Abstract
HIV stigma has a profound impact on clinical outcomes and undermines the quality of life of people living with HIV (PLWH). Among HIV-negative individuals, misinformation and prejudicial attitudes about HIV can fuel stigma and contribute to discrimination against PLWH. Antenatal care (ANC), with its focus on universal HIV testing, provides a unique entry point to address HIV stigma. This study describes the development of a counseling intervention to address HIV stigma among women and their partners attending a first ANC appointment in Tanzania. Formative work to inform the intervention consisted of qualitative interviews with 32 pregnant and postpartum women (both women living with HIV and HIV-negative women) and 20 healthcare workers. Data were analyzed iteratively, using a thematic analysis approach, to identify intervention targets. The resulting intervention, Maisha (Swahili for “Life”), includes three sessions informed by the HIV Stigma Framework and Cognitive-Behavioral Therapy: a video and brief counseling session prior to HIV testing and, for those who test seropositive for HIV, two additional sessions building on the video content. A pilot test of the intervention is in process. Addressing HIV stigma at the first ANC visit can help individuals living with HIV to overcome stigma-related barriers to the initiation and maintenance of HIV care, and can reduce stigmatizing attitudes among those who test negative for HIV.
Keywords: Antiretroviral therapy (ART), HIV testing and counseling (HTC), Option B+, prevention of mother-to-child transmission of HIV (PMTCT), stigma reduction
INTRODUCTION
Antenatal care (ANC) is a critical entry point for HIV prevention and treatment, with the potential to contribute to a sustainable approach to eliminating HIV/AIDS. Through robust programs that target prevention of mother-to-child transmission (PMTCT) of HIV, countries with generalized HIV epidemics have achieved nearly universal HIV testing for pregnant women, and have drastically reduced infant HIV infections (World Health Organization, 2017). The long-term success of PMTCT depends on women’s engagement in care throughout the pregnancy and postpartum periods (Psaros et al., 2015). Multiple studies have highlighted the impact of HIV stigma on PMTCT care engagement, namely the role of stigma in impeding timely diagnosis, ART initiation and adherence, and disclosure to others for ongoing support (Buregyeya et al., 2017; Gesesew et al., 2017). Stigma is a persistent barrier to the utilization of HIV/AIDS services, which impedes the UNAIDS 90–90-90 initiatives to test, diagnose and treat all people living with HIV (Bajunirwe et al., 2018). Directly addressing HIV stigma at the time when women enter ANC has the potential to enhance the impact of PMTCT programs by facilitating linkage and retention in care, which in turn can help improve the well-being of pregnant women living with HIV (Grossman & Stangl, 2013).
According to Tanzania’s PMTCT guidelines, women are tested for HIV during their first ANC appointment, initiate antiretroviral therapy (ART) immediately upon diagnosis, and then receive PMTCT care in the ANC clinic throughout pregnancy (Tanzania Ministry of Health and Social Welfare, 2013). However, data in Tanzania demonstrate that a significant proportion of women do not return to PMTCT care in the clinic where they are diagnosed with HIV. A medical record review across PMTCT sites in Moshi, Tanzania found that, among 468 women who were diagnosed with HIV during their first ANC visit, 109 (23%) never returned to that clinic for PMTCT care and were considered lost to follow-up (Mazuguni et al., 2019). Similarly, in a systematic review and meta-analysis of PMTCT studies in Africa, a majority of loss to follow-up occurred in the first six months after initiation of care (Knettel et al., 2018). Studies suggest that a primary reason for dropping out of care or silently transferring to another facility is HIV stigma (Ford et al., 2017; Knettel et al., 2018; McMahon et al., 2017). Stigma that is expected from or perpetuated by a male partner is of particular importance to women enrolled in PMTCT programs. Women often rely on male partners for social and financial support in this setting, and fear of abandonment by a partner, especially during pregnancy, may lead to hiding one’s HIV status and avoiding HIV care engagement (Clouse et al., 2014; Watt et al., 2019). Together, these data support a recommendation of early counseling of pregnant women living with HIV, with a focus on stigma, to increase uptake of PMTCT services at the clinic where they initially present for care.
Targeting an HIV stigma intervention to individuals entering ANC has the additional impact of addressing HIV stigmatizing attitudes in the community. The apprehension of HIV testing introduces heightened emotions which, according to stress activation theory, offers a teachable moment that may lead to changes in attitudes and behavior (Eaton et al., 2011; Lawson & Flocke, 2009). Addressing the deeply personal side of HIV during the pre-test period can lead to what Goffman calls “wise” individuals who are actively supportive of members of a stigmatized group (Goffman, 1963). Studies suggest that even brief health behavior messages delivered during HIV testing can have long-term impacts on attitudes and behaviors (American Psychological Association, 2014; Eichler et al., 2002). HIV stigma reduction interventions have shown promise in reducing stigma among people living with HIV, though evidence of the impact of these interventions is scarce(Andersson et al., 2020; Barroso et al., 2014; Kemp et al., 2019). Technology-based HIV interventions have potential to reduce HIV stigma promote HIV prevention behaviors, and should be studied further for their potential reach and scalability (Noar et al., 2009; Relf et al., 2015)
To address the challenge of HIV stigma in ANC, we developed Maisha (Swahili for “Life”), a video-assisted counseling intervention for pregnant women and their male partners. Maisha is a three-part intervention led by trained counselors, which aims to reduce HIV stigma among the general population and promote HIV care engagement among women living with HIV. This study describes the formative research that informed the design of Maisha; a pilot randomized control trial of the Maisha intervention was initiated in April 2019 in two ANC clinics in Northern Tanzania (ClinicalTrials.gov, NCT03600142).
METHODS
Study Site
The study was conducted in two urban health clinics in Moshi, Tanzania where ANC and PMTCT services are provided. The two clinics together see approximately 2500 pregnant women for antenatal care each year, with approximately 120 (4.8%) infected with HIV. Women are strongly encouraged to attend the first antenatal care appointment with the father of the child, and approximately 60% are accompanied by a male partner to the first appointment. Upon presenting for ANC, women and their partners both receive routine HIV Testing and Counseling (HTC). Those who test positive are offered additional post-test counseling and education, immediately connected to the appropriate HIV service within the clinic (PMTCT for pregnant women and the adult HIV Care and Treatment Center for male partners), and provided with antiretroviral therapy for same-day initiation of treatment.
Study Overview
The formative data presented here reflect the process of intervention development for Maisha, prior to the initiation of a pilot randomized control trial. The intervention development was conducted in three phases: 1) development of an intervention model based on a conceptual framework, 2) formative data to inform the intervention content and delivery modality, and 3) intervention refinement by iteratively piloting preliminary versions. The overall goals of the intervention were to: reduce stigmatizing attitudes among HIV-negative individuals; mitigate HIV stigma (internalized and anticipated) among individuals living with HIV; and promote retention in PMTCT.
Phase 1: Conceptual foundation for preliminary intervention development.
