Abstract
Background:
Antenatal care coverage is very low in low-and middle-income countries, including Ethiopia. Self-reported pregnant women’s satisfaction may be important in identifying the demographic, provider-, and facility-related factors that can be improved to increase antenatal care satisfaction. However, there is a paucity of data on pregnant women’s satisfaction in Ethiopia, particularly in the study setting. Therefore, this study aimed to assess antenatal care service satisfaction and associated factors among pregnant women at public health facilities in the Harari region of eastern Ethiopia.
Methods:
A health institution–based cross-sectional study was conducted among women who were attending antenatal care clinics in February 2017. All 531 pregnant women were selected using a systematic random sampling method. Data were collected using an interviewer-administered questionnaire, entered into EpiData version 3.1, and analyzed using SPSS version 22.0 software. A logistic regression model was applied to control for confounders. The level of significance was determined at a p-value of less than 0.05.
Results:
The magnitude of pregnant women’s satisfaction with antenatal care services was 70.3% (95% confidence interval (CI) = 66.4%–74.3%). Receiving antenatal care services from the hospital (adjusted odds ratio (AOR) = 2.44, 95% CI = 1.50–3.98), did not attend formal education (AOR = 2.53, 95% CI = 1.52–4.20) and attended primary education (AOR = 2.17, 95% CI = 1.17–4.04), having a repeated visit to antenatal care (AOR = 4.62, 95% CI = 2.98–7.17), initiating antenatal care services within the first trimester (AOR = 1.74, 95% CI = 1.12–2.71), having no history of stillbirth (AOR = 2.52, 95% CI = 1.37–4.65), and waiting for no more than 30 min in the health facility to get service (AOR = 2.31, 95% CI = 1.28–4.16) were factors associated with pregnant women’s satisfaction with antenatal care services.
Conclusion:
More than two-thirds of pregnant women were satisfied with the antenatal care service. The type of health facility, education status, number and initiation time of antenatal visit, history of stillbirth, and waiting time to get service were factors associated with pregnant women’s satisfaction with antenatal care services.
Keywords: Antenatal care, pregnant women, satisfaction, Harari region, Ethiopia
Introduction
Globally, pregnancy and childbirth are significant phenomena for pregnant women and their families, making them vulnerable to both women and fetuses.1 More than 99% of maternal deaths occur in low-and middle-income countries. Although, by 2015, maternal mortality had decreased by over 44%, maternal mortality levels have continued to remain unacceptably high in sub-Saharan Africa (SSA).2–5 Inadequate access to quality antenatal care (ANC) and poor satisfaction contribute significantly to these preventable maternal deaths.6
In Ethiopia, the maternal mortality ratio was 412 per 100,000 live births according to the 2016 Ethiopian Demographic Health Survey (EDHS), which is among countries with high maternal deaths.4,5 The country is committed to achieving the Sustainable Development Goals (SDGs), which plans to reduce maternal death to less than 70 deaths per 100,000 live births between 2016 and 2030. However, progress has been stagnated in low- and middle-income countries, including Ethiopia.4,5,7
The ANC is considered one of the best strategies to reduce maternal morbidity and mortality.4,8,9 Although the 2016 World Health Organization (WHO) ANC model recommends a minimum of eight ANC contacts, with the first contact scheduled to take place in the first trimester, two contacts scheduled in the second trimester, and five contacts scheduled in the third trimester, Ethiopia still applies the 2002 WHO focused antenatal care (FANC) model, which recommends that pregnant women need to have a minimum of four antenatal visits for a normal pregnancy. Worldwide, 85% of the pregnant women had at least one ANC visit, whereas only 58% had the recommended four ANC visits.10,11 In Ethiopia, 62% of pregnant women had at least one ANC visit and only 32% of pregnant women in Ethiopia had the recommended four ANC visits as per the 2016 EDHS.4 The 5-year Ethiopian health sector transformation plan targets to increase the proportion of women receiving at least four ANC visits up to 68% to 95% in 2020.4,5,12
In many African countries, the utilization of ANC services is directly related to the satisfaction of the clients.13,14 Different studies conducted in Ethiopia revealed that the pregnant women’s satisfaction with ANC service ranges between 33.4% and 83.9%. The pregnant women’s satisfaction with ANC was 60.4% in Jimma town, 53.3% in Bahir Dar Special Zone, 33.4% in Bursa Woreda of Sidama Zone, and 83.9% in Alganesh Health Center Shire, North West Tigray.15–18 Patent’s satisfaction with the service also affects other people’s service utilization in such a way that the satisfied patient will express their satisfaction and recommendation to the other four to five people, and the dissatisfied one will complain to 20 or more other people about their dissatisfaction with the services.19,20
Determinants such as the history of previous ANC, sex of service provider, initiation time, number of ANC visits, history of stillbirth, history of abortion, planned pregnancy, facility type, distance and waiting time, and maternal education had a potential impact on pregnant women’s satisfaction.14,15,21–26 However, there is an inconsistency between the above-mentioned studies, which is influenced by socio-cultural, economic, and geographical variations.23 One of the challenges that we continuously faced recently is suboptimal quality ANC and client dissatisfaction. Thus, assessing the extent of women’s satisfaction with health services is crucial, as satisfied clients are more likely to adhere to treatment and receive the benefits of ANC. Although client satisfaction is essential for further improvement of the quality of ANC and to provide quality healthcare services for pregnant women, there is a paucity of data on pregnant women’s satisfaction in Ethiopia, particularly in the study settings. Therefore, this study aimed to assess ANC satisfaction and associated factors among pregnant women at public health facilities in the Harari region, eastern Ethiopia.
