Abstract
Aim
Building strategies for the country‐level dissemination of Kangaroo mother care (KMC) to reduce the mortality rate in preterm and low birth weight babies and improve quality of life. KMC is an evidence‐based healthcare method for these infants. However, KMC implementation at the global level remains low.
Methods
The international network in Kangaroo mother brought 172 KMC professionals from 33 countries together for a 2‐day workshop held in conjunction with the XIIth International KMC Conference in Bogota, Colombia, in November 2018. Participants worked in clusters to formulate strategies for country‐level dissemination and scale‐up according to seven pre‐established objectives.
Results
The minimum set of indicators for KMC scale‐up proposed by the internationally diverse groups is presented. The strategies for KMC integration and implementation at the country level, as well as the approaches for convincing healthcare providers of the safety of KMC transportation, are also described. Finally, the main aspects concerning KMC follow‐up and KMC for term infants are presented.
Conclusion
In this collaborative meeting, participants from low‐, middle‐ and high‐income countries combined their knowledge and experience to identify the best strategies to implement KMC at a countrywide scale.
Keywords: health plan implementation, Kangaroo mother care, low birth weight infants, premature infants
Abbreviations
- KMC
Kangaroo mother care
- ENAP
Every newborn action plan
Key Notes.
Kangaroo mother care (KMC) is an evidence‐based method of caring for preterm and low birth weight infants.
The XIIth International KMC conference discussed topics around indicators for KMC scale‐up, strategies for KMC integration and implementation at country level, safe KMC transportation, KMC follow‐up and skin‐to‐skin care for term infants.
KMC is no longer perceived as an alternative for the poor, but as a universal best‐care tool.
1. BACKGROUND
Preterm birth is now the leading global cause of mortality in infants under 5 years of age (16%) and an important cause of disability and loss of human potential. 1 , 2 Kangaroo mother care (KMC) is a method developed in 1978 in Bogota, Colombia, for caring for low birth weight infants weighing less than 2500 g and/or preterm infants under 37 weeks’ gestational age. 3 KMC includes the kangaroo position with continuous skin‐to‐skin contact between mother and infant with exclusive breastfeeding and follow‐up after discharge. 4 The World Health Organization currently recommends KMC for clinically stable newborn infants weighing 2000 g or less at birth. 5 Enough scientific evidence is currently available on its improved outcomes, including short‐ and long‐term physical and mental health benefits. 6 , 7 , 8 , 9
Kangaroo mother care is an important intervention towards the realisation of United Nation's Sustainable Development Goal 3: ensure healthy lives and promote well‐being for all at all ages. 6 , 7 , 10 , 11 As KMC is vital for the survival, well‐being and development of small or preterm newborn infants, it can contribute significantly to the achievement of Target 3.2, which focuses on ending preventable neonatal deaths, with each country aiming for a neonatal mortality rate of less than 12 per 1000 live births by 2030. 10 Despite clear evidence of its many benefits, the global implementation of KMC has encountered resistance. 12 Reasons include social and cultural barriers, reluctance of healthcare providers to help parents care for their fragile infants and merely sporadic inclusion of KMC in national newborn infant priorities and policies. 13 , 14
The International Network in KMC was established in 1996 and aims to facilitate the sharing of new scientific evidence and innovative solutions to promote KMC implementation among professionals. The 2018 workshop focused on strategies for the integrated dissemination of KMC at national level, and the workshop outputs are the basis for this article.
2. METHOD
The XIIth International KMC Conference held at the Pontificia Universidad Javeriana in Bogotá, Colombia, from 14 to 17 November 2018 was attended by professionals from low‐,middle‐ and high‐income settings who included doctors, paediatricians, neonatologists, nurses, midwives, psychologists, physiotherapists, public health experts and programme managers. The conference comprised a 2‐day workshop, followed by a 2‐day scientific congress. Facilitated groups including 172 participants coming from 33 countries worked together to elaborate strategies for country‐level dissemination and scale‐up of KMC across seven pre‐established topics (Table 1). At the congress, each group presented the strategies for further participant discussion (n = 290 from 43 countries).
