Abstract
Objective:
Although many emergency departments (EDs) have telestroke capacity, it is unclear why some EDs consistently use telestroke and others do not. We compared the characteristics and practices of EDs with robust and low assimilation of telestroke.
Methods:
We conducted semi-structured interviews with representatives of EDs that received telestroke services from 10 different networks and had used telestroke for a minimum of two years. We used maximum diversity sampling to select EDs for inclusion and applied a positive deviance approach, comparing programs with robust and low assimilation. Data collection was informed by the Consolidated Framework for Implementation Research. For the qualitative analysis, we created site summaries and conducted a supplemental matrix analysis to identify themes.
Results.
Representatives from 21 EDs with telestroke, including 11 with robust assimilation and 10 with low assimilation, participated. In EDs with robust assimilation, telestroke workflow was highly protocolized, programs had the support of leadership, telestroke use and outcomes were measured, and individual providers received feedback about their telestroke use. In EDs with low assimilation, telestroke was perceived to increase complexity, and ED physicians felt telestroke did not add value or had little value beyond a telephone consult. EDs with robust assimilation identified four sets of strategies to improve assimilation: strengthening relationships between stroke experts and ED providers, improving and standardizing processes, addressing resistant providers, and expanding the goals and role of the program.
Conclusion.
Greater assimilation of telestroke is observed in EDs with standardized workflow, leadership support, ongoing evaluation and quality improvement efforts, and mechanisms to address resistant providers.
Keywords: telestroke, telehealth, emergency departments, telemedicine, assimilation
Introduction
Acute stroke care depends on efficient evaluation and treatment focused on rapid reperfusion, either via intravenous tissue plasminogen activator (tPA) or mechanical thrombectomy. Evaluation of patient eligibility by neurologists is time sensitive, and many hospitals, especially in rural areas, do not have this expertise readily available. As a result, stroke patients may receive lower quality care. To fill this need, telestroke has allowed remote neurologists to use real time, secure videoconferencing to guide local emergency department (ED) providers through key decisions including tPA eligibility, need for thrombectomy, and need for patient transfer. Telestroke services have been shown to improve stroke care1,2 and increase use of tPA, which in turn decreases disability and may decrease mortality.3–5 The number of hospitals with telestroke has rapidly grown both in the US and other industrialized nations.6 Estimates indicate that 27% – 36% of all U.S. hospitals now have telestroke capacity.7,8 However, simply having telestroke capacity is not sufficient to improve patient outcomes; it has to be used. Many health information technology innovations are unsuccessful because healthcare organizations fail to achieve assimilation, defined as institutionalization of an innovation. When an innovation is assimilated, it is fully embedded into organizational operations and is consistently used.9 In the case of telestroke, robust assimilation means that ED staff use telestroke with the majority of suspect stroke cases that they perceive may benefit from a consult.
Prior work has highlighted that assimilation of telestroke is a challenge for some EDs. However, it remains unclear why some EDs are able to assimilate telestroke and others are not. To address this knowledge gap, we conducted semi-structured interviews with ED staff from 10 different telestroke networks across the U.S. We applied a positive deviance approach where we compared the experience of EDs with robust assimilation to those without.
Methods
Positive Deviance Approach
The positive deviance approach leverages variation that occurs naturally (e.g., in assimilation of an innovation) to understand what drives the variation and highlight the promising strategies of high performers. This approach assumes that knowledge about what works already exists, and the identified promising practices are feasible because they are already being employed by some organizations.10 By comparing and contrasting positive deviants (i.e., EDs with robust telestroke assimilation) and negative deviants (i.e., EDs with low assimilation), the goal is to identify practices that are reliably present in positive deviant sites and reliably absent in negative deviant sites.11 Although the positive deviance approach is used widely in healthcare,12 to our knowledge it has never been applied to understand variation on the topic of telestroke.
Study Participants and Sampling Strategy
We recruited representatives of spoke EDs (i.e., EDs receiving telestroke services from remote neurologists) with at least two years of experience with telestroke. We focused on mature programs given our focus on assimilation rather than early start-up experiences and challenges. As part of a larger project, our study team has identified 1306 hospitals with telestroke capacity that received telestroke services from 15 different “hub” organizations that provided telestroke consults.8 Hub organizations included both academic centers and private companies. We recruited EDs in two ways: 1) by directly contacting ED representatives and 2) by asking hub representatives to recommend 3–5 EDs in their networks that varied with respect to assimilation. Hub representatives provided ED names and contact information but did not provide assimilation details to the study team to ensure blinding. In selecting EDs for recruitment, we used maximum variation sampling to represent the diversity of experiences with telestroke across U.S. region, rurality, hospital type, bed size, and telestroke network type. Although we were not aware of assimilation status at the time we invited ED staff to participate, we continued to recruit until we obtained at least 8 EDs with robust assimilation and 8 with low assimilation, consistent with prior positive deviance studies.11
Interviews
We invited ED representatives to participate in a 60-minute telephone interview. Invitations were emailed, and recipients were instructed that they could participate or designate another person from their staff who was knowledgeable about the telestroke program to participate. One individual from each ED was interviewed, and participants included stroke coordinators, ED nurse managers, and ED medical directors. Interviewees were given a $100 gift card for their participation, and they provided verbal informed consent. Interviews were completed from November 2019-February 2020.
