Abstract
Aim
ANGPTL8 is a cytokine expressed and secreted by liver and adipose tissue, and is involved in glucose, lipid, and energy metabolism. Although studies have shown that ANGPTL8 is elevated in type 2 diabetes mellitus (T2DM) and cardiovascular disease, few have examined the association between ANGPTL8 single-nucleotide polymorphisms and the risk of macrovascular complications in T2DM patients. This study aimed to explore the relationship between rs2278426 and carotid intima–media thickening (cIMT) in T2DM.
Methods
A total of 217 T2DM patients and 201 healthy control subjects with normal glucose tolerance were recruited in the study. T2DM patients were divided into two groups: T2DM patients without cIM thickening (cIMT <1 mm, 109 cases) and T2DM patients with cIM thickening (cIMT ≥1 mm, 108 cases). rs2278426 genotypes in all 418 subjects were determined and the risk of T2DM and T2DM with cIM thickening analyzed.
Results
CT+TT-genotype frequency in T2DM was higher than in controls with normal glucose tolerance, and the proportion of the CT+TT genotype in the group with cIMT was higher than in the group (P<0.05). In addition, T alleles were associated with waist:hip ratio, triglycerides, high density–lipoprotein cholesterol, plasma glucose at 2 hours’ oral glucose tolerance, and homeostatic model assessment of insulin resistance (P<0.05).
Conclusion
Generally, carriers of the T allele at rs2278426 are more likely to develop T2DM, and the risk of cIM thickening is significantly increased for T-allele carriers with T2DM, which indicates an increased risk of macroangiopathy.
Keywords: type 2 diabetes mellitus, angiopoietin‑like protein 8, carotid intima–media thickness, polymorphism, rs2278426
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disease, and its incidence is increasing worldwide.1 According to data from the International Diabetes Federation, global DM prevalence increased from 108 million in 1980 to 463 million in 2019. It is estimated that global prevalence will reach 700 million by 2045.2,3 With development in the course of DM, the risk of microvascular and macrovascular complications increases. Among these are microvascular complications, mainly including diabetic nephropathy, retinopathy, and neuropathy, and macrovascular complications, mainly including coronary artery disease, peripheral vascular disease, and carotid artery disease.4 Due to the lack of early symptoms or signs of T2DM, some T2DM patients have DM complications before clinical diagnosis, which seriously threatens disease control and their quality of life.2 As a representative of macrovascular diseases, cardiovascular disease (CVD) is the main cause of death of T2DM patients.5 Therefore, early prevention and diagnosis of DM and its macrovascular complications are particularly important.
The pathological basis of diabetic macroangiopathy is atherosclerosis, which is often evaluated by carotid intima–media thickening (cIMT) from the inner surface to the outer surface of the carotid artery.6,7 Because the process of atherosclerosis can directly affect blood-vessel walls and compensatory dilation often occurs before stenosis, it is difficult to predict the degree of atherosclerosis in the early stages by the degree of stenosis of the lumen secondary to the formation of plaques. Pignoli et al found that cIMT measured by B-ultrasound is highly reliable and repeatable and can be used for the evaluation and diagnosis of atherosclerosis.6,8–10 Since atherosclerosis is closely related to cardiovascular and other major vascular diseases, cIMT has also been widely used in observational epidemiological studies and clinical trials as an alternative marker of CVD.11–17
T2DM macroangiopathy is affected by many factors. Research data show that >75% of T2DM patients have DM-related lipid-metabolism abnormalities, due to hyperinsulinemia, insulin (Ins) resistance, and apoptosis of islet β cells, which are mainly mixed-lipid abnormalities, which increase the incidence of macrovascular diseases.5,18–22 In recent decades, genetic factors have also been widely studied. More and more susceptibility genes have been found, and single-nucleotide polymorphisms (SNPs) of these susceptible genes have also been proved to be related to the occurrence and development of macroangiopathy.23–26 Therefore, SNP-related research has important clinical value in the prevention, diagnosis, treatment, and prognosis of T2DM and macroangiopathy.
ANGPTL8 (also known as RIFL, lipasin and betatrophin) is a cytokine secreted mainly by the liver and adipose cells. Its expression and secretion are affected by the nutritional or metabolic state of the body, and it can regulate the metabolism of glucose and lipid to different degrees.27–32 In previous studies, our research team found that the serum concentration of ANGPTL8 is significantly increased in newly diagnosed T2DM patients.33 In follow-up clinical studies, other researchers obtained the same results with us,34 and serum ANGPTL8 concentration has been found to be independently related to fasting blood glucose and T2DM.35 In addition, ANGPTL8 is also associated with pre-DM, retinopathy, and renal function in T2DM patients.36–38 On the other hand, ANGPTL8 and its protein-family members can participate in the regulation of lipid metabolism by inhibiting the activity of lipoprotein lipase (LPL) and increasing the level of circulating triglycerides (TGs).31,39 Clinical studies have shown that the level of circulating ANGPTL8 in obese and overweight patients is significantly increased.40 Therefore, ANGPTL8 may be involved in the occurrence and development of T2DM and its macrovascular lesions through its important regulatory role in glucose and lipid metabolism.
The rs2278426 polymorphism of the ANGPTL8 gene is an SNP locus discovered in recent years. The wild-type gene of this locus is C and the mutant gene T. The frequency of the T allele is about 5% in Caucasians, 25% in Mexican Americans, and 50% in Native Americans. In a Japanese study, T-allele carriers were more likely to have T2DM and impaired glucose tolerance.26 Other researchers have also found that the T allele is related to low density–lipoprotein cholesterol (LDL-C) and high-density–lipoprotein cholesterol (HDL-C), and individuals carrying the T allele may have lower total cholesterol (TC) and HDL-C levels.25 However, the relationship between polymorphism of this locus and cIMT in T2DM has not been reported. In this study, we explored the relationship between the rs2278426 polymorphism of ANGPTL8 and cIMT in T2DM, which may provide a new way for the early prediction, prevention, and diagnosis of T2DM macroangiopathy.
Methods
Subjects for Genotyping
We genotyped the ANGPTL8 rs2278426 SNP in 217 T2DM patients and 201 healthy control subjects with normal glucose tolerance (NGT) from Jiangsu Province, China. T2DM patients were divided into two groups: those without cIMT (cIMT<1 mm, 109 cases) and those with cIMT (cIMT≥1 mm, 108 cases). We used the WHO DM diagnosis and classification standard of 1999, ie, the blood glucose ≥11.1mmol/L, fasting blood glucose≥7.0mmol/L, or plasma glucose at 2 hours (2hPG) ≥11.1mmol/L on the oral glucose-tolerance test.
