Introduction
Torture is a silent, global epidemic and pernicious source of trauma [1]. A 2015 meta-analysis estimated that of the three million refugees in the United States, approximately 44% or 1.3 million were tortured [2]. Women are particularly vulnerable within communities impacted by war and experience greater risk for poor health outcomes because of restricted access to health, legal, and economic resources [3,4]. Torture and trauma experiences that occur in the context of war or migration have long-term consequences for the physical and mental health and life course of surviving refugees and carries important significance for various aspects of youth adjustment through indirect transmission.
Intergenerational transmission of trauma is defined as the passage of trauma-related dysfunction experienced by one generation onto members of future generations who were not themselves exposed to the original trauma [5]. An emerging body of evidence highlights the relevance of intergenerational trauma among migrant and refugee populations [6–14]. The focus to date has been the development of a conceptual understanding of the impacts of war trauma on generations following the original exposure. Yet there remains a dearth of information on the mechanisms of action surrounding the perpetuation of trauma across generations to inform the development of family centered interventions to address these impacts.
Purpose
The purpose of the study was to explore and identify key relationships between maternal caregiver exposure to war trauma and torture, mental health, and physical health with youth adjustment. Identifying and understanding these relationships was conceptualized by the research team as a formative step in developing a family-centered intervention to address the generational effects of trauma on the well-being and adjustment of refugee mothers and youth. While the dominant torture treatment paradigm offers important and effective elements in recovery, the paradigm remains centered on individual recovery and thus generally disregards the impact of torture and war across and between generations. It is crucial to identify key explanatory factors and the mechanism of action involved in the transmission of trauma to inform the development of a family-centered intervention that mitigates the impact of the generational effects of trauma in families who have experienced trauma from torture and/or war.
The specific aims of the study were:
To investigate the associations between maternal torture and war trauma experiences, mental health distress and physical health problems with youth adjustment.
To examine whether maternal mental health distress and physical health problems mediated, moderated, or acted through a combined conditional process, the relationship between maternal torture and war trauma experiences and youth adjustment.
Torture is an intimate violation of dignity and personhood. The United Nations definition of torture as written in the Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment (1984) is: “any act by which severe pain or suffering, whether physical or mental, is intentionally inflicted on a person for such purposes as obtaining from him or a third person information or a confession, punishing him for an act he or a third person has committed or is suspected of having committed, or intimidating or coercing him or a third person, or for any reason based on discrimination of any kind, when such pain or suffering is inflicted by or at the instigation of or with the consent or acquiescence of a public official or other person acting in an official capacity…[15]” Secondary torture is the torture of close contacts or members of an individual’s family [16]. War trauma is the “exposure to an extremely traumatic event in the context of war. Extreme trauma refers to directly experiencing, witnessing, or learning about an event that involves actual or threatened death or serious injury, or other threat to physical integrity” [17].
Methods
Findings reported in this manuscript are situated within a larger explanatory mixed methods study. Data collection in the quantitative strand examined associations between maternal experiences of war trauma and torture, maternal mental and physical health, and maternal reported youth adjustment. The research team partnered with two prominent refugee-serving, community-based organizations: Karen Organization of Minnesota, which led study recruitment and remains engaged as a cultural broker, and The Center for Victims of Torture, which provided consultation in study design and analysis. Details of the involvement are specified below.
Sample
Karen refugees from Burma comprised the study sample. Minnesota has one of the most rapidly growing communities of refugees from Burma in the United States, and is strategically positioned as a site to build the science surrounding the effective provision of health services to a culturally unique post-trauma migrant population. There are an estimated 17,000 Karen currently residing in the state [18]. Karen refugees from Burma have experienced high rates of war trauma and resultant negative health outcomes [19]. Prior research has documented primary torture (27.4%), secondary torture (51.4%), and war trauma (86%) among resettled Karen refugees [20].
The primary recruitment source was the Karen Organization of Minnesota programs involving adolescent and young adult Karen youth. Maternal caregivers were contacted by phone by the organization’s community health liaison. Participants were given a brief description of the study and asked whether they would like additional information. For those individuals who gave permission, the PI and a Karen interpreter with specialized training in working with survivors of war trauma and torture placed a follow up telephone call to the individual. If the potential participant expressed further interest, an enrollment/data collection appointment was scheduled.
Criteria for inclusion were: women above the age of 18; Karen refugee resettled to the United States greater than one year prior to enrollment; caregiving responsibility for at least one child between the ages of 11 and 23; and reported primary or secondary torture or war trauma exposure. Criteria for exclusion included: severe or unstable mental or physical illness such as: acute psychosis, presence or risk of safety concerns, and/or a physical disability or illness, which prevented the potential participant from engaging in the interviews. We selected women with children from late childhood through adolescence and early adulthood because in our prior research this is a timeframe during which Karen families report disruption in balance and cohesion [21].
