Abstract
Background:
Research on the role of trait versus state characteristics of a variety of measures among persons experiencing pain has been a focus for the past few decades. Studying the trait versus state nature of the Pain Catastrophizing Scale (PCS) and the Patient Health Questionnaire (PHQ-8) depression scale would be highly informative given both are commonly measured in pain populations and neither scale has been studied for trait/state contributions..
Methods:
The PHQ-8 and PCS were obtained on persons undergoing knee arthroplasty at baseline, 2-, 6-, and 12-months post-surgery (N=402). The multitrait generalization of the latent trait-state model was used to partition trait and state variability in PCS and PHQ-8 item responses simultaneously. A set of variables were used to predict trait catastrophizing and trait depression.
Results:
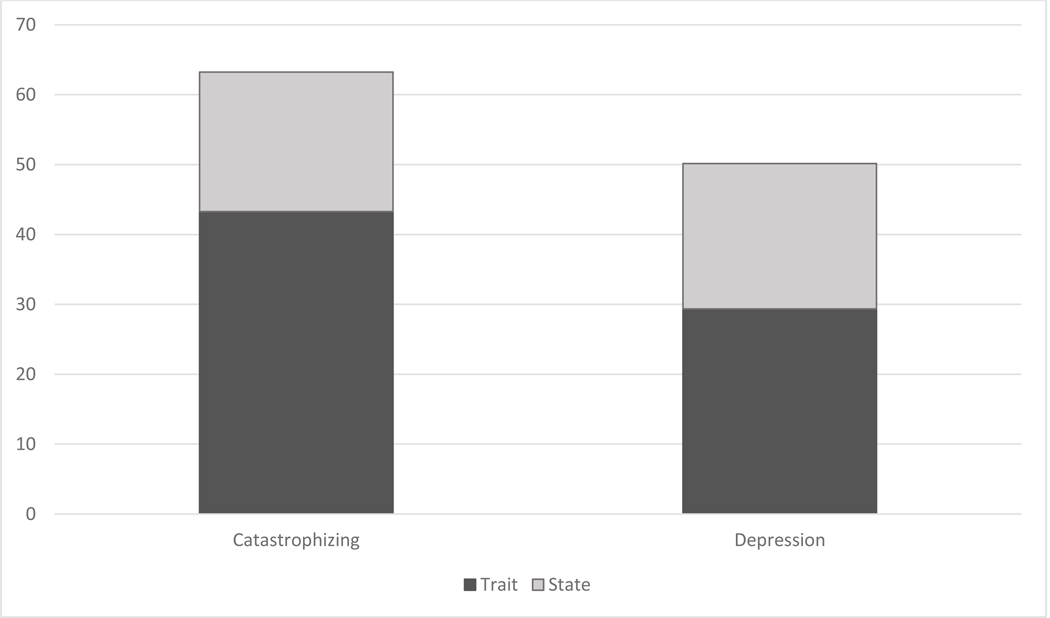
For total scores, the latent traits and latent states explain 63.2% (trait=43.2%; state=20.0%) and 50.2% (trait=29.4%; state=20.8%) of the variability in PCS and PHQ-8, respectively. Patients with a high number of bodily pain sites, high levels of anxiety, young patients, and African American patients had high levels of trait catastrophizing and trait depression. The PCS and the PHQ-8 consist of both enduring trait and dynamic state characteristics, with trait characteristics dominating for both measures.
Conclusion:
Clinicians and researchers using these scales should not assume the obtained measurements solely reflect either trait or state-based characteristics.
Significance:
Clinicians and researchers using the PCS or PHQ-8 scales are measuring both state and trait characteristics and not just trait or state-based characteristics.
1. INTRODUCTION
The role of relatively stable personality-based traits versus situational state characteristics, particularly when pain is experienced, has been a target for research for the past few decades.[8,21,45,46] Pain catastrophizing, a maladaptive cognitive coping style that leads to a magnified threat level when considering potentially painful events [43,45] and depression, a mental health disorder that frequently co-occurs with pain, [28,29,37] have been the focus of much of this work.
Researchers have used a variety of study designs to disentangle the impact of trait versus state characteristics on pain catastrophizing and depression. For example, some experimental pain studies have conceptualized pain catastrophizing as either dispositional (trait) or situational (state).[7,20,32,33] The Pain Catastrophizing Scale (PCS), which asks subjects to recall past painful experiences when they feel pain, has been considered a measure of trait-based pain catastrophizing.[44] The PCS thus elicits patients’ responses that reflect on their clinical pain. A state-based catastrophizing measure (i.e., the Situational Catastrophizing Scale (SCS)),[7] adapted from the original PCS, was designed to assess responses immediately after an experimentally induced pain procedure.[3,17] The assumption here is that the PCS scores reflect trait catastrophizing in the absence of an experimental pain stimuli or intervention while the SCS captures state catastrophizing. The validity of this assumption has not been tested.
Other studies have used longitudinal designs to argue that because changes in pain and pain catastrophizing are associated, pain catastrophizing should be considered a situational state characteristic.[30,47] Longitudinal studies of depression suggest a similar pattern with reductions in pain demonstrating strong bi-directional associations with reductions in depression.[29]
The extent to which the PCS or the Patient Health Questionnaire (PHQ-8) depression scale,[25] capture trait versus state components has not been examined. Trait versus state performance characteristics of a scale has potentially important implications. Scales that capture a greater percentage of state versus trait characteristics, for example, may be more responsive to changes in a patient’s status.
A trait is a stable disposition while a state reflects occasion-specific fluctuations and is influenced by situational factors.[45] A method for disentangling contributions of state versus trait characteristics of a scale is the family of latent state-trait modeling approaches.[15,38] These analytic methods partition out stable (i.e., trait) versus labile (i.e., state) components of each item comprising a scale and estimates the overall contribution to each component. Our purposes were to: 1) determine the percentage contribution of trait versus state components for both the PCS [44] and the PHQ-8 depression measures,[25] and 2) determine whether the trait component for each measure differs for the following predictor variables: pain, anxiety, physical function impairment, race/ethnicity, bodily chronic pain sites, treatment arm and age.