Methods and materials
Study setting and design
A health facility–based cross-sectional study design was conducted in public health facilities found in the Harari region from February 1 to 30, 2017. The Harari regional state is one of the nine regional states found in Ethiopia. Harar city is the capital of the Harari region found 510 km away from Addis Ababa in the eastern part of the country. The Harari region is the smallest regional state in Ethiopia, with nine Woredas and 36 Kebeles, and 59,487 total households. According to the 2016 Harari Regional Health Bureau report, the region has a total population of 240,000, of those 123,072 are females and 53,383 are women of reproductive age group. There are two public hospitals and eight public health centers with 591 health professionals in the region. ANC services are provided using 2002 WHO FANC model by male or female midwives/clinical nurses in all public health facilities in the region.
Study population
All pregnant women attending ANC service in public health facilities found in the Harari region were the source population, and all pregnant women utilizing ANC services during the study period in public health facilities found in the Harari region were the study population.
Inclusion and exclusion criteria
Pregnant women who were registered for ANC service during the data collection period were included and those who were unable to respond were excluded.
Sample size determination
The sample size was calculated for both objectives of this study. The sample size for the first objective (magnitude of satisfaction with ANC service) was calculated using a single population proportion formula (n = (Z α/2)2pq / d2)) with the following assumptions: confidence level at 95%, the best estimate of population proportion 60.4% taken from a previous study done in Jimma town,14 and 5% margin of error. Then, the sample size was 368.
The sample size for the second objective (factors associated with pregnant women’s satisfaction with ANC service) was calculated by using the Statcalc of Epi Info statistical software version 7 with the following assumptions: confidence level = 95%, Power = 80%, the ratio of unexposed to exposed almost equivalent to 1.
Using double population formula
where p1 = current estimate of population proportion, P1 (for non-exposed group), q1 = 1 – p1, p2 = current estimate of population proportion, P2 (for exposed group), q2 = 1 – p2, p3 = estimated average of p1 and p2, q3 = estimated average of q1 and q2, Zα = the Z value corresponding to the alpha error (two-tailed), Zβ = the Z value corresponding to the beta error, and by taking variables that have association with ANC service satisfaction like time of initiation of ANC,16 frequency of ANC visits,16 history of stillbirth15 from different previous studies, the sample size was calculated. Then, the history of stillbirth was the variable that gave us the largest sample size of 506.
Finally, by comparing the sample sizes for the first and second objectives, the largest sample size was found to be 506 from the second objective, and by adding 10% for the non-response rate, the final sample size became 531.
Sampling technique
First, by taking the most recent quarterly (3 months) report of ANC users in each public health facility as a baseline, the monthly estimated number of pregnant women for ANC service was determined. Then, the number of pregnant women from each public health facilities was determined by proportionally allocating the calculated 531 sample size to the total number of pregnant women who received ANC services in 1 month. And then, systematic random sampling was applied to select the required number of study subjects.
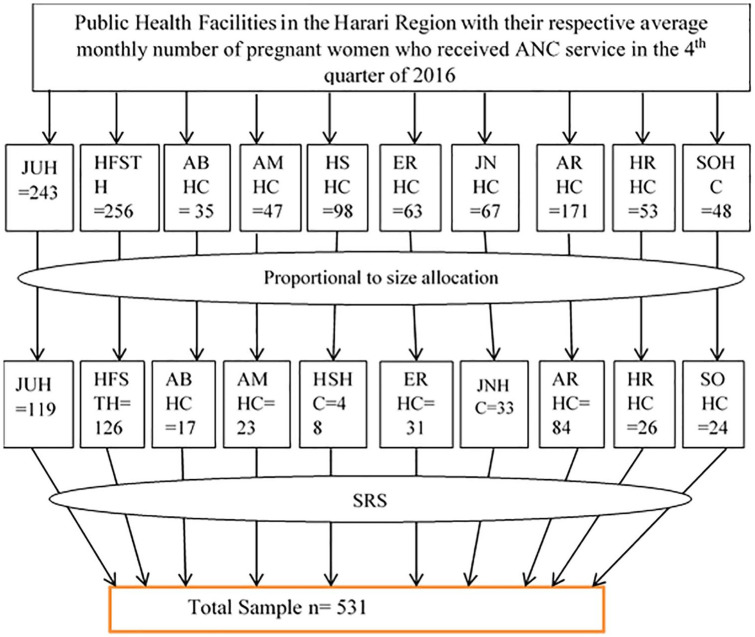
There were 3243 pregnant women who received ANC in all public health facilities, which implies that on average, 1081 pregnant women received ANC in each month in all public health facilities. By proportionally allocating the calculated 531 sample size to the total number of pregnant women who received ANC services in each month (531/1081), we found the sampling fraction as one-half (1/2). Then, every other pregnant woman registered for ANC services during the data collection period was recruited in each health facility for this study (Figure 1).
Figure 1.
Schematic representation of sampling method.