TABLE 1.
Workshop's specific objectives
| Workshop's specific objectives |
|---|
| 1. Minimum set of indicators to assess dissemination at country level |
| 2. Integrating KMC to the objectives of NGOs, development partners and other institutions (public and private) |
| 3. Implementation of KMC in all hospitals in a country |
| 4. KMC transportation |
| 5. All on board: Ministry of health, academia and professional associations |
| 6. Systems for follow‐up |
| 7. KMC for term infants |
3. RESULTS
3.1. Minimum set of indicators for assessing dissemination at country level
Indicators play a critical role in simplifying complex data to facilitate monitoring and evaluation of heath interventions. 15 This group discussed the indicators needed for priority‐setting in terms of national KMC coverage and impact, as well as information required by the public and investment and policy decision makers. Discussions were based on the measurement of strategic objectives of the “Every Newborn Action Plan” (ENAP) 16 , 17 (Figure 1). Indicators developed by the Colombian Kangaroo Foundation in collaboration with the Colombian Health Ministry were also considered. The latter indicators were derived from information obtained from over 40,000 KMC infants at three centres of excellence in Colombia and include processes and outcomes at both 40 weeks’ corrected gestational age and 1 year 18 , 19 (Table 2).
FIGURE 1.
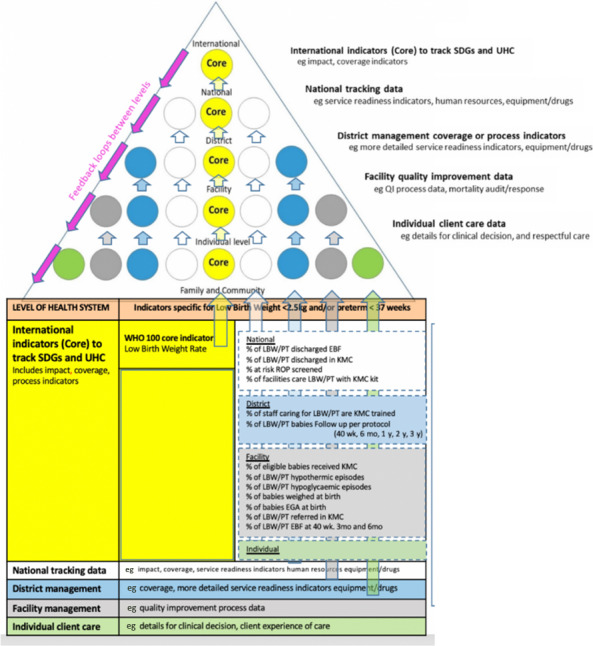
Routine data needs of different health system levels, adapted for kangaroo mother care. Based on: Louise T. Day et al, Chapter 5 “Use Data for Action” (Figure 5.1) “Survive and Thrive Transforming care for every small and sick newborn” WHO 2019
TABLE 2.
Colombian quality KMC indicators for processes and outcomes a
| Stage of KMC practice | Adherence indicators | Outcomes indicators |
|---|---|---|
| Immediately after birth |
|
Parent satisfaction |
| Intra‐hospital KMC programme in the NCU |
|
|
| Intra‐hospital KMC programme in the KMC ward |
|
|
| KMC from discharge at home up to 40 wk gestational age |
|
|
| KMC from 40 wk to 12 mo corrected age |
|
|
Abbreviations: NCU, neonatal care unit; NICU, neonatal intensive care unit; ROP, retinopathy of prematurity.