Studying the trait versus state nature of pain catastrophizing and depression would be highly informative given that depression and pain catastrophizing are commonly quantified using the PHQ-8 and PCS, respectively, and both contribute to the development and persistence of chronic pain conditions.[23,32,37] Additionally, neither instrument has been studied to determine state versus trait contributions. Effectiveness of clinical interventions may differ in altering either trait or state characteristics. Ability to differentiate trait and state characteristics of catastrophizing and depression allows for testing if a particular treatment is more effective for one but not the other characteristic. Additionally, examining the effect of factors other than treatments (stress, individual or societal events, etc.) on depression and pain may depend on the degree to which a measure captures state vs. trait aspects of a symptom. Knee arthroplasty surgery results in large group-level improvements but also large variation in extent of individual-level baseline status and improvement in pain and function following surgical recovery.[12,13,31] Substantial between-person baseline variation and mean change over time in depression and pain catastrophizing also are found in KA.[18,30,40,47] It is therefore an ideal patient group for the study of trait versus state characteristics of these measures.
Our purpose was to determine the extent to which the PCS and the PHQ-8 measure trait versus state characteristics. We partitioned the variances of the PCS and PHQ-8 into trait versus state contributions and we expected to find that the measures reflect both trait and state characteristics.[10,15]
2. METHODS
2.1. Study Design and Participants
The current study is a secondary analysis of our Knee Arthroplasty Skills Training (KASTPain) trial. The protocol and full results of the trial have been reported elsewhere.[39,40] Our study was a three-arm randomized clinical trial conducted at five sites (Duke University, New York University Medical Center, Virginia Commonwealth University, Wake Forest University, and Southern Illinois University). Institutional review boards from all sites approved the study and all participants signed consent forms prior to participation.
To be admitted, participants were aged 45 years or older, diagnosed with osteoarthritis, and had their arthroplasty surgery scheduled 1–8 weeks after consent. Participants had to be English speaking and scored 16 or greater on the Pain Catastrophizing Scale. Patients were excluded if they were scheduled for bilateral knee surgery or revision surgery, had hip or KA within 6 months of the surgery of interest, had been diagnosed with inflammatory arthritis (e.g., rheumatoid arthritis), planned to have hip or KA within 6 months after the index knee surgery, scored ≥20 on a depression screener indicating severe clinical depression[41] or scored ≤2 on a cognitive screener indicating cognitive deficit.[6]
The main trial findings indicated that there was no effect of either pain coping skills or arthritis education relative to usual care on the primary outcome (i.e., Western Ontario and McMaster Universities (WOMAC) Pain scale)[2] and all secondary outcomes (e.g., WOMAC Function, Pain Catastrophizing Scale, physical performance measures).[22,23]
2.2. Randomization and Masking
Briefly, participants were randomized using permuted block sizes of three or six, stratified by surgeon. This randomization approach ensures that variation attributed to surgeon and site in a variety of known and unknown factors (e.g., operative/postoperative anesthesia and pain control, surgical technique) is balanced among treatment groups. We used the REDCap web interface to reveal randomized group assignment after baseline data collection. Participants and interventionists were not blinded. Data collectors, surgeons and investigators were blinded to group assignment until data collection was completed.
2.3. Interventions
The three treatment arms were usual care, pain coping skills training or arthritis education. Usual care consisted of usual postoperative rehabilitation. Participants randomized to either pain coping skills training or arthritis education received usual postoperative rehabilitation and in addition, received eight, 50-minute sessions of one-on-one instruction delivered over an approximate 2-month perioperative period beginning approximately 2 weeks pre-surgery. The first session was delivered in-person and the remaining sessions were delivered by telephone.
Pain coping skills training was delivered by site physical therapists with at least two years of clinical experience treating patients with KA. Training consisted of a 2-day training session conducted by clinical psychologists at Duke University who were highly experienced in the delivery of pain coping skills training. Physical therapists also relied on a detailed training manual and regular conference calls with the study team to guide the fidelity of treatment delivery. All treatment sessions were audio-recorded. Local clinical psychologists held monthly conference calls with physical therapists and monitored treatment delivery by listening to audiotapes throughout the study.
Arthritis education was delivered by registered nurses with at least two years of experience in the care of persons with osteoarthritis. Nurses were trained by DLR using a detailed manual. This treatment arm was designed to account for treatment effects attributable to similar amounts of time and attention from a caring provider. By comparing treatment effects in the arthritis education arm to that in the pain coping arm, we could determine effects attributable to the presumed active ingredient under study, pain coping skills. More detail on the trial was well as the treatment manuals is provided in the main paper.[40]
2.4. Follow-up
Trained data collectors, blind to treatment group, collected all baseline data (in person) and follow-up data by telephone (using up to 8 attempts) at 2 months, 6 months and 12 months following surgery, the primary endpoint. Participants were compensated $50 at baseline and $80 for completing all follow-up assessments.
2.5. Depression and Pain Catastrophizing Measures
The Patient Health Questionnaire (PHQ-8) contains 8 items and was used to quantify extent of depressive symptoms.[27] For each depressive symptom, respondents are asked how often they have been bothered by it in the past 2 weeks, with responses being not at all, several days, more than half the days, and nearly every day; thus each item is scored from 0 to 3. The PHQ-8 corresponds highly with the well validated PHQ-9,[25,48] has identical severity thresholds, and is scored from 0 to 24 with higher scores indicating more severe depressive symptoms.
The 13-item Pain Catastrophizing Scale (PCS) is one of the best validated and widely-used catastrophizing measures.[44] Respondents are asked to what degree they experience of 13 specific thoughts or feelings when they are in pain. Each item is scored 0 to 4 with response options being not at all, to a slight degree, to a moderate degree, to a great degree, or all the time. The PCS total score ranges from 0 (no catastrophizing) to 52 (very high pain catastrophizing). Both the PCS and the PHQ-8 were measured at baseline and 2 months, 6 months and 12 months following surgery by data collectors who were blinded to treatment arm.