JHU = Jugol hospital, HFS = Hiwot Fana specialized teaching hospital, ABHC = Aboker Health center, AMHC = Amir-Nur Health Center, HSHC = Hasenge Health Center, ERHC = Erer Health Center, JNHC = Jenella Heath Center, ARHC = Arategna Health Center, HRHC = Harawe Health Center, SOHC = Sofi Health Center.
Measurement of pregnant women’s satisfaction with ANC
We used a questionnaire that contained socio-demographic characteristics, the obstetric profile of pregnant women, characteristics of the health facilities, and measure of satisfaction with the ANC services. The outcome variable satisfaction was assessed using a 5-point Likert-type scale ranging from very dissatisfied to very satisfied (1 = very dissatisfied, 2 = dissatisfied, 3 = neutral, 4 = satisfied, 5 = very satisfied points) with 29 measuring items. Then, very satisfied and satisfied were merged as “satisfied,” and neutral, dissatisfied, and very dissatisfied were merged as “unsatisfied” for the sake of regression analysis.27,28 Neutral responses were classified as dissatisfied considering that they may represent a fearful way of expressing dissatisfaction. This is likely because the interview was undertaken within the health facilities, and as a culture, mothers may have been reluctant to express their dissatisfaction with the services they received.
Then, the satisfaction of pregnant women with ANC services was measured using the following operational definitions:
Satisfied with ANC services = when a pregnant woman is scored satisfied with 22 or more of the 29 satisfaction measurement items. (Satisfied with 75% of the satisfaction measurement items)
Unsatisfied with ANC services = when a pregnant woman is scored satisfied with fewer than 22 satisfaction items. (Satisfied with <75% of the satisfaction measurement items)27,28
Data collection tools and quality
The data were collected using structured questionnaires and measurement scales that were adapted from reviewing the literature reviews.15,16,29,30 The questionnaires were translated into the local language, that is, Amharic, for data collection and then retranslated back into English. Two days of training was given to the data collectors and supervisors on the data collection tool and data collection procedure. The questionnaire was pretested on 5% of the sample size out of the study area in Haramaya hospital 1 month before the actual data collection period for the amendment of the questionnaires. The data collectors were 10 in number and supervised by two diploma nurses and the principal investigator. The data collectors and supervisors were non-staff members and women to make pregnant women feel more confidential and secured. The clients were interviewed using a direct face-to-face structured interview at the exit time after receiving the ANC services.
Data processing and analysis
After data collection, data were cleaned, checked for completeness, coded and entered into EpiData Version 3.1, and analyzed using SPSS Version 22.0 statistical software. Categorical variables were described using frequency, percentage, and tables. Continuous variables were assessed for normality and were described using the summary measures (mean and standard deviation (SD)). The outcome variable satisfaction was assessed using a 5-point Likert-type scale and then dichotomized “satisfied” and “unsatisfied” for the sake of regression analysis. Bivariable logistic regression analysis was used, and crude odds ratio (COR) was computed to assess the association between each independent and the outcome variables. Then, variables with a p-value <0.25 were included in the multivariable logistic regression analysis to control for all possible confounders. Hosmer–Lemeshow goodness-of-fit test was done to test for model fitness during multivariable logistic regression analysis. A multicollinearity test was carried out to see the correlation between the independent variables. The associated factors were identified by estimating the adjusted odds ratio (AOR) with 95% confidence interval (CI). Finally, statistical significance was declared at p < 0.05.
Results
From 531 sample size, a total of 516 pregnant women were enrolled in the study, giving a response rate of 97.4%.
Socio-demographic characteristics
The mean and SD age of the pregnant women was 23.9 ± 4.4 (range = 18–40) years. The majority of the respondents 209 (40.5%) were between 20 and 24 years of age. A total of 384 (74.4%) pregnant women were Muslim, and 299 (57.9%) were urban residents. A total of 212 (41.1%) pregnant women had no formal education. A total of 344 (66.7%) pregnant women were housewives and 514 (99.6%) were married (Table 1).
Table 1.
Socio-demographic characteristics of pregnant women attending antenatal care at public health facilities in the Harari region, eastern Ethiopia, February 2017.
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Age in years | 15–19 | 80 | 15.5 |
| 20–24 | 209 | 40.5 | |
| 25–29 | 160 | 31.0 | |
| 30–34 | 50 | 9.7 | |
| 35–39 | 15 | 2.9 | |
| 40–44 | 2 | 0.4 | |
| Religion | Orthodox | 113 | 21.9 |
| Muslim | 384 | 74.4 | |
| Protestant | 19 | 3.7 | |
| Residence | Urban | 299 | 57.9 |
| Rural | 217 | 42.1 | |
| Ethnicity | Oromo | 381 | 73.8 |
| Amhara | 75 | 14.5 | |
| Gurage | 30 | 5.8 | |
| Others | 30 | 5.8 | |
| Educational status | No formal education | 212 | 41.1 |
| Primary | 97 | 18.8 | |
| Secondary and above | 207 | 40.1 | |
| Occupation | Housewife | 344 | 66.7 |
| Merchant | 63 | 12.2 | |
| Employed | 77 | 14.9 | |
| Daily laborer | 12 | 2.3 | |
| Farmer | 16 | 3.1 | |
| Student | 4 | 0.8 | |
| Partner’s educational status | No formal education | 240 | 46.5 |
| Primary | 58 | 11.2 | |
| Secondary and above | 216 | 41.9 | |
| Has no partner | 2 | 0.4 | |
| Marital status | Married | 514 | 99.6 |
| Unmarried | 02 | 0.4 |
Obstetric and reproductive health profiles of participants
Among all pregnant women, 282 (54.7%) had at least one history of ANC visits. A total of 290 (56.2%) respondents initiated ANC within the first trimester of pregnancy, and for 347 (67.2%) pregnant women, their current visit was for the second or more visits. Regarding parity, 290 (56.2%) mothers were multiparous and 319 (61.8%) were multigravida mothers. Sixty-eight (13.2%) and 42 (8.1%) mothers had a history of stillbirth and a history of abortion, respectively (Table 2).
