Abstract
Objective:
To establish reliability and validity of the abbreviated (10-item) Center for Epidemiologic Studies Depression Scale (CESD-10) among individuals post stroke.
Method:
The psychometric properties of the CESD-10 were evaluated in 1219 adults with stroke admitted to an eligible inpatient rehabilitation facilities (n=11) across 9 different states post stroke during 2005 to 2006. This study was a secondary data analysis of the existing publicly available clinical trial dataset, Stroke Recovery in Underserved Populations study. Reliability, validity, factory structure and item-level psychometrics of the CESD-10 were examined. In addition, the predictive accuracy of the CESD-10 was compared against the CESD-20 (criterion).
Results:
The CESD-10 was highly correlated with the CESD-20 (r=0.97). The CESD-10 had good internal reliability (Cronbach’s α=0.86). The CESD-20 and CESD-10 had similar accuracy in classifying individuals as depressed (Kappa=0.85).
Conclusion:
The 10-item CESD is a valid measure of depression for individuals post stroke.
Keywords: Stroke, Depression, Patient Outcome Assessment, Risk factors
Stroke is a leading cause of disability and death globally.1,2 In the United States of America, approximately 795,000 individuals experience a new or recurrent stroke annually.3 Stroke causes physical, emotional, social, and health barriers that often diminish patients’ quality of life. Post stroke impairments and outcomes vary depending on the location and size of infarct. Despite rapid advancements in stroke care, long-term and chronic health impact remain significant concerns, particularly when considering increasing life expectancy in the global populations (WHO, 2018; a non-modifiable stroke risk). Studies found that post-stroke depression (PSD) can negatively impact patient recovery,4–6 including increased mortality risk,7–9 functional dependence,10 and lower quality of life.11,12 The etiology of PSD is still under investigation, as psychological awareness of deficits and neurobiological changes are known contributors to PSD.13
Although depression is a common complication after stroke,13–15 it often goes undiagnosed.16 Epidemiological estimates of PSD are approximately one-third of stroke survivors.17 There are effective pharmacological interventions for depression post stroke.18,19 Positive response to PSD treatment with medication has been shown to increase survival rate and activities of daily living of stroke survivors.20 Additional research is needed to effectively screen for PSD, understand appropriate timing and duration of pharmacological treatments, and develop specific protocols for behavioral intervention. A quick and easy screening tool to capture risk for PSD and changes in mood could support early intervention and research for stroke survivors. Clinically, a valid and efficient PSD screening measure could increase identification and treatment of depression, thereby limiting the insidious impact of PSD and improve overall outcomes after stroke. There are a few screening tools for depression available, including the Patient Health Questionnaire-9,21 Beck Depression Inventory-II,22 and the Center for Epidemiologic Studies Depression Scale (CESD).23
The CESD was developed in the 1970s and is a common screening tool for depression in adult populations.23–25 The full measure consists of 20 questions and asks individuals how frequently they have had symptoms related to depression over the past week.23 While the CESD is a reliable and valid measure, there has been concerns that the length of the test combined with the number of responses for each question makes the tool confusing and cumbersome.26 A shortened version including 10 of the original 20 items was thus developed.27,28 The validity and reliability of the 10-item CESD has been investigated in older adults,29 as well as those with spinal cord injury,30 psychiatric disorders,31 and HIV.32 Wulsin and colleagues demonstrated that CESD-10 could identify patients with more severe depression and associated poor stroke outcomes.33
The purpose of this investigation was to utilize the CESD data from the Stroke Recovery in Underserved Populations database to evaluate the psychometrics of a 10-item shortened version of the CESD with stroke survivors. No study to date has examined the validity, reliability and item-level psychometrics of the CESD-10 in individuals post stroke. We hypothesized the CESD-10 will be deemed equivalent as the CESD-20 and have good psychometric properties.
Methods
Data Source
We conducted a secondary data analysis of a publicly available, de-identified dataset: Stroke Recovery in Underserved Populations 2005-2006 (https://doi.org/10.3886/ICPSR36422.v1), a clinical trial that investigated positive emotion, race difference, and outcomes post-stroke.34–36 Participants were 1219 adults post stroke admitted to one of 11 inpatient rehabilitation facilities across 9 different states (New Jersey, New York State, Iowa, California, Illinois, Texas, Washington-Arlington-Alexandria, Kentucky, Florida) during 2005 to 2006.37 Assessments were conducted in person at admission and discharge, and via telephone at 3-month and 12-month post discharge follow-up. Data from the CESD-20 completed at discharge from inpatient rehabilitation were used for this study.