The development of Maisha was informed by an earlier formative study, “Postpartum HIV Care Engagement in the Context of Option B+ in Tanzania” (NIH Grant R21 AI124344). The study involved retrospective reviews of existing data and literature, structured observations to assess the clinic-level implementation of Option B+, qualitative interviews with patients, healthcare workers, and program administrators, and enrollment of a cohort of 200 women living with HIV and enrolling in PMTCT care during pregnancy in Tanzania.
As we began our program of research, we conducted a systematic review and metaanalysis of care engagement under Option B+ policies in Africa, where we observed that 27% of women were lost to follow-up (LTFU) within six month of initiating HIV care in PMTCT, rates which are higher than the general population of people living with HIV (PLWH) (Knettel et al., 2018). We then conducted a review of Tanzanian clinic data in the first year of Option B+ implementation, and found that 59% of women in PMTCT were LTFU by two years postpartum (Cichowitz et al., 2018). We conducted clinic-level observations that identified several factors that could be driving these high rates of LTFU, including limitations in healthcare worker training, staff shortages, high patient volumes, and a high burden of record-keeping for clinic nurses (Chumba, 2018). In our cohort of HIV-infected pregnant and postpartum women, participants reported high rates of depression and anxiety, internalized shame/stigma, and fears of abandonment (Minja et al., 2019; Ngocho et al., 2019) which hindered HIV disclosure, influenced attitudes toward ART, and contributed to substandard care engagement (Knettel et al., 2019; Watt et al., 2018). Additional findings from the Option B+ study are presented in Table 1.
Table 1.
Formative research findings informing the Maisha intervention
| Author(s) and Year | Objectives | Key Findings |
|---|---|---|
| Knettel et al., 2018 | • Examine rates and predictors of loss to follow-up (LTFU) in PMTCT in Africa via systematic review and meta-analysis of 35 studies | • 10% LTFU after first appointment and 27% LTFU 6 months after initiation; greater LTFU than general pop. of PLWH • Stigma, fear of disclosure, and low social support were key drivers of LTFU |
| Cichowitz et al., 2018 | • Review medical records assessing LTFU following the introduction of Option B+ in Tanzania | • Two years after delivery, 58.7% were LTFU • High LTFU occurred across the PMTCT continuum, including immediately after enrollment in ANC and in the postpartum period • Individuals newly diagnosed with HIV were more likely to be LTFU |
| Chumba, 2018 | • Evaluate facility-level implementation of Option B+ at clinics in northern Tanzania | • Challenges at clinic level included lack of provider training, high patient volumes, and record-keeping burden, leading to decreased provider-patient interaction |
| Ngocho et al., 2019 | • Assess prevalence and predictors of depression among women in PMTCT | • 25% of women met criteria for possible depression and 14% endorsed thoughts of self-harm/suicide • Internalized shame/stigma, food insecurity, and being single were all significantly associated with depression |
| Minja et al., 2019 | • Identify predictors of attitudes related to long-term use of ART | • Negative attitudes about ART were linked to depression, internalized shame/stigma, and lack of HIV acceptance |
| Knettel et al., 2019 | • Explore patterns and predictors of HIV disclosure among women in PMTCT | • Among women diagnosed during pregnancy, 20% had not disclosed to anyone at 3 months postpartum and 44% had not disclosed to the father of the child • Fears of stigma and abandonment drive non-disclosure |
| Watt et al., 2018 | • Examine rates and predictors of poor care engagement in cohort of 200 Tanzanian women in PMTCT | • 21% had poor care engagement at 6 months postpartum • Poorer engagement among patients who were younger, who had not disclosed status, and were newly diagnosed |
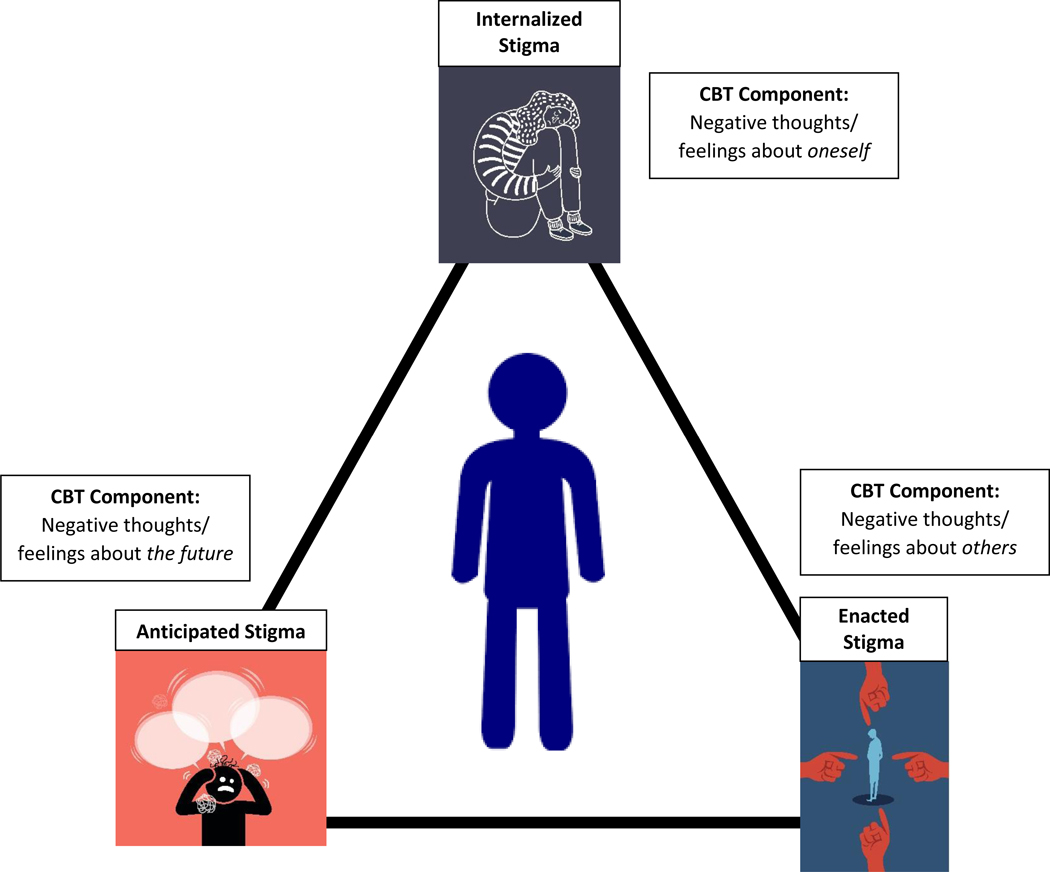
To conceptualize the various aspects of stigma, we used Earnshaw and Chaudoir’s (2009) HIV Stigma Framework, which emphasizes the unique experiences of stigma among PLWH and describes the various stigmatizing attitudes and behaviors that contribute to the experience of stigma. In the general public, stigma exists in the form of discriminatory or prejudicial behavior that is driven by negative attitudes about PLWH. This may include beliefs that HIV is due to immoral behavior or personal weakness, discomfort or desire to avoid PLWH, fear of transmission driven by misinformation, and outward shunning or mistreatment of PLWH (Turan et al., 2011; Maretha J. Visser et al., 2008). Among PLWH, the Framework identifies three components of HIV stigma: internalized (negative beliefs and feelings about oneself), enacted (actual prejudice and discrimination from others), and anticipated stigma (fear of mistreatment that may occur if one’s status becomes known) (Earnshaw & Chaudoir, 2009).
