions during COVID-19 crisis. This could help decision-makers in handling this pandemic infection and build consensus among dental community during the COVID-19 outbreak.
MATERIALS AND METHODS
PROTOCOL AND REGISTRATION
This systematic review was developed following The Preferred Reporting Items for Systematic Reviews and Meta Analysis (PRISMA) guidelines.[14] PROSPERO only registers systematic reviews with health-related outcomes thus, this systematic review was not eligible for registration at PROSPERO.
ELIGIBILITY CRITERIA
All publications in English and non-English languages that matched the search terms were included in this review. Considering the recent discovery and announcement of the virus in late December 2019, the search included all publications from inception up to March 19, 2020.
INFORMATION SOURCES
Studies included in this review were identified by searching the COVID-19 Open Research Dataset (CORD-19 2020),[15] which contains all COVID-19 and coronavirus-related research from PubMed, WHO, bioRxiv and medRxiv pre-prints (Update published on March 13th, 2020). An updated literature search was performed lastly on March 19th, 2020 on the following databases: WHO’s COVID-19 Research Database,[16] NIH’s LitCOVID,[17] Dimensions COVID-19 Research Export File publications,[18] MEDLINE via PubMed, Cochrane library, Google Scholar, and ScienceDirect. The search was comprehensive with no restrictions to any language. Non-English papers and abstracts were translated. The search was developed and conducted by both authors of this study.
SEARCH STRATEGY
The search strategy was designed following PICOS approach to include all studies that discuss dental considerations including risk, prevention, standard of care, and recommendations during the COVID-19 outbreak. For this, a number of search terms were used in all databases which comprised of: COVID; COVID-19; COVID-2019; 2019-nCoV; SARS-CoV-2; Corona; oral; mouth; dental; dentist; dentistry; dentition; stomatology; stomatognathic; teeth; tooth; gingiva; periodontal; periodontium; saliva; and salivary.
The main search was carried out using the COVID-19 Open Research Dataset (CORD-19 2020), which includes (29,506) research studies and was last updated on March 13, 2020. The studies included any of the following terms: oral; mouth; dental; dentist; dentistry; dentition; stomatology; stomatognathic; teeth; tooth; gingiva; periodontal; periodontium; saliva; salivary; COVID; COVID-19; COVID-2019; 2019-nCoV; SARS-CoV-2 or Corona were retrieved. Then duplicate articles were eliminated. Later, the titles of the selected articles were screened followed by reviewing the abstracts of the selected studies. This was done by two independent researchers to determine the studies’ eligibility and relevance to the research question. Lastly, all articles that were published prior to 2020 were eliminated, and the remaining articles were retrieved in full text.
STUDY SELECTION AND DATA EXTRACTION
Considering the novelty of the disease, all studies that matched the search terms were included. Studies were expected to be heterogenous, which is acceptable as the aim was to provide a comprehensive overview and answer questions related to COVID-19. The search was performed by two calibrated researchers independently, and any disagreement in data collection was resolved by consensus meeting.
RESULTS
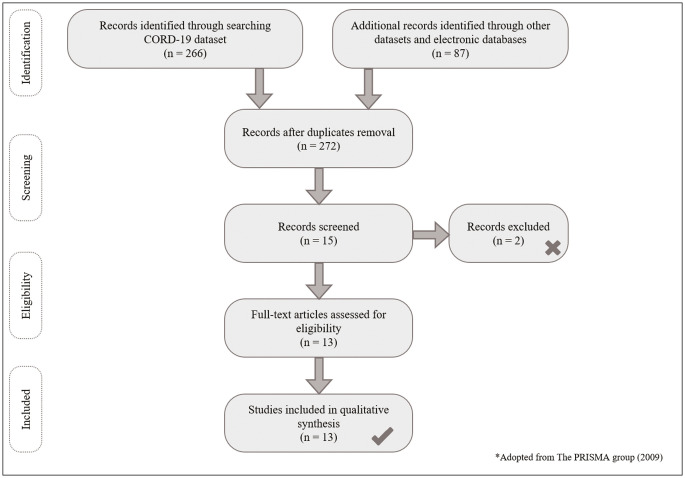
In this systematic review, a number of (353) articles were retrieved from (4) datasets and (4) different databases as follows: CORD-19, 2020 (266), WHO’s COVID-19 (56), NIH’s LitCOVID (6), Dimensions COVID-19 (16), PubMed (4), Cochrane library (0), Google Scholar (4) and ScienceDirect (1). The initial search started on March 16, 2020 and was updated on March 19, 2020. After duplicate elimination of (81) articles, titles, and abstracts of the remaining (272) articles were screened for eligibility by both researchers.