Measures
We examined psychometrics of the CESD-10 and compared its predictive accuracy with the CESD-20. The 20-item CESD23 is a measure of depression symptoms cross-validated with the diagnostic and statistical manual of mental disorders-III. The original CESD-20 was determined to be a reliable and valid measure of depression among individuals with stroke.38 Each item has the same numerical rating scale from 0- “Rarely,” 1- “Some,” 2- “Occasionally,” and 3- “Most”. There are 4 positive affect questions amidst the other items querying depressive symptoms that are reverse scored (e.g. 3- “Rarely” and 0- “Most”). The total score ranges from 0 to 60 with higher scores representing higher depressive symptoms. The CESD-20 is valid to identify clinical depression when the total response score is at or above 16.39
The CESD-10 has the same rating scale of 0-3 as the CESD-20 for all items with two items that assess positive affect using the reversed rating. Previous research indicates that a score at or above 10 of the CESD-10 offers adequate sensitivity and specificity to identify clinical depression.28
We used the Functional Independence Measure (FIM™)40 scores to indicate patients’ functional independence levels. We compared functional levels as an outcome between the CESD-10 and CESD-20. The FIM assesses level of independence across 18 items that cover both motor (e.g., grooming, dressing, walking distance, etc.) and cognitive domains (e.g., communication, social interaction, memory, etc.). Each item is rated from total assistance (1) to complete independence (7). In addition to domain scores based upon the 13 motor items and 5 cognitive items, the FIM™ yields a total score that ranges from 18 to 126, with higher scores indicating higher level of functional independence.
Statistical Analyses
SPSS version 25 was used for all analyses except Rasch analysis. Internal consistency was assessed using Cronbach’s alpha and concurrent validity was assessed using Kappa statistics. Sensitivity, specificity, and predictive accuracy were assessed for the CESD-10 (cut-off 10 or higher indicate depression) as compared to the CESD-20 (cut off 16 or higher indicate depression). A factor analysis was conducted with varimax orthogonal rotation given theoretical design of CESD-10. Independent samples t-test and chi-square test for association were used to compare individuals above and below CESD-10 cutoff for demographics and functional independence. We also examined item-level psychometrics with Rasch analysis using Winsteps 4.5.1. We used the Rasch analysis rating scale model (RSM) to examine unidimensionality and item-difficulty hierarchy of the CESD-10. We chose Rasch RSM because all items have the same 4-point rating scale structure. We expected to cross-validate the factor analysis result by conducting unidimensionality statistics using Rasch analysis. We conducted Rasch residual Principal Component Analysis (PCA) to extract the primary Rasch (unidimensional) dimension. It is expected to have more than 40% Rasch dimension, less than 5% variance explained by the first contrast of Rasch residual and the eigenvalue of the first contrast less than or equal to 2.0 to be unidimensional.41–44 We examined rating scale statistics, item fit statistics, item hierarchy, person separation strata and ceiling/floor effects using Rasch analysis. The three rating scale criteria included; a minimum of ten responses in each rating category, a monotonic pattern of category measure, and the outfit mean square less than 2.0.45,46 For fit statistics, we used a conventional range of 0.6 to 1.4 of Infit mean square (Infit MNSQ) and Outfit mean square (Outfit MNSQ) with standardized fit statistics (ZSTD) within ±2 to show a good fit.42,47 Person separation index (Gp) is defined as true standard deviation divided by averaged measurement error.48 Person strata, calculated as (4Gp + 1)/3,49 representing statistically different levels of person ability distinguished by all items. From a measurement perspective, instruments should be able to statistically divide a sample into at least three distinct levels.50 The item-person map was used determine the ceiling and floor effects. Percentages greater than 5% of the sample with the minimum or maximum score were considered as significant ceiling/floor effects.51,52