2.6. Other Measures
Anxiety was assessed the 7-item Generalized Anxiety Disorder (GAD-7) scale which has been shown to be a valid severity measure for not only generalized anxiety disorder but other common anxiety disorders as well.[26] Pain severity and physical function were assessed with the Western Ontario and McMaster Universities Osteoarthritis (WOMAC) scales for which higher scores indicate worse pain and greater functional difficulty, respectively. We used a fibromyalgia diagnostic screening instrument that asked participants to identify each of the 16 areas on their body they were experiencing pain for at least the prior 3 months including, for example, the low back, neck, right shoulder right hip, and right upper leg (below hip to knee).[1,35]
2.7. Predictors of Interest
The seven baseline predictors of interest were treatment arm, age, race (dichotomized to either African American or non-African American), anxiety, physical function, pain severity, and number of bodily pain sites. These variables were chosen based on prior evidence of associations with depressive symptoms and catastrophizing.[2,9,24,34,35,42]
2.8. Statistical Analysis
The latent trait-state model has been used to partition trait, state and error (residual) components of constructs including depression.[10,11,15] The latent trait-state models are parametric representation of inter-individual differences in intra-individual change. [10,11,15,16] We used the multitrait generalization of the latent trait-state model to partition trait and state variability in PCS and PHQ-8 individual item responses simultaneously.[16] Aside from trait and state, all other sources of variability in item responses were subsumed under item residuals. We used diagonally-weighted least squares estimator (WLSMV) and the y* parameterization (i.e., the underlying continuous latent response variate) in model estimation to explicitly take account of the ordinal response format of PCS and PHQ-8 items.
The model involved four first-order time-specific PCS and four PHQ-8 factors accounting for the variability of y* in their respective scales. The trait PCS and trait PHQ-8 contributions were defined as second-order factors (traits) accounting for the covariances among the respective first-order factors, hence the partitioning of covariances among the first-order factors into traits and the first-order factor disturbances (states). States capture time effect and person X time interactions. Conceptually, this means that at one extreme, the occasion-specific factors are uncorrelated. That is, a construct measured at a specific occasion is unrelated to (or unpredictable from) the measurement of the same construct at all other occasions. In this case, the construct is considered as purely state. At the other extreme, the first-order occasion-specific factors are perfectly correlated. That is, the measurement of a construct on one occasion tells us everything about this construct at all other occasions. In this case, the construct is considered as purely trait. Between the two extremes, the multitrait generalization of the latent trait-state model allows constructs to have both trait (common across all occasions) and state (occasion specific) characteristics. Such phrases as “individual situational stability” and “individual situational variability” often correspond to the latent trait and latent state variables in the latent trait-state model.
As a part of the research design, participants with PCS scores < 16 were excluded. Thus, in the current study, PCS items were treated as censored variables for the low scores. For the PCS items, we used tobit modeling with below censoring, which is a standard and well accepted likelihood model to take into account design-based censoring when study data comprises truncated data (i.e., as in our parent study, baseline data did not include PCS score of less than 16)[5] The small amount of missing data (e.g., 90% retention at 12-month follow-up) was handled with the full information maximum likelihood method. Due to the cluster sampling of patients within surgeons, we used the Huber and White sandwich estimator to obtain correct test statistics and standard errors. In the prediction model, we added five predictors of both trait catastrophizing and trait depression to the first model. Parenthetically, the simultaneous prediction of trait and state variables results in a parametrically under-identified model and therefore the focus was solely on prediction of trait characteristics
3. RESULTS
A total of 402 patients consented to participate of whom 384 underwent knee arthroplasty. A total of 267 (66%) were female, 143 (34%) were African American and the mean number of baseline chronic bodily pain sites was 5.5 (sd = 4.0). Mean age of the sample was 63.2 (sd = 8.0) years. The mean baseline PHQ-8 score was 6.0 (sd = 5.0) and the mean PCS score was 30.0 (sd = 9.3). Baseline characteristics of the sample are summarized in Table 1 while baseline and follow-up data for the PCS and PHQ-8, are summarized in Table 2.
Table 1.
Characteristics of the Sample Prior to Surgery
| Baseline Characteristics | (n =402) | |
|---|---|---|
| Age, mean (SD) | 63.2 | (8.0) |
| Sex (female), N (%) | 267 | (66) |
| Body mass index (Kg/m2), mean (SD) | 32.3 | (6.2) |
| Race or ethnic group, N, (%) | ||
| White | 249 | (59) |
| African American | 143 | (34) |
| Hispanic | 13 | (3) |
| Asian | 8 | (2) |
| Declineda | 6 | (1) |
| Current Income, N (%) | ||
| < $10,000 | 42 | (10) |
| $10,000 to $24,999 | 84 | (21) |
| $25,000 to $49,999 | 91 | (23) |
| $50,000 to $99,999 | 94 | (23) |
| $100,000 or > | 53 | (13) |
| Declined | 38 | (10) |
| Current work status, N (%) | ||
| Employed | 132 | (33) |
| Not working in part due to health problems | 102 | (25) |
| Not working for other reasons | 167 | (42) |
| Declined | 1 | (0.2) |
| Education, N (%) | ||
| Less than high school | 26 | (7) |
| High school graduate | 91 | (23) |
| Some college | 103 | (26) |
| College degree or higher | 182 | (45) |
| Marital Status, N (%) | ||
| Married | 197 | (49) |
| Divorced | 80 | (20) |
| Never Married | 49 | (12) |
| Widowed | 47 | (12) |
| Separated | 20 | (5) |
| Member of an unmarried couple | 7 | (2) |
| Declined | 2 | (1) |
| Current smoker (yes) N, (%) | 47 | (12) |
| Health History | ||
| Modified Charlson comorbidity, mean (SD)b | 8.7 | (4.1) |
| Knee pain duration, median years (IQR) | 6 | (3–15) |
| Opioid use at baseline, N, (%) | 121 | (32) |
| Psychological Health | ||
| Patient Health Questionnaire (PHQ-8), mean (SD)c | 6.0 | (5.0) |
| Generalized Anxiety Scale (GAD-7), mean (SD)d | 5.4 | (4.9) |
| Pain Catastrophizing Scale, mean (SD)i | 30.0 | (9.3) |
| Outcome Scores | ||
| WOMAC Pain Scale, mean (SD)f | 11.4 | (3.4) |
| WOMAC Physical Function, mean (SD)g | 37.2 | (11.6) |
Abbreviations: WOMAC, Western Ontario and McMaster Universities Osteoarthritis Index
Race/ethnicity category of “Other” indicates, other (not specified), or missing. Sum may equal > 100% because of multiple categories.
Modified Charlson Comorbidity score range is 0 to 45. Higher scores equate to greater comorbidity burden.
PHQ-8 score range is 0 to 24. Higher scores equate to more depressive symptoms.
GAD-7 score range is 0 to 21. Higher scores equate to more anxiety.
Arthritis Self Efficacy Scale score range is 0 to 80. Higher scores equate to more self-efficacy.