As we sought to integrate our prior data collected with women in ANC into the HIV Stigma Framework, we observed that Earnshaw and Chaudoir’s three components of stigma track onto the cognitive behavioral therapy (CBT) ‘cognitive triad’ (Beck & Rush, 1979). Internalized stigma is closely associated with negative thoughts, feelings, and beliefs about oneself, anticipated stigma is associated with negativity about the future, and enacted stigma leads to negativity about others/the world. By increasing self-awareness of these patterns of thought and increasing cognitive flexibility, the burden of stigma may be reduced. Thus, we designed the Maisha intervention to address these three forms of stigma using principles of CBT, informed by a prior stigma reduction intervention conducted with women living with HIV in South Africa (Tshabalala & Visser, 2011). To encourage long-term HIV care engagement, we also utilized Third Wave behavioral concepts stemming from Acceptance and Commitment Therapy to foster a sense of personal acceptance and motivate value-driven behavior (Hayes et al., 2006; Hunot et al., 2013).
Another key consideration for the development of the intervention was to ensure future scalability, given the limited resources in the clinic and the high volume of ANC patients. We aimed to make use of existing/available resources in the Tanzanian setting and explore acceptability among key stakeholders, including healthcare workers and patients. We therefore chose to develop the intervention as a video-assisted counseling session prior to HIV testing; we hypothesized this would be a scalable approach, as it could be easily administered to a group of patients (e.g., in a clinic waiting room), would require little material investment, and could be overseen by existing clinic staff with minimal time commitment. The counseling content was designed with the long-term goal of integration into existing clinic appointments.
Phase 2: Formative data collection to inform intervention content.
Next, the preliminary model for the intervention was assessed, expanded, and revised based on qualitative interviews and focus group discussions with a range of stakeholders (Table 2). Women living with HIV were recruited from our previous research cohort of pregnant and postpartum women living with HIV. HIV-negative women were recruited among patients attending antenatal care in the two study clinics, and healthcare providers and home-based care workers were recruited among employees at the two study clinics. Data collection was conducted by Tanzanian members of the research team who had training in qualitative methods and were involved in the development of the Maisha intervention. The interview guide was informed by our research objectives and our literature review. The guides were tailored to each population group; they explored HIV testing and counselling experiences, elicited individual and community perceptions of PLWH, and sought recommendations for addressing HIV stigma. Participants living with HIV were asked about their own experiences with and fears of stigma.
Table 2.
Qualitative data collection to inform the intervention development
| Participant group | n |
|---|---|
| Women living with HIV | |
| Pregnant (newly diagnosed) | 7 |
| Pregnant (established diagnosis) | 4 |
| Postpartum (newly diagnosed) | 4 |
| Postpartum (established diagnosis) | 5 |
| HIV-negative women | 12 |
| Healthcare workers | 7 |
| Home based care workers | 13* |
Across two FGDs
The qualitative data were analyzed iteratively by the research team; discussions identified emerging content and areas for exploration in subsequent interviews. Analysis was conducted using applied thematic analysis (Guest et al., 2012). Transcripts were coded thematically in NVivo 12 across the broad domains of our research (drivers of stigma, manifestations of stigma, and opportunities for stigma reduction). Coded content was reviewed by multiple readers and consensus discussion led to the identification of major themes in each domain. The coding process was then repeated to apply the thematic codes. Qualitative memos were written for each domain and population group in order to synthesize the data and make comparisons across population groups (Birks et al., 2008).
Phase 3: Refinement of intervention through an iterative process.
The study team from the U.S. and Tanzania met regularly to discuss the emerging findings and develop the framework for the intervention. A study advisory board was convened to review the findings and provide input on the intervention design, including the video script. The study advisory board included representatives from the council health management team (CHMT), leadership in the study clinics, local non-governmental organizations, and representatives from the Kilimanjaro Christian Medical Center (KCMC) Hospital’s community advisory board (CAB) for HIV trials. The study advisory board meeting resulted in a more refined iteration of the intervention. The revised intervention content was discussed in a workshop with clinic staff and in a half day meeting with members of the KCMC CAB. These meetings resulted in a full script for the video, along with session counseling content. The Maisha video was recorded in Moshi, with characters portrayed by individuals recruited from the CAB who were highly knowledgeable about HIV.
Ethics
The study was approved by the ethical review boards of Duke University, University of Utah, Kilimanjaro Christian Medical Centre, and the Tanzanian National Institute for Medical Research. All human subjects who participated in-depth interviews and focus group discussions provided written informed consent and received compensation for time and travel (5,000 Tanzanian Shillings; approximately 2 US dollars).
RESULTS
Qualitative Data
The qualitative exploration revealed key drivers and manifestations of HIV stigma in the community, as well as internalized stigma (i.e., feelings of shame) among those who were living with HIV (Table 3). Notably, women living with HIV described limited experiences of enacted stigma, but significant fears related to anticipated stigma. They feared negative responses from family members, their male partner, or broader social circle if their HIV status were to become known. This fear led to highly selective disclosure and disruptions in their PMTCT care engagement and medication adherence (e.g., missed clinic visits due to fear of being seen at the clinic, inability to explain absences from work or home, missed doses due to inability to take pills discretely).
Table 3.
Key findings from the qualitative research
| Drivers of stigma | ||
|
Fear of HIV infection HIV associated with moral weakness HIV associated with death |
“Even If they were seated close together they would move so as to make sure there is no contact… Contact seems to them as contamination.” (HIV-negative woman) | |
| “To them (the community), when they see someone has become thin, they don’t even think that maybe they are stressed/depressed, or why the child hasn’t gone to school or the child didn’t pass the exams. They just say they are done, they have ‘ngoma’ (an informal word for HIV).” (Woman living with HIV) | ||
| Manifestations of stigma | ||
|
Gossip Isolation Change in relationship status |
“They arrived home, and the stigma started with the husband. The husband started to stigmatize her. He told her, “I don’t want to see you in my home anymore. Go to your parent’s house. To this day, I haven’t seen that lady return to the clinic…” (Clinic nurse) | |
| Internalized stima | ||
|
Feelings of otherness Sense of failure Suicidal ideation |
“I had no peace, I was saying to myself I am dying...I don’t know about the baby in my womb, how will it be...I am dying with (the baby).” (Woman living with HIV) | |
| Anticipated stigma | ||
|
Fear of social isolation Fear of blame and judgment Leads to non-disclosure |
“We don’t advise you to share the information with everybody. Because some of the people cannot keep secrets. You might share the news with that person and then she turns it into an announcement. You just look for someone whom you can trust with your secrets.” (Clinic nurse) | |
| Opportunities to address stigma | ||
|
HIV normalization Education Role models |
“[The clinic] made me who I am now; they said don’t think that it’s only you...there are beautiful women here when you see them you won’t believe it.” (Woman living with HIV) | |
| “I will give you an example of the diabetic patients who take pills every day – HIV patients think that they are the only patients who take pills every day, but there are diabetic and hypertensive patients who take their medications every day.” (Healthcare worker) | ||
Across all population groups, the perceived drivers of community-level HIV stigma included a fear of infection, which was primarily related to misinformation about HIV transmission, and fear of infection through casual contact. Negative associations of HIV with moral and physical weakness (sexual promiscuity, sickness and death) also emerged as drivers of stigma. Participants noted that enacted stigma most commonly manifested itself as unkind gossip about people living with HIV and their families, social isolation, and dissolution of relationships with partners. There were reports of rare cases of other serious forms of enacted stigma including intimate partner violence and public humiliation. When asked for recommendations on addressing HIV stigma, participants most frequently suggested providing community members with education about HIV (namely on transmission) and normalizing the idea of HIV as a clinical condition.