Using a commercial kit (DP348-03; Tiangen Biotech, Beijing, China), genomic DNA was isolated from whole blood cells treated with EDTA according to product specifications. We mixed 500 μL blood with 1 mL cell lysate, centrifuged at 10,000 rpm for 1 minute, discarded the supernatant, retained the nucleus precipitation, and mixed with 200 μL buffer. Then, we added 220 μL prepared protease K solution, mixed this well, and kept it at 56°C for 10 minutes. After 5 minutes at room temperature, proper amount of buffer solution was added and the mixture transferred to the adsorption column, then centrifuged at 12,000 rpm for 30 seconds. Tinse solution was added, the whole centrifuged at 12,000 rpm for 30 seconds, and the adsorption column washed and dried for 2 minutes. DNA on the column was eluted by centrifugation at 12,000 rpm for 2 minutes, and genomic DNA was obtained. Consent was obtained from all T2DM patients and control subjects, and the experimental design was approved by the ethics committee of Affiliated Hospital of Jiangsu University.
Genotyping of Polymorphisms
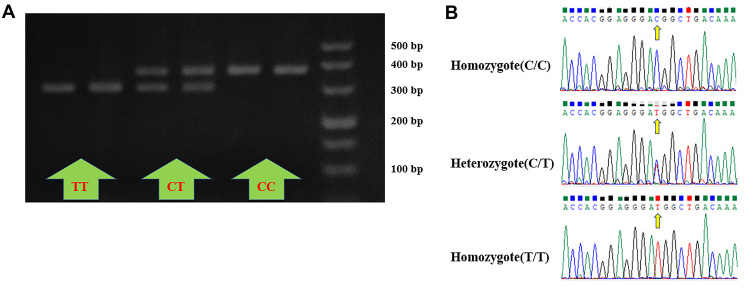
Using the genomic DNA of subjects as the template, DNA fragments containing ANGPTL8 rs2278426 was amplified by PCR (forward primer 5ʹ-CAGGAGTTCTATTGTGCGGC-3ʹ, reverse primer 5ʹ-CCTGATGCAACTATCGCACC-3ʹ). PCR products were digested by restriction enzymes and products analyzed by 3% agarose-gel electrophoresis (80V, 45 minutes). PCR products containing the T allele can be divided into two fragments of 331bp and 56bp by restriction endonuclease (BseGI). Because of the smallness of the 56 bp fragment, the migration of electrophoresis is too fast, and it cannot be observed. Therefore, the electrophoretic results of restriction-enzyme products were CC (one band at 387 bp), CT (two bands at 387 bp and 331 bp), and TT (one band at 331 bp; Figure 1A). PCR reaction and restriction enzyme digestion–reaction kits were purchased from Thermo Fisher Scientific.
Figure 1.
Genotyping and validation results of rs2278426. (A) Electrophoretic results of restriction-enzyme products: CC (one band at 387 bp), CT (two bands at 387 bp and 331 bp), and TT (one band at 331 bp). (B) Results of DNA sequencing: CC, CT, and TT genotypes from top to bottom, and position indicated by arrows was the mutation site.
In addition, we randomly selected PCR products representing different genotypes for two-way sequencing analysis to verify the genotyping results of restriction enzyme–digestion reaction. The results showed that the similarity between the PCR products of ANGPTL8 rs2278426 and the original gene provided by the NCBI website was 99%, and the cleavage site was the same as the mutation site. The results of DNA sequencing were consistent with those of restriction-enzyme digestion. The two-way gene sequencing was completed by the Beijing Genomics Institution, and results were analyzed with Chromas 2.33 (Figure 1B).
Anthropometric and Biochemical Measurements
Neck circumference (NC), waist circumference (WC), and hip circumference (HC) of all patients were measured to the nearest 0.1 cm. Waist:hip ratio (WHR) was calculated as WC divided by HC, and BMI calculated as weight divided by height squared (kg/m2). Glucose oxidase was used to detect plasma glucose at each time point of the oral glucose-tolerance test and chemiluminescence used to measure Ins levels. Hemoglobin A1C (HbA1c) was detected by HPLC. HDL-C, LDL-C, TGs, and TC were measured by the kinetic method (Beckman Coulter, Brea, CA, USA). The Ins-resistance index was assessed by a steady-state model (Homeostatic Model Assessment of Insulin Resistance [HOMA-IR] = fasting plasma glucose [FPG] × fasting Ins [Fins]/22.5). The cIMT was measured by ultrasound, and mean values of left and right common cIMT were calculated.
Statistical Analysis
Data were analyzed using IBM SPSS version 20.0 software. Quantitative data conforming to normal distribution are expressed as means ± SD, and Student’s t-test was used for comparison between the groups. For data of abnormal distribution, medians and quartile spacingwere used, and for comparison between the groups the nonparametric Mann–Whitney U test was used. Qualitative data are expressed as frequency, and χ2 tests were used to compare differences in rs2278426 genotype and allele frequency between the groups. Logistic regression was used to estimate the relative risk of genotypes. Differences were considered significant at P<0.05. Distribution of SNP genotype and allele frequency were calculated using direct counting, then tested for fitting Hardy-Weinberg balance with goodness-of-fit χ2 test. When P>0.05, the genotype-distribution frequency conforms with the Hardy–Weinberg equilibrium law, and samples are representative of the population.
Results
Comparison of General Data and Biochemical Indices
Compared with the NGT group, BMI, NC, WC, WHR, systolic blood pressure (SBP), FPG, 2hPG, HbA1c, FIns), Ins at 2h on Ins-release test (2hIns), and HOMA-IR increased, while HDL-C and LDL-C decreased significantly in the T2DM without cIMT group (cIMT<1 mm, P<0.05). On the other hand, BMI, NC, WC, HC, WHR, SBP, diastolic BP (DBP), total TGs, FPG, 2hPG, HbA1c, FIns, 2hIns, and HOMA-IR were significantly higher, while HDL-C was significantly lower in the T2DM with cIMT group (cIMT≥1 mm) than in the NGT group (P<0.05). In T2DM patients, levels of HC, SBP, DBP, TG, and FIns were significantly higher in the cIMT group, while HDL-C was significantly lower in the cIMT group (P<0.05, Table 1).
