Abstract
PURPOSE
To examine the retention rates and efficacy of silicone punctal plugs for the treatment of dry eye disease (DED) in patients with ocular graft-versus-host-disease (oGVHD) in comparison to dry eye disease due to non-oGVHD etiologies.
METHODS
We reviewed the case-records of 864 consecutive patients with DED who were symptomatic despite topical therapy and had silicone punctal plugs placed over an eight-year- period at a single academic center. We compared plug retention rates in oGVHD and non-oGVHD DED patients using Kaplan-Meier analyses. Furthermore, we analyzed changes in objective ocular surface parameters including tear breakup time (TBUT), Schirmer’s test, and corneal fluorescein staining (CFS) score in plug-retaining patients at two-, six- and twelve-month follow-up.
RESULTS
Median age of dry eye patients was 58 years, and 606 (70%) of patients were women. In the cohort, 264(31%) patients were diagnosed with oGVHD. Plug retention was significantly lower in oGVHD-DED patients compared to non-oGVHD-DED patients (p<0.0001). We observed significant improvement in CFS scores in plug retaining-oGVHD and non-oGVHD DED patients at all time points. Tear break-up time was significantly prolonged at six- and twelve-months follow-up in non-oGVHD patients, whereas significant change in TBUT in oGVHD patients was recorded only at twelve months post plug placement. Schirmer’s score improved significantly in plug retaining-non-oGVHD DED patients at six- and twelve-months follow-up, however no significant change was observed in Schirmer’s score in oGVHD DED patients.
CONCLUSIONS
An improvement in ocular surface disease parameters was observed in both plug-retaining oGVHD and non-oGVHD DED patients. However, a majority of oGVHD DED patients spontaneously lost their punctal plugs within 90 days of placement. Therefore, regular follow-up after plug placement is recommended to detect plug loss and ensure adequate disease control.
Keywords: punctal plugs, dry eye disease, silicone plugs, graft-versus-host-disease
INTRODUCTION
Dry eye disease (DED) is a multifactorial disorder of the ocular surface caused by tear deficiency or excessive tear evaporation, causing damage to the interpalpebral ocular surface, and is associated with symptoms of ocular discomfort, irritation and visual disturbances.[1,2] The prevalence of dry eye disease in adults varies between 5–50% worldwide, and has been associated with multiple risk factors including autoimmune disorders like ocular graft-versus- host disease (oGVHD), Sjögren’s syndrome, and rheumatoid arthritis.[3–10] The first line management for treatment of DED includes patient education, environmental modification, dietary changes, systemic medication changes, eyelid hygiene and artificial tears.[11] However, these treatments are often inadequate for patients with severe aqueous insufficiency; thus, punctal plugs placement is necessitated for natural tear retention. The fact that plugs can provide passive relief (i.e. they are effective regardless of patient compliance) and their reversibility makes them an attractive option for many patients.[12]
In 1935, WP Beetham first reported the occlusion of the nasolacrimal tract as an effective method for conserving ocular surface moisture and improving symptoms caused by lacrimal insufficiency.[13] Four decades later, Freeman proposed the blockade of the nasolacrimal duct with punctal plugs as an effective and reversible technique for the management of dry eye disease.[14] Although punctal plug placement aids in reducing the symptoms of dry eye disease, frequent spontaneous plug loss impedes their efficacy. Studies in the literature have reported 15–50% rate of plug loss over follow-up periods ranging from two to six months.[12,15–17]
Allogeneic hematopoietic stem cell transplantation (HSCT) from human leukocyte antigen (HLA)- matched donors is a well-established therapy for malignant and benign hematologic diseases.[18] Chronic GVHD is a potentially life-threatening complication in patients undergoing HSCT.[19–22] Ocular involvement is seen in 40–60% of GVHD patients; typically presenting with symptoms associated with dry eye disease including gritty or painful eyes, redness or excessive tearing, and in some cases, corneal perforation and vision loss.[23–26] In oGVHD, donor-derived immune cells attack the host tissues leading to inflammation, proliferation of fibroblasts, and fibrotic changes in the periductal areas of the tear glands as well as the associated secretory apparatus.[27–29] This inflammation-mediated tissue damage typically results in irreversible loss of lacrimal gland function leading to reduced tear volume and altered tear composition.[30] Thus, punctal occlusion has become a treatment of choice in the management of oGVHD patients with severe aqueous insufficiency.
The objective of this retrospective study was to evaluate the retention rates of silicone punctal plugs in 1520 eyes of 864 patients with DED due to oGVHD or non-oGVHD etiologies, and analyze their efficacy in improving objective ocular surface parameters.
