Abstract
Background
eHealth has recently made rapid progress in care, support and treatment. However, studies on the use of eHealth to support people with a mild intellectual disability in daily life are limited. A systematic review was conducted to provide an overview of this use of eHealth.
Methods
Seven databases were searched for relevant studies and assessed according to the PRISMA guidelines. Descriptive analyses were deployed using the Matching Person to Technology model to evaluate the key areas contributing to successful eHealth use.
Results
Most of the 46 studies included were small‐scale case studies and focused on using eHealth to acquire daily living skills and vocational skills. In addition, several studies focused on eHealth use for self‐support in daily living, and three studies focused on remote professional support.
Conclusions
eHealth offers opportunities to support people with mild intellectual disability in various different contexts of daily life. Scientific research on this topic is in its early stage, and further high‐quality research is needed.
Keywords: eHealth, intellectual disability, support, systematic review, technology
1. INTRODUCTION
Around the world, increasing use is being made of health services and information delivered or enhanced over the Internet or related technologies, also referred to as eHealth (Eysenbach, 2001). This development may primarily be inspired by the potential of eHealth to improve the quality of the care provided while also upholding affordable care (Proudfoot et al., 2011). In addition, eHealth provides an opportunity for personalized, tailor‐made, remote and on‐demand support and treatment (Oh et al., 2005; Proudfoot et al., 2011; van Gemert‐Pijnen et al., 2011; Wanglin et al., 2016). Various systematic reviews and meta‐analyses in general health care have indicated that the effectiveness of eHealth is promising in a broad range of settings, such as improving physical activity, facilitating independent living, promoting smoking cessation, preventing depression and anxiety and reducing mental health and stress symptoms (e.g., Cotie et al., 2018; Deady et al., 2017; Graham et al., 2016; Sapci & Sapci, 2019; Stratton et al., 2017). Hence, eHealth has potential in promoting health, behaviour and participation.
Just as in general health care, the use of eHealth within the care for people with intellectual disability has increased markedly (Deady et al., 2017; Stratton et al., 2017). People with intellectual disability, in particular those with mild intellectual disability, have become more familiar with using the computer, the Internet and smartphones in the last decade (Chadwick, Wesson, & Fullwood, 2013; Tanis et al., 2012), resulting in more active and independent use of eHealth for various objectives compared to people with more severe levels of intellectual disability. Moreover, the use of eHealth among people with mild intellectual disability may contribute significantly to participation in the community, whereas the use of eHealth among people with more severe levels of intellectual disability is often focused on activating preferred stimuli. Due to these differences, these groups of people will use different sorts of eHealth for different purposes. Furthermore, developments such as the move from institutional to community care in the field of intellectual disability have led to a transformation in the location and manner in which support is delivered (Hall, 2011). Due to this transition, people with intellectual disability need support that is organized more flexibly, and targeted to the personal context (McConkey, Keogh, Bunting, Garcia Iriate, & Flatman Watson, 2016). As such, eHealth may respond to these changing support needs (Perry et al., 2009). Therefore, we have chosen to focus this review on the use of eHealth to support the daily life of people with mild intellectual disability, to improve their participation in the community.
Studies on the use of eHealth among people with mild intellectual disability range from a focus on treatment and therapy settings (e.g., Cooney, Jackman, Coyle, & O’Reilly, 2017; Vereenooghe et al., 2017) to studies focusing on support for daily life (e.g., Boot, Owuor, Dinsmore, & MacLachlan, 2018; Perry et al., 2009). Both support and treatment/therapy are important domains that contribute to a good life or decrease or resolve mental health problems among people with mild intellectual disability (Thompson et al., 2009; Watfern, Heck, Rule, Baldwin, & Boydell, 2019). Whereas eHealth interventions in treatment or therapy settings are primarily focused on mental health problems or challenging behaviour using an individual approach within a limited timeframe, support is often needed lifelong and is primarily focused on promoting personal functioning to enable participation. Hence, the difference between eHealth intervention focusing on support on the one hand and treatment/therapy on the other is likely to have consequences for the features of the eHealth interventions. For that reason, the data will result in two reviews, one focusing on the use of eHealth on supporting people with mild intellectual disability in daily life and another based on studies using eHealth in a treatment and therapy setting (in preparation).
In order to use eHealth effectively in supporting people with mild intellectual disability in daily functioning, it is necessary to gain insight into the needs, preferences and characteristics of people with mild intellectual disability, the environmental factors and the functions and features of the eHealth applications (Scherer et al., 2005). Yardley et al. (2016) moreover state that the effective use of eHealth is strongly influenced by a person‐based approach in which eHealth is tailored to users’ abilities, needs and level of language comprehension. Research into factors which influence effective eHealth use emphasizes the importance of involving all stakeholders and the interdependencies between human characteristics, technology and the environment (Van Gemert‐Pijnen et al., 2011). These factors are incorporated into the Matching Person to Technology (MPT) model (e.g., Scherer & Craddock, 2002; Scherer, Sax, Vanbiervliet, Cushman, & Scherer, 2005). MPT distinguishes three primary areas that need to be assessed for eHealth to be effective: (1) service users’ characteristics, (2) environmental factors and (3) functions and features of the eHealth application. The MPT model advocates for personalizing the planning, design and implication of eHealth applications, so they are based on a service user's individual needs and preferences and aligned to the environment. There should be a match—from the standpoint of the service user—between the functions and features of the technology and the needs and preferences of the service user, as well as the environment in which the eHealth application will be used by the service user. When there is a match, the service user will be more inclined to use and benefit from the eHealth application, for example to be satisfied as well as to experience improved outcomes, such as quality of life. Hence, by distinguishing these three areas, MPT is a practical as well as a research resource to identify significant aspects for effective eHealth use in people with intellectual disability.
Various reviews (e.g., Collins & Collet‐Klingenberg, 2018; Den Brok & Sterkenburg, 2015; Kagohara et al., 2013; Ramdoss et al., 2012) have already been conducted regarding the use of eHealth among people with intellectual disability, but this systematic review is the first to disassemble the key areas of client needs and preferences, environmental factors and functions and features of eHealth applications. The central aim of this study is to gain insight into how eHealth is used to support people with mild intellectual disability in their daily life. In order to do this, a clear framework of relevant factors matching an individual with a specific eHealth application is required (Scherer & Craddock, 2002). The MPT model provides such a framework of relevant factors and was therefore used as a guideline in describing the eHealth applications and related factors in the papers included in this review. Moreover, it provides the opportunity to identify potential knowledge gaps and formulate recommendations for future research regarding the needs and preferences of people with mild intellectual disability, the environmental factors and the functions and features of the eHealth applications. The increasing use of eHealth to provide health care for people with mild intellectual disability underlines the urgency of this overview.
2. METHOD
2.1. Search strategy
Seven bibliographic databases (Embase, MEDLINE (Ovid), Cochrane, Web of Science, PsycINFO (Ovid), CINAHL (EBSCO) and Google Scholar) were systematically searched on 5 September 2018, using a preset search string which was composed with the help of an experienced information specialist. Embase, MEDLINE, Web of Science and Google Scholar were chosen as they provide an optimal database combination for medically oriented systematic reviews (Bramer, Rethlefsen, Kleijnen, & Franco, 2017). In addition, PsycINFO and CINAHL were chosen as these databases focus primarily on studies in the field of behavioural sciences, mental health, nursing and allied health. Finally, Cochrane was chosen as it contains high‐quality studies with independent evidence to inform decision making in health care. Hence, the combination of these seven databases includes medically oriented as well as psychologically oriented literature and was expected to contain all relevant studies. Studies had to have been published in English in peer‐reviewed journals between January 1996 and September 2018. An updated search was conducted on 6 September 2019 to explore the most recent studies.
The PICO approach, specifying Population, Intervention, Comparison, and Outcome, was used to compose the search string and to determine the inclusion and exclusion criteria (Liberati et al., 2009). Population was specified as people with a mild intellectual disability (IQ 50–69) (Carr, Linehan, O'Reilly, Noohan Walsh, & Mc Evoy, 2016); people with more severe intellectual disability (IQ < 50) were excluded. Studies containing a mixed population of people with mild‐to‐moderate intellectual disability were included either when results were reported separately for both target populations or when no statistical differences were reported between the two target populations. Regarding the Intervention, studies should concern the use of eHealth in providing support for people with mild intellectual disability working closely together with a professional (e.g., healthcare provider). eHealth facilitating tasks of professionals (e.g., a digital scoring program for tests), communication between healthcare professionals themselves, surveillance technology and specific communication (e.g., high‐tech augmentative and alternative communication (AAC)), or assistive technology for motor problems (e.g., electronic wheelchair with eye‐tracking control) were not included in this review. Support was defined as “resources and strategies that aim to promote the development, education, interests, and the personal well‐being of a person and that enhance personal functioning” (Thompson et al., 2009, p. 135). Initially, the Comparison and Outcome components were not specified in the search strategy as eHealth is a novel and emerging area in healthcare provision for people with mild intellectual disability, and hence, all information about eHealth in the context of professional support was considered to be of interest for this study. Similarly, study designs were not specified as various designs could provide relevant information for this review. However, given the substantial number of studies identified (see Figure 1), studies were only selected in the screening phase when the results focused on adaptive skills (except academic skills trained in an educational context) or aspects related to personal and emotional well‐being. Because of the aim to provide an overview of how eHealth is used to support people with mild intellectual disability in their daily life, we focus on adaptive skills and personal and emotional well‐being (Arvidsson & Granlund, 2016; Boot et al., 2018). Conceptual skills (e.g. mathematics, science) trained in an educational context were not included in this review. Furthermore, this selection increased the homogeneity of studies.
FIGURE 1.
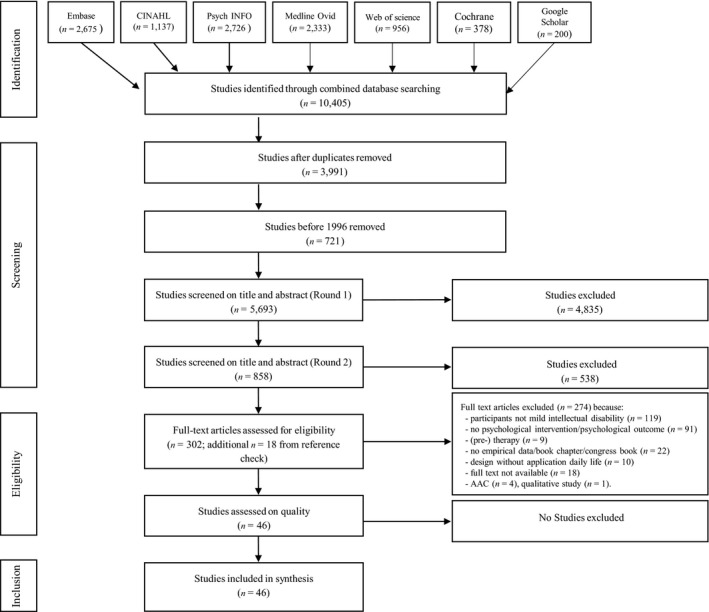
Flowchart of study selection for systematic review
Table 1 provides an overview of the search terms and strategy applied in Embase using both Emtree and additional text words for “intellectual disability,” “eHealth” and “support.” Emtree is a controlled vocabulary thesaurus that Embase uses for indexing articles. Other databases have similar thesauri (e.g. PubMed uses Medical Subject Headings (MeSH)). As can be seen in Table 1, in order to optimize the search strategy, eHealth terms were embedded in support terms for more relevant results (Bramer et al., 2017) and combined with text words referring to “intellectual disability.” It should also be noted that, in addition to the term “support,” the terms “therapy” and “assessment” were also included in the research strategy. These terms were included as we initially wanted to cover a broad range of concepts related to eHealth. However, given the large number of relevant studies remaining after the screening phase (see Figure 1), the decision was made to focus this review on eHealth in support of daily life (another review will focus on the use of eHealth in psychological interventions and therapy, in preparation). With the help of an experienced information specialist, similar search strategies were used in the other databases.
TABLE 1.
