ABSTRACT
Objectives:
The extent to which locomotive syndrome is associated with low back pain (LBP), health-related quality of life (HRQOL), and impairment of activities of daily living among elderly men and women remains poorly documented. This study evaluated associations between locomotive syndrome and both HRQOL and LBP as assessed using a questionnaire completed by elderly individuals, including some >80 years old.
Methods:
We conducted a survey assessing locomotive syndrome using the loco-check, HRQOL using the Short-Form 36 questionnaire (SF-36), and LBP using the Roland-Morris Disability Questionnaire (RDQ) among individuals >60 years old. SF-36 and RDQ scores were compared between 253 subjects with and without locomotive syndrome.
Results:
Fifty-seven men (48%) and 71 women (53%) were diagnosed with locomotive syndrome. Subjects of both sexes with locomotive syndrome scored significantly lower for eight items from SF-36. Physical and mental component summary scores were significantly worse in women with locomotive syndrome in their 60s and 70s. RDQ scores were significantly higher in participants with locomotive syndrome for men in their 60s and for both men and women in their 70s.
Conclusions:
Locomotive syndrome was associated with impaired HRQOL and worse LBP among men and women >60 years old. Differences in HRQOL and LBP between subjects with and without locomotive syndrome were significant for both men and women in their 60s and 70s, but not in their 80s. Locomotive syndrome should be prevented to maintain HRQOL, particularly for men and women in their 60s and 70s.
Keywords: health-related quality of life, locomotive syndrome, low back pain
INTRODUCTION
One cause of health disparities among individuals aged 65 years or more is impairment in locomotive function, which is associated with increased risk of needing nursing support.1) Locomotive syndrome was proposed by the Japanese Orthopaedic Association (JOA) in 2007.2,3) It is a condition involving declines in gait and sit-to-stand function resulting from disorders of the locomotive organs.2,3) Locomotive syndrome is diagnosed using the loco-check, a simple tool for evaluating the severity of locomotive syndrome designed for easy application in elderly individuals in home care.2) Several previous studies have confirmed that the loco-check is a useful tool for diagnosing locomotive syndrome4) and that loco-check results correlate well with measures of health-related quality of life (HRQOL) and individual physical functions.5,6,7)
Locomotive syndrome is well understood to relate to the impairment of activities of daily living (ADL). However, the association of locomotive syndrome with low back pain or the way it affects HRQOL or impairment of ADL among elderly men and women is not well understood, particularly for those over 80 years old. The purpose of the present study was to evaluate associations between locomotive syndrome, HRQOL, and low back pain as evaluated using a questionnaire in individuals aged 60 years or more, including those over 80 years old.
METHODS
Patients and Study Design
We carried out a survey in 2013 investigating locomotive syndrome and HRQOL by sending a questionnaire to elderly people and asking them to respond individually. The survey was conducted in collaboration with the Health and Welfare Department, Medical Health Division of Kita-Akita City. Inclusion criteria were being at least 60 years old and resident in the Ani area of Kita-Akita City. The questionnaire was distributed to elderly people living in the Ani area by members of the Health and Welfare Department. Completed questionnaires were retrieved at a subsequent health check-up. A total of 253 valid responses (118 men, 135 women; age range, 60–88 years) with written informed consent to the questionnaire were obtained and analyzed. The study protocol was approved by the ethics committee of our institute (IRB #669). This study was conducted in accordance with the Declaration of Helsinki.
Diagnosis of Locomotive Syndrome
Locomotive syndrome was diagnosed using the loco-check questionnaire, which was prepared by the JOA to evaluate the locomotive organs. The loco-check consists of the following seven items:
1. You cannot put a sock on while standing on one leg.
2. You often trip up or slip when moving around the house.
3. You need to hold onto a handrail when climbing stairs.
4. You have difficulty performing moderately heavy housework.
5. You have difficulty carrying home 2 kg of shopping (e.g., equivalent to two 1-L cartons of milk).
6. You cannot walk for 15 min nonstop.
7. You cannot cross the road before the pedestrian crossing light turns red.
Participants answered each loco-check question with either “yes” or “no”. If a “yes” answer was obtained for at least one question, the subject was diagnosed with locomotive syndrome.