WOMAC Pain Scale score range is 0 to 20. Higher scores equate to more function limiting pain.
WOMAC Function scale range is 0 to 68. Higher scores equate to more difficulty with functional activities.
Short Physical Performance Battery score range is 0 to 12. Higher scores equate to better performance.
Pain Catastrophizing Scale range is 0 to 52. Higher scores equate to more pain catastrophizing.
Table 2.
Baseline and follow-up scores on the Pain Catastrophizing Scale and the Patient Health Questionaire-8
| Baseline (pre-op) | 2-month postop | 6-month postop | 12-month postop | |||||
|---|---|---|---|---|---|---|---|---|
| Scale | Score (sd, range) | # missing out of n = 402 | Score (sd, range) | # missing out of n = 384 | Score (sd, range) | # missing out of n = 384 | Score (sd, range) | # missing out of n = 384 |
| PCS | 30.0 (9.3, 16–52) | - | 9.6 (10.9, 0–52) | 45 | 6.9 (10.7, 0–48) | 53 | 6.8 (11.2, 0–52) | 38 |
| PHQ-8 | 6.0 (5.0, 0–22) | - | 4.5 (4.4, 0–24) | 39 | 3.2 (4.2, 0–21) | 52 | 3.2 (4.0, 0–24) | 38 |
The fitting of a multitrait-multioccasion generalization of the latent trait-state model of catastrophizing and depression converged properly. The model fit was adequate: χ2=3,706, df=3,393, p<.001; RMSEA=0.015; 90% CI = 0.011 – 0.018; CFI=0.937; TLI=0.935. Item-level trait, state, and residual variance partitioning appears in Table 3. For all items, trait variability is larger than state variability. Item variability due to both trait and state is larger for catastrophizing items than depression items.
Table 3.
Variance partitioning of items in the Pain Catastrophizing Scale (PCS) and Patient Heath Questionnaire-8 (PHQ-8)
| Trait (%) | State (%) | Residual (%) | |
|---|---|---|---|
| Catastrophizing (PCS) | |||
| 1. Worry about pain ending. | 42.13 | 18.50 | 39.37 |
| 2. Can’t go on. | 40.66 | 16.44 | 43.00 |
| 3. Terrible and never getting better. | 47.23 | 19.45 | 33.32 |
| 4. Awful and overwhelms | 50.74 | 26.52 | 22.74 |
| 5. Can’t stand it | 50.78 | 22.02 | 27.20 |
| 6. Become afraid pain get worse. | 39.99 | 17.41 | 42.60 |
| 7. Think of prior pain. | 32.22 | 15.78 | 52.10 |
| 8. Anxious for pain to go away. | 38.17 | 16.10 | 45.73 |
| 9. Can’t keep it out of my mind. | 46.12 | 22.48 | 31.40 |
| 10. Keep thinking about how much it hurts. | 47.90 | 22.97 | 29.13 |
| 11. Keep thinking how badly want pain to stop. | 37.80 | 24.79 | 27.41 |
| 12. Nothing I can to do reduce pain. | 41.40 | 18.42 | 40.18 |
| 13. Something serious might happen. | 37.30 | 18.80 | 43.90 |
| Depression (PHQ-8) | |||
| 1. Little interest in doing things | 32.66 | 20.52 | 46.82 |
| 2. Feeling down, hopeless | 38.11 | 30.89 | 30.40 |
| 3. Trouble sleeping, too little or too much | 21.53 | 13.47 | 64.90 |
| 4. Feeling tired, little energy | 29.58 | 19.68 | 50.74 |
| 5. Poor appetite or overeating | 21.78 | 14.58 | 66.64 |
| 6. Feeling bad about yourself | 33.89 | 26.34 | 39.77 |
| 7. Trouble concentrating | 30.13 | 22.07 | 47.80 |
| 8. Moving or speaking too slowly | 27.21 | 18.67 | 54.12 |
Overall results from variance partitioning are depicted in the Figure. For both catastrophizing and depression, the trait - state variance ratio was approximately 2:1 for the PCS and 3:2 for the PHQ-8 scores indicating that both sets of test scores reflect enduring trait-like characteristics more than situational or state-like characteristics. The catastrophizing scores reflect greater amount of both trait and state characteristics than the respective depression scores. Overall, the latent traits and latent states explain 63.2% (trait=43.2%; state=20.0%) and 50.2% (trait=29.4%; state=20.8%) of the variability in PCS and PHQ-8, respectively.
Figure:
The Figure illustrates the Partitioning of Trait versus State Variability of Pain Catastrophizing Scale and the Patient Health Questionnaire-8 Depression Scale over Four Measurement Occasions
In a second model, we re-estimated the multitrait generalization of the latent trait-state model of catastrophizing and depression with anxiety, physical function impairment, pain severity, and number of bodily pain sites, age, race/ethnicity, and treatment status as the predictors of latent trait catastrophizing and trait depression. Standardized path coefficients are displayed in Table 4. Chronic bodily pain sites, anxiety, age, and race/ethnicity were significant predictors of both trait catastrophizing and trait depression. Specifically, patients with higher anxiety or a greater number of bodily pain sites as well as younger or African-American patients had higher levels of trait catastrophizing and trait depression than those with lower anxiety, fewer bodily pain sites, older patients, and patients who were not self-identified as African American. Poorer physical functioning was associated with higher trait catastrophizing but not depression. Neither trait catastrophizing nor depression differed significantly between treatment groups or by pain severity.
Table 4.
Predictors of trait catastrophizing and trait depression from the multitrait-multioccasion extension of the latent trait-state model
| Trait | ||
|---|---|---|
| Predictor | Catastrophizing | Depression |
| Anxiety severity | 0.27*** | 0.52*** |
| Number of bodily pain sites | 0.16** | 0.19*** |
| Race (African American) | 0.17** | 0.12* |
| Age | −0.18*** | −0.13*** |
| Physical function impairment | 0.20** | 0.03ns |
| Pain severity | −0.07ns | 0.04ns |
| Treatment | 0.01ns | −0.03ns |
p<0.05
p<0.01
p<0.001;
ns=not significant.
