Abstract
Objective
To determine if an Emergency Department-initiated fall prevention intervention can reduce subsequent fall-related and all-cause ED visits and hospitalizations in older adults.
Methods
The Geriatric Acute and Post-acute Fall Prevention (GAPcare) intervention was a randomized controlled trial conducted from January 2018 to October 2019. Participants at two urban academic EDs were randomly assigned (1:1) to an intervention or usual care arm. Intervention participants received a brief tailored, structured pharmacy and physical therapy (PT) consultation in the ED with automated communication of their recommendations to participants’ primary care physicians.
Results
Of 284 study eligible participants, 110 non-institutionalized older adults (≥65 years old) with a recent fall consented to participate; median age was 81 years old, 67% were female, 94% were white, and 16.3% had cognitive impairment. As compared to usual care participants (n=55), intervention participants (n=55) were half as likely to experience a subsequent ED visit (adjusted incidence rate ratio (aIRR): 0.47 (0.29–0.74)) and one third as likely to have fall-related ED visits (aIRR 0.34 (0.15–0.76)) within six months. Intervention participants experienced half the rate of all hospitalizations (aIRR 0.57 (0.31–1.04), but confidence intervals were wide. There was no difference in fall-related hospitalizations between groups (aIRR 0.99 (0.31–3.27). Self-reported adherence to pharmacy and PT recommendations was moderate; 73% of pharmacy recommendations were adhered to and 68% of PT recommendations were followed.
Conclusions
GAPcare, a post-fall, in-ED multidisciplinary intervention with pharmacists and PTs reduced six-month ED encounters in 2 urban EDs. The GAPcare intervention could provide a model of care to other healthcare systems aiming to reduce costly and burdensome fall-related events in older adults.
Trial Registration:
ClinicalTrials.gov; NCT03360305; https://www.clinicaltrials.gov/ct2/show/NCT03360305
Keywords: Falls, geriatrics, geriatrics, emergency department, physical therapy, pharmacist
INTRODUCTION
Background
The mortality for falls in older adults, aged 65 and older, is increasing1 in the Unites States (US). Geriatric falls come at a considerable cost to individuals and payors; they lead to 3 million annual US Emergency Department (ED) visits,2 are a leading cause of institutionalization and functional decline,3 and contribute an estimated $50 billion4 in US medical costs each year. Falling once doubles the chance of falling again,5 making older adults who present for falls to the ED a high-risk group for intervention.6,7 Although multidisciplinary interventions drawing on professionals like pharmacists and PTs have shown promise in other countries, US ED fall prevention interventions have not been rigorously tested.7,8
Importance
We recently reported the short-term results of a randomized, controlled trial, GAPcare (the Geriatric Acute and Post-Acute Fall Prevention Intervention), that determined a brief tailored, structured pharmacy and physical therapy (PT) consultation is feasible in the ED – as it does not prolong ED length of stay and pharmacy and PT assessments are completed in twenty minutes, on average.9 Additionally, we established acceptability of GAPcare through in-depth interviews and surveys with patients, caregivers, and clinicians.9–11 Geriatric emergency medicine guidelines suggest that a multidisciplinary teams composed of pharmacists and PTs could aid emergency physicians with fall assessments.12,13 Pharmacist-led interventions which use motivational interviewing techniques to modify behavior surrounding medication use (Medication Therapy Management (MTM)) have been shown to be_useful in reducing fall risk-increasing medication;14,15 and adverse drug event related healthcare visits.16,17 Additionally, PT services in the ED for a ground-level fall was associated with a significantly lower likelihood of a fall-related ED revisit within 30 days (odds ratio (OR)=0.655, p<.001) and 60 days (OR=0.684, p<.001).18
Goals of This Investigation
Some EDs currently consult these professionals, in particular as part of ED observation care, but this care is clinician-prompted and therefore subject to unmeasured clinician-, patient-, and facility-level factors, which makes outcome attribution and measurement challenging.19 GAPcare, as a randomized controlled trial, could provide a solution to this problem. The aim of this investigation was to determine whether GAPcare could reduce subsequent fall-related and all-cause ED visits and hospitalizations.
METHODS
Intervention setting
We conducted a randomized controlled trial of the GAPcare intervention at two urban academic EDs in Providence, Rhode Island: The Miriam Hospital and Rhode Island Hospital. The Miriam Hospital is an academic community hospital with 82,000 adult ED patient visits per year. The Rhode Island Hospital ED is the only level I trauma and tertiary referral center in the state and has an annual volume of 100,000 adult ED patient visits.
Sample and recruitment
ED patients 65 years old and older were eligible to participate if they presented to the ED within 7 days of a fall, could communicate in English or Spanish, and the ED clinician planned to discharge them from the ED (i.e., not admit to the hospital). Individuals with altered mental status (e.g., intoxicated), who were homeless, or could not provide a phone number for follow-up were excluded. Because skilled nursing facility (SNF) patients already have access to PT and fall prevention strategies differ in facilities (e.g. home safety evaluations not relevant), we excluded SNF patients.
Research staff reviewed the electronic health record (EHR) of potentially study eligible ED patients when pharmacy and PT were available for consultation (7AM to 4PM Monday – Friday). Research staff approached all patients 65 years old and older who presented from the community or an assisted living facility and whose EHR did not indicate that any exclusion criteria were present. Patients were asked if they experienced a “slip, trip, or fall” in the past week. If meeting this criterion, the research staff assessed their study eligibility and determined if the ED clinicians planned to discharge them. For patients interested in participating in the study who scored less than four on the Six-Item Screener20 (signifying high likelihood of cognitive impairment), their legally authorized representatives were asked to provide written consent.
After consent, at each study site the research staff used REDCap21 to randomly assign participants to the usual care or the intervention arm (1:1 allocation) with block sizes of six and four, stratified by hospital. We performed block randomization in order to balance randomization between hospital sites, as one is a trauma center and the other lacks trauma designation. Randomization tables were generated in SAS 9.4 and uploaded to REDCap21; study arm assignment for each participant was only available to research assistants after completion of the consent process. The hospital institutional review board (IRB) approved this study. ClinicalTrials.gov identifier: NCT03360305.
The GAPcare intervention
Participants first were assessed by an ED clinician who directed their medical care. For patients randomly assigned to the intervention arm, the research staff initiated a pharmacist and PT consult, who evaluated participants consecutively at their bedside. Our previously published protocol provides more details about the intervention.22 The pharmacist and PT documented their encounter using a structured note9 that was integrated into the EHR to enhance information sharing with other hospital-based and outpatient clinicians. Study instruments and the time of assessment are included in the supplement (Supplementary Table 1).