HRQOL as Evaluated by the Short-Form 36 Questionnaire
HRQOL was evaluated using the Short-Form 36 questionnaire version 2 (SF-36v2). SF-36v2 covers eight categories: physical functioning (PF), role physical (RP), bodily pain (BP), general health (GH), vitality (VT), social functioning (SF), role emotional (RE), and mental health (MH). Raw scores for these eight categories were linearly transformed with standard scoring algorithms yielding scores that were then further adjusted using a Japanese norm-based scoring system to generate normalized scores with a mean of 50 ± 10 (standard deviation, norm-based scores in 2007).8) Furthermore, a physical component summary (PCS) score and a mental component summary (MCS) score were calculated from these eight subscales for simple evaluation of HRQOL.9) All eight norm-based scores were compared between subjects diagnosed with locomotive syndrome [Locomo (+) group] and those not diagnosed with locomotive syndrome [Locomo (-) group] in both men and women. We also evaluated PCS and MCS scores between Locomo (+) and Locomo (-) groups separated into age strata: 60s (60–69 years old; 46 men, 53 women), 70s (70–79 years old; 48 men, 60 women), and 80s (80–88 years old; 24 men, 22 women).
Low Back Pain as Evaluated by the Roland-Morris Disability Questionnaire
Low back pain was assessed using the Roland-Morris Disability Questionnaire (RDQ).10,11) The Japanese version of the RDQ (24 questions) has been confirmed to meet psychometric standards in terms of reliability, validity, and responsiveness.12) A higher RDQ score indicates a lower quality of life (QOL) due to impairment by low back pain. RDQ scores were also compared between the Locomo (+) and Locomo (-) groups separated into the same age strata in men and women.
Statistical Analyses
Results are expressed as medians [lower quartile, upper quartile] for nonparametric data. The Kolmogorov-Smirnov test revealed that all data were nonparametric. The incidence of locomotive syndrome in age decades from 60s to 80s was analyzed using Fisher’s exact test. Correlations between PCS or MCS and RDQ in men and women were analyzed using Spearman’s rank correlation coefficient test. Differences in data between Locomo (+) and Locomo (-) groups were assessed using the Mann-Whitney U-test. Differences with values of P < 0.05 were considered statistically significant. All statistical analyses were performed using EZR statistical software (The R Foundation for Statistical Computing).13)
RESULTS
Frequency of Locomotive Syndrome
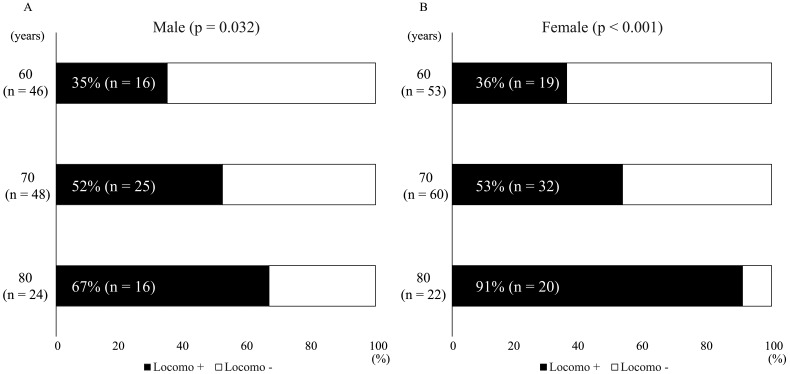
The frequencies of locomotive syndrome for men in their 60s, 70s, and 80s were 35% (n = 16), 52% (n = 25), and 67% (n = 16), respectively (Fig. 1A); for women, the frequencies were 36% (n = 19), 53% (n = 32), and 91% (n = 20), respectively (Fig. 1B). The incidence of locomotive syndrome was significantly higher with advancing age in both men (P = 0.032) and women (P < 0.001). No significant differences in the frequencies of locomotive syndrome were evident between men and women in their 60s, 70s, or 80s.
Fig. 1.