Interviews followed a semi-structured protocol. Topics included history and structure of the telestroke program, telestroke workflow, changes to the telestroke program implemented over time, barriers, and utilization of telestroke by individual providers and at the broader organizational level. Three members of the study team trained in qualitative research conducted the interviews. Interviews were recorded and transcribed. Harvard University’s institutional review board determined the research to be exempt.
Assimilation Measure
Interviewees were asked to estimate the proportion of times that telestroke consults were initiated among suspected stroke patients who were considered eligible for telestroke according to their local protocols. Eligibility for telestroke varied by ED, and representatives used their own definition of eligibility in determining assimilation status. We determined the cutoffs for assimilation categories after reviewing the distribution. Utilization rates of 90% or higher ware classified as robust assimilation while under 30% were classified as poor assimilation. All other cases (31–75%) were classified as medium assimilation. To facilitate comparisons, we grouped EDs with poor and medium assimilation and refer to them as low assimilators in the results.
Topics in Semi-Structured Protocols
We employed an inductive and deductive approach informed by the Consolidated Framework for Implementation Research (CFIR).13–15 CFIR is a conceptual framework with 39 individual constructs that may impact the use of a new technology or service. CFIR is frequently used to assess drivers of assimilation.1
For each interview, the content of the interview was summarized and organized by the CFIR constructs that the study team identified as relevant to telestroke assimilation following literature and preliminary transcript review (Figure 1), and by other topics that emerged during interviews (e.g., use of telephone in the telestroke process). The site summaries were completed by the lead author (LUP). Site summaries also included relevant quotes related to each CFIR construct. To further support the identification of themes, we then conducted a supplemental matrix analysis, with each ED as a column and salient categories that we developed from codes included in the site summaries as rows.16,17 Matrices have been used in qualitative data analysis to streamline the process of identifying similarities, differences, and trends in responses across groups of informants.18 A matrix provides a visual display of data that facilitates the search for and a detailed analysis of patterns, themes, and other relationships and informs subsequent conclusions.17–19 In this particular case, three tables were created (robust assimilation, poor assimilation, and medium assimilation) by the second author (JS) and reviewed by LUP. A distilled summary of each participant’s response in relation to each of the codes was placed within the relevant cell. Three team members (LUP, KZ, and JS) reviewed the tables for themes, which was achieved by making direct comparisons across all codes within a row, looking for areas of difference across robust, poor, and medium assimilation sites. Interpretations were then compared and discussed with the wider team. The final description of themes reflects a shared understanding of the data.
Figure 1:
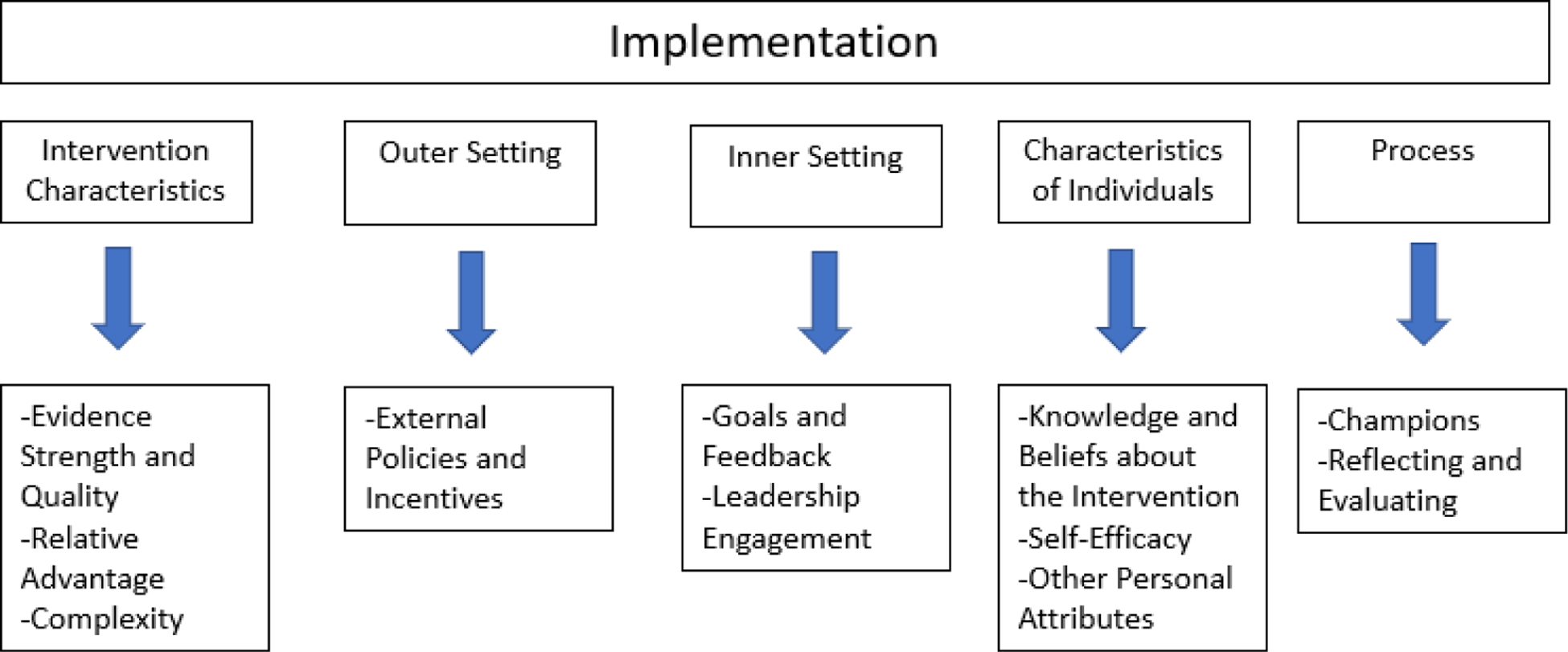
Relevant Domains for Telestroke Assimilation from the Consolidated Framework for Implementation Research.