Search strategy Embase using MeSH Emtree and additional text words
| Embase final search strategy |
|---|
| ('telehealth'/de OR 'telemedicine'/de OR 'teleconsultation'/de OR 'telepsychiatry'/de OR 'telerehabilitation'/de OR 'teletherapy'/de OR 'assistive technology'/de OR 'computer assisted therapy'/de OR microcomputer/exp OR 'e‐mail'/de OR 'Internet'/de OR 'social media'/de OR 'mobile phone'/exp OR 'information technology'/de OR multimedia/de OR 'educational technology'/exp OR 'self help device'/de OR 'text messaging'/de OR (Telehealth* OR Telecare* OR telemedicine* OR teleconsultat* OR telepsychiatr* OR telemonitor* OR teletherap* OR telerehab* OR ((Tele OR telephone) NEXT/3 (health* OR medicine* OR consultat* OR psychiatr* OR therap* OR monitor* OR rehab*)) OR e‐health OR ehealth OR mHealth OR (((assist* OR therap* OR aided OR treat* OR deliver* OR application* OR support* OR training OR education* OR learning OR surveillan* OR counsel* OR cbt OR intervent* OR rehabilitat* OR assessment* OR feedback OR support OR care OR help OR service OR assistance OR self‐help) NEAR/3 (technolog* OR media OR computer* OR Web‐based OR Web‐site* OR web‐interface* OR webinterface* OR web‐page* OR web‐resource* OR webpage* OR website* OR email OR online OR Internet OR computer*‐program* OR software OR cyber* OR Remote OR virtual* OR device* OR 'text messaging' OR sms OR whatsapp OR skype)) NOT assist*‐reproduct*‐technol*) OR (((e OR electronic*) NEXT/1 (mail* OR health)) NOT electronic‐health‐record*) OR 'social media' OR ((mobile OR cell*) NEXT/1 phone*) OR smartphone* OR microcomputer OR ipad OR ipads OR (tablet* NEAR/3 (use OR usage)) OR 'information technology' OR multimedia OR domotic*):ab,ti) |
| AND ('intellectual impairment'/de OR 'mental deficiency'/exp OR 'learning disorder'/de OR 'developmental disorder'/de OR (((mental* OR intellect* OR learning OR developmental* OR neurodevelopmental*) NEAR/3 (retard* OR impair* OR deficien* OR disab* OR handicap* OR difficult* OR limitation* OR delay*)) OR multipl*‐disab* OR cognitive‐disabilit* OR learning‐disorder* OR (cognitive‐impairment* NOT (dement* OR alzheimer* OR parkinson OR psychiatr* OR older OR aged OR elderly OR injur*)) OR development*‐disorder* OR retarded OR (down* NEAR/3 (syndrome*))):ab,ti) NOT ([animals]/lim NOT [humans]/lim) NOT ([Conference Abstract]/lim OR [Letter]/lim OR [Note]/lim OR [Editorial]/lim) AND [english]/lim |
2.2. Study selection
In line with the PRISMA guidelines (Liberati et al., 2009), the selection process consisted of four phases: (1) identification, (2) screening, (3) eligibility and (4) inclusion (see Figure 1). First, in the identification phase, studies were identified in the seven different databases, returning 10,405 studies. Next, in the screening phase, 3,991 duplicates and 721 studies exceeding the publication date limit (<1,996) were removed, reducing the number of studies to 5,693. After this step, the titles and abstracts of the remaining studies were screened independently in two rounds by two reviewers (CO and NF) based on the inclusion criteria (see Table 2) in order to remove evidently unsuitable studies. Titles and abstracts were screened in two rounds. As eHealth is relatively uncharted territory in the intellectual disability field, an initial screening was conducted with a broad focus to select all studies targeting people with intellectual disability and eHealth use in the most significant healthcare domains, namely assessment, support and treatment and therapy. In the second round, we focused on studies with participants with mild intellectual disability in which eHealth was used to support daily life. The data from the studies using eHealth in a treatment and therapy setting will be discussed in another review (in preparation). Book chapters, duplicates, reviews, essays and dissertation abstracts were excluded. This strategy resulted in 90% agreement between the two reviewers. Differences in judgement were discussed with a third reviewer (PE) until full consensus was reached.
TABLE 2.
Inclusion and exclusion criteria of identified studies
|
Inclusion criteria
|
| Exclusion criteria |
|
Participants:
|
|
Intervention:
|
|
General:
|
Next, in the eligibility phase, the full texts of 302 studies were read by two reviewers (CO and NF) and two colleagues experienced in intellectual disability research. The full texts were assessed against the inclusion and exclusion criteria (see Table 2). In case of uncertainty about the criteria, the authors of the study were contacted for clarification. Differences in judgement were discussed with all reviewers, until full consensus was reached. At this stage, 274 studies were excluded for various reasons (see Figure 1), resulting in the inclusion of 28 eligible studies in this review. The reference lists of these studies were searched for potentially eligible studies and led to an additional 18 eligible studies, giving a total of 46 studies included in the review.
The next step in the eligibility phase was to assess the quality of the studies included. As this review included studies with a mixture of single‐case and group designs, a quality appraisal tool specifically designed to assess both designs was required. Therefore, in line with previous systematic reviews focusing on people with intellectual disability (e.g., McNair, Woodrow, & Hare, 2017; Patterson, Williams, & Jones, 2019), the Evaluative Method for Determining Evidence‐Based Practice (EMDEBP) (Reichow, Volkmar, & Cicchetti, 2008) was used. Although this tool uses different criteria for single‐case and group designs, both types of studies are evaluated on primary quality indicators (e.g., participant characteristics and visual analysis) and secondary quality indicators (e.g., interobserver agreement and fidelity). Primary quality indicators were rated on an ordinal scale (i.e., unacceptable, acceptable and high quality) whereas secondary quality indicators were rated on a dichotomous scale (Evidence or No Evidence of indicator). Using a codebook, the studies were scored on the quality indicators. The first author (CO) rated all studies; 11 studies (23.9%) were independently scored by a second reviewer (SN) to reduce reviewer bias (Mc Donagh, Peterson, Raina, Chang & Shekelle, 2013). The level of agreement between the two reviewers was 71%; disagreements were discussed until full consensus was reached and adaptations were made to the codebook to optimize the descriptions of items. Afterwards, the scoring was discussed with all authors. The ratings from the primary and secondary quality indicators were then combined to compute an overall research report strength: weak (i.e., high‐quality and evidence ratings on less than half the primary and secondary indicators, respectively), adequate (i.e., high‐quality ratings on most primary indicators and evidence ratings on about half the secondary indicators) or strong (i.e., high‐quality ratings on all primary indicators and evidence ratings on most secondary indicators).
Table 3 provides an in‐depth summary of the ratings on the primary and secondary quality indicators of the EMDEBP tool. Nine out of ten studies using a group design were rated as having weak research report strength; the study by Fage et al. (2018) was rated as having adequate research report strength. Regarding primary indicators, all received mainly acceptable ratings. This suggests that group design studies (a) provided sufficient demographic and clinical information about their participants, (b) chose appropriate outcome measures given their indicated goals, (c) employed control groups, (d) provided sufficient information regarding their intervention and outcome measures and (e) applied appropriate statistical tests to measure the effectiveness of interventions. With respect to secondary indicators, group design studies consistently demonstrated evidence of effect size. However, there was little to no evidence of random assignment, interobserver agreement, blind raters, fidelity, attrition, generalization and social validity. Indeed, as none of the group design studies used a randomized controlled trial (RCT) design, the expectation was that there would be no evidence of random assignment and blind raters. Without these measures, it becomes rather difficult to distinguish the true effect of an intervention from potential individual differences and biased scores on outcomes. It should be noted, however, that Fage et al. (2018) used a single‐blind condition (i.e. the researchers were unfamiliar with the medical condition of the groups of participants during the intervention).
TABLE 3.
(a) Results critical appraisal group design studies. (b) Results of critical appraisal single‐case design studies
| (a) | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Group research | Primary quality indicators | Secondary quality indicators | Quality | ||||||||||||
| Participant characterics | Independent variable | Comparison condition | Dependent variable | Link research question ‐ data analysis | Use statistical analysis | Random assignment | Interobserver agreement | Blind raters | Fidelity | Attrition | Generalization and/or maintenance | Effect size | Social validity | ||
| 1. Davies et al. (2002a) | H | A | A | A | A | A | E | NE | NE | NE | E | NE | E | NE | W |
| 2. Davies et al. (2002b) | A | H | H | H | U | A | NE | NE | NE | NE | NE | NE | E | NE | W |
| 3. Davies et al. (2003a) | A | A | H | U | H | H | NE | NE | NE | NE | NE | NE | E | NE | W |
| 4. Davies et al. (2003b) | U | A | H | H | A | H | E | NE | NE | NE | NE | NE | E | NE | W |
| 5. Padgett et al. (2006) | A | A | A | A | A | U | NE | NE | NE | NE | NE | E | NE | NE | W |
| 6. Davies et al. (2010) | A | A | A | A | A | A | NE | E | NE | NE | E | NE | E | NE | W |
| 7. Stock et al. (2013) | A | A | U | A | A | H | NE | NE | NE | NE | NE | E | E | E | W |
| 8. de Wit et al. (2015) | A | A | A | H | H | A | NE | NE | NE | NE | E | NE | NE | E | W |
| 9. Kerkhof et al. (2017) | A | A | H | U | A | U | NE | NE | NE | NE | NE | NE | NE | E | W |
| 10. Fage et al. (2018) | H | A | H | H | H | H | NE | NE | E | NE | E | NE | E | E | A |
| Total | U = 1 | U = 0 | U = 1 | U = 2 | U = 1 | U = 2 | NE = 8 | NE = 9 | NE = 9 | NE = 10 | NE = 6 | NE = 8 | NE = 3 | NE = 6 | A = 1 |
| A = 7 | A = 9 | A = 4 | A = 4 | A = 6 | A = 4 | E = 2 | E = 1 | E = 1 | E = 0 | E = 4 | E = 2 | E = 7 | E = 4 | W = 9 | |
| H = 2 | H = 1 | H = 5 | H = 4 | H = 3 | H = 4 | ||||||||||
| (b) | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Single subject research | Primary quality indicators | Secondary quality indicators | |||||||||||
| Participant characterics | Independent variable | Dependent variable | Baseline condition | Visual analysis | Experimental control | Interobserver agreement | Kappa | Fidelity | Blind raters | Generalization and/or maintenance | Social validity | Quality | |
| 11. Sigafoos et al. (2005); USA | A | H | H | H | H | H | E | NE | NE | NE | E | NE | A |
| 12. Cannella‐Malone et al. (2006); USA | A | H | H | H | H | H | E | NE | E | NE | NE | E | A |
| 13. Van Laarhoven and Van Laarhoven‐Myers (2006); USA | A | A | U | U | H | H | E | NE | E | NE | E | NE | W |
| 14. Sigafoos et al. (2007); AUS | A | H | H | H | H | H | E | NE | NE | NE | E | NE | A |
| 15. Cihak and Schrader (2008); USA | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 16. Hansen and Morgan (2008); USA | A | H | H | H | H | H | NE | NE | NE | NE | E | NE | W |
| 17. Mechling and Gustafson (2008); USA | U | H | H | H | H | H | E | NE | E | NE | E | NE | W |
| 18. Ayres et al. (2009); USA | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 19. Mechling et al. (2009); USA | A | H | H | H | H | H | E | NE | E | NE | E | NE | A |
| 20. Van Laarhoven et al. (2009); USA | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 21. Ayres and Cihak (2010); USA | H | H | H | A | U | H | E | NE | E | NE | E | NE | W |
| 22. Mechling and O'Brien (2010); USA | A | H | H | H | H | H | E | NE | E | NE | E | E | A |
| 23. Taber‐Doughty et al. (2010); USA | A | H | H | H | H | H | E | NE | E | NE | E | E | A |
| 24. Van Laarhoven et al. (2010); USA | H | H | H | A | H | H | E | NE | E | NE | E | E | A |
| 25. Mechling and Savidge (2011); USA | U | H | H | H | A | H | E | NE | E | NE | E | NE | W |
| 26. Taber‐Doughty et al. (2011); USA | H | H | H | A | U | U | E | NE | NE | NE | E | E | W |
| 27. Bereznak et al. (2012); USA | H | H | H | H | H | H | E | NE | E | NE | E | NE | S |
| 28. Van Laarhoven et al. (2012); USA | A | A | U | U | U | U | E | NE | E | NE | NE | E | W |
| 29. Alexander et al. (2013); USA | H | H | H | H | H | H | E | NE | E | NE | E | NE | S |
| 30. Bouck et al. (2014); USA | A | H | H | H | H | H | E | NE | E | NE | E | E | A |
| 31. Campillo et al. (2014); SPA | H | H | H | A | U | H | E | NE | NE | E | NE | NE | W |
| 32. Burckley et al. (2015); USA | H | H | H | H | A | A | E | NE | NE | NE | E | E | A |
| 33. McMahon et al. (2015); USA | H | H | H | H | H | H | E | NE | E | E | NE | E | S |
| 34. Smith et al. (2015); USA | H | H | H | H | H | H | E | NE | E | NE | E | NE | S |
| 35. Spriggs et al. (2015); USA | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 36. Goo et al. (2016); USA | H | H | H | H | H | H | E | NE | E | NE | E | NE | S |
| 37. Smith et al. (2016); USA | H | A | H | H | H | H | E | NE | E | NE | E | E | A |
| 38. Cavkaytar et al. (2017); TR | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 39. Cullen, Alber‐Morgan, et al. (2017); USA | A | H | H | H | H | H | E | NE | E | NE | E | E | A |
| 40. Cullen, Simmons‐Reed, et al. (2017); USA | A | H | H | H | H | H | E | NE | E | NE | E | E | A |
| 41. Douglas et al. (2018); USA | H | H | H | H | H | H | E | NE | E | NE | E | E | S |
| 42. Golish et al. (2018); USA | A | H | U | A | A | H | E | NE | NE | E | E | NE | W |
| 43. Orum Çattik and Ergenekon (2018); TR | A | H | H | H | H | H | NE | NE | NE | NE | E | E | A |
| 44. Price et al. (2018); USA | A | A | H | A | H | H | NE | NE | NE | NE | E | NE | W |
| 45. Shepley et al. (2018); USA | H | H | H | H | H | H | E | NE | E | NE | E | NE | S |
| 46. Van Laarhoven et al. (2018); USA | A | H | H | H | H | H | E | NE | E | NE | NE | E | A |
| Total | U = 2 | U = 0 | U = 3 | U = 2 | U = 4 | U = 2 | NE = 3 | NE = 36 | NE = 9 | NE = 33 | NE = 5 | NE = 16 | S = 12 |
| A = 16 | A = 4 | A = 0 | A = 6 | A = 3 | A = 1 | E = 33 | E = 0 | E = 27 | E = 3 | E = 31 | E = 19 | A = 14 | |
| H = 18 | H = 32 | H = 33 | H = 28 | H = 29 | H = 33 | W = 10 | |||||||
Abbreviations: A, adequate quality; A, adequate report strenght; E, evidence of indicator; H, high quality; NE, no evidence of indicator; S, strong report strength; U, unacceptable quality; W, weak report strenght.