(A) Incidence of locomotive syndrome in men and (B) women in their 60s, 70s, and 80s
Association of HRQOL and Low Back Pain with Locomotive Syndrome
Among men, 57 subjects (48%) were diagnosed with locomotive syndrome. For men, all norm-based scores of the eight sub-components of SF-36v2 were significantly lower in the Locomo (+) group than in the Locomo (-) group (P = 0.036 to P < 0.001) (Table 1). For men, PCS was significantly lower and the RDQ score was significantly higher in the Locomo (+) group than in the Locomo (-) group (P = 0.002 and P = 0.006, respectively). RDQ scores correlated significantly with PCS scores (r = –0.352, P < 0.001) (Fig. 2A), but not with MCS scores (Fig. 2B) in men.
Table 1. Associations between SF36/RDQ scores and locomotive syndrome in men.
| Locomo (-) (n = 61) |
Locomo (+) (n =57) |
P value | |
| SF36 | |||
| BP-N | 54.6 [44.7, 61.7] | 44.7 [40.3, 54.6] | 0.016 |
| GH-N | 46.9 [44.2, 54.8] | 45.8 [40.5, 49.5] | 0.036 |
| MH-N | 54.5 [49.1, 59.9] | 49.1 [43.8, 57.2] | 0.002 |
| PF-N | 54.2 [50.6, 57.8] | 47.0 [36.2, 50.6] | < 0.001 |
| RP-N | 55.7 [52.4, 55.7] | 42.4 [35.8, 52.4] | < 0.001 |
| SF-N | 57.0 [57.0, 57.0] | 57.0 [44.1, 57.0] | 0.021 |
| VT-N | 56.3 [49.8, 62.7] | 49.8 [43.4, 56.3] | 0.003 |
| RE-N | 56.1 [51.9, 56.1] | 43.6 [35.3, 56.1] | < 0.001 |
| SF36 summary component score | |||
| PCS | 49.1 [43.2, 53.8] | 42.5 [35.4, 49.9] | 0.002 |
| MCS | 54.2 [47.8, 58.8] | 52.7 [46.9, 58.2] | 0.291 |
| RDQ | 0 [0, 0] | 0 [0, 3] | 0.006 |
Data are shown as median [lower quartile, upper quartile].
Fig. 2.
Correlations between physical (PCS) and mental component summary (MCS) scores from the SF-36 questionnaire and the Roland-Morris Disability Questionnaire (RDQ). (A) Correlations between PCS score and (B) MCS score and RDQ score in men. (C) Correlations between PCS score and (D) MCS score and RDQ score in women. PCS and RDQ were significantly negatively correlated in men (r = –0.352, P < 0.001) and in women (r = –0.6, P < 0.001).
Among women, 71 participants (53%) were diagnosed with locomotive syndrome. For women, all norm-based scores of the eight sub-component scores of SF-36v2 were also significantly lower in the Locomo (+) group than in the Locomo (-) group (P < 0.001) (Table 2). Both PCS and MCS scores were significantly lower in the Locomo (+) group than in the Locomo (-) group (P < 0.001 and P = 0.009, respectively). Furthermore, the RDQ score was significantly higher in the Locomo (+) group than in the Locomo (-) group. RDQ scores correlated significantly with PCS scores (r = –0.6, P < 0.001) (Fig. 2C), but not with MCS scores (Fig. 2D) in women.
Table 2. Associations between SF36/RDQ scores and locomotive syndrome in women.
| Locomo (-) (n = 64) |
Locomo (+) (n =71) |
P value | |
| SF36 | |||
| BP-N | 54.6 [49.2, 61.7] | 40.3 [35.4, 49.2] | < 0.001 |
| GH-N | 46.9 [44.2, 54.8] | 40.5 [37.8, 46.9] | < 0.001 |
| MH-N | 55.8 [46.5, 59.9] | 43.8 [38.4, 51.8] | < 0.001 |
| PF-N | 53.8 [50.6, 54.2] | 39.8 [23.5, 50.6] | < 0.001 |
| RP-N | 55.7 [45.8, 55.7] | 39.1 [29.1, 54.1] | < 0.001 |
| SF-N | 57.0 [50.6, 57.0] | 50.6 [37.7, 57.0] | < 0.001 |
| VT-N | 56.3 [47.4, 59.7] | 43.4 [40.2, 53.0] | < 0.001 |
| RE-N | 56.1 [47.7, 56.1] | 43.6 [31.1, 56.1] | < 0.001 |
| SF36 summary component score | |||
| PCS | 50.5 [45.7, 54.0] | 39.1 [26.5, 49.8] | < 0.001 |
| MCS | 55.4 [45.5, 59.3] | 50.1 [44.3, 53.6] | 0.009 |
| RDQ | 0.0 [0.0, 0.0] | 1.0 [0.0, 8.0] | < 0.001 |
Data are shown as median [lower quartile, upper quartile].