SOURCE: Damschroder et al., 200915
Results
A total of 21 spoke EDs (17 short-term acute care hospitals [STACH] and 4 critical access hospitals [CAH]) in 11 states across 10 different telestroke networks participated. The remote neurologists for telestroke consultations worked for both academic medical centers (n=16) and private companies (n=5) (Table 1). In all but one of the 21 EDs, telestroke was available at all times (24 hours a day). ED staff who participated in interviews included: stroke coordinators (n=10), ED medical directors (n=4), and other (e.g., ED nurse managers, ED physicians) (n=7).
Table 1:
Characteristics of Participating Spoke Hospitals
| Total (N=21) | Robust Assimilators (n=11) | Low Assimilators (n=10) | ||||
|---|---|---|---|---|---|---|
| Characteristic | # | % | # | % | # | % |
| Region | ||||||
| Northeast | 4 | 19 | 1 | 9 | 3 | 30 |
| West | 6 | 28 | 3 | 27 | 3 | 30 |
| South | 7 | 33 | 4 | 36 | 3 | 30 |
| Midwest | 4 | 19 | 3 | 27 | 1 | 10 |
| Hospital Type | ||||||
| Short term acute care hospital | 17 | 81 | 9 | 82 | 8 | 80 |
| Critical access hospital | 4 | 19 | 2 | 18 | 2 | 20 |
| Stroke Certification | ||||||
| None | 15 | 71 | 7 | 64 | 8 | 80 |
| Acute Stroke Ready | 2 | 10 | 2 | 18 | 0 | 0 |
| Primary Stroke Center | 4 | 19 | 2 | 18 | 2 | 20 |
| Location | ||||||
| Rural | 10 | 48 | 4 | 36 | 6 | 60 |
| Non-rural | 11 | 52 | 7 | 64 | 4 | 40 |
| Number of beds in hospital | ||||||
| <20 | 2 | 10 | 0 | 0 | 2 | 20 |
| 21–199 | 13 | 62 | 7 | 64 | 6 | 60 |
| 200+ | 6 | 28 | 4 | 36 | 2 | 20 |
| Type of Organization Providing Remote Neurologists | ||||||
| Academic Medical Center | 16 | 76 | 8 | 73 | 8 | 80 |
| Private company | 5 | 24 | 3 | 27 | 2 | 20 |
| Years with Telestroke | ||||||
| ~ 2 | 2 | 10 | 2 | 18 | 0 | 0 |
| 2–4 | 1 | 5 | 0 | 0 | 1 | 10 |
| 4+ | 18 | 86 | 9 | 82 | 9 | 90 |
| Local Stroke Expert/Neurologist | ||||||
| Yes | 10 | 48 | 6 | 55 | 4 | 40 |
| No | 11 | 52 | 5 | 45 | 6 | 60 |
NOTE: Table reflects hospital characteristics as of November 2019.
Assimilation Status and Change Over Time
Of the participating EDs, 11 had robust assimilation and 10 had low assimilation (6 medium and 4 poor). The majority of EDs of all types indicated that assimilation increased over time. Reasons that assimilation improved included that the “program proved itself,” “leadership pushed it,” the process became more formalized, the comfort level with the intervention and workflow increased, and hesitant providers were educated about telestroke and persuaded to use it. As described by a participant from a rural ED in the West, “We were using it intermittently in the beginning. We didn’t realize its potential and what it could do for us. Then, as time went on, you’re like, ‘Oh, that works really well with that patient. Here comes the next one, let’s go ahead and try it again.’ It just got better and better and more confident in using it. It’s a new piece of equipment. You look at it, and you’re not sure if you’re doing things right.”
Constructs Association with Differences in Assimilation
There were four CFIR constructs (complexity, relative advantage, self-efficacy, knowledge and beliefs) where there were notable differences across robust and low assimilators (Table 3). For complexity, robust assimilators frequently mentioned that telestroke workflow was highly protocolized (e.g., with clear eligibility criteria, consistent steps) which reduced complexity; though even robust assimilators sometimes cited complexity as an ongoing challenge. On the other hand, low assimilators were more likely to mention complexity as a major barrier to assimilation, and reported that telestroke increased door-to-needle times, was inefficient, and/or provided an unnecessary second opinion that generally confirmed decisions that the ED physician had already made.