Pharmacy consultation
Pharmacists performed a bedside evaluation after reviewing a list of recently dispensed medication for each participant in the EHR. During a brief MTM session, pharmacists used motivational interviewing to ask open-ended questions to determine patients’ knowledge of their medications and willingness to change medications to reduce fall risk. The pharmacists identified one to three medications that could be stopped or modified to reduce fall risk and communicated the medication-related action plan in writing to participants and the ED treatment team. The medication-related action plan was automatically faxed to each participants’ primary care physician (PCP) at the end of the ED visit. The medication-related action plan specified that medication changes were at the discretion of the PCP and were not necessarily enacted by the ED clinician.
PT-led fall risk assessment and plan
After diagnostic imaging was reviewed and the ED clinician determined it was safe for the participant, the PT performed a bedside evaluation. PTs performed a gait, balance, and lower extremity strength assessment using common fall risk instruments (the Timed Up and Go23, AM-PAC “6 clicks”24, Tinetti25, Five Times Sit-to-Stand26). Although many measures of function are available, we chose these assessments because they have been validated for fall prediction (see Supplementary Table 1), local PTs already employ them for hospitalized patients, they are integrated into our EHR, and they were recommended by our geriatric-trained PT. They also provided PT-related discharge planning, and recommended a PT action plan, which was individually tailored to the patient’s needs. For instance, patients without significant impairment in balance and strength were referred to a community fall prevention programs, whereas others were advised to receive outpatient, home PT, occupational therapy, a home-safety evaluation, or if necessary, to be directly admitted to a SNF. The PT action plan was communicated in writing to the patient and ED clinician and faxed together with the medication-related action plan to PCPs.
Usual care arm
Participants randomly assigned to the usual care arm received medical care as guided by the ED clinician and a “Check for Safety” brochure by the Centers for Disease Control and Prevention (CDC),27 which contains a checklist of home safety measures to prevent falls. The ED clinician could choose to contact the PCP, consult case management, and provide medical equipment (e.g. walkers, canes) for participants in both arms, but in-ED pharmacy and PT consults were not available to usual care participants.
Evaluation
Participant-reported outcomes
Participants were telephoned at one, three, and six months and asked to complete surveys detailing their falls and healthcare visits. At six months after the ED visit, participants were interviewed in their home to obtain their self-reported adherence to pharmacy and PT recommendations, review their current medication lists, and inquire about self-reported fall occurrence and healthcare visits.
EHR data extracted outcomes
To increase data collection accuracy, we followed recommendations28 for manual EHR review and data extraction, including creating and using a standardized data extraction form, implementing a standardized protocol for manual data extraction, training the data extractors, blinding data extractors to the study arm, and conducting quality assurance by reviewing a 10% sample of the data collected. We also searched obituaries and called PCPs for information on all patients missing follow-up. When participant-report and EHR extracted data differed, two study authors (SM, EG) reviewed both records and reconciled them. If reconciliation using existing records was not possible or data relevant to the study outcomes was missing, the lead investigator (EG) called the patient, family, primary care physician, or the medical examiner to obtain additional information.
Sample size considerations
A meta-analysis of fall prevention programs found a 30% reduction in the incidence rate of falls.29 In a prior study, 31% of older patients presenting to the ED after a fall had a subsequent fall within six months.26,30 Using these findings, we planned to recruit n=120 participants with n=60 in each arm. With this sample size, we could detect at least an 25% absolute reduction in subsequent falls occurring within six months with 80% power α=0.05 (31% in usual care vs. 6% intervention arm).
Statistical analysis
Outcomes were analyzed according to an intention-to-treat principle with all participants analyzed in the arm to which they were randomized. If disposition was changed after randomization from ED discharge to hospital admission, participants were still analyzed according to the group they were assigned. Because each participant could contribute a different amount of follow-up time (e.g. due to death), we calculated person-month rates for our measured outcomes of fall-related ED visits, all ED visits, fall-related hospitalizations (excluding procedures and other planned surgeries) and hospitalizations. Finally, we used a negative binomial regression model to compare fall event rates between the two arms and conducted sensitivity analyses with Anderson Gill Models. Negative binomial regression with robust standard errors and Anderson Gill models are preferable for fall-related event analyses since they allow for variable follow up time and consideration of multiple recurrent events.31,32 In addition, they allow for investigation of the intervention effect and the effects of confounding variables; in all models, we excluded periods of hospitalization from time at risk.
We chose a negative binomial model over a Poisson model due to over-dispersion present in our data. We also fit zero-inflated models, but they did not improve model fit. We calculated the number-needed-to-treat using the Nelson-Aalen estimator to estimate the cumulative number of expected events.33 We developed mean cumulative function graphs for all and fall-related ED visits to show the mean number of events over time and illustrate when during follow-up the intervention was helpful. Finally, we report adherence to our pharmacy and PT recommendations (as measured during the six-month follow-up assessment) to illustrate uptake of recommendations by participants. Analyses were completed using SAS 9.4.
We adjusted for gender, age, number of falls in the three months prior to the ED visit, comorbidities (Charlson Comorbidity Index), baseline function (activities of daily living (ADLs)), injury severity, and hospital site (trauma vs. non-trauma center). These factors were identified a priori before conducting analyses. We also included several variables in our model that we thought were srelevant to reduced falls and healthcare utilization based on our clinical expertise and prior falls research, particularly by Close et al. in their landmark clinical trial on falls.34 Specifically, Close et al. included baseline function (Barthel activity of daily living scores) and prior falls. We also know that unintentional falls increase with age (Ashmann et al.35). In addition to age, function, and prior falls, we adjusted for gender, comorbidities (Charlson Comorbidity Index), injury severity, prior assistive equipment use, number of prior falls in the prior three months and hospital site (trauma vs. non-trauma center). Because women have a higher life expectancy than men, they fall more often. The Charlson Comorbidity Index is a frequently used variable in geriatric health services research because it is predictive of mortality in this population, as well as healthcare utilization. We hypothesized that people with more injurious falls, prior falls and existing assistive equipment use would be more likely to suffer recurrent falls and healthcare utilization. Similarly, patients who experienced more severe injuries after a fall, are more likely to be transported by ambulance to a trauma center, so we included this as both a blocking factor and a covariate.
RESULTS
Characteristics of study subjects
Of 478 ED patients assessed for study eligibility from January 25, 2018 to March 31, 2019, 284 were eligible for inclusion, and 110 consented to participate (Figure 1). The main reasons for ineligibility were that the ED clinician originally planned to admit the patient to the hospital, the patient resided in a SNF, or the patient had an altered mental status. The primary reasons patients cited for declining to participate were a belief that falls were not a problem for them and because family members were present in the ED.
Figure 1.