Procedures
Study activities and procedures were approved by the University of Minnesota Institutional Review Board (00000729). Data collection was field based, all surveys were completed during an in person encounter between the participant, interpreter, and primary author over a 6-month period. Participants chose whether to meet in their homes or a neutral, familiar location within the community. Following informed consent, participants completed the demographic questionnaire and self-report structured assessments. A skilled Karen interpreter with specialized training in supporting survivors of torture and war trauma provided professional language and cultural assistance for data collection.
Measures
Basic demographics including gender, age, marital status, employment, educational background, housing circumstances, and length of resettlement were collected via survey with all participants. Data collected from participants included self-reported mental health status [22]; maternal report of youth adjustment through the Strengths and Difficulties Questionnaire (SDQ) [23] for each child living in the household between the ages of 11 and 23 who was not married and/or raising their own children; maternal report of torture/war trauma experiences with a severity assessment [24]; maternal report of physical health symptoms and diagnoses.
Karen Mental health Screening Instrument (brief version).
The 5-item screening tool was developed by Brink et al. to screen for mental distress associated with major depression disorder (MDD) and posttraumatic stress disorder (PTSD) symptoms in newly arrived Karen refugees from Burma (α = 0.83) [22]. The screening tool assesses the frequency of concentration and memory issues, feelings of worthlessness, fear of losing control, social problems relation to trauma, and daily functioning within the past month using a 4-point Likert-type rating response scale ranging from 0- “not at all” to 3- “almost always.” Higher scores indicated greater endorsement of mental distress associated with MDD and PTSD symptoms.
General War Trauma and Torture Scale.
The three-item screening tool implemented in our study was adapted from a four-item version used by Shannon et al.(2015) to assess whether participants experienced primary and secondary torture and/or trauma in the context of war using a dichotomous yes/no response scale [24]. We modified the scale: 1) to prompt participants to respond to a question on the torture of family members within the second item inquiring about the experiences of family members in conflict, rather than as a standalone fourth item; and 2) included an evaluation of severity of impact of each experience from the perspective of participants using a Likert-type response scale ranging from 1-“very positive” to 5-“very negative.” Higher scores on the perceived severity of impact items indicated greater perceived impact of the experience.
Physical Health Questionnaire.
Physical health was assessed through a series of open-ended questions prompting participants on physical symptoms, diagnosed medical conditions, prescribed medications, and provider interactions, for example: “Do you take medicine to help with panic, thinking too much, difficulty sleeping, or heaviness in your heart? If so, which?” Responses to open ended questions were categorized and coded numerically by the primary author. The physical health problems variable was included as a predictor in the moderated mediation analysis. Self-reported health conditions included chronic pain, hypertension, diabetes, insomnia, headaches, liver disease, asthma, dizziness, high cholesterol, stomach and intestinal issues, heart problems, memory issues, regularity of visits to a health provider, and prescribed medications.
Strengths and Difficulties Questionnaire (maternal assessment of youth).
The 25-item screening tool was developed by Goodman et al. to evaluate the behaviors and adjustment of youth from the perspective of a parent or other informant (α = 0.83, total difficulties) [23]. Items assess emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems and prosocial behaviors. Maternal caregivers were asked to rate the behaviors and adjustment of their youth using a 3-pt rating response scale (1- “not true,” 2- “somewhat true,” and 3- “certainly true”). The youth adjustment variable was operationalized in the study as the total difficulties score on the SDQ.
Analysis
Regression analyses were performed to examine the associations between maternal experiences of torture and war trauma, mental health distress and physical health problems with youth functioning. Mediation regression analysis as described by Hayes to investigate whether the impact of torture on youth adjustment was indirect, via its impact on maternal mental or physical health [25]. Following Hayes’ methodology, bootstrapping analysis was conducted using 5000 samples to determine the mediating indirect effect of mental health distress on the relationship between maternal torture experiences and youth adjustment with a 95% confidence interval. The thousands of iterations created an empirical representation of the sampling distribution and constructed a confidence interval to test the indirect effects at a range of percentiles within the bootstrap distribution [26]. Finally, moderated mediation regression analysis was performed to examine whether the physical health problems of maternal caregivers moderated the size of the indirect effect of mental health distress on the relationship between their torture and war trauma experiences and youth adjustment. This step was a conducted to follow up on whether the mental health distress endorsed by maternal caregivers indirectly influenced the impact of torture and war trauma experiences on their youth’s adjustment; and, to what extent this mechanism was stronger for participants who reported greater physical health problems. In the moderated mediation model, we included maternal torture experiences, mental health distress, physical health problems and youth adjustment variables, and estimated the parameters through three hierarchical linear regressions [25, 26]. R version 3.6.1 [27], SPSS 26.0 [28] and Process Macro for SPSS Version 3 [25] statistical software packages were utilized to conduct analyses.