Table 3:
CFIR Themes by Assimilation Status
| Construct | Quotes of EDs with Robust Assimilation | Quotes of EDs with Low Assimilation |
|---|---|---|
| Evidence Strength and Quality | “I think, they [ED staff] understand the metrics that we’re trying to meet are not just because they’re metrics, it’s because it improves outcomes. And so, I think understanding the impact that they’re having on outcomes is something that really motivates. It should motivate all of us.”-Non-Rural STACH,South | N/A |
| “On the actual clinical practice and doing the best thing for our patient side as well, that’s also a benefit, because there are nuances in some of these decisions, especially when it comes to the potential LVO patients, large vessel occlusion patients, and who might benefit from endovascular therapy and who might not.” -Rural CA, South | ||
| Relative Advantage | “It’s easier to delay a phone call and be back and forth and not be, not get the help from our specialist partners on a phone call. But when it’s on video chat that, that is a much more immediate response and much more comprehensive evaluation of the patient.” -Non-Rural STACH,South | “If we [the ED physicians] have questions, we’ll discuss by phone, but our neurologists are comfortable with that discussion without actually having to watch the patient on a video screen.” -Non-Rural STACH, Midwest |
| “Now that we’ve been using tPA, we are comfortable with just doing that and just talking [over the phone].” -Rural STACH, South | ||
| “They’re able to do full exams and see for themselves exactly how the patient is presenting, actually interact with that patient through that portal. I don’t know, I just think that adds tremendous value versus just a phone call with descriptions. My description may be different than your description of a patient, or someone else’s description. So, there’s always subjectivity in there when you’re trying to describe symptoms or trying to describe presentation. And so, being able to interface or interact through that portal is pretty, I think that certainly adds value.” -Non-Rural STACH, South | ||
| Complexity | “You’ve got to have a standardized process that you follow every single time. I’m actually working with our management… There’s some management engineers that are really helping… Like Lean Six Sigma, there’re people that look at things from a very different perspective. I think what we’re really trying to do is standardize.” -Non-Rural STACH, Northeast | “Many of the physicians feel like whatever the neurologist is doing on the other end, be it the stroke scale, may feel like they’re already doing that, so essentially why get another opinion when I can just talk to them on the phone and give them the assessment that the physician has made already.”-Rural STACH, West |
| “No, if we do use telestroke then it’s a greater length of stay. That’s probably our own fault because the telestroke has parameters, goals, they want you to call within 15 minutes. But our docs have never utilized it like that. They’ve always done their own workups and then decided, “Oh, I don’t really know what this is. Let me get a video consult.” That’s more how they’ve used it rather than, I guess more used it as a second opinion rather than the first decision.” -Rural STACH, West | ||
| External Policies and Incentives | “So much of this went hand in hand with our certification with just the revamping of the stroke process in general.” -Non-Rural CAH, Midwest | N/A |
| “I got the ED physicians more involved in the telestroke process by tying it to an effort to improve door-to-needle times.” -Non-Rural STACH, Midwest | ||
| Goals and Feedback | “Those [ED physicians] who were hesitant to call [telestroke] are the ones that have learned and have the feedback coming back. “Well look, here’s the positive MRI, we could have possibly given them tPA.” I think it’s a good feedback mechanism; it really helps encourage them.” -Non-Rural STACH, Midwest | N/A |
| “Any case where tPA took longer than 45 minutes, [the provider] gets called into the principal’s office, and have to explain why that happened. And then we also have a really good stroke coordinator who compiles all of the code strokes for the previous week or month and sends them out to everybody so that you can see everybody else’s struggles and successes as well as learning opportunities.” -Non-Rural STACH, West | ||
| Leadership engagement | “But in the beginning of the program, we did have pushback from a couple of providers who are no longer here who indicated that they really didn’t believe in using tPA. They didn’t feel that it made that much of a difference. And the administration kind of came through with ‘this is what best practice guidelines are and if you’re not going to practice by these then you won’t be practicing medicine here.’-Rural STACH,South | N/A |
| “So my E.D. medical director used… So our stroke medical director is usually an E.D. physician. And my E.D. medical director used to be the stroke medical director and then he got promoted. So I think having, and he helped before I took over… He helped kind of grow the whole stroke program, and help get them primary stroke certified, and he really kind of enforces what we need to do.” -Non-Rural STACH, Midwest | ||
| Knowledge and Beliefs about the Intervention | “I also think they enjoy passing the block of decision making to somebody else because they already have so much on their plate. Our ED is getting busier and busier as well. So because of that, even if they’re not totally buying into tPA, I don’t see any decrease of activation.” -Rural STACH, West | “[With telestroke] the ED physician has to order the tPA. So if you read the emergency medicine literature on tPA, there’s not been this whole hearted buy-in to tPA as a good drug to treat acute strokes like there has been in neurology… Because there’s risk of bleeding, and if you look at long-term outcomes, there’s debates as to whether there’s really any difference in long-term outcomes with this drug. So it’s one thing if the neurologist says we should give it and they order it, it’s another thing if the ED physician has to order it. Because when you order it, you’re taking responsibility for what happens when you order the drug and give something to somebody. So that generated some philosophical debates about, “Why should I, the ED physician, be ordering a drug that a neurologist says the patient should get?” And that goes back to the debates between emergency medicine and neurology as to whether this drug really is as good as it might be advertised as for strokes.” -Non-Rural STACH, South |