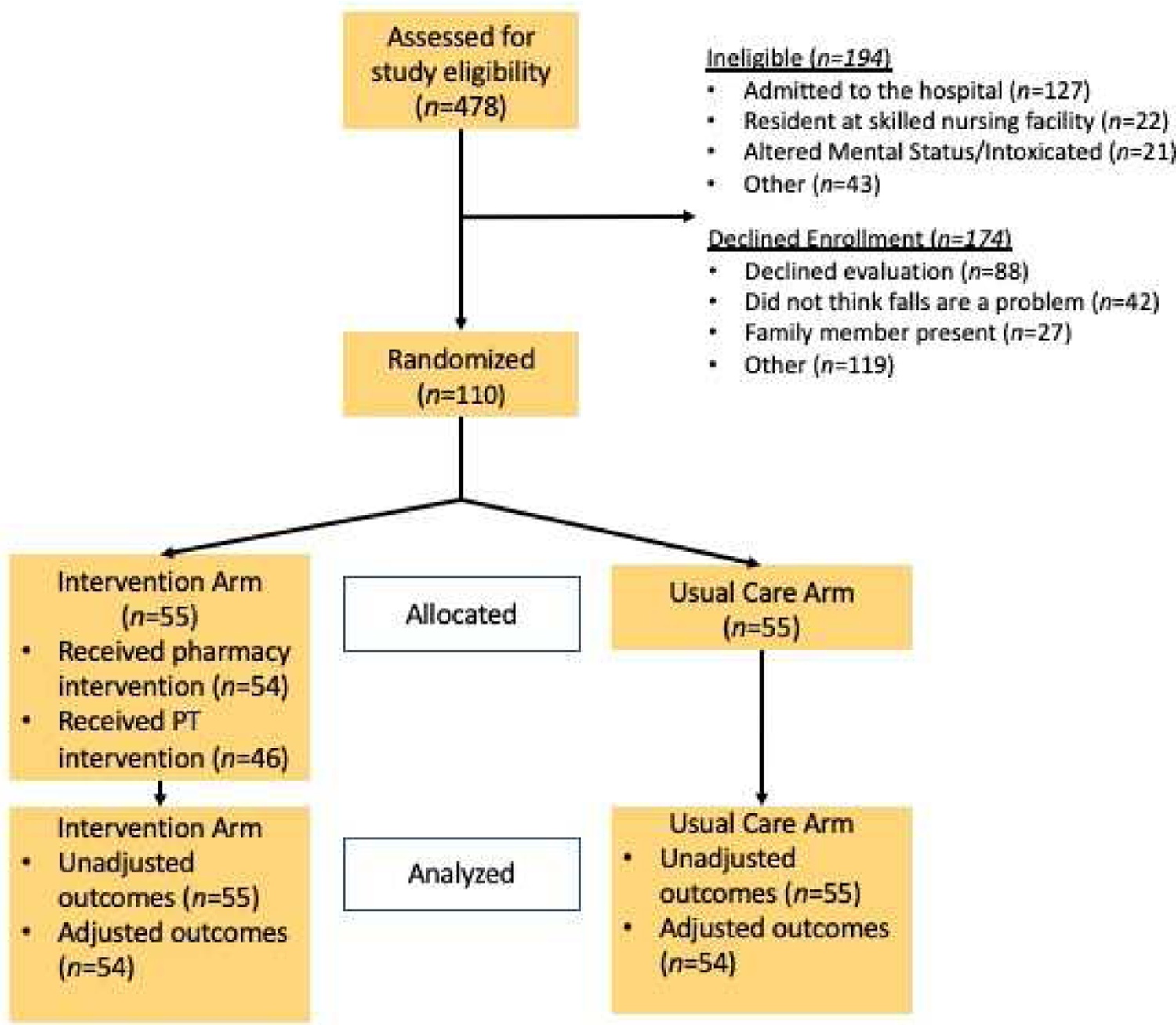
CONSORT Flow Diagram of Trial Participants
We enrolled 110 participants in GAPcare. Although we initially intended to recruit 120 participants, the study was closed early to recruitment per the advice by the study’s Data Safety Monitoring Board, which believed that feasibility and initial efficacy was sufficiently established. Of the 55 participants in the intervention arm, 54 received the pharmacy intervention and 46 completed the PT intervention. PT did not complete an evaluation on every intervention participant for several reasons; newly diagnosed spine fracture, intracranial hemorrhage, desire to leave the ED prior to PT arrival, and deferral request by orthopedic surgery or PT. No participants experienced any adverse events as a result of participating in the intervention. Median time from consult request to arrival was 14 minutes (IQR 10, 20) for pharmacy and 22 minutes (IQR 14, 34) for PT. Median duration of consult was 20 minutes for pharmacy (IQR 13, 24) and 20 minutes for PT (IQR 14, 29). ED length of stay was not increased in the intervention arm: usual care 5.3 hours vs. intervention 5.0 hours (p<0.94). Additional feasibility outcomes are reported in our prior GAPcare manuscript.9
Of the 110 participants, most were female (67%), white (96%), with a median age of 81 years old (Table 1). There were no statistically significant differences (p<0.05) in gender, race, age, presence of cognitive impairment and major comorbidities between arms. After the index ED visit, 39 (70.9%) of control and 35 (63.6%) of intervention participants were discharged home (p=0.58) (Table 2).9 Of the remaining participants, 6 (10.9%) control and 10 (18.8%) intervention participants went to SNF. In both the control and intervention arm, 10 (18.8%) participants per arm were admitted.
Table 1.