Table 2.
Obstetric and reproductive health profiles of pregnant women attending ANC at public health facilities in the Harari region, eastern Ethiopia, February 2017.
| Variables | Categories | Frequency | % |
|---|---|---|---|
| History of previous ANC | Yes | 282 | 54.7 |
| No | 234 | 45.3 | |
| Initiation time of ANC | 1st trimester | 290 | 56.2 |
| 2nd trimester | 189 | 36.6 | |
| 3rd trimester | 37 | 7.2 | |
| Frequency of ANC visit/current visit | First visit | 169 | 32.8 |
| Repeated visit | 347 | 67.2 | |
| Gravidity | Gravida 1 | 197 | 38.2 |
| Gravida 2–5 | 294 | 57.0 | |
| Gravida >5 | 25 | 4.8 | |
| Parity | Nulliparous | 202 | 39.1 |
| Multipara | 290 | 56.2 | |
| Grand multipara | 24 | 4.7 | |
| History of stillbirth | Yes | 68 | 13.2 |
| No | 448 | 86.8 | |
| History of abortion | Yes | 42 | 8.1 |
| No | 474 | 91.9 | |
| Status of current pregnancy | Intended | 496 | 96.1 |
| Unintended | 20 | 3.9 |
ANC: antenatal care.
Health service–related characteristics
Of all the participants, 273 (52.9%) pregnant women attended their ANC at the health centers and 396 (76.7%) mothers received ANC by female health professionals. A total of 440 (85.3%) participants had waited for 30 min or less in the health facility to get ANC service and 362 (70.2%) of the respondents had less than 20-min consultation time. A total of 445 (86.2%) pregnant women perceived as they had privacy during the examination. However, 296 (57.4%) pregnant women reported that healthcare providers did not explain the procedure before the examination. Working time was convenient for 501 (97.1%) respondents, and 371 (71.4%) pregnant women spent 30 min or less to reach the health facility (Table 3).
Table 3.
Health service characteristics of pregnant women attending ANC at public health facilities in the Harari region, eastern Ethiopia, February 2017.
| Variables | Categories | Frequency | % |
|---|---|---|---|
| Health facility type | Hospital | 243 | 47.1 |
| Health center | 273 | 52.9 | |
| Sex of ANC service provider | Female | 396 | 76.7 |
| Male | 120 | 23.3 | |
| Waiting time to get service | ⩽30 min | 440 | 85.3 |
| >30 min | 76 | 14.7 | |
| Duration of consultation time | ⩾20 min | 154 | 29.8 |
| <20 min | 362 | 70.2 | |
| Service provider explain the procedure before examination | Yes | 220 | 42.6 |
| No | 296 | 57.4 | |
| Privacy during examination | Yes | 445 | 86.2 |
| No | 71 | 13.8 | |
| The convenience of working time | Yes | 501 | 97.1 |
| No | 15 | 2.9 | |
| Time is taken to reach the health facility | ⩽30 min | 371 | 71.9 |
| >30 min | 145 | 28.1 |
ANC: antenatal care.
ANC service satisfaction among pregnant women
A total of 363 (70.3% (95% CI = 66.4%–74.3%)) pregnant women were satisfied with the ANC services offered at the public health facilities in the Harari region.
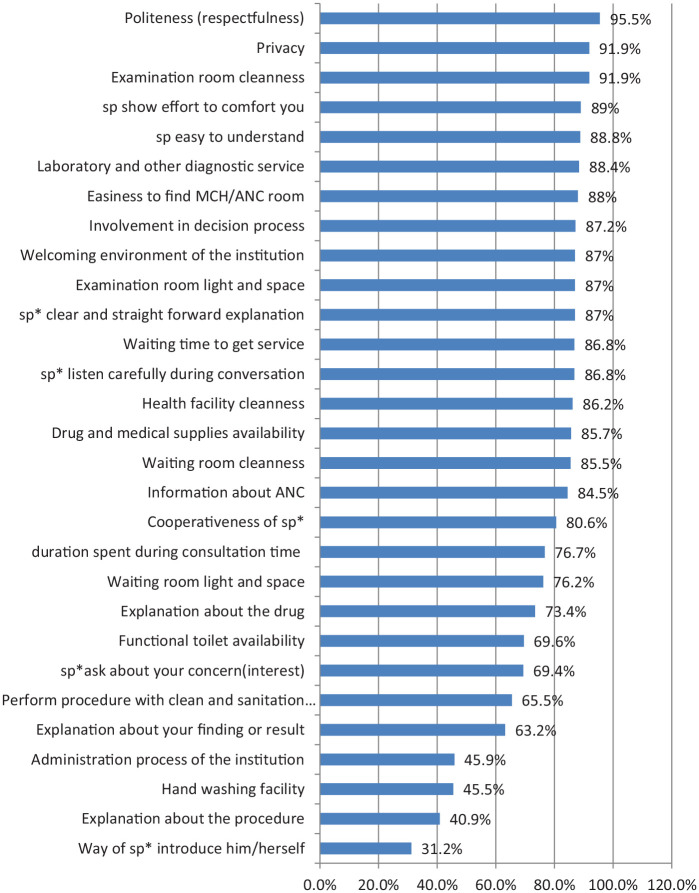
Of the 29 items used to measure the overall satisfaction of pregnant women with ANC services, examination room cleanness–related satisfaction (474 (91.9%)), patient privacy–related satisfaction (474 (91.9%)), and service provider’s politeness and/or respectfulness-related satisfaction (493 (95.5%)) were among the components with the highest satisfaction score. However, pregnant women’s satisfaction related to service provider explanation about the procedure (211 (40.9%)), the presence of handwashing facility in the institution (235 (45.5%)), and the administration process of institution (237 (45.9%)) were among the components with the lowest score (Figure 2).