The screening process had identified (15) relevant abstracts, of those, (2) articles that did not match the scope of this systematic review and were thereafter excluded. Full texts of the remaining (13) studies were retrieved and reviewed thoroughly using PRISMA flow chart in Figure 1. Reference lists of those studies were screened further to identify possible relevant studies using snowballing method. These (13) articles were screened and divided into two groups: risk assessment group (3) articles including,[19,20,21] and recommendation group (10) articles. The recommendation group includes[1,22,23,24,25,11,26,27,28,29] [Table 1]. Lastly, recommendations were grouped into four categories: Patient’s Precautions, Dentist’s Precautions, Dental Environment and Recommendations for Decision Makers [Table 2].
Figure 1.
PRISMA flow diagram for studies selection
Table 1.
Study characteristics
| Authors | Country | Type of study | Category |
|---|---|---|---|
| Gu et al.[19] | Shanghai, China | Review | Risk assessment |
| To et al.[20] | Hong Kong, China | Clinical study | Risk assessment |
| Xu et al.[21] | Chengdu, China | In vitro study | Risk assessment |
| Ge et al.[1] | Hangzhou, China | Review | Recommendation |
| Guo et al.[22] | Beijing, China | Observational study | Recommendation |
| Li and Meng[23] | Wuhan, China | Review | Recommendation |
| Meng et al.[24] | Wuhan, China | Review | Recommendation |
| Peng et al.[25] | Chengdu, China | Review | Recommendation |
| Qu and Zhou[11] | Chengdu, china | Review | Recommendation |
| Sacsaquispe-Contreras[26] | Sheffield, UK | Review | Recommendation |
| Sabino-Silva et al.[27] | Canada, Brazil | Review | Recommendation |
| Tang et al.[28] | Nanjing, China | Review | Recommendation |
| Zhang and Jiang[29] | Shanghai, China | Review | Recommendation |
Table 2.
Study recommendations
| Authors | Patient’s precautions | Dentist’s precautions | Dental environment | Decision makers | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Screening and triage | Cases to be treated | Opera tional protocol | Psycho logical support | Dentist health | Protective measures | Dentist training | Psycho logical support | Waiting area | Air filter | Surface disinfec tion | Medical waste | Report ing system | Referral system | National restriction of clinics | Public education | |
| Ge et al.[1] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||||||||
| Guo et al.[22] | Yes | |||||||||||||||
| Li and Meng[23] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | |||||||
| Meng et al.[24] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||||||
| Peng et al.[25] | Yes | Yes | Yes | Yes | Yes | Yes | ||||||||||
| Qu and Zhou[11] | Yes | |||||||||||||||
| Sacsaquispe-Contreras[26] | Yes | Yes | Yes | Yes | Yes | |||||||||||
| Sabino-Silva et al.[27] | Yes | |||||||||||||||
| Tang et al.[28] | Yes | Yes | Yes | Yes | Yes | Yes | ||||||||||
| Zhang and Jiang[29] | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | ||||||||
RISK ASSESSMENT
Healthcare providers risk: all studies included in this systematic review have reported that dentists are at high risk due to the nature of close proximity between dentist and patient in the operational setting, which makes it difficult to maintain the recommended safely one-meter distance.[27] Meng et al.[24] reported nine confirmed cases with COVID-19 among dentists and dental team including students working in School and Hospital of Stomatology, Wuhan University (SHSWU). In addition, the virus has been found in large quantities in saliva of infected patients, which increases the risk of cross-transmission.[20,25] Xu et al.[21] reported high expression of ACE2 receptors which is the receptor for 2019-nCoV, on oral mucosa mainly on human tongue and buccal mucosa. Gu et al.[19] reported a possible oral-fecal transmission, which brings the risk even higher.[25]
Sources of transmission: COVID-19 has been reported to transmit as droplet and aerosol infection since the size of the virus is considerably large.[2] Yet, using high-speed handpiece, ultrasonic scaler and three-way syringe generates aerosol from patient’s saliva that could be mixed with blood, in the operatory room air.[1,25] This could remain in the air for some time, splash into the dentist’s eyes, which has been reported as a source of transmission,[30] and could contaminate other surfaces within the clinic.[22,29] Furthermore, talking loudly, coughing, sneezing, or gagging are other sources of transmission in addition to the human-to-human contact within the dental settings.[23,31]
Characteristics of the virus: 2019-nCoV is larger than MERS-CoV and SARS-CoV, yet it has higher transmissibility and is more contagious than both.[25,32] The incubation period ranges from 4 to 14 days and could reach up to 24 days.[9,33] This could result in some infected patients visiting the dental clinic without showing any symptoms but could still transmit the infection. Some studies reported silent COVID-19 carriers.[34] This brings the importance of following strict infection control measures during the outbreak.[1,24,25,29]
People at risk: symptoms of COVID-19 have been reported to affect elder patients more severely with reported fatality rate of 0.39% to 4.05%, depending on the geographic location in China according to Meng et al.[24] Children are less prone to infection yet they could be carriers to the disease.[25,27] This is important especially for dentists to consider while treating pediatric patients.