4. DISCUSSION
4.1. Main findings
Our study had several clinically important and novel findings. First, clinicians should be aware that both state (i.e., situational) and trait (i.e., dispositional) features contribute to PCS and PHQ-8 measures. Second, trait contributions were larger than that of state characteristics for both measures. Therefore, when clinicians use these scales to quantify extent of pain catastrophizing or depressive symptoms at a point in time during the plan of care, the measures reflect both state and trait characteristics with trait characteristics being more dominant. Third, trait-based catastrophizing and depression was higher in patients who are younger, African-American, and those with higher anxiety, or have a large number of bodily pain sites.
4.2. Comparisons to prior evidence
Our study is the first to our knowledge to use a latent trait-state model to simultaneously estimate both state and trait contributions to the PCS and the PHQ-8. Other depression scales have been studied for state/trait contributions and reported somewhat similar findings. For example, the child and parent versions of the Children’s Depression Inventory (CDI) [10] and the Center for Epidemiological Studies-Depression inventory (CES-D) [15] captured both state and trait characteristics. The CES-D was found to reflect approximately equal trait and state characteristics in adolescents.[15] The CDI, on the other hand, shows different patterns of trait/state contributions depending on the age of the participant. For children, dynamic state characteristics of the CDI dominate while for adolescents and adults completing the age-appropriate versions of the CDI, stable trait characteristics dominate.[10] Evidence suggests contributions of state versus trait characteristics of depression measures may vary with younger children demonstrating greater state characteristics while adolescent and adult responses reflecting a greater percentage of stable trait characteristics. These data combined with our findings also suggest that state and trait contributions to depression scores likely vary depending on the age of the sample and the scale being studied. We previously reported no treatment effect between three arms when the outcomes are potentially comprised of traits and states.[40] We replicated no treatment effect on catastrophizing and depression traits after partialling out the states in this study.
4.3. Clinical and research-based relevance
The extent to which the PCS or the PHQ-8 reflect stable trait or situational state characteristics does not necessarily inform longitudinal mean-level change in these measures. For example, in the main results from our knee replacement trial from which our current data is derived,[40] PCS scores demonstrated substantial change from a mean of 30.0 (sd = 9.3) preoperatively to a mean of 6.8 (sd = 11.2) one-year following surgery. Smaller but still potentially important changes occurred with PHQ-8 scores, from a mean of 6.0 preoperatively to a mean of 3.2 one year post surgery. While PCS and PHQ-8 scores at a single time point reflect mostly a stable trait more so than a dynamic state, the participants’ life situations and particularly their knee pain severity also changed substantially over the study period and this likely led to substantial changes in both the PCS and PHQ-8. For example, WOMAC Pain scores improved by almost 75% (from a mean of 11.39 at the preoperative visit to a mean of 3.07 one year following surgery) and 74.9% of the sample reported being satisfied with their outcome one-year following surgery. Presumably stable traits are known to change over time, particularly following important life events [4] and in the presence of chronic pain.[21]
In our view, it is important not to equate a score’s propensity to reflect trait and state characteristics at a point in time with the extent to which scores change over time. A patient’s score can change over time, sometimes dramatically as our study illustrated, in spite of the fact that the majority of the score at a point in time reflects trait characteristics.
Prior research has suggested that because the PCS scores improve over time as pain decreases, that the scale reflects a situational state and that the scale does not reflect trait-based characteristics.[30,47] Our data fundamentally question these assumptions and provide strong evidence to indicate that in spite of sometimes substantial changes over time for some patients, the PCS and the PHQ-8 capture stable trait characteristics along with a smaller but likely still important proportion of state characteristics. Clinicians should not assume that score changes in PCS or PHQ-8 scores indicate that the measures only capture situational state characteristics. A larger proportion of PCS and PHQ-8 scores reflect trait more than state characteristics.
Investigators conducting experimental pain studies have developed pain catastrophizing measures with the intent of capturing trait versus state characteristics when testing responses to experimentally induced pain.[7,19] Our data question the scientific premise for using the PCS and modified versions of the PCS for inferring pure trait versus state pain catastrophizing. It is likely that these measures reflect both trait and state characteristics. Additionally, our findings indicate neither individual items nor summary scores for the PCS or PHQ-8 should be used to inform inferences regarding pure state versus trait characteristics.
4.4. Study limitations and generalizability
While our study has substantial strengths including a reasonably large sample with four measurement occasions over a one-year period, there are some important limitations. We studied only persons undergoing knee arthroplasty and depression symptoms were relatively mild; however, at all time points, we had a full range of depressive symptom scores from no depressive symptoms to severe depressive symptoms. Timeframes of interest vary for the two measures (i.e., patients are asked to consider the prior two weeks for the PHQ-8 and no timeframe is mentioned in PCS instructions) and we were unable to determine the role timeframe played in trait versus state contributions for the two measures. Our analytic approach only provides estimates of state versus trait characteristics for the sample as a whole over the one-year period and not for individual participants. Our study also does not consider individual person effects of day-to-day life situations and stressors. To make inferences about day-to-day individual effects of mood and behavior, a dynamic structural equation modeling approach, with much more frequent data collection, would be appropriate.[49] We had a restricted range of PCS scores preoperatively because of our inclusion criteria. However, all follow-up PCS score ranges covered the full extent of pain catastrophizing from none to severe. We treated all PCS items as censored at the lower end of the scale and used tobit modeling to properly address the 16 or greater PCS inclusion criterion in our analyses. We cannot exclude the possibility that our findings may have been influenced by these sample characteristics and patterns of change. It is important to replicate our findings on samples of patients with different disorders and full ranges of PCS and PHQ-8 scores across all measurement occasions. As a variance partitioning method, latent trait-state models are not suitable for making inferences about mean changes. We have addressed the mean change issues in pain, pain catastrophizing and depression using a variety of statistical models.[14,29,40] Given the four measurement occasions over a period of one year, the states are defined as occasion-specific variability unaccounted for by the stable traits. As such, states may not necessarily be interpreted as the variability in people’s day to day life situations. To make inferences about day to day changes in mood and behavior, definition of states adopted in dynamic structural equation modeling (DSEM), which require intensive data collections (e.g., hourly, daily), may be more appropriate as it allows for making inferences about traits and states in each and every person.[49] Finally, our analysis of predictors was limited because the analytic approach precludes simultaneous identification of predictors of both trait and state characteristics. State-based predictors of PCS and PHQ-8 scores are unexplored in our study.