Out of the thirty‐six studies using a single‐case design, 10 studies were rated as having weak research report strength, 13 had acceptable research report strength, and 13 had strong research report strength. Overall, all primary indicators (i.e., participant characteristics, independent variable, dependent variable, baseline condition, visual analysis and experimental control) received mainly acceptable‐to‐high ratings, suggesting that single‐case design studies: (a) described their participants, their interventions and outcomes sufficiently, (b) were properly controlled and (c) presented the required data visually. In terms of secondary indicators, there was no evidence of kappa or blind raters. In addition, there was evidence of fidelity in 26 studies and evidence of social validity in 19 studies. In 32 studies evidence was obtained for interobserver agreement and in 30 studies evidence was obtained for generalization.
Overall, as half of the included studies have adequate‐to‐strong research report strength, the evidence base for the use of eHealth in supporting people with mild intellectual disability in daily life functioning can be considered promising (Reichow et al., 2008).
2.3. Data extraction and analysis
A narrative analysis was used based on qualitative descriptions regarding the use of eHealth in the studies included. A coding scheme was developed based on the MPT model to extract data about the participants and their living arrangements, the environment and the eHealth application that was used in the intervention. In accordance with that scheme, we extracted the following data about the characteristics of service users: gender, age, comorbidity and previous experience with technology. The data extracted about the environmental factors focused on where and by whom the intervention was delivered and whether the researchers worked closely together with relatives or other people who were significant to the person with mild intellectual disability. Finally, we extracted data about the features and functions of the eHealth application, for example the kind of application, the goal it was used for, and opportunities for personal customization of the application.
3. RESULTS
The characteristics of the 46 studies included in the review are presented in Table 4. After a brief description of the designs, the country of origin, the number of participants in the studies and the function of eHealth, the studies will be examined with reference to the three key areas of MPT: service users’ characteristics (i.e., personal and psychosocial characteristics, needs and preferences), environmental factors and features of eHealth applications.
TABLE 4.
Characteristics of the included studies
| Author (year); country | Design | Participants | Technology/features of applications | Type of support | Support function |
|---|---|---|---|---|---|
| Group design studies | |||||
| 1. Davies et al. (2002a); USA | 2 groups BSD | N = 12; | Automated multimedia | Task completion and | SS |
| IQ = mean 62.6 (range 45–90; all except 1 < 70 WAIS‐R) | Scheduling system designed to operate on the Windows | Self‐regulation in time management | |||
| 4 F/8 M, age 19–46 | CE palmtop computer platform | ||||
| 2. Davies et al. (2002b); USA | Beta study; 2 groups WSD | N = 10; IQ = 54.8 (SD 10.37; range 39–72; WAIS‐R) | Visual Assistant prototype | Complete vocational skills independently (pizza box assembly + software package) | SS |
| 2 F/8 M, age 18–70 | |||||
| 3. Davies et al. (2003a); USA | Pilot study with a WSD | N = 9; IQ average 65.1 (range 56–72) | ATM‐SIM is a multimedia training tool | Skill teaching by simulation (money ATM) | SLS |
| 4 F/5 M, age 25–58 | |||||
| 4. Davies et al. (2003b); USA | Two‐group, WSD (beta testing) | N = 40, mean IQ = 55.53 (SD 10.69, range 24–76) | Pocket PC palmtop computer platform | Decision making in vocational tasks | SS |
| 17 F/23 M, age mean 29.38 (SD 10.97, range 18–54) | |||||
| 5. Padgett et al. (2006); USA | MPB | N = 5; FAS 4 > mild intellectual disability, 1 mild intellectual disability (mild: 55–69) 1 F/4 M, age 5–7 | VR game | Skill teaching (fire safety skills) | SLS |
| 6. Davies et al. (2010); USA | BSD two treatment conditions | N = 23; IQ = mean 54.32 (range 40–66). EG mean IQ = 52 (SD 8.39), CG mean IQ = 57.50 (SD 4.96). | Wayfinder (specially designed, cognitively accessible GPS‐based software prototype) | Facilitate independent bus travelling | SS |
| 14 F/9 M, age 18–49 | |||||
| 7. Stock et al. (2013); USA | n.r. | N = 26, average IQ = 56.1 (SD = 9.56; range 36–73) 14 F/12 M, age average 32.3 (SD 9.77; range 18–52); | Wayfinder (specialized GPS‐based system) + Pharos 600e smartphone | Facilitate independent bus travelling | SS |
| 8. de Wit et al. (2015); NL | Uncontrolled feasibility study | N = 39; 29 CPP and 10 mild intellectual disability; | Web‐based program MPC | Enabling professional support in daily functioning | FRCP |
| 4 F/6 M, age 47.6 (SD 8.4) | |||||
| 9. Kerkhof et al. (2017); NL | Participatory design and two pilots using pre‐ and post‐test design | N = 7; 1 ASD no intellectual disability, 3 moderate intellectual disability, 3 mild intellectual disability; ASD, epilepsy | Memory application on individual touch screens | Structure and support daily activities | SS |
| 10. Fage et al. (2018); FR | Co‐design and pre‐ and post‐intervention assessment | N = 48; 29 ASD and 19 intellectual disability, intellectual disability IQ = 60.53 (SD 4.50) WISC‐IV | iPad + assistive applications and socio‐cognitive remediation applications | Assisting to perform classroom routines in mainstream classrooms and providing exercises for socio‐cognitive processes | SLS + SS |
| 10 F/ 9 M, age 14.23 (SD 0.29) | |||||
| Single‐case designs | |||||
| 11. Sigafoos et al. (2005); USA | Delayed MPB across subjects | N = 3; 2 moderate intellectual disability, 1 mild intellectual disability (IQ = 50) | Portable Windows XP‐based Mercury MiniMerc™ computer + video | Skill teaching (popcorn in microwave) | SLS |
| 3 M, age 34–36 | |||||
| 12. Cannella‐Malone et al. (2006); USA | MPB across subject with ATD | N = 6; 4 moderate intellectual disability, 2 mild intellectual disability (IQ = 51 and 69), ASD | Portable Windows XP‐based Mercury MiniMerc™ computer + instructional video | Skill teaching (setting table, putting away groceries) | SLS |
| 1 F/5 M, age 27 and 36 | |||||
| 13. Van Laarhoven and Van Laarhoven‐Myers (2006); USA | Within‐subject adapted alternating treatment design |
N = 3; 1 moderate intellectual disability, 2 mild intellectual disability (IQ = 51 and 52) 1 F/2 M, age 17–19 |
Laptop computer + video | Skill teaching (laundry, washing table and microwave pizza) | SLS |
| 14. Sigafoos et al. (2007); AUS | MPB across subjects | N = 3; 2 moderate intellectual disability, 1 mild intellectual disability (IQ = 69), ASD 3 M, age 27 | Portable Windows XP‐based Mercury MiniMerc™ computer + video | Skill teaching (wash dishes) | SLS |
| 15. Cihak and Schrader (2008); USA | ATD |
N = 4; 2 severe intellectual disability, 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 50), ASD 4 M, age 16 |
Laptop computer + video | Skill teaching (preparing family packs and first aid kits, making copies and sending fax) | SLS |
| 16. Hansen and Morgan (2008); USA | MBD across participants | N = 3; 2 moderate intellectual disability, 1 mild intellectual disability (IQ = 55) | DVD and CD‐ROM instruction + computer | Skill teaching (purchase in grocery store) | SLS |
| 3 M, age 16–17 | |||||
| 17. Mechling and Gustafson (2008); USA | A‐ATD |
N = 6; 4 moderate intellectual disability, 2 mild intellectual disability (IQ = 54 and 64), ASD 6 M, age 15–21 |
Portable DVD player | Task completion | SLS |
| 18. Ayres et al. (2009); USA | MPB across behaviours and replicated across participants | N = 3; 2 n.r., 1 mild intellectual disability (IQ = 53). ASD | I Can!—Daily Living and Community Skills (Sandbox Learning Company, n.d.) software + computer | Skill teaching (setting table, making soup and a sandwich) | SLS |
| 1 F/2 M, age 7–9 | |||||
| 19. Mechling et al. (2009); USA | MPB across three cooking recipes | N = 3; 1 BF, 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 51), ASD 3 M, age 16–17 | The Cyrano Communicator™ (Hewlett Packard iPAQ Pocket PC with pre‐installed software) | Task completion by self‐monitoring (cooking recipes) | SS |
| 20. Van Laarhoven et al. (2009); USA | MPB across behaviours | N = 1; IQ = 52; 1p36 deletion syndrome | Video iPod™ | Skill teaching by self‐instruction (cleaning bathroom, mopping floor and cleaning kennels) | SLS |
| 1 M, age 17 | |||||
| 21. Ayres and Cihak (2010); USA | MPB across behaviours | N = 3; 1 TBI, 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 51) | I Can!—Daily Living and Community Skills software program + computer | Skill teaching (setting table, making soup and a sandwich) | SLS |
| 1 F/2 M, age 15 | |||||
| 22. Mechling and O’Brien (2010); USA | MPB across students and one bus route | N = 3; 1 moderate intellectual disability, 2 mild intellectual disability (IQ = 52 and 70); 1 PDD‐NOS 2 F/1 M, age 19–20 | Laptop computer + touch screen | Skill teaching (public bus transportation) | SLS |
| 23. Taber‐Doughty et al. (2010); USA | ATD | N = 4; 2 moderate intellectual disability, 2 mild intellectual disability, 1 hearing impairment | Computer contained within a secure box + single video camera. Sensors, speakers and microphones, two‐way video monitor. | Task completion at home by support of telecare staff | FRCP |
| 1 F/3 M, age 42–47 | |||||
| 24. Van Laarhoven et al. (2010); USA | A‐ATD | N = 2; 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 52) WISC 2 M, age 13–14 | Laptop computer + video +PowerPoint presentation | Skill teaching (making microwave pasta and folding laundry) | SLS |
| 25. Mechling and Savidge (2011); USA | MPB across three sets of novel structured work tasks | N = 3; 2 moderate intellectual disability, 1 mild intellectual disability (IQ = 54), ASD/ADHD 1 F/2 M, age 14 | Cyrano Communicator™ (Pidion BM−150R with pre‐installed software by One Write Company). | Task completion and transition (shoebox tasks and navigation) | SS |
| 26. Taber‐Doughty et al. (2011); USA | ATD | N = 3; 2 mild intellectual disability (IQ = 61–72) | 8‐G iPad Nanos | Skill teaching (cooking) | SLS |
| 3 F, age 12–13 | |||||
| 27. Bereznak et al. (2012); USA | MPB across behaviours replicated across participants | N = 3; 2 < IQ 40, 1 mild intellectual disability (IQ = 68), ASD | iPhone 3 G + iPhone app for instructional videos | Skill teaching by self‐monitoring (using washing machine, making noodles and using copy machine) | SLS |
| 3 M, age 15–18 | |||||
| 28. Van Laarhoven et al. (2012); USA | Modified pre‐ and post‐test control group design | N = 6; 1 no intellectual disability, 1 BF, 3 moderate intellectual disability, 1 mild intellectual disability (IQ = 65), ASD | DVD | Maintenance vocational skill (food preparation) | SLS |
| 1 F/5 M, age 16 | |||||
| 29. Alexander et al. (2013); USA | MPB across participants | N = 7; 2 mild intellectual disability (IQ = 57 and 64), ASD | iPad 2 | Skill teaching (sorting mail) | SLS |
| 1 F/6 M, age 15–18 | |||||
| 30. Bouck et al. (2014); USA | ATD | N = 3; 1 severe intellectual disability, 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 57), ASD | iPad2 + Upad lite app to create recipes | Task completion (cooking) | SLS |