A Taskforce coordinated by ‘Fundacion Canguro’ produced a detailed implementation and quality assurance plan for the Colombian Ministry of Health in (year), including process (adherence) and outcome quality indicators. 18
The ENAP measurement improvement roadmap (2015‐2020) aims to transform global measurement for newborn infants to enable the use of data to track progress towards the 2030 targets of the Sustainable Development Goals. KMC is one of the selected core coverage indicators currently being validated. 20 The workshop group used the data pyramid 20 to discuss the way countries choose which indicators to measure and the levels of the health system at which to measure them. Agreement on core KMC indicators is vital for national and international tracking of progress, but the selection of indicators for measurement at subnational, at district level, facility and individual levels requires country prioritisation. Figure 1 illustrates the proposed minimum set of indicators necessary to evaluate the strategy of KMC diffusion discussed in other workshop groups 21 .
3.2. Integrating KMC with the objectives of different partners and institutions
This group discussed the integration of KMC with the objectives of non‐governmental organisations, development partners and other public and private institutions, by looking specifically at barriers and recommendations across four areas (Table 3) :
Standard definition of KMC in the creation of KMC programmes, without simplifying the method;
best practices to support the first implementation of a KMC programme and promote sustainability;
set of accessible KMC manuals; and
aligning public and private providers of KMC.
TABLE 3.
Barriers and recommendations for integrating KMCs objectives
| Barriers | Recommendations and next steps | |
|---|---|---|
| Standardisation of KMC’s definition |
|
|
| Supporting first implementation of a KMC programme and promoting sustainability |
|
|
| Compiling KMC manuals that are accessible |
|
|
| Aligning public and private providers for KMC |
|
|
Kangaroo position as soon as possible, kangaroo nutrition based on exclusive breastfeeding and kangaroo discharge policies: home discharge in kangaroo position in an outpatient KMC follow‐up clinic.
3.3. Implementation of KMC in all hospitals in a country
This working group lobbied for state policies on KMC led by the national Ministry of Health, as well as routine positive reinforcement across the spectrum ranging from government bodies to health facilities. Collaboration between government, academia and KMC programmes was identified as a priority in ensuring KMC implementation in all hospitals in a country. This collaboration would require the establishment of effective intersectoral coordination mechanisms at central and local levels of KMC implementation (Table 4).
TABLE 4.
Levels/ steps of KMC implementation to facilitate hospital adoption
| Stage | Levels/steps to hospital‐level adoption of the KMC program |
|---|---|
| Planning and initiation of the KMC programme in the hospital (infrastructure and training) |
|
| Sustaining the KMC programme (hospital budget, human resources) |
|
| Facilitate ambulatory KMC follow‐up units |
|
| Periodic assessment of the KMC program |
|
To fulfil basic hospital requirements for KMC implementation (Table 5), welcoming parents in the neonatal intensive care unit 24 hours a day, 7 days a week is an initial step towards a KMC‐friendly environment. Strategies for increasing families’ adherence to KMC include hosting families of hospitalised preterm infants by providing housing, food and transportation facilities. KMC implementation depends on identifying possible solutions to parental difficulties such as geographical barriers, financial limitations, lack of family support or paid family leave and medical problems.
TABLE 5.
Basic hospital needs for KMC implementation
| Facility preparedness for kangaroo mothers |
|
| KMC method in general |
|
The group also discussed a perceived need for more trained KMC champions and leaders from health centres, hospitals and the community. This would include adding KMC to health professions’ curricula and creating a separate manual for community KMC. Community involvement to diffuse KMC might be possible with surrogate KMC providers and community health agents to support the mother after discharge. Participants emphasised the need for the establishment of culturally adaptable KMC ambulatory programmes with the necessary infrastructure, equipment and personnel. They advocated mother‐friendly laws, such as extended and paid family leave, as well as education and empowerment of mothers, fathers and the community. Additionally, they highlighted the importance of capturing hospital data and using statistics on deliveries, preterm infants, low birth weight infants, length of stay in the neonatal intensive care unit, morbidity, mortality and other infant outcomes. Periodic assessment of quality indicators of KMC implementation was also recommended. Lastly, participants stressed the importance of conducting periodic surveys to ensure baseline knowledge of KMC implementation. 14 The results of these surveys should inform the actions of professionals, leaders and policymakers.