Results
Table 1 displays the sample characteristics at admission. The majority of participants were White (75%), women (51%), married (52%), and had an ischemic stroke (73%). The average age was 69 (SD = 13) years at the time of the survey. There were no significant differences between individuals identified as depressed or not depressed on the CESD-10 scale based upon demographic variables: age (p = .540), gender (p = .403), race (p = .215), married (p = .070), and education years (p = .927) (Table 1). There were differences in vocational activity by depression status prior to stroke (p = .033) although of small effect (Phi = .10). To explore this difference in depression by pre-stroke vocational activity, an analysis of variance was conducted using CESD total scores across each vocational category. The ANOVA was also significant (p < .001). Post hoc analyses revealed significant mean differences, such that individuals who were employed at the time of stroke endorsed lower levels of depression symptoms than individuals who were homemakers (mean difference = −3.86; p = .027), unemployed (mean difference = −2.43; p = .036), or retired due to disability (mean difference = −3.27; p = .010) at the time of stroke. In addition, individuals who were retired due to age at time of stroke reported lower symptoms of depression than individuals who were retired due to disability (mean difference = −2.68; p = .043). There was no significant difference in depression at discharge by length of stay (p = .080). However, FIM™ Total score at admission (p < .001), discharge (p < .001), and 12-month follow-up (p < .001) were significantly different based upon depression grouping by CESD-10. Participants who were not identified as depressed at discharge had significantly higher functional independence at admission (mean difference = 5.39; p < .001), discharge (mean difference = 8.76; p < .001), and 12-month follow-up (mean difference = 8.12; p < .001) compared to people identified as depressed.
Table 1.
Sample characteristics as classified by CESD-10 at discharge
| Baseline Characteristics N = 1219 |
Non-Depressed n = 824 |
Depressed n = 395 |
p-value | |
|---|---|---|---|---|
| M(SD)/ % | M(SD)/ % | M(SD)/ % | ||
| Age (years) | 68.5(13.3) | 68.3 (13.6) | 68.8 (12.7) | .540 |
| Gender (woman) | 51.2% | 50.5% | 53.0% | .403 |
| Race | .215 | |||
| White | 75.3% | 73.8% | 78.5% | |
| Black | 16.4% | 17.8% | 13.4% | |
| Hispanic | 6.1% | 6.3% | 5.6% | |
| Other | 2.2% | 2.1% | 2.5% | |
| Education | .927 | |||
| < High School | 20.7% | 21.0% | 20.1% | |
| High School | 35.8% | 35.3% | 36.8% | |
| Some College | 22.1% | 22.5% | 21.2% | |
| College and above | 21.4% | 21.2% | 21.8% | |
| Marital Status | .070 | |||
| Married | 52.4% | 50.7% | 56.1% | |
| Never married | 17.0% | 18.4% | 14.0% | |
| Divorced or separated | 8.8% | 8.1% | 10.2% | |
| Widowed | 21.8% | 22.9% | 19.6% | |
| Employment at admit | .033 | |||
| Employed | 21.3% | 22.7% | 18.4% | |
| Student | 0.7% | 0.7% | 0.8% | |
| Homemaker | 2.6% | 2.1% | 3.8% | |
| Not Employed | 7.6% | 6.5% | 9.9% | |
| Retired- Age | 62.9% | 63.9% | 61.0% | |
| Retired- Disability | 4.8% | 4.2% | 6.1% | |
| Length of Stay (days) | 20.5 (11.3) | 20.1 (11.2) | 21.3 (11.4) | .080 |
| FIM Total at admit | 55.8 (19.8) | 57.5 (19.5) | 52.2 (20.0) | < .001 |
| FIM Total at discharge | 81.3 (24.0) | 84.1 (22.5) | 75.4 (25.9) | < .001 |
| FIM Total at 12 months | 106.9 (20.9) | 109.4 (18.8) | 101.2 (24.5) | < .001 |
Note: Depression classification was determined using cut-off score of 10 or higher to indicate depression.
The mean score for the CESD-20 was 12.14 and ranged from 0 to 58. The mean score for the CESD-10 was 7.28 and ranged from 0 to 30. The Pearson correlation between the total score of the CESD-20 and CESD-10 was 0.97. The CESD-10 had similar internal consistency as the CESD-20 (Cronbach’s alpha = .86 versus .91, respectively). The CESD-20 classified 32.2% of the sample as depressed, and the CESD-10 identified 32.4%. The Kappa statistic (.85) showed strong agreement of depression classification between the CESD-10 and CESD-20. The CESD-10 had a sensitivity of 90% and specificity of 95% (Table 2).