| Self-Efficacy | “I think everybody has been very supportive, because I think they know that having that extra support and making decisions about a medication, that can be dangerous. I think having that extra support makes everyone feel a lot better about the care we’re providing.” -Non-Rural STACH,South | “We rarely hook up the neurologist to do telestroke because we feel that the decision to give tPA and decisions to make regarding stroke treatment are well within the capabilities of emergency physicians.” -Non-Rural STACH, Midwest |
| “The majority of our doctors feel confident in their own decisions [about administering tPA]. -Rural STACH, West | ||
| “The biggest thing is it’s a big confidence booster, because it makes us more resolute about most of the decisions we make. Then, in the questionable cases, it really helps sway the decision-making process one direction or another when we are uncertain.” -Rural CAH, South | ||
| Other Personal Attributes | “We want to share the liability with the neurologist…And I would say that most of my partners are very happy to document and to say the neurologist told me to do it. And so that’s why I did it.” -Non-Rural STACH, West | “Well, I think they just didn’t feel comfortable with it [tPA]. One of the physicians actually had a bad experience with it. He used it and the patient bled out. He’s one of the ones that we actually have a difficult time with [in initiating telestroke].” -Non-Rural STACH, South |
| “It [telestroke] helps with at least a perception of decreased liability on the one side if we have neurology helping us make these decisions on whether to lyse or not. -Rural CAH, South | ||
| Champion | “We have a very strong ED [champion.] When we got telestroke, he laid down the policy that if you get a stroke patient within a five hour window of last known normal, you will activate telestroke period, end of story.” -Rural STACH,South | N/A |
| Reflecting and Evaluating | “We look at those outliers [cases telestroke is not used] and figure out why were they not activated. Was it because of the symptoms? Was it because of the information we received prehospital? Whatever the answer may be, but we’re consistent with our utilization if we identify that it’s consistent with signs and symptoms of a stroke, that’s in the order set, that’s in the care plan for that patient every time.” -Non-Rural CAH, Midwest | N/A |
| “So we abstract data into a stroke registry called Get With The Guidelines. We actually have ways to go in there and look to say, “Oh did we miss calling TeleStroke on this patient. Or were they eligible and we didn’t pull the trigger to call TeleStroke.” -Non-Rural STACH, Northeast |
For relative advantage, robust assimilators reported that telestroke had numerous advantages over a telephone consult. They explained that videoconferencing allows the neurologist to directly interact with and comprehensively evaluate the patient. Low assimilators, on the other hand, often argued that a telephone consult was a suitable alternative to telestroke, and videoconferencing provided little additional value.
Self-efficacy of ED providers also differed across assimilation categories. In EDs with robust assimilation, telestroke increased the confidence of EDs providers in clinical decision-making. In contrast, low assimilators often reported that ED providers were confident administering tPA without a consult. Finally, negative beliefs about tPA (i.e., concerns that tPA is not effective in improving stroke outcomes and can harm patients) impacted telestroke utilization in EDs in all assimilation categories, though programs differed in the way those beliefs impacted telestroke use. Participants representing EDs with robust assimilation pointed out that their providers’ lack of certainty about tPA made them more willing to use telestroke and share the responsibility for decision-making with a remote neurologist. In contrast, low assimilators frequently suggested that negative views about tPA (and the view that telestroke results in greater tPA use) reduced willingness to activate telestroke.
There were a number of other CFIR constructs that were predominantly discussed by robust assimilators. Participants frequently explained that they they embedded their programs within broader efforts to improve stroke care and decrease door-to-needle times, often in an effort to achieve stroke certification (external policies and incentives construct). The perception that telestroke was successful in improving quality of care and outcomes was mentioned as an important factor supporting assimilation (evidence strength and quality). They also reported having hospital leaders (leadership construct) and clinic champions (champion construct) who promoted the program. Many participants noted that individual ED providers supported the program because they welcomed the opportunity to share liability with consulting neurologists (other personal attributes construct).
Finally, two practices related to quality improvement were common among programs with robust assimilation. Participants frequently discussed evaluating their telestroke programs to support quality improvement (reflecting and evaluating construct) and setting goals and providing feedback to individual providers about their telestroke use (goals and feedback construct). Interestingly, there were several notable areas where there did not appear to be a relationship with assimilation including: type of organization (academic, vendor) providing telestroke services, whether the hospital had neurologists on staff, and whether telestroke was used only in the ED vs. also in the inpatient setting.
Strategies to Improve Assimilation
Participants representing EDs with robust assimilation identified 13 strategies that facilitate consistent use of telestroke across four categories: 1) strengthening relationships between stroke experts and ED providers; 2) improving and standardizing processes; 3) addressing resistant providers; and 4) expanding the goals and role of the program (Table 4).