3.4. KMC transportation
Methods of neonatal transportation vary widely by geographical area, and there is insufficient knowledge of the use of KMC for neonatal transport. In countries like Brazil, Spain, South Africa and Colombia, incubators are used for inter‐facility transport and transport from community to health facilities. In India, a home‐made styrofoam box with two openings for inserting feeding and oxygen tubes and an X‐ray film for monitoring the baby is used. Neonates are carried skin‐to‐skin or on the lap of an adult in rural India. In South Africa, private cars are used for transport within the community. In Mali, Cameroon and Malawi, babies are wrapped and placed between two 1.5‐L bottles filled with hot water. In Belgium, skin‐to‐skin contact has been the favourite mode of back transfer in the neonatal department of Erasme Hospital for the last 3 years. 22 Participants regarded the lack of policy on KMC between national government, regional authorities and hospitals as a major challenge in implementing KMC neonatal transport. Health personnel do not advocate this mode of transport because they have not been trained in KMC transport and it is not practised at their workplace. Other barriers are resistance to using KMC for transportation and parents’ uneasiness about the kangaroo position, especially for unstable infants.
An initial step in informing and convincing primary healthcare centres and first‐level hospitals of the safety and efficiency of KMC transportation is to create a manual and incorporate these guidelines into the curricula of health professionals. Participants recommended using KMC transport not only between hospitals (if the baby is stable) but also within hospitals.
3.5. Getting health ministries, academia and professional associations on board
This group worked to identify conditions for engagement in KMC implementation and scale‐up. Collaboration between ministries, academia and professional bodies and the strengthening of various components of their activities has been identified as essential for bridging the policy‐implementation gap in KMC.
Participants used a previously developed stages‐of‐change model for KMC implementation (Figure 2) to frame the conditions and steps needed to accelerate implementation. 13 As these may differ, depending on whether KMC has already been implemented in a country or not, a situational analysis is recommended to assess quality and coverage of essential newborn infant care and the nature of existing KMC services. Results of the situational analysis should be validated on existing evidence. Once implementation is underway, an adequate monitoring system is essential to generate statistics, which could include indicators on implementation outcomes and cost‐effectiveness, morbidity and mortality, quality of life, impact on children's developmental and parental outcomes (Figure 2). Participants also discussed the snowball effect of establishing a KMC programme reference centre to serve as a model centre and demonstration site. Once this centre is established, more centres of excellence could be implemented to make KMC programmes available throughout a country. In addition, centres of excellence could provide education on KMC to future health professionals.
FIGURE 2.
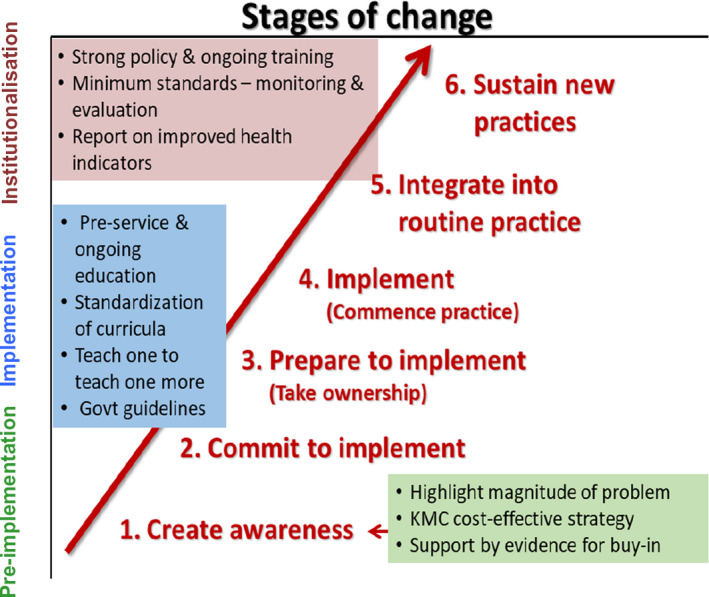
Conditions for engagement and progress with KMC implementation and scale‐up
3.6. Establishing KMC follow‐up systems to assure safety and document benefits
Different institutions have established outpatient KMC programmes for the ambulatory care and systematic follow‐up of high‐risk newborn infants at least during their first year of life. Infants are discharged to a KMC outpatient clinic where the continuation of hospital initiated kangaroo position and nutrition (ambulatory phase of KMC) takes place. This phase, which usually concludes when the infant reaches term (40 weeks after conception), is focused on assisting the late transition to extrauterine life until the infant achieves the so‐called “stable growth period”. After that, many KMC outpatient clinics also provide high‐risk neonate follow‐up programmes extending from term to at least 1 year of corrected age, focused not only on survival but on quality of life. Nevertheless, these programmes are usually not established as national follow‐up systems, but in many countries, they are the only opportunity for these infants to have a high‐risk follow‐up.