Women living with HIV were asked about their experiences learning their HIV status. Almost all participants described feeling overwhelmed and unprepared upon receiving their HIV diagnosis. Although they felt generally supported by the clinic nurses who provided their diagnosis, they typically felt unable to ask questions or express concerns due to the shock of the news. Participants described counseling in subsequent encounters as brief and largely didactic, with little opportunity to explore perceived challenges. Several participants noted that the most impactful message they received from providers was that they could live a long and normal life, including sharing stories of other patients who are living normal lives with HIV; similarly, seeing other patients at the HIV clinic was often a source of hope and social support, and these encounters mitigated the sense of social isolation.
Stakeholder Feedback
The study advisory board was convened for a half-day meeting to elicit stakeholder feedback on the intervention content. The research team shared both the conceptual model for the intervention, as well as findings from the qualitative data collection. Overall, the study advisory board members felt that the proposed intervention model to address HIV stigma in the clinic would have positive impacts for individuals living with HIV as well as the general population, and that it would complement the existing standard of care. During the meeting, participants split into small groups and were tasked with developing a storyline for the video. Groups reconvened and consensus was reached on some key messages that should be included in the video: normalize anxieties about HIV testing and HIV diagnosis while making connections between HIV and other chronic illnesses, celebrate pregnancy and childbirth, develop empathy for people living with HIV, acknowledge the roles of the partner and other family members, and show that there is hope for the future if diagnosed with HIV.
A primary area of discussion in the study advisory board workshop was the opportunity to include male partners in the intervention. It was noted that women are advised to bring their male partners to the first ANC appointment to participate in couple’s HIV testing, and about half of women present with a male partner. The group came to the consensus that male partners should be included in the intervention based on two rationale: 1) it takes advantage of an opportunity to address HIV stigmatizing attitudes among men, and 2) it may improve the outcomes for women if their male partners are also participating. Based on this input, the study team revised the intervention content and the study protocol (including an amendment to the ethical review committee) to include male participants in the intervention.
Resulting Maisha Curriculum
The resulting intervention consisted of three counselor-facilitated intervention sessions that are conducted with the woman, either alone or with her partner. The first video-assisted session is presented to all women and accompanying male partners at the first ANC visit, prior to HIV testing. If the woman or her partner tests seropositive for HIV, both immediately return to the counselor for an additional counseling session, and a third session (for the woman only) is provided two weeks later. The intervention has two overarching goals:
Reduce HIV stigmatizing attitudes among patients who learn that they are HIVnegative.
- Address internalized and anticipated stigma among those who are living with HIV, specifically:
- If newly diagnosed, mitigate internalized and anticipated stigma, which prepares them to accept their HIV status and engage in PMTCT care.
- If established diagnosis, address internalized and anticipated stigma that may interfere with care engagement.
In order to respond to the various scenarios of presentation at ANC (presenting with or without a partner; presenting with a known HIV status or not), we developed several variations of each guide to be responsive to the participants’ unique situation. The curriculum was designed for delivery by lay counselors who were not health care providers and did not necessarily have formal training in mental health but may have some background in counseling.
Session 1: Video-assisted counseling.
Upon enrollment, women (alone or with their partners) watch an 8-minute video addressing stigma and care engagement in the context of antenatal care. The video depicts Salma and Bahati, a couple who both test positive for HIV during a first ANC visit. After experiencing some initial distress and disbelief, the couple receives counseling and support from a clinic nurse. They then decide to disclose to Bahati’s mother, who lives with them. Both Salma and Bahati commit to taking daily ART and Salma gives birth to a child who is HIV-negative.
Throughout the video, there is a distinct emphasis on the normalization of PLWH; namely, that PLWH are just like anyone else and are valued members of the community. The video demonstrates that disclosure of one’s status to a small circle of trusted family members and friends can assist with self-acceptance of a diagnosis and build social support for long-term care engagement. An additional key message is that, with early and consistent adherence to medication, PLWH can live a long, healthy life and give birth to an HIV-negative child. The video includes several scenes of the normal daily lives of Salma and Bahati (e.g., the child playing with neighbors and the family sharing a meal), which is meant to elicit a sense of hope for the future.
The role of Bahati’s mother in the film is also important to note. In Tanzanian culture, the husband’s mother is often a highly respected figure, and women typically stay with their motherin-law after giving birth. In the qualitative interviews, women living with HIV frequently expressed concern about how their mother-in-law will respond. In this instance, the mother-in-law responded with kindness and support. This scenario is meant to challenge a viewer’s automatic thoughts that a response to a disclosure will be negative. In one scene, the mother-in-law takes her hypertensive medication as Salma and Bahati take their ART, demonstrating that HIV is a chronic illness like any other.
Post-video discussion.
At the conclusion of the video, a counselor leads the viewer(s) in a discussion of the video content, how it may relate to their own situation and attitudes, and how it might inform their attitudes and behavior in the future. The discussion starts by asking the woman (and accompanying partner, if present) about her reaction to various aspects of the video, and relating it to her own experience of HIV testing, as well as her fears and worries about testing. She is asked to imagine what her reaction might be to anHIV diagnosis, and how she might navigate disclosure and social support. For women presenting with a partner, the session content is nearly identical, but the counselors are trained to effectively facilitate a couple-based session. This includes strategies for eliciting equal participation from both partners, recognizing and addressing power differentials, and fostering healthy communication among the partners (Malary et al., 2015).
After reviewing the video, the three components of HIV stigma (internalized, anticipated, enacted) are introduced using a visual model (Figure 1) and discussed from both the perspective of a person living with HIV and others in the community.
Figure 1.
Visual model representing the stigma framework
By drawing parallels between their own experiences and those of Salma and Bahati, patients reduce the sense of distance and ‘otherness’ that can drive stigmatizing attitudes. The counselor also acknowledges that the case of Salma and Bahati represents a very positive outcome, and that each person must make choices based on her individual circumstances. Among women who present to ANC with an established HIV diagnosis, the counselor explores how the woman’s own experience has been similar or different to Salma’s, and additional emphasis is placed on the importance of ART adherence. Among patients with an unknown status, the session concludes with a summary that, if the patient tests seropositive for HIV, there are medications and resources available to help her accept the diagnosis and lead a full, healthy life, and if she tests seronegative for HIV, she can be a positive source of support for PLWH. Session 1, including both the video and counseling content, was designed to take 20 to 30 minutes.