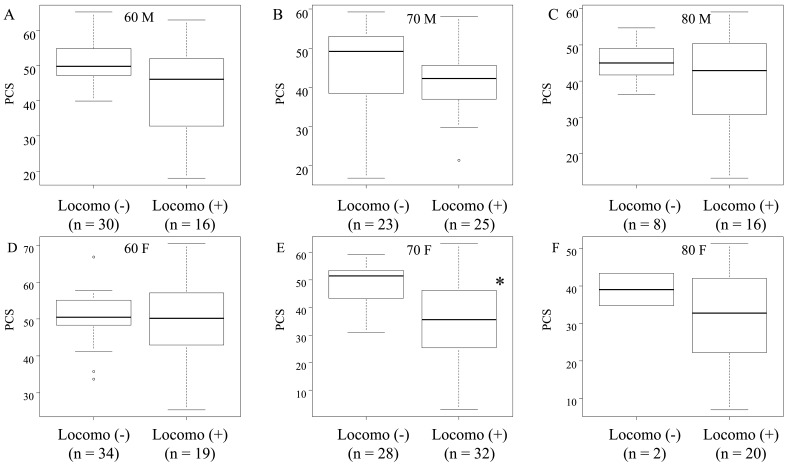
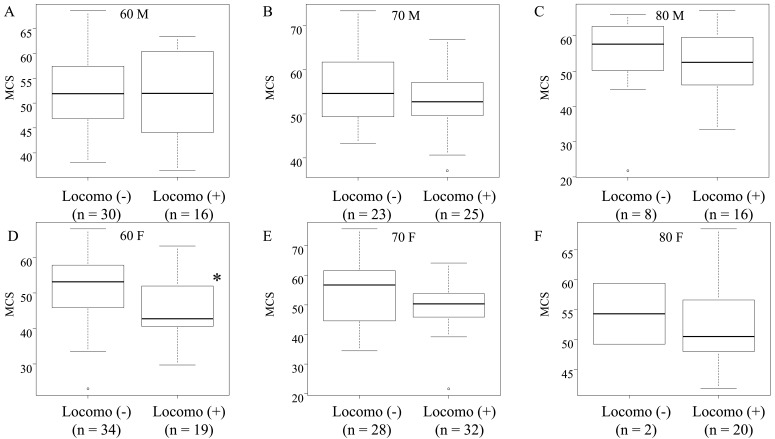
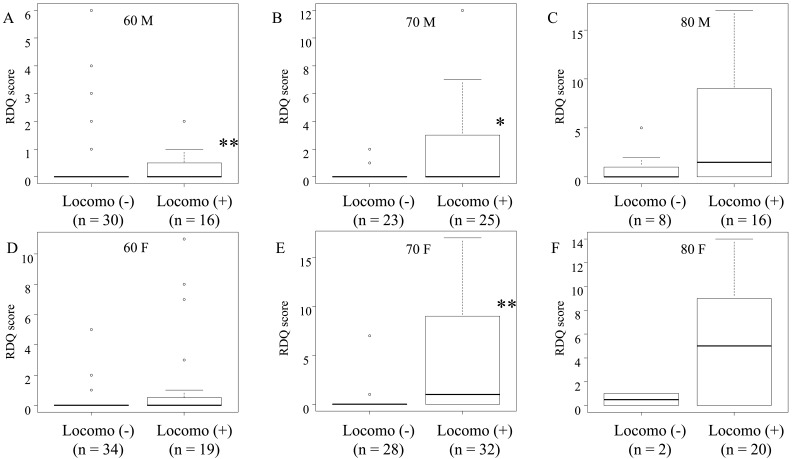
Association of PCS and MCS Scores of the SF-36 and Low Back Pain with Locomotive Syndrome
The PCS score was significantly lower in the Locomo (+) group than in the Locomo (-) group only for women in their 70s (P = 0.001) (Fig. 3E). No significant differences in PCS scores were seen between Locomo (+) and Locomo (-) groups for men in any age group or for women in their 60s or 80s (Fig. 3A–D, F). The MCS score was significantly lower in the Locomo (+) group than in the Locomo (-) group only for women in their 60s (P = 0.009) (Fig. 4D). MCS scores for other age strata of men and women did not exhibit any significant differences between the Locomo (+) and Locomo (-) groups (Fig. 4A–C, E, F). The RDQ score was significantly higher in the Locomo (+) group than in the Locomo (-) group for men in their 60s and 70s and for women in their 70s (P = 0.006, P = 0.018, and P < 0.001, respectively) (Fig. 5A, B, E). No significant differences in RDQ scores were seen between Locomo (+) and Locomo (-) groups for men in their 80s or for women in their 60s or 80s (Fig. 5C, D, F).
Fig. 3.
Differences in PCS scores from the SF-36 questionnaire. PSC scores for men in their (A) 60s, (B) 70s, and (C) 80s. PSC scores for women in their (D) 60s, (E) 70s, and (F) 80s. Locomo (-), absence of locomotive syndrome; Locomo (+), presence of locomotive syndrome. *P < 0.001 vs. Locomo (-) group, Mann-Whitney U-test.
Fig. 4.
Differences in MCS scores from the SF-36 questionnaire. MCS scores for men in their (A) 60s, (B) 70s, and (C) 80s. PSC scores for women in their (D) 60s, (E) 70s, and (F) 80s. *P < 0.01 vs. Locomo (-) group, Mann-Whitney U-test.
Fig. 5.