Results
Participants were 96 Karen refugee maternal caregivers from Burma resettled in the United States with primary caregiving responsibilities. Nearly all women participants reported being married or remarried (92.7%). Participants reported trauma from torture (primary torture 26%; secondary torture 26%) or war trauma alone (47.9%). Participants spent an average of 23.4 (SD=10.73) years living in a refugee camp, and 5.12 (SD=4.28) years post-resettlement in the United States. Mean scores and standard deviations for scales assessing mental health distress, physical health, experiences of war trauma and torture, and youth adjustment are reported in Table 1.
Table 1.
Means (M), Standard Deviations (SD) and Frequencies (%) for torture and war trauma experiences, mental health distress, physical health problems, and youth adjustment reported by maternal caregivers (n=96).
| Variables | % | M | SD |
|---|---|---|---|
| Maternal Age | 45.16 | 7.34 | |
| Maternal Marital Status (%) | |||
| Married/Remarried | 89 (92.7%) | ||
| Divorced/Separated | 4 (4.2%) | ||
| Widowed | 3 (3.1%) | ||
| Maternal Employment status (%) | |||
| Employed | 35 (36.5%) | ||
| Unemployed | 32 (33.3%) | ||
| Disabled | 29 (30.2%) | ||
| Time spent in camps in Thailand | 23.45 | 10.73 | |
| Time spent in resettlement in U.S. | 5.12 | 4.28 | |
| Torture (%) | |||
| Primary | 25 (26.0%) | ||
| Secondary | 25 (26.0%) | ||
| War trauma | 46 (47.9%) | ||
| Mental Health Distress | 4.34 | 3.16 | |
| Screened Positive (%) | 51 (53.1%) | ||
| Screened Negative (%) | 45 (46.9%) | ||
| Physical Health Problems Overall (%) | 70 (72.9%) | ||
| Physical Pain | 53 (55.2%) | ||
| Hypertension | 39 (40.61%) | ||
| Headaches | 34 (35.41%) | ||
| Gastrointestinal Issues | 25 (26.04%) | ||
| Dizziness | 23 (23.96%) | ||
| Youth adjustment | |||
| Emotional | 3.30 | 2.49 | |
| Conduct | .86 | 1.04 | |
| Hyperactivity | 1.63 | 1.79 | |
| Peer | 1.05 | 1.20 | |
| Prosocial | 9.54 | 1.01 | |
| Total SDQ | 6.85 | 3.97 | |
| Youth Age | 16.23 | 4.18 | |
| Youth Gender | |||
| Women | 41 (56.94%) | ||
| Men | 31 (43.06%) | ||
| Youth Country of Birth | |||
| Thailand Border Camps | 59 (81.9%) | ||
| Burma/Myanmar | 13 (18.1%) |
Pearson correlations indicated maternal experiences of war trauma and torture were significantly correlated with all explanatory variables with the size of the correlations ranging from moderate to large (Table 2).
Table 2.
Pearson correlations between maternal torture, mental health, physical health and youth adjustment variables
| Variable | 1 | 2 | 3 |
|---|---|---|---|
| Torture experiences | |||
| Mental health distress | .67** | ||
| Physical health problems | .62*** | .51*** | |
| Youth adjustment | −.39* | −.44** | −.49** |
Correlation is significant at the 0.05 level (2-tailed).
Correlation is significant at the 0.01 level (2-tailed).
Correlation is significant at the 0.001 level (2-tailed).
In addition, these variables were related to one another suggesting a complex set of inter-relationships. The results presented in Table 2 confirm the following conditions for testing mediation [28].
Maternal torture experiences were correlated with the primary outcome variable of youth adjustment
Maternal torture experiences were correlated with maternal mental health and physical health variables
Proposed mediator variable of maternal mental health distress was correlated with outcome variable of youth adjustment
The results of the mediation analysis are shown in Figure 1a.
Figure 1a.