Session 2: Stigma-focused counseling for PLWH.
All participants are asked to return to the counselor after HTC to share the results of their HIV test. If both the woman (and her partner, if present) test seronegative, the counselor gives a brief reminder linking back to the video content and encourages them to reduce community stigma toward PLWH through kindness and support. If the woman and/or her partner indicate that they tested seropositive (or entered ANC with an established HIV diagnosis), the counselor introduces Session 2.
The goal of Session 2 is to link back to the video content, address immediate stigma-related concerns, and foster commitment to initiate and/or continue treatment. For a woman who tested seropositive, the goal is to have her return for her next scheduled follow-up appointment for PMTCT. For a male partner who tested seropositive, the counselor helps him to prepare to link to the HIV care and treatment center (CTC) in the same clinic in order to begin HIV care. The stigma visual (Figure 1) is used to discuss how issues of internalized, anticipated and enacted stigma might relate to their situation of living with HIV, and to try and reduce these as barriers of HIV care engagement.
A key finding from our qualitative data was that women who received a new HIV diagnosis did not feel like they had the time or space to adequately process their feelings with the provider before they left the clinic. Therefore, an important goal of Session 2 is to support patients in exploring their personal reactions, using the Stigma Framework and cognitive-behavioral principles as guides. For example, participants are encouraged to share their personal (internalized) feelings, their fears about what comes next (anticipated) and how they might be treated if they disclose their status to others (enacted). If the couple has discordant HIV test results, then the counselor will help the seronegative individual to develop empathy and commitment to provide support to the seropositive individual.
The counselor introduces the concept that, when the mind is in a troubled or worried state, we tend to expect the worst possible outcome. However, the reality of a situation is often not nearly so bad. This concept is then used to consider the possibility of seeking support for one’s diagnosis by disclosing her status to another person. Together, the counselor and participant consider who that person might be, how they might respond, and the potential risks and benefits of disclosure. The counselor clearly communicates that disclosure is not always the best choice and decisions to disclose should be made carefully, but that disclosure to a trusted individual can be an important pathway to receiving social support for HIV.
To address the issues of ART adherence and care engagement, the participant is guided to list her personal values. These often include a desire to be a good mother, daughter, and spouse, to support her family, to advance in her career, and to live according to her faith. The counselor notes that the HIV diagnosis is unchangeable, and therefore acceptance of the HIV is an important goal for the future. Next, the counselor asks, “How do the next steps of coming to the clinic and taking medication relate to the values you just described?” Together, the counselor and participant then connect each of the listed values to HIV care engagement. To conclude the session, the counselor seeks a commitment from the patient to start the medication (or continue medication for individuals with an established HIV diagnosis) and return to the clinic in two weeks for her next clinic appointment and the final counseling session. On average, session 2 was designed between 30 and 50 minutes, because it requires more in-depth discussion and reflection compared to session 1. Session duration will depend on the nature of the participant (and her partner, if present) and the level of distress due to the HIV diagnosis.
Session 3: Follow-up counseling for women living with HIV.
The goal of the third and final session for women living with HIV is to provide continued assistance in managingstigma, foster a longer-term commitment to PMTCT care, and develop a plan for overcoming barriers to care. There is also an emphasis on extending the knowledge and skills from Maisha into one’s daily life.
Session 3 begins with the counselor checking in with the participant on her initiation of ART and her adherence since the previous session two weeks ago. If the participant has been perfectly adherent, the counselor congratulates her and briefly reiterates the importance of ART in achieving PMTCT goals and supporting her identified values. If the participant reports lapses in adherence, they engage in a more detailed conversation exploring barriers to adherence and weighing these against potential benefits and personal values. The counselor is trained to recognize and accept ambivalence, and to acknowledge that such changes can be challenging.
Next, a similar conversation occurs surrounding HIV disclosures and any experiences of enacted stigma. Participants are encouraged to challenge their own perspectives by considering the questions, “If someone you cared for very much had HIV and they were struggling with it, but kept silent, how would you feel? Would you want to know? How would you respond if they did tell you?” Reports of enacted stigma are normalized by the counselor, who expresses that other people may be experiencing shock, sadness, or anger at hearing the patient’s diagnosis, which are the same emotions that the patient herself may have felt. Just as she is learning to be more accepting of her diagnosis, perhaps her family and friends will come to accept it as well.
If the participant has not experienced enacted stigma, but is reporting strong feelings of anticipated stigma, these same concepts are explored, along with reminder of the CBT content from Session 2 – that our expectations of what might occur are often worse than the reality of the situation. The counselor explains that when disclosures are carefully considered and made to a small circle of trusted people, they tend to enhance social support and contribute to positive health outcomes. At this stage, women with established HIV diagnoses are asked to consider whether they might engage with networks of people living with HIV, either through local non-governmental organizations or through personal connections. Women who express interest are then engaged in a conversation about how they might proceed with this goal, which could lead to a sense of advocacy and empowerment to address community-level stigma.
Additional Third Wave cognitive behavioral concepts are introduced in Session 3, including the acceptance of worry as a normal response to life’s challenges. The stigma visual (Figure 1) is used again to make a point that one’s feelings (internalized stigma) and thoughts (anticipated stigma) are connected. Participants are introduced to the idea that “it is the mind’s job to worry” to protect people from danger, but that this worry does not necessarily reflect the positive reality of what might occur. To demonstrate this point, the facilitator refers back to the video, reminding the participants that Salma and Bahati experienced significant worry about disclosing their status to Bahati’s mother, and then she ended up accepting them. The session also introduces the concept that a calm, healthy body will support a calm, healthy mind and vice versa. Participants are encouraged to support their physical health by sleeping and eating well, staying physically active, and doing the things they enjoy. The counselor leads the participant in a relaxation breathing exercise to reinforce the concept of “healthy mind, healthy body”, and the participant is encouraged to practice the exercise at home.
Finally, the counselor and participant consolidate the components of Maisha into an individualized action plan. For all participants, this begins with the importance of committing to and maintaining consistent HIV care engagement and ART adherence. They make a plan for building or maintaining social support, either through conversations with people who already know their status, new disclosures to people they trust, or engaging with other patients at the clinic. The counselor and patient review the aspects of stigma that are most troubling to them, how they relate to personal values, and how they may be addressed moving forward. Finally, they review plans for personal coping by adopting healthy lifestyle changes. The intervention concludes with the counselor congratulating the participant for coming to the clinic and investing in her future and the future of her child. Similar to session 2, session 3 was designed to last between 30 and 50 minutes.
DISCUSSION
While the urgency of initiating pregnant women living with HIV on lifelong ART is clinically justified, women are often not ready to accept their status and to commit to lifelong treatment (Katirayi et al., 2016; McLean et al., 2017). Our research suggests that, after HIV diagnosis, some women never return to the clinic where they initially presented for ANC, and that others drop out of care or silently transfer to another clinic due to perceived stigma (Knettel et al., 2018; Mazuguni et al., 2019). The formative data we collected to inform this intervention is consistent with other literature; there is an “othering” of people living with HIV, which manifests itself in social distancing and moral judgment (de Vries et al., 2011; Petros et al., 2006; Tsai et al., 2013; Van Breda, 2012). The anticipation of stigmatizing reactions leads women living with HIV to conceal their status and avoid care where they may be identified as living with HIV (Buregyeya et al., 2017).The decision of care site should be a woman’s choice, but stigma should not drive women to attend a clinic that is potentially less convenient and less familiar.