5. Conclusions
Our study demonstrated that the PCS and the PHQ-8 consist of both enduring trait and dynamic state characteristics but both measures reflected enduring trait characteristics more so than dynamic state characteristics for both the summary scores and for individual items. Clinicians and researchers using these scales are measuring both state and trait characteristics and not purely trait or state-based characteristics when using either the PCS or PHQ-8. Effectiveness of clinical interventions may differ in altering either trait or state characteristics. Trialists interested in testing the efficacy of interventions should consider whether the intervention is designed to impact trait or state characteristics of catastrophizing and depression. Instrument selection may by driven, in part, by whether a particular treatment is more effective for one but not the other characteristic.
What is already known about this topic?
Catastrophizing and depression scales are often assumed to measure either trait or state characteristics.
Trait versus state components of depression scales differ as a function of age.
What does this study add?
The trait - state variance ratio was 2:1 for catastrophizing and 3:2 for depression.
Bodily pain sites, anxiety, young, and African American patients had high levels of trait catastrophizing and trait depression.
Acknowledgements:
This study was funded by grants from the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (UL1TR000058) and the National Institute of Arthritis Musculoskeletal and Skin Diseases (NIAMS) (UM1AR062800). The authors also thank the participants who enrolled in this study. They also thank the physical therapists and nurses for their role in providing the interventions under study, as well as study staff and study psychologists, at Duke University, New York University, Southern Illinois University, Virginia Commonwealth University, and Wake Forest University. With the exception of the federal government grant funding listed above, the authors indicate no conflicts of interest.
Funding Source: The National Institutes of Health (NIH) National Center for Advancing Translational Sciences (UL1TR000058) and the National Institute of Arthritis Musculoskeletal and Skin Diseases (NIAMS) (UM1AR062800). None declared.
Footnotes
Conflict of Interest: None declared.
Conflicts of interest: The investigators received federal grant funding to support the work and report no other conflicts of interest.
Contributor Information
Levent Dumenci, Department of Epidemiology and Biostatistics, 1301 Cecil B. Moore, Ave., Ritter Annex, Room 939, Temple University, Philadelphia, PA, USA
Kurt Kroenke, Indiana University School of Medicine, and Regenstrief Institute, Indianapolis, Indiana, USA
Francis J. Keefe, Pain Prevention and Treatment Research, Department of Psychiatry and Behavioral Sciences, Duke University, Durham, NC, USA
Dennis C. Ang, Department of Medicine, Section of Rheumatology, Wake Forest School of Medicine, Winston-Salem, NC, USA
James Slover, Department of Orthopaedic Surgery, New York University Medical Center, New York, New York, USA
Robert A. Perera, Dept of Biostatistics, VA Commonwealth Univ, Richmond VA, USA,
Daniel L. Riddle, Departments of Physical Therapy, Orthopaedic Surgery and Rheumatology, Virginia Commonwealth University, Richmond, VA, USA
REFERENCES
- [1].Arnold LM, Stanford SB, Welge JA, Crofford LJ. Development and testing of the fibromyalgia diagnostic screen for primary care. J Womens Heal 2012;21:231–239. [DOI] [PubMed] [Google Scholar]
- [2].Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 1988;15:1833–1840. [PubMed] [Google Scholar]
- [3}.Birnie KA, Chambers CT, Chorney J, Fernandex CV, McGrath PJ. Dyadic analysis of child and parent trait and state pain catastrophizing in the process of children’s pain communication. Pain 2016:157(4) 938–948. [DOI] [PubMed] [Google Scholar]
- [4].Bleidorn W, Hopwood CJ, Lucas RE. Life Events and Personality Trait Change. J Pers 2018;86:83–96. [DOI] [PubMed] [Google Scholar]
- [5].Breen R The Tobit Model for Censored Data” Regression Models: Censored, Samples Selected, or Truncated Data. Thousand Oaks, California, Sage, 1996. [Google Scholar]
- [6].Callahan CM, Unverzagt FW, Hui SL, Perkins AJ, Hendrie HC. Six-item screener to identify cognitive impairment among potential subjects for clinical research. Med Care 2002;40:771–781. [DOI] [PubMed] [Google Scholar]
- [7].Campbell CM, Kronfli T, Buenaver LF, Smith MT, Berna C, Haythornthwaite JA, Edwards RR. Situational Versus Dispositional Measurement of Catastrophizing: Associations With Pain Responses in Multiple Samples. J Pain 2010;11:443–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Chien AJ, Dunner DL. The tridimensional personality questionnaire in depression: State versus trait issues. J Psychiatr Res 1996;30:21–27. [DOI] [PubMed] [Google Scholar]
- [9].Chibnall JT Tait RJ. Confirmatory factor analysis of the Pain Catastrophizing Scale in African American and Caucasian Workers’ Compensation claimants with low back injuries. Pain 2005. 113:369–375. [DOI] [PubMed] [Google Scholar]
- [10].Cole DA, Martin NC. The longitudinal structure of the children’s depression inventory: Testing a latent trait-state model. Psychol Assess 2005;17:144–155. [DOI] [PubMed] [Google Scholar]
- [11].Cole DA, Nolen-Hoeksema S, Girgus J, Paul G. Stress exposure and stress generation in child and adolescent depression: A latent trait-state-error approach to longitudinal analyses. J Abnorm Psychol 2006;115:40–51. [DOI] [PubMed] [Google Scholar]