Colombia with its 53 outpatient KMC programmes has an advanced KMC follow‐up system for infants born premature or with less than 2500 g, with official guidelines developed by the Kangaroo Foundation and adopted nationally by the Ministry of Health. 23 However, there are limited data on compliance with national recommendations, as there is no adequate KMC monitoring system. The group believed that compliance could be increased if KMC could be initiated as soon as possible during hospitalisation and if follow‐up took place at the same city where hospital‐based KMC was provided, given that follow‐up rates fall when families come from diverse and isolated populations. The minimum requirements for scaling up a high‐risk follow‐up system at country level should include written national KMC guidelines.
3.7. KMC for term infants: state of the art
This group wrote a “Resolution of the international network of KMC about skin‐to‐skin care for full‐term newborn infants” (Appendix S1). The preamble states that “Skin‐to‐skin care is the ideal habitat for initial physiological and behavioural development of the full‐term newborn infant and is the foundation of optimal health and development throughout life”. Indeed, skin‐to‐skin care promotes physiological stability, increases and maintains appropriate infant body temperature, as well as rewarming babies and preventing hypothermia 24 , 25 even in the term infant. The only difference between term and preterm infants regarding KMC is the duration of the Kangaroo position given that term babies can already regulate their temperature and will only tolerate short periods in the kangaroo position. KMC reduces the pain of procedures, provides increased protection against pathogens and reduces rates of infection. 23 It also increases initiation, duration and exclusivity of breastfeeding; improves sucking competence; and increases milk production. It lengthens good sleep periods, improves alertness, increases non‐distressed vocalisations, social interactions and awareness and reduces crying. 24 Furthermore, it can provide comfort and a sense of security, protect infants from the negative effects of separation and facilitate maternal‐infant interactions, promoting bonding and attachment. 26 Given the benefits, participants proposed that initial skin‐to‐skin care is the natural state in which all newborn infants should receive comfort, nutrition and security. All mothers or designated caregivers should practise skin‐to‐skin care, regardless of the feeding method, immediately after birth for all stable newborn infants. In those who were initially unstable at birth, skin‐to‐skin care should be initiated as soon as possible.
4. DISCUSSION
The XIIth international conference on KMC focused on collaboratively building the best strategy for country‐level dissemination and scale‐up of the Kangaroo method, including rigorous follow‐up. To date, diffusion of KMC in many countries has typically been carried out by KMC centres working independently without health system integration or KMC networks. During this conference, health professionals from around the world reviewed current evidence and experience with local implementation to build a roadmap for systematic dissemination of KMC at scale. Prior to implementation of KMC, the following should be evaluated: size and location of the target population; enabling policies; estimated cost of implementation; existing national resources including centres of excellence for training; local barriers; and access to KMC kits. These should include lycra bands or other binders for kangaroo positioning, a small cap, socks and a sleeveless shirt. Once this information is available, a second step would be to understand the quality of KMC practice: Are KMC protocols available, according to the level of care? Is KMC transportation available? How is KMC follow‐up organised? Are the eligibility criteria for the KMC ward or for home discharge available in writing? Does KMC follow‐up at home occur up to a gestational age of 40 weeks? Are high‐risk follow‐up services provided for up to 1 or 2 years of corrected age? The collection of this information is imperative for implementing quality KMC countrywide.