Participant Characteristics by Study Arm
| Characteristic | Study arm | |||
|---|---|---|---|---|
| Usual care (n=55) | Intervention (n=55) | |||
| N | (%) | N | (%) | |
| Gender | ||||
| Female | 37 | 67 | 37 | 67 |
| Male | 18 | 33 | 18 | 33 |
| Ethnicity1 | ||||
| Hispanic/Latino | 2 | 4 | 0 | 0 |
| non-Hispanic/non-Latino | 53 | 96 | 54 | 100 |
| Race | ||||
| White | 54 | 98 | 51 | 93 |
| Black | 0 | 0 | 2 | 4 |
| American Indian/Alaskan Native | 0 | 0 | 1 | 2 |
| White and Asian | 0 | 0 | 1 | 2 |
| Other | 1 | 2 | 0 | 0 |
| Age (mean (SD)) | 80.1 | 8.5 | 81.9 | 8.3 |
| Education level2 | ||||
| Grades 1 through 8 (Elementary/middle school) | 3 | 6 | 4 | 8 |
| Grades 9 through 11 (Some high school) | 7 | 14 | 4 | 8 |
| Grades 12 or GED (High school graduate) | 21 | 41 | 18 | 36 |
| College 1 year to 3 years (Some college or technical school) | 9 | 18 | 8 | 16 |
| College 4 years or more (College graduate) | 11 | 22 | 16 | 32 |
| Cognitive impairment (Six item screener score)3 | ||||
| 3 or less | 8 | 15 | 10 | 20 |
| 4 | 13 | 24 | 2 | 4 |
| 5 | 17 | 31 | 20 | 39 |
| 6 | 17 | 31 | 22 | 43 |
| Number of falls in previous 3 months4 | ||||
| 0 | 25 | 45 | 29 | 57 |
| 1 | 10 | 18 | 10 | 20 |
| 2 | 10 | 18 | 5 | 10 |
| 3 | 4 | 7 | 5 | 10 |
| 4 | 1 | 2 | 2 | 4 |
| 5 or more falls | 5 | 9 | 3 | 6 |
| Number of injurious falls in previous 3 months5 | ||||
| No falls | 25 | 45 | 29 | 57 |
| No injurious falls | 16 | 29 | 15 | 29 |
| 1 | 8 | 15 | 9 | 17 |
| 2 | 4 | 7 | 1 | 2 |
| 3 | 2 | 4 | 0 | 0 |
| Injured during current fall6 | ||||
| No | 11 | 20 | 12 | 22 |
| Yes | 44 | 80 | 42 | 78 |
| Current use of assistive device7 | ||||
| No | 15 | 27 | 14 | 26 |
| Yes | 40 | 73 | 40 | 74 |
| Life-limiting comorbidities (Charlson comorbidity index)8 | ||||
| 0 | 10 | 18 | 11 | 20 |
| 1 | 14 | 26 | 15 | 28 |
| 2 | 13 | 24 | 16 | 30 |
| 3 | 6 | 11 | 8 | 15 |
| 4 | 4 | 7 | 4 | 7 |
| 6 | 4 | 7 | 0 | 0 |
| 7 | 3 | 6 | 0 | 0 |
| Function (Activities of Daily Living (median (IQR) | 18 | 16–20 | 18 | 15–20 |
1 intervention arm participant selected did not know
Data for 4 usual care participant and 5 intervention arm participants
Data for 1 intervention arm participant missing
Data for 1 intervention arm participant missing
Data for 1 intervention arm participant missing
Data for 1 intervention arm participant missing
Data for 1 intervention arm participant missing
All items of the CCI were missing for 1intervnetion and 1 usual care participant; 13 participants (8 usual care, 5 intervention) were missing 1 CCI item and 4 participants (all intervention) were missing 2 items. Data from these individuals is shown.
Table 2.
Outcomes by Study Arm
| Usual Care (n=55) | Intervention (n=55) | |
|---|---|---|
| Initial disposition (n(%)) | ||
| Discharged to home | 39 (71%) | 35 (63%) |
| Discharged SNF | 6 (11%) | 10 (18%) |
| Admitted | 10 (18%) | 10 (18%) |
| Disposition at end of study9 | ||
| Home or short-term stay in SNF | 41 (75%) | 47 (85%) |
| Permanent move to SNF | 4 (7%) | 5 (9%) |
| Deceased/Hospice | 10 (18%) | 3 (5%) |
| Percentage of days spent by location | ||
| At home or short-term stay in SNF | 87.3% | 80.8% |
| Hospitalized | 2.3% | 1.6% |
| Permanent move to SNF | 7.0% | 7.6% |
| Deceased | 10.0% | 3.4% |
| Healthcare utilization outcomes by events | ||
| Total number of person-months | 297 | 319 |
| Fall-related ED visits | 24 | 9 |
| All ED visits | 66 | 30 |
| Fall-related hospitalizations | 6 | 7 |
| All hospitalizations | 34 | 19 |
| Health utilization outcomes by person (n(%)) | ||
| Participants with one or more fall-related ED visit(s) | 15 (27%) | 8 (15%) |
| Participants with one or more ED visit(s) | 29 (53%) | 20 (36%) |
| Participants with one or more fall-related hospitalization(s) | 6 (11%) | 6 (11%) |
| Participants with one or more hospitalization(s) | 21 (38%) | 13 (23%) |
Participants who moved permanently to SNF and then died or entered into hospice were counted in the “Deceased/Hospice” category
ED visits and hospitalizations during the six-month follow-up period
As seen in Table 2, intervention participants had less all-cause ED visits, fall-related ED visits, all-cause hospitalizations, and fall-related hospitalizations than the usual care arm. Twelve (11%) of the 110 study participants died or transitioned to hospice during follow-up, predominately from the usual care arm. Eight patients withdrew and eleven were lost to follow-up, but consented to continued EHR abstraction.
In the adjusted analyses, we found that participants in the intervention arm had half the rate of all-cause ED visits compared to the usual care arm (Table 3). Moreover, participants receiving the intervention had nearly one third the rate of fall-related ED visits per month. Intervention participants experienced half the rate of all hospitalizations, but confidence intervals were wide. There was no difference in fall-related hospitalizations between groups (Table 3 and Supplementary Table 2). The number needed to treat for the GAPcare intervention to prevent one ED visit in 6 person months was 2 (95% CI 1–7) and to prevent one fall-related ED visit was 4 (95% CI 2–24). We also conducted exploratory analyses on how participants’ permanent move to a SNF may have impacted our findings; we found no major differences in results when we removed time in a SNF from time at risk (Supplementary Table 3 and Supplementary Figure 1).
Table 3.
Unadjusted and Adjusted Healthcare Event Rates and Incident Rate Ratios from Negative Binomial Models
| Unadjusted Rate per 10 person-months (95% CI) | IRR (95% CI) | Adjusted Rate per 10 person-months* (95% CI) | IRR (95% CI) | |||
|---|---|---|---|---|---|---|
| Usual care (n=55) | Intervention (n=55) | Usual care (n=54) | Intervention (n=54) | |||
| Fall-related ED visits | 0.84 (0.56, 1.25) | 0.29 (0.15, 0.56) | 0.35 (0.16, 0.75) | 0.34 (0.12, 0.99) | 0.12 (0.04, 0.38) | 0.34 (0.15, 0.76) |
| All ED visits | 2.30 (1.81, 2.93,) | 0.97 (0.68, 1.38) | 0.42 (0.27, 0.65) | 1.54 (1.04, 2.30) | 0.73 (0.45, 1.17) | 0.47 (0.29, 0.74) |
| Fall-related hospitalizations | 0.24 (0.12, 0.51) | 0.19 (0.09, 0.32) | 0.79 (0.27, 2.36) | 0.22 (0.09, 0.56) | 0.22 (0.08, 0.52) | 0.99 (0.31, 3.27) |
| All hospitalizations | 1.19 (0.85, 1.66) | 0.61 (0.39, 0.96) | 0.52 (0.30, 0.91) | 0.77 (0.46, 1.31) | 0.44 (0.24, 0.82) | 0.57 (0.31, 1.04) |
Adjusted for gender, age, number of falls in prior 3 months, CCI, ADL, hurt during index fall, hospital site, prior assistive equipment use (except for fall-related hospitalizations models due to quasi-complete separation) ;
N=54 for adjusted analysis due to missing data.