Table 1.
Comparison of General Data and Biochemical Indices
| NGT (n=201) | T2DM (n=217) | ||
|---|---|---|---|
| cIMT <1 mm (n=109) | cIMT ≥1 mm (n=108) | ||
| Age | 48.78±9.31 | 58.06±12.21 | 65.71±9.40 |
| Sex (M/F) | 92/109 | 62/47 | 66/42 |
| BMI (kg/m2) | 23.69±3.75 | 24.63±3.49* | 25.32±3.19* |
| NC (cm) | 34.11±3.38 | 36.15±3.47* | 36.48±3.33* |
| WC (cm) | 81.47±11.83 | 88.90±10.04* | 91.36±8.90* |
| HC (cm) | 94.62±7.09 | 95.02±8.11 | 97.30±7.16*,† |
| WHR | 0.85±0.07 | 0.93±0.05* | 0.93±0.06* |
| SBP (mmHg) | 120.25±15.04 | 130.71±16.12* | 136.52±15.01*,† |
| DBP (mmHg) | 78.25±11.19 | 78.77±9.55 | 81.38±9.25*,† |
| TC (mmol/L) | 4.69±0.83 | 4.56±1.04 | 4.82±1.03 |
| HDL-C (mmol/L) | 1.37±0.99 | 1.12±0.32* | 0.99±0.25*,† |
| LDL-C (mmol/L) | 2.70 (2.29–3.19) | 2.53 (2.03,2.90)* | 2.62 (2.05,3.23) |
| TGs (mmol/L) | 1.39±0.82 | 1.55±0.73 | 1.92±0.76*,† |
| FPG (mmol/L) | 5.15±0.46 | 9.89±3.56* | 9.40±2.97* |
| 2hPG (mmol/L) | 5.88±1.11 | 17.76±5.53* | 17.78±5.12* |
| HbA1c | 5.40±0.28 | 8.96±1.91* | 8.82±1.85* |
| FIns (μIU/mL) | 5.68 (4.12–7.94) | 7.28 (4.14,12.47)* | 9.85 (5.07,16.00)*,† |
| 2hIns (μIU/mL) | 25.76 (17.14–43.82) | 31.01 (16.94,52.34) | 40.09 (24.62,63.74)* |
| HOMA-IR | 1.31 (0.92–1.84) | 3.07 (1.83,5.11)* | 4.04 (2.22,6.65)* |
Notes: *P≤0.05between NGT and cIMT<1 mm or cIMT ≥1 mm; P≤0.05 between cIMT<1 mm and cIMT ≥1 mm.
Abbreviations: BMI, body -mass index; NC, neck circumference; WC, waist circumference; HC, hip circumference; WHR, waist:hip ratio; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL-C, highdensity–lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; TGs, total triglycerides; FPG, fasting plasma glucose; 2hPG, plasma glucose at 2 hours (oral glucose-tolerance test); HbA1c, hemoglobin A1C; Fins, fasting insulin; 2hIns, insulin at 2 hours on insulin-release test.
rs2278426 Gene Polymorphism and Risk of T2DM
Frequency of the CC, CT, and TT genotypes was 65.2%, 29.9%, and 5.0% in the NGT group and 54.4%, 38.7%, and 6.9% in the T2DM group, respectively. The Hardy–Weinberg test was used to test genetic balance in all subjects (χ2=0.367, P>0.05 in controls; χ2=0, P>0.05 in T2DM), as shown in Table 2. There were significant differences in the distribution of genotypes between the two groups, and the frequency of CT-genotype distribution in the T2DM group increased significantly. In analysis of the dominant model, the distribution frequency of CT+TT in the T2DM group (45.6%) was significantly higher than in the NGT group (34.8%, P<0.05). Relative-risk analysis showed that the CT+TT genotype was a risk factor of T2DM (OR 1.57, 95% CI 1.05–2.32). Distribution of rs2278426 alleles also showed the same trend of difference. Distribution frequency of the T allele in the T2DM group was 26.3%, significantly higher than in the NGT group (19.9%, P<0.05), and T carriers had a higher risk of T2DM (OR 1.43, 95% CI 1.03–1.98; Table 3).
Table 2.
Hardy-Weinberg Equilibrium Coincidence Test of rs2278426 SNP
| Genotype | NGT | χ2 | P | T2DM | χ2 | P | ||
|---|---|---|---|---|---|---|---|---|
| Observed Cases | Expected Cases | Observed Cases | Expected Cases | |||||
| C/C | 131 | 129 | 0.367 | 0.833 | 118 | 118 | 0.000 | 0.999 |
| C/T | 60 | 64 | 84 | 84 | ||||
| T/T | 10 | 8 | 15 | 15 | ||||
Table 3.
rs2278426 Gene Polymorphism and Risk of T2DM
| NGT (n=201) | T2DM (n=217) | P | OR (95% CI) | |
|---|---|---|---|---|
| rs2278426 (C/T) | ||||
| CC | 131 (65.2%) | 118 (54.4%) | 0.079 | |
| CT | 60 (29.9%) | 84 (38.7%) | 0.036* | 1.55 (1.02–2.35) |
| TT | 10 (5.0%) | 15 (6.9%) | 0.229 | 1.66 (0.72–3.84) |
| Recessive model | ||||
| CC+CT | 191 (95.0%) | 202 (93.1%) | ||
| TT | 10 (5.0%) | 15 (6.9%) | 0.404 | 1.41 (0.62–3.23) |
| Dominant model | ||||
| CC | 131 (65.2%) | 118 (54.4%) | ||
| CT+TT | 70 (34.8%) | 99 (45.6%) | 0.025* | 1.57 (1.05–2.32) |
| Allele | ||||
| C | 322 (80.1%) | 320 (73.7%) | ||
| T | 80 (19.9%) | 114 (26.3%) | 0.029* | 1.43 (1.03–1.98) |
Note: *P≤0.05.
rs2278426 Gene Polymorphism and Risk of Carotid Intima–Media Thickening in T2DM
Frequency of the CC, CT and TT genotypes was 65.1%, 29.4%, and 5.5% in the T2DM without cIMT group and 43.5%, 48.1%, and 8.3% in the T2DM with cIMT group. There were significant differences in genotype distribution between the groups (P<0.05). Frequency of the CC genotype was lower and that of the CT+TT genotype higher in the T2DM with cIMT group. In the dominant model, distribution frequency of the CT+TT genotype was significantly higher in the T2DM with cIMT group (56.5%) than the T2DM without cIMT group (34.9%, P<0.05). Relative-risk analysis showed that the CT+TT genotype was a risk factor of cIMT in T2DM patients (OR 2.42, 95% CI 1.40–4.19). The distribution of rs2278426 alleles also showed the same trend. Frequency of the T allele was 32.4% in the T2DM with cIMT group, significantly higher than in the T2DM without cIMT group (20.2%, P<0.05), and T2DM patients with the T allele had a higher risk of cIMT (OR 1.89, 95% CI 1.22–2.93); Table 4).