PATIENT’S PRECAUTIONS
Screening and triage: studies included in this review recommended screening patients before entering the dental facilities. This could be over the phone by asking COVID-19 targeted questions before any dental appointments.[11,24] It is recommended to have a screening unit to measure patients’ temperature using contact-free forehead thermometer and ask targeted questions relating to COVID-19 [Table 3].[1,24,25]
Table 3.
COVID-19 triage form
| Patient’s name and contact information: _____________________________ | |||
|---|---|---|---|
| Body temperature at initial screening: below 37.3°C equal to or above 37.3°C | |||
| Serial | Question | Yes | No |
| 1 | Body temperature at initial screening and triage equal to or higher than 37.3oC | ||
| 2 | Do you have fever or had fever within the past 14 days? | ||
| 3 | Did you use any antipyretic medication? | ||
| 4 | Do you have any symptoms of lower respiratory tract infection as cough or dyspnea “difficulty breathing” or had any within the past 14 days? | ||
| 5 | Have you traveled or visited a neighborhood with documented COVID-19 epidemics? | ||
| 6 | Have you come into close contact with a patient confirmed with COVID-19 within the past 14 days? | ||
| 7 | Have you come into close contact with someone who traveled or was in a neighborhood of a COVID-19 epidemic area, who later started developing fever of lower respiratory tract infection within the past 14 days? | ||
| 8 | Have you recently participated in any meeting or gathering with a large group of people, or had close contact with many unacquainted people? | ||
| Criteria | Action needed |
| * Postpone all routine dental care | |
| If all answers are NO (patient is unsuspected asymptomatic) | Perform only ER dental care |
| If answers NO to all questions from 1–4 and the body temperature at initial screening is below 37.3oC, AND answers YES to any question from 5–8 (patient is suspected asymptomatic) | Reschedule appointment after 14 days and ask patient to self-quarantine at home for 14 days. |
| If answers YES to any questions from 1–4 OR the body temperature at initial screening equals to or higher than 37.3oC (patient is suspected symptomatic) | Give the patient mask, register information, refer to hospital and apply strict measures. |
| Confirmed COVID-19 patients | Treat dental ER only with strict infection control measures using highest level of personal protection |
a. Unsuspected asymptomatic patients: treat only ER following a standard regime.
b. Suspected asymptomatic patients: reschedule appointment and instruct to self-quarantine at home for 14 days.
c. Suspected symptomatic or body temperature higher than 37.3oC: register patient information, refer to hospital, and clean reception area ASAP. In case of dental ER, follow the highest level of personal protection.
d. COVID-19 confirmed patients: treat only ER and follow the highest level of personal protection.
Zhang and Jiang[29] recommended triage personnel to follow grade-1 medical protection in addition to wearing goggles and gowns.