Table 4:
Strategies to Improve Assimilation
| Strategy | Illustrative Quote |
|---|---|
| Strengthening relationships between stroke experts and ED providers | |
| Take steps to increase familiarity with and develop rapport with consulting neurologists | “We have a provider who is nervous about interacting with the … he’s intimidated by the stroke neurologist at [the hub], which there’s no reason to be, they don’t do anything on their end to be intimidating. But I think it’s just, oh my gosh, I’m speaking to an expert. And so I think some of them are just nervous to interact with them. And so they have come down to our hospital and interacted with our physicians several times, which helps with that.” -Rural STACH, South |
| Engage regularly with the hub. Invite representatives from the hub to visit and encourage the hub to provide data | “Even the director of the stroke neurology program [within the hub] has been down to visit with our physicians. He comes down about once a year at least, and he’s very proactive. Like what are your issues? What problems are you seeing? He wants to know what they’re facing and he comes down and talks to them. I’d say he comes once a year. Just does a check on our equipment himself and just looks at our room to see how things are set up and how we do it. So they’re real involved.” -Rural STACH, South |
| “I can’t say enough about the folks at [the hub] because they’re very engaged, very supportive. We get lots of appropriate data from them. We have an annual meeting with all of the spoke and hub sites, network, and share any kind of barriers that we’re experiencing or any kind of successes that they’ve experienced.” -Rural STACH, South | |
| “We do a bi-directional review once a month with them and we share cases. So we get a lot of education from them, as well. And I feel as close to the telestroke neurologist as I do to our own neurologist.”-Rural STACH, West | |
| Improving and standardizing processes | |
| Ensure process is protocolized | “I think you’ve got to have a standardized process that you follow every single time. I’m actually working with our management… There’s some management engineers that are really helping… Like Lean Six Sigma, there’re people that look at things from a very different perspective. I think what we’re really trying to do is standardize. We do this the same way every time. Then run people through the paces and do drills and give feedback, good and bad. I always do these… Sometimes I’ll do a timeline and I’ll put wins and opportunities where we can shave off minutes but also what they’ve done well.” -Non-Rural STACH, Midwest |
| “There’s definitely more buy in now that we have like a formalized program and formalized processes for all the different patients that come by EMS and personal vehicles We have the formalized stroke alert, so we have more buy in. it’s not a question anymore. It’s just become an algorithm.” -Rural STACH, West | |
| Make telestroke a nurse-driven process (i.e., do not give ED physicians the responsibility to activate telestroke) | “I do have some push back from the physicians and I’m not sure if it’s like a control thing that they don’t want to be taking direction from nursing, but we’re really kind of pushing for this to go to a nurse-driven process, right? So the charge nurse… Part of our new roll out is to really train them in the decision making process. Are they within the window? Let’s go down our exclusion criteria. If they go the left side of that algorithm, then you’re making the call to TeleStroke immediately. And it’s going to be the nurse that is going to decide this because what we’ve found is that we have this revolving door of physicians, we have a lot of local physicians coming in and out, processes are different from hospital to hospital.” -Non-Rural STACH, Northeast |
| Communicate that telestroke is not optional. In being responsive to provider input and concern, clarify that providers are expected to utilize the service. | “Don’t make it sound optional, because I think if you go that route and say, ‘use it if you want to,’ or “use it if you’re comfortable,’ you’re going to have people that are set in their ways to say, ‘yeah, I’m not comfortable and I don’t want to be comfortable.’ So I think it’s got to be kind of top-down. You want to get their buy-in and you want to let them make it their own…but at the same time saying, ‘yeah, you can modify this part of it or you can modify this to make it work, but in the end you still have to use the neurologist,’ and make that the mandate. I think that’s how it will be best accomplished.”-Non-Rural CAH, South |
| Work out the specific roles and responsibilities of each party (bedside nurse, consulting neurologist, ED physician) during the telestroke consult | “And so I think that that was some of the feeling out process, when they’re both in the room, who’s going to talk, who’s going to say this? Who’s going to do this part? Because that’s a little bit different versus the in-room, versus the physical presence, on the telemedicine. So everybody kind of has their own spiel when they go into a room, right? You’re used to saying things a certain way or doing things a certain way. So when this other person’s on, do you yield, who’s yielding, and who’s leading the show. So, that was an interesting challenge.” -Non-Rural CAH, Midwest |
| Engage key stakeholders in developing telestroke workflows | “It helped open up the ideas about how are we going to get the 45-minute tPA and they got everyone in the discussion, all of the key stakeholders, we had staff sit-down like, ‘Okay, [how] do you think this part’s going to work? [How] do you think that’s going to work?’ I think having all of the components together and just being transparent about it really helped them buy-in.”-Non-Rural STACH, Midwest |
| Collect data on use of telestroke by individual providers and provide feedback about use | “So I give them… so every month they have an E.D. physician meeting, and I go there and I give them their stroke data of “This is how many you called. This is how much tPA you gave. This is your door to needle. This is our average. This is what we’re missing in the documentation”. So they get that follow up, at minimum, once a month. -Non-Rural STACH, Midwest |
| “At the end of the month, I send out these letters that we create to be like, ‘Here’s the case rundown. Guess what guys, that patient went to therapy. They were actually walking with a walker by the time they left.’ I think it’s more investment of knowing what happens in the end. That they’re truly part of the process and not just one stop in the ER and then that’s it. But knowing that what you did in the front end really affected what happens in the end. That’s been my success.” -Non-Rural STACH, Midwest | |
| Addressing resistant providers | |
| Remind providers who are not sold on the efficacy of tPA of the benefits of shared liability, and the fact that they are more likely to be sued for failure to administer tPA than for an adverse outcome associated with use of tPA | “I always let them know, especially nowadays with stroke being such a debilitating process, that nowadays you’re more likely to get sued for not giving alteplase than for giving it and something happening. I’m like, “If there’s even a question, these guys are the experts. Use them. That’s what they’re here for. We’re not paying by the call. They are here for us. Use them. Let them do it.” --Rural STACH, Northeast |