Table 4.
rs2278426 Gene Polymorphism and the Risk of Carotid Intima–Media Thickening in T2DM
| cIMT<1 mm (n=109) | cIMT ≥1 mm (n=108) | P | OR (95% CI) | |
|---|---|---|---|---|
| rs2278426 (C/T) | ||||
| CC | 71 (65.1%) | 47 (43.5%) | 0.006* | |
| CT | 32 (29.4%) | 52 (48.1%) | 0.002* | 2.45 (1.38–4.35) |
| TT | 6 (5.5%) | 9 (8.3%) | 0.136 | 2.26 (0.75–6.78) |
| Recessive model | ||||
| CC+CT | 103 (94.5%) | 99 (91.7%) | ||
| TT | 6 (5.5%) | 9 (8.3%) | 0.411 | 1.56 (0.53–4.54) |
| Dominant model | ||||
| CC | 71 (65.1%) | 47 (43.5%) | ||
| CT+TT | 38 (34.9%) | 61 (56.5%) | 0.001* | 2.42 (1.40–4.19) |
| Allele | ||||
| C | 174 (79.8%) | 146 (67.6%) | ||
| T | 44 (20.2%) | 70 (32.4%) | 0.004* | 1.89 (1.22–2.93) |
Note: *P≤0.05.
Comparison of General Data among Genotypes
In all subjects, WHR with the CT+TT genotype was significantly higher than the CC genotype. This may be due to relatively larger WC in CT+TT carriers (P=0.071), but in the NGT and T2DM groups, the difference weakened. In the NGT group, SBP and DBP with the CT+TT genotype were slightly higher than the CC genotype, but did not reach statistical significance (P=0.052 and P=0.058, respectively). There were no significant differences among the genotypes in other general data (Table 5).
Table 5.
Comparison of General Data and Biochemical Indices Among Genotypes
| Overall | NGT | T2DM | |||||||
|---|---|---|---|---|---|---|---|---|---|
| CC | CT+TT | P | CC | CT+TT | P | CC | CT+TT | P | |
| WC (cm) | 85.13±11.81 | 87.20±11.04 | 0.071 | 80.66±11.85 | 83.00±11.70 | 0.182 | 90.09±9.61 | 90.17±9.52 | 0.949 |
| WHR | 0.89±0.07 | 0.91±0.07 | 0.012* | 0.85±0.07 | 0.86±0.07 | 0.130 | 0.93±0.05 | 0.94±0.05 | 0.483 |
| SBP (mmHg) | 126.18±17.09 | 128.66±16.33 | 0.140 | 118.75±14.74 | 123.07±15.29 | 0.052 | 134.44±15.73 | 132.61±15.94 | 0.399 |
| DBP (mmHg) | 78.63±10.92 | 80.03±9.45 | 0.175 | 77.16±11.57 | 80.30±10.20 | 0.058 | 80.27±9.94 | 79.84±8.93 | 0.744 |
| TC (mmol/L) | 4.67±0.95 | 4.72±0.94 | 0.551 | 4.63±0.84 | 4.82±0.81 | 0.116 | 4.71±1.06 | 4.66±1.02 | 0.688 |
| HDL-C (mmol/L) | 1.25±0.70 | 1.15±0.79 | 0.167 | 1.38±0.91 | 1.34±1.14 | 0.802 | 1.10±0.26 | 1.01±0.32 | 0.020* |
| LDL-C (mmol/L) | 2.75±1.48 | 2.70±0.78 | 0.690 | 2.90±1.89 | 2.89±0.74 | 0.954 | 2.58±0.79 | 2.57±0.79 | 0.892 |
| TG (mmol/L) | 1.42±0.68 | 1.78±0.93 | 0.000* | 1.24±0.65 | 1.65±1.01 | 0.001* | 1.62±0.66 | 1.87±0.87 | 0.014* |
| FPG (mmol/L) | 7.25±3.26 | 7.83±3.28 | 0.076 | 5.12±0.49 | 5.20±0.38 | 0.236 | 9.62±3.40 | 9.69±3.15 | 0.866 |
| 2hPG (mmol/L) | 11.47±7.09 | 12.94±7.08 | 0.038* | 5.82±1.08 | 6.00±1.14 | 0.271 | 17.70±5.50 | 17.85±5.12 | 0.837 |
| HbA1c | 7.05±2.22 | 7.45±2.20 | 0.075 | 5.40 (5.20–5.60) | 5.40 (5.20–5.60) | 0.739 | 8.90±1.95 | 8.89±1.79 | 0.975 |
| FIns (μIU/mL) | 6.24 (4.05–10.19) | 7.22 (4.79–12.35) | 0.110 | 5.41 (3.85–7.35) | 6.22 (4.73–8.59) | 0.623 | 8.07 (4.37–14.07) | 9.35 (5.11–15.75) | 0.542 |
| 2hIns (μIU/mL) | 28.86 (17.14–49.77) | 36.07 (20.17–55.83) | 0.005* | 24.62 (17.13–43.59) | 33.44 (17.43–49.53) | 0.947 | 34.42 (17.78–51.20) | 40.70 (21.89–57.99) | 0.247 |
| HOMA-IR | 1.68 (1.07–3.46) | 2.33 (1.36–4.29) | 0.005* | 1.21 (0.82–1.70) | 1.42 (1.03–2.00) | 0.085 | 3.29 (1.87–5.73) | 3.66 (2.33–6.58) | 0.249 |
Note: *P≤0.05.
Comparison of Lipid-Metabolism Indices among Genotypes
In both overall subjects and the NGT and T2DM groups individually, we found that TGs of CT+TT-genotype carriers were significantly higher than CC-genotype carriers (P<0.05). Also, in the T2DM group HDL-C levels with the CT+TT genotype were significantly lower than with the CC genotype (P<0.05), and no significant difference was found in subjects overall or the NGT group (Table 5).