Figure 2.
The percentages of items used to measure the overall ANC services satisfaction for pregnant women in public health facilities in the Harari region, eastern Ethiopia, February 2017.
Sp*: service provider.
Factors associated with pregnant women’s satisfaction with ANC services
Both bivariable and multivariable binary logistic regression analyses were done to identify the determinants of pregnant women’s satisfaction with ANC services. In multivariable logistic regression analysis, the odds of ANC satisfaction were 2.44 times higher among pregnant women who received the service in hospital than those who utilized in the health center (AOR = 2.44, 95% CI = 1.50–3.98). Women who attended no formal education and attended primary education had 2.53 and 2.17 higher odds of satisfaction with ANC services compared with those who had secondary and above education (AOR = 2.53, 95% CI = 1.52–4.20) and (AOR = 2.17, 95% CI = 1.17–4.04), respectively. Moreover, pregnant women who had more than one ANC visit had 4.62 times the odds of being satisfied with ANC services than those who had a first visit (AOR = 4.62, 95% CI = 2.98–7.17). Furthermore, the odds of pregnant women’s satisfaction were 1.74 times higher among women who initiated their ANC in the first trimester of pregnancy compared with those who had initiated after the first trimester of their pregnancy (AOR = 1.74, 95% CI = 1.12–2.71). Pregnant women who had no history of stillbirth had 2.52 times the odds of being satisfied with ANC services compared with their counterparts (AOR = 2.52, 95% CI = 1.37–4.65). Besides, pregnant women who waited for less than 30 min in the health facility to get service had 2.31 times higher odds of satisfaction with ANC than those who waited for more than 30 min (AOR = 2.31, 95% CI = 1.28–4.16) (Table 4).
Table 4.
Factors associated with ANC service satisfaction among pregnant women attending ANC at public health facilities in the Harari region, eastern Ethiopia, February 2017.
| Variables | Categories | Overall satisfaction | Crude OR (95% CI) | Adjusted OR (95% CI) | |
|---|---|---|---|---|---|
| Satisfied N (%) | Unsatisfied N (%) | ||||
| Type of health institution | Hospital | 188 (77.4) | 55 (22.6) | 1.91 (1.29–2.82) | 2.44 (1.50–3.98)* |
| Health center | 175 (64.1) | 98 (35.9) | 1 | ||
| Educational status of respondents | No formal education | 157 (74.1) | 55 (25.9) | 1.65 (1.09–2.51) | 2.53 (1.52–4.20)* |
| Primary | 75 (77.3) | 22 (22.7) | 1.97 (1.13–3.43) | 2.17 (1.17–4.04)**** | |
| Secondary and above | 131 (63.3) | 76 (36.7) | 1 | ||
| History of previous ANC | Yes | 207 (73.4) | 75 (26.6) | 1.38 (0.94–2.01) | 1.53 (0.99–2.35) |
| No | 156 (66.7) | 78 (33.3) | 1 | ||
| Frequency of current ANC visit | Revisit | 280 (80.7) | 67 (19.3) | 4.33 (2.89–6.47) | 4.62 (2.98–7.17)* |
| First visit | 83 (49.1) | 86 (50.9) | 1 | ||
| Time of initiation of ANC | Within the first trimester | 217 (74.8) | 73 (25.2) | 1.62 (1.11–2.38) | 1.74 (1.12–2.71)**** |
| After the first trimester | 146 (64.6) | 80 (35.4) | 1 | ||
| History of stillbirth | No | 327 (73.0) | 121 (27.0) | 2.40 (1.43–4.04) | 2.52 (1.37–4.65)** |
| Yes | 36 (52.9) | 32 (47.1) | 1 | ||
| History of abortion | Yes | 33 (78.6) | 9 (21.4) | 1.60 (0.74–3.43) | 1.66 (0.68–4.04) |
| No | 330 (69.6) | 144 (30.4) | 1 | ||
| Waiting time to get service | ⩽30 min | 321 (73.0) | 119 (27.0) | 2.18 (1.33–3.60) | 2.31 (1.28–4.16)*** |
| >30 min | 42 (55.3) | 34 (44.7) | 1 | ||
| Duration of consultation time | ⩾20 min | 119 (77.3) | 35 (22.7) | 1.64 (1.06–2.55) | 1.45 (0.87–2.42) |
| <20 min | 244 (67.4) | 118 (32.6) | 1 | ||
ANC: antenatal care; OR: odds ratio; CI: confidence interval.
