Abstract
Researchers and journalists have argued that work-related factors may be partly responsible for disproportionate COVID-19 infection and death rates among vulnerable groups. We evaluate these claims by examining racial and ethnic differences in the likelihood of work-related exposure to COVID-19. We extend previous studies by considering 12 racial and ethnic groups and five types of potential occupational exposure to the virus: exposure to infection, physical proximity to others, face-to-face discussions, interactions with external customers and the public, and working indoors. Most importantly, we stratify our results by occupational standing, defined as the proportion of workers within each occupation with at least some college education. This measure serves as a proxy for whether workplaces and workers employ significant COVID-19-related risk reduction strategies. We use the 2018 American Community Survey to identify recent workers by occupation, and link 409 occupations to information on work context from the Occupational Information Network to identify potential COVID-related risk factors. We then examine the racial/ethnic distribution of all frontline workers and frontline workers at highest potential risk of COVID-19, by occupational standing and by sex. The results indicate that, contrary to expectation, White frontline workers are often overrepresented in high-risk jobs while Black and Latino frontline workers are generally underrepresented in these jobs. However, disaggregation of the results by occupational standing shows that, in contrast to Whites and several Asian groups, Latino and Black frontline workers are overrepresented in lower status occupations overall and in lower status occupations associated with high risk, and are thus less likely to have adequate COVID-19 protections. Our findings suggest that greater work exposures likely contribute to a higher prevalence of COVID-19 among Latino and Black adults and underscore the need for measures to reduce potential exposure for workers in low status occupations and for the development of programs outside the workplace.
Introduction
In the United States, Black, Latino, and Native American adults have experienced substantially higher rates of COVID-19 infection and mortality during 2020 than Whites and Asians [1–5]. Researchers and journalists argue that the difference is due, at least in part, to two work-related factors: (1) Black, Latino, and Native American workers are more likely to hold jobs that have to be done at their workplace rather than remotely, and (2) Latino and Black workers face greater risks of exposure to COVID-19 in their jobs than others [5–16]. This argument is consistent with the long history and contemporary effects of structural racism on occupational segregation in the US [17–20]. In this paper, we investigate these claims by examining differences in the likelihood of work-related exposure to COVID-19 by race and ethnicity.
It is difficult to quantify the importance of occupational vs. other exposures to the coronavirus. Most studies have used two approaches to argue that occupational risks to COVID-19 are higher for marginalized racial and ethnic groups than for Whites. We use a combination of these approaches. The most common strategy has been to look at racial/ethnic differences in recent (generally pre-pandemic) employment in industries or occupations that are considered essential or frontline during the pandemic [6,21,22]. As we discuss later, these earlier studies have been based on various definitions of essential and frontline. A second approach, sometimes used in conjunction with the first, has been to estimate relative risk of different groups during the pandemic from survey data about whether jobs entail high exposure to disease or infection and/or require close proximity to other people [7]. Based on the recent availability of death records for 2020 in some locations, several studies have employed an additional strategy. They have used occupational codes from death certificates to directly identify occupations with exceptionally high mortality during the pandemic period and examine differential mortality by race and ethnicity [16,23].
We extend this work in several ways. First, we consider 12 racial/ethnic groups. Previous studies on occupations and COVID-19 have largely been limited to four broad racial/ethnic categories (White, Black, Latino and Asian), although workers in other racial/ethnic groups or in Asian and Latino subgroups may be disproportionately exposed to COVID-19 [4]. Second, we examine five distinct job characteristics that could expose individuals to a high risk of contracting COVID-19: exposure to disease/infection; proximity to others; face-to-face discussions; interactions with external customers or the public; and working mostly indoors. Third, we examine results separately by occupational standing, defined here as the proportion of workers within each occupation with at least some college education. Occupational standing is closely linked to the type of activities performed, the physical work environment, control over working conditions, and attitudes toward workplace rules [24–26]. Despite the high risks often faced by physicians, nurses and other health personnel, lower status workers, including those in occupational sectors other than the health industry, appear to face especially high exposure to COVID-19 in the workplace [15,27]. A likely reason is that lower status workers have less access to risk mitigation strategies than higher status workers. As research in health inequality shows, those at higher socioeconomic status generally have access to a wider array of resources to protect health than others do [28]. In the case of potential workplace exposure to COVID-19, higher status workers are likely to have better access to personal protective equipment (PPE), frequent sanitation, enforced distancing, partitions, improved ventilation, and new filtration systems [27,29]. Examining results by occupational standing leads to a clearer picture of racial/ethnic differentials in potential exposure to COVID-19 transmission. We also present separate results by sex because of vastly different occupational profiles for men and women.
Data
We use data from two sources. Information on employment status, type of job, years of education, sex and race/ethnicity come from the 2018 American Community Survey (ACS), which is the most recent large, nationally representative survey fielded prior to the pandemic. Access is provided by the Integrated Public Use Microdata Series (IPUMS) [30]. Variables related to work context are drawn from the Occupational Information Network (O*NET), a database of work characteristics by detailed occupation collected by the US Department of Labor [31]. Approval for this research was obtained from the Institutional Review Boards at the University of California Los Angeles and Princeton University.
Using continuous data collection from random samples of incumbent workers, O*NET obtains information about job characteristics – such as work-related activities, work environment, and skills required to do the job – for almost 1000 detailed occupations. We use six variables from O*NET version 24.3, which contains information collected through 2019 and was released in May 2020 [31]. The six variables that we identified are among the hazardous job characteristics that may expose workers to SARS-Cov2 [15,27] – a virus that appears to be transmitted primarily through respiratory droplets and aerosols when an infected person coughs, sneezes, talks or breathes near others [32]. The six workplace variables reflect five types of risk: exposure to infection, physical proximity to others, face-to-face discussions, interactions with external customers and the public, and working indoors.
Variables
Race/ethnicity
Individuals were classified according to the following 12 race/ethnicity categories as reported by the head of the household in the ACS: White, Black, Latino, Chinese, Filipino, Vietnamese, Korean, other Asian, Native American (American Indian/Alaskan Native), Pacific Islander (Native Hawaiian/Pacific Islanders), mixed race, and other race/ethnicity. The three largest groups in the other Asian category are Indian, Japanese and Pakistani. In our analysis, all racial/ethnic categories except Latino exclude those who reported themselves as Latino/Hispanic in the ACS question on ethnicity.