Kangaroo mother care is a complex intervention. Integrated and coordinated implementation throughout a country requires close involvement of several partners. First, hospitals should provide the minimum set of inputs required to deliver quality KMC to patients. Secondly, scientific societies and training institutions should promote KMC knowledge transfer to under‐ and post‐graduate students and conduct local KMC research. Finally, government is responsible for promoting KMC and developing national KMC guidelines, minimum standards and supportive policies (Table 4).
The working groups suggested key responsibilities for government, academia and professional bodies in KMC implementation and scale‐up. The role of government and national agencies could include incorporating and integrating KMC into national policies and programmes. For academia, priority initiatives for creating uniformity in KMC across a country could include the incorporation of KMC into medical and health sciences curricula as an integral part of training in newborn infant care. Professional bodies should be urged to have KMC as a standing agenda item for meetings and to use current updated evidence in their dissemination activities. Professionals to target include paediatricians, neonatologists, nurses, midwives, obstetricians, therapists, community specialists and social workers. Specific detailed dissemination, implementation and monitoring strategies were not discussed by the working groups.
At the hospital level, there are two subgroups of needs: infrastructure for families and babies; and human resources with competencies in neonatal care and KMC. In low‐income countries, participants agreed that necessities included drinking water and running water and soap in the neonatal unit, the ward, and the ambulatory programme. Additional needs for mothers are food, comfortable chairs, beds, lycra bands or other binders to secure babies in KMC position. Needs for babies include oxygen cannulas to enable feeding and holding the baby in the kangaroo position as soon as possible. Open neonatal units would enable mothers to remain with their babies and express milk and/or feed directly at the breast.
For KMC programme implementation and sustainability, infrastructure and staff should be accounted for, as well as dissemination costs at country level, but possible savings through reducing the number of days of hospitalisation should be considered. While KMC is a low‐cost intervention, it is not a no‐cost intervention. A careful and realistic identification of implementation and running costs must be made to properly plan and execute a sustainable KMC program. In hospital, KMC involves training and allocation of additional human resources, access to space to accommodate mothers and families within neonatal care facilities. Ambulatory KMC clinics do have human and physical resources needs (office space, equipment, supplies, health care providers, administrative support, etc) which must be provided on a continuous and reliable basis to support ambulatory KMC and high‐risk follow‐up activities at least during the first year of corrected age as a minimum. 27 Each country's economic burden of care for these infants will depend on the available investments in survival and quality of life. As the cost of a KMC programme is based on volume of cases, institutions attending to deliveries with high‐risk neonates are encouraged to implement intra‐hospital programmes, complemented by ambulatory programmes able to receive babies from several institutions.
All groups agreed on the importance of systems for monitoring compliance with ambulatory KMC (at hospital and patient level). Participants did not have direct experience or adequate knowledge of community follow‐up care for high‐risk KMC babies after discharge because to date many countries are still working to ensure survival rather than quality of life after survival; however, they suggested following strategies such as those developed by the World Health Organization for the Integrated Management of Newborn and Childhood Illnesses. 28
The strength of this report is that information was derived from participants representing 33 countries. This enabled the collection of rich contextual data on KMC practice and implementation across the globe. It is, however, acknowledged that the views expressed were those of workshop participants and may not necessarily reflect the true state of KMC implementation in some of the countries.