Timing of events in follow-up
As seen in Figure 2.a), the Mean Cumulative Function difference curves indicate that the intervention prevented all-cause ED visits in the first two months and between four and five and a half months of the study – during this time period the difference between the usual care (blue) and intervention (red) arms increased. Overall, the intervention prevented approximately 0.75 falls per six person-months. For fall-related ED visits, (Figure 2.b) the usual care arm slope is steeper than the intervention arm slope, particularly initially. The greatest difference between the curves is at four and a half months, indicating that the effects built throughout follow-up; this plot shows that the intervention prevented approximately 0.3 falls per six person-months.
Figure 2.
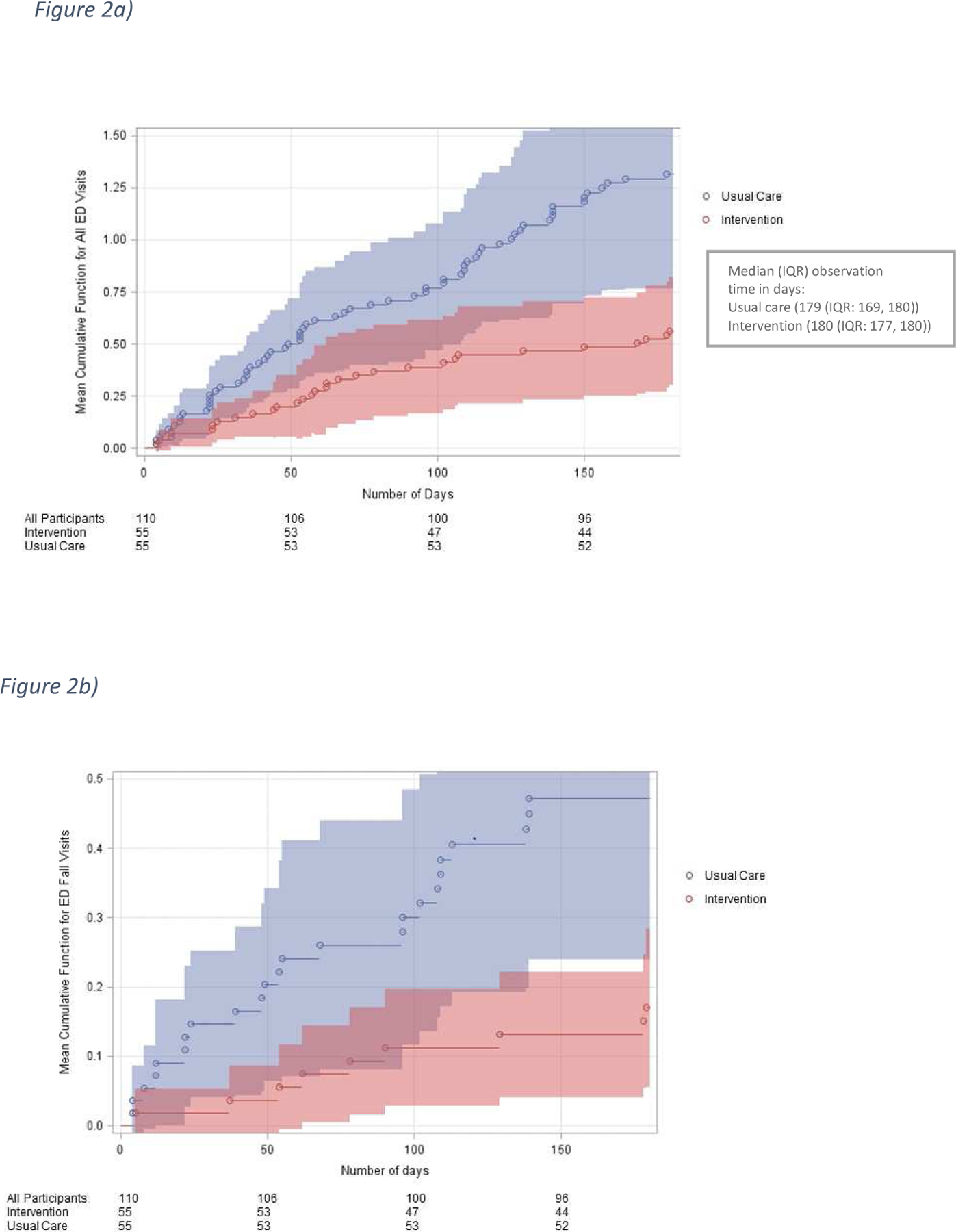
Mean Cumulative Function Curves for all ED visits (a) and (b) fall-related ED visits over time
Adherence to pharmacy recommendations
Pharmacists made 219 medication suggestions about 120 medications, with an average of 2.2 recommendations per participant. Among the 154 recommendations with follow-up data, 73 percent of the recommendations made by the pharmacist to reduce subsequent fall risk were adhered to partially or fully; 51% (79) of the recommendations were fully, 22% (34) were partially, and 27% (41) were not adhered to. These recommendations included: use over the counter alternatives to a medication (11%; 25), use increased precaution when taking a medication with known side effect of falls (11%; 25), stop a medication completely (9%; 19), and change timing of medication (9%, 20).
Adherence to PT recommendations
PTs made 156 recommendations with an average of 3.3 recommendations per participant, who received PT in the ED. Of the 100 recommendations assessed at six-month follow-up, participants reported being fully adherent to 45% (45) recommendations, partially adherent with 23% (23) recommendations, and non-adherent to 32% (32) of recommendations. Pt provided general education about falls to 84% (39), recommended new or increased walker use to 52% (24), home PT to 41% (19), SNF stay to 41% (19), footwear education 37% (17), and initiating home exercises to 22% (10).
Several lessons were learned during implementation of the GAPcare model that could be helpful for other EDs planning to institute a similar intervention and are highlighted in Table 4 (adapted from previously published study on GAPcare9).
Table 4.