Occupational standing
In order to rank occupations, we use a well-established sociological indicator of occupational ranking, known as “occupational education” [33] as a proxy for access to workplace risk mitigation measures. For each occupation, we calculate occupational education from the ACS as the percent of persons in the occupation who completed at least one year of college education (note that this variable classifies individuals by the educational attainment of all people in their occupation rather than by their own educational attainment). We use this measure, which we refer to as “occupational standing,” to divide the 409 occupations reported by ACS respondents in our analysis into quartiles, i.e., each group comprising about one-quarter of the occupations (not one-quarter of the workers).
Frontline status
During the pandemic, many workers have been sheltered from occupational exposure to infection by working remotely, e.g., from home. To distinguish between workers who are more vs. less able to work remotely, studies have used varying criteria to define “essential” and/or “frontline occupations.” In this analysis, we include only occupations classified as “frontline” based on the definition offered by Dingel and Neiman [34] and used by Blau et al. [22]: occupations in which one-third or fewer workers can feasibly work from home, ascertained from responses to 15 questions in O*NET. A total of 249 out of 409 occupations in our analysis are considered frontline according to these criteria.
We do not consider whether occupations are classified as essential or subject to lockdown because there has been enormous variation across states, localities, and time period in definitions and their application during the pandemic. For example, janitors, maids, bus drivers, retail sales workers, and personal care workers would not be classified as essential according to industry guidelines issued by the Department of Homeland Security (DHS) Cybersecurity and Infrastructure Security Agency (CISA) [22], yet many individuals in these occupations have likely been working away from home much or most of the time since March, 2020.
Defining high risk occupations
The five types of risk we consider from O*NET data – exposure to infection, physical proximity to others, face-to-face discussions, interactions with external customers and the public, and working indoors – are based on the following O*NET questions (in their original wording):
How often does your current job require that you be exposed to diseases or infection?
How physically close to other people are you when you perform your current job?
How often does your current job require face-to-face discussions with individuals and within teams?
In your current job, how important are interactions that require you to deal with external customers (as in retail sales) or the public in general (as in police work)?
How often does your current job require you to work outdoors, exposed to all weather conditions? [And:] How often does your current job require you to work outdoors, under cover (like in an open shed)?
Each of these questions has five possible categorical responses; the responses reflect frequency of exposure for questions 1,3, and 5; degrees of closeness for question 2, and importance of interactions for question 4.
For each of the first four risk indicators, we define high risk occupations as those for which the mean response in the O*NET data falls in the highest quartile (25%) of the full set of 409 occupations in the analysis. For the fifth risk indicator we use two questions reflecting the frequency with which employees work outdoors; the responses for these two questions are highly correlated. Because indoor work is higher risk than outdoor work ceteris paribus, we take the maximum of the O*NET values for these two variables and define high risk as the quartile of occupations with the lowest value, thereby identifying jobs with the lowest frequency of working outdoors as high risk.
Analytic strategy
In order to match occupations reported in the ACS with characteristics in O*NET, we converted the occupation code (Standard Occupational Classification or SOC) in O*NET into the four-digit 2010 census occupational code recorded in the 2018 ACS using a crosswalk provided at https://www.bls.gov/emp/documentation/crosswalks.htm. In cases where one census occupational code corresponded to multiple O*NET occupations, we took unweighted averages of the characteristics of the O*NET occupations and assigned these to the census occupational code. We linked occupations between the ACS and O*NET for all employed persons who reported holding a job in ACS with the exception of those in the military (because O*NET data were not available for military occupations); this linkage yielded about 1.9 million individuals in the ACS in 409 occupations. Approximately 88 percent of these individuals reported about the job they held during the past year with the remaining respondents reporting about the job held between one and five years prior to the survey.
It is important to note that unemployment and labor force participation rates vary considerably by race, ethnicity, and sex. For example, in the third quarter of 2020, the unemployment rate for Black men 16+ years old was 13.8 percent compared to 7.4 percent for White men and 9.6 percent for Asian men [35]. Moreover, job losses during the first half of 2020 occurred disproportionately among Black, Latino and Asian groups [36]. Another problem with obtaining an accurate description of the labor force is that unemployment rates have fluctuated throughout the period of the pandemic. As a consequence of these issues, our analysis does not account for differential unemployment and labor force participation rates.
As noted above, the analysis includes only individuals who worked in the five years prior to the ACS, the vast majority of whom worked in the year prior to the ACS; we refer to these individuals as either “recent workers” or simply as “workers.” After determining the percent of workers in each racial/ethnic group that hold frontline occupations, we measure the overrepresentation vs. underrepresentation of frontline workers in high-risk occupations. For each of the five risk factors, these estimates denote the proportion of frontline workers in the highest quartile of exposure that are in a given racial/ethnic group relative to the proportion of all frontline workers that are in that racial/ethnic group. We subsequently stratify workers in the highest risk group according to their quartile of occupational standing. The first quartile of occupational standing comprises occupations with the lowest standing. Similar to the unstratified estimates, we then consider the proportion of workers in a specified level of occupational standing (for each of the five risk factors) that are in a given racial/ethnic group relative to the proportion of all frontline workers that are in that group.
The results are presented in five figures: the first includes all 12 racial/ethnic groups, whereas each of the remaining graphs, which include occupational standing, considers three racial/ethnic groups. All of the figures are heatmaps, with shades of orange indicating overrepresentation of workers in a given risk category relative to all frontline workers (for the particular racial/ethnic group), and shades of green indicating the corresponding underrepresentation in a given risk category. Progressively darker shades reflect successively more extreme values of overrepresentation (orange) or underrepresentation (green). The figures are based on separate calculations for male and female frontline workers.
All calculations use weights provided in the ACS. The data underlying these graphs are presented in S1 Appendix.
Results
Table 1 shows the percentages of workers in frontline occupations by sex and race/ethnicity. Employment in frontline occupations varies considerably across groups. For both men and women, Latinos are the most likely workers to hold frontline occupations whereas Chinese and Korean workers are the least likely to do so. Latino, Black, Native American, and Pacific Islander men are the most likely to have frontline occupations – more than 70% of male workers in each of these groups are classified as frontline. In contrast, Vietnamese, Latino, and Filipino women are the most likely female workers to hold frontline occupations. Asian women are at least as likely as Asian men to work in frontline occupations.