Table 2.
Agreement between CESD-10 and CESD-20
| CESD-10 | CESD-20 |
|
|---|---|---|
| Non-Depressed | Depressed | |
| Non-depressed | 786 | 38 |
| Depressed | 41 | 354 |
| Kappa agreement | .85 (.84–.87)1 | |
| Sensitivity | 90% (87%–93%)1 | |
| Specificity | 95% (93%–96%)1 | |
| PPV | 90% (86%–92%)1 | |
| NPV | 95% (94%–97%)1 | |
Note: CESD-20- Center for Epidemiologic Studies Depression Scale- 20 items original version; CESD-10- Center for Epidemiologic Studies Depression Scale- 10 item version; PPV- Positive Predictive Value; NPV- Negative Predictive Value.
Depression classification on the CESD-10 was determined using cut-off score of 10 or higher to indicate depression. Depression classification on the CESD-20 was determined using cut-off score of 16 or higher to indicate depression.
95% confidence intervals
The two-factor solution of the factor analysis explained 55.5% of the total variance (Table 3). Only factors 1 and 2 had Eigen values greater than 1. The interpretation of the strong item loadings was consistent with the eight negative affect items loading on to Factor 1 and the two positive affect items loading on to Factor 2 with no cross-factor loadings greater than .5. These results are consistent with the original CESD-20 factor structure of “negative” and “positive” affect.
Table 3.
Factor structure of CESD-10
| Scale Items | Factor Loadings |
|
|---|---|---|
| Negative Affect | Positive Affect | |
| Bothered by things | 0.59 | -- |
| Trouble focusing | 0.66 | -- |
| Felt depressed | 0.60 | -- |
| Everything was an effort | 0.72 | -- |
| Felt fearful | 0.71 | -- |
| Restless sleep | 0.68 | -- |
| Felt lonely | 0.54 | -- |
| Could not get going | 0.66 | -- |
| Hopeful about the future | -- | 0.86 |
| Was happy | -- | 0.81 |
Note. Loadings < .5 suppressed. Factor 1 accounted for 45% of the variance with an eigenvalue of 4.46. Factor 2 accounted for 11% of the variance with an eigenvalue of 1.09.
Rasch PAC result supported the factor analysis finding, indicating multidimensionality of the CESD-10. Specifically, Rasch dimension explained 38.1% variance of the data (slightly below 40%), first contrast explained 10.5% variance of the data (>5%) and the eigenvalue of the first contrast was larger than 2.0. Due to the intent to gather more information on item-level performance of the CESD-10, we still conducted planned Rasch analysis. However, we suggested the readers interpret the Rasch analysis results with caution as the data marginally violated the unidimensionality assumption. For item-level psychometrics, all CESD-10 items met three rating scale criteria and fit the model. For the item hierarchy, we found the items with least depressive symptoms were ‘felt lonely’ and ‘felt fearful’, while the items with the most depressive symptoms were ‘felt everything was an effort’ and ‘had trouble focusing’ (Table 4). The CESD-10 can only separate the participants into two levels of depressive symptoms (e.g. low and high), with a person strata of 1.99. We noticed about 391 participants (3.2%) had the maximum scores of the CESD-10, although less than 5% cutoff, this finding indicating the CESD-10 may potentially have a ceiling effect to measure depressive symptoms (too easy to capture the full range of depression in patients post stroke, particularly on the severe end). The person-item map also showed that the average person’s depressive symptoms were more severe than what the CESD-10 items could measure (Figure 1).
Table 4.
Item Difficulty in Hierarchical Order of the CESD-10.