METHODS
We obtained the approval of the Institutional Review Board and Ethics Committee at Massachusetts Eye and Ear for this study. The study was conducted in compliance with the Health Insurance Portability and Accountability Act (HIPAA) of 1996 and adhered to the tenants of the Declaration of Helsinki. We conducted a retrospective review of clinical charts of all patients who underwent punctal plug placement for the treatment of dry eye disease at the Cornea Service of Massachusetts Eye and Ear over an eight-year period from January 2011 to January 2019.
Consecutive patients diagnosed with DED who underwent silicone punctal plug placement (Eagle Vision, Inc., Memphis, Tennessee; or Softplug-Oasis Medical, Inc, San Dimas, California) were identified from the institutional electronic patient database using International Classification of Diseases (ICD) diagnostic codes and current procedural terminology (CPT) codes. The documented data included demographic information, medical history, ophthalmic history, ocular diagnosis, prescribed medications, initial date of punctal plug placement, and the status of punctal plug retention at follow-up. We assessed the efficacy of punctal plugs by evaluating the change in objective ocular surface disease parameters, including tear breakup time (TBUT, in seconds), Schirmer’s test (in millimeters) and corneal fluorescein staining score (CFS, as per the National Eye Institute grading scale) at baseline and two-, six- and twelve-months post-punctal plug placement. The patients who spontaneously lost their punctal plugs were not included in the data analysis beyond the immediate follow-up when the extrusion was detected. The patients who were lost follow-up or whose data were not recorded during the follow-up, were also excluded from the data analysis.
Both upper and lower puncta were occluded in patients with severe dry eye disease, and either lower or upper puncta in milder cases. Punctal plug size was selected by the treating ophthalmologist, sometimes using the Coroneo Punctal Gauging system (Eagle Vision, Inc, Memphis, Tennessee). Topical anesthetic (0.5% proparacaine; Alcon Inc., Fort Worth, Texas) was applied to the punctum using a cotton tipped applicator and the plug was inserted under a slit lamp biomicroscope. Proper fitting of the plug was assessed by ensuring that the dome of the plug was flush with the lid margin contour. Patients were asked to return for follow-up at regular intervals to assess plug retention and record changes in ocular surface disease paramters.
STATISTICAL ANALYSES
We performed Kaplan-Meier curve analysis to accurately account for the varying durations of follow-up after plug placement using Prism 8 Software for MacOSX v.X.5.3 (GraphPad Software Inc., La Jolla, CA). For this analysis, we defined spontaneous plug loss as the absence of a plug in the punctum in which it was previously placed. For survival analysis, we considered each patient as one sample (N = 864), and punctal plug loss was counted as a single “event”.
Continuous variables are reported as mean (± standard deviation), and categorical variables are reported in numbers (percentage). We performed a one-way ANOVA with repeated measures to compare the ocular surface disease parameters at baseline and follow-ups for plug-retaining patients. A value of p<0.05 was considered statistically significant for all comparisons.
RESULTS
This retrospective study cohort included a total of 864 patients, with 264 (31%) patients with DED associated oGVHD and 600 (69%) patients with DED due to other causes. Patients with oGVHD DED had a median age of 56 years (21–75 years), and 123 patients (47%) were female; 141 patients (53%) were male. The non-oGVHD DED patient cohort had a median age of 58 (13–98 years), and the majority of patients were female (483, 81%). Amongst the oGVHD DED patients, 188 (71%) had meibomian gland dysfunction (MGD), and 22 (8%) had conjunctival fibrosis (CF), whereas 362 (60%) and 54 (2%) non-oGVHD DED patients had MGD and CF, respectively.
Patients who underwent punctal plug placement reported ocular discomfort (n=778, 90%), blurred vision (n=101, 12%), ocular redness (n=221, 25%) and ocular pain (n=112, 13%). Punctal plugs were placed bilaterally in 86% and 71% of oGVHD and non-oGVHD DED patients, respectively. At the time of punctal plug placement, all patients had been prescribed artificial tears. At presentation, oGVHD DED patients were on 0.05% topical cyclosporine (Restasis) (n=259, 98%), corticosteroids (n=109, 41%), anti-microbial drugs (n=98, 37%), anti-glaucoma drugs (n=20, 8%) and autologous serum tears (n=14, 5%). Ocular GVHD patients on systemic immunosuppressive therapy were on corticosteroids (n=177, 67%), tacrolimus (n=133, 50%), mycophenolate (n=46, 17%) and cyclosporine (n=20, 8%). Non-oGVHD DED patients were prescribed topical cyclosporine (n=476, 79%), corticosteroids (n=83, 14%), anti-glaucoma drugs (n=60, 10%), anti-microbial drugs (n=37, 6%), and autologous serum tears (n=20, 3%). Only a very small proportion of non-oGVHD DED patients were prescribed immunosuppressive therapy including corticosteroids (n=38, 6%), tacrolimus (n=17, 3%), cyclosporine (n=16, 3%) and mycophenolate (n=4, <1%). Details of the prescribed systemic and ophthalmic medications are summarized in Table 1.