2. Cases to be treated during the outbreak: Guo et al.[22] reported a 38% reduction in cases seeking dental treatment during Wuhan outbreak. The main cases were pulpal infection 56.1% followed by abscess and oral infection, then trauma. All studies have recommended limiting dental care to ER cases only and rescheduling routine visits after the outbreak. Palliative treatment is preferred over regular appointment during the outbreak.[22,24]
3. Operational protocol: Ge et al.[1] recommended using 0.12% Chlorhexidine (CHX) mouthwash prior to any dental procedure to reduce the number of microorganisms within the oral cavity. However, Peng et al.[25] recommended using 1% hydrogen peroxide or 0.2% povidone, while Li and Meng[23] recommended using mouthwash containing povidone iodine (1%), cetylpyridinium chloride (0.05% ~ 0.10%) or essential oil components. Rubber dam isolation is essential to reduce the risk of cross-transmission through saliva.[24] According to Peng et al.,[25] antiretraction handpiece is preferred over regular ones yet, any splash or aerosol forming procedure using handpiece, ultrasonic scaler or water coolant are preferably avoided.[1,25] Ge et al.[1] and Meng et al.[24] recommended using chemomechanical caries removal or a traumatic restorative technique (ART) with rubber dam instead of rotary instruments. Manual scaling is preferred over ultrasonic instrument. Minimizing gagging reflex with suction tip or impression tray, and disinfecting prosthesis and impression after removal from patient’s mouth is advised. Dental extraction should be performed while the patient is on supine position to avoid operating on the patient’s breath way. Endodontic treatment requires rubber dam with efforts to reduce unnecessary contact with other objects or equipment. Panoramic radiographs and CBCT are preferred over intraoral radiographs that could result in oral mucosal irritation and over excretion of saliva and in turn, increases susceptibility of infection. It is recommended to use a single clinic, with limited number of patients, and any suspected case that needs urgent treatment is advised to be treated on the last appointment of the day.[1,24]
4. Psychological support: Qu and Zhou[11] discussed in their review the possible effects of psychological COVID-19 related distress on oral mucosal disease and oral psychosomatic disorders. Susceptible patients are prone to TMD, periodontal disease, recurrence of aphthous ulcers and lichen planus. They recommended replacing on site diagnosis with remote consultations as well as focusing on providing psychological stress relief rather than regular operational methods. Meng et al.[24] reported provision of more than 1,600 consultations to dental patients through SHSWU online platform.
DENTIST’S PRECAUTIONS
Dentist’s general health: it is important during the outbreak for dentists to remain safe. Sacsaquispe-Contreras[26] is recommended for dentists to measure their daily temperature and remain home if they feel ill. If a dentist encounters a confirmed COVID-19 patient, and started feeling symptoms, it is forbidden to work and spread infection, and thus, self-quarantine at home for 14 days is recommended. Coughing and sneezing should be covered with tissues that is discarded immediately with careful attention to avoid touching the eyes, mouth and nose with unwashed hands.[24,29]
Protective measures: all studies have stressed on the importance of hand hygiene in controlling disease transmission. Hands should be washed thoroughly before and after contact with every patient.[25] Personal Protective Equipment (PPE) including gowns is recommended during treatment of all patients. Wearing surgical mask is the standard, yet particulate respirator such as N95, EU FFP2, or equivalent is required while performing aerosol generating procedures. A higher-level respirator such as EU FFP3 conforming to European Standard 149 (EN149) is recommended when treating COVID-19 suspected patients.[1,23,24] Sacsaquispe-Contreras[26] is recommended to replace the mask every 2 h while Zhang and Jiang[29] recommended enhanced grade-2 with non-aerosol and enhanced grade-3 with aerosol generating procedures as well as changing the mask every 4 h. Eye protection with goggles and face shield are recommended.[27,28,29]
Dentist training: it is recommended to train dentists and dental auxiliaries on infection control measures during the outbreak and follow strict protocol to control spread of the disease within the dental facility. This training could be delivered online to minimized human to human contact.[24] In addition, dentists need to be aware of the protocol to deal with different categories of patients encountered. They need to be updated on operational protocol while treating patients preferably using the 4-handed operation technique.[23,24,28,29]
Psychological support: Meng et al.[24] highlighted the importance of providing psychological support to dentists, dental students and healthcare workers during the outbreak. Increased patients’ demands, fear of the emerging disease and the amount of strict measures are collectively causing substantial distress on the dental team. In addition, the new experience of virtual learning and online education could raise additional stress to dental students.[24]