Comparison of Glucose- and Insulin-Metabolism Indices among Genotypes
Compared with CC-genotype carriers, CT+TT-genotype carriers had significantly higher 2hPG overall. FPG levels showed a similar trend, but did not reach statistical significance (P=0.076). HbA1c levels with the CT+TT genotype were also higher than with the CC genotype (P=0.075). Levels of 2hIns and HOMA-IR with the CT+TT genotype were significantly higher than those with the CC genotype (P<0.05). In the NGT group and T2DM groups, there was no significant difference in glucose or Ins metabolism between the genotypes, except that HOMA-IR with the CT+TT genotype in the NGT group was slightly higher than with the CC genotype (P=0.085, Table 5).
Logistic Regression Analysis of Risk of Carotid Intima–Media Thickening in T2DM
Risk factors of cIMT in T2DM patients were age, sex, BMI, TGs, SBP, and rs2278426 T allele. After adjusting for age, sex, BMI, TGs, and SBP, the rs2278426 T allele was still an independent risk factor of cIMT in T2DM (Table 6).
Table 6.
Logistic Regression Analysis of Risk of Carotid Intima–Media Thickening in T2DM
| β | SE | Wald χ2 | P | OR | 95% CI | |
|---|---|---|---|---|---|---|
| rs2278426 (T) | 0.939 | 0.314 | 8.921 | 0.003 | 2.557 | 1.381–4.734 |
| Age | 0.073 | 0.017 | 19.038 | 0.000 | 1.075 | 1.041–1.111 |
| Sex | 0.447 | 0.315 | 2.013 | 0.156 | 1.563 | 0.843–2.898 |
| BMI | 0.007 | 0.048 | 0.019 | 0.891 | 1.007 | 0.917–1.105 |
| TGs | 0.628 | 0.225 | 7.793 | 0.005 | 1.875 | 1.206–2.914 |
| SBP | 0.010 | 0.010 | 0.935 | 0.333 | 1.010 | 0.990–1.031 |
| Constant | −8.746 | 1.934 | 20.444 | 0.000 | 0.000 |
Discussion
In this study, we found that the ANGPTL8 gene rs2278426 polymorphism was related to T2DM and cIMT in T2DM, and also to Ins resistance, glucose, and lipid metabolism. In general, the T allele of this locus can increase the risk of T2DM. At the same time, T2DM patients with the T allele are more likely to have cIMT. In addition to environmental factors, the occurrence and development of T2DM are closely related to genetic factors. Many genes and polymorphisms have been confirmed to be related to T2DM. It has been found that the T allele at ANGPTL8 rs2278426 significantly increased the risk of T2DM.26 In this study, we first verified previous research results and reached the same conclusions. Analysis of the dominant model showed that the frequency of the CT+TT genotype in T2DM group (45.6%) was significantly higher than in the NGT group (34.8%). Relative-risk analysis showed that the CT+TT genotype was a risk factor of T2DM (OR 1.57, 95% CI 1.05–2.32). Distribution of rs2278426 alleles also showed the same trend of difference. T carriers had a higher risk of T2DM (OR 1.43, 95% CI 1.03–1.98), suggesting that the rs2278426 polymorphism is closely related to T2DM.
With disease progression, most T2DM patients will inevitably develop diabetic complications, such as macroangiopathy, microangiopathy, and neuropathy, which will seriously affect their quality of life and increase the social burden.4 Among all complications, CVD is the main cause of death in T2DM patients. T2DM macroangiopathy is characterized by arterial IMT and atherosclerosis, and its occurrence is affected by many factors, such as BP, blood glucose, blood-lipid level, Ins resistance, while genetic factors have been studied widely in recent decades.25,26 Among these, SNPs of various susceptibility genes have been confirmed to be related to the occurrence and development of IMT, atherosclerosis, and macroangiopathy in T2DM patients.23–26 In this study, we found that rs2278426-genotype frequency was different in T2DM patients with and without cIMT. Genotype distribution of ANGPTL8 rs2278426 in T2DM was CC 47 (43.5%), CT 52 (48.1%), and TT nine (8.3%). Frequency of the CT genotype increased significantly in the T2DM group, while the CC genotype decreased significantly. Further dominant-model analysis showed that the frequency of the CT+TT genotype in T2DM group was significantly higher than in the T2DM group (34.9%). Relative-isk analysis showed that the CT+TT genotype was a risk factor of cIMT in T2DM patients (OR 2.42, 95% CI 1.40–4.19). Distribution of rs2278426 alleles also showed the same trend. T2DM patients with the T allele were at higher risk of cIMT (OR 1.89, 95% CI 1.22–2.93). Multivariate logistic regression analysis showed that the T allele of rs2278426 may be an independent risk factor of cIMT in T2DM patients (OR 2.557, P=0.003) after adjusting for age, sex, BMI, and other factors. Therefore, the rs2278426 gene polymorphism may be related to the risk of cIMT in T2DM patients. We note that in another study, the researchers also found that frequency of the T allele of rs2278426 in CVD patients was higher than in non-CVD patients, but the difference was not statistically significant.41 This may be due to ethnic differences or different grouping indicators.
T2DM macroangiopathy is characterized by atherosclerosis. In addition to the classic lipid-metabolism factors, the occurrence and development of T2DM macroangiopathy are also related to many factors, such as Ins resistance and hyperglycemia. ANGPTL8 is composed of 198 amino acids, about 22 kDa in size. It is a cytokine secreted mainly by liver and adipose cells,27 and the relationship between ANGPTL8 and lipid metabolism, glucose metabolism, and Ins resistance has been widely studied.29–33 A previous study by our group found that levels of circulating ANGPTL8 in patients with newly diagnosed T2DM was significantly higher than in healthy controls with NGT.33 Later, more and more studies found that ANGPTL8 is also related to pre-DM, retinopathy, and renal function in T2DM patients.36–38 Some researchers believe that the effect of ANGPTL8 on glucose metabolism may be related to Ins resistance. In animal experiments, expression of ANGPTL8 is increased in OB/OB, DB/DB and pregnant mice. In Ins-resistant mice induced by S961, serum levels of ANGPTL8 also increased, and similar results have been found in clinical studies.34,42–45 On the other hand, Guo et al found that in HepG2 cells, ANGPTL8 can improve Ins resistance through the Akt–GSK3β or Akt–FoxO1 signaling pathway.32 Similarly, Luo et al found that ANGPTL8 can improve Ins resistance and adipose-tissue inflammation in diet-induced obese mice.46 Therefore, changes in protein structure and stability caused by ANGPTL8 rs2278426 polymorphism may lead to Ins resistance and glucose-metabolism disorders.13 In this study, we found that 2hPG, FIns, and HOMA-IR with the CT+TT genotype were significantly higher than with the CC genotype (P<0.05). These results suggest that ANGPTL8 rs2278426 polymorphismmay be involved in the process of T2DM and cIMT in T2DM through Ins resistance and glucose-metabolism disorders.