| 2 F/1 M, age 13–15 | |||||
| 31. Campillo et al. (2014); SPA | AB | N = 3; 1 severe intellectual disability, 1 n.r., 1 mild intellectual disability (IQ = 58) | Samsung Q1 Ultra + Tic‐Tac software | Make time visual | SS |
| ASD | |||||
| 1 F/2 M, age 19–29 | |||||
| 32. Burckley et al. (2015); USA | MPB across setting | N = 1; mild intellectual disability IQ = 54, PDD‐NOS; | iPad 2 + Book Creator software | Skill teaching (shopping) | SLS |
| 1 F, age 18 | |||||
| 33. McMahon et al. (2015); USA | A‐ATD | N = 6; 1 moderate intellectual disability, 5 mild intellectual disability (IQ = 51–65), 1 ASD 2 F/4 M, age 18–24 | Google Maps on mobile device (iPhone/iPad) + Navigator Heads Up Display app on mobile device (= augmented reality navigation app) | Skill teaching + self‐monitoring (travelling and navigation) | SS |
| 34. Smith et al. (2015); USA | MPB across participants | N = 3; 1 n.r., 2 moderate intellectual disability, 1 mild intellectual disability, ASD | Mobile device + iSkills app | Skill teaching + self‐initiation (changing computer memory) | SLS |
| 3 M, age 15–16 | |||||
| 35. Spriggs et al. (2015); USA | MPB across participants | N = 4; 1 n.r., 3 mild intellectual disability (IQ = 50–67), ASD, PDD‐NOS, ADHD | iPad + My Pictures Talk™ application | Independent task transition | SLS |
| 1 F/3 M, age 17–19 | |||||
| 36. Goo et al. (2016); USA | MPB across students | N = 4; 2 moderate intellectual disability, 2 mild intellectual disability (IQ = 55) | HP Pavilion g series laptop | Skill teaching (purchasing) | SLS |
| 4 M, age 18 | |||||
| 37. Smith et al. (2016); USA | MPB across settings embedded in a MPB across participants | N = 4; 2 moderate intellectual disability, 1 mild intellectual disability (IQ = 62) BIF (IQ = 72, ASD, SLI | iPhone 4s + 20 application icons + videos | Skill teaching by self‐instruction (independent initiation self‐instruction daily living and vocational tasks | SLS |
| 4 M, age 15–19 | |||||
| 38. Cavkaytar et al. (2017); TR | MPB across participants | N = 3; 3 mild intellectual disability (IQ = 68) 3 F, age 19–32 | Nokia BH−503 stereo Bluetooth headset + iPad I tablet computer | Skill teaching by combining remote professional and self‐support | SLS + FRCP |
| 39. Cullen, Alber‐Morgan, et al. (2017); USA | MPB across tasks; MPB across participants |
N = 3; 1 no intellectual disability, 1 n.r., 1 mild intellectual disability (IQ = 74) 3 M, age 22 |
iPad + My Pics Talk app | Task completion by self‐direction (tasks in integrated employment settings) | SS |
| 40. Cullen, Simmons‐Reed, et al. (2017); USA | MPB across participants | N = 3; 2 no intellectual disability, 1 mild intellectual disability (IQ = 70) 3 M, age 20–24 | iPad 4 + My Pics app | Task completion by self‐direction (cleaning) | SLS |
| 41. Douglas et al. (2018); USA | MPB across participants and replicated across conditions | N = 4; 3 moderate intellectual disability, 1 mild intellectual disability (IQ = 56) WISC‐IV | iPad 2 + Photo Grocery List | Creating a shopping list (after determining low or almost empty items) | SLS |
| 4 M, age 11–14 | |||||
| 42. Golish et al. (2018); USA | Double‐baseline case study design | N = 3; 1 > mild intellectual disability and 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 64) WAIS III | iPad + visual timer | Make time visual | SS |
| 3 M, age 32–55 | |||||
| 43. Orum Çattik and Ergenekon (2018); TR | MPB across participants |
N = 3; 1 moderate intellectual disability, 2 mild intellectual disability 3 M, age 15–16 |
Bug in ear/tablet computer target skills | Skill teaching (paying electric bill, using tram) | FRCP + SLS |
| 44. Price et al. (2018); USA | MPB across participants and settings |
N = 4; 1 ASD, 1 DS, 2 mild intellectual disability 3 F/1 M, age 17–19 |
Smartphone + Google Maps app | Facilitate independent bus travelling | SS |
| 45. Shepley et al. (2018); USA | MPB across participants | N = 4; 1 moderate intellectual disability, 3 mild intellectual disability (IQ = 51–57), ASD | iPod Touch + My Pictures Talk app | Task completion by self‐instruction skills (set the table, cook receipt, make a cup of punch and snack task) | SLS |
| 2 F/2 M, age 12–14 | |||||
| 46. Van Laarhoven et al. (2018); USA | ATD | N = 4; 1 n.r., 1 no intellectual disability, 1 moderate intellectual disability, 1 mild intellectual disability (IQ = 62), seizure disorder | iPad + the Go Talk Now app by Attainment + the HP Slate PowerPoint | Skill teaching (prepare conference room) | SS |
| 2 F/2 M, age 15–18 | |||||
Design: (A) ATD, (adapted) alternating treatment design; BSD, between‐subjects design; MBD/MPBD, multiple‐baseline/multiple‐probe baseline design; SSI, semi‐structured interview; WSD, within‐subjects design. Participants: ASD, autism spectrum disorder; CPP, chronic psychiatric patients; CG/EG, control group/experimental group; FAS, foetal alcohol syndrome; BIF, borderline intellectual functioning; SLI, speech language impairment; and TBI, traumatic brain injury. SS, self‐support; SLS, support learning skill; FRCP, facilitate remote contact professional.
Regarding the design of the studies included, the vast majority of the studies applied a quantitative design (n = 44); two studies used a mixed‐method design. Ten studies applied a group design and 36 studies used a single‐case design. The majority of the single‐case design studies (n = 25) used a multiple (probe) baseline design, nine studies used an (alternative) alternating treatment design (A‐ATD), and two studies used an AB design. Six of the studies explicitly stated that the study was a feasibility study, a beta study or a pilot evaluation (Campillo et al., 2014; Davies, Stock, & Wehmeyer, 2002b, 2003b; De Wit, Dozeman, Ruwaard, Alblas, & Riper, 2015; Fage et al., 2018; Kerkhof et al., 2017).
The vast majority of the studies were conducted in the United States (n = 39). The remaining studies were conducted in the Netherlands (n = 2), Turkey (n = 2), Australia (n = 1), France (n = 1) and Spain (n = 1). Studies with six participants or fewer predominantly focused on eHealth for support in daily life (n = 38); most studies were small‐scale case studies with six participants or fewer.
The eHealth applications described in the studies can be divided into three distinct functions in the support of daily living (see Table 4). First, eHealth is primarily used as a temporary aid to facilitate training or learning a single daily living skill, a practical skill performed in the community, a vocational skill or a combination of these skills, such as purchasing groceries (e.g., Ayres, Maguire, & McClimon, 2009; Sigafoos et al., 2005). Second, eHealth is used as a permanent support aid in a home situation or vocational context for people with mild intellectual disability themselves, for example to support independent task completion (e.g., Golish, Waldman‐Levi, Swierat, & Toglia, 2018; Van Laarhoven, Johnson, Van Laarhoven‐Myers, Grider, & Grider, 2009). Third, eHealth is used as a facilitator for remote professional support to carry out daily activities, such as video calling to ask for help or remote coaching via a Bluetooth earpiece (e.g., Cavkaytar, Tomris, & Acungil, 2017; Taber‐Doughty, Shurr, Brewer, & Kubik, 2010).
3.1. Service users’ characteristics
3.1.1. Personal and psychosocial characteristics
In total, the studies included in the review reported on 346 participants (197 males) of whom 210 had a mild intellectual disability (IQ 50–70). This review therefore focuses on the outcomes related to these 210 people. Autism spectrum disorder was the most frequently reported comorbidity in 24 studies. Although most participants were adults aged between 18 and 65 (n = 162; 77%), half of the studies (n = 23) specifically focused on children (n = 48; 23%). Twelve studies reported on one or more participants with mild intellectual disability and challenging behaviour such as aggression and anxiety or using psychotropic medication (Ayres & Cihak, 2010; Ayres et al., 2009; Bereznak, Ayres, Mechling, & Alexander, 2012; Bouck, Savage, Meyer, Taber‐Doughty, & Hunley, 2014; Burckley, Tincani, & Guld Fisher, 2015; Campillo et al., 2014; Mechling, Gast, & Seid, 2009; Mechling & O’Brien, 2010; Mechling & Savidge, 2011; Spriggs, Knight, & Sherrow, 2015; Taber‐Doughty et al., 2011; Van Laarhoven & Van Laarhoven‐Myers, 2006).
3.1.2. Needs
Only one study specifically reported a systematic and methodical approach to determining the needs of participants before starting the intervention with eHealth. That is, Golish et al. (2018) used a participant‐centred interview to inventory tasks in which the participants required assistance because they found independent completion difficult. In this study, support staff delivered information on task priorities first, and then, the participant decided which task to target for the intervention. Eight studies reported objectives in an Individual Education Plan (IEP), which could be considered as a systematic inventory of needs (Alexander, Ayres, Smith, Shepley, & Mataras, 2013; Ayres & Cihak, 2010; Bereznak et al., 2012; Bouck et al., 2014; Cavkaytar et al., 2017; Goo, Hua, & Therrien, 2016; Mechling et al., 2009; Smith et al., 2016).
3.1.3. Preferences
Three studies reported service users’ preferences before and after the intervention, by asking participants about their preference for using an iPad or a pen or pencil (Bouck et al., 2014), about preferred strategies for successful task performance (Taber‐Doughty et al., 2011) and about participants’ preferences regarding onsite and remote support staff (Taber‐Doughty et al., 2010). Motivation and preference related to the target skill were determined in four studies. In two studies this was done in order to add relevant reinforcers to the device (Burckley et al., 2015; Mechling & Savidge, 2011). In one study, the participant preferred to start with a given task because he perceived it as easy to complete (Golish et al., 2018), and in another study, the content of the applications was personalized (e.g., by adding personal photos and videos) to the preferences of the participants (Fage et al., 2018). Four studies reported the preferences of participants who were asked a simple preference question with respect to the instructional method on a device or the tool in the intervention (Cihak & Schrader, 2008; McMahon, Smith, Cihak, Wright, & Gibbons, 2015; Mechling et al., 2009; Mechling & Savidge, 2011).
3.1.4. Expectations and perceptions of eHealth
Cullen, Alber‐Morgan, Simmons‐Reed, and Izzo (2017) reported participants being asked about their perception and desired adjustments for the successful use of an iPad and an app in a vocational context in the near future. In addition, one study reported a participatory design using a memory application in real life, in which participants’ expectations and perceptions of this application were used as input to optimize the application (Kerkhof et al., 2017). The other 44 studies did not report expectations and perceptions of eHealth.
3.1.5. Previous experience with eHealth and digital skills
In various studies, the presence of digital skills is mentioned as an essential element of access to and actual use of eHealth (Hoppestad, 2013; Raspa et al., 2018; Tanis et al., 2012). For this reason, the previous digital experience of participants was extracted from the studies included in this review.