| CESD-10 Items | Score | Infit | Outfit | |||
|---|---|---|---|---|---|---|
| Measure | SE | MNSQ | ZSTD | MNSQ | ZSTD | |
| Everything was an effort | .60 | .04 | 1.08 | 2.00 | 1.07 | 1.26 |
| Had trouble focusing | .15 | .04 | 1.05 | 1.14 | 1.12 | 1.91 |
| Bothered by things | .13 | .04 | .99 | −.261 | .22 | 3.49| |
| Sleep was restless | .11 | .04 | 1.30 | 6.44 | 1.36 | 5.37 |
| Was happy | −.01 | .04 | .95 | −1.22 | .91 | 1.40| |
| Felt depressed | −.02 | .04 | .76 | −5.96 | .72 | 4.89| |
| Could not get going | −.0 | .04 | .81 | −4.51 | .76 | −4.02 |
| Hopeful about the future | −.13 | .04 | 1.33 | 6.52 | 1.40 | 5.41 |
| Felt fearful | −.34 | .04 | .88 | −2.36 | .84 | −2.38 |
| Felt lonely | −.43 | .04 | .94 | −1.18 | .81 | −2.63 |
Abbreviations: SE: Standard error; MNSQ: mean square; ZSTD: standardized fit statistics.
Figure 1.
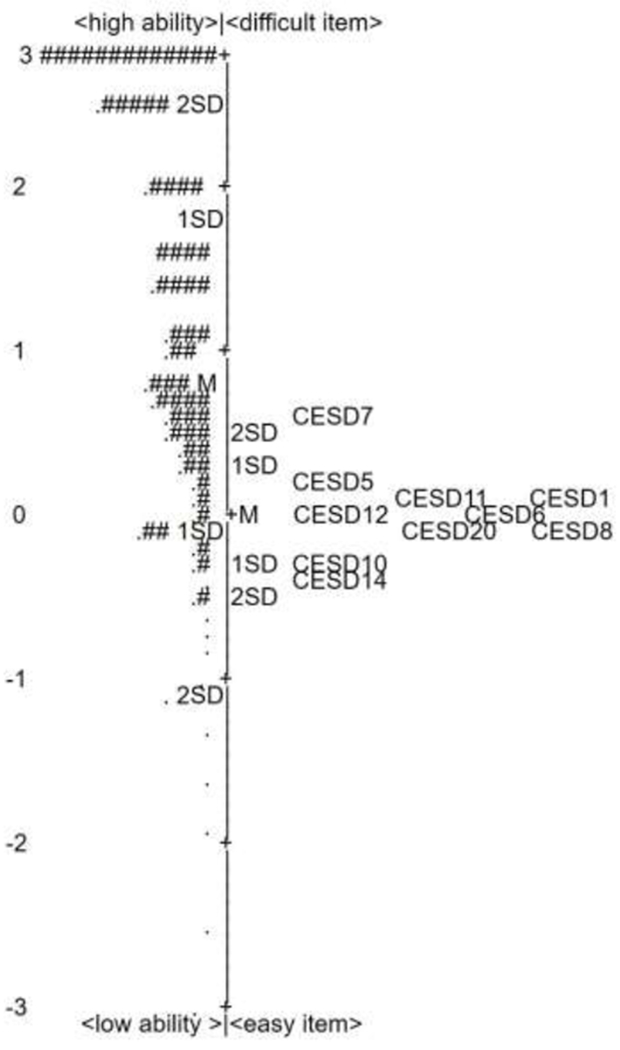
Item-Person Map of Person Ability and Item Difficulty of the CESD-10 in Stroke
Note: M: Mean of the person ability/item difficulty.
1SD: one standard deviation from the mean of person ability/item difficulty.
Each “#” is 17 persons. Each “.” is 1 to 16 persons.
Discussion
This study extends our understanding of validity and reliability for the CESD-10 as a screening tool for depression. The findings indicated that the CESD-10 had similar precision as the CESD-20 to identify individuals with post-stroke depression. Our finding is similar to the results of CESD-10 in other clinical populations (e.g., older adults, HIV, SCI, and psychiatric disorders).29–32 We found approximately a third of our sample identified as post-stroke depressed using the CESD-10 at discharge, this finding is similar as the estimates in the prior research.17
Our findings suggest the CESD-10 is a multidimensional scale. This may be due to the difference when measuring a person’s negative or positive affect. Rasch analysis results suggested ‘felt lonely’ and ‘felt fearful’ could be used as the initial screening items for detecting depression in the post-stroke population. These findings also indicate a potential benefit from adding more difficult items to the CESD-10 to be able to identify the individuals with more severe post-stroke depressive symptoms. However, limited nuance on the severe end do not preclude the utility of the CESD-10 from being used as a brief screener that warrants additional evaluation for post-stroke depression.