DENTAL ENVIRONMENT
Waiting area: Ge et al.[1] recommended booking fewer patients to clinic during the outbreak. Patient should keep a minimal safe one-meter distance in the waiting area. It is advisable to have hand hygiene instructions on the waiting area to educate patients. The waiting area should be adequately ventilated and cleaned at least twice a day.[1,28]
Air filter: the operational room needs to be adequately ventilated to minimize the risk of transmission within the dental facility. Air filters are recommended and the use of mechanical HVE or HEPA filters was advised by Ge et al.[1,35]
Surface disinfection: 2019-nCoV spread by aerosol and droplet could contaminate the surfaces within the dental operational room.[1] Therefore, strict cleaning protocol of the surfaces including door handles, chairs and room desks using a solution containing (62 to 71% ethanol, 0.5% hydrogen peroxide, and 0.1% sodium hypochlorite) should be followed after each patient. Zhang and Jiang[29] recommended using ultraviolet radiation to disinfect operatory room. Dental chair needs to be wiped after every patient and the operatory surfaces needs to be wiped minimally twice a day. Dentists are recommended to keep their belongings aside and refrain from using jewelry while treating confirmed cases.[1,25,29]
Medical wastes: medical wastes during COVID-19 outbreak are considered infectious medical wastes and should be handled and discarded in accordance to the Medical Waste Management Regulations in the region.[23] Peng et al.[25] and Li and Meng[23] reported using double-layer yellow anti-leakage medical waste marked with a special tag according to the Chinese regulations.
RECOMMENDATIONS FOR DECISION MAKERS
Reporting system: dental clinics need to have a standard protocol in screening patients during COVID-19.[1] They need to develop a good reporting systems and information records for easier tracking of suspected patients later.[23,25]
Referral system: dental clinics that are operating during COVID-19 outbreak are required to develop a good referral system to the hospitals for suspected and confirmed COVID-19 patients.[24,25] Even more, a good referral system needs to be coordinated between dental clinics to allow referral of suspected cases to dental facilities that are well prepared.[1,23,24,25,28]
National restriction of dental clinics: Zhang and Jiang[29]reported national restriction of dental clinics except for ER in China. This could be an essential step to control the spread of the highly transmissible COVID-19 during the outbreak.[29]
Public education: it is recommended to educate the public and potential patients through online consultation and platforms about the high transmissibility of COVID-19 and the precautions concerned with dentistry.[23] Meng et al.[24] advised moving towards online education and lectures for the dental students highlighting the rule of encouraging students to use their acquired skills in self-directed learning.[23,24,29]
DISCUSSION
As a result of the high transmissibility rate of COVID-19 and lack of unproven cure, it has been escalated as a global pandemic outbreak.[6] Cross-infection with MERS-CoV and SARS-CoV that are less transmissible than 2019-nCoV within the dental facility has been reported, with recommendations to resume dental care one month after recovery.[36] Ricci et al.[37] reported a cross-transmission of pneumonia resulting from contaminated dental unit waterline. Although COVID-19 cross-transmission within the dental facility has not been documented so far, yet the disease is still emerging, and this should not be eliminated.
Studies included in this systematic review highlighted various aspects of risks and general precautions within dental facilities. These studies focused on reinforcing infection measures as a standard of care and minimizing human-to-human contact during the outbreak.[2] Dentists need to maintain a high level of personal protection including PPE, face mask,[38] preferably N95 with aerosol-generating procedures, and face shield to reduce the risk of cross-contamination.[1,29] Overall, the consensus is to screen all patients prior to initiating any dental procedure and restricting dental care to emergency cases only.[22] However, this could create an increased demand in future for routine dental care, which amplifies the burden on dental healthcare system when the COVID-19 threat is resolved. Furthermore, SARS-CoV-2 has been reported to remain viable in aerosol up to 3 h with an estimated half-life of 5.6–6.8 h on stainless-steel and plastic respectively.[39] Thus, complying with strict infection control measures and minimizing aerosol generation with special attention to operatory ventilation and surface disinfection is crucial.[40,41,42] COVID-19 medical wastes are considered highly infectious and should be handled in accordance with medical waste management regulations.[23] The WHO[43] recommends using an autoclavable leak-proof yellow plastic bag marked with a biohazard symbol and tagged as highly infectious. This should be placed in container and collected once a day or when three-quarters of the plastic bag is filled.