None of the studies reported a systematic assessment of the digital skills of participants before starting the intervention. However, 14 studies reported participants’ previous experience with a digital device (Ayres & Cihak, 2010; Bereznak et al., 2012; Burckley et al., 2015; Cannella‐Malone et al., 2006; De Wit et al., 2015; Douglas, Uphold, Steffen, & Kroesch, 2018; Mechling et al., 2009; Mechling & O’Brien, 2010; Shepley, Spriggs, Samudre, & Elliot, 2018; Smith et al., 2016; Smith, Shepley, Alexander, Davis, & Ayres, 2015; Spriggs et al., 2015; Van Laarhoven, Blood, Chan, & Winiarski, 2012; Van Laarhoven, Kraus, Karpman, Nizzi, & Valentino, 2010). These experiences varied from playing online games to executing simple acts on a computer such as typing letters. Four studies stated that the participants did not have any digital experience prior to the intervention (Campillo et al., 2014; Cullen, Alber‐Morgan, et al., 2017; Goo et al., 2016; Taber‐Doughty et al., 2011). The majority of the studies included (n = 28) were silent on participants’ digital experience.
3.2. Environmental factors
3.2.1. Context of service users’ daily lives
Although the vast majority of the studies (n = 43) reported the context of the eHealth intervention, hardly any information was reported about the personal circumstances of the participants (e.g., living conditions, working conditions and social network). Nine studies provided information about the personal context of participants: six of these studies described the personal context because the eHealth intervention was (partially) applied at their homes (De Wit et al., 2015; Fage et al., 2018; Golish et al., 2018; Kerkhof et al., 2017; Taber‐Doughty et al., 2010; Van Laarhoven & Van Laarhoven‐Myers, 2006). In the three remaining studies, with the intervention being applied in the educational context, it was stated that the participants lived in a community‐group home, with family or friends, without further details (Cannella‐Malone et al., 2006; Cullen, Simmons‐Reed, & Weaver, 2017; Sigafoos et al., 2005, 2007).
3.2.2. Context of eHealth interventions
The six studies which reported interventions taking place in the participant's home mostly focused on daily living skills such as cooking and everyday household tasks (De Wit et al., 2015; Golish et al., 2018; Kerkhof et al., 2017; Taber‐Doughty et al., 2010; Van Laarhoven et al., 2012; Van Laarhoven & Van Laarhoven‐Myers, 2006). In addition, four interventions took place only in the community (Burckley et al., 2015; Davies, Stock, Holloway, & Wehmeyer, 2010; Orum Çattik & Ergenekon, 2018; Stock, Davies, Hoelzel, & Mullen, 2013) and were, for example, focused on travelling on public transport and making purchases in a local grocery shop. Furthermore, in six studies, the interventions were applied in a vocational setting, targeting aspects such as independent task completion (Cannella‐Malone et al., 2006; Cavkaytar et al., 2017; Cullen, Alber‐Morgan, et al., 2017; Sigafoos et al., 2005, 2007; Van Laarhoven et al., 2009). In two studies, a vocational setting was organized in the office of a software company (Davies, Stock, & Wehmeyer, 2002a, 2003b). Notably, most eHealth interventions were performed in an educational context (n = 25), of which five interventions even combined an educational and a societal context (Goo et al., 2016; Hansen & Morgan, 2008; McMahon et al., 2015; Mechling & O'Brien, 2010; Price, Marsh, & Fisher, 2018) and one intervention combined an educational context with the home context (Fage et al., 2018). In one additional study, the intervention was applied in a day care centre (Campillo et al., 2014), targeted at making time visual in waiting situations. Four studies did not report a clear intervention context.
Interestingly, various studies mentioned examples where contextual barriers hindered optimal eHealth use, such as problems with the technological functioning of eHealth because of the low quality of the Internet connection (e.g., De Wit et al., 2015) and professionals’ concerns about their lack of digital skills limiting their opportunities to support persons with intellectual disability (e.g., Taber‐Doughty et al., 2011).
3.2.3. Training in how to use the eHealth application
The majority of the studies included (n = 30) reported device training before starting an intervention with an eHealth application. Eighteen of these studies used evidence‐based instructional practices to teach participants to use the eHealth application, such as a system of least prompting, most‐to‐least and least‐to‐most prompting, constant and progressive time delay prompting, and model‐lead test format (Ayres & Cihak, 2010; Ayres et al., 2009; Bereznak et al., 2012; Cavkaytar et al., 2017; Cullen, Alber‐Morgan, et al., 2017; Cullen, Simmons‐Reed, et al., 2017; McMahon et al., 2015; Mechling & O’Brien, 2010; Mechling & Savidge, 2011; Price et al., 2018; Shepley et al., 2018; Smith et al., 2015, 2016; Spriggs et al., 2015; Stock et al., 2013; Van Laarhoven, Carreon, Bonneau, & Lagerhausen, 2018; Van Laarhoven et al., 2009, 2010). In three of these studies, those providing the intervention worked closely with participants, using modelling and guiding them until independent use was achieved (Campillo et al., 2014; Fage et al., 2018; Padgett, Strickland, & Coles, 2006). In addition, two of these studies used workshops with support staff to help participants become familiar with using the application (De Wit et al., 2015; Kerkhof et al., 2017). Furthermore, seven of these studies reported device training without giving additional details. The remaining 16 studies did not provide or report any device training.
3.2.4. Professionals providing the eHealth intervention
In three studies, support staff performed the intervention without the involvement of the researchers (Campillo et al., 2014; De Wit et al., 2015; Taber‐Doughty et al., 2010). In five other studies, the intervention was performed by a teacher without any involvement from the researchers (Cihak & Schrader, 2008; Douglas et al., 2018; Shepley et al., 2018; Spriggs et al., 2015; Van Laarhoven et al., 2012). Researchers collaborated closely with the teachers in three studies (Ayres & Cihak, 2010; Smith et al., 2015, 2016) and with support staff in only one study (Kerkhof et al., 2017). Parents were also involved in one study, guiding their children at home using training apps (Fage et al., 2018). Notably, in half of the studies, the eHealth intervention was performed by the researchers themselves (n = 21).
In the remaining 12 studies, it was not clear who was performing the intervention, because of the use of general terms such as “instructor” (Mechling et al., 2009; Mechling & Gustafson, 2008; Mechling & O’Brien, 2010; Mechling & Savidge, 2011), “trainer” (Cannella‐Malone et al., 2006; Sigafoos et al., 2005, 2007), “experimenter” (Cullen, Alber‐Morgan, et al., 2017; Cullen, Simmons‐Reed, et al., 2017), “project staff” (Davies, Stock, & Wehmeyer, 2002b), “others” (Golish et al., 2018) or “staff, experimenter and a person who had experience working with adults with ID” (Davies et al., 2003b).
3.3. Features of the eHealth applications
In the studies included in this review, support was provided through a range of eHealth applications (see Table 4). In 13 studies, a portable application such as a smartphone or a personal digital device was deployed for support. In addition, an iPad/iPod tablet was used in 16 studies, frequently combined with an app, specific software, videos, a Bluetooth earpiece and an e‐book (Alexander et al., 2013; Burckley et al., 2015; Cavkaytar et al., 2017; Cullen, Alber‐Morgan, et al., 2017; Cullen, Simmons‐Reed, et al., 2017; Douglas et al., 2018; Fage et al., 2018; Golish et al., 2018; McMahon et al., 2015; Orum Çattik & Ergenekon, 2018; Shepley et al., 2018; Smith et al., 2015; Spriggs et al., 2015; Taber‐Doughty et al., 2011; Van Laarhoven et al., 2009, 2018). A computer or laptop was used in 11 studies, in combination with specific software, showing step‐by‐step pictures or videos of target skills. Virtual Reality (Padgett et al., 2006) and Augmented Reality (McMahon et al., 2015) were each applied in one study.
The applications used in the studies had different features: (a) monitoring the progress of task performance, time, sequence of activities during the day and presence of professional staff (n = 7) (Bouck et al., 2014; Campillo et al., 2014; Douglas et al., 2018; Golish et al., 2018; Kerkhof et al., 2017; Spriggs et al., 2015; Van Laarhoven et al., 2018); (b) prompting task or skill execution using pictures, videos and audio (n = 27) (Alexander et al., 2013; Ayres & Cihak, 2010; Ayres et al., 2009; Bereznak et al., 2012; Burckley et al., 2015; Cannella‐Malone et al., 2006; Cihak & Schrader, 2008; Cullen, Alber‐Morgan, et al., 2017; Cullen, Simmons‐Reed, et al., 2017; Davies et al., 2002a, 2002b, 2003; Goo et al., 2016; Hansen & Morgan, 2008; Mechling et al., 2009; Mechling & Gustafson, 2008; Mechling & O’Brien, 2010; Mechling & Savidge, 2011; Sigafoos et al., 2005, 2007; Smith et al., 2015, 2016; Taber‐Doughty et al., 2011; Van Laarhoven et al., 2009, 2010, 2012; Van Laarhoven & Van Laarhoven‐Myers, 2006); (c) providing real‐time information and feedback in the users' context (e.g., prompting during a trip on a public bus) (n = 7) (Davies et al., 2010; Fage et al., 2018; McMahon et al., 2015; Orum Çattik & Ergenekon, 2018; Price et al., 2018; Shepley et al., 2018; Stock et al., 2013); (d) providing a realistic and safe learning situation (e.g., virtual reality) (n = 2) (Davies, Stock, & Wehmeyer, 2003a; Padgett et al., 2006); and (e) facilitating remote contact and communication with professional care staff (n = 3) (Cavkaytar et al., 2017; De Wit et al., 2015; Taber‐Doughty et al., 2010).
4. DISCUSSION
In line with general health care, the use of eHealth within the intellectual disability field has increased in recent years. Due to the transition from institutional to community care (Hall, 2011), there is a need for flexible support targeting the personal context of the person with intellectual disability (McConkey et al., 2016). As such, eHealth may contribute to this changing support need (Perry, Beyer, & Holm, 2009). In this respect, the MPT model provides a valuable framework within which to consider the factors for effective eHealth for supporting people with mild intellectual disability. The MPT model emphasizes the importance of considering three key areas: (1) the characteristics of the person with mild intellectual disability (e.g., personal and psychosocial characteristics, needs and preferences of people with mild intellectual disability), (2) environmental factors and (3) functions and features of eHealth. Our study resulted in three main findings related to using eHealth to support people with mild intellectual disability in performing daily activities, discussed below.
The first main finding is that the majority of the studies do not inventory the personal needs and preferences of people with mild intellectual disability as a starting point to find the most appropriate eHealth application in a personal situation to meet the subject's personal goals. Therefore, there seems to be little space for the voices of people with mild intellectual disability themselves or to explore how the opportunities of eHealth match their preferences. Studies reporting on how technology can help a person to fulfil personal needs underline the importance of a personalized, tailor‐made approach in this matching process (Boot et al., 2018; Collins & Collet‐Klingenberg, 2018; Frielink, Oudshoorn, & Embregts, 2019; Manzoor & Vimarlund, 2018; Scherer & Federici, 2015). With respect to personalized and tailor‐made support, the absence of a needs assessment is not unique to the intellectual disability field. In the care of elderly people, too, only a few studies have explored aspects such as their needs and preferences for using the Internet and eHealth technologies in managing their health (e.g., Ware et al., 2017). The absence of a user‐centred focus in developing and implementing eHealth technologies is postulated to contribute to usability problems and high attrition rates (Van Gemert‐Pijnen et al., 2011).
The second main finding is that important persons in the informal and formal networks of people with mild intellectual disability (e.g., relatives, support staff, teachers) are rarely involved in the phase of selecting an appropriate eHealth application or in the phase of implementing the application, whether in daily practice or otherwise. In most eHealth interventions included in this review, the researcher delivered the intervention within an educational context. Although it is fairly common for researchers to introduce and train eHealth interventions, family members and support staff are important stakeholders who support people with intellectual disability in using eHealth in daily life and they should be involved in the introduction and training phase (Tanis et al., 2012). In some studies included in this review, the researchers contacted support staff/teachers or family members, yet there was limited collaboration overall (e.g., teachers and parents were interviewed about the future possibilities of eHealth but did not take an active role during the intervention). Successful implementation and actual use of eHealth are commonly achieved in close collaboration with key stakeholders (Chadwick et al., 2013; Palmer, Wehmeyer, Davies, & Stock, 2012; Van Gemert‐Pijnen et al., 2018) and require fine‐tuning to the opportunities and challenges encountered in a daily living context (Beyer & Perry, 2013; Clifford Simplican, Shivers, Chen, & Leader, 2018; Parsons et al., 2008). As such, collaboration with staff and family members is essential, as people with mild intellectual disability have difficulty generalizing their learned skills to a new context, and their support needs are lifelong (Thompson et al., 2009). This means that they need repeated performance of tasks to maintain skills (De Wit, Moonen, & Douma, 2012). Future researchers are therefore encouraged to collaborate closely with support staff/teachers and family members of people with intellectual disability in designing, introducing and using eHealth.