Table 1:
Number of recent workers and percentage in frontline occupations by race/ethnicity and sex
| Male | Female | |||
|---|---|---|---|---|
| Race/Ethnicity | Number of Recent Workers | Frontline (%) | Number of Recent Workers | Frontline (%) |
| White | 675,542 | 59.5 | 632,421 | 46.2 |
| Black | 76,649 | 72.9 | 87,168 | 57.5 |
| Latino | 133,868 | 77.9 | 120,853 | 61.8 |
| Chinese | 13,095 | 40.9 | 14,265 | 41.3 |
| Filipino | 7,798 | 61.7 | 10,403 | 61.2 |
| Vietnamese | 5,150 | 63.5 | 5,519 | 66.2 |
| Korean | 4,303 | 44.0 | 4,684 | 47.8 |
| Other Asian | 22,072 | 42.1 | 18,654 | 57.9 |
| Native American | 7,018 | 75.5 | 7,059 | 56.7 |
| Native Hawaiian/Pacific Islander | 1,402 | 73.0 | 1,353 | 54.1 |
| Mixed Race | 17,555 | 63.2 | 17,857 | 52.0 |
| Other Race | 1,695 | 64.3 | 1,778 | 57.3 |
| Total | 966,147 | 63.7 | 922,014 | 50.5 |
Note: Data are from the 2018 American Community Survey (ACS). Percentages are calculated using weights provided by the ACS; numbers are unweighted counts of ACS respondents. All racial/ethnic categories except Latino exclude those who reported themselves as Latino/Hispanic in the ACS question on ethnicity.
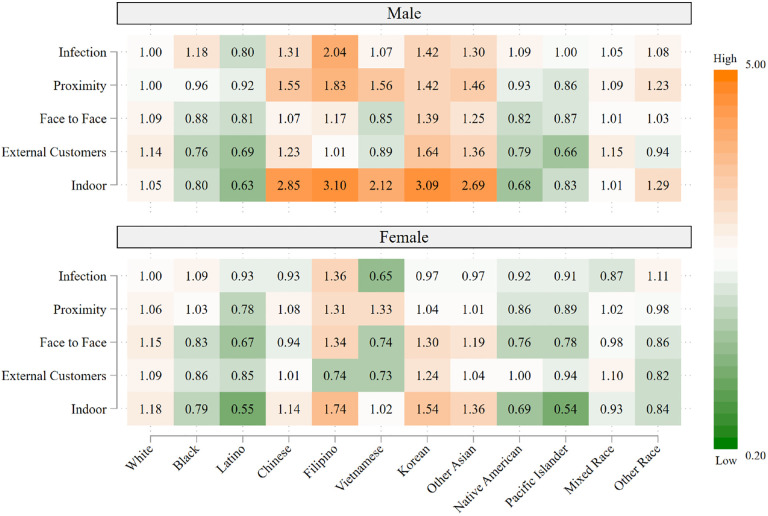
Fig 1 depicts overrepresentation and underrepresentation of the 12 racial/ethnic groups for each of the five occupational exposures related to viral transmission, by sex. For example, consider the value of 0.80 for Latino males regarding risk of infection (top row, third column of Fig 1). This value suggests that Latinos are underrepresented by 20% in frontline jobs that entail a high risk of infection relative to the proportion of frontline workers that are Latino. It can be obtained from S1 Appendix in the following way: Latino males comprise 17.4% of frontline jobs in the highest quartile of infection risk (5th column of S1.4) and 21.6% of all frontline workers (5th column of S1.2); 17.4/21.6= .806 or, allowing for slight round-off error, the value of 0.80 in Fig 1.
Fig 1. Representation of frontline workers in high-risk occupations relative to representation as frontline workers, by race/ethnicity and sex.
Data are from the 2018 American Community Survey (ACS). Occupations are considered to be high-risk if the average value for the risk factor in the O*NET data falls in the highest quartile of the occupations in the analysis.
Surprisingly in light of elevated COVID-19 mortality among Latino, Black, and Native American populations, Fig 1 shows that these workers are generally underrepresented in high-risk occupations; the main exception is a modest overrepresentation of Black workers in occupations involving risk of infection. In contrast, Whites are modestly overrepresented according to several components of risk, particularly exposure to external customers for men and indoor work for women. The most extreme results are those for Asians, with all ethnic groups of Asian men having more than a twofold overrepresentation in occupations involving indoor work; Filipino men are additionally highly overrepresented in occupations involving high risk of infection.
Fig 1 highlights the complexity of identifying the racial/ethnic groups with the largest occupational exposure to the virus. Contrary to expectation based on earlier studies and the media, the values in Fig 1 suggest that Black and Latino workers do not face higher occupational risks related to viral exposure compared with Whites. However, this conclusion is likely to be incorrect. The classification of high-risk occupations that we have considered thus far does not capture variation among occupations in COVID-19 risk reduction measures that are deployed in the workplace and are more likely to be implemented in higher status occupations. For example, home health aides (relatively low occupational standing and disproportionately held by workers of color) and physicians (high occupational standing and disproportionately White) are both frontline occupations at high risk for infection and physical proximity to other people, but physicians are far more likely to have access to and use PPE, work in frequently sanitized environments, and have had specialized training to reduce potential exposure to infections at work [37,38].
To get a clearer picture of COVID-19 transmission-related risks faced by workers in different occupations and different racial/ethnic groups, the remaining graphs use quartile of occupational standing as a proxy measure for workplace risk mitigation during the COVID-19 pandemic. The most common frontline occupations in the highest (4th) quartile of occupational standing are predominantly in the healthcare sector, most notably registered nurses, physicians, and surgeons. In contrast, the most common frontline occupations in the lowest (1st) quartile include cashiers, drivers, janitors, laborers, stock clerks, and housekeeping cleaners. S2 Appendix lists the most frequently held frontline occupations for each of the five risk indicators, stratified by occupational standing quartile. Only occupations that include at least five percent of workers in the quartile are shown. Although many of the high-risk occupations across all statuses are in the healthcare sector, numerous occupations outside of the healthcare sector are high-risk on at least one of the five indicators. Among the lowest status occupations, these high-risk occupations include janitors, maids, and other cleaners; carpenters; maintenance and repair workers; food preparation workers and servers; machine operators; stock clerks; and cashiers.