Depression is an important consequence post stroke and has critical implications for recovery and functioning. Findings from this study demonstrated that individuals classified as depressed on the CESD-10, had lower functional independence at discharge. In addition, this lower functional independence persisted 12 months post injury for those identified as depressed on the CESD-10 compared to those not identified as depressed. These findings are consistent with prior studies that have shown worse outcomes for individuals with post-stroke depression compared to non-depressed individuals.1,2,53 Lower functional recovery is likely linked with increased economic burden although this question is beyond the scope of this study. It is important to detect and monitor depression to improve recovery rate and functional outcomes of individuals post stroke. Investigations of novel interventions for post stroke depression require well-validated measures to assess participants’ level of depression and response to treatment. Brief screening measures for depression validated for individuals post stroke may decrease time and patient burden, which could increase detection and intervention.
This study has several limitations. We did not interview the participants to compare the CESD-10 classification result by a licensed psychologist or psychiatrist to validate the accuracy of the CESD-10. We also did not use current diagnostic and statistical manual of mental disorders (5th edition). A prospective study validating the use of the CESD-10 against current depression diagnostic criteria using clinical interview would enhance the evidence base for this measure.
Conclusion
Overall, this study demonstrated the CESD-10 had equivalent validity and reliability as the well-validated CESD-20 in stroke survivors. Validation of this shortened screening measure, CESD-10, allows for reduced burden in clinical practice and research assessments of post-stroke depression. Identifying depression in stroke survivors is crucial and can be the first step towards improved outcomes in mortality, quality of life, and economic burden after stroke. It is recommended that future research continue to examine effectiveness of this shortened measure of depression to improve early detection and early prevention for post-stroke depression for the individuals, their families, and larger society.
Acknowledgments
The authors have no conflicts of interest to report. The authors alone are responsible for the content and writing of the paper. This study was funded, in part, by the National Institutes of Health, the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Center for Medical Rehabilitation Research (K01HD101589) (PI: Li).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Michael W. Williams, University of Houston, Department of Psychology, Houston, TX.
Chih-Ying Li, University of Texas Medical Branch, Department of Occupational Therapy, Galveston, TX, Phone 409-772-9492.
Catherine C. Hay, Texas Woman’s University, Houston, TX & TIRR Memorial Hermann, Houston, TX, Phone 713-794-2112.
References
- 1.Feigin VL, Krishnamurthi RV, Parmar P, et al. Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology. 2015;45(3): 161–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Katan M, Luft A. Global burden of stroke. Semin Neurol. 2018;38(02):208–211. [DOI] [PubMed] [Google Scholar]
- 3.Virani SS, Alonso A, Benjamin EJ, et al. Heart disease and stroke statistics—2020 update: a report from the American Heart Association. Circulation. 2020:E139–E596. [DOI] [PubMed] [Google Scholar]
- 4.El Husseini N, Goldstein LB, Peterson ED, et al. Depression status is associated with functional decline over 1-year following acute stroke. J Stroke Cerebrovasc Dis. 2017;26(7): 1393–1399. [DOI] [PubMed] [Google Scholar]
- 5.Chemerinski E, Robinson R, JT K. Improved recovery in activities of daily living associated with remission of poststroke depression. Stroke. 2001;32 (1): 113–117. [DOI] [PubMed] [Google Scholar]
- 6.Ayerbe L, Ayis S, Crichton S, Wolfe CD, Rudd AG. The long-term outcomes of depression up to 10 years after stroke; the South London Stroke Register. J Neurol Neurosurg Psychiatiy. 2014;85(5): 514–521. [DOI] [PubMed] [Google Scholar]