Table 1.
Clinical characteristics of 1520 eyes of 864 DED patients with or without oGVHD at baseline.
| DED without oGVHD (n=600, 69%) | DED with oGVHD (n=264, 31%) | ||
|---|---|---|---|
| Age, median (range) | 58 (13–98) | 56 (21–75) | |
| Sex | Female (%) | 483 (81%) | 123 (47%) |
| Male (%) | 117 (19%) | 141 (53%) | |
| Punctal Plugs | |||
| Bilateral | 427 (71%) | 228 (86%) | |
| Unilateral | 173 (29%) | 37 (14%) | |
| Use of topical ophthalmic medications (n,%) | |||
| Artificial Tears | 600 (100%) | 264 (100%) | |
| Restasis | 476 (79%) | 259 (98%) | |
| Corticosteroids | 83 (14%) | 109 (41%) | |
| Anti-glaucoma drugs | 60 (10%) | 20 (8%) | |
| Anti-microbial drugs | 37 (6%) | 98 (37%) | |
| Serum Tears | 20 (3%) | 14 (5%) | |
| Use of systemic immunosuppressive drugs | |||
| Corticosteroids | 38 (6%) | 177 (67%) | |
| Tacrolimus | 17 (3%) | 133 (50%) | |
| Cyclosporine | 16 (3%) | 20 (8%) | |
| Mycophenolate | 4 (<1%) | 46 (17%) | |
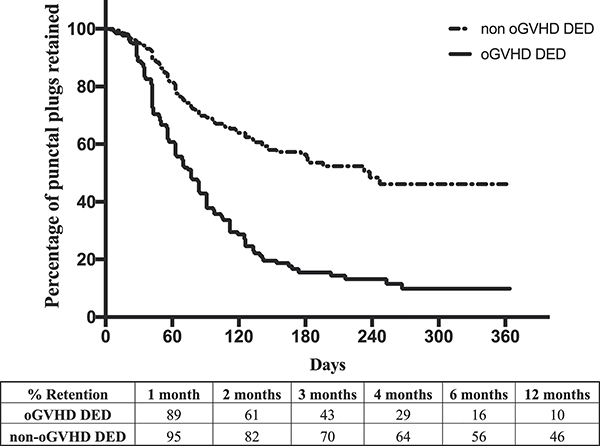
Kaplan-Meier analysis of punctal plug retention in patients with oGVHD DED compared to non-oGVHD DED patients is presented in Figure 1. The median duration of punctal plug retention was 77 days in oGVHD DED patients compared to 238 days in non-oGVHD DED patients. The plug retention rate was significantly less in oGVHD DED patients compared to non-oGVHD DED patients at two (61% vs. 82%), six (16% vs. 56%) and twelve (10% vs. 46%) months post-plug placement (p<0.0001).