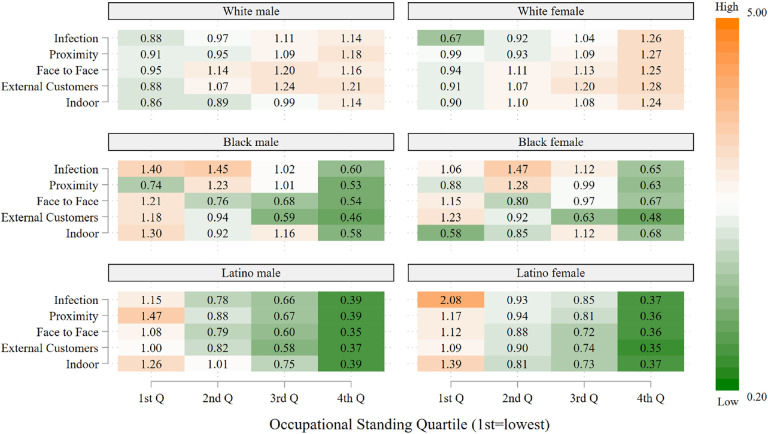
Fig 2, which stratifies the estimates in Fig 1 by occupational standing for White, Black, and Latino workers, presents a more nuanced picture of racial/ethnic variation in occupational risks than Fig 1. Among workers in high-risk occupations on each of the five indicators, White workers, both men and women, are generally overrepresented in the 3rd and especially the 4th (i.e., highest) occupational standing quartile. Black and Latino workers, on the other hand, are generally overrepresented in the 1st quartile while being vastly underrepresented (especially Latinos) in the 4th occupational standing quartile. Latino male workers have the largest overrepresentation (1.5 or 50% greater representation relative to their proportion of all frontline workers) in the lowest status occupations associated with physical proximity, working, for example, as carpenters, roofers, and food preparation and serving-related workers. Latino female workers have the largest overrepresentation (2.1) in the lowest ranking occupations associated with high infection risk, working primarily as maids and other cleaners.
Fig 2. Representation of frontline workers in high-risk occupations relative to representation as frontline workers by occupational standing: White, Black and Latino workers, by sex.
Data are from the 2018 American Community Survey (ACS). Occupations are considered to be high-risk if the average value for the risk factor in the O*NET data falls in the highest quartile of the occupations in the analysis. Occupational standing is defined as the percentage of ACS respondents reporting this occupation title who completed at least one year of college education. The 1st quartile represents the lowest quartile of occupational standing and the 4th quartile the highest quartile of occupational standing.
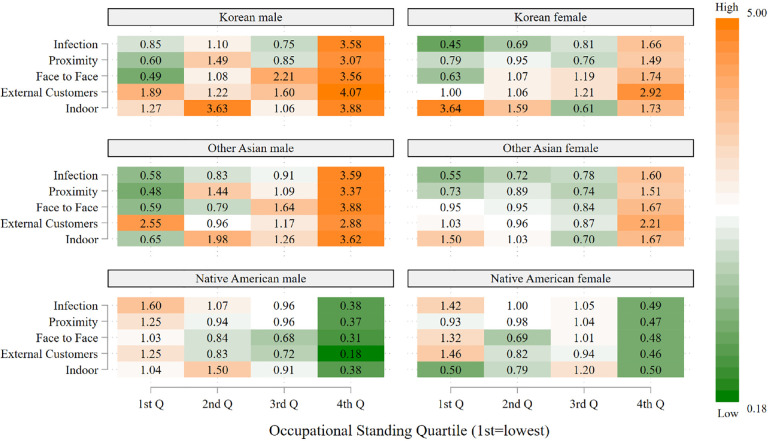
Figs 3–5 present heatmaps for the remaining racial/ethnic groups, in the same format as Fig 2. As shown in Fig 3, Chinese, Filipino and Vietnamese men, as well as Filipino women, occupy a much larger share of high status, high-risk occupations relative to their share of frontline occupations, often three to four times as large; this occurs across all five risk indicators. In general, the overrepresentation of men in high-risk jobs with high occupational standing exceeds that for women in these ethnic groups. As shown in the top two panels of Fig 4, a similar pattern occurs for Korean and other Asian workers, i.e., large overrepresentation, especially for men, in high-risk occupations with high occupational standing. The majority of Filipino men and women, and Chinese and Korean women, who are in high status frontline occupations are registered nurses. The other frequently held occupations for these groups are also in the healthcare sector. Chinese and Korean men with the highest status frontline occupations are most likely to be physicians and surgeons, but are also employed as dentists, pharmacists and registered nurses. The high proportion of Asians in the healthcare sector largely accounts for their disproportionate presence in high-risk occupations, particularly those involving exposure to infection, close proximity to others, and indoor locations.
Fig 3. Representation of frontline workers in high-risk occupations relative to representation as frontline workers by occupational standing: Chinese, Filipino, and Vietnamese workers, by sex.
Data are from the 2018 American Community Survey (ACS). Occupations are considered to be high-risk if the average value for the risk factor in the O*NET data falls in the highest quartile of the occupations in the analysis. Occupational standing is defined as the percentage of ACS respondents reporting this occupation title who completed at least one year of college education. The 1st quartile represents the lowest quartile of occupational standing and the 4th quartile the highest quartile of occupational standing.
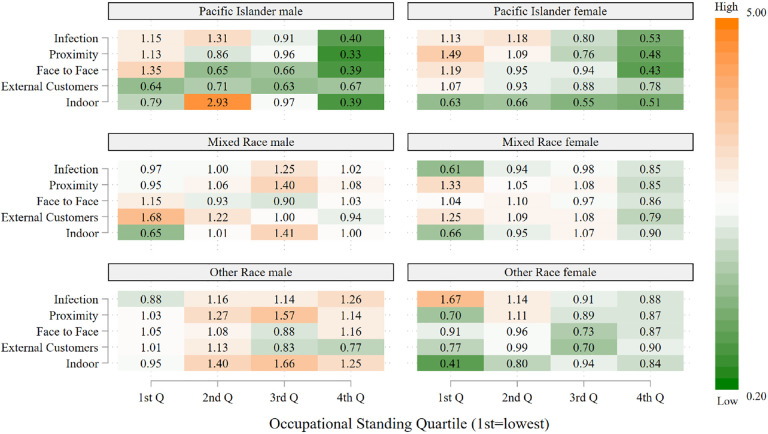
Fig 5. Representation of frontline workers in high-risk occupations relative to representation as frontline workers by occupational standing: Pacific Islander, Mixed Race, and Other Race workers, by sex.