Asterisk shows that the variable is significant at p-value: *p = 0.001; **p = 0.003; ***p = 0.005; ****p = 0.014 in multivariable logistic regression analyses.
Discussions
This study assessed pregnant women’s satisfaction with ANC services and associated factors in the Harari region of eastern Ethiopia. Accordingly, pregnant women’s satisfaction with ANC services was 70.3% (95% CI = 66.4%–74.3%), which is in line with a study conducted in Uganda (74.6%).31 This finding is lower than the study carried out in Sweden (82%) and Tigray Ethiopia (83.9%).18,32 However, the present finding is higher than studies in Pakistan (46%),33 Oman (59%),34 and studies in Ethiopia, for example, in Jimma (60.4%),15 Bahir Dar (52.3%),16 and Sidama (33.4%).17 This variation might be due to differences in service quality provided, the study setting, and the measurement used for the satisfaction assessment. Moreover, the variation may be due to difference in the study setting, this study includes both hospitals and health centers while the other studies15–17 included only the health centers. In fact, hospitals have better resources and infrastructure than health centers and there is a high chance of having quality services in the hospital than in the health centers.
Regarding the factors associated with pregnant women’s satisfaction with ANC, facility type, initiation of ANC in the first trimester of pregnancy, number of ANC visits, educational status, waiting time, and history of stillbirth were independently associated with ANC service satisfaction.
The educational status of pregnant women was significantly associated with ANC satisfaction. Women who did not attend formal education and attend primary education had 2.53 and 2.17 higher odds of satisfaction with ANC services compared with those who had secondary or higher education. This finding is congruent with studies in Malaysia35 and Sidama, Ethiopia.17 However, this is in contrast with studies conducted in Nepal and Nigeria.36,37 The possible reasons may be women with a higher level of schooling need more quality care for satisfaction since they have a better understanding about the service and know what to expect from that service.
The findings of this study indicated that the frequency of ANC visits was a significant factor for women’s satisfaction with ANC services. Pregnant women who had more than one ANC visit had 4.62 times the odds of being satisfied with ANC services than those who had the first visit. This was in agreement with findings in Nigeria,13 Riyadh,38 and Ethiopia,16,26 in which pregnant women’s satisfaction was significantly higher among women who had more visits. The positive association could be due to developing awareness of its importance by repeated visits, increasing client needs, and effective response to this need by the healthcare professional. Moreover, a satisfied woman is more likely to increase compliance with ANC visits.35
The 2016 WHO guideline recommends at least eight ANC visits, and the first visit should take place before the first trimester of pregnancy.10 We found a significant association between several ANC visits during the first trimester and satisfaction. The odds of pregnant women’s satisfaction was 1.74 times higher among women who initiated their ANC in the first trimester of pregnancy compared with those who had initiated after the first trimester of their pregnancy. This finding was consistent with previous studies in Malawi,39 Uganda,31 and Ethiopia.16,17 This might be because early initiation of ANC will increase pregnant women’s chance of having a repeated visit, which in turn affects the expectations and perception of pregnant women.
Furthermore, pregnant women who had no history of stillbirth had 2.52 times the odds of being satisfied with ANC services compared with their counterparts. This result is consistent with the results of a study done in Jimma town.15 The probable reason may be that the past pregnancy ends up in stillbirth, which may lead to having more expectations of the ANC services they need, and when the service they receive is below their expectations, there is a chance of dissatisfaction with the service.
Also, the health institution type and waiting time in the facility affect pregnant women’s satisfaction with the ANC. The odds of ANC satisfaction were 2.44 times higher among pregnant women who received the service in the hospital than those who utilized in the health center. Pregnant women who waited for less than 30 min in the health facility to get service had 2.31 times higher odds of satisfaction with ANC than those who waited for more than 30 min. This is supported by studies in China, Addis Ababa, and Jimma, Ethiopia.15,40,41 This difference might be because hospitals have better resources, including infrastructure, human power, medical equipment, and materials than health centers.
Limitation of the study
This finding is not without certain limitations. First, it is a cross-sectional study design, and the cause–effect relationship for all significant associations may not be established. Second, we included pregnant women irrespective of previous exposure, so women who were on their first visit could not be able to judge the quality of some components of services accurately. Finally, we included only public health facilities in the study setting. This may not be representative of pregnant women who are attending private facilities.
Conclusion
The proportion of satisfaction of pregnant women with ANC services was relatively high. More than two-thirds of pregnant women were satisfied with the ANC. Receiving ANC service from the hospital, having no formal education and having a primary education, having a repeated visit to ANC, initiating ANC services within the first trimester, having no history of stillbirth, and waiting for no more than 30 min in the health facility to get service were identified as positively significant associated factors with ANC service satisfaction. We recommend health facilities and stakeholders to give due attention to improving timely responsiveness and clinical care quality. They also should emphasize improving infrastructure in health facilities like hand washing and toilet facilities and reduce long waiting times to receive ANC.