A good coordinated referral system between dental offices and hospitals that are prepared for COVID-19 patients is mandated with special care to identify suspected asymptomatic cases.[24] Cognitive behavioral therapy is beneficial to distressed dentists, dental team and dental patients.[44,45] In addition, with the fourth industrial evolution, integrating robotics, artificial intelligence, and teledentistry to the dental education and practice became a necessity for the twenty-first century.[46,47] This could help in maintaining continuity of dental care without straining resources or jeopardizing safety, in the case of occurrence of a future public emergency of a similar scale.
One of the limitations of the included studies in this review is the fact that most of these studies are done within a single country, and they follow Chinese rules and regulations which could potentially introduce the risk of reporting and regulatory bias. WHO[48] and CDC[49] recommendations for hand hygiene and infection control measures could be considered. Another limitation is the scarcity of literature within this consistently emerging disease, which requires further investigations and the development of a global consensus in the fight against this pandemic crisis.
CONCLUSION
In summary, 2019-nCoV infection is a serious disease that requires public health attention. Dental institutions around the globe need to take a firm action to ensure safety and control transmission within dental facilities. While literature about association and cross-transmission of COVID-19 within the dental office is not yet reported; however, the current epidemic of the emerging infection rings the alarm bell. Reinforcing strict infection control measures and reducing person-to-person contact is a key step in fighting the spread of this highly transmissible disease. Minimizing aerosol-generating procedures and limiting treatment to dental emergency is advised. Lastly, it is the responsibility of the dental care workers to keep themselves alert and well-informed. This systematic review provided insights on risks and precautions to control cross-transmission within the dental setting. Further investigations and clinical trials are urgently needed.
ACKNOWLEDGEMENT
Not applicable.
FINANCIAL SUPPORT AND SPONSORSHIP
Not applicable.
CONFLICTS OF INTEREST
All authors declare no conflict of interest relevant to this article.
AUTHORS CONTRIBUTIONS
Both Khawlah A. Turkistani and Khadijah A. Turkistani contributed equally to the concept, design, literature search, manuscript preparation, manuscript editing, manuscript review and are guarantors.
ETHICAL POLICY AND INSTITUTIONAL REVIEW BOARD STATEMENT
Not applicable.
PATIENT DECLARATION OF CONSENT
Not applicable.
DATA AVAILABILITY STATEMENT
Not applicable.
REFERENCES
- 1.Ge ZY, Yang LM, Xia JJ, Fu XH, Zhang YZ. Possible aerosol transmission of COVID-19 and special precautions in dentistry. J Zhejiang Univ Sci B. 2020;21:361–8. doi: 10.1631/jzus.B2010010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: A study of a family cluster. Lancet. 2020;395:514–23. doi: 10.1016/S0140-6736(20)30154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: A descriptive study. Lancet. 2020;395:507–13. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-11. [cited 2020 Mar 16]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200131-sitrep-11-ncov.pdf?sfvrsn=de7c0f7_4 .
- 5.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-51. [cited 2020 Mar 16]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10 .
- 6.World Health Organization. Coronavirus Disease 2019 (COVID-19): Situation Report-151. [cited 2020 Jun 20]. Available from: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200619-covid-19-sitrep-151.pdf?sfvrsn=8b23b56e_2 .
- 7.Tanne JH, Hayasaki E, Zastrow M, Pulla P, Smith P, Rada AG. Covid-19: How doctors and healthcare systems are tackling coronavirus worldwide. BMJ. 2020;368:m1090. doi: 10.1136/bmj.m1090. [DOI] [PubMed] [Google Scholar]
- 8.Wang J, Zhou M, Liu F. Exploring the reasons for healthcare workers infected with novel coronavirus disease 2019 (COVID-19) in China. J Hosp Infect. 2020;105:100–1. doi: 10.1016/j.jhin.2020.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li Q, Guan X, Wu P, Wang X, Zhou L, Tong Y, et al. Early transmission dynamics in Wuhan, China, of novel coronavirus-infected pneumonia. N Engl J Med. 2020;382:1199–207. doi: 10.1056/NEJMoa2001316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leggat PA, Kedjarune U, Smith DR. Occupational health problems in modern dentistry: A review. Industrial Health. 2007;45:611–21. doi: 10.2486/indhealth.45.611. [DOI] [PubMed] [Google Scholar]
- 11.Qu X, Zhou XD. Psychological intervention in oral patients in novel coronavirus pneumonia outbreak period. Chin J Stomatol. 2020;55:e003. [Google Scholar]
- 12.Jin YH, Cai L, Cheng ZS, Cheng H, Deng T, Fan YP, et al. A rapid advice guideline for the diagnosis and treatment of 2019 novel coronavirus (2019-nCoV) infected pneumonia (standard version) Mil Med Res. 2020;7:4. doi: 10.1186/s40779-020-0233-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu X, Zhang L, Du H, Zhang J, Li Y, Qu J, et al. SARS-CoV-2 infection in children. N Engl J Med. 2020;382:1663–5. doi: 10.1056/NEJMc2005073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman D. + G Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann Intern Med. 2009;151:264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 15.COVID-19 Open Research Dataset CORD-19. [cited by 2020 Mar 16]. Available from: https://www.semanticscholar.org/cord19 .