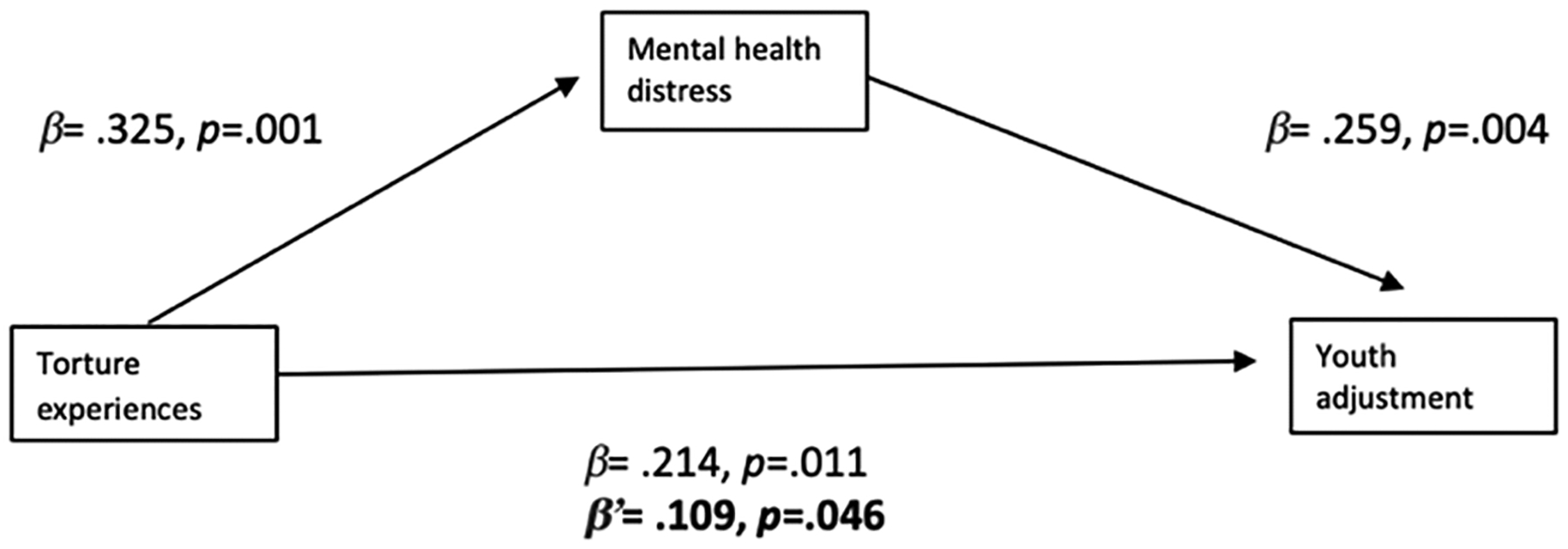
Mediation model indicating the relationship between torture experiences and youth adjustment is partially dependent on mental health distress reported by the maternal caregiver.
Maternal torture experiences were significantly and positively related to mental health distress, and mental health distress was significantly and negatively associated with youth adjustment. When statistically controlling for mental health distress, the type of torture and war trauma experiences were not significantly associated with youth adjustment. This result indicated the direct effect of torture experiences on youth adjustment disappeared without mental health distress. The bootstrap confidence interval displayed in Table 3 confirmed the indirect effect of torture and war trauma experiences on youth adjustment was dependent on mental health distress reported by maternal caregiver with R2 =.357 or 35.7% of variance explained. Thus, the relationship between torture experiences and youth adjustment was found to be statistically significant.
Table 3.
Bootstrap results for the indirect effect
| Mediator | Effect | R2 | SE | LL 95% CI | UL 95% |
|---|---|---|---|---|---|
| Mental health distress | 2.792 | .357 | .520 | 1.851 | 3.764 |
Notes. SE = standard error; LL95%CI= lower level of 95% confidence interval; UL95%CI= upper level of the 95% confidence interval
Presented in Table 4 are the results of the moderated mediation analysis treating mental health distress as the mediator when the physical health problems variable was used as the moderator in the relationship between maternal mental health distress and youth adjustment. Physical health problems was found to moderate the degree to which mental health distress mediated the relationship between torture and war trauma experiences and youth adjustment with R2= .409 or 40.9% of the variance explained.
Table 4.
Moderated mediation model for the relationship between maternal torture experiences and youth adjustment (outcome).
| (R* = .409) | B | SE | t | p |
|---|---|---|---|---|
| Torture experiences | 1.781 | .348 | 2.245 | .027 |
| Mental health distress | 2.206 | .578 | 4.816 | .001 |
| Physical health problems | 2.053 | .229 | 4.596 | .001 |
| Mental health distress x | ||||
| Physical health problems | 2.348 | .461 | 4.608 | .005 |
As shown in Figure 1b, the indirect mediation effect of maternal mental health distress on the relationship between torture experiences and youth adjustment was influenced by the level of physical health problems endorsed by participants. Results of the moderated mediation analysis suggested a conditional process by which the level of physical health problems reported by maternal caregivers explained the indirect mediation effect of mental health distress on the relationship between torture and war trauma experiences and youth adjustment.