5. CONCLUSION
Over the years, the conferences and workshops facilitated by the international network in KMC have become strategic meetings where KMC scientists, researchers and practitioners meet and share best practices, innovations, successes and challenges in KMC implementation. At the XIIth international KMC Conference in 2018, participants used their combined knowledge and experiences to propose a way forward for providing access to KMC to infants around the world irrespective of country of origin. We acknowledged that KMC is no longer perceived as an alternative for the poor, but as a tool for the best care of premature and low birth weight infants in low‐, middle‐ and high‐income settings. To further strengthen scale‐up of high quality KMC globally, the 2018 workshop identified the need for more focus on national policies and KMC protocols and agreed on core KMC process and outcome indicators and the integrated and coordinated dissemination of KMC. Furthermore, KMC‐trained multidisciplinary staff and the establishment of a network of Kangaroo community leaders to support new parents are vital to promote dissemination of KMC as a standard of care for all premature or low birth weight infants. The knowledge summarised in this paper combined with the available scientific evidence of KMC benefits must be used to further support the extension of KMC coverage to the 15 million preterm and low birth weight KMC candidates who are born each year.
CONFLICT OF INTEREST
The authors have no conflict of interest to declare.
Supporting information
ACKNOWLEDGEMENTS
The authors express their sincere gratitude to all the workshop participants for sharing their knowledge and experience.
Charpak N, Angel MI, Banker D, et al. Strategies discussed at the XIIth international conference on Kangaroo mother care for implementation on a countrywide scale. Acta Paediatr. 2020;109:2278–2286. 10.1111/apa.15214
Funding information
The international conference was funded by Pontificia Javeriana University, San Ignacio Hospital, Colombian Ministry of Health, Colombian Health Insurance Companies, (Compensar, Aliansalud) New Venture Fund for Global Policy and Advocacy Award and the Kangaroo Foundation (Fundación Canguro). The writing of this article did not receive any funding.
REFERENCES
- 1. Lawn JE, Blencowe H, Oza S, et al. Every newborn: progress, priorities, and potential beyond survival. Lancet. 2014;384(9938):189‐205. [DOI] [PubMed] [Google Scholar]
- 2. Liu L, Oza S, Hogan D, et al. Global, regional, and national causes of under‐5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. Lancet. 2016;388(10063):3027‐3035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ruiz‐Peláez JG, Charpak N, Cuervo LG. Kangaroo Mother Care, an example to follow from developing countries. BMJ. 2004;329(7475):1179‐1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Charpak N, Ruiz JG, Zupan J, et al. Kangaroo mother care: 25 years after. Acta Paediatr. 2005;94(5):514‐522. [DOI] [PubMed] [Google Scholar]
- 5. World Health Organization . Kangaroo Mother Care: A Practical Guide. Geneva: World Health Organization; 2003. [Google Scholar]
- 6. Boundy EO, Dastjerdi R, Spiegelman D, et al. Kangaroo mother care and neonatal outcomes: a meta‐analysis. Pediatrics. 2016;137(1):e20152238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Conde‐Agudelo A, Díaz‐Rossello JL. Kangaroo mother care to reduce morbidity and mortality in low birthweight infants. Cochrane Database Syst Rev. 2016;8:CD002771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Charpak N, Tessier R, Ruiz JG, et al. Twenty‐year follow‐up of kangaroo mother care versus traditional care. Pediatrics. 2017;139(1):e20162063. [DOI] [PubMed] [Google Scholar]
- 9. Tessier R, Cristo M, Vellez S, et al. Kangaroo mother care: a method for protecting high risk LBW and premature infants against developmental delay. Infant Behav Dev. 2003;26:384‐397. [Google Scholar]
- 10. United Nations Development Program . Sustainable Development Goals ‐ Goal 3: Health and wellbeing; 2018. http://www.undp.org/content/undp/en/home/sustainable-development-goals/goal-3-good-health-and-well-being.html. Accessed December 11, 2019.