The Maisha intervention uses strategies shown to be effective in prior stigma reduction research by targeting the attitudinal drivers of stigma, while also addressing stigma during a critical period when women are making decisions about HIV care behaviors (Kemp et al., 2019). By addressing stigma when attitudes toward one’s HIV status are still forming (for new diagnoses) or at a critical juncture of pregnancy (for established diagnoses), we can promote healthy decision-making and facilitate readiness to initiate and/or maintain ART, establishing the foundation for lifelong care engagement. As HIV universal test-and-treat policies become more common (Kulkarni et al., 2013; Wringe et al., 2017), this intervention can offer lessons for promoting readiness for ART in the general population.
In addition, the Maisha intervention has the potential to reduce broader community stigmatizing attitudes that undermine both the emotional and physical well-being of people living with HIV. Antenatal care is a catchment point for not only pregnant women, but also their male partners. Research has suggested that men often have higher HIV stigmatizing attitudes (Treves-Kagan et al., 2017; M. J. Visser et al., 2009); this intervention offers an opportunity to address the men’s beliefs, attitudes and practices in relation to people living with HIV. The routine HIV testing experience potentially offers a moment when individuals are prime to change their perceptions, as they themselves are considering the possibility of an HIV diagnosis. Given the limited evidence base in HIV stigma reduction interventions, and in particular an absence of stigma reduction interventions that can be implemented at the health systems level (Stangl et al., 2013), this model offers the potential to advance our understanding of how HIV stigmatizing attitudes may be addressed in a general population.
The Maisha intervention was designed based on behavioral theory and formative data collected from various stakeholders, and was iterated through input from a study advisory board. Nevertheless, the resulting intervention has some potential limitations, particularly as it relates to scalability and integration into a clinical setting. The intervention was intentionally designed to be brief, but we know that even an additional 15-minute contact with patients can be untenable for healthcare providers who are already stretched beyond their limits. In the pilot test of the intervention, delivery will happen by study-trained facilitators whose primary job will be delivery of the intervention. This was necessary to control intervention fidelity and coverage, but it is not a sustainable approach. If Maisha is found to be effective, group delivery and additional video-assisted content will be considered in order to integrate the intervention into routine care. In addition, opportunities to extend the stigma reduction intervention beyond the initial ANC visit may help to have longer term impacts on stigma attitudes and HIV care engagement. This could be as simple as introducing posters and other visuals into the clinic, or integrating content into subsequent antenatal and postnatal appointments. The long-term goal should be to create a create a stigma-free environment for women living with HIV, which will require changing community norms and attitudes around HIV.
CONCLUSION
This paper described the development of an HIV stigma reduction intervention that can be integrated into ANC to have impacts on both stigmatizing attitudes among the general population, as well as internalized and anticipated stigma constructs among people living with HIV. The intervention was developed using a theoretical framework and based on formative data collection; it evolved significantly through input from a study advisory board of diverse stakeholders and subsequent community feedback. A pilot feasibility trial of the intervention was initiated in April 2019 (ClinicalTrials.gov, NCT03600142). The trial will produce further evidence on the feasibility and acceptability of the Maisha intervention, as well as its potential impact on HIV stigma constructs and PMTCT care engagement.
HIGHLIGHTS.
Antenatal care is an innovative setting to address community-level HIV stigma.
Men can be reached for HIV stigma reduction in the antenatal care setting.
Acknowledging stigma prior to HIV testing can help mitigate internalized and anticipated stigma.
Acknowledgments
Funding: This project is funded by a grant from the Fogarty International Center at the National Institutes of Health (NIH; R21 TW011053) and a pilot grant from the Duke Center for AIDS Research (P30 AI064518), and based on prior NIH-funded research (R21 AI124344). We also acknowledge fellowship support received from the NIH Office of Behavioral and Social Science Research (OBSSR) and the Fogarty International Center (D43 TW009337).
AUTHOR BIOGRAPHIES
Melissa H. Watt, Ph.D. is an Associate Professor of Global Health at Duke University. She has a program of HIV stigma research in Tanzania and leads the Maisha study together with Dr. Mmbaga.
Brandon A. Knettel, Ph.D. is a postdoctoral fellow at Duke Global Health Institute. He is currently working in Tanzania as a VECD Fogarty Global Health Fellow conducting research on HIV care engagement and mental health treatment.
Elizabeth T. Knippler, BA is a current MPH student at the UNC Gillings School of Global Public Health and previously served as the Maisha study coordinator while at the Duke Global Health Institute.
Godfrey Kisigo, MD is a Tanzanian physician currently pursuing Masters of Science in Global Health at Duke University. His research interests include reproductive health and sustainable models for HIV care.
James Ngocho, MD, MPhil Is an Assistant Lecturer at Kilimanjaro Christian Medical University College with training in medicine and public mental health. A co-investigator on the Maisha study.
Jenny Renju, PhD holds a joint position as an Assistant Professor of Public health at the London School of Hygiene and Tropical Medicine and a Senior Lecturer at Kilimanjaro Christian Medical University college. Her work explores the implementation of HIV policies across sub-Saharan Africa.
Jane Rogathi, RN, PhD is the acting Dean of the Kilimanjaro Christian Medical University School of Nursing. Her research focuses on the gender based violence and birth outcomes.
Saumya S. Sao is an undergraduate student at Duke University studying the intersection of gender and health.
Linda Minja, BSc is a junior statistician at the Kilimanjaro Clinical Research Institute. She assists in the data management and coordination of Maisha study.
Haika Osaki, MPH., is a researcher at the Kilimanjaro Clinical Research Institute. She is currently serving as the study coordinator for the randomized controlled trial of the Maisha intervention.
Rimel N. Mwamba, BA, is a research trainee at the Duke Global Health Institute. Her area of research interest is on HIV disclosure and its impact on HIV outcomes.
Blandina Mmbaga, MD, PhD is a pediatrician at the Kilimanjaro Christian Medical Centre and Director of Kilimanjaro Clinical Research Clinical Institute. She leads the Maisha study together with Dr. Watt.