The third main finding is that various eHealth applications can be successfully implemented following structured training using behavioural therapeutic principles for people with mild intellectual disability. Most eHealth tools offer opportunities to customize the tool to personal preferences. In this respect, it is important to take the aspects of Universal Design into account in designing eHealth tools (Hoppestad, 2013; Wehmeyer, Smith, Palmer, & Davies, 2004). Universal Design emphasizes flexibility, a tailored approach, simplicity and intuitive use as well as perceptible information (Damianidou, Foggett, Arthur‐Kelly, Lyons, & Wehmeyer, 2018; Wehmeyer et al., 2004; Wehmeyer, Tassé, Davies, & Stock, 2012). Developing eHealth applications while taking these aspects into account increases the likelihood of actual use in the daily life of people with mild intellectual disability, enabling them to benefit from eHealth in the same way as people in the general population (Raspa et al., 2018; Watfern et al., 2019; Wehmeyer et al., 2004). Although studies reported on the potential of eHealth, optimizing the actual use of eHealth requires that attendance must be paid to the collaboration with service users and their personal network (informal and professional) from the very beginning of eHealth use.
The studies included in this review used a range of eHealth applications with different functions and features. The major function of eHealth in the studies included was as a temporary tool to support the learning process for practical daily living skills or vocational skills. This is in line with earlier systematic reviews, illustrating that technology could be useful in facilitating a learning process (e.g. Collins & Collet‐Klingenberg, 2018; Damianidou et al., 2018; Kagohara et al., 2013; Ramdoss et al., 2012). In addition, although less frequently, eHealth was also used in other functions, for instance as a self‐supportive tool and for the provision of remote professional contact. It would be beneficial for future eHealth applications to focus on these functions, too, especially because of their potential to empower people with mild intellectual disability and fine‐tune their personal needs in their own environment (Den Brok & Sterkenburg, 2015; Wennberg & Kjellberg, 2010; Zaagsma, Volkers, Schippers, Wilschut, & van Hove, 2019). These eHealth applications could contribute to important issues in the lives of people with mild intellectual disability, such as making their own choices in various domains in life, enhanced independent functioning and being an active member of society (Carey, Friedman, & Nelson Bryen, 2005; Haight et al., 2013; Wehmeyer et al., 2012).
This literature review reveals various opportunities for future research. First, although the studies included showed promising results from using eHealth for different goals in various life domains, there were methodological weaknesses in these studies (i.e., most studies have a small sample size, lack of follow‐up measurements, and weak study designs such as pilot, feasibility and beta studies). These weaknesses limit the generalization of the findings. Future research should build out with well‐executed studies. In addition to more large‐scale studies, such as randomized controlled trials, single‐case studies can also contribute to the development and effective implementation of eHealth for people with mild intellectual disability to support them in daily living activities. A case study design performs well in providing insights into what will work for this person in this context, making it valuable for a better understanding of complex social contexts such as health care (Yin, 2014). An important requirement in this respect is to design good‐quality case studies. Guidelines such as the What Works Clearinghouse single‐case design technical documentation (Kratochwill et al., 2010) could help in this respect. Next, using models for the effective use of technology, such as the Matching Person to Technology model, could improve the process of matching the need of an individual with intellectual disability to the best‐fitting tool in the personal context (Scherer et al., 2005). Although many studies emphasize the importance of this matching process for successful eHealth use and underline the involvement of all stakeholders, including those with mild intellectual disability, it is remarkable that this process seems to be underestimated and hardly reported (Lussier‐Desrochers et al., 2017; Parsons, Daniels, Porter, & Robertson, 2008; Wennberg & Kjellberg, 2010). Third, and in addition to the focus on eHealth use for support in daily life, the domain of psychological interventions and therapy is also imperative. Therefore, a systematic inventory of available scientific knowledge of psychological interventions and therapy using eHealth among people with intellectual disability is a necessary step in further research (Oudshoorn, Frielink, Nijs & Embregts, in preparation).
Some limitations of this systematic review need to be addressed as well. First, only studies in the English language were selected for inclusion in this review, so any studies published in other languages have been missed; potentially valuable knowledge published in other languages could help provide a more complete overview of studies about this topic. Second, different outcome measures limited the opportunities for a structured analysis of the outcomes, as is the case with a meta‐analysis. It would have been interesting to investigate the link between using a well‐defined plan and well‐executed implementation of an eHealth tool (e.g., according to the three elements of MPT) and the effect on outcomes. Third, one of the main challenges of this review was to determine what is included in the concept “eHealth,” as it is often used as an umbrella term for different aspects of delivering and facilitating health care (Oh et al., 2005; Skär & Söderberg, 2017). A clear definition could decrease the risk of misinterpretation of what is intended by providing eHealth and stimulate the exchange of relevant knowledge about eHealth to support people with mild intellectual disability. It is therefore important for future research to focus on a more concrete definition and conceptualization of what eHealth is.
To conclude, eHealth can contribute to the expansion of opportunities to support people with mild intellectual disability in various domains of their daily lives and their participation in the community. Studies about using eHealth to support people with mild intellectual disability show promising results; however, there is a need for a clear focus on the implementation of the eHealth tool before evaluating its effectiveness. With this focus, reliable insights can be obtained into the added value of eHealth for supporting the daily life of people with mild intellectual disability.
CONFLICT OF INTEREST
The authors declare no conflicts of interest.
ETHICAL APPROVAL
This review does not involve any human participants.
ACKNOWLEDGMENTS
The authors would like to thank Wichor Bramer, Information Specialist at Erasmus Medical Center Rotterdam, for his assistance with the literature search and the fellow researchers Judith Austin, Wietske van Oorsouw and Elsbeth Taminiau from Tranzo, Tilburg School of Social and Behavioral Sciences, Tilburg University, for their help in the screening phase.
Oudshoorn CEM, Frielink N, Nijs SLP, Embregts PJCM. eHealth in the support of people with mild intellectual disability in daily life: A systematic review. J Appl Res Intellect Disabil. 2020;33:1166–1187. 10.1111/jar.12758
The research was funded by ASVZ. ASVZ has not imposed any restrictions on free access to or publication of the research data. All authors declare that they have no conflict of interest. This manuscript has not been previously published and is not under consideration in the same or substantially similar form in any other (peer‐reviewed) media. All authors listed have contributed sufficiently to the project to be included as authors, and all those who are qualified to be authors are listed in the author byline. We have included acknowledgements, conflicts of interest and funding sources on the title page.
Funding information
This research was funded by service provider ASVZ. The authors would like to thank the Prinsen Geerligs Foundation for their contribution to making this systematic review possible.
REFERENCES
*Included publications in systematic review
- *Alexander, J. L. , Ayres, K. M. , Smith, K. A. , Shepley, S. B. , & Mataras, T. K. (2013). Using video modeling on an iPad to teach generalized matching on a sorting mail task to adolescents with autism. Research in Autism Spectrum Disorders, 7, 1346–1357. 10.1016/j.rasd.2013.07.021 [DOI] [Google Scholar]
- Arvidsson, P. , & Granlund, M. (2016). The relationship between intelligence quotient and the aspects of everyday functioning and participation for people who have mild and borderline intellectual functioning. Journal of Applied Research in Intellectual Disabilities, 31, 66–78. [DOI] [PubMed] [Google Scholar]
- *Ayres, K. , & Cihak, D. (2010). Computer‐ and video‐based instruction of food‐preparation skills: Acquisition, generalization, and maintenance. Intellectual and Developmental Disabilities, 48, 195–208. [DOI] [PubMed] [Google Scholar]
- *Ayres, K. , Maguire, A. , & McClimon, D. (2009). Acquisition and generalization of chained tasks taught with computer based video instruction to children with autism. Education and Training in Developmental Disabilities, 44, 493–508. [Google Scholar]
- *Bereznak, S. , Ayres, K. M. , Mechling, L. C. , & Alexander, J. L. (2012). Video self‐prompting and mobile technology to increase daily living and vocational independence for students with autism spectrum disorders. Journal of Developmental and Physical Disabilities, 24, 269–285. 10.1007/s10882-012-9270-8 [DOI] [Google Scholar]
- Beyer, S. , & Perry, J. (2013). Promoting independence through the use of assistive technology. Tizard Learning Disability Review, 18, 179–185. 10.1108/TLDR-03-2013-0028 [DOI] [Google Scholar]
- Boot, F. H. , Owuor, J. , Dinsmore, J. , & MacLachlan, M. (2018). Access to assistive technology for people with intellectual disabilities: A systematic review to identify barriers and facilitators. Journal of Intellectual Disability Research, 62, 900–921. 10.1111/jir.12532 [DOI] [PubMed] [Google Scholar]
- *Bouck, E. C. , Savage, M. , Meyer, N. K. , Taber‐Doughty, T. , & Hunley, M. (2014). High‐tech or low‐tech? Comparing self‐monitoring systems to increase task independence for students with autism. Focus on Autism and Other Developmental Disabilities, 29, 156–167. [Google Scholar]
- Bramer, W. M. , Rethlefsen, M. L. , Kleijnen, J. , & Franco, O. H. (2017). Optimal database combinations for literature searches in systematic reviews: A prospective exploratory study. Systematic Reviews, 6(245), 1–12. 10.1186/s13643-017-0644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Burckley, E. , Tincani, M. , & Guld Fisher, A. (2015). An iPad‐based picture and video activity schedule increases community shopping skills of a young adult with autism spectrum disorder and intellectual disability. Developmental Neurorehabilitation, 18, 131–136. 10.3109/17518423.2014.945045 [DOI] [PubMed] [Google Scholar]
- *Campillo, C. , Herrera, G. , Remírez de Ganuza, C. , Cuesta, J. L. , Abellán, R. , Campos, A. , … Amati, F. (2014). Using Tic‐Tac software to reduce anxiety‐related behaviour in adults with autism and learning difficulties during waiting periods: A pilot study. Autism, 18, 264–271. 10.1177/1362361312472067 [DOI] [PubMed] [Google Scholar]
- *Cannella‐Malone, H. , O'Reilly, M. , de la Cruz, B. , Edrisinha, C. , Sigafoos, J. , & Lancioni, G. E. (2006). Comparing video prompting to video modeling for teaching daily living skills to six adults with developmental disabilities. Education and Training in Developmental Disabilities, 41, 344–356. [Google Scholar]
- Carey, A. C. , Friedman, M. G. , & Nelson Bryen, D. (2005). Use of electronic technologies by people with intellectual disabilities. Mental Retardation, 43, 322–333. [DOI] [PubMed] [Google Scholar]
- Carr, A. , Linehan, C. , O'Reilly, G. , Noohan Walsh, P. , & Mc Evoy, J. (2016). The handbook of intellectual disability and clinical psychology practice (2nd ed.). London and New York: Routledge. [Google Scholar]
- *Cavkaytar, A. , Tomris, G. , & Acungil, A. T. (2017). Effectiveness of teaching café waitering to adults with intellectual disability through audio‐visual technologies. Education and Training in Developmental Disabilities, 52, 77–90. [Google Scholar]