On the other hand, regulation of ANGPTL8 on lipid metabolism may be realized by changing the active state of LPL. Two LPLs can be combined to form a biologically active LPL dimer, which hydrolyzes TGs from chylomicrons and very low–density lipoproteins to free fatty acids, which are absorbed by such peripheral tissue as fat, muscle, and heart, and also leads to the production of atherosclerotic factors, such as LDL-C.29 Mamputu et al found that exogenous LPL can increase the adhesiveness of human monocytes and make it easier for them to enter the vascular wall. Therefore, the expression of LPL in the arterial wall promotes the formation of foam cells, which is very important in the pathogenesis of atherosclerosis.47 In addition, LPL can also promote proliferation of smooth-muscle cells, and proliferation and transformation of smooth-muscle cells also play an important role in the occurrence and development of atherosclerosis.48 Therefore, LPL is considered an important atherogenic factor. After ANGPTL8 is combined with ANGPTL3, it can destroy the dimer of LPL and inhibit the activity of LPL.49 In clinical studies, levels of ANGPTL8 in the circulation of obese and overweight patients increases significantly.40 The T allele at rs2278426 of ANGPTL8 represents Arg59Trp replacement, but the circulating level of ANGPTL8 is not affected.50 Bioinformatis analysis has shown that Arg59Trp replacement caused by the T allele can reduce stability of the ANGPTL8 protein.51 Therefore, the protein’s stability and interaction with ANGPTL3 may change. In subjects overall, as well as both the NGT and T2DM groups, we found that TG levels with the CT+TT genotype were significantly higher than with the CC genotype (P<0.05), while in the T2DM group HDL-C level of the CT+TT genotypes were significantly lower than the CC genotype (P<0.05). Therefore, the higher risk of cIMT in T-allele carriers may also be caused by the abnormal regulation of LPL and disorders in lipid metabolism caused by structural change of the ANGPTL8 protein.13 The rs2278426 T allele of the ANGPTL8 gene may cause changes in protein structure, disorder the inhibition of ANGPTL8 on LPL activity, increase the production of atherosclerotic factors, and increase the risk of cIMT in T2DM patients.
In general, this study found that ANGPTL8 rs2278426 was related to blood glucose, Ins resistance, TG levels, and cIMT in T2DM. Levels of blood glucose, TGs, and Ins resistance in CT+TT-genotype and T-allele carriers were significantly higher than in CC-genotype or C-allele carriers. Combined with previous studies and the results of this study, we speculate that ANGPTL8 polymorphism may participate in the process of cIMT by affecting Ins resistance, blood-glucose control, and lipid metabolism by regulating LPL activity. At the same time, there are some shortcomings in this study. Firstly, the sample in this study was rather small, secondly, we did not strictly restrict the use of statins in T2DM patients, and thirdly, this was a cross-sectional study, which cannot fully reveal the mechanism of gene polymorphism affecting the risk of cIMT. In future, while controlling the influence of drug factors, prospective studies of larger samples should be carried out so as to explore the mechanism behind them more deeply. In sum, we found that the CT+TT genotype of ANGPTL8 rs2278426 increased the risk of cIMT in T2DM patients.
Conclusion
In this study, we found that frequency of the CT+TT genotype at rs2278426 was significantly increased in T2DM patients with cIMT comparws to those with T2DM without cIMT. The rs2278426 polymorphism of the ANGPTL8 gene was associated with glucose, lipid, Ins metabolism, and risk of cIMT in T2DM patients. Compared with the CC genotype, the CT+TT genotype increased the risk of cIMT in T2DM patients.
Funding
This study was supported in part by grants from the National Natural Science Foundation of China (81870548, 81570721), Key Research and Development Projects of Social Development in Jiangsu Province, China (BE2018692), the Natural Science Foundation of Jiangsu Province, China (BK2019222, BK20151331), the High Caliber Medical Personnel Foundation of Jiangsu Province (LGY2016053), the Six Talent Peaks Project in Jiangsu Province (2015-WSN-006), the Science and Technology Commission of Zhenjiang City (SH2019041), and the 169-Phase V Science Research Project of Zhenjiang.
Compliance with Ethical Standards
Patients and control subjects were informed about the purpose of the study, which was conducted in accordance with the Declaration of Helsinki.
Disclosure
The authors report no potential conflicts of interest in this work.