Data are from the 2018 American Community Survey (ACS). Occupations are considered to be high-risk if the average value for the risk factor in the O*NET data falls in the highest quartile of the occupations in the analysis. Occupational standing is defined as the percentage of ACS respondents reporting this occupation title who completed at least one year of college education. The 1st quartile represents the lowest quartile of occupational standing and the 4th quartile the highest quartile of occupational standing.
Fig 4. Representation of frontline workers in high-risk occupations relative to representation as frontline workers by occupational standing: Korean, Other Asian, and Native American workers, by sex.
Data are from the 2018 American Community Survey (ACS). Occupations are considered to be high-risk if the average value for the risk factor in the O*NET data falls in the highest quartile of the occupations in the analysis. Occupational standing is defined as the percentage of ACS respondents reporting this occupation title who completed at least one year of college education. The 1st quartile represents the lowest quartile of occupational standing and the 4th quartile the highest quartile of occupational standing.
These findings for Asian workers contrast strikingly with those for Native Americans in the bottom panel of Fig 4. Native American workers, both men and women, occupy high-risk jobs in the lowest level of occupational standing more frequently than expected relative to their numbers as frontline workers, particular for jobs that entail a high risk of infection. Patterns for Pacific Islanders, shown in the top panel of Fig 5, reveal similar patterns to those of Native Americans. No clear pattern emerges for the remaining racial/ethnic groups considered, mixed race and other race.
Discussion
In this study, we extended earlier work on racial/ethnic differences in potential work-related exposure to COVID-19 by examining 12 racial/ethnic groups and by considering five indicators of risk exposure. Our central innovation is to use occupational standing as a proxy for whether workers and their workplaces employ significant COVID-19-related risk reduction strategies (PPE, distancing, sanitation, improved ventilation, etc.) – something not measured in the data we use nor in any other large, nationally representative data sets, to our knowledge. We argue that higher status workers, even in high-risk occupations, are more likely to have access to (and to use) workplace COVID-19 risk mitigation measures than low status workers because they are more likely: (a) to work for employers who voluntarily practice risk mitigation and provide PPE and other tools for workers to do so, (b) if not, to demand risk reduction measures and have the bargaining power to obtain them, and (c) to understand (or learn about) COVID-19 transmission routes and to comply with risk reduction strategies or implement their own [27–29].
Once we disaggregate our results by occupational standing, we see large differences in the racial and ethnic distribution of frontline occupations. In contrast to White frontline workers, Latino, Black, and Native American frontline workers are overrepresented in lower status occupations overall, as well as lower status occupations associated with high risk, and thus are probably less likely than Whites to have adequate COVID-19 protections.
In contrast, Asians show more complex patterns, reflecting factors such as immigration history, labor market segregation, and ethnic economic niches. For example, female Filipino workers are disproportionately employed in high-risk occupations across all of the five risk categories. However, they are much more likely to be in higher status occupations than other Asian groups, in part because of a history of immigration of Filipino nurses and other health professionals to the US [39].
Although most earlier studies found lower occupational risks for White workers compared with other groups, specific findings vary due largely to the types of occupations examined (e.g., essential) and the occupational characteristics chosen to denote risk for COVID-19. Based on data from the 2014–2017 Medical Expenditure Panel Survey and the 2017–2018 American Time Use Survey, Selden and Berdahl found that Black, Latino, and Asian workers were slightly more likely than Whites to work in essential jobs, i.e., at businesses that were allowed to remain open during COVID-19-related shutdowns, although essential White workers were more likely to be able to work from home [21]. Hawkins used data from the 2019 Current Population Survey linked with two measures of risk from O*NET (infection and close proximity) and found an elevated risk for Black workers but virtually none for Latinos for jobs in essential industries [7]. In a report by the Urban Institute based on the 2018 ACS that used O*NET data to identify occupations involving close proximity to other workers, researchers concluded that Black, Latino, and Native American workers were more likely than White workers to have jobs that put them at high risk for viral transmission [14]. Another study, based on employment data for 2014–2019 and two O*NET measures (working indoors and in close proximity to others), found disproportionate risk exposure for both Black and Latino workers in some occupations [13].
In contrast to much of the earlier work, we focus on frontline occupations rather than essential industries because of the large variation among states and local jurisdictions and over time in the definition of essential industries versus the relative stability of the frontline occupation classification. We also expand measurement of risk of viral transmission from previous work that has relied on only one or two occupation-related characteristics. However, our main contribution is that we distinguish between lower and higher status occupations, a strategy that uncovers important differences among racial and ethnic groups that were not apparent in the previous studies.
The racial/ethnic differences by occupational standing highlighted in this paper are consistent with a large literature unrelated to the COVID-19 pandemic. Social science and public health research shows that the history and contemporary effects of racism in the US have led to a labor force highly segregated by race and ethnicity, with Latino and Black workers holding many of the lowest status and least secure jobs [17,18,40,41]. There is also ample evidence that workers in low status occupations were already at higher risk of accidents, injury, infection, and other health problems prior to the pandemic and that these workers also have less control and decision-making ability over how their workplaces are run [42]. Workers in low status jobs may also be more likely to face employer resistance to implementing stricter safety measures that may reduce productivity or profits [40,43–45]. Thus, a realistic depiction of COVID-19 risks for Latino and Black workers requires consideration of occupational standing.
Despite the insights provided by this study, our analysis has several important limitations. First, the 2018 ACS data on recent jobs used here may not provide an accurate picture of employment or occupational distributions during the pandemic. Unemployment rates rose markedly in many areas of the country during the early part of 2020. For example, the rate was 14.7% in April 2020 compared to 3.5% in February 2020 for the US population age 16+ [46]. Unemployment rates were even higher for some racial/ethnic groups, including the Latino (18.9% in April) and Black populations (16.8% in May) [47,48]. Business closures, layoffs, and unemployment rates have varied a great deal from state to state and over time. Thus, it is impossible to determine whether or not workers were employed during 2020 at a particular time and place. Other consequences of the pandemic, such as virtual schooling, have led many parents, especially mothers, to leave the labor force entirely, at least until the pandemic is over [49]. Despite these caveats, we believe that the ACS data provide the best picture currently available of the occupational distribution of the US population at a time close to the onset of the pandemic. A related limitation is that, because our analyses provide no evidence about exposure for people who are unemployed or outside the labor force, our conclusions are necessarily restricted to the employed population.