Figure 1.
Kaplan-Meier curve for punctal plug retention in DED patients with oGVHD in comparison to patients with DED due to other underlying etiologies.
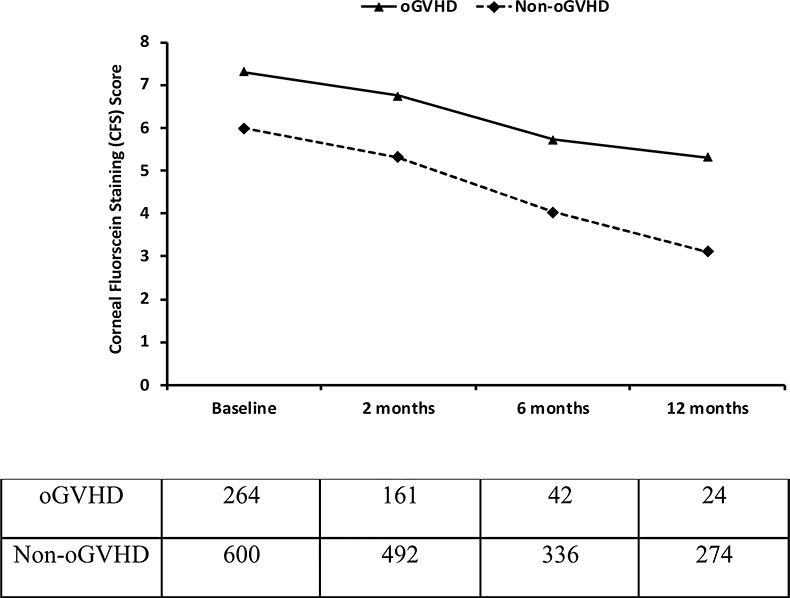
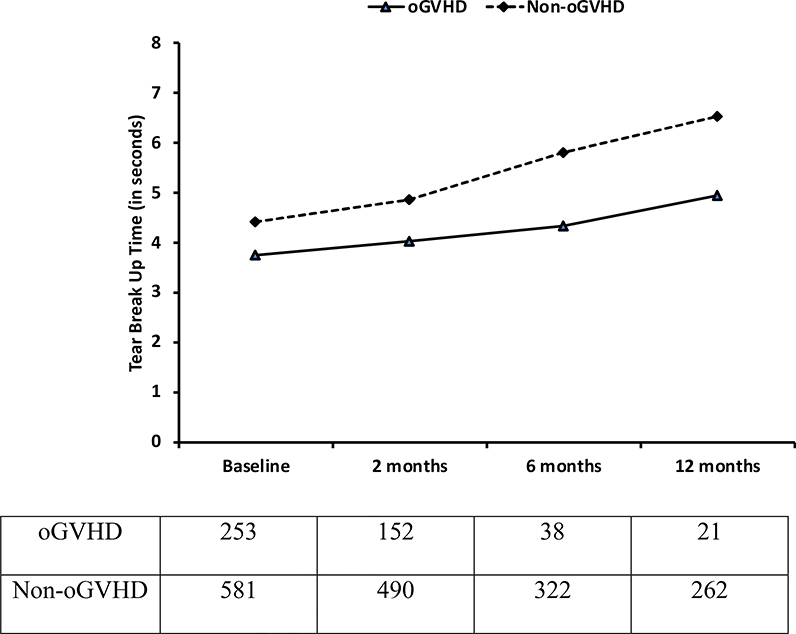
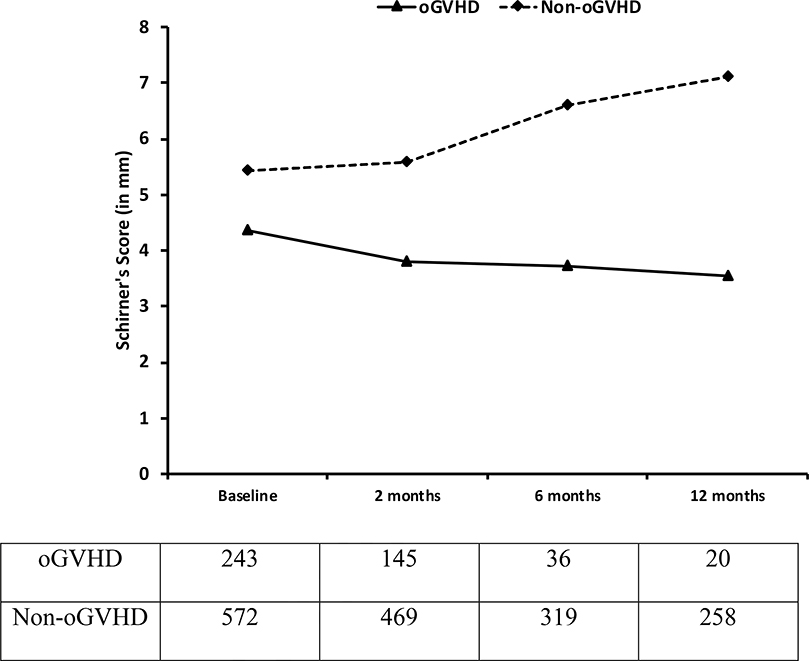
In plug-retaining oGVHD DED patients, CFS scores significantly decreased at two- (6.75±1.25, p=0.0244), six- (5.71±1.36, p=0.0035), and twelve- (5.31±0.46, p=0.0329) month follow-up compared to initial presentation (7.29±2.15). (Figure 2) A more marked reduction was seen in plug-retaining non-oGVHD DED patients at two- (5.31±3.51, p=0.0097), six- (4.02±2.87, p<0.0001), twelve- (3.11±2.45, p<0.0001) month follow-ups, compared to baseline (5.99±3.64). TBUT was significantly prolonged in plug-retaining non-GVHD DED patients at six- (5.81±3.89 secs, p=0.0026) and twelve- (6.54±4.15 secs, p=0.0014) month follow-ups compared to TBUT (4.42±4.13 secs) at the time of plug placement. TBUT increased significantly only at twelve months post-placement in oGVHD patients (4.95±0.72 secs, p=0.018) compared to baseline (3.75±1.94 secs). (Figure 3) A significant increase in Schirmer’s test score was recorded in non-oGVHD patients at six- (6.59±2.35 mm, p=0.014) and twelve- (7.11±3.59 mm, p=0.04) month follow-ups compared to baseline (5.41±4.96 mm). There was no significant change in the Schirmer’s score in plug-retaining oGVHD DED patients.