- Chadwick, P. , Wesson, C. , & Fullwood, C. (2013). Internet access by people with intellectual disabilities: Inequalities and opportunities. Future Internet, 5, 376–397. 10.3390/fi5030376 [DOI] [Google Scholar]
- *Cihak, D. F. , & Schrader, L. (2008). Does the model matter? Comparing video self‐modeling and video adult modeling for task acquisition and maintenance by adolescents with autism spectrum disorder. Journal of Special Education Technology, 23, 9–20. [Google Scholar]
- Clifford Simplican, S. , Shivers, C. , Chen, J. , & Leader, G. (2018). “With a Touch of a Button”: Staff perceptions on integrating technology in an Irish service provider for people with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 31, e130–e139. [DOI] [PubMed] [Google Scholar]
- Collins, J. C. , & Collet‐Klingenberg, L. (2018). Portable electronic assistive technology to improve vocational task completion in young adults with an intellectual disability: A review of literature. Journal of Intellectual Disabilities, 22, 1–20. [DOI] [PubMed] [Google Scholar]
- Cooney, P. , Jackman, C. , Coyle, D. , & O’Reilly, G. (2017). Computerised cognitive‐behavioural therapy for adults with intellectual disability: Randomised controlled trial. The British Journal of Psychiatry, 211, 95–102. 10.1192/bjp.bp.117.198630 [DOI] [PubMed] [Google Scholar]
- Cotie, L. M. , Prince, S. A. , Elliott, C. G. , Ziss, M. C. , McDonnell, L. A. , Mullen, K. A. , … Reed, J. L. (2018). The effectiveness of eHealth interventions on physical activity and measures of obesity among working‐age women: A systematic review and meta‐analysis. Obesity Reviews, 9, 1340–1358. 10.1111/obr.12700 [DOI] [PubMed] [Google Scholar]
- *Cullen, J. M. , Alber‐Morgan, S. R. , Simmons‐Reed, E. A. , & Izzo, M. V. (2017). Effects of self‐directed video prompting using iPads on the vocational task completion of young adults with intellectual and developmental disabilities. Journal of Vocational Rehabilitation, 46, 361–375. [Google Scholar]
- *Cullen, J. M. , Simmons‐Reed, E. A. , & Weaver, L. (2017). Using 21st century video prompting technology to facilitate the independence of individuals with intellectual and developmental disabilities. Psychology in the Schools, 54, 965–978. 10.1002/pits.22056 [DOI] [Google Scholar]
- Damianidou, D. , Foggett, J. , Arthur‐Kelly, M. , Lyons, G. , & Wehmeyer, M. L. (2018). Effectiveness of technology types in employment‐related outcomes for people with intellectual and developmental disabilities: An extension meta‐analysis. Advances in Neurodevelopmental Disorders, 2, 262–272. 10.1007/s41252-018-0070-8 [DOI] [Google Scholar]
- *Davies, D. K. , Stock, S. E. , Holloway, S. , & Wehmeyer, M. L. (2010). Evaluating a GPS‐based transportation device to support independent bus travel by people with intellectual disability. Intellectual and Developmental Disabilities, 48, 454–463. 10.1352/1934-9556-48.6.454 [DOI] [PubMed] [Google Scholar]
- *Davies, D. K. , Stock, S. E. , & Wehmeyer, M. L. (2002a). Enhancing independent time‐management skills of individuals with mental retardation using a palmtop personal computer. Mental Retardation, 40, 358–365. [DOI] [PubMed] [Google Scholar]
- *Davies, D. K. , Stock, S. E. , & Wehmeyer, M. L. (2002b). Enhancing independent task performance for individuals with mental retardation through use of a handheld self‐directed visual and audio prompting system. Education and Training in Mental Retardation and Developmental Disabilities, 37, 209–218. [Google Scholar]
- *Davies, D. K. , Stock, S. E. , & Wehmeyer, M. L. (2003a). A palmtop computer‐based intelligent aid for individuals with intellectual disabilities to increase independent decision making. Research & Practice for Persons with Severe Disabilities, 28, 182–193. 10.2511/rpsd.28.4.182 [DOI] [Google Scholar]
- *Davies, D. K. , Stock, S. E. , & Wehmeyer, M. L. (2003b). Application of computer simulation to teach ATM access to individuals with intellectual disabilities. Education and Training in Developmental Disabilities, 38, 451–456. [Google Scholar]
- *De Wit, J. , Dozeman, E. , Ruwaard, J. , Alblas, J. , & Riper, H. (2015). Web‐based support for daily functioning of people with mild intellectual disabilities or chronic psychiatric disorders: A feasibility study in routine practice. Internet Interventions, 2, 161–168. 10.1016/j.invent.2015.02.007 [DOI] [Google Scholar]
- De Wit, M. , Moonen, X. , & Douma, J. (2012). Guideline effective interventions for youngsters with MID. Recommendations for the Development and Adaptation of Behavioural Change Interventions for Youngsters with Mild Intellectual Disabilities. Retrieved from https://www.kenniscentrumlvb.nl/wpcontent/uploads/woocommerce_uploads/2018/10/guideline_effective_interventions_mid_lr_formaat_2012‐06‐27.pdf [Google Scholar]
- Deady, M. , Choi, I. , Calvo, R. A. , Glozier, N. , Christensen, H. , & Harvey, S. B. (2017). eHealth interventions for the prevention of depression and anxiety in the general population: A systematic review and meta‐analysis. BMC Psychiatry, 17, 1–14. 10.1186/s12888-017-1473-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Den Brok, W. L. J. E. , & Sterkenburg, P. S. (2015). Self‐controlled technologies to support skill attainment in persons with an autism spectrum disorder and/or an intellectual disability: A systematic literature review. Disability and Rehabilitation: Assistive Technology, 10, 1–10. [DOI] [PubMed] [Google Scholar]
- *Douglas, K. H. , Uphold, N. M. , Steffen, S. , & Kroesch, A. M. (2018). Promoting literacy with self‐created grocery list on mobile devices. The Journal of Special Education, 51, 201–210. [Google Scholar]
- Eysenbach, G. (2001). What is e‐health? Journal of Medical Internet Research, 3(2). 10.2196/jmir.3.2.e20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Fage, C. , Consel, C. Y. , Balland, E. , Etchegoyhen, K. , Amestoy, A. , Bouvard, M. , & Sauzéon, H. (2018). Tablet apps to support first school inclusion to children with autism spectrum disorders (ASD) in mainstream classrooms: A pilot study. Frontiers in Psychology, 9, 1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frielink, N. , Oudshoorn, C. , & Embregts, P. (2020). eHealth in support for daily functioning of people with intellectual disability: Views of service users, relatives, and professionals on both its advantages and disadvantages and its facilitating and impeding factors. Journal of Intellectual and Developmental Disability. 10.3109/13668250.2020.1744878 [DOI] [Google Scholar]
- *Golish, K. , Waldman‐Levi, A. , Swierat, R. P. , & Toglia, J. (2018). Adults with intellectual disabilities: Case studies using everyday technology to support daily living skills. British Journal of Occupational Therapy, 81, 514–524. [Google Scholar]
- *Goo, M. , Hua, Y. , & Therrien, W. J. (2016). Effects of computer‐based video instruction on the acquisition and generalization of grocery purchasing skills for students with intellectual disability. Education and Training in Developmental Disabilities, 51, 150–161. [Google Scholar]
- Graham, A. L. , Carpenter, K. M. , Cha, S. , Cole, S. , Jacobs, M. A. , Raskob, M. , & Cole‐Lewis, H. (2016). Systematic review and meta‐analysis of Internet interventions for smoking cessation among adults. Substance Abuse and Rehabilitation, 7, 55–69. 10.2147/SAR.S101660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haight, A. , Lee, D. , Shaw, C. , Hawthorne, M. , Chamberlain, S. , Newman, D. W. , … Beail, N. (2013). What things make people with learning disability happy and satisfied with their lives: An inclusive research project. Journal of Applied Research in Intellectual Disabilities, 26, 26–33. [DOI] [PubMed] [Google Scholar]
- Hall, E. (2011). Shopping for support: Personalisation and the new spaces and relations of commodified care for people with learning disabilities. Social & Cultural Geography, 12, 589–603. 10.1080/14649365.2011.601236 [DOI] [Google Scholar]
- *Hansen, D. L. , & Morgan, R. L. (2008). Teaching grocery store purchasing skills to students with intellectual disabilities using a computer‐based instruction program. Education and Training in Developmental Disabilities, 43, 431–442. [Google Scholar]
- Hoppestad, B. S. (2013). Current perspective regarding adults with intellectual and developmental disabilities accessing computer technology. Disability and Rehabilitation: Assistive Technology, 8, 190–194. [DOI] [PubMed] [Google Scholar]
- Kagohara, D. M. , van der Meer, L. , Ramdoss, S. , O'Reilly, M. F. , Lancioni, G. E. , Davis, T. N. , … Sigafoos, J. (2013). Using iPods and iPads in teaching programs for individuals with developmental disabilities: A systematic review. Research in Developmental Disabilities, 34, 147–156. 10.1016/j.ridd.2012.07.027 [DOI] [PubMed] [Google Scholar]
- *Kerkhof, Y. J. F. , den Ouden, M. E. M. , Soeteman, S. , Scholten, A. , Ben Allouch, S. , & Willems, C. G. (2017). Development of a memory application for structuring and supporting daily activities of clients with intellectual disabilities. Technology and Disability, 29, 77–89. 10.3233/TAD-160164 [DOI] [Google Scholar]
- Kratochwill, T. R. , Hitchcock, J. , Horner, R. H. , Levin, J. R. , Odom, S. L. , Rindskopf, D. M. , & Shadish, W. R. (2010). Single‐case designs technical documentation. Retrieved from What Works Clearinghouse Website http://ies.ed.gov/ncee/wwc/pdf/wwc_scd.pdf [Google Scholar]
- Liberati, A. , Altman, D. G. , Tetzlaff, J. , Mulrow, C. , Gøtzsche, P. C. , Ioannidis, J. P. A. , … Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta‐analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med, 6, 1–28. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lussier‐Desrochers, D. , Normand, C. L. , Romero‐Torres, A. , Lachapelle, Y. , Godin‐Tremblay, V. , Dupont, M.‐È. , … Bilodeau, P. (2017). Bridging the digital divide for people with intellectual disability. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 11(1). 10.5817/CP2017-1-1 [DOI] [Google Scholar]
- Manzoor, M. , & Vimarlund, V. (2018). Digital technologies for social inclusion of individuals with disabilities. Health and Technology, 8, 377–390. 10.1007/s12553-018-0239-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McConkey, R. , Keogh, F. , Bunting, B. , Garcia Iriate, E. , & Flatman Watson, S. (2016). Relocating people with intellectual disability to new accommodation and support settings: Contrasts between personalized arrangements and group home placements. Journal of Intellectual Disabilities, 20, 109–120. 10.1177/1744629515624639 [DOI] [PubMed] [Google Scholar]
- Mc Donagh, M , Peterson, K. , Raina, P. , Chang, S. , & Shekelle, P. (2013). Avoiding bias in selecting studies. In: Methods Guide for Effectiveness and Comparative Effectiveness Review [Internet], (2008). Rockville (MD): Agency for Healthcare Research and Quality (US) https://www.ncbi.nlm.nih.gov/books/NBK47095 [PubMed] [Google Scholar]
- *McMahon, D. D. , Smith, C. C. , Cihak, D. F. , Wright, R. , & Gibbons, M. M. (2015). Effects of digital navigation aids on adults with intellectual disabilities: Comparison of paper map, Google Maps, and Augmented Reality. Journal of Special Education Technology, 30, 157–165. 10.1177/0162643415618927 [DOI] [Google Scholar]
- McNair, L. , Woodrow, C. , & Hare, D. (2017). Dialectical behaviour therapy [DBT] with people with intellectual disabilities: A systematic review and narrative analysis. Journal of Applied Research in Intellectual Disabilities, 30, 787–804. 10.1111/jar.12277 [DOI] [PubMed] [Google Scholar]
- *Mechling, L. C. , Gast, D. L. , & Seid, N. H. (2009). Using a personal digital assistant to increase independent task completion by students with autism spectrum disorder. Journal of Autism and Developmental Disorders, 39, 1420–1434. 10.1007/s10803-009-0761-0 [DOI] [PubMed] [Google Scholar]
- *Mechling, L. C. , & Gustafson, M. R. (2008). Comparison of static picture and video prompting on the performance of cooking‐related tasks by students with autism. Journal of Special Education Technology, 23, 31–45. 10.1177/016264340802300304 [DOI] [Google Scholar]
- *Mechling, L. C. , & O'Brien, E. (2010). Computer‐based video instruction to teach students with intellectual disabilities to use public bus transportation. Education and Training in Developmental Disabilities, 45, 230–241. [Google Scholar]
- *Mechling, L. C. , & Savidge, S. (2011). Using a personal digital assistant to increase completion of novel tasks and independent transitioning by students with autism spectrum disorder. Journal of Autism and Developmental Disorders, 41, 687–704. 10.1007/s10803-010-1088-6 [DOI] [PubMed] [Google Scholar]
