Editor,
Since the World Health Organization’s declaration of the pandemic status of Coronavirus Disease 2019 (or COVID-19) on 11 March 2020, many countries across the world, including the United Kingdom, had imposed nationwide lockdown. Routine healthcare services were cancelled, and patients were advised to avoid hospital visits, unless critically necessary, to minimize the risk of COVID-19 transmission, leading to significant disruption to the provision of healthcare service and patient care.
Ophthalmology represents one of the busiest and most heavily outpatient-oriented specialties, with ~7.5 million outpatient appointments and >500,000 surgical procedures being provided in the United Kingdom each year.1 The recent pandemic lockdown had resulted in cancellation of thousands of ophthalmic clinical visits and surgeries, which could potentially lead to permanent and significant harm to patient’s vision.2 In addition, our recent survey among the general public with eye diseases highlighted a significant negative psychosocial impact of lockdown on individuals with visual impairment, with around 50% of them expressing fear of further sight loss due to delayed review or treatment.3 Therefore, it is important that efficient measures are implemented during and after the COVID-19 pandemic to avoid any irreversible sight loss among these patients. However, effective reformation, adaptation, and delivery of the ophthalmic service require a full grasp of the impact of pandemic lockdown, for which the data are limited in the literature.
With this in mind, we recently conducted a retrospective analysis of the changing trend in capacity and workload of the ophthalmology service in Queen’s Medical Centre, Nottingham, United Kingdom, between 01 June 2019 and 31 June 2020. All data, including the number of clinical and surgical activities, and cases that breached the 18-week referral-to-treatment (RTT) waiting time (https://www.england.nhs.uk/rtt/), were collected from the hospital-wide database and were analysed. The 18-week RTT is a national initiative implemented by the UK government to ensure that all patients were reviewed and treated in hospitals within 18 weeks of the referral initiated by their primary care physicians. It is often used as an indicator of the backlog of clinical and surgical work. For this study, the date, 18 March 2020, was used as the cut-off point to analyse the impact of COVID-19 lockdown. This study was approved by the Nottingham University Hospital NHS Trust as a service evaluation study (Ref: 20-351 C).
When comparing June 2019 (pre-COVID-19) and June 2020 (during COVID-19 pandemic), we observed a substantial 63% and 67% reduction in the outpatient and surgical activities, respectively. In addition, there was a significant ~1800% increase in the number of virtual- or tele-consultation visits (p < 0.0001; Figure 1), highlighting the real-world utility and patient receptivity of telemedicine during the COVID-19 period. From 18 March 2020 to 01 July 2020 (a 15-week period), there was a significant increase in the 18-week RTT breaches/waiting list in outpatient review (by 75%) and surgeries (by 471%; Figure 2). Cataract surgery (53%) formed the majority of the surgical backlog, followed by YAG laser procedures (24%) and oculoplastic surgeries (8%; Table 1).
Figure 1.

A direct month-to-month comparison of clinical and surgical activities in ophthalmology before COVID-19 (June 2019) and during COVID-19 period (June 2020).
Figure 2.
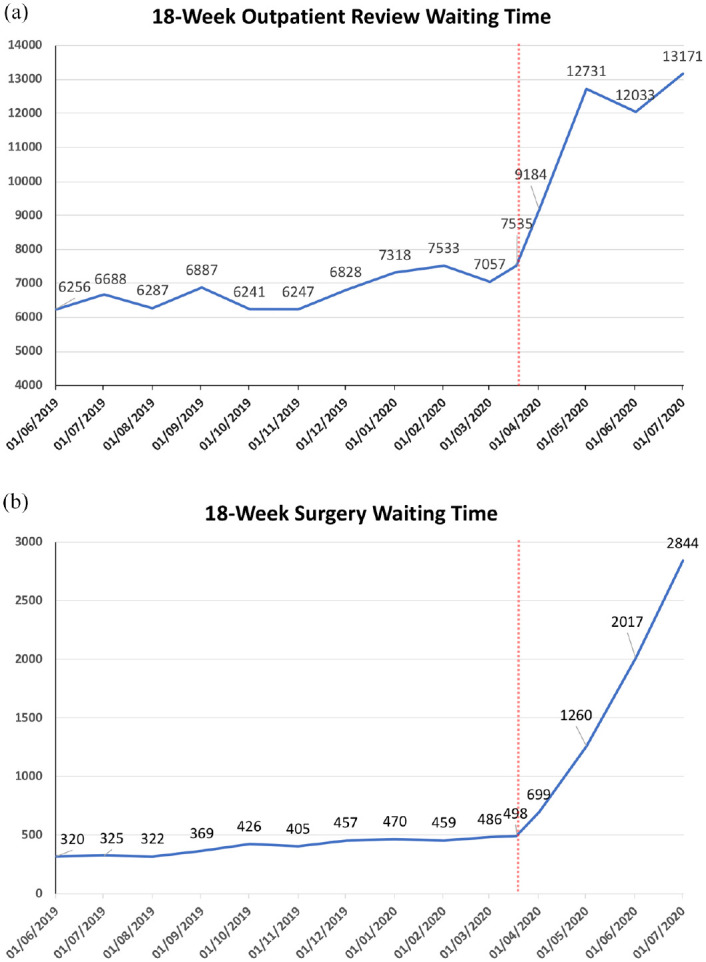
The number of ophthalmology cases that breached the 18-week referral-to-treatment waiting time for outpatient review (a) and surgery (b). The vertical red dotted line indicated the time point (18 March 2020) where ophthalmic routine services were cancelled.
Table 1.