Figure 2.
A statistically significant reduction in the Corneal Fluorescein Staining (CFS) scores was recorded in both oGVHD DED and non-oGVHD DED patients who retained punctal plugs at two-, six- and twelve-month follow-up after placement.
Figure 3.
Tear Breakup Time (TBUT) was significantly prolonged at six- and twelve-month follow-ups in plug-retaining non-oGVHD DED patients, whereas TBUT was significantly prolonged only at twelve-month follow-up in oGVHD DED patients.
DISCUSSION
In this retrospective study, we examined the retention rates of silicone punctal plugs for treatment of DED in patients with oGVHD in comparison to those without oGVHD. We evaluated objective clinical parameters including CFS, TBUT and Schirmer’s test score to determine the efficacy of punctal plugs in these patient populations.
Ocular manifestations affect an overwhelming majority of patients with chronic GVHD after allogeneic HSCT.[31,32] Although many ocular tissues maybe affected by the immune mediated response associated with GVHD, dry eye disease is the most commonly associated with oGVHD.[26,33–36] Exam findings in oGVHD patients may include severe punctate keratopathy, filamentary keratitis and in rare instances, corneal thinning and perforation.[19,20,37] These findings arise due to decreased aqueous tear production following immune mediated lacrimal gland destruction, making punctal occlusion an attractive therapeutic strategy, as punctal occlusion partially restores the tear film by impeding the drainage of tears and artificial tear supplements.[38] The benefits of punctal occlusion on tear retention and ocular surface health have been well-documented, with multiple reports demonstrating that punctal occlusion leads to improvement in both objective and subjective dry eye disease symptoms.[12,39–41] Rarely, punctal plug placement leads to complications such as canaliculitis, discomfort, epiphora, lesions of the conjunctiva and cornea, or pyogenic granuloma.[39] Additionally, studies have attributed exacerbation of DED following punctal plug placement to the development of an inflammatory milieu on the ocular surface due to the presence of proinflammatory cytokines in the retained tears of these patients.[42,43]
Our data suggest that punctal plugs significantly improve ocular surface parameters in both oGVHD and non-oGVHD patients with dry eye. In both groups, CFS improved at all time points, however a significant improvement in TBUT was only seen at six and twelve month post placement in non-oGVHD patients and only at twelve months in oGVHD patients. These results are consistent with other reports in the literature; Mansour and colleagues have reported improvement in Rose Bengal staining and lower discomfort scores following punctal occlusion in patients with DED secondary to Sjogren’s syndrome.[44] Furthermore, Ogawa and colleagues have reported complete resolution of dry eye symptoms and improved ocular surface disease parameters post-punctal plug placement in patients who were not responsive to treatment with autologous serum tears.[45]
We found that spontaneous extrusion of punctal plugs occurs in a majority of oGVHD-associated DED patients within 90 days of plug placement. The retention rates reported in our study are consistent with previous reports of punctal plug retention in patients of DED, both with and without oGVHD.[12,15–17,46–48] The lower retention rate of punctal plugs in oGVHD DED patients has been attributed to punctal subepithelial fibrosis.[48] Yaguchi et al. further recommended lacrimal punctal cauterization in chronic oGVHD DED patients to overcome recurrent plug extrusion.[49]
The retrospective design for the evaluation of objective ocular surface disease parameters are the primary limitations of this study. Long-term follow-up is challenging in the setting of chronic GVHD due to increased morbidity, and because our practice is a tertiary care center with patients often return to their referring ophthalmologists once their condition stabilizes, resulting in a decrease in follow-up visits. In addition, during the analysis of ocular surface parameters, we did not take into account the therapeutic effect of concurrent ophthalmic and/or systemic medications that patients may have been prescribed for DED.
In summary, our data suggest that punctal plug placement for the treatment of DED secondary to chronic ocular GVHD leads to significant improvement in ocular surface parameters. However, since spontaneous plug extrusion occurs in a majority of oGVHD patients over a period of few months post-placement, it is essential for the ophthalmologists to closely follow-up with patients for punctal plug replacement or adopt alternative therapies for the management of the ocular surface disease.
Figure 4.
Schirmer’s test score was significantly increased at six- and twelve-month follow-up in plug-retaining non-oGVHD DED patients, whereas no change in Schirmer’s test score was observed in oGVHD DED patients.
ACKNOWLEDGMENTS
The authors would like to thank Dr. Hamid Alemi for his valuable feedback regarding the data analysis.
FUNDING SUPPORT
This study was supported by the National Eye Institute/National Institutes of Health Grant 5K12EY016335 to JY (trainee).