Footnotes
Competing Interests: The authors declare that they have no competing interests in relation to this research.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- American Psychological Association. (2014). Counseling in HIV Testing Programs. http://www.apa.org/about/policy/counseling.aspx [Google Scholar]
- Andersson GZ, Reinius M, Eriksson LE, Svedhem V, Esfahani FM, Deuba K, Rao D, Lyatuu GW, Giovenco D, & Ekström AM (2020). Stigma reduction interventions in people living with HIV to improve health-related quality of life. The Lancet HIV, 7(2), e129–e140. 10.1016/S2352-3018(19)30343-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bajunirwe F, Tumwebaze F, Akakimpa D, Kityo C, Mugyenyi P, & Abongomera G. (2018). Towards 90–90-90 Target: Factors Influencing Availability, Access, and Utilization of HIV Services—A Qualitative Study in 19 Ugandan Districts. BioMed Research International, 2018, 1–10. 10.1155/2018/9619684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barroso J, Relf MV, Williams MS, Arscott J, Moore ED, Caiola C, & Silva SG (2014). A Randomized Controlled Trial of the Efficacy of a Stigma Reduction Intervention for HIV-Infected Women in the Deep South. AIDS Patient Care and STDs, 28(9), 489–498. 10.1089/apc.2014.0014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, & Rush AJ (Eds.). (1979). Cognitive therapy of depression (13. print). Guilford Press. [Google Scholar]
- Birks M, Chapman Y, & Francis K. (2008). Memoing in qualitative research: Probing data and processes. Journal of Research in Nursing, 13(1), 68–75. 10.1177/1744987107081254 [DOI] [Google Scholar]
- Buregyeya E, Naigino R, Mukose A, Makumbi F, Esiru G, Arinaitwe J, Musinguzi J, & Wanyenze RK (2017). Facilitators and barriers to uptake and adherence to lifelong antiretroviral therapy among HIV infected pregnant women in Uganda: A qualitative study. BMC Pregnancy and Childbirth, 17 10.1186/s12884-017-1276-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chumba LN (2018). Facility-Level Factors Affecting Implementation of the Option B+ Protocol for Prevention of Mother-to-Child Transmission of HIV (PMTCT) in Kilimanjaro, Tanzania. https://dukespace.lib.duke.edu/dspace/handle/10161/17002
- Cichowitz C, Mazuguni F, Minja L, Njau P, Antelman G, Ngocho J, Knettel BA, Watt MH, & Mmbaga BT (2018). Vulnerable at Each Step in the PMTCT Care Cascade: High Loss to Follow Up During Pregnancy and the Postpartum Period in Tanzania. AIDS and Behavior. 10.1007/s10461-018-2298-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clouse K, Schwartz S, Van Rie A, Bassett J, Yende N, & Pettifor A. (2014). “What they wanted was to give birth, nothing else”: Barriers to retention in Option B+ HIV care among postpartum women in South Africa . J Acquir Immune Defic Syndr, 67(1), e12–8. 10.1097/QAI.0000000000000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Vries DH, Galvin S, Mhlanga M, Cindzi B, & Dlamini T. (2011). “Othering” the health worker: Self-stigmatization of HIV/AIDS care among health workers in Swaziland. Journal of the International AIDS Society, 14(1), 60 10.1186/1758-2652-14-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Earnshaw VA, & Chaudoir SR (2009). From conceptualizing to measuring HIV stigma: A review of HIV stigma mechanism measures. AIDS and Behavior, 13(6), 1160–1177. 10.1007/s10461-009-9593-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton LA, Cherry C, Cain D, & Pope H. (2011). A Novel Approach to Prevention for At-Risk HIV-Negative Men Who Have Sex With Men: Creating a Teachable Moment to Promote Informed Sexual Decision-Making. American Journal of Public Health, 101(3), 539–545. 10.2105/AJPH.2010.191791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eichler MR, Ray SM, & del Rio C. (2002). The effectiveness of HIV post-test counselling in determining healthcare-seeking behavior. AIDS (London, England), 16(6), 943–945. [DOI] [PubMed] [Google Scholar]
- Ford D, Muzambi M, Nkhata MJ, Abongomera G, Joseph S, Ndlovu M, Mabugu T, Grundy C, Chan AK, Cataldo F, Kityo C, Seeley J, Katabira E, Gilks CF, Reid A, Hakim J, & Gibb DM (2017). Implementation of Antiretroviral Therapy for Life in Pregnant/Breastfeeding HIV+ Women (Option B+) Alongside Rollout and Changing Guidelines for ART Initiation in Rural Zimbabwe: The Lablite Project Experience. Journal of Acquired Immune Deficiency Syndromes, 74(5), 508–516. 10.1097/QAI.0000000000001267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gesesew HA, Tesfay Gebremedhin A, Demissie TD, Kerie MW, Sudhakar M, & Mwanri L. (2017). Significant association between perceived HIV related stigma and late presentation for HIV/AIDS care in low and middle-income countries: A systematic review and meta-analysis. PloS One, 12(3), e0173928. 10.1371/journal.pone.0173928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goffman E. (1963). Stigma: Notes on the management of spoiled identity. Prentice-Hall. [Google Scholar]
- Grossman CI, & Stangl AL (2013). Editorial: Global action to reduce HIV stigma and discrimination. Journal of the International AIDS Society, 16(3 Suppl 2), 18881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G, MacQueen KM, & Namey EE (2012). Applied Thematic Analysis. SAGE. [Google Scholar]
- Hayes SC, Luoma JB, Bond FW, Masuda A, & Lillis J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. 10.1016/j.brat.2005.06.006 [DOI] [PubMed] [Google Scholar]
- Hunot V, Moore THM, Caldwell DM, Furukawa TA, Davies P, Jones H, Honyashiki M, Chen P, Lewis G, & Churchill R. (2013). “Third wave” cognitive and behavioural therapies versus other psychological therapies for depression. The Cochrane Database of Systematic Reviews, 10, CD008704. 10.1002/14651858.CD008704.pub2 [DOI] [PubMed] [Google Scholar]
- Katirayi L, Namadingo H, Phiri M, Bobrow EA, Ahimbisibwe A, Berhan AY, Buono N, Moland KM, & Tylleskär T. (2016). HIV-positive pregnant and postpartum women’s perspectives about Option B+ in Malawi: A qualitative study. Journal of the International AIDS Society, 19(1), 20919 10.7448/IAS.19.1.20919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp CG, Jarrett BA, Kwon C-S, Song L, Jetté N, Sapag JC, Bass J, Murray L, Rao D, & Baral S. (2019). Implementation science and stigma reduction interventions in low- and middle-income countries: A systematic review. BMC Medicine, 17(1), 6 10.1186/s12916-018-1237-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knettel BA, Minja L, Chumba L, Oshosen M, Cichowitz C, Mmbaga BT, & Watt MH (2019). Serostatus disclosure among a cohort of HIV-infected pregnant women enrolled in HIV care in Moshi, Tanzania: A mixed-methods study. SSM Population Health, 100323. 10.1016/j.ssmph.2018.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knettel Brandon A., Cichowitz C, Ngocho JS, Knippler ET, Chumba LN, Mmbaga BT, & Watt MH (2018). Retention in HIV Care During Pregnancy and the Postpartum Period in the Option B+ Era: A Systematic Review and Meta-Analysis of Studies in Africa. Journal of Acquired Immune Deficiency Syndromes, 77(5), 427–438. 