Differences in RDQ scores from the Roland-Morris Disability Questionnaire. RDQ scores for men in their (A) 60s, (B) 70s, and (C) 80s. RDQ scores for women in their (D) 60s, (E) 70s, and (F) 80s. * P < 0.05, ** P < 0.01 vs. Locomo (-) group, Mann-Whitney U-test.
DISCUSSION
Influence of Locomotive Syndrome on HRQOL
In the present study, both men and women >60 years old diagnosed with locomotive syndrome had worse HRQOL and more frequent low back pain. Several previous studies have reported that locomotive syndrome causes impairment of HRQOL. HRQOL, as evaluated using the EuroQol 5 dimension (EQ-5D)-three-level5,6) and SF-367) scores, is reportedly reduced by the presence of locomotive syndrome. Tanaka et al. reported that the Japanese version of the EQ-5D-five-level (EQ-5D-5L) index correlated significantly with locomotive syndrome.14) Participants in these previous studies were >20 years,6) >40 years,5,14) and >50 years old.7)
The present study focused on elderly individuals >60 years old, with 46 subjects (18%) >80 years old. The percentage of subjects >80 years old with locomotive syndrome was 67% in men and 91% in women. Differences in HRQOL between the Locomo (+) and Locomo (-) groups were not significant in sub-analyses of subjects >80 years old in this study. Compared with individuals in their 60s and 70s, the percentages with locomotive syndrome were significantly higher in men and women in their 80s. Most individuals in their 80s were diagnosed with locomotive syndrome, and it is therefore not surprising that no significant difference in HRQOL was found between individuals with and without locomotive syndrome for subjects in their 80s. We consider that locomotive syndrome is a significant contributor to impairment of HRQOL, especially among individuals in their 70s or younger.