Supplemental Material
Supplemental material, sj-pdf-1-smo-10.1177_2050312120973480 for Pregnant women’s satisfaction with antenatal care services and its associated factors at public health facilities in the Harari region, Eastern Ethiopia by Simon Birhanu, Melake Demena, Yohannes Baye, Assefa Desalew, Bedru Dawud and Gudina Egata in SAGE Open Medicine
Acknowledgments
We would like to acknowledge the staff of the Harari Regional Health Bureau, Harar City Municipality, public health facilities found in the Harari region, study participants, data collectors, and supervisors for cooperation.
Footnotes
Author contributions: S.B. initiated the research and drafted the manuscript, and the other authors contributed to the proposal writing, data entry, and analysis. All authors read and approved the final version of the manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical approval: Before starting the data collection process, ethical clearance was secured from the Haramaya University Institutional Health Research Ethics Review Committee (IHRERC) (Ref. No. IHRERC/0030/2017). Official letters were written from Haramaya University to the Harari Regional Health Bureau, and cooperation letters were written to all public health facilities in the region on which the study was carried out.
Informed consent: Written informed consent was obtained from all subject before the study.
ORCID iDs: Simon Birhanu  https://orcid.org/0000-0002-7852-5902
https://orcid.org/0000-0002-7852-5902
Assefa Desalew  https://orcid.org/0000-0001-6065-0708
https://orcid.org/0000-0001-6065-0708
Supplemental material: Supplemental material for this article is available online.
References
- 1. White Ribbon Alliance. Respectful maternity care: the universal rights of childbearing women, 2010, p. 1–6, https://www.whiteribbonalliance.org/wp-content/uploads/2017/11/Final_RMC_Charter.pdf
- 2. World Health Organization. Maternal mortality, Vol. 74, 2019, p. 601, https://www.who.int/news-room/fact-sheets/detail/maternal-mortality [Google Scholar]
- 3. UNICEF. Maternal mortality—UNICEF DATA. Unicef, 2019, http://data.unicef.org/topic/maternal-health/maternal-mortality
- 4. ICF CSA (CSA) [Ethiopia]. Ethiopia demographic and health survey 2016: key indicators report. Addis Ababa, Ethiopia; Rockville, MD: CSA and ICF, 2016 [Google Scholar]
- 5. WHO, UNICEF, UNFPA and the World Bank. Trends in maternal mortality 1990 to 2015. Estimates Developed by WHO, UNICEF, UNFPA and the World Bank, 2015, https://www.unfpa.org/sites/default/files/pub-pdf/9789241565141_eng.pdf
- 6. Lawn JE, Lee ACC, Kinney M, et al. Two million intrapartum-related stillbirths and neonatal deaths: where, why, and what can be done? Int J Gynecol Obstet 2009; 107(SUPPL.): S5–S19. [DOI] [PubMed] [Google Scholar]
- 7. World Health Organization (WHO). WHO maternal and reproductive health, 2016, http://who.int/mediacentre/factsheets/fs388/en/
- 8. Campbell OM, Graham WJ. Strategies for reducing maternal mortality: getting on with what works. Lancet 2006; 368(9543): 1284–1299. [DOI] [PubMed] [Google Scholar]
- 9. Haftu A, Hagos H, Mehari MA, et al. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray Public Health institutions, 2017: cohort study 11 medical and health sciences 1114 paediatrics and reproductive medicine 11 medical and heal. BMC Res Notes 2018; 11(1): 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization (WHO). WHO recommendations on antenatal care for a positive pregnancy experience: summary. World Heal Organ 2018; 10: 1–10. [PubMed] [Google Scholar]
- 11. World Health Organization. WHO recommendation on antenatal care for positive pregnancy experience. WHO Recomm Antenatal Care Posit Pregnancy Exp 2016; 2016: 152. [PubMed] [Google Scholar]
- 12. World Health Organization. WHO antenatal care randomized trial: manual for the implementation of the new model. 2002, pp. 1–42, https://apps.who.int/iris/handle/10665/42513
- 13. Nwaeze IL, Enabor OO, Oluwasola TAO, et al. Perception and satisfaction with quality of antenatal care services among pregnant women at the university college hospital, Ibadan, Nigeria. Ann Ib Postgrad Med 2013; 11(1): 22–28. [PMC free article] [PubMed] [Google Scholar]
- 14. Edie GE, Obinchemti TE, Tamufor EN, et al. Perceptions of antenatal care services by pregnant women attending government health centres in the Buea Health District, Cameroon: a cross sectional study. Pan Afr Med J 2015; 21: 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Chemir F, Alemseged F, Workneh D. Satisfaction with focused antenatal care service and associated factors among pregnant women attending focused antenatal care at health centers in Jimma town, Jimma zone, South West Ethiopia; a facility based cross-sectional study triangulated with qualitative study. BMC Res Notes 2014; 7(1): 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ejigu T, Woldie M, Kifle Y. Quality of antenatal care services at public health facilities of Bahir-Dar special zone, Northwest Ethiopia. BMC Health Serv Res 2013; 13(1): 443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Tesfaye DT, Mekonnen AH, Negesa BL. Maternal antenatal care service satisfaction and factors associated with rural health centers, Bursa District, Sidama Zone, Southern Ethiopia: a cross-sectional study. J Womens Heal Care 2017; 6(2): 1000363. [Google Scholar]