- [12].Collins JE, Donnell-Fink LA, Yang HY, Usiskin IM, Lape EC, Wright J, Katz JN, Losina E. Effect of Obesity on Pain and Functional Recovery Following Total Knee Arthroplasty. J Bone Jt Surg Am 2017;99:1812–1818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Dowsey MM, Robertsson O, Sundberg M, Lohmander LS, Choong PFM, Dahl A. Variations in pain and function before and after total knee arthroplasty: a comparison between Swedish and Australian cohorts. Osteoarthr Cartil 2017;25:885–891. [DOI] [PubMed] [Google Scholar]
- [14].Dumenci L, Perera RA, Keefe FJ, Ang DC, Slover J, Jensen MP, Riddle DL. Model-based pain and function outcome trajectory types for patients undergoing knee arthroplasty: A secondary analysis from a randomized clinical trial. Osteoarthr Cartil 2019;27:878–884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Dumenci L, Windle M. A latent trait-state model of adolescent depression using the center for epidemiologic studies-depression scale. Multivariate Behav Res 1996;31:313–330. [DOI] [PubMed] [Google Scholar]
- [16].Dumenci L, Windle M. A multitrait-multioccasion generalization of the latent trait-state model: Description and application. Struct Equ Model 1998;5:391–410. [Google Scholar]
- [17].Edwards RR, Campbell CM, Fillingim RB. Catastrophizing and experimental pain sensitivity: Only in vivo reports of catastrophic cognitions correlate with cognitive responses. J Pain 2005:6(5) 338–1339. [DOI] [PubMed] [Google Scholar]
- [18].Edwards RR, Haythornthwaite JA, Smith MT, Klick B, Katz JN. Catastrophizing and depressive symptoms as prospective predictors of outcomes following total knee replacement. Pain ResManag 2009;14:307–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Edwards RR, Smith MT, Stonerock G, Haythornthwaite JA. Pain-related catastrophizing in healthy women is associated with greater temporal summation of and reduced habituation to thermal pain. Clin J Pain 2006;22:730–737. [DOI] [PubMed] [Google Scholar]
- [20].Fabian LA, McGuire L, Goodin BR, Edwards RR. Ethnicity, Catastrophizing, and Qualities of the Pain Experience. Pain Med 2011;12:314–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Fishbain DA, Cole B, Cutler RB, Lewis J, Rosomoff HL, Rosomoff RS. Chronic pain and the measurement of personality: Do states influence traits? Pain Med 2006;7:509–529. [DOI] [PubMed] [Google Scholar]
- [22].Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, Scherr PA, Wallace RB. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–M94. [DOI] [PubMed] [Google Scholar]
- [23].Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW, Berman LB. The 6-minute walk: a new measure of exercise capacity in patients with chronic heart failure. Can Med Assoc J 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- [24].Hooten WM, Knight-Brown M, Townsend CO, Laures HJ. Clinical outcomes of multidisciplinary pain rehabilitation among african american compared with caucasian patients with chronic pain. Pain Med. 2012;13:1499–1508. [DOI] [PubMed] [Google Scholar]
- [25].Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry 2010;32:345–359. [DOI] [PubMed] [Google Scholar]
- [26].Kroenke K, Spitzer RL, Williams JBW, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med 2007;146:317–325. [DOI] [PubMed] [Google Scholar]
- [27].Kroenke K, Strine TW, Spitzer RL, Williams JB, Berry JT, Mokdad AH. The PHQ-8 as a measure of current depression in the general population. JAffectDisord 2009;114:163–173. [DOI] [PubMed] [Google Scholar]
- [28].Kroenke K, Unutzer J. Closing the False Divide: Sustainable Approaches to Integrating Mental Health Services into Primary Care. J Gen Intern Med 2017;32:404–410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kroenke K, Wu J, Bair MJ, Krebs EE, Damush TM, Tu W. Reciprocal relationship between pain and depression: A 12-month longitudinal analysis in primary care. J Pain 2011;12:964–973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Lape EC, Selzer F, Collins JE, Losina, E. Stability of measures of pain catastrophizing and widespread pain following total knee replacement (TKR). Arthiritis Care Res 2019;Publish Ah. [DOI] [PubMed] [Google Scholar]
- [31].Lingard EA, Katz JN, Wright EA, Sledge CB. Predicting the outcome of total knee arthroplasty. J Bone Jt Surg Am 2004;86-A:2179–2186. [DOI] [PubMed] [Google Scholar]
- [32].Martel MO, Wasan AD, Jamison RN, Edwards RR. Catastrophic thinking and increased risk for prescription opioid misuse in patients with chronic pain. Drug Alcohol Depend 2013;132:335–341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Mathur VA, Kiley KB, Carroll CP, Edwards RR, Lanzkron S, Haythornthwaite JA, Campbell CM. Disease-Related, Nondisease-Related, and Situational Catastrophizing in Sickle Cell Disease and Its Relationship With Pain. J Pain 2016;17:1227–1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Meints SM, Wang V, Edwards RR. Sex and race differences in pain sensitization among patients with chronic low back pain. J Pain 2018:19(12) 1461–1479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].McConnell S, Kolopack P, Davis AM. The Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC): a review of its utility and measurement properties. Arthritis Rheum. 2001;45(5):453–61. [DOI] [PubMed] [Google Scholar]
- [36].Mun CJ, Ruehlman L, Karoly P. Examining the Adjustment Patterns of Adults With Multiple Chronic Pain Conditions and Multiple Pain Sites: More Pain, No Gain. J Pain In press, 2019). [DOI] [PubMed] [Google Scholar]