Summary of the surgical backlog that had breached the 18-week referral-to-treatment waiting time.
| Types of surgery | Total N = 2017; n (%) |
|---|---|
| Cataract surgery | 1078 (53.4) |
| YAG laser procedures | 491 (24.3) |
| Oculoplastic surgeries | 165 (8.2) |
| Squint surgeries | 81 (4.0) |
| Orbital and lacrimal surgeries | 53 (2.6) |
| Corneal and conjunctival surgeries | 42 (2.1) |
| Vitreoretinal surgeries | 41 (2.0) |
| Glaucoma surgeries | 28 (1.4) |
| Others | 38 (1.9) |
COVID-19 has paralysed the healthcare system globally and understanding of the true impact helps strategise service delivery planning and workforce/resource allocation during the post-COVID-19 period, ultimately minimizing any harm to patients’ vision and quality of life. To our best knowledge, this represents the first study evaluating the true magnitude of the impact of COVID-19 on the ophthalmology services in the United Kingdom. Babu and colleagues4 similarly reported a significant impact of COVID-19 pandemic on the ophthalmology service in India, with clinical and surgical services being reduced by >95%. Interestingly, only a low (~2%) utility of tele-consultation was observed, which was in contrast to our findings. The disparity is likely attributed to the cultural difference, level of education, and patient receptivity of telemedicine.
Cataract surgery is by far the most commonly performed procedure in ophthalmology. In view of its elective nature, cancellation of routine ophthalmic service has resulted in a significant increase in the cataract surgery backlog during the COVID pandemic, as shown in our study. Lin and colleagues5 have recently highlighted several valuable strategies to cope with the backlog of cataract surgery, including the adoption of telemedicine, modification of face-to-face encounters, better theatre organisation, and immediate sequential bilateral cataract surgery, among others.
With the mounting pressure on ophthalmic service compounded by the recent pandemic, adoption of digitalized healthcare systems using telemedicine and/or artificial intelligence-assisted platforms is urgently required to tackle this unprecedented impact on healthcare systems and patients.6,7 However, it is noteworthy to mention that any plan to maximize throughput of clinical visits and ophthalmic elective surgeries, particularly cataract surgery, needs to be carried out in the context of the entire service and prioritization of emergency services.
Acknowledgments
We thank Kathryn Skill, Jaimie Porter, Arun Lakshmanan and Lynn Soar for their help with the data extraction.
Footnotes
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: D.S.J.T. acknowledges support from the Medical Research Council / Fight for Sight Clinical Research Fellowship (MR/T001674/1) and the Fight for Sight / John Lee, Royal College of Ophthalmologists Primer Fellowship (24CO4).
Conflict of interest statement: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
ORCID iD: Darren Shu Jeng Ting  https://orcid.org/0000-0003-1081-1141
https://orcid.org/0000-0003-1081-1141
Contributor Information
Darren Shu Jeng Ting, Academic Ophthalmology, Division of Clinical Neuroscience, School of Medicine, University of Nottingham, University Park, Nottingham NG7 2RD, UK; Department of Ophthalmology, Queen’s Medical Centre, Nottingham, UK.
Rashmi Deshmukh, Department of Ophthalmology, Queen’s Medical Centre, Nottingham, UK.
Dalia G. Said, Academic Ophthalmology, Division of Clinical Neuroscience, School of Medicine, University of Nottingham, Nottingham, UK Department of Ophthalmology, Queen’s Medical Centre, Nottingham, UK.
Harminder S. Dua, Academic Ophthalmology, Division of Clinical Neuroscience, School of Medicine, University of Nottingham, University Park, Nottingham NG7 2RD, UK Department of Ophthalmology, Queen’s Medical Centre, Nottingham, UK.
References
- 1. MacEwan C, Davis A, Chang L. Ophthalmology GIRFT Programme National Specialty Report (2019), https://gettingitrightfirsttime.co.uk/wp-content/uploads/2019/12/OphthalmologyReportGIRFT19P-FINAL.pdf (accessed 27 July 2020).
- 2. Foot B, MacEwen C. Surveillance of sight loss due to delay in ophthalmic treatment or review: frequency, cause and outcome. Eye (Lond) 2017; 31: 771–775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ting DSJ, Krause S, Said DG, et al. Psychosocial impact of COVID-19 pandemic lockdown on people living with eye diseases in the UK. Eye (Lond). Epub ahead of print 10 August 2020. DOI: 10.1038/s41433-020-01130-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Babu N, Kohli P, Mishra C, et al. To evaluate the effect of COVID-19 pandemic and national lockdown on patient care at a tertiary-care ophthalmology institute. Indian J Ophthalmol 2020; 68: 1540–1544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Lin PF, Naveed H, Eleftheriadou M, et al. Cataract service redesign in the post-COVID-19 era. Br J Ophthalmol. Epub ahead of print 23 July 2020. DOI: 10.1136/bjophthalmol-2020-316917. [DOI] [PubMed] [Google Scholar]
- 6. Ting DSJ, Ang M, Mehta JS, et al. Artificial intelligence-assisted telemedicine platform for cataract screening and management: a potential model of care for global eye health. Br J Ophthalmol 2019; 103: 1537–1538. [DOI] [PubMed] [Google Scholar]
- 7. Ting DSJ, Foo VH, Yang LWY, et al. Artificial intelligence for anterior segment diseases: emerging applications in ophthalmology. Br J Ophthalmol. Epub ahead of print 12 June 2020. DOI: 10.1136/bjophthalmol-2019-315651. [DOI] [PubMed] [Google Scholar]