Lessons Learned and Planned Adaptations
| Category | Lessons learned | Adaptations and planned improvements |
|---|---|---|
| Recruitment | Delayed identification of potentially eligible participants with falls by the research staff, and disqualification due to missed falls | Instituted automated alert in EHR to research staff for ≥65-year-old patient receiving head/neck imaging (probable fall). Broadened eligibility to include falls one week prior to ED visit. |
| Eligibility criteria | PT assessment of intervention participants changed planned ED disposition to SNF instead of home | Changed eligibility criteria - participants remained in study regardless of ED disposition to allow for observation of PT effect on disposition (intention-to-treat principle) |
| Staffing | Limited availability of PT and pharmacists during evening and weekend hours | Initiated discussions with hospital leaders to expand pharmacist and PT coverage. Board-certified resident pharmacists will be trained to supplement the main ED pharmacist’s activities. |
| Outcome assessment | Participants often experienced hospitalizations, SNF stays, worsening medical conditions, or death in follow-up making self-reported outcome reporting inconsistent | Relied primarily on EHR rather than self-reported outcomes for analysis. Future studies (GAPcare II) will use objective measures for fall events, like wearable sensors. |
LIMITATIONS
Although we found clinically important and significant differences in healthcare utilization between arms in the GAPcare study, we originally designed the study to evaluate feasibility and initial efficacy to reduce falls. It is possible we had incomplete capture of data by using the EHR, but we believe we captured a majority of the data because (1) Rhode Island Hospital ED is the only tertiary referral and trauma center in the state, (2) the health system is the largest in the state (256,000 ED visits annually of 446,000 ED visits statewide in 2018) and encompasses four acute-care hospitals, all of which use the same EHR. We lack a complete understanding of the role SNFs played in participant outcomes; our exploratory analyses showed no major differences in outcomes for patients who permanently moved to SNF, but we do not know if there were differences in short-term SNF use between arms and if those may have impacted the efficacy of the intervention. We did not have sufficient sample to evaluate if ethnic and racial minority adults benefit from this intervention. Similar to other fall prevention trials in multimorbid, frail patients,36 many patients declined enrollment (n=174), potentially reducing the generalizability of our results. Implementing GAPcare may be challenging at hospitals that lack a geriatric ED champion, buy-in from ED directors and pharmacy and PT leadership, so securing interest in the intervention by these parties is an important first step. It is unclear whether pharmacy or PT consultation contributed more to fall reduction; future research could include a factorial trial design to better disentangle the treatment effects of these two intervention components.
DISCUSSION
In this randomized controlled trial of 110 participants, we found that a brief, tailored, structured fall prevention intervention administered by pharmacists and PTs reduced subsequent ED visits whether or not related to falls. It is notable that pharmacy and PT recommendations were generally followed. The study findings are promising and indicate the value of further examining this intervention in a larger trial with a longer follow-up period and more diverse patient population.
GAPcare might have been efficacious because the intervention occurred immediately after the fall while the patient was in the ED. Performing a fall prevention intervention in the ED (as opposed to after the ED visit) decreases the delay to evaluation and treatment, which is critical because older adults are at high risk of subsequent falls in the immediate post-fall period.37–39 A London based study of 397 older ED patients who had a fall and received a home-based occupational therapy assessment significantly reduced falls (OR 0.39 (95% CI 0.23–0.60),34 but when this program was implemented in the Netherlands, there was no reduction in falls.40 In the latter study from the Netherlands, although recruitment was initiated in the ED, fall assessments were completed on average 5 to 10 weeks after the initial ED visit.
We believe GAPcare was successful because it greatly improves upon the status quo of fall evaluation in the ED. Emergency clinicians primarily perform a trauma assessment of older adults who present for falls. Reasons for the fall are rarely investigated6,41 and so valuable prevention opportunities are missed. By engaging pharmacists and PTs to help identify and recommend changes to medication-related and function-related risk factors, we believe we achieved success in reducing future undesirable events. We suggest clinicians consider falls a symptom rather than a discrete clinical complaint. A fall often indicates that there has been a decline in strength, vision, cognition, balance, or another vital health parameter in an older person’s life, falls are rarely purely environmental or “mechanical”41. In a study by Sri-On et al. of older adults presenting the ED with a fall, there were high rates of six-month adverse events - recurrent falls (21%), ED visits (43%) and hospitalizations (33%) – and rates were similar whether the ED clinician termed the fall “mechanical” or not.41 If we fail to recognize and ameliorate risk factors for the fall in the ED or rely on referral to our primary care colleagues, we will miss opportunities to reduce fall-related morbidity and mortality.
Another reason we believe our intervention was successful is because we combined PT with pharmacist-led MTM. Deprescribing interventions, in which modifying fall-risk medication is the only component of the intervention, may not reduce falls.42,43 Qualitative studies on deprescribing showed that physicians avoid discussing deprescribing because “preventative medication is not easy to reduce”44,45, “lack of benefit/risk information of prescribing”44,45 and “medications [are] initiated by specialists”44. We may have had success with GAPcare because the fall was a trigger event, that necessitated deprescribing and motivational interviewing is promising in bringing about behavior change.46 Also, specialists with access to the EHR could view the pharmacist note and could modify the drugs they prescribed. We may have also had more success because older patients who seek care in EDs may be on more fall-risk increasing medication, and could therefore experience a greater benefit from deprescribing. Early PT, such as in GAPcare, reduces pain and improves patient satisfaction,47 and exercise-based interventions can reduce falls.48 Because PTs are skilled in determining patients’ ability to mobilize safely and recognizing the patient needs for social and environmental support, patients receiving PT consults may have had fewer unrecognized and unmet needs upon discharge, which contributed to a reduction in subsequent ED visits.
It is important to consider the cost of the GAPcare intervention, as cost and staffing could be a barrier to widespread uptake. PTs can bill for their ED evaluations49 and MTM by pharmacists is covered by Medicare for patients with polypharmacy (on five or more medications). Southerland et al. evaluated the financial feasibility of multidisciplinary consultations in the ED, and found that a pharmacist is financially self-sustaining at 7.7 medication reconciliation consultations and a PT is self-sustaining at 5.7 consults per workday.50 An average fall-related ED visits costs Medicare $5000 – 6000.51 Future research can help determine if GAPcare reduces healthcare costs and is cost effective.
In summary, GAPcare is the first ED-initiated randomized controlled trial in the US evaluating a multidisciplinary pharmacy and PT consultation in the ED to reduce future fall-related and all-cause healthcare visits. Our findings suggest that ED visits are decreased after a brief, structured fall prevention intervention. Implementation of the GAPcare intervention in other EDs could help improve emergency care for falls, start prevention efforts when they are most needed, and reduce subsequent burdensome healthcare visits.
Supplementary Material
Acknowledgments:
Financial Support:
This publication was made possible by the National Institute on Aging (R03AG056349; K76AG059983), and SAEMF/EMF. SAEMF/EMF GEMSSTAR for Emergency Medicine Supplemental Funding (RF2017-010).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Prior Presentations: New England Regional Meeting of the Society of Academic Emergency Medicine, Worchester, MA (March 2019), American College of Emergency Physicians Annual Conference Research Forum Denver, CO (October 2019)
Conflict of Interest Disclosure:
EG, SM, LR, SL, HM, RM report no conflicts of interest.