Footnotes
FINANCIAL DISCLOSURE
The authors of this manuscript have no financial conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- [1].Craig JP, Nichols KK, Akpek EK, Caffery B, Dua HS, Joo C-K, et al. TFOS DEWS II Definition and Classification Report. Ocul Surf 2017;15:276–83. https://doi.Org/10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- [2].Pflugfelder SC, Solomon A, Stern ME. The Diagnosis and Management of Dry Eye. Cornea 2000;19:644–9. 10.1097/00003226-200009000-00009. [DOI] [PubMed] [Google Scholar]
- [3].Moss SE, Klein R, Klein BEK. Prevalance of and risk factors for dry eye syndrome. Arch Ophthalmol 2000;118:1264–8. 10.1001/archopht.118.9.1264. [DOI] [PubMed] [Google Scholar]
- [4].McCarty CA, Bansal AK, Livingston PM, Stanislavsky YL, Taylor HR. The epidemiology of dry eye in Melbourne, Australia. Ophthalmology 1998;105:1114–9. 10.1016/S0161-6420(98)96016-X. [DOI] [PubMed] [Google Scholar]
- [5].Ogawa Y, Okamoto S, Wakui M, Watanabe R, Yamada M, Yoshino M, et al. Dry eye after haematopoietic stem cell transplantation. Br J Ophthalmol 1999;83:1125–30. 10.1136/bjo.83.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Akpek EK, Bunya VY, Saldanha IJ. Sjögren’s Syndrome: More Than Just Dry Eye. Cornea 2019;38:658–61. 10.1097/ICO.0000000000001865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II Epidemiology Report. Ocul Surf 2017;15:334–65. 10.1016/jjtos.2017.05.003. [DOI] [PubMed] [Google Scholar]
- [8].Villani E, Nucci P. Dry eye in rheumatoid arthritis: Tear film osmolarity and inflammation. Cornea 2015;34:e6 10.1097/ICO.0000000000000346. [DOI] [PubMed] [Google Scholar]
- [9].Dana R, Bradley JL, Guerin A, Pivneva I, Stillman IÖ, Evans AM, et al. Estimated Prevalence and Incidence of Dry Eye Disease Based on Coding Analysis of a Large, All-age United States Health Care System. Am J Ophthalmol 2019. https://doi.Org/10.1016/j.ajo.2019.01.026. [DOI] [PubMed] [Google Scholar]
- [10].Schaumberg DA, Dana R, Buring JE, Sullivan DA. Prevalence of dry eye disease among US men: Estimates from the physicians’ health studies. Arch Ophthalmol 2009;127:763–8. 10.1001/archophthalmol.2009.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Jones L, Downie LE, Korb D, Benitez-del-Castillo JM, Dana R, Deng SX, et al. TFOS DEWS II Management and Therapy Report. Ocul Surf 2017;15:575–628. 10.1016/jjtos.2017.05.006. [DOI] [PubMed] [Google Scholar]
- [12].Balaram M, Schaumberg DA, Dana MR. Efficacy and tolerability outcomes after punctal occlusion with silicone plugs in dry eye syndrome. Am J Ophthalmol 2001;131:30–6. [DOI] [PubMed] [Google Scholar]
- [13].Beetham WP. Filamentary Keratitis. Trans Am Ophthalmol Soc 1935;33:413–35. [PMC free article] [PubMed] [Google Scholar]
- [14].Freeman JM. The punctum plug: evaluation of a new treatment for the dry eye. Trans Am Acad Ophthalmol Otolaryngol 1975. [PubMed] [Google Scholar]
- [15].Sakamoto A, Kitagawa K, Tatami A. Efficacy and Retention Rate of Two Types of Silicone Punctal Plugs in Patients With and Without Sj??gren Syndrome. Cornea 2004;23:249–54. 10.1097/00003226-200404000-00006. [DOI] [PubMed] [Google Scholar]
- [16].Horwath-Winter J, Thaci A, Gruber A, Boldin I. Long-term Retention Rates and Complications of Silicone Punctal Plugs in Dry Eye. Am J Ophthalmol 2007;144:441–444.e1. 10.1016/j.ajo.2007.05.019. [DOI] [PubMed] [Google Scholar]
- [17].Parikh NB, Francis JH, Latkany RA. Retention Rate of Silicone Punctal Plugs Placed by Residents in a General Clinic Setting. Ophthalmic Plast Reconstr Surg 2010;26:400–2. 10.1097/IOP.0b013e3181cd6145. [DOI] [PubMed] [Google Scholar]
- [18].Shikari H, Antin JH, Dana R. Ocular Graft-versus-Host Disease: A Review. Surv Ophthalmol 2013;58:233–51. 10.1016/j.survophthal.2012.08.004. [DOI] [PubMed] [Google Scholar]