- 7.Everson SA, Roberts RE, Goldberg DE, Kaplan GA. Depressive symptoms and increased risk of stroke mortality over a 29-year period. Arch Intern Med. 1998; 158(10): 1133–1138. [DOI] [PubMed] [Google Scholar]
- 8.Pan A, Sun Q, Okereke OI, Rexrode KM, Hu FB. Depression and risk of stroke morbidity and mortality: a meta-analysis and systematic review. JAMA. 2011;306(11):1241–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Razmara A, Valle N, Markovic D, et al. Depression Is Associated with a Higher Risk of Death among Stroke Survivors. J Stroke Cerebrovasc Dis. 2017;26(12):2870–2879. [DOI] [PubMed] [Google Scholar]
- 10.Schöttke H, Gerke L, Düsing R, Möllmann A. Post-stroke depression and functional impairments–A 3-year prospective study. Compr Psychiatry. 2020:152171. [DOI] [PubMed] [Google Scholar]
- 11.Kim E-S, Kim J-W, Kang H-J, et al. Longitudinal impact of depression on quality of life in stroke patients. Psychiatry Investig. 2018;15(2):141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gbiri CA, Akinpelu AO, Odole AC. Prevalence, pattern and impact of depression on quality of life of stroke survivors. Int J Psychiatry Clin Pract. 2010;14(3):198–203. [DOI] [PubMed] [Google Scholar]
- 13.Robinson RG, Jorge RE. Post-stroke depression: A review. Am J Psychiatry. 2016;173(3):221–231. [DOI] [PubMed] [Google Scholar]
- 14.Hackett ML, Pickles K. Part I: frequency of depression after stroke: an updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014;9(8): 1017–1025. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell AJ, Sheth B, Gill J, Yadegarfar M, Stubbs B, Meader N. Prevalence and predictors of post-stroke mood disorders: A meta-analysis and meta-regression of depression, anxiety and adjustment disorder. Gen Hosp Psychiatry. 2017;47:48–60. [DOI] [PubMed] [Google Scholar]
- 16.Hackett ML, Hill KM, Hewison J, et al. Stroke survivors who score below threshold on standard depression measures may still have negative cognitions of concern. Stroke. 2010;41(3):478–481. [DOI] [PubMed] [Google Scholar]
- 17.Paolucci S. Epidemiology and treatment of post-stroke depression. Neuropsychiatr Dis Treat. 2008;4(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun Y, Liang Y, Jiao Y, et al. Comparative efficacy and acceptability of antidepressant treatment in poststroke depression: a multiple-treatments meta-analysis. BMJ open. 2017;7(8):e016499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cui M, Huang CY, Wang F. Efficacy and Safety of Citalopram for the Treatment of Poststroke Depression: A MetaAnalysis. J Stroke Cerebrovasc Dis. 2018;27(11):2905–2918. [DOI] [PubMed] [Google Scholar]
- 20.Robinson RG, Jorge RE. Post-Stroke Depression: A Review. Am J Psychiatry. 2016;173(3):221–231. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA. 1999;282(18):1737–1744. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, TX: Psychological Corporation; 1996. [Google Scholar]
- 23.Radloff L The CES-D Scale: A Self Report Depression Scale for Research in the General Population. New York: NY: West Publishing Co; 1977. [Google Scholar]
- 24.Lyness JM, Noel TK, Cox C, King DA, Conwell Y, Caine ED. Screening for depression in elderly primary care patients. A comparison of the Center for Epidemiologic Studies-Depression Scale and the Geriatric Depression Scale. Arch Intern Med. 1997;157(4):449–454. [PubMed] [Google Scholar]
- 25.Schein RL, Koenig HG. The Center for Epidemiological Studies-Depression (CES-D) Scale: assessment of depression in the medically ill elderly. Int J Geriatr Psychiatry. 1997;12(4):436–446. [PubMed] [Google Scholar]
- 26.Kohout F The Pragmatics of Survey Field Work Among the Elderly. New York, NY: Oxford University Press; 1992. [Google Scholar]
- 27.Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D (Center for Epidemiological Studies Depression) depression symptoms index. J Aging Health. 1993;5(2):179–193. [DOI] [PubMed] [Google Scholar]
- 28.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale). Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- 29.Irwin M, Artin K, Oxman M. Screening for depression in the older adult: criterion validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D). Arch Intern Med. 1999;159 (15):1701–1704. [DOI] [PubMed] [Google Scholar]
- 30.Miller WC, Anton HA, Townson AF. Measurement properties of the CESD scale among individuals with spinal cord injury. Spinal Cord. 2008;46(4):287–292. [DOI] [PubMed] [Google Scholar]