REFERENCES
- 1.Hartholt KA, Lee R, Burns ER, van Beeck EF. Mortality From Falls Among US Adults Aged 75 Years or Older, 2000–2016. Jama. 2019;321(21):2131–2133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.National Safety Council. Older Adult Falls. https://injuryfacts.nsc.org/home-and-community/safety-topics/older-adult-falls/. Published 2020. Accessed April 8, 2020.
- 3.Sirois MJ, Emond M, Ouellet MC, et al. Cumulative incidence of functional decline after minor injuries in previously independent older Canadian individuals in the emergency department. Journal of the American Geriatrics Society. 2013;61(10):1661–1668. [DOI] [PubMed] [Google Scholar]
- 4.Florence CS, Bergen G, Atherly A, Burns E, Stevens J, Drake C. Medical Costs of Fatal and Nonfatal Falls in Older Adults. Journal of the American Geriatrics Society. 2018;66(4):693–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O’Loughlin JL, Robitaille Y, Boivin JF, Suissa S. Incidence of and risk factors for falls and injurious falls among the community-dwelling elderly. American journal of epidemiology. 1993;137(3):342–354. [DOI] [PubMed] [Google Scholar]
- 6.Salter AE, Khan KM, Donaldson MG, et al. Community-dwelling seniors who present to the emergency department with a fall do not receive Guideline care and their fall risk profile worsens significantly: a 6-month prospective study. Osteoporosis international : a journal established as result of cooperation between the European Foundation for Osteoporosis and the National Osteoporosis Foundation of the USA. 2006;17(5):672–683. [DOI] [PubMed] [Google Scholar]
- 7.Guirguis-Blake JM, Michael YL, Perdue LA, Coppola EL, Beil TL, Thompson JH. U.S. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews In: Interventions to Prevent Falls in Community-Dwelling Older Adults: A Systematic Review for the U.S. Preventive Services Task Force. Rockville, MD: Agency for Healthcare Research and Quality (US); 2018. [PubMed] [Google Scholar]
- 8.Kahn JH, Magauran BG Jr., Olshaker JS, Shankar KN. Current Trends in Geriatric Emergency Medicine. Emergency medicine clinics of North America. 2016;34(3):435–452. [DOI] [PubMed] [Google Scholar]
- 9.Goldberg EM, Marks SJ, Ilegbusi A, Resnik L, Strauss DH, Merchant RC. GAPcare: The Geriatric Acute and Post-Acute Fall Prevention Intervention in the Emergency Department: Preliminary Data. J Am Geriatr Soc. 2020;68(1):198–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldberg EM, Gettel CJ, Hayes K, Shield RR, Guthrie KM. GAPcare: The Geriatric Acute and Post-Acute Fall Prevention Intervention for Emergency Department Patients – A Qualitative Evaluation. OBM Geriatrics. 2019;3(4):1–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gettel CJ, Hayes K, Shield RR, Guthrie KM, Goldberg EM. Care transition decisions after a fall-related ED visit: a qualitative study of patients’ and caregivers’ experiences. Acad Emerg Med. 2020. [DOI] [PMC free article] [PubMed]
- 12.Carpenter CR, Hwang U, Biese K, Carter D, HOgan T, Karounos M, Malone M, Melady D, Rosen A, Rosenberg M, Schneider S, Shah M, Spiegel T, Stern M. ACEP Accredits Geriatric Emergency Care for Emergency Departments. http://www.acepnow.com/article/acep-accredits-geriatric-emergency-care-emergency-departments/. Published 2017. Accessed April 19, 2017.
- 13.Geriatric emergency department guidelines. Ann Emerg Med. 2014;63(5):e7–25. [DOI] [PubMed] [Google Scholar]
- 14.Mott DA, Martin B, Breslow R, et al. Impact of a medication therapy management intervention targeting medications associated with falling: Results of a pilot study. Journal of the American Pharmacists Association : JAPhA. 2016;56(1):22–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blalock SJ, Casteel C, Roth MT, Ferreri S, Demby KB, Shankar V. Impact of enhanced pharmacologic care on the prevention of falls: a randomized controlled trial. The American journal of geriatric pharmacotherapy. 2010;8(5):428–440. [DOI] [PubMed] [Google Scholar]
- 16.McDonnell PJ, Jacobs MR. Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother. 2002;36(9):1331–1336. [DOI] [PubMed] [Google Scholar]
- 17.Senst BL, Achusim LE, Genest RP, et al. Practical approach to determining costs and frequency of adverse drug events in a health care network. Am J Health Syst Pharm. 2001;58(12):1126–1132. [DOI] [PubMed] [Google Scholar]
- 18.Lesser A, Israni J, Kent T, Ko KJ. Association Between Physical Therapy in the Emergency Department and Emergency Department Revisits for Older Adult Fallers: A Nationally Representative Analysis. Journal of the American Geriatrics Society. 2018;66(11):2205–2212. [DOI] [PubMed] [Google Scholar]
- 19.Southerland LT, Vargas AJ, Nagaraj L, Gure TR, Caterino JM. An Emergency Department Observation Unit Is a Feasible Setting for Multidisciplinary Geriatric Assessments in Compliance With the Geriatric Emergency Department Guidelines. Academic Emergency Medicine. 2018;25(1):76–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Carpenter CR, DesPain B Fau - Keeling TN, Keeling Tn Fau - Shah M, Shah M Fau - Rothenberger M, Rothenberger M. The Six-Item Screener and AD8 for the detection of cognitive impairment in geriatric emergency department patients. 2011(1097–6760 (Electronic)). [DOI] [PMC free article] [PubMed]
- 21.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Goldberg EM, Resnik L, Marks SJ, Merchant RC. GAPcare: the Geriatric Acute and Post-acute Fall Prevention Intervention—a pilot investigation of an emergency department-based fall prevention program for community-dwelling older adults. Pilot and Feasibility Studies. 2019. [DOI] [PMC free article] [PubMed]
- 23.Huded JM, Dresden SM, Gravenor SJ, Rowe T, Lindquist LA. Screening for Fall Risks in the Emergency Department: A Novel Nursing-Driven Program. Western Journal of Emergency Medicine. 2015;16(7):1043–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jette DU, Stilphen M, Ranganathan VK, Passek SD, Frost FS, Jette AM. Validity of the AM-PAC “6-Clicks” inpatient daily activity and basic mobility short forms. Physical therapy. 2014;94(3):379–391. [DOI] [PubMed] [Google Scholar]