- [37].Murray CJ, Vos T, Lozano R, Naghavi M, Flaxman AD, Michaud C, Ezzati M, Shibuya K, Salomon JA, Abdalla S, Aboyans V, Abraham J, Ackerman I, Aggarwal R, Ahn SY, Ali MK, Alvarado M, Anderson HR, Anderson LM, Andrews KG, Atkinson C, Baddour LM, Bahalim AN, Barker-Collo S, Barrero LH, Bartels DH, Basanez MG, Baxter A, Bell ML, Benjamin EJ, Bennett D, Bernabe E, Bhalla K, Bhandari B, Bikbov B, Bin AA, Birbeck G, Black JA, Blencowe H, Blore JD, Blyth F, Bolliger I, Bonaventure A, Boufous S, Bourne R, Boussinesq M, Braithwaite T, Brayne C, Bridgett L, Brooker S, Brooks P, Brugha TS, Bryan-Hancock C, Bucello C, Buchbinder R, Buckle G, Budke CM, Burch M, Burney P, Burstein R, Calabria B, Campbell B, Canter CE, Carabin H, Carapetis J, Carmona L, Cella C, Charlson F, Chen H, Cheng AT, Chou D, Chugh SS, Coffeng LE, Colan SD, Colquhoun S, Colson KE, Condon J, Connor MD, Cooper LT, Corriere M, Cortinovis M, de Vaccaro KC, Couser W, Cowie BC, Criqui MH, Cross M, Dabhadkar KC, Dahiya M, Dahodwala N, Damsere-Derry J, Danaei G, Davis A, De LD, Degenhardt L, Dellavalle R, Delossantos A, Denenberg J, Derrett S, Des Jarlais DC, Dharmaratne SD, Dherani M, Diaz-Torne C, Dolk H, Dorsey ER, Driscoll T, Duber H, Ebel B, Edmond K, Elbaz A, Ali SE, Erskine H, Erwin PJ, Espindola P, Ewoigbokhan SE, Farzadfar F, Feigin V, Felson DT, Ferrari A, Ferri CP, Fevre EM, Finucane MM, Flaxman S, Flood L, Foreman K, Forouzanfar MH, Fowkes FG, Fransen M, Freeman MK, Gabbe BJ, Gabriel SE, Gakidou E, Ganatra HA, Garcia B, Gaspari F, Gillum RF, Gmel G, Gonzalez-Medina D, Gosselin R, Grainger R, Grant B, Groeger J, Guillemin F, Gunnell D, Gupta R, Haagsma J, Hagan H, Halasa YA, Hall W, Haring D, Haro JM, Harrison JE, Havmoeller R, Hay RJ, Higashi H, Hill C, Hoen B, Hoffman H, Hotez PJ, Hoy D, Huang JJ, Ibeanusi SE, Jacobsen KH, James SL, Jarvis D, Jasrasaria R, Jayaraman S, Johns N, Jonas JB, Karthikeyan G, Kassebaum N, Kawakami N, Keren A, Khoo JP, King CH, Knowlton LM, Kobusingye O, Koranteng A, Krishnamurthi R, Laden F, Lalloo R, Laslett LL, Lathlean T, Leasher JL, Lee YY, Leigh J, Levinson D, Lim SS, Limb E, Lin JK, Lipnick M, Lipshultz SE, Liu W, Loane M, Ohno SL, Lyons R, Mabweijano J, MacIntyre MF, Malekzadeh R, Mallinger L, Manivannan S, Marcenes W, March L, Margolis DJ, Marks GB, Marks R, Matsumori A, Matzopoulos R, Mayosi BM, McAnulty JH, McDermott MM, McGill N, McGrath J, Medina-Mora ME, Meltzer M, Mensah GA, Merriman TR, Meyer AC, Miglioli V, Miller M, Miller TR, Mitchell PB, Mock C, Mocumbi AO, Moffitt TE, Mokdad AA, Monasta L, Montico M, Moradi-Lakeh M, Moran A, Morawska L, Mori R, Murdoch ME, Mwaniki MK, Naidoo K, Nair MN, Naldi L, Narayan KM, Nelson PK, Nelson RG, Nevitt MC, Newton CR, Nolte S, Norman P, Norman R, O’Donnell M, O’Hanlon S, Olives C, Omer SB, Ortblad K, Osborne R, Ozgediz D, Page A, Pahari B, Pandian JD, Rivero AP. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012;380:2197–2223. [DOI] [PubMed] [Google Scholar]
- [38].Prenoveau JM, Craske MG, Zinbarg RE, Mineka S, Rose RD, Griffith JW. Are anxiety and depression just as stable as personality during late adolescence? Results from a three-year longitudinal latent variable study. J Abnorm Psychol 2011;120:832–843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Riddle DL, Keefe FJ, Ang D, Saleh KJ, Dumenci L, Jensen MP, Bair MJ, Reed SD, Kroenke K. A phase III randomized three-arm trial of physical therapist delivered pain coping skills training for patients with total knee arthroplasty: the kastpain protocol. BMC Musculoskelet Disord 2012;13:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Riddle DL, Keefe FJ, Ang DC, Slover JD, Jensen MP, Bair MJ, Kroenke K, Perera RA, McKee D, Dumenci L. Pain coping skills training for patients who catastrophize about their pain prior to knee arthroplasty: A multisite randomized clinical trial. J Bone Jt Surg Am 2019;101:218–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999;282:1737–1744. [DOI] [PubMed] [Google Scholar]
- [42].Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2007;14:317–325. [DOI] [PubMed] [Google Scholar]
- [43].Sullivan MJ, Thorn B, Haythornthwaite JA, Keefe F, Martin M, Bradley LA, Lefebvre JC. Theoretical perspectives on the relation between catastrophizing and pain. Clin J Pain 2001;17:52–64. [DOI] [PubMed] [Google Scholar]
- [44].Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psych Assess 1995;7:524–532. [Google Scholar]
- [45].Turner JA, Aaron LA. Pain-related catastrophizing: what is it? Clin J Pain 2001;17:65–71. [DOI] [PubMed] [Google Scholar]
- [46].Turner JA, Jensen MP, Warms CA, Cardenas DD. Catastrophizing is associated with pain intensity, psychological distress, and pain-related disability among individuals with chronic pain after spinal cord injury. Pain 2002;98:127–134. [DOI] [PubMed] [Google Scholar]
- [47].Wade JB, Riddle DL, Thacker LR. Is pain catastrophizing a stable trait or dynamic state in patients scheduled for knee arthroplasty? Clin J Pain 2012;28. [DOI] [PubMed] [Google Scholar]
- [48].Wu Y, Levis B, Riehm KE, Saadat N, Levis AW, Azar M, Rice DB, Boruff J, Cuijpers P, Gilbody S, Ioannidis JPA, Kloda LA, McMillan D, Patten SB, Shrier I, Ziegelstein RC, Akena DH, Arroll B, Ayalon L, Baradaran HR, Baron M, Bombardier CH, Butterworth P, Carter G, Chagas MH, Chan JCN, Cholera R, Conwell Y, de Man-van Ginkel JM, Fann JR, Fischer FH, Fung D, Gelaye B, Goodyear-Smith F, Greeno CG, Hall BJ, Harrison PA, Härter M, Hegerl U, Hides L, Hobfoll SE, Hudson M, Hyphantis T, Inagaki MD, Jetté N, Khamseh ME, Kiely KM, Kwan Y, Lamers F, Liu SI, Lotrakul M, Loureiro SR, Löwe B, McGuire A, Mohd-Sidik S, Munhoz TN, Muramatsu K, Osório FL, Patel V, Pence BW, Persoons P, Picardi A, Reuter K, Rooney AG, Santos IS, Shaaban J, Sidebottom A, Simning A, Stafford MD, Sung S, Tan PLL, Turner A, van Weert HC, White J, Whooley MA, Winkley K, Yamada M, Benedetti A, Thombs BD. Equivalency of the diagnostic accuracy of the PHQ-8 and PHQ-9: a systematic review and individual participant data meta-analysis. Psychol Med. 2019:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Asparouhov T, Hamaker EL, Muthen B. Dynamic Structural Equation Models. Struct Equ Modeling. 2018;25:359–388. [Google Scholar]