- 18. Fseha B. Assessment of mothers level of satisfaction with antenatal care services provided at Alganesh Health Center Shire, North West Tigray, Ethiopia. Biomed J Sci Tech Res 2019; 16(1): 11798–11802. [Google Scholar]
- 19. Press I, Ganey RF, Malone MP. Satisfied patients can spell financial well-being. Healthc Financ Manage 1991; 45(2): 34–63840. [PubMed] [Google Scholar]
- 20. Pascoe GC. Patient satisfaction in primary health care: a literature review and analysis. Eval Program Plann 1983; 6(3–4): 185–210. [DOI] [PubMed] [Google Scholar]
- 21. Finlayson K, Downe S. Why do women not use antenatal services in low- and middle-income countries? A meta-synthesis of qualitative studies. PLoS Med 2013; 10(1): 1001373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Okedo-Alex IN, Akamike IC, Ezeanosike OB, et al. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ Open 2019; 9(10): 031890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Christiaens W, Bracke P. Assessment of social psychological determinants of satisfaction with childbirth in a cross-national perspective. BMC Pregnan Childbirth 2007; 7: 1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Bleich SN, Ozaltin E, Murray CJL. How does satisfaction with the health-care system relate to patient experience. Bull World Health Organ 2009; 87(4): 271–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kloos H, Etea A, Degefa A, et al. Illness and health behaviour in Addis Ababa and rural central Ethiopia. Soc Sci Med 1987; 25(9): 1003–1019. [DOI] [PubMed] [Google Scholar]
- 26. Lakew S, Ankala A, Jemal F. Determinants of client satisfaction to skilled antenatal care services at Southwest of Ethiopia: a cross-sectional facility based survey. BMC Pregnan Childbirth 2018; 18(1): 1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mekonnen ME, Yalew WA, Anteneh ZA. Women’s satisfaction with childbirth care in Felege Hiwot Referral Hospital, Bahir Dar City, Northwest Ethiopia, 2014: cross sectional study women’s health. BMC Res Notes 2015; 8(1): 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tayelgn A, Zegeye DT, Kebede Y. Mothers’ satisfaction with referral hospital delivery service in Amhara Region, Ethiopia. BMC Pregnan Childbirth 2011; 11: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Matejić B, Milićević MT, Vasić V, et al. Maternal satisfaction with organized perinatal care in Serbian public hospitals. BMC Pregnan Childbirth 2014; 14(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. (UNICEF) UNCF. Antenatal care in Kosovo: quality and access. Calif Manage Rev 2009; 2009: 52, https://womensnetwork.org/wp-content/uploads/2018/10/20130510124417860.pdf [Google Scholar]
- 31. Tetui M, Ekirapa EK, Bua J, et al. Quality of antenatal care services in eastern Uganda: implications for interventions. Pan Afr Med J 2012; 13: 27–15. [PMC free article] [PubMed] [Google Scholar]
- 32. Hildingsson I, RÃ¥destad I. Swedish women’s satisfaction with medical and emotional aspects of antenatal care. J Adv Nurs 2005; 52(3): 239–249. [DOI] [PubMed] [Google Scholar]
- 33. Majrooh MA, Hasnain S, Akram J, et al. Coverage and quality of antenatal care provided at primary health care facilities in the “Punjab” province of Pakistan. PLoS ONE 2014; 9(11): 113390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ghobashi M, Khandekar R. Satisfaction among expectant mothers with antenatal care services in the Musandam region of Oman. Sultan Qaboos Univ Med J 2008; 8(3): 325–332. [PMC free article] [PubMed] [Google Scholar]
- 35. Rahman MM, Ngadan DP, Arif MT. Factors affecting satisfaction on antenatal care services in Sarawak, Malaysia: evidence from a cross sectional study. Springerplus 2016; 5(1): 725. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Fagbamigbe AF, Idemudia ES. Assessment of quality of antenatal care services in Nigeria: evidence from a population-based survey. Reprod Health 2015; 12(1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Joshi C, Torvaldsen S, Hodgson R, et al. Factors associated with the use and quality of antenatal care in Nepal: a population-based study using the demographic and health survey data. BMC Pregnancy Childbirth 2014; 14(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Kamil A, Khorshid E. Maternal perceptions of antenatal care provision at a tertiary level hospital, Riyadh. Oman Med J 2013; 28(1): 33–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Lungu F, Malata A, Chirwa E, et al. Quality assessment of focused antenatal care services in Malawi. Afr J Midwifery Womens Health 2011; 5(4): 169–175. [Google Scholar]
- 40. Sun J, Lin Q, Zhao P, et al. Reducing waiting time and raising outpatient satisfaction in a Chinese public tertiary general hospital-an interrupted time series study. BMC Public Health 2017; 17(1): 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Bekana M, Negash S, Yusuf L. Client satisfaction on antenatal care service by pregnant women in public and private hospitals in Addis Ababa, Ethiopia: a cross-sectional comparative descriptive study. J Gynecol Reprod Med 2020; 4(1): 1–8. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-smo-10.1177_2050312120973480 for Pregnant women’s satisfaction with antenatal care services and its associated factors at public health facilities in the Harari region, Eastern Ethiopia by Simon Birhanu, Melake Demena, Yohannes Baye, Assefa Desalew, Bedru Dawud and Gudina Egata in SAGE Open Medicine