10.1097/QAI.0000000000001616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kulkarni SP, Shah KR, Sarma KV, & Mahajan AP (2013). Clinical uncertainties, health service challenges, and ethical complexities of HIV “test-and-treat”: A systematic review. American Journal of Public Health, 103(6), e14–23. 10.2105/AJPH.2013.301273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawson PJ, & Flocke SA (2009). Teachable moments for health behavior change: A concept analysis. Patient Education and Counseling, 76(1), 25–30. 10.1016/j.pec.2008.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malary M, Shahhosseini Z, Pourasghar M, & Hamzehgardeshi Z. (2015). Couples Communication Skills and Anxiety of Pregnancy: A Narrative Review. Materia Socio-Medica, 27(4), 286–290. 10.5455/msm.2015.27.286-290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazuguni F, Mwaikugile B, Cichowitz C, Watt MH, Mwanamsangu A, Mmbaga BT, Njau P, Mahande MJ, Todd J, & Renju J. (2019). Unpacking Loss to Follow-Up Among HIV-Infected Women Initiated on Option B+ In Northern Tanzania: A Retrospective Chart Review. EA Health Research Journal, 3(1), 6–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLean E, Renju J, Wamoyi J, Bukenya D, Ddaaki W, Church K, Zaba B, & Wringe A. (2017). “I wanted to safeguard the baby”: A qualitative study to understand the experiences of Option B+ for pregnant women and the potential implications for “test-and-treat” in four sub-Saharan African settings. Sexually Transmitted Infections, 93(Suppl 3). 10.1136/sextrans-2016-052972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon SA, Kennedy CE, Winch PJ, Kombe M, Killewo J, & Kilewo C. (2017). Stigma, Facility Constraints, and Personal Disbelief: Why Women Disengage from HIV Care During and After Pregnancy in Morogoro Region, Tanzania. AIDS and Behavior, 21(1), 317–329. 10.1007/s10461-016-1505-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minja L, Cichowitz C, Knettel BA, Mahande MJ, Kisigo G, Knippler ET, Ngocho JS, Mmbaga BT, & Watt MH (2019). Attitudes Toward Long-Term Use of Antiretroviral Therapy Among HIV-Infected Pregnant Women in Moshi, Tanzania: A Longitudinal Study. AIDS and Behavior. 10.1007/s10461-019-02622-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngocho JS, Watt MH, Minja L, Knettel BA, Mmbaga B, Williams PP, & Sorsdahl S. (2019). Depression and anxiety among pregnant women living with HIV in Kilimanjaro Region, Tanzania. PLOS ONE, (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noar SM, Black HG, & Pierce LB (2009). Efficacy of computer technology-based HIV prevention interventions: A meta-analysis: AIDS, 23(1), 107–115. 10.1097/QAD.0b013e32831c5500 [DOI] [PubMed] [Google Scholar]
- Petros G, Airhihenbuwa CO, Simbayi L, Ramlagan S, & Brown B. (2006). HIV/AIDS and ‘othering’ in South Africa: The blame goes on. Culture, Health & Sexuality, 8(1), 67–77. 10.1080/13691050500391489 [DOI] [PubMed] [Google Scholar]
- Psaros C, Remmert JE, Bangsberg DR, Safren SA, & Smit JA (2015). Adherence to HIV care after pregnancy among women in sub-Saharan Africa: Falling off the cliff of the treatment cascade. Curr HIV/AIDS Rep, 12(1), 1–5. 10.1007/s11904-014-0252-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relf MV, Silva SG, Williams MS, Moore E, Arscott J, Caiola C, & Barroso J. (2015). Feasibility of Using an iPod Touch Device and Acceptability of a Stigma Reduction Intervention with HIV-Infected Women in the Deep South. AIDS and Behavior, 19(10), 1896–1904. 10.1007/s10461-015-1031-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangl AL, Lloyd JK, Brady LM, Holland CE, & Baral S. (2013). A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: How far have we come? Journal of the International AIDS Society, 16(3Suppl 2). 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanzania Ministry of Health and Social Welfare. (2013). National guidelines for comprehensive care services for prevention of mother-to-child transmission of HIV and keeping mothers alive. [Google Scholar]
- Treves-Kagan S, El Ayadi AM, Pettifor A, MacPhail C, Twine R, Maman S, Peacock D, Kahn K, & Lippman SA (2017). Gender, HIV Testing and Stigma: The Association of HIV Testing Behaviors and Community-Level and Individual-Level Stigma in Rural South Africa Differ for Men and Women. AIDS and Behavior, 21(9), 2579–2588. 10.1007/s10461-016-1671-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai AC, Bangsberg DR, Kegeles SM, Katz IT, Haberer JE, Muzoora C, Kumbakumba E, Hunt PW, Martin JN, & Weiser SD (2013). Internalized Stigma, Social Distance, and Disclosure of HIV Seropositivity in Rural Uganda. Annals of Behavioral Medicine, 46(3), 285–294. 10.1007/s12160-013-9514-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tshabalala J, & Visser M. (2011). Developing a Cognitive Behavioural Therapy Model to Assist Women to Deal with HIV and Stigma. South African Journal of Psychology, 41(1), 17–28. 10.1177/008124631104100103 [DOI] [Google Scholar]
- Turan JM, Bukusi EA, Onono M, Holzemer WL, Miller S, & Cohen CR (2011). HIV/AIDS Stigma and Refusal of HIV Testing Among Pregnant Women in Rural Kenya: Results from the MAMAS Study. AIDS and Behavior; New York, 15(6), 1111–1120. 10.1007/s10461-010-9798-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Breda AD (2012). Stigma as ‘othering’ among Christian theology students in South Africa. SAHARA-J: Journal of Social Aspects of HIV/AIDS, 9(4), 181–191. 10.1080/17290376.2012.745272 [DOI] [PubMed] [Google Scholar]
- Visser MJ, Makin JD, Vandormael A, Sikkema KJ, & Forsyth BWC (2009). HIV/AIDS stigma in a South African community. AIDS Care, 21(2), 197–206. 10.1080/09540120801932157 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser Maretha J., Kershaw T, Makin JD, & Forsyth BWC (2008). Development of parallel scales to measure HIV-related stigma. AIDS and Behavior, 12(5), 759–771. 10.1007/s10461-008-9363-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watt MH, Cichowitz C, Kisigo G, Minja L, Knettel BA, Knippler E, Ngocho J, Manavalan P, & Mmbaga BT (2019). Predictors of postpartum HIV care engagement for women enrolled in prevention of mother-to-child transmission (PMTCT) programs in Tanzania. AIDS Care, 31(6), 687–698. 10.1080/09540121.2018.1550248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). Global guidance on criteria and processes for validation: Elimination of Mother-to-Child Transmission of HIV and Syphilis. http://www.who.int/reproductivehealth/publications/emtct-hiv-syphilis/en/
- Wringe A, Moshabela M, Nyamukapa C, Bukenya D, Ondenge K, Ddaaki W, Wamoyi J, Seeley J, Church K, Zaba B, Hosegood V, Bonnington O, Skovdal M, & Renju J. (2017). HIV testing experiences and their implications for patient engagement with HIV care and treatment on the eve of “test and treat”: Findings from a multicountry qualitative study. Sexually Transmitted Infections, 93(Suppl 3). 10.1136/sextrans-2016-052969 [DOI] [PMC free article] [PubMed] [Google Scholar]