There are also several limitations of the O*NET database and its specific measures we rely on to estimate workplace exposures to COVID-19. These measures were not designed with a pandemic in mind and thus do not include key information on viral transmission risk. A critical omission for analyses of COVID-19 is data on the implementation of, and worker compliance with, COVID-19 transmission workplace mitigation measures. This lack of information underscores the need to disaggregate workers by occupational standing, as we have done here. There are other limitations to the O*NET data when used in studies of infection-related risks. For example, in the case of contact with others, it would be useful to know the average duration of close contacts, the nature of the contacts and the characteristics of the people with whom the worker interacts. For all of our measures of risk, our analysis would benefit if O*NET provided information on how characteristics of each individual occupation vary by demographic factors (e.g., race/ethnicity, sex, and age) of the workers.
Despite these limitations, our results strongly suggest that higher work exposures to COVID-19 likely contribute to a higher prevalence of the virus among Latino, Black, and Native American, compared to White, adults in the US. Until communities achieve widespread vaccination against COVID-19 or an effective treatment method is available for COVID-19, the focus needs to be on risk reduction, particularly in places where transmission is high.
Reducing potential exposure for workers in low status occupations requires multiple coordinated measures beyond PPE. Carlsten et al. draw on industrial hygiene’s hierarchy of controls framework to outline three types of measures employers should take to mitigate COVID-19 risks for their workers: (a) eliminating exposure to the SARS CoV-2 virus completely would clearly be the most effective measure, (b) engineering and administrative controls the next most effective, and (c) PPE the least effective, albeit essential (particularly combined with engineering and administrative controls) if eliminating exposure is not possible [15]. Aside from reducing community transmission – something which is beyond employers’ control – workplace COVID-19 exposure elimination strategies include requiring symptom and illness reporting, rapid and effective testing, preventing workers with symptoms or positive tests from coming to work, and providing telecommuting and work-from-home options when possible [15]. Particularly for businesses employing lower income workers, these policies are more likely to succeed (and be more humane) if employers provide sick leave and free or subsidized health care for workers who test positive or show symptoms of COVID-19. However, testing can be expensive for uninsured workers and current tests often fail to provide rapid and accurate results. Furthermore, COVID-19 can be asymptomatically transmitted, and the length and strength of post-infection immunity are unknown. If workers who develop symptoms or test positive would lose their jobs and/or pay, they would have an incentive to not report illnesses or related symptoms. For all these reasons, eliminating risk in the workplace is likely to be difficult as long as COVID-19 remains prevalent in the population.
Engineering controls are designed to be independent of individual behavior. Controls to reduce COVID-19 risk include physical barriers between people and improved ventilation systems. Administrative controls include social/physical distancing, regular cleaning and disinfecting, and staggered work schedules. Because these measures require individuals to behave in a consistently careful and controlled manner, they can be hard to enforce [15]. Finally, in concert with exposure, engineering, and administrative controls, employers can provide personal protective equipment for their employees. Analysis of survey data from June 2020 for non-health care workers who were unable to work remotely showed that voluntary use of COVID-19 workplace hazard controls (defined as PPE and other physical barriers) was approximately double when employers provided these hazard controls than when they did not [29]. The differences were particularly large among low-income workers, perhaps because they were less likely to be able to afford PPE themselves.
From a public policy point of view, the question is how to ensure that employers protect workers by implementing these risk mitigation strategies, particularly in workplaces employing workers with low occupational standing. In the US, employers are legally required to provide a workplace free of recognized health and safety hazards. The federal Occupational Safety and Health Administration (OSHA) and related state governmental agencies have provided guidance to employers about exposure controls against COVID-19 transmission [50], but there is little evidence on what proportion of employers nationwide have implemented effective controls during the pandemic and when they have done so [51]. Many employers have been faced with huge declines in revenues and major logistical challenges, making new investments in COVID-19 risk mitigation particularly difficult, although federal Paycheck Protect Program loans to businesses have helped to provide funds for work protection measures to some employers. Equally important, however, are programs outside of the workplace to control the COVID-19 pandemic, including: (1) a campaign to achieve rapid and universal vaccination, targeting frontline workers and particularly those in racial and ethnic groups with higher COVID-19 infection rates; (2) COVID-19 health communication and education programs tailored for Black, Latino, Native American, and other populations that address distrust of vaccines and experiences of racism in public health and medical care; and (3) effective community-based and free or low-cost testing, tracing, and treatment programs particularly centered on the uninsured and underinsured population.
Supplementary Material
S1 Appendix: Racial/ethnic distributions within each occupational subset displayed in main text figures
S2 Appendix: Common high-risk occupations by occupational standing quartile
Acknowledgment
The authors would like to thank Francine Blau at Cornell University, Josefine Koebe at Universität Hamburg, and Pamela Meyerhofer at Montana State University for sharing their code to identify frontline occupations. We also thank Dana Glei for her suggestions on an earlier draft of this paper.
References
- 1.Andrasfay T, Goldman N. Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proc Natl Acad Sci. 2021;118. doi: 10.1073/pnas.2014746118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sáenz R, Garcia MA. The Disproportionate Impact of COVID-19 on Older Latino Mortality: The Rapidly Diminishing Latino Paradox. J Gerontol Ser B. 2020;XX: 1–7. doi: 10.1093/geronb/gbaa158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rentsch CT, Kidwai-Khan F, Tate JP, Park LS, Jr JTK, Skanderson M, et al. Patterns of COVID-19 testing and mortality by race and ethnicity among United States veterans: A nationwide cohort study. PLOS Med. 2020;17: e1003379. doi: 10.1371/journal.pmed.1003379 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang D, Gee GC, Bahiru E, Yang EH, Hsu JJ. Asian-Americans and Pacific Islanders in COVID-19: Emerging Disparities Amid Discrimination. J Gen Intern Med. 2020. [cited 6 Nov 2020]. doi: 10.1007/s11606-020-06264-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leggat-Barr K, Uchikoshi F, Goldman N. COVID-19 Risk Factors and Mortality among Native Americans. medRxiv. 2021; 2021.03.13.21253515. doi: 10.1101/2021.03.13.21253515 [DOI] [Google Scholar]
- 6.Casura L, Lowe R Jr., Martinez C, Serpas S, Castellanos V, Singelmann J. Frontline workers in the U.S.: race, ethnicity, and gender. International Union for the Scientific Study of Population; 2020. Sep. Available: https://www.niussp.org/article/frontline-workers-in-the-u-s-race-ethnicity/ [Google Scholar]
- 7.Hawkins D. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity. Am J Ind Med. 2020;65. doi: 10.1002/ajim.23145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Covid-19 Deaths Skew Younger Among Minorities - WSJ. The Wall Street Journal. 17 August 2020. Available: https://www-wsj-com.libproxy1.usc.edu/articles/covid-19-deaths-strike-early-for-many-minorities-11597582801. Accessed 10 Nov 2020.