- 11. Lawn JE, Mwansa‐Kambafwile J, Horta BL, Barros FC, Cousens S. 'Kangaroo mother care' to prevent neonatal deaths due to preterm birth complications. Int J Epidemiol. 2010;39(Suppl 1):i144‐i154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Engmann C, Wall S, Darmstadt G, Valsangkar B, Claeson M. Consensus on kangaroo mother care acceleration. Lancet. 2013;382(9907):e26‐e27. [DOI] [PubMed] [Google Scholar]
- 13. Cattaneo A, Amani A, Charpak N, et al. Report on an international workshop on kangaroo mother care: lessons learned and a vision for the future. BMC Pregnancy Childbirth. 2018;18(1):170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Engler AJ, Ludington‐Hoe SM, Cusson RM, et al. Kangaroo care: national survey of practice, knowledge, barriers, and perceptions. MCN Am J Matern Child Nurs. 2002;27(3):146‐153. [DOI] [PubMed] [Google Scholar]
- 15. Von Schirnding Y. Health in Sustainable Development Planning: The Role of Indicators. Geneva: World Health Organization; 2002. [Google Scholar]
- 16. Moxon SG, Ruysen H, Kerber KJ, et al. Count every newborn: a measurement improvement roadmap for coverage data. BMC Pregnancy Childbirth. 2015;15(Suppl 2):S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Guenther T, Moxon S, Valsangkar B, et al. Consensus‐based approach to develop a measurement framework and identify a core set of indicators to track implementation and progress towards effective coverage of facility‐based Kangaroo Mother Care. J Glob Health. 2017;7(2):020801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Charpak N, Villegas J.Actualización de los lineamientos técnicos para la implementación de Programas Madre Canguro en Colombia, con énfasis en la nutrición del neonato prematuro o de bajo peso al nacer. Ministerio de Salud; 2017. http://fundacioncanguro.co/wp-content/uploads/2017/10/implementacion-programa-canguro1.pdf Accessed December 11, 2019. [Google Scholar]
- 19. Canguro Fundación . Portal de Formación en Método Madre Canguro; 2016. http://fundacioncanguro.co/KMCT/en/ Accessed December 11, 2019.
- 20. Day LT, Ruysen H, Gordeev VS, et al. "Every Newborn‐BIRTH" protocol: observational study validating indicators for coverage and quality of maternal and newborn health care in Bangladesh, Nepal and Tanzania. J Glob Health. 2019;9(1):010902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. World Health Organization . Survive and thrive: transforming care for every small and sick newborn (Fig 5.1). Geneva: World Health Organization; 2019. https://www.who.int/maternal_child_adolescent/documents/care-small-sick-newborns-survive-thrive/en/ Accessed December 11, 2019. [Google Scholar]
- 22. Hennequin Y, Grevesse L, Gylbert D, Albertyn V, Hermans S, Van Overmeire B. Skin‐to‐skin back transfers provide a feasible, safe and low‐stress alternative to conventional neonatal transport. Acta Paediatr. 2018;107(1):163‐164. [DOI] [PubMed] [Google Scholar]
- 23. Heena Bhandekar SM. Effectiveness of Kangaroo mother care in reducing pain during minor procedures in preterm neonates. J Clin Diagnost Res. 2018;6(1):PO15‐PO9. [Google Scholar]
- 24. Moore ER, Anderson GC, Bergman N, Dowswell T. Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2012;5:CD003519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Anderson GC, Moore E, Hepworth J, Bergman N. Early skin‐to‐skin contact for mothers and their healthy newborn infants. Cochrane Database Syst Rev. 2003;2. [DOI] [PubMed] [Google Scholar]
- 26. Tessier R, Cristo M, Velez S, et al. Kangaroo mother care and the bonding hypothesis. Pediatrics. 1998;102(2):e17. [DOI] [PubMed] [Google Scholar]
- 27. Ruiz JG, Charpak N, Castillo M, et al. Latin American Clinical Epidemiology Network Series ‐ Paper 4: economic evaluation of Kangaroo mother care: cost utility analysis of results from a randomized controlled trial conducted in Bogotá. J Clin Epidemiol. 2017;86:91‐100. [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization . Towards a grand convergence for child survival and health: a strategic review of options for the future building on lessons learnt from IMNCI. Geneva: World Health Organization; 2016. https://apps.who.int/iris/bitstream/handle/10665/251855/WHO-MCA-16.04-eng.pdf?sequence=1Accessed December 11, 2019. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