- [19].Shikari H, Amparo F, Saboo U, Dana R. Onset of Ocular Graft-Versus-Host Disease Symptoms After Allogeneic Hematopoietic Stem Cell Transplantation. Cornea 2015;34:243–7. 10.1097/ICO.0000000000000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Saboo US, Amparo F, Abud TB, Schaumberg DA, Dana R. Vision-Related Quality of Life in Patients with Ocular Graft-versus-host Disease. Ophthalmology 2015;122:1669–74. 10.1016/j.ophtha.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Stevenson W, Shikari H, Saboo U, Amparo F, Dana R. Bilateral corneal ulceration in ocular graft-versus-host disease. Clin Ophthalmol 2013;7:2153 10.2147/OPTH.S51180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Ogawa Y, Kim SK, Dana R, Clayton J, Jain S, Rosenblatt MI, et al. International chronic ocular graft-vs-host-disease (GVHD) consensus group: Proposed diagnostic criteria for chronic GVHD (Part I). Sci Rep 2013. 10.1038/srep03419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Inamoto Y, Valdes-Sanz N, Ogawa Y, Alves M, Berchicci L, Galvin J, et al. Ocular Graft-versus-Host Disease after Hematopoietic Cell Transplantation: Expert Review from the Late Effects and Quality of Life Working Committee of the Center for International Blood and Marrow Transplant Research and Transplant Complications Working. Biol Blood Marrow Transplant 2019. 10.1016/j.bbmt.2018.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Balaram M, Rashid S, Dana R. Chronic ocular surface disease after allogeneic bone marrow transplantation. Ocul Surf 2005;3:203–11. [DOI] [PubMed] [Google Scholar]
- [25].Ogawa Y, Okamoto S, Wakui M, Watanabe R, Yamada M, Yoshino M, et al. Dry eye after haematopoietic stem cell transplantation. Br J Ophthalmol 1999. 10.1136/bjo.83.10.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Nassiri N, Eslani M, Panahi N, Mehravaran S, Ziaei A, Djalilian AR. Ocular graft versus host disease following allogeneic stem cell transplantation: a review of current knowledge and recommendations. J Ophthalmic Vis Res 2013;8:351–8. [PMC free article] [PubMed] [Google Scholar]
- [27].Jacobs R, Tran U, Chen H, Kassim A, Engelhardt BG, Greer JP, et al. Prevalence and risk factors associated with development of ocular GVHD defined by NIH consensus criteria. Bone Marrow Transplant 2012;47:1470–3. 10.1038/bmt.2012.56. [DOI] [PubMed] [Google Scholar]
- [28].Curtis LM, Datiles MB, Steinberg SM, Mitchell SA, Bishop RJ, Cowen EW, et al. Predictive models for ocular chronic graft-versus-host disease diagnosis and disease activity in transplant clinical practice. Haematologica 2015;100:1228–36. 10.3324/HAEMATOL.2015.124131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Dietrich-Ntoukas T, Cursiefen C, Westekemper H, Eberwein P, Reinhard T, Bertz H, et al. Diagnosis and Treatment of Ocular Chronic Graft-Versus-Host Disease: Report From the German-Austrian-Swiss Consensus Conference on Clinical Practice in Chronic GVHD. Cornea 2012;31:299–310. 10.1097/ICO.0b013e318226bf97. [DOI] [PubMed] [Google Scholar]
- [30].Nair S, Vanathi M, Mahapatra M, Seth T, Kaur J, Velpandian T, et al. Tear inflammatory mediators and protein in eyes of post allogenic hematopoeitic stem cell transplant patients. Ocul Surf 2018;16:352–67. 10.1016/jjtos.2018.04.007. [DOI] [PubMed] [Google Scholar]
- [31].Ogawa Y, Kuwana M. Dry eye as a major complication associated with chronic graft- versus-host disease after hematopoietic stem cell transplantation. Cornea, 2003. [DOI] [PubMed] [Google Scholar]
- [32].Amparo F, Shikari H, Saboo U, Dana R. Corneal fluorescein staining and ocular symptoms but not Schirmer test are useful as indicators of response to treatment in chronic ocular GVHD. Ocul Surf 2018;16:377–81. 10.1016/jjtos.2018.05.002. [DOI] [PubMed] [Google Scholar]