- 25.Tinetti ME, Williams TF, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. The American journal of medicine. 1986;80(3):429–434. [DOI] [PubMed] [Google Scholar]
- 26.Buatois S, Miljkovic D, Manckoundia P, et al. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. Journal of the American Geriatrics Society. 2008;56(8):1575–1577. [DOI] [PubMed] [Google Scholar]
- 27.Stevens JA. The STEADI Tool Kit: A Fall Prevention Resource for Health Care Providers. The IHS primary care provider. 2013;39(9):162–166. [PMC free article] [PubMed] [Google Scholar]
- 28.Worster A, Bledsoe RD, Cleve P, Fernandes CM, Upadhye S, Eva K. Reassessing the methods of medical record review studies in emergency medicine research. Ann Emerg Med. 2005;45(4):448–451. [DOI] [PubMed] [Google Scholar]
- 29.Robertson MC, Campbell AJ, Gardner MM, Devlin N. Preventing injuries in older people by preventing falls: a meta-analysis of individual-level data. Journal of the American Geriatrics Society. 2002;50(5):905–911. [DOI] [PubMed] [Google Scholar]
- 30.Tiedemann A, Sherrington C, Orr T, et al. Identifying older people at high risk of future falls: development and validation of a screening tool for use in emergency departments. Emergency medicine journal : EMJ. 2013;30(11):918–922. [DOI] [PubMed] [Google Scholar]
- 31.Donaldson MG, Sobolev B, Cook WL, Janssen PA, Khan KM. Analysis of recurrent events: a systematic review of randomised controlled trials of interventions to prevent falls. Age and Ageing. 2008;38(2):151–155. [DOI] [PubMed] [Google Scholar]
- 32.Robertson MC, Campbell AJ, Herbison P. Statistical Analysis of Efficacy in Falls Prevention Trials. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2005;60(4):530–534. [DOI] [PubMed] [Google Scholar]
- 33.Richard J Cook. Number Needed to Treat for Recurrent Events. Journal of Biometrics & Biostatistics 2013;4(3):2155–6180. [Google Scholar]
- 34.Close J, Ellis M, Hooper R, Glucksman E, Jackson S, Swift C. Prevention of falls in the elderly trial (PROFET): a randomised controlled trial. Lancet (London, England). 1999;353(9147):93–97. [DOI] [PubMed] [Google Scholar]
- 35.Ashman JJ, Schappert SM, L. S Emergency department visits among adults aged 60 and over: United States, 2014–2017. Hyattsville, MD, 2020. [PubMed] [Google Scholar]
- 36.Barker A, Cameron P, Flicker L, et al. Evaluation of RESPOND, a patient-centred program to prevent falls in older people presenting to the emergency department with a fall: A randomised controlled trial. PLoS medicine. 2019;16(5):e1002807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lam C, Kang J-H, Lin H-Y, Huang H-C, Wu C-C, Chen P-L. First Fall-Related Injuries Requiring Hospitalization Increase the Risk of Recurrent Injurious Falls: A Nationwide Cohort Study in Taiwan. PLoS ONE. 2016;11(2):e0149887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sri-On J, Tirrell GP, Bean JF, Lipsitz LA, Liu SW. Revisit, Subsequent Hospitalization, Recurrent Fall, and Death Within 6 Months After a Fall Among Elderly Emergency Department Patients. Ann Emerg Med. 2017;70(4):516–521.e512. [DOI] [PubMed] [Google Scholar]
- 39.Shankar KN, Treadway NJ, Taylor AA, Breaud AH, Peterson EW, Howland J. Older adult falls prevention behaviors 60 days post-discharge from an urban emergency department after treatment for a fall. Injury epidemiology. 2017;4(1):18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hendriks MRC, Bleijlevens MHC, Van Haastregt JCM, et al. Lack of Effectiveness of a Multidisciplinary Fall-Prevention Program in Elderly People at Risk: A Randomized, Controlled Trial. Journal of the American Geriatrics Society. 2008;56(8):1390–1397. [DOI] [PubMed] [Google Scholar]
- 41.Sri-on J, Tirrell GP, Lipsitz LA, Liu SW. Is there such a thing as a mechanical fall? The American journal of emergency medicine. 2016;34(3):582–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Thillainadesan J, Gnjidic D, Green S, Hilmer SN. Impact of Deprescribing Interventions in Older Hospitalised Patients on Prescribing and Clinical Outcomes: A Systematic Review of Randomised Trials. Drugs Aging. 2018;35(4):303–319. [DOI] [PubMed] [Google Scholar]
- 43.Curtin D, Jennings E, Daunt R, et al. Deprescribing in Older People Approaching End of Life: A Randomized Controlled Trial Using STOPPFrail Criteria. Journal of the American Geriatrics Society. 2020;68(4):762–769. [DOI] [PubMed] [Google Scholar]
- 44.Magin P, Goode S, Pond D. GPs, medications and older people: A qualitative study of general practitioners’ approaches to potentially inappropriate medications in older people. Australas J Ageing. 2015;34(2):134–139. [DOI] [PubMed] [Google Scholar]
- 45.Schuling J, Gebben H, Veehof LJ, Haaijer-Ruskamp FM. Deprescribing medication in very elderly patients with multimorbidity: the view of Dutch GPs. A qualitative study. BMC Fam Pract. 2012;13:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lundahl B, Moleni T, Burke BL, et al. Motivational interviewing in medical care settings: a systematic review and meta-analysis of randomized controlled trials. Patient Educ Couns. 2013;93(2):157–168. [DOI] [PubMed] [Google Scholar]
- 47.Lau PM, Chow DH, Pope MH. Early physiotherapy intervention in an Accident and Emergency Department reduces pain and improves satisfaction for patients with acute low back pain: a randomised trial. Aust J Physiother. 2008;54(4):243–249. [DOI] [PubMed] [Google Scholar]
- 48.Sherrington C, Fairhall NJ, Wallbank GK, et al. Exercise for preventing falls in older people living in the community. Cochrane Database Syst Rev. 2019;1:Cd012424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Plummer L, Sridhar S, Beninato M, Parlman K. Physical Therapist Practice in the Emergency Department Observation Unit: Descriptive Study. Physical therapy. 2015;95(2):249–256. [DOI] [PubMed] [Google Scholar]
- 50.Southerland LT, Savage EL, Muska Duff K, et al. Hospital costs and reimbursement model for a Geriatric Emergency Department. Academic Emergency Medicine.n/a(n/a). [DOI] [PMC free article] [PubMed]
- 51.Hoffman GJ, Hays RD, Shapiro MF, Wallace SP, Ettner SL. Claims-based Identification Methods and the Cost of Fall-related Injuries Among US Older Adults. Med Care. 2016;54(7):664–671. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