- 16.World Health Organization Database. [cited by 2020 Mar 19]. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/global-research-on-novel-coronavirus-2019-ncov .
- 17.LitCOVID (provided by the NIH) [cited by 2020 Mar 19]. Available from: https://www.ncbi.nlm.nih.gov/research/coronavirus/
- 18.COVID-19 Research Export File (provided by Dimensions) [cited by 2020 Mar 19]. Available from: https://docs.google.com/spreadsheets/d/1-kTZJZ1GAhJ2m4GAIhw1ZdlgO46JpvX0ZQa232VWRmw/edit#gid=2034285255 .
- 19.Gu J, Han B, Wang J. COVID-19: Gastrointestinal manifestations and potential fecal-oral transmission. Gastroenterology. 2020;158:1518–9. doi: 10.1053/j.gastro.2020.02.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.To KK, Tsang OT, Chik-Yan Yip C, Chan KH, Wu TC, Chan JMC, et al. Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis. 2020;71:841–3. doi: 10.1093/cid/ciaa149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu H, Zhong L, Deng J, Peng J, Dan H, Zeng X, et al. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int J Oral Sci. 2020;12:8. doi: 10.1038/s41368-020-0074-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guo H, Zhou Y, Liu X, Tan J. The impact of the COVID-19 epidemic on the utilization of emergency dental services. J Dent Sci. 2020. Available from: https://doi.org/10.1016/j.jds.2020.02.002 . [DOI] [PMC free article] [PubMed]
- 23.Li Z, Meng L. The Prevention and control of new coronavirus infection in oral diagnosis and treatment. Chin J Stomatol. 2020;55:e001. doi: 10.3760/cma.j.issn.1002-0098.2020.0001. [DOI] [PubMed] [Google Scholar]
- 24.Meng L, Hua F, Bian Z. Coronavirus disease 2019 (COVID-19): Emerging and future challenges for dental and oral medicine. J Dent Res. 2020;99:481–7. doi: 10.1177/0022034520914246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng X, Xu X, Li Y, Cheng L, Zhou X, Ren B. Transmission routes of 2019-nCoV and controls in dental practice. Int J Oral Sci. 2020;12:9. doi: 10.1038/s41368-020-0075-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sacsaquispe-Contreras S. NEW CORONAVIRUS 2019 (COVID-19): Tips for the dentist. Herediana Stomatological Magazine. 2020;30:5–6. [Google Scholar]
- 27.Sabino-Silva R, Jardim ACG, Siqueira WL. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin Oral Investig. 2020;24:1619–21. doi: 10.1007/s00784-020-03248-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang HS, Yao ZQ, Wang WM. Emergency management of prevention and control of novel coronavirus pneumonia in departments of stomatology. Chin J Stomatol. 2020;55:e002. doi: 10.3760/cma.j.cn112144-20200205-00037. [DOI] [PubMed] [Google Scholar]
- 29.Zhang W, Jiang X. Measures and suggestions for the prevention and control of the novel coronavirus in dental institutions. Front Oral Maxillofac Med. 2020;2:4. [Google Scholar]
- 30.Lu C-W, Liu X-F, Jia Z-F. 2019-nCoV transmission through the ocular surface must not be ignored. Lancet. 2020;395:e39. doi: 10.1016/S0140-6736(20)30313-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Del Rio C, Malani PN. 2019 Novel coronavirus-important information for clinicians. JAMA. 2020;323:1039–40. doi: 10.1001/jama.2020.1490. [DOI] [PubMed] [Google Scholar]
- 32.Chen J. Pathogenicity and transmissibility of 2019-nCoV-A quick overview and comparison with other emerging viruses. Microbes Infect. 2020;22:69–71. doi: 10.1016/j.micinf.2020.01.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of 2019 novel coronavirus infection in China. N Engl J Med. 2020;382:1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–33. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pelleu GB, Jr, Shreve WB, Wachtel LW. Reduction of microbial concentration in the air of dental operating rooms. I. High-efficiency particulate air filters. J Dent Res. 1970;49:315–9. doi: 10.1177/00220345700490022001. [DOI] [PubMed] [Google Scholar]