References
- 1.Kahn SE. Clinical review 135: the importance of beta-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab. 2001;86(9):4047–4058. doi: 10.1210/jcem.86.9.7713 [DOI] [PubMed] [Google Scholar]
- 2.Carracher AM, Marathe PH, Close KL. International Diabetes Federation 2017. J Diabetes. 2018;10(5):353–356. doi: 10.1111/1753-0407.12644 [DOI] [PubMed] [Google Scholar]
- 3.NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants [published correction appears in Lancet. 2017 Feb 4;389(10068):e2]. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beckman JA, Creager MA, Libby P. Diabetes and atherosclerosis: epidemiology, pathophysiology, and management. JAMA. 2002;287(19):2570–2581. doi: 10.1001/jama.287.19.2570 [DOI] [PubMed] [Google Scholar]
- 5.Vamos EP, Millett C, Parsons C, et al. Nationwide study on trends in hospital admissions for major cardiovascular events and procedures among people with and without diabetes in England, 2004–2009. Diabetes Care. 2012;35(2):265–272. doi: 10.2337/dc11-1682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pignoli P, Tremoli E, Poli A, et al. Intimal plus medial thickness of the arterial wall: a direct measurement with ultrasound imaging. Circulation. 1986;74(6):1399–1406. doi: 10.1161/01.cir.74.6.1399 [DOI] [PubMed] [Google Scholar]
- 7.Wikstrand J. Methodological considerations of ultrasound measurement of carotid artery intima-media thickness and lumen diameter. Clin Physiol Funct Imaging. 2007;27(6):341–345. doi: 10.1111/j.1475-097X.2007.00757.x [DOI] [PubMed] [Google Scholar]
- 8.Bots ML, Mulder PG, Hofman A, et al. Reproducibility of carotid vessel wall thickness measurements. The Rotterdam Study. J Clin Epidemiol. 1994;47(8):921–930. doi: 10.1016/0895-4356(94)90196-1 [DOI] [PubMed] [Google Scholar]
- 9.Persson J, Formgren J, Israelsson B, et al. Ultrasound-determined intima-media thickness and atherosclerosis. Direct and indirect validation. Arterioscler Thromb. 1994;14(2):261–264. doi: 10.1161/01.atv.14.2.261 [DOI] [PubMed] [Google Scholar]
- 10.Espeland MA, Craven TE, Riley WA, et al. Reliability of longitudinal ultrasonographic measurements of carotid intimal-medial thicknesses. Asymptomatic Carotid Artery Progression Study Research Group. Stroke. 1996;27(3):480–485. doi: 10.1161/01.str.27.3.480 [DOI] [PubMed] [Google Scholar]
- 11.Coskun U, Yildiz A, Esen OB, et al. Relationship between carotid intima-media thickness and coronary angiographic findings: a prospective study. Cardiovasc Ultrasound. 2009;7:59. doi: 10.1186/1476-7120-7-59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geroulakos G, O’Gorman DJ, Kalodiki E, et al. The carotid intima-media thickness as a marker of the presence of severe symptomatic coronary artery disease. Eur Heart J. 1994;15(6):781–785. doi: 10.1093/oxfordjournals.eurheartj.a060585 [DOI] [PubMed] [Google Scholar]
- 13.Crouse JR, Toole JF, McKinney WM, et al. Risk factors for extracranial carotid artery atherosclerosis. Stroke. 1987;18(6):990–996. doi: 10.1161/01.str.18.6.990 [DOI] [PubMed] [Google Scholar]
- 14.Poli A, Tremoli E, Colombo A, et al. Ultrasonographic measurement of the common carotid artery wall thickness in hypercholesterolemic patients. A new model for the quantitation and follow-up of preclinical atherosclerosis in living human subjects. Atherosclerosis. 1988;70(3):253–261. doi: 10.1016/0021-9150(88)90176-1 [DOI] [PubMed] [Google Scholar]
- 15.Tell GS, Howard G, McKinney WM. Risk factors for site specific extracranial carotid artery plaque distribution as measured by B-mode ultrasound. J Clin Epidemiol. 1989;42(6):551–559. doi: 10.1016/0895-4356(89)90151-0 [DOI] [PubMed] [Google Scholar]
- 16.Salonen R, Salonen JT. Progression of carotid atherosclerosis and its determinants: a population-based ultrasonography study. Atherosclerosis. 1990;81(1):33–40. doi: 10.1016/0021-9150(90)90056-o [DOI] [PubMed] [Google Scholar]
- 17.Salonen R, Salonen JT. Carotid atherosclerosis in relation to systolic and diastolic blood pressure: kuopio Ischaemic Heart Disease Risk Factor Study. Ann Med. 1991;23(1):23–27. doi: 10.3109/07853899109147926 [DOI] [PubMed] [Google Scholar]
- 18.Taskinen MR, Borén J. New insights into the pathophysiology of dyslipidemia in type 2 diabetes. Atherosclerosis. 2015;239(2):483–495. doi: 10.1016/j.atherosclerosis.2015.01.039 [DOI] [PubMed] [Google Scholar]
- 19.Taskinen MR. Type 2 diabetes as a lipid disorder. Curr Mol Med. 2005;5(3):297–308. doi: 10.2174/1566524053766086 [DOI] [PubMed] [Google Scholar]
- 20.Chapman MJ, Ginsberg HN, Amarenco P, et al. Triglyceride-rich lipoproteins and high-density lipoprotein cholesterol in patients at high risk of cardiovascular disease: evidence and guidance for management. Eur Heart J. 2011;32(11):1345–1361. doi: 10.1093/eurheartj/ehr112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24(4):683–689. doi: 10.2337/diacare.24.4.683 [DOI] [PubMed] [Google Scholar]
- 22.Nichols GA, Hillier TA, Erbey JR, et al. Congestive heart failure in type 2 diabetes: prevalence, incidence, and risk factors. Diabetes Care. 2001;24(9):1614–1619. doi: 10.2337/diacare.24.9.1614 [DOI] [PubMed] [Google Scholar]
- 23.Ma X, Lu R, Gu N, et al. Polymorphisms in the glucagon-like peptide 1 receptor (GLP-1R) gene are associated with the risk of coronary artery disease in chinese han patients with type 2 diabetes mellitus: a case-control study. J Diabetes Res. 2018;2018:1054192. doi: 10.1155/2018/1054192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ezhilarasi K, Dhamodharan U, Vijay V. BSMI single nucleotide polymorphism in vitamin D receptor gene is associated with decreased circulatory levels of serum 25-hydroxyvitamin D among micro and macrovascular complications of type 2 diabetes mellitus. Int J Biol Macromol. 2018;116:346–353. doi: 10.1016/j.ijbiomac.2018.05.026 [DOI] [PubMed] [Google Scholar]
- 25.Hanson RL, Leti F, Tsinajinnie D, et al. The Arg59Trp variant in ANGPTL8 (betatrophin) is associated with total and HDL-cholesterol in American Indians and Mexican Americans and differentially affects cleavage of ANGPTL3. Mol Genet Metab. 2016;118(2):128–137. doi: 10.1016/j.ymgme.2016.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu J, Yagi K, Nohara A, et al. High frequency of type 2 diabetes and impaired glucose tolerance in Japanese subjects with the angiopoietin-like protein 8 R59W variant. J Clin Lipidol. 2018;12(2):331–337. doi: 10.1016/j.jacl.2017.12.011 [DOI] [PubMed] [Google Scholar]