- [33].Saboo US, Amparo F, Abud TB, Schaumberg DA, Dana R. Vision-Related Quality of Life in Patients with Ocular Graft-versus-Host Disease. Ophthalmology, 2015. https://doi.Org/10.1016/j.ophtha.2015.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Lin X, Cavanagh HD. Ocular manifestations of graft-versus-host disease: 10 years’ experience. Clin Ophthalmol 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Kheirkhah A, Qazi Y, Arnoldner MA, Suri K, Dana R. In vivo confocal microscopy in dry eye disease associated with chronic graft-versus-host disease. Investig Ophthalmol Vis Sci 2016;57:4686–91. 10.1167/iovs.16-20013. [DOI] [PubMed] [Google Scholar]
- [36].Nassar A, Tabbara KF, Aljurf M. Ocular manifestations of graft-versus-host disease. Saudi J Ophthalmol 2013;27:215–22. 10.1016/j.sjopt.2013.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Kheirkhah A, Coco G, Satitpitakul V, Dana R. Subtarsal Fibrosis Is Associated With Ocular Surface Epitheliopathy in Graft-Versus-Host Disease. Am J Ophthalmol 2018;189:102–10. 10.1016/j.ajo.2018.02.020. [DOI] [PubMed] [Google Scholar]
- [38].Riemens A, Boome L te, Imhof S, … JK-C opinion in, 2010 undefined. Current insights into ocular graft-versus-host disease. JournalsLwwCom n.d. [DOI] [PubMed] [Google Scholar]
- [39].Murube J, Murube E. Treatment of dry eye by blocking the lacrimal canaliculi. Surv Ophthalmol n.d.;40:463–80. 10.1016/s0039-6257(96)82013-3. [DOI] [PubMed] [Google Scholar]
- [40].Sabti S, Halter JP, Braun Fränkl BC, Goldblum D. Punctal occlusion is safe and efficient for the treatment of keratoconjunctivitis sicca in patients with ocular GvHD. Bone Marrow Transplant 2012;47:981–4. 10.1038/bmt.2011.205. [DOI] [PubMed] [Google Scholar]
- [41].Ervin A-M, Law A, Pucker AD. Punctal occlusion for dry eye syndrome. Cochrane Database Syst Rev 2017;6:CD006775 10.1002/14651858.CD006775.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Behrens A, Doyle JJ, Stern L, Chuck RS, McDonnell PJ, Azar DT, et al. Dysfunctional Tear Syndrome. Cornea 2006;25:900–7. 10.1097/01.ico.0000214802.40313.fa. [DOI] [PubMed] [Google Scholar]
- [43].Yen MT, Pflugfelder SC, Feuer WJ. The effect of punctal occlusion on tear production, tear clearance, and ocular surface sensation in normal subjects. Am J Ophthalmol 2001;131:314–23. 10.1016/s0002-9394(00)00822-9. [DOI] [PubMed] [Google Scholar]
- [44].Mansour K, Leonhardt CJ, Kalk WW, Bootsma H, Bruin KJ, Blanksma LJ, et al. Lacrimal Punctum Occlusion in the Treatment of Severe Keratoconjunctivitis Sicca Caused by Sjögren Syndrome. Cornea 2007;26:147–50. 10.1097/01.ico.0000244877.30997.6a. [DOI] [PubMed] [Google Scholar]
- [45].Ogawa Y, Okamoto S, Mori T, Yamada M, Mashima Y, Watanabe R, et al. Autologous serum eye drops for the treatment of severe dry eye in patients with chronic graft-versus-host disease. Bone Marrow Transplant 2003;31:579–83. 10.1038/sj.bmt.1703862. [DOI] [PubMed] [Google Scholar]
- [46].Kaido M, Ishida R, Dogru M, Tsubota K. Comparison of Retention Rates and Complications of 2 Different Types of Silicon Lacrimal Punctal Plugs in the Treatment of Dry Eye Disease. Am J Ophthalmol 2013;155:648–653.e1. 10.1016/J.AJO.2012.10.024. [DOI] [PubMed] [Google Scholar]
- [47].Tai MC, Cosar CB, Cohen EJ, Rapuano CJ, Laibson PR. The clinical efficacy of silicone punctal plug therapy. Cornea 2002. 10.1097/00003226-200203000-00001. [DOI] [PubMed] [Google Scholar]
- [48].Sabti S, Halter JP, Braun Fränkl BC, Goldblum D. Punctal occlusion is safe and efficient for the treatment of keratoconjunctivitis sicca in patients with ocular GvHD. Bone Marrow Transplant 2012;47:981–4. 10.1038/bmt.2011.205. [DOI] [PubMed] [Google Scholar]
- [49].Yaguchi S, Ogawa Y, Kamoi M, Uchino M, Tatematsu Y, Ban Y, et al. Surgical management of lacrimal punctal cauterization in chronic GVHD-related dry eye with recurrent punctal plug extrusion. Bone Marrow Transplant 2012;47:1465–9. 10.1038/bmt.2012.50. [DOI] [PubMed] [Google Scholar]