Figure 1b.
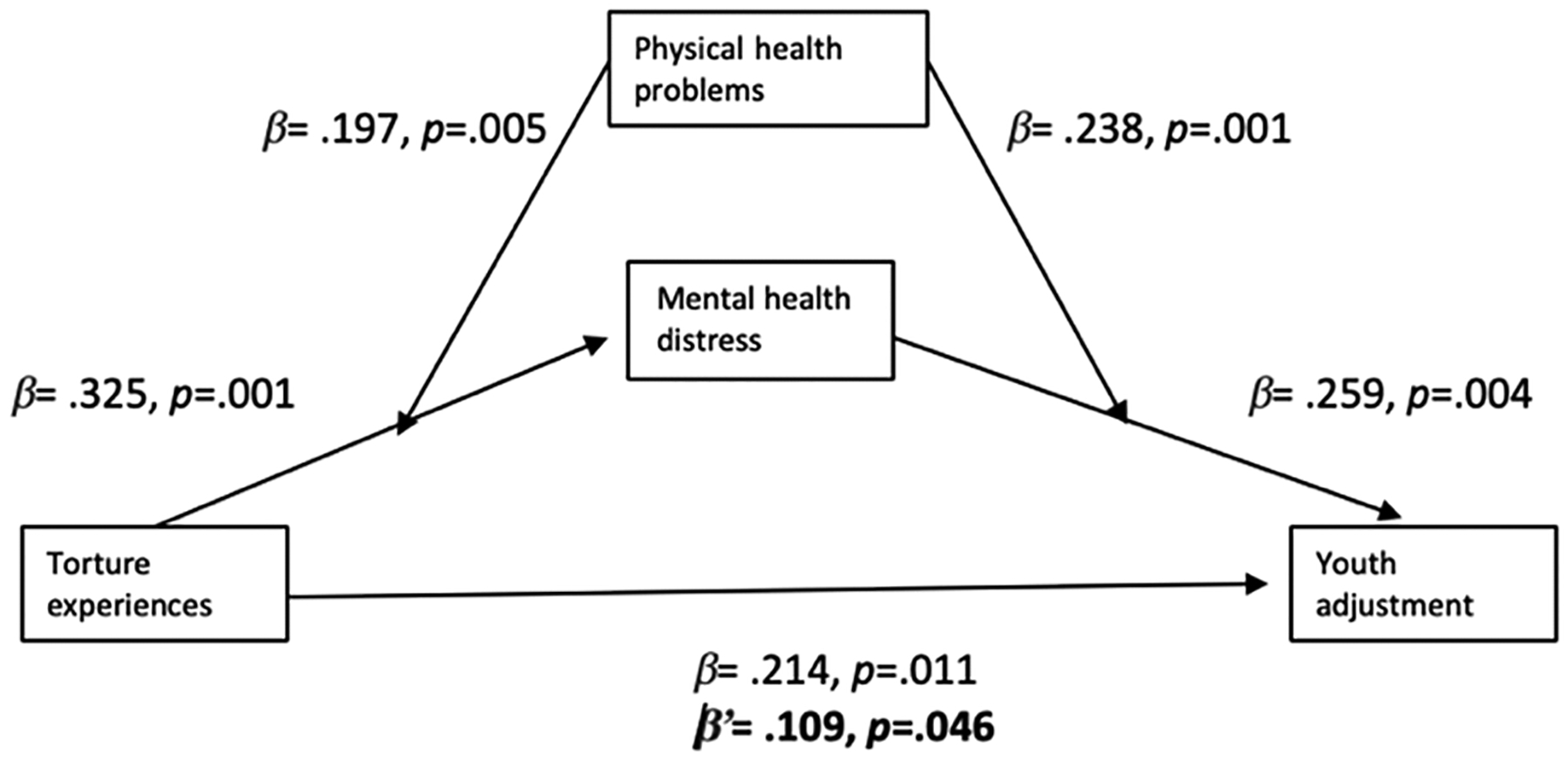
Moderated mediation model illustrating the effect of the mental health distress on the relationship between maternal torture experiences and youth adjustment varies based on the degree of physical health problems endorsed by the mother.
Note. Change in beta weight when the mediator is present is highlighted in bold.