- 9.Oppel RA Jr, Gebeloff R, Lai KKR, Wright W, Smith M. The Fullest Look Yet at the Racial Inequity of Coronavirus. The New York Times. 5 July 2020. Available: https://www.nytimes.com/interactive/2020/07/05/us/coronavirus-latinos-african-americans-cdc-data.html. Accessed 10 Nov 2020. [Google Scholar]
- 10.Reckdahl K. “The impact of work”: On-the-job coronavirus exposure a key driver in Black, Latino communities. NOLA.com. 17 October 2020. Available: https://www.nola.com/news/business/article_d0e20ff2-0a62-11eb-8314-af3dffbffd15.html. Accessed 10 Nov 2020. [Google Scholar]
- 11.U.S. News and World Report. AHA News: Hispanics Are Paying the Price for Being “Essential” During the Pandemic. US News & World Report. 9 Oct 2020. Available: https://www.usnews.com/news/health-news/articles/2020-10-09/aha-news-hispanics-are-paying-the-price-for-being-essential-during-the-pandemic. Accessed 10 Nov 2020. [Google Scholar]
- 12.Erdman SL. More Hispanic workers impacted by Covid-19 in food processing and agriculture workplaces, CDC study finds. CNN. 20 October 2020. Available: https://www.cnn.com/2020/10/20/health/cdc-study-covid-hispanic-workers/index.html. Accessed 10 Nov 2020. [Google Scholar]
- 13.Cox-Ganser JM, Henneberger PK. Occupations by Proximity and Indoor/Outdoor Work: Relevance to COVID-19 in All Workers and Black/Hispanic Workers. Am J Prev Med. 2021. [cited 30 Mar 2021]. doi: 10.1016/j.amepre.2020.12.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dubay L, Aarons J, Brown KS, Kenney GM. How Risk of Exposure to the Coronavirus at Work Varies by Race and Ethnicity and How to Protect the Health and Well-Being of Workers and Their Families. Urban Institute; 2020. Dec. Available: https://www.urban.org/research/publication/how-risk-exposure-coronavirus-work-varies-race-and-ethnicity-and-how-protect-health-and-well-being-workers-and-their-families/view/full_report [Google Scholar]
- 15.Carlsten C, Gulati M, Hines S, Rose C, Scott K, Tarlo SM, et al. COVID-19 as an occupational disease. Am J Ind Med. 2021;64: 227–237. doi: 10.1002/ajim.23222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hawkins D, Davis L, Kriebel D. COVID-19 deaths by occupation, Massachusetts, March 1–July 31, 2020. Am J Ind Med. 2021;64: 238–244. doi: 10.1002/ajim.23227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bailey ZD, Krieger N, Agénor M, Graves J, Linos N, Bassett MT. Structural racism and health inequities in the USA: evidence and interventions. The Lancet. 2017;389: 1453–1463. doi: 10.1016/S0140-6736(17)30569-X [DOI] [PubMed] [Google Scholar]
- 18.del Río C, Alonso-Villar O. The Evolution of Occupational Segregation in the United States, 1940–2010: Gains and Losses of Gender–Race/Ethnicity Groups. Demography. 2015;52: 967–988. doi: 10.1007/s13524-015-0390-5 [DOI] [PubMed] [Google Scholar]
- 19.Chetty R, Hendren N, Jones MR, Porter SR. Race and Economic Opportunity in the United States: an Intergenerational Perspective*. Q J Econ. 2020;135: 711–783. doi: 10.1093/qje/qjz042 [DOI] [Google Scholar]
- 20.Pager D, Shepherd H. The Sociology of Discrimination: Racial Discrimination in Employment, Housing, Credit, and Consumer Markets. Annu Rev Sociol. 2008;34: 181–209. doi: 10.1146/annurev.soc.33.040406.131740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Selden TM, Berdahl TA. COVID-19 And Racial/Ethnic Disparities In Health Risk, Employment, And Household Composition. Health Aff (Millwood). 2020;39: 1624–1632. doi: 10.1377/hlthaff.2020.00897 [DOI] [PubMed] [Google Scholar]
- 22.Blau FD, Koebe J, Meyerhofer PA. Who are the Essential and Frontline Workers? National Bureau of Economic Research; 2020. Sep. Report No.: w27791. doi: 10.3386/w27791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chen Y-H, Glymour M, Riley A, Balmes J, Duchowny K, Harrison R, et al. Excess mortality associated with the COVID-19 pandemic among Californians 18–65 years of age, by occupational sector and occupation: March through October 2020. medRxiv. 2021; 2021.01.21.21250266. doi: 10.1101/2021.01.21.21250266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hoven H, Wahrendorf M, Siegrist J. Occupational position, work stress and depressive symptoms: a pathway analysis of longitudinal SHARE data. J Epidemiol Community Health. 2015;69: 447–452. doi: 10.1136/jech-2014-205206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Landsbergis PA, Grzywacz JG, LaMontagne AD. Work organization, job insecurity, and occupational health disparities. Am J Ind Med. 2014;57: 495–515. doi: 10.1002/ajim.22126 [DOI] [PubMed] [Google Scholar]
- 26.Clougherty JE, Souza K, Cullen MR. Work and its role in shaping the social gradient in health. Ann N Y Acad Sci. 2010;1186: 102–124. doi: 10.1111/j.1749-6632.2009.05338.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gaitens J, Condon M, Fernandes E, McDiarmid M. COVID-19 and Essential Workers: A Narrative Review of Health Outcomes and Moral Injury. Int J Environ Res Public Health. 2021;18: 1446. doi: 10.3390/ijerph18041446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Phelan JC, Link BG, Tehranifar P. Social Conditions as Fundamental Causes of Health Inequalities: Theory, Evidence, and Policy Implications. J Health Soc Behav. 2010;51: S28–S40. doi: 10.1177/0022146510383498 [DOI] [PubMed] [Google Scholar]