| Work with resistant providers one-on-one to understand their concerns; compromise about workflow or consider customizing workflow for individual providers to increase utilization | “So for instance, we have one provider that really just wants to lay eyes on the patient before anything is done. So they don’t like the whole idea of going to CAT scan. And so what we did with that provider, is we essentially told them if you can see the patient as they’re being wheeled back and you can do a real quick, 30 second to a minute interview with that patient. If that makes you feel better, we’re fine with that. That’s going to still allow us to meet all of our goals. So, trying to find out the reason why certain providers were hesitant…” -Non-Rural CAH, Midwest |
| Encourage the stroke coordinator to work with a clinic champion in communicating with resistant providers. | “I also think that it’s really important to have… if you don’t have an E.D. position stroke medical director, you need to have at least one E.D. physician that’s like a stroke champion. Because if I have issues with them not following protocol, with their times are dropping a little bit, I send it straight to the stroke medical director, who’s an E.D. physician, and he quickly follows up with either that physician, or sends out an email to the whole group saying ‘this is what’s right now.’ Sometimes they don’t always like to listen, but I think having that, the buy in from the E.D. medical director and a physician down in the E.D., it really helps.” -Non-Rural STACH, Midwest |
| Expanding the goals and role of the program | |
| Ensure that telestroke is not just narrowly focused on the decision to administer tPA (e.g., use telestroke to inform decisions regarding thrombectomy, transfer) and educate staff to recognize patients who may be appropriate for telestroke | “We try to educate [our providers] that telestroke is more than just tPA.” -Non-Rural STACH, Midwest |
| “I encouraged them to cast a broader net so that we don’t miss those few atypical presentations that may come.” -Non-Rural STACH, South | |
| Embed implementation of telestroke within a broader effort to improve stroke care or obtain formal stroke certification(s) | “So much of this went hand in hand with our certification with just the revamping of the stroke process in general.” -Non-Rural CAH, Midwest |
| “From the hospital standpoint, they’re obviously interested in the quality metrics for time to CT and time to tPA. So having the stroke neurologist and a protocol approach to sort of drive that [is responsible for the high assimilation rate].” -Non-Rural STACH, Northeast | |
| “So I think that it was corporate division wide pushes to improve stroke metrics, which our hospital tracks very closely and so we’ve continued to evolve that program to where now anybody that gets tPA in more than 45 minutes is scrutinized. And so we have a average tPA administration time from, should be door to needle in less than 45, and 90th percentile should be less than 60 minutes. And so I think it was part of a multi year plan to kind of meet some of those national stroke metrics and then try and exceed them.” -Non-Rural STACH, West |
Discussion
Across 21 EDs with telestroke capacity, we observed significant variation in assimilation, the fraction of the time telestroke was used for an eligible patient. In EDs with robust assimilation, telestroke workflow was highly protocolized, programs had the support of leadership and clinic champions, and program staff provided feedback to individual providers about their telestroke use. In EDs with lower assimilation, telestroke was perceived to increase complexity and to add little value beyond a telephone consult. Providers in EDs with low assimilation often declared that they were comfortable administering tPA without a consult.
Our findings echo as well as differ from the limited prior qualitative work on telestroke. At three hospitals in Norway, difference in use of telestroke appeared to be driven by low motivation of front-line providers as well as perceived complexity of using telestroke (space, logistics).20 In the U.S., a study of two telestroke networks from 2014 found more consistent use of telestroke in EDs that had stroke center certification, a dedicated telestroke coordinator, a stroke committee of key stakeholders, local neurological expertise, and continuous telestroke process improvement.21 Our study also found that complexity, continuous process improvement, goals and feedback, and local leadership are key. However, we did not identify any relationships between program staffing models or local neurological expertise and assimilation.
What can individual EDs and telestroke hubs do to improve assimilation? First, it is useful to set clear expectation for utilization, measure utilization across eligible patients, and provide regular feedback on how the ED compares to peers. Second, programs should ensure there is a local champion who is taking ownership of the telestroke program and investing in its success. A champion can become familiar with the particular needs and concerns of individual providers and drive continuous process improvement. Third, generating clear protocols for telestroke activation and workflow appeared to be important. Knowledge of and use of protocols may be a marker of sites maintaining a level of stroke center certification, which has been shown to help drive assimilation in prior work. Fourth, ongoing education and conversations with skeptical ED physicians may be needed. Others have described skepticism about tPA among some ED physicians and resistance to external neurologist’s recommendations.22,23 Strategies may include educating providers on the medicolegal environment related to tPA, ensuring that telestroke consultations inform more than just the decision to administer tPA, and allowing multiple ED staff to activate telestroke so it is not solely a physician-driven process.
Our study has several limitations. First, we focused on the experiences of spoke EDs because the spoke is responsible for activated telestroke and as a result, controls telestroke utilization; however, it is likely that characteristics and practices of the hubs with the remote neurologists also influence assimilation. Second, we interviewed different categories of telestroke program stakeholders (e.g., stroke coordinators, ED physicians) who may have different perspectives on telestroke implementation. Third, we found that robust assimilators were more likely to have a highly protocolized workflow, but it is possible that the protocol itself is not the mechanism for effective assimilation; rather, sites with robust processes of care and strong organizational cultures that enable assimilation are more likely to rely on protocols. Fourth, hub representatives helped identify EDs that varied with respect to assimilation. It is possible that this recruitment method introduced selection bias. For example, hub representatives may have selected EDs with stronger ties to the hub and greater willingness to participate in research.