Discussion
Results of the study suggested three key novel findings. First, we identified statistically significant and negative associations between maternal exposure to torture and youth adjustment. Maternal caregivers who endorsed torture reported poorer adjustment in their youth as compared to maternal caregivers who had experienced war trauma and not torture. Second, we identified mental health distress of maternal caregivers mediated the relationship of torture and war trauma experiences and youth adjustment. That is, the impact of torture and war trauma experiences on youth adjustment was influenced by the mental health distress reported by participants. Third, we discovered the mediating role of mental health distress on associations between maternal torture experiences and youth adjustment was dependent on how strongly mothers endorsed physical health problems. Mental health distress explained greater variation in the relationship between maternal torture and war trauma experiences and youth adjustment among mothers who reported greater physical health problems than mothers who reported lesser physical health problems.
We situate these findings within two dominant models relevant to the impact of trauma within families. First, behavioral and environmental models of intergenerational trauma propose that the disruption of the maternal child relationship – whether through attachment, engagement, affection, or other factors can perpetuate the negative experiences of trauma longitudinally and across generations. Our findings are consistent with literature associating maternal trauma and resulting mental health distress with the impaired psychosocial functioning and adjustment of youth [7, 9, 11, 13, 14]. Shaped through behavioral, interpersonal, and environmental contexts, younger persons adapt responses (modeled or learned) to the effects of trauma experienced by the parent. For example, documented emotional separation and attachment behaviors observed among offspring of holocaust survivors, particularly in the context of additional stressors [29–31] or the mirroring of emotion regulation observed between refugee youth and their caregivers [32, 33].
A second interpretation of the relationship between maternal torture, youth adjustment, and the physical and mental health experiences that influence the strength of this relationship derives from models of caregiver stress. Migrant and refugee youth may serve as cultural and linguistic brokers for their parents in post-migration contexts given their more efficient language acquisition and integration [34–37]. We question whether this relationship extends into a caregiving role as youth support parents in the navigation of the health system in spaces of resettlement.
As parental (in our findings, specifically maternal) mental health and physical health deteriorate, the frequency and amount to which youth are involved in these caregiving relationships may intensify. This is complicated by the fact that youth may have a vague or incomplete understanding of the circumstances of torture and trauma leading to the impaired mental and physical health states of their parents. Our findings suggested the physical and emotional proximity necessitated in a maternal caregiver role position youth much more intimately within her response to trauma.
Our study adds to the existing literature in two critical ways. First, the study team located no prior studies that identified key relationships between mental health, physical health and youth adjustment for resettled refugee women and families who have experienced trauma across generations in the context of torture and war. Second, existing models of intergenerational trauma explain the impact of maternal trauma experiences on youth as linear. Based on our findings, we identified a more complex pathway where torture and war trauma of a maternal caregiver affects her children, and the effect of trauma resulting from torture and war experiences is influenced by the extent of the physical health problems of the mother and her severity of mental health distress.
Although results provided important insight into factors that regulate the effects of trauma across generations, there are several limitations to the study. The data are cross sectional which limited our interpretation of the direction of associations and perspective on the more dynamic relationships within a family. All data were self-reported by maternal caregiver report, thus introducing a high likelihood of common method variance (CMV) and a false internal consistency [38]. In the context of our study, the circumstance of CMV results from women who have experienced trauma resulting from torture and/or war who may consistently over or under rate the adjustment of their own children and/or family functioning. Therefore, social desirability as well as the accuracy of recall in light of the effects of trauma on memory are important considerations. While these limitations must be considered in the interpretation of results, there were many key points of convergence between our findings and those reported by others conducting related investigations. Additionally, in subsequent phases of the study on which this report is based, we integrated paternal caregiver and youth perspectives on family functioning and youth adjustment to mitigate this source of bias. Finally, a Karen interpreter facilitated all study interactions. It is possible that cultural and linguistic nuances and meaning were lost through the Karen to English language interpretation of participant responses.
The current study is significant in that it enhances our mechanistic understanding of factors relevant to the intergenerational effects of trauma within families where maternal caregivers experienced trauma from torture and/or war. Future research integrating the perspectives of paternal caregivers and youth is important to allow for direct within-family comparisons and result in a deeper understanding of patterns of intergenerational trauma. Additional studies must examine the impact of family-centered interventions to address the effects of intergenerational trauma on the well-being and adjustment of refugee mothers and youth across diverse migrant/refugee samples.
Acknowledgements
We acknowledge the essential contributions in early project phases by the Center for Victims of Torture, headquartered in St. Paul, Minnesota. Specifically, we thank the Director of Research, Craig Higson Smith for his guidance and expertise. We thank the Karen Organization of Minnesota for key project support. We attribute the depth and richness of the data, in part, to our interpreter, Ehtaguy Zar.