- 29.Billock RM, Groenewold MR, Free H, Haring Sweeney M, Luckhaupt SE. Required and Voluntary Occupational Use of Hazard Controls for COVID-19 Prevention in Non–Health Care Workplaces — United States, June 2020. MMWR Morb Mortal Wkly Rep. 2021;70. doi: 10.15585/mmwr.mm7007a5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ruggles S, Flood S, Goeken R, Grover J, Meyer E, Pacas J, et al. IPUMS USA: Version 10.0 [dataset]. Minneapolis, MN: IPUMS; 2020. Available: 10.18128/D010.V10.0 [DOI] [Google Scholar]
- 31.O*NET OnLine. National Center for O*NET Development; Available: https://www.onetonline.org/
- 32.Wilson N, Corbett S, Tovey E. Airborne transmission of covid-19. BMJ. 2020;370. doi: 10.1136/bmj.m3206 [DOI] [PubMed] [Google Scholar]
- 33.Hauser RM, Warren JR. Socioeconomic Indexes for Occupations: A Review, Update, and Critique: Sociol Methodol. 2016. [cited 6 Nov 2020]. Available: https://journals.sagepub.com/doi/10.1111/1467-9531.271028
- 34.Dingel JI, Neiman B. How Many Jobs Can be Done at Home? National Bureau of Economic Research; 2020. Apr. Report No.: w26948. doi: 10.3386/w26948 [DOI] [Google Scholar]
- 35.Unemployment rates by age, sex, race, and Hispanic or Latino ethnicity. Washington, DC: U.S. Bureau of Labor Statistics; 2020. Oct. Report No.: E-16. [Google Scholar]
- 36.Gemelas J, Davison J, Keltner C, Ing S. Inequities in Employment by Race, Ethnicity, and Sector During COVID-19. J Racial Ethn Health Disparities. 2021. [cited 30 Mar 2021]. doi: 10.1007/s40615-021-00963-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sterling MR, Tseng E, Poon A, Cho J, Avgar AC, Kern LM, et al. Experiences of Home Health Care Workers in New York City During the Coronavirus Disease 2019 Pandemic: A Qualitative Analysis. JAMA Intern Med. 2020;180: 1453–1459. doi: 10.1001/jamainternmed.2020.3930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shang J, Chastain AM, Perera UGE, Dick AW, Fu CJ, Madigan EA, et al. The state of infection prevention and control at home health agencies in the United States prior to COVID-19: A cross-sectional study. Int J Nurs Stud. 2021;115: 103841. doi: 10.1016/j.ijnurstu.2020.103841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Choy CC. Empire of Care: Nursing and Migration in Filipino American History. Duke University Press; 2003. [Google Scholar]
- 40.Hall M, Greenman E. The Occupational Cost of Being Illegal in the United States: Legal Status, Job Hazards, and Compensating Differentials. Int Migr Rev. 2015;49: 406–442. doi: 10.1111/imre.12090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wilson FD. Generational changes in racial inequality in occupational attainment, 1950–2010: A synthetic cohort analysis. Bois Rev. 2017;14: 387–425. doi: 10.1017/S1742058X17000170 [DOI] [Google Scholar]
- 42.Steege AL, Baron SL, Marsh SM, Menéndez CC, Myers JR. Examining occupational health and safety disparities using national data: A cause for continuing concern. Am J Ind Med. 2014;57: 527–538. doi: 10.1002/ajim.22297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Krieger N, Chen JT, Waterman PD, Hartman C, Stoddard AM, Quinn MM, et al. The inverse hazard law: Blood pressure, sexual harassment, racial discrimination, workplace abuse and occupational exposures in US low-income black, white and Latino workers. Soc Sci Med. 2008;67: 1970–1981. doi: 10.1016/j.socscimed.2008.09.039 [DOI] [PubMed] [Google Scholar]
- 44.Quandt SA, LaMonto NJ, Mora DC, Talton JW, Laurienti PJ, Arcury TA. COVID-19 Pandemic among Latinx Farmworker and Nonfarmworker Families in North Carolina: Knowledge, Risk Perceptions, and Preventive Behaviors. Int J Environ Res Public Health. 2020;17: 5786. doi: 10.3390/ijerph17165786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McClure ES, Vasudevan P, Bailey Z, Patel S, Robinson WR. Racial Capitalism Within Public Health—How Occupational Settings Drive COVID-19 Disparities. Am J Epidemiol. 2020;189: 1244–1253. doi: 10.1093/aje/kwaa126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.U.S. Bureau of Labor Statistics. Unemployment Rate [UNRATE], retrieved from FRED. Federal Reserve Bank of St. Louis; 2020. Nov. Available: https://fred.stlouisfed.org/series/UNRATE [Google Scholar]
- 47.U.S. Bureau of Labor Statistics. Unemployment Rate - Hispanic of Latino [LNS14000009], retrieved from FRED. Federal Reserve Bank of St. Louis; 2020. Nov. Available: https://fred.stlouisfed.org/series/LNS14000009 [Google Scholar]
- 48.U.S. Bureau of Labor Statistics. Unemployment Rate - Black or African American [LNS14000006], retrieved from FRED. Federal Reserve Bank of St. Louis; 2020. Nov. Available: https://fred.stlouisfed.org/series/LNS14000006 [Google Scholar]
- 49.Kochhar R. Fewer mothers and fathers in U.S. are working due to COVID-19 downturn; those at work have cut hours. Washington, D.C.: Pew Research Center; 2020. Oct. Available: https://www.pewresearch.org/fact-tank/2020/10/22/fewer-mothers-and-fathers-in-u-s-are-working-due-to-covid-19-downturn-those-at-work-have-cut-hours/ [Google Scholar]
- 50.Protecting Workers: Guidance on Mitigating and Preventing the Spread of COVID-19 in the Workplace | Occupational Safety and Health Administration. Washington, DC: Occupational Safety & Health Administration; 2021. Jan. Available: https://www.osha.gov/coronavirus/safework [Google Scholar]
- 51.Michaels D, Wagner GR. Occupational Safety and Health Administration (OSHA) and Worker Safety During the COVID-19 Pandemic. JAMA. 2020;324: 1389–1390. doi: 10.1001/jama.2020.16343 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
S1 Appendix: Racial/ethnic distributions within each occupational subset displayed in main text figures
S2 Appendix: Common high-risk occupations by occupational standing quartile