- 36.Samaranayake LP, Peiris M. Severe acute respiratory syndrome and dentistry: A retrospective view. J Am Dent Assoc. 2004;135:1292–302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ricci ML, Fontana S, Pinci F, Fiumana E, Pedna MF, Farolfi P, et al. Pneumonia associated with a dental unit waterline. Lancet. 2012;379:684. doi: 10.1016/S0140-6736(12)60074-9. [DOI] [PubMed] [Google Scholar]
- 38.Bailey R, Giglio P, Blechman H, Nunez C. Effectiveness of disposable face masks in preventing cross contamination during dental procedures. J Dent Res. 1968;47:1062–5. doi: 10.1177/00220345680470061001. [DOI] [PubMed] [Google Scholar]
- 39.van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, et al. Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med. 2020;382:1564–7. doi: 10.1056/NEJMc2004973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kampf G, Todt D, Pfaender S, Steinmann E. Persistence of coronaviruses on inanimate surfaces and their inactivation with biocidal agents. J Hosp Infect. 2020;104:246–51. doi: 10.1016/j.jhin.2020.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Otter JA, Yezli S, Salkeld JA, French GL. Evidence that contaminated surfaces contribute to the transmission of hospital pathogens and an overview of strategies to address contaminated surfaces in hospital settings. Am J Infect Control. 2013;41:S6–11. doi: 10.1016/j.ajic.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 42.Turkistani KA. Precautions and recommendations for orthodontic settings during the COVID-19 outbreak: A review. AJODO. 2020;158:175–81. doi: 10.1016/j.ajodo.2020.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization. Safe Management of Wastes from Health-Care Activities: A Summary. [cited by 2020 Mar 18]. Available from: https://apps.who.int/iris/bitstream/handle/10665/259491/WHO-FWC-WSH-17.05-eng.pdf?sequence=1&isAllowed=y .
- 44.Peruzzo DC, Benatti BB, Ambrosano GM, Nogueira-Filho GR, Sallum EA, Casati MZ, et al. A systematic review of stress and psychological factors as possible risk factors for periodontal disease. J Periodontol. 2007;78:1491–504. doi: 10.1902/jop.2007.060371. [DOI] [PubMed] [Google Scholar]
- 45.Shamim T. The psychosomatic disorders pertaining to dental practice with revised working type classification. Korean J Pain. 2014;27:16–22. doi: 10.3344/kjp.2014.27.1.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Böhm da Costa C, Peralta FdS, Ferreira de Mello ALS. How has teledentistry been applied in public dental health services? An integrative review. Telemed J E Health. 2020;26:945–54. doi: 10.1089/tmj.2019.0122. [DOI] [PubMed] [Google Scholar]
- 47.Estai M, Kanagasingam Y, Mehdizadeh M, Vignarajan J, Norman R, Huang B, et al. Teledentistry as a novel pathway to improve dental health in school children: A research protocol for a randomised controlled trial. BMC Oral Health. 2020;20:1–9. doi: 10.1186/s12903-019-0992-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.World Health Organization. [cited by 2020 Mar 19]. Hand Hygiene: Why, How and When?. Available from: https://apps.who.int/iris/bitstream/handle/10665/44102/9789241597906_eng.pdf;jsessionid=00A9D7ACABAD2EE63D8BB679B4BD7885? sequence=1 .
- 49.Centers for Disease Control and Prevention. [cited by 2020 Apr 2]. Coronavirus Disease 2019 (COVID-19) Hand Hygiene Recommendations: Guidance for Healthcare Providers about Hand Hygiene and COVID-19. Available from: https://www.cdc.gov/coronavirus/2019-ncov/hcp/hand- hygiene.html .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.