Grant support
This research was supported by a grant from National Institute of Neurological Disorders and Stroke (R01NS111952)
Our findings reveal that assimilation can be an ongoing challenge even among established programs. The differences across robust and low assimilators that we identified, and the strategies presented here may be useful to programs that aim to increase telestroke utilization.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Work performed: RAND Corporation and Harvard Medical School
References
- 1.Totten AM, Hansen RN, Wagner J, et al. Telehealth for Acute and Chronic Care Consultations. Rockville, MD: Agency for Healthcare Research and Quality;2019. [PubMed] [Google Scholar]
- 2.Schwamm LH, Holloway RG, Amarenco P, et al. A review of the evidence for the use of telemedicine within stroke systems of care: a scientific statement from the American Heart Association/American Stroke Association. Stroke. 2009;40(7):2616–2634. [DOI] [PubMed] [Google Scholar]
- 3.Man S, Xian Y, Holmes DN, et al. Association Between Thrombolytic Door-to-Needle Time and 1-Year Mortality and Readmission in Patients With Acute Ischemic Stroke. Jama. 2020;323(21):2170–2184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Adeoye O, Nyström KV, Yavagal DR, et al. Recommendations for the Establishment of Stroke Systems of Care: A 2019 Update. Stroke. 2019;50(7):e187–e210. [DOI] [PubMed] [Google Scholar]
- 5.Sharma R, Zachrison KS, Viswanathan A, et al. Trends in Telestroke Care Delivery: A 15-Year Experience of an Academic Hub and Its Network of Spokes. Circulation Cardiovascular quality and outcomes. 2020;13(3):e005903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Akbik F, Hirsch J, Chandra R, et al. Telestroke—the promise and the challenge. Part one: growth and current practice. Journal of neurointerventional surgery. 2017;9(4):357–360. [DOI] [PubMed] [Google Scholar]
- 7.Zachrison KS, Boggs KM, M Hayden E, Espinola JA, Camargo CA. A national survey of telemedicine use by US emergency departments. Journal of telemedicine and telecare. 2018:1357633X18816112. [DOI] [PubMed] [Google Scholar]
- 8.Richard JV, Wilcock AD, Schwamm LH, et al. Assessment of Telestroke Capacity in US Hospitals. JAMA neurology. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Panzano PC, Sweeney HA, Seffrin B, Massatti R, Knudsen KJ. The assimilation of evidence-based healthcare innovations: a management-based perspective. The journal of behavioral health services & research. 2012;39(4):397–416. [DOI] [PubMed] [Google Scholar]
- 10.Newby KV, Parsons J, Brooks J, Leslie R, Inglis N. Identifying strategies to increase influenza vaccination in GP practices: a positive deviance approach. Family practice. 2016;33(3):318–323. [DOI] [PubMed] [Google Scholar]
- 11.Rose AJ, McCullough MB. A practical guide to using the positive deviance method in health services research. Health services research. 2017;52(3):1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lawton R, Taylor N, Clay-Williams R. Positive deviance: a different approach to achieving patient safety. BMJ Quality & Safety.23:880–888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Haverhals LM, Sayre G, Helfrich CD, et al. E-consult implementation: lessons learned using consolidated framework for implementation research. The American journal of managed care. 2015;21(12):e640. [PMC free article] [PubMed] [Google Scholar]
- 14.Hadjistavropoulos H, Nugent M, Dirkse D, Pugh N. Implementation of internet-delivered cognitive behavior therapy within community mental health clinics: a process evaluation using the consolidated framework for implementation research. BMC psychiatry. 2017;17(1):331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation science. 2009;4(1):50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Forman JH, Robinson CH, Krein SL. Striving toward team-based continuity: provision of same-day access and continuity in academic primary care clinics. BMC health services research. 2019;19(1):145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Miles MB, Huberman AM, Saldaña J. Qualitative data analysis: A methods sourcebook. 3rd. ed: Thousand Oaks, CA: Sage; 2014. [Google Scholar]
- 18.Averill JB. Matrix analysis as a complementary analytic strategy in qualitative inquiry. Qualitative health research. 2002;12(6):855–866. [DOI] [PubMed] [Google Scholar]
- 19.Lambert-Kerzner A, Maynard C, McCreight M, et al. Assessment of barriers and facilitators in the implementation of appropriate use criteria for elective percutaneous coronary interventions: a qualitative study. BMC cardiovascular disorders. 2018;18(1):164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sørensen T, Dyb K, Rygh E, Salvesen R, Thomassen L. A qualitative description of telemedicine for acute stroke care in Norway: technology is not the issue. BMC health services research. 2014;14(1):643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Singh R, Mathiassen L, Switzer JA, Adams RJ. Assimilation of web-based urgent stroke evaluation: a qualitative study of two networks. JMIR medical informatics. 2014;2(1):e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoffman JR. Should physicians give tPA to patients with acute ischemic stroke? Against: and just what is the emperor of stroke wearing? The Western journal of medicine. 2000;173(3):149–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Radecki RP. Skepticism about thrombolytics in stroke is not unreasonable. Nature Reviews Neurology. 2012;8(3):176–176. [DOI] [PubMed] [Google Scholar]