Locomotive Syndrome with Respect to Sex and Age
In the present study, PCS and MCS scores were significantly worse in women with locomotive syndrome in their 60s and 70s, but not in men with locomotive syndrome in the same age groups. Age and sex reportedly influence locomotive syndrome. Sasaki et al. reported that the prevalence of locomotive syndrome in the general population was higher among women than among men, and tended to increase with age in both sexes.4) Another previous study reported that age, sex, the EQ-5D-utility value, and the EQ-5D-visual analog scale (VAS) score were each independently associated with locomotive syndrome as identified using the loco-check.5) Furthermore, Tanaka et al. reported that the EQ-5D-5L index was significantly lower in a group with locomotive syndrome than in a group without locomotive syndrome, after adjusting for age and sex.14)
Several factors may contribute to the sex differences in the relation between PCS and MCS and locomotive syndrome in the present study. Osteoporosis is more common in women than in men,15) and our previous study demonstrated that the incidence of osteoporosis and osteopenia increased with age decade in women.16) Although Yoshimura et al. reported that stage I locomotive syndrome was related to sarcopenia and frailty in people >60 years old,17) the prevalences of sarcopenia in men and women were reported to be similar among community-dwelling individuals.18) The incidence of osteoporosis or other physical dysfunctions such as osteoarthritis may therefore contribute more to lower PCS scores in women than in men. Moreover, women were more likely to be frail than men of the same age in all age groups.19,20,21) The definition of frail contains factors related to mental state, and this increased frailty may therefore be caused by the lower MCS score among women than among men in the Locomo (+) group this study.
Locomotive Syndrome and Low Back Pain
Subjects with locomotive syndrome diagnosed using the loco-check had worse RDQ scores, which reflect impairment of physical-related QOL due to low back pain. In the present study, this was particularly evident for men in their 60s and for both men and women in their 70s. Many previous studies have indicated that locomotive syndrome, which can originate from several musculoskeletal disorders (including degenerative changes to the lumbar spine, osteoporosis, and osteoarthritis), is associated with low back pain as evaluated with RDQ7) and using a VAS.4) Furthermore, Shigematsu et al. reported that elderly patients with lumbar spinal stenosis (LSS) displayed lower EQ-5D-utility values and a greater number of “yes” answers in the loco-check than elderly persons without LSS.22) We also previously demonstrated that LSS identified using a questionnaire was associated with progression of locomotive syndrome as evaluated with the assessment of the risk of locomotive syndrome.23) Based on these results, the early detection of locomotive syndrome using the loco-check may prove useful in preventing the progression of locomotive syndrome.
Diagnosis of Locomotive Syndrome Using the Loco-check Test
In the present study, we diagnosed locomotive syndrome using the loco-check. Recently, the JOA introduced a battery of short tests for the early detection of locomotive syndrome and its attendant risks2,3): the Stand-up Test24), the Two-step Test25), and the 25-question Geriatric Locomotive Function Scale (GLFS-25).26) Compared with the GLFS-25, which contains 25 questions, the loco-check is a simpler tool for evaluating the severity of locomotive syndrome and was designed for easy application to elderly individuals in home care. Several previous studies have confirmed that the loco-check is a useful tool for diagnosing locomotive syndrome. Sasaki et al. reported that the loco-check offered high sensitivity when using the GLFS-25 as a screening tool.4) Several other reports have demonstrated that loco-check results correlated with HRQOL and with individual physical functions.5-7) Noge et al. reported that the number of “yes” answers in the loco-check was associated with poorer results for SF-36 physical factor and grip power, knee extensor strength, one-leg standing, 10-m walking speed, and timed up and go test.27) In addition, the number of affirmative answers on the loco-check correlated positively with the stage of locomotive syndrome.6) The loco-check is therefore considered a useful tool in screening for and diagnosing locomotive syndrome.
Study Limitations
Several limitations must be considered when interpreting the results of this study. First, we did not analyze participant comorbidities such as spinal disorders, osteoporosis, or osteoarthritis; moreover, we did not include data regarding physical function. Second, we could not include physical background data such as height, weight, body mass index, smoking, or the other factors, although those factors may influence HRQOL.
Conclusions
Locomotive syndrome, as diagnosed using the loco-check, was associated with impaired QOL, as evaluated by the SF-36 score, and worse low back pain assessed using the RDQ questionnaire among both men and women >60 years old. Locomotive syndrome was associated with worse PCS and MCS scores from the SF-36 questionnaire among women in their 60s and 70s. Individuals in their 60s and 70s with locomotive syndrome showed worse RDQ scores, which indicated greater impairment of QOL due to low back pain. However, in this study, those differences were not significant for subjects in their 80s.