Research reported in this publication was supported by the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award Number K12HD055887. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
All authors have no conflict of interest to report. We acknowledge the essential contributions in early project phases by the Center for Victims of Torture, headquartered in St. Paul, Minnesota. Specifically, we thank the Director of Research, Craig Higson Smith for his guidance and expertise. We thank the Karen Organization of Minnesota for key project support. We attribute the depth and richness of the data, in part, to our interpreter, Ehtaguy Zar.
Contributor Information
Sarah J. Hoffman, University of Minnesota School of Nursing
Maria M. Vukovich, University of Denver Graduate School of Professional Psychology, International Disaster Psychology Program
Abigail H. Gewirtz, University of Minnesota Department of Family Social Sciences
Jayne A. Fulkerson, University of Minnesota School of Nursing
Cheryl L. Robertson, University of Minnesota School of Nursing
Joseph E. Gaugler, University of Minnesota School of Public Health
References
- 1.United Nations General Assembly. Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment. 1984. https://www.ohchr.org/en/professionalinterest/pages/cat.aspx. Accessed 26 Dec 2019.
- 2.Higson-Smith C. Updating the estimate of refugees resettled in the United States who have suffered torture. Center for Victims of Torture. 2015. https://www.cvt.org/sites/default/files/SurvivorNumberMetaAnalysis_Sept2015_0.pdf. Accessed 26 Dec 2019. [Google Scholar]
- 3.Shishehgar S, Gholizadeh L, DiGiacomo M, Green A. Davidson PM. Health and socio-cultural experiences of refugee women: An integrative review. J Immigr Minor Health. 2016. pp 1–15 [DOI] [PubMed] [Google Scholar]
- 4.Sidebotham E, Moffatt J, Jones K. Sexual violence in conflict: a global epidemic. Obstet Gynaecol. 2016;18(4):247–50. [Google Scholar]
- 5.Sangalang CC, Vang C. Intergenerational trauma in refugee families: a systematic review. J Immigr Minor Health. 2017;19(3):745–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wieling E. Family interventions for populations exposed to traumatic stress related to war and violence. J Marital Fam Ther. 2018;44(2):189–92. [DOI] [PubMed] [Google Scholar]
- 7.Daud A, Skoglund E, Rydelius PA. Children in families of torture victims: Transgenerational transmission of parents’ traumatic experiences to their children. Int J Soc Welf. 2005;14(1):23–322. [Google Scholar]
- 8.Dalgaard NT, Todd BK, Daniel SI, Montgomery E. The transmission of trauma in refugee families: associations between intra-family trauma communication style, children’s attachment security and psychosocial adjustment. Attach Hum Dev. 2016;18(1):69–89. [DOI] [PubMed] [Google Scholar]
- 9.Daud A, af Klinteberg B, Rydelius PA. Resilience and vulnerability among refugee children of traumatized and non-traumatized parents. Child Adolesc Psychiatry Mental Health. 2008;2(1):7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Montgomery E. Tortured families: a coordinated management of meaning analysis. Fam Process. 2004;43(3):349–71. [DOI] [PubMed] [Google Scholar]
- 11.Sangalang CC, Jager J, Harachi TW. Effects of maternal traumatic distress on family functioning and child mental health: an examination of Southeast Asian refugee families in the US. Soc Sci Med. 2017;184:178–86. [DOI] [PubMed] [Google Scholar]
- 12.Van Ee E, Kleber RJ, Mooren T. War trauma lingers on: Associations between maternal posttraumatic stress disorder, parent–child interaction, and child development. Infant Ment Health J. 2012;33(5):459–68. [DOI] [PubMed] [Google Scholar]
- 13.Burchert S, Stammel N, Knaevelsrud C. Transgenerational trauma in a post-conflict setting: Effects on offspring PTSS/PTSD and offspring vulnerability in Cambodian families. Psychiatry Res. 2017;254:151–7. [DOI] [PubMed] [Google Scholar]
- 14.East PL, Gahagan S, Al-Delaimy WK. The impact of refugee mothers’ trauma, posttraumatic stress, and depression on their children’s adjustment. J Immigr Minor Health. 2018;20(2):271–82. [DOI] [PubMed] [Google Scholar]
- 15.United Nations General Assembly. Convention against Torture and Other Cruel, Inhuman or Degrading Treatment or Punishment. 1984. https://www.un.org/documents/ga/res/39/a39r046.htm
- 16.Office of Refugee Resettlement, Administration for Children and Families, & United States Department of Health and Human Services. 2010. Torture survivors program (TSP) eligibility determination guidance; https://www.acf.hhs.gov/sites/default/files/orr/eligibility_guidelines_orr_2010_1.pdf [Google Scholar]
- 17.American Psychiatric Association. Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author; 2000. [Google Scholar]
- 18.Karen History. (2019). Retrieved from https://www.mnkaren.org/about/.