- 27.Dang F, Wu R, Wang P, et al. Fasting and feeding signals control the oscillatory expression of angptl8 to modulate lipid metabolism. Sci Rep. 2016;6:36926. doi: 10.1038/srep36926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhang R, Abou-Samra AB. A dual role of lipasin (betatrophin) in lipid metabolism and glucose homeostasis: consensus and controversy. Cardiovasc Diabetol. 2014;13:133. doi: 10.1186/s12933-014-0133-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ren G, Kim JY, Smas CM. Identification of RIFL, a novel adipocyte-enriched insulin target gene with a role in lipid metabolism. Am J Physiol Endocrinol Metab. 2012;303(3):E334–51. doi: 10.1152/ajpendo.00084.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stephens JM. RIFL aims to be a new player in lipid metabolism. Am J Physiol Endocrinol Metab. 2012;303(3):E332–3. doi: 10.1152/ajpendo.00169.2012 [DOI] [PubMed] [Google Scholar]
- 31.Zhang R. Lipasin, a novel nutritionally-regulated liver-enriched factor that regulates serum triglyceride levels. Biochem Biophys Res Commun. 2012;424(4):786–792. doi: 10.1016/j.bbrc.2012.07.038 [DOI] [PubMed] [Google Scholar]
- 32.Rong Guo X, Li Wang X, Chen Y, et al. ANGPTL8/betatrophin alleviates insulin resistance via the Akt-GSK3β or Akt-FoxO1 pathway in HepG2 cells. Exp Cell Res. 2016;345(2):158–167. doi: 10.1016/j.yexcr.2015.09.012 [DOI] [PubMed] [Google Scholar]
- 33.Hu H, Sun W, Yu S, et al. Increased circulating levels of betatrophin in newly diagnosed type 2 diabetic patients. Diabetes Care. 2014;37(10):2718–2722. doi: 10.2337/dc14-0602 [DOI] [PubMed] [Google Scholar]
- 34.Chen X, Lu P, He W, et al. Circulating betatrophin levels are increased in patients with type 2 diabetes and associated with insulin resistance. J Clin Endocrinol Metab. 2015;100(1):E96–100. doi: 10.1210/jc.2014-2300 [DOI] [PubMed] [Google Scholar]
- 35.Ebert T, Kralisch S, Hoffmann A, et al. Circulating angiopoietin-like protein 8 is independently associated with fasting plasma glucose and type 2 diabetes mellitus. J Clin Endocrinol Metab. 2014;99(12):E2510–7. doi: 10.1210/jc.2013-4349 [DOI] [PubMed] [Google Scholar]
- 36.Chen CC, Susanto H, Chuang WH, et al. Higher serum betatrophin level in type 2 diabetes subjects is associated with urinary albumin excretion and renal function. Cardiovasc Diabetol. 2016;15:3. doi: 10.1186/s12933-015-0326-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang YY, Zhang D, Jiang ZY, et al. Positive association between betatrophin and diabetic retinopathy risk in type 2 diabetes patients. Horm Metab Res. 2016;48(3):169–173. doi: 10.1055/s-0035-1550009 [DOI] [PubMed] [Google Scholar]
- 38.Yin Y, Ding X, Peng L, et al. Increased serum ANGPTL8 concentrations in patients with prediabetes and type 2 diabetes. J Diabetes Res. 2017;2017:8293207. doi: 10.1155/2017/8293207 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shimamura M, Matsuda M, Kobayashi S, et al. Angiopoietin-like protein 3, a hepatic secretory factor, activates lipolysis in adipocytes. Biochem Biophys Res Commun. 2003;301(2):604–609. doi: 10.1016/s0006-291x(02)03058-9 [DOI] [PubMed] [Google Scholar]
- 40.Ye J, Qin Y, Wang D, et al. The relationship between circulating ANGPTL8/betatrophin concentrations and adult obesity: a meta-analysis. Dis Markers. 2019;2019:5096860. doi: 10.1155/2019/5096860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.El-Lebedy D. Interaction between endothelial nitric oxide synthase rs1799983, cholesteryl ester-transfer protein rs708272 and angiopoietin-like protein 8 rs2278426 gene variants highly elevates the risk of type 2 diabetes mellitus and cardiovascular disease. Cardiovasc Diabetol. 2018;17(1):97. doi: 10.1186/s12933-018-0742-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fu Z, Berhane F, Fite A, et al. Elevated circulating lipasin/betatrophin in human type 2 diabetes and obesity. Sci Rep. 2014;4:5013. doi: 10.1038/srep05013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Espes D, Martinell M, Carlsson PO. Increased circulating betatrophin concentrations in patients with type 2 diabetes. Int J Endocrinol. 2014;2014:323407. doi: 10.1155/2014/323407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Trebotic LK, Klimek P, Thomas A, et al. Circulating betatrophin is strongly increased in pregnancy and gestational diabetes mellitus. PLoS One. 2015;10(9):e0136701. doi: 10.1371/journal.pone.0136701 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ebert T, Kralisch S, Wurst U, et al. Betatrophin levels are increased in women with gestational diabetes mellitus compared to healthy pregnant controls. Eur J Endocrinol. 2015;173(1):1–7. doi: 10.1530/EJE-14-0815 [DOI] [PubMed] [Google Scholar]
- 46.Luo D, Chen X, Yang W, et al. Angiopoietin-like 8 improves insulin resistance and attenuates adipose tissue inflammation in diet-induced obese mice. Exp Clin Endocrinol Diabetes. 2020;128(5):290–296. doi: 10.1055/a-0725-7897 [DOI] [PubMed] [Google Scholar]
- 47.Mamputu JC, Desfaits AC, Renier G. Lipoprotein lipase enhances human monocyte adhesion to aortic endothelial cells. J Lipid Res. 1997;38(9):1722–1729. [PubMed] [Google Scholar]
- 48.Mamputu JC, Levesque L, Renier G. Proliferative effect of lipoprotein lipase on human vascular smooth muscle cells. Arterioscler Thromb Vasc Biol. 2000;20(10):2212–2219. doi: 10.1161/01.atv.20.10.2212 [DOI] [PubMed] [Google Scholar]
- 49.Kovrov O, Kristensen KK, Larsson E, et al. On the mechanism of angiopoietin-like protein 8 for control of lipoprotein lipase activity. J Lipid Res. 2019;60(4):783–793. doi: 10.1194/jlr.M088807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abu-Farha M, Melhem M, Abubaker J, et al. ANGPTL8/Betatrophin R59W variant is associated with higher glucose level in non-diabetic Arabs living in Kuwaits. Lipids Health Dis. 2016;15:26. doi: 10.1186/s12944-016-0195-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Ghasemi H, Karimi J, Khodadadi I, et al. Association between rs2278426 (C/T) and rs892066 (C/G) variants of ANGPTL8 (betatrophin) and susceptibility to type2 diabetes mellitus. J Clin Lab Anal. 2019;33(1):e22649. doi: 10.1002/jcla.22649 [DOI] [PMC free article] [PubMed] [Google Scholar]