ACKNOWLEDGMENTS
The authors wish to thank Eriko Kamada and Maki Takeshita for their help with data analysis. We also thank the staff of the Health and Welfare Department, Medical Health Division of Kita-Akita City, for helping with the distribution and collection of the survey questionnaires.
Footnotes
CONFLICTS OF INTEREST: The authors declare that no conflicts of interest exist.
REFERENCES
- 1.Nakamura K: A “super-aged” society and the “locomotive syndrome”. J Orthop Sci 2008;13:1–2. 10.1007/s00776-007-1202-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nakamura K: The concept and treatment of locomotive syndrome: its acceptance and spread in Japan. J Orthop Sci 2011;16:489–491. 10.1007/s00776-011-0108-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nakamura K,Ogata T: Locomotive syndrome: definition and management. Clin Rev Bone Miner Metab 2016;14:56–67. 10.1007/s12018-016-9208-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sasaki E,Ishibashi Y,Tsuda E,Ono A,Yamamoto Y,Inoue R,Takahashi I,Umeda T,Nakaji S: Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci 2013;18:121–129. 10.1007/s00776-012-0329-2 [DOI] [PubMed] [Google Scholar]
- 5.Iizuka Y,Iizuka H,Mieda T,Tajika T,Yamamoto A,Takagishi K: Association between “loco-check” and EuroQol, a comprehensive instrument for assessing health-related quality of life: a study of the Japanese general population. J Orthop Sci 2014;19:786–791. 10.1007/s00776-014-0602-7 [DOI] [PubMed] [Google Scholar]
- 6.Shigematsu H,Tanaka M,Munemoto M,Kawasaki S,Iwata E,Okuda A,Masuda K,Yamamoto Y,Suga Y,Tanaka Y: Affirmative answers on loco-check as a predictor of health-related quality of life and locomotive syndrome progression in the elderly: a cross-sectional study. Mod Rheumatol 2019;13:1–6. 10.1080/14397595.2019.1621459 [DOI] [PubMed] [Google Scholar]
- 7.Hirano K,Imagama S,Hasegawa Y,Ito Z,Muramoto A,Ishiguro N: The influence of locomotive syndrome on health-related quality of life in a community-living population. Mod Rheumatol 2013;23:939–944. 10.3109/s10165-012-0770-2 [DOI] [PubMed] [Google Scholar]
- 8.Ware JE., Jr SF-36 health survey update. Spine 2000;25:3130–3139. 10.1097/00007632-200012150-00008 [DOI] [PubMed] [Google Scholar]
- 9.Fukuhara S,Suzukamo Y. Manual of SF-36v2 Japanese version. Institute for Health Outcomes & Process Evaluation Research, Kyoto [in Japanese].