- 19.Hoffman SJ, Robertson CL. A systematic review of Karen refugee health. Int J Migr Health Soc Care. 2016;12(1):1–15. [Google Scholar]
- 20.Shannon PJ, Vinson GA, Wieling E, Cook T, Letts J. Torture, war trauma, and mental health symptoms of newly arrived Karen refugees. J Loss Trauma. 2015;20(6):577–90. [Google Scholar]
- 21.Hoffman SJ, Robertson CL, Tierney JD. What about the next generation that’s coming? The recontextualization of mothering post-refugee resettlement. Adv Nurs Sci. 2017;40(2):122–53. [DOI] [PubMed] [Google Scholar]
- 22.Brink DR, Shannon PJ, Vinson GA. Validation of a brief mental health screener for Karen refugees in primary care. Fam Pract. 2015;33(1):107–11. [DOI] [PubMed] [Google Scholar]
- 23.Goodman R, Meltzer H, Bailey V. The Strengths and Difficulties Questionnaire: A pilot study on the validity of the self-report version. Eur Child Adolesc Psychiatry. 1998;7:125–30. [DOI] [PubMed] [Google Scholar]
- 24.Shannon PJ, Vinson GA, Wieling E, Cook T, Letts J. Torture, war trauma, and mental health symptoms of newly arrived Karen refugees. Journal of Loss and Trauma. 2015;20(6):577–90. [Google Scholar]
- 25.Hayes AF: Introduction to mediation, moderation and conditional process analysis: A regression based approach (2 ed). 2018. https://processmacro.org/download.html. Accessed 26 Dec 2019
- 26.Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behav Res Ther. 2017;98:39–57. [DOI] [PubMed] [Google Scholar]
- 27.R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2019. https://www.R-project.org/. Accessed 26 Dec 2019. [Google Scholar]
- 28.IBM Corp. IBM SPSS Statistics for Windows, Version 26.0 Armonk, NY: IBM Corp; 2019. [Google Scholar]
- 29.Fossion P, Leys C, Vandeleur C, Kempenaers C, Braun S, Ver-banck P, Linkowski P. Transgenerational transmission of trauma in families of Holocaust survivors: the consequences of extreme family functioning on resilience, sense of coherence, anxiety and depression. J Affect Disord. 2015;171:48–53. [DOI] [PubMed] [Google Scholar]
- 30.Danieli Y, Norris FH, Engdahl B. A question of who, not if: psychological disorders in Holocaust survivors’ children. Psychol Trauma. 2017;9(S1):98. [DOI] [PubMed] [Google Scholar]
- 31.Shmotkin D, Shrira A, Goldberg SC, Palgi Y. Resilience and vulnerability among aging Holocaust survivors and their families: an intergenerational overview. J Intergener Relatsh. 2011;9(1):7–21. [Google Scholar]
- 32.Stauffer S. Trauma and disorganized attachment in refugee children: integrating theories and exploring treatment options. Refugee Surv Q. 2008;27(4):150–63. [Google Scholar]
- 33.Bek-Pedersen K, Montgomery E. Narratives of the past and pre-sent: young refugees’ construction of a family identity in exile. J Refug Stud. 2006;19(1):94–112. [Google Scholar]
- 34.Lazarevic V. Effects of cultural brokering on individual wellbeing and family dynamics among immigrant youth. J Adolesc. 2017;55:77–87. [DOI] [PubMed] [Google Scholar]
- 35.Bauer E. Practicing kinship care: children as language brokers in migrant families. Childhood. 2016;23(1):22–36. [Google Scholar]
- 36.Pina LR, Gonzalez C, Nieto C, Roldan W, Onofre E, Yip JC. How Latino children in the us engage in collaborative online information problem solving with their families. Proc ACM Human-Comp Interaction. 2018;2(CSCW):140. [Google Scholar]
- 37.Chao X. ‘What defines me is what I have been through’: Bhutanese refugee youth identity in the United States. Br J Sociol Educ. 2019; p. 1–17. [Google Scholar]
- 38.Morales A, Wang KT. The relationship among language brokering, parent–child bonding, and mental health correlates among Latinx college students. J Ment Health Couns. 2018;40(4):316–32736. [Google Scholar]