- 31.Björgvinsson T, Kertz SJ, Bigda-Peyton JS, McCoy KL, Aderka IM. Psychometric properties of the CES-D-10 in a psychiatric sample. Assessment. 2013;20(4):429–436. [DOI] [PubMed] [Google Scholar]
- 32.Zhang W, O’Brien N, Forrest JI, et al. Validating a shortened depression scale (10 item CES-D) among HIV-positive people in British Columbia, Canada. PLoS One. 2012;7(7):e40793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wulsin L, Alwell K, Moomaw CJ, et al. Comparison of two depression measures for predicting stroke outcomes. J Psychosom Res. 2012;72(3):175–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ostir GV, Berges IM, Ottenbacher ME, Clow A, Ottenbacher KJ. Associations between positive emotion and recovery of functional status following stroke. Psychosom Med. 2008;70(4):404–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ostir GV, Berges I, Ottenbacher M, Graham JE, Ottenbacher KJ. Positive emotion following a stroke. J Rehabil Med. 2008;40(6):477–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ottenbacher KJ, Campbell J, Kuo YF, Deutsch A, Ostir GV, Granger CV. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke. 2008;39(5):1514–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ostir G, Ottenbacher K, Kuo YF. Stroke Recovery in Underserved Populations 2005-2006 [United States]. Inter-university Consortium for Political and Social Research [distributor]; 2016. [Google Scholar]
- 38.Shinar D, Gross CR, Price TR, Banko M, Bolduc PL, Robinson RG. Screening for depression in stroke patients: the reliability and validity of the Center for Epidemiologic Studies Depression Scale. Stroke. 1986;17(2):241. [DOI] [PubMed] [Google Scholar]
- 39.Parikh RM, Eden DT, Price TR, Robinson RG. The sensitivity and specificity of the Center for Epidemiologic Studies Depression Scale in screening for post-stroke depression. Int J Psychiatry Med. 1989;18(2):169–181. [DOI] [PubMed] [Google Scholar]
- 40.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993;74(5):531–536. [DOI] [PubMed] [Google Scholar]
- 41.Reeve BB, Burke LB, Chiang Y-p, et al. Enhancing measurement in health outcomes research supported by Agencies within the US Department of Health and Human Services. Qual Life Res. 2007;16(1):175–186. [DOI] [PubMed] [Google Scholar]
- 42.Bond TG, Fox CM. Model Fit and Unidimensionality Applying the Rasch Model: Fundamental Measurement in the Human Sciences. Second ed. New York, NY: Routledge; 2012:235–260. [Google Scholar]
- 43.Patient-Reported Outcome Measurement Information System (PROMIS®). Instrument Development and Validation. Scientific Standards. Version 2.0. 2013.
- 44.A User’s Guide to Winsteps Ministep 3.70.0: Rasch Model Computer Programs [computer program], Chicago, IL: Winsteps; 2012. [Google Scholar]
- 45.Linacre JM. Optimizing rating scale category effectiveness. J Appl Meas. 2002;3(1):85–106. [PubMed] [Google Scholar]
- 46.Balasubramanian CK, Li C-Y, Bowden MG, Duncan PW, Kautz SA, Velozo CA. Dimensionality and item-difficulty hierarchy of the lower extremity Fugl-Meyer Assessment in individuals with subacute and chronic stroke. Arch Phys Med Rehabil. 2016;97(4):582–589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wright BD, Linacre JM, Gustafson JE, Martin-Löf P. Reasonable mean-square fit values. Rasch Measurement Transactions. 1994; 8(3):370. [Google Scholar]
- 48.Wright BD, Masters GN. Rating Scale Analysis. Chicago, IL: MESA Press; 1982. [Google Scholar]
- 49.Wright B Number of person or item strata (4G+ 1)/3. Rasch Measurement Transactions. 2002;16:888. [Google Scholar]
- 50.Fisher WP Jr. Reliability, Separation, Strata Statistics. Rasch Measurement Transactions. 1992;6(3):238. [Google Scholar]
- 51.Li C-Y, Romero S, Bonilha HS, et al. Linking existing instruments to develop an activity of daily living item bank. Eval Health Prof. 2018;41(1):25–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Velozo CA, Choi B, Zylstra SE, Santopoalo R. Measurement qualities of a self-report and therapist-scored functional capacity instrument based on the Dictionary of Occupational Titles. J Occup Rehabil. 2006;16(1):106–119. [DOI] [PubMed] [Google Scholar]
- 53.Robinson RG. Poststroke depression prevalence, diagnosis, treatment, and disease progression. Biol Psychiatiy. 2003;54(3):376–387. [DOI] [PubMed] [Google Scholar]