- 10.Roland M,Morris R: A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine 1983;8:141–144. 10.1097/00007632-198303000-00004 [DOI] [PubMed] [Google Scholar]
- 11.Roland M,Morris R: A study of the natural history of low-back pain. Part II: development of guidelines for trials of treatment in primary care. Spine 1983;8:145–150. 10.1097/00007632-198303000-00005 [DOI] [PubMed] [Google Scholar]
- 12.Suzukamo Y,Fukuhara S,Kikuchi S,Konno S,Roland M,Iwamoto Y,Nakamura T, Committee on Science Project, Japanese Orthopaedic Association: Validation of the Japanese version of the Roland-Morris Disability Questionnaire. J Orthop Sci 2003;8:543–548. 10.1007/s00776-003-0679-x [DOI] [PubMed] [Google Scholar]
- 13.Kanda Y: Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant 2013;48:452–458. 10.1038/bmt.2012.244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tanaka S,Ando K,Kobayashi K,Seki T,Hamada T,Machino M,Ota K,Morozumi M,Kanbara S,Ito S,Ishiguro N,Hasegawa Y,Imagama S: Association between locomotive syndrome and the Japanese version of the EQ-5D-5L in middle-aged and elderly people in Japan. Nagoya J Med Sci 2020;82:5–14. 10.18999/nagjms.82.1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yoshimura N,Muraki S,Oka H,Kawaguchi H,Nakamura K,Akune T: Cohort profile: research on Osteoarthritis/Osteoporosis Against Disability study. Int J Epidemiol 2010;39:988–995. 10.1093/ije/dyp276 [DOI] [PubMed] [Google Scholar]
- 16.Miyakoshi N,Hongo M,Mizutani Y,Shimada Y: Prevalence of sarcopenia in Japanese women with osteopenia and osteoporosis. J Bone Miner Metab 2013;31:556–561. 10.1007/s00774-013-0443-z [DOI] [PubMed] [Google Scholar]
- 17.Yoshimura N,Muraki S,Iidaka T,Oka H,Horii C,Kawaguchi H,Akune T,Nakamura K,Tanaka S: Prevalence and co-existence of locomotive syndrome, sarcopenia, and frailty: the third survey of Research on Osteoarthritis/Osteoporosis Against Disability (ROAD) study. J Bone Miner Metab 2019;37:1058–1066. 10.1007/s00774-019-01012-0 [DOI] [PubMed] [Google Scholar]
- 18.Papadopoulou SK,Tsintavis P,Potsaki G,Papandreou D: Differences in the prevalence of sarcopenia in community-dwelling, nursing home and hospitalized individuals. A systematic review and meta-analysis. J Nutr Health Aging 2020;24:83–90. 10.1007/s12603-019-1267-x [DOI] [PubMed] [Google Scholar]
- 19.Collard RM,Boter H,Schoevers RA,Oude Voshaar RC: Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012;60:1487–1492. 10.1111/j.1532-5415.2012.04054.x [DOI] [PubMed] [Google Scholar]
- 20.Gordon EH,Peel NM,Samanta M,Theou O,Howlett SE,Hubbard RE: Sex differences in frailty: a systematic review and meta-analysis. Exp Gerontol 2017;89:30–40. 10.1016/j.exger.2016.12.021 [DOI] [PubMed] [Google Scholar]
- 21.Gordon EH,Hubbard RE: Differences in frailty in older men and women. Med J Aust 2020;212:183–188. 10.5694/mja2.50466 [DOI] [PubMed] [Google Scholar]
- 22.Shigematsu H,Tanaka M,Kawasaki S,Iwata E,Masuda K,Morimoto Y,Yamamoto Y,Tanaka Y: Loco-check presents a useful tool to determine health-related quality of life in elderly people with lumbar spinal stenosis. J Orthop Sci 2019;24:715–719. 10.1016/j.jos.2018.12.001 [DOI] [PubMed] [Google Scholar]
- 23.Kasukawa Y,Miyakoshi N,Hongo M,Ishikawa Y,Kudo D,Kijima H,Kimura R,Ono Y,Takahashi Y,Shimada Y: Lumbar spinal stenosis associated with progression of locomotive syndrome and lower extremity muscle weakness. Clin Interv Aging 2019;14:1399–1405. 10.2147/CIA.S201974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muranaga S: Evaluation of the muscular strength of the lower extremities using the standing movement and clinical application. J Showa Med Assoc 2001;61:362–367. [Google Scholar]
- 25.Muranaga S,Hirano K: Development of a convenient way to predict ability to walk, using a two-step test. J Showa Med Assoc 2003;63:301–303. [Google Scholar]
- 26.Ogata T,Muranaga S,Ishibashi H,Ohe T,Izumida R,Yoshimura N,Iwaya T,Nakamura K: Development of a screening program to assess motor function in the adult population: a cross-sectional observational study. J Orthop Sci 2015;20:888–895. 10.1007/s00776-015-0737-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Noge S,Ohishi T,Yoshida T,Kumagai H: Quantitative assessment of locomotive syndrome by the loco-check questionnaire in older Japanese females. J Phys Ther Sci 2017;29:1630–1636. 10.1589/jpts.29.1630 [DOI] [PMC free article] [PubMed] [Google Scholar]