- Oh, H. , Rizo, C. , Enkin, M. , Jadad, A. , Powell, J. , & Pagliari, C. (2005). What is eHealth (3): A systematic review of published definitions. Journal of Medical Internet Research, 7, 1–12. 10.2196/jmir.7.1.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Orum Çattik, E. O. , & Ergenekon, Y. (2018). Effectiveness of video modeling combined with auditory technology support in teaching skills for using community resources to individuals with intellectual disabilities. Education and Science, 43, 237–257. 10.15390/EB.2018.7182 [DOI] [Google Scholar]
- *Padgett, L. S. , Strickland, D. , & Coles, C. D. (2006). Case study: Using a virtual reality computer game to teach fire safety skills to children diagnosed with fetal alcohol syndrome. Journal of Pediatric Psychology, 31, 65–70. 10.1093/jpepsy/jsj030 [DOI] [PubMed] [Google Scholar]
- Palmer, S. B. , Wehmeyer, M. L. , Davies, D. K. , & Stock, S. E. (2012). Family members’ reports of the technology use of family members with intellectual and developmental disabilities. Journal of Intellectual Disabilities Research, 56, 402–414. 10.1111/j.1365-2788.2011.01489.x [DOI] [PubMed] [Google Scholar]
- Parsons, S. , Daniels, H. , Porter, J. , & Robertson, C. (2008). Resources staff beliefs and organizational culture: Factors in the use of information and communication technology for adults with intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 21, 19–33. [Google Scholar]
- Patterson, C. W. , Williams, J. , & Jones, R. (2019). Third‐wave therapies and adults with intellectual disabilities: A systematic review. Journal of Applied Research in Intellectual Disabilities, 32(6), 1295–1309. 10.1111/jar.12619 [DOI] [PubMed] [Google Scholar]
- Perry, J. , Beyer, S. , & Holm, S. (2009). Assistive technology, telecare and people with intellectual disabilities: Ethical considerations. Journal Medical Ethics, 35, 81–86. 10.1136/jme.2008.024588 [DOI] [PubMed] [Google Scholar]
- *Price, R. , Marsh, A. J. , & Fisher, M. H. (2018). Teaching young adults with intellectual and developmental disabilities community‐based navigation skills to take public transportation. Behavioral Analysis Practice, 11, 46–50. 10.1007/s40617-017-0202-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Proudfoot, J. , Klein, B. , Barak, A. , Carlbring, P. , Cuijpers, P. , Lange, A. , … Andersson, G. (2011). Establishing guidelines for executing and reporting internet intervention research. Cognitive Behavior Therapy, 40(2), 82–97. 10.1080/16506073.2011.573807 [DOI] [PubMed] [Google Scholar]
- Ramdoss, S. , Lang, R. , Fragale, C. , Britt, C. , O’Reilly, M. , Sigafoos, J. , … Lancioni, G. E. (2012). Use of computer‐based interventions to promote daily living skills in individuals with intellectual disabilities: A systematic review. Journal of Developmental and Physical Disabilities, 24, 197–215. 10.1007/s10882-011-9259-8 [DOI] [Google Scholar]
- Raspa, M. , Fitzgerald, T. , Furberg, R. D. , Wylie, A. , Moultrie, R. , DeRamus, M. , … McCormack, L. (2018). Mobile technology use and skills among individuals with fragile X syndrome: Implications for health care decision making. Journal of Intellectual Disability Research, 62, 821–832. 10.1111/jir.12537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reichow, B. , Volkmar, F. R. , & Cicchetti, D. V. (2008). Development of the evaluative method for evaluating and determining evidence‐based practices in autism. Journal of Autism and Developmental Disorders, 38, 1311–1319. 10.1007/s10803-007-0517-7 [DOI] [PubMed] [Google Scholar]
- Sapci, A. H. , & Sapci, H. A. (2019). Innovative assisted living tools, remote monitoring technologies, artificial intelligence‐driven solutions, and robotic systems for aging societies: Systematic review. Journal of Medical Internet Research Aging, 2(2), e15429 10.2196/15429 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scherer, M. J. , & Craddock, G. (2002). Matching Person & Technology (MPT) assessment process. Technology and Disability, 14, 125–131. [Google Scholar]
- Scherer, M. J. , & Federici, S. (2015). Why people use and don't use technologies: Introduction to the special issue on assistive technologies for cognition/cognitive support technologies. NeuroRehabilitation, 37, 315–319. 10.3233/NRE-151264 [DOI] [PubMed] [Google Scholar]
- Scherer, M. J. , Sax, C. , Vanbiervliet, A. , Cushman, L. A. , & Scherer, J. V. (2005). Predictors of assistive technology use: The importance of personal and psychosocial factors. Disability and Rehabilitation, 27, 1321–1331. 10.1080/09638280500164800 [DOI] [PubMed] [Google Scholar]
- *Shepley, S. B. , Spriggs, A. D. , Samudre, M. , & Elliot, M. (2018). Increasing daily living independence using video activity schedules in middle school students with intellectual disability. Journal of Special Education Technology, 33, 71–82. 10.1177/0162643417732294 [DOI] [Google Scholar]
- *Sigafoos, J. , O'Reilly, M. , Cannella, H. , Edrisinha, C. , de la Cruz, B. , Upadhyaya, M. , … Young, D. (2007). Evaluation of a video prompting and fading procedure for teaching dish washing skills to adults with developmental disabilities. Journal of Behavioral Education, 16, 93–109. 10.1007/s10864-006-9004-z [DOI] [Google Scholar]
- *Sigafoos, J. , O'Reilly, M. , Cannella, H. , Upadhyaya, M. , Edrisinha, C. , Lancioni, G. E. , … Young, D. (2005). Computer‐presented video prompting for teaching microwave oven use to three adults with developmental disabilities. Journal of Behavioral Education, 14, 189–201. 10.1007/s10864-005-6297-2 [DOI] [Google Scholar]
- Skär, L. , & Söderberg, S. (2017). The importance of ethical aspect when implementing eHealth services in healthcare: A discussion paper. Journal of Advanced Nursing, 74, 1043–1050. [DOI] [PubMed] [Google Scholar]
- *Smith, K. A. , Ayres, K. A. , Alexander, J. , Ledford, J. R. , Shepley, C. , & Shepley, S. B. (2016). Initiation and generalization of self‐instructional skills in adolescents with autism and intellectual disability. Journal of Autism and Developmental Disorders, 46, 1196–1209. 10.1007/s10803-015-2654-8 [DOI] [PubMed] [Google Scholar]
- *Smith, K. A. , Shepley, S. B. , Alexander, J. L. , Davis, A. , & Ayres, K. M. (2015). Self‐instruction using mobile technology to learn functional skills. Research in Autism Spectrum Disorders, 11, 93–100. 10.1016/j.rasd.2014.12.001 [DOI] [Google Scholar]
- *Spriggs, A. D. , Knight, V. , & Sherrow, L. (2015). Talking picture‐schedules: Embedding video models into visual activity schedules to increase independence for students with ASD. Journal of Autism and Developmental Disorders, 45, 3846–3861. 10.1007/s10803-014-2315-3 [DOI] [PubMed] [Google Scholar]
- *Stock, S. E. , Davies, D. K. , Hoelzel, L. A. , & Mullen, R. J. (2013). Evaluation of a GPS‐based system for supporting independent use of public transportation by adults with intellectual disability. Inclusion, 1, 133–144. 10.1352/2326-6988-01.02.133 [DOI] [Google Scholar]
- Stratton, E. , Lampit, A. , Choi, L. , Calvo, R. A. , Harvey, S. B. , & Glozier, N. G. (2017). Effectiveness of eHealth interventions for reducing mental health conditions in employees. A systematic review and meta‐analysis. PLoS One, 12, 1–23. 10.1371/journal.pone.0189904 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Taber‐Doughty, T. , Bouck, E. C. , Tom, K. , Jasper, A. D. , Flanagan, S. M. , & Bassette, L. (2011). Video modeling and prompting: A comparison of two strategies for teaching cooking skills to students with mild intellectual disabilities. Education and Training in Developmental Disabilities, 46, 499–513. [Google Scholar]
- *Taber‐Doughty, T. , Shurr, J. , Brewer, J. , & Kubik, S. (2010). Standard care and telecare services: Comparing the effectiveness of two service systems with consumers with intellectual disabilities. Journal of Intellectual Disability Research, 54, 843–859. 10.1111/j.1365-2788.2010.01314.x [DOI] [PubMed] [Google Scholar]
- Tanis, E. S. , Palmer, S. B. , Wehmeyer, M. L. , Davies, D. , Stock, S. , Lobb, K. , & Bishop, B. (2012). A self‐report computer‐based survey of technology use by people with intellectual and developmental disabilities. Intellectual and Developmental Disabilities, 50, 53–68. 10.1352/1934-9556-50.1.53 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson, J. R. , Bradley, V. J. , Buntinx, W. H. E. , Schalock, R. L. , Shogren, K. A. , Snell, M. E. , … Yeager, M. H. (2009). Conceptualizing supports and the support needs of people with intellectual disability. Intellectual and Developmental Disabilities, 47, 135–146. 10.1352/1934-9556-47.2.135 [DOI] [PubMed] [Google Scholar]
- Van Gemert‐Pijnen, J. E. W. C. , Nijland, N. , Van Limburg, M. , Eng, B. , Ossebaard, H. C. , Kelders, S. M. , … Seydel, E. R. (2011). A holistic framework to improve the uptake and impact of eHealth technologies. Journal of Medical Internet Research, 13, 1–18. 10.2196/jmir.1672 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Gemert‐Pijnen, L. , Kelders, S. M. , Kip, H. , & Sanderman, R. (Eds.) (2018). eHealth research, theory and development. A Multidisciplinary Approach. Abingdon/New York: Routledge. [Google Scholar]
- *Van Laarhoven, T. , Blood, E. , Chan, J. M. , & Winiarski, L. (2012). Maintaining vocational skills of individuals with autism and developmental disabilities through video modeling. Education and Training in Developmental Disabilities, 47, 447–461. [Google Scholar]
- *Van Laarhoven, T. , Carreon, A. , Bonneau, W. , & Lagerhausen, A. (2018). Comparing mobile technologies for teaching vocational skills to individuals with autism spectrum disorders and/or intellectual disabilities using universally‐designed prompting systems. Journal of Autism and Developmental Disorders, 48, 2516–2529. 10.1007/s10803-018-3512-2 [DOI] [PubMed] [Google Scholar]
- *Van Laarhoven, T. , Johnson, J. W. , Van Laarhoven‐Myers, T. , Grider, K. L. , & Grider, K. M. (2009). The effectiveness of using a video iPod as a prompting device in employment settings. Journal Behavioral Education, 18, 119–141. 10.1007/s10864-009-9077-6 [DOI] [Google Scholar]
- *Van Laarhoven, T. , Kraus, E. , Karpman, K. , Nizzi, R. , & Valentino, J. (2010). A comparison of picture and video prompts to teach daily living skills to individuals with autism. Focus on Autism and Other Developmental Disabilities, 25, 195–208. 10.1177/1088357610380412 [DOI] [Google Scholar]
- *Van Laarhoven, T. , & Van Laarhoven‐Myers, T. (2006). Comparison of three video‐based instructional procedures for teaching daily living skills to persons with developmental disabilities. Education and Training in Developmental Disabilities, 41, 365–381. [Google Scholar]
- Vereenooghe, L. , Gega, L. , & Langdon, P. E. (2017). Intellectual disability and computers in therapy: Views of service users and clinical psychologists. Cyberpsychology: Journal of Psychosocial Research on Cyberspace, 11(1). 10.5817/CP.2017-1-11 [DOI] [Google Scholar]
- Wanglin, B. C. , Szafranski, D. D. , & Gros, D. F. (2016). Telehealth technologies in evidence‐based psychotherapy In Luiselli J. K., & Fischer A. J. (Eds.), Computer‐assisted and web‐based innovations in psychology, special education, and health (pp. 119–140). Oxford, UK: Academic Press. [Google Scholar]
- Ware, P. , Bartlett, S. J. , Paré, G. , Symeonidis, I. , Tannenbaum, C. , Bartlett, G. , … Ahmed, S. (2017). Using eHealth technologies: Interests, preferences, and concerns of older adults. Interactive Journal of Medical Research, 6(1), e3 10.2196/ijmr.4447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watfern, C. , Heck, C. , Rule, C. , Baldwin, P. , & Boydell, K. M. (2019). Feasibility and acceptability of a mental health website for adults with an intellectual disability: Qualitative evaluation. JMIR Mental Health, 6, e12958 10.2196/12958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wehmeyer, M. L. , Smith, S. J. , Palmer, S. B. , & Davies, D. K. (2004). Technology use by students with intellectual disabilities: An overview. Journal of Special Education Technology, 19, 7–20. 10.1177/016264340401900402 [DOI] [Google Scholar]
- Wehmeyer, M. L. , Tassé, M. J. , Davies, S. K. , & Stock, S. (2012). Support needs of adults with intellectual disability across domains: The role of technology. Journal of Special Education Technology, 27, 11–22. 10.1177/016264341202700203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- *Wennberg, B. , & Kjellberg, A. (2010). Participation when using cognitive assistive devices from the perspective of people with intellectual disabilities. Occupational Therapy International, 17, 168–176. 10.1002/oti.296 [DOI] [PubMed] [Google Scholar]
- Yardley, L. , Spring, B. J. , Riper, H. , Morrison, L. G. , Crane, D. H. , Curtis, K. , … Blandford, A. (2016). Understanding and promoting effective engagement with digital behavior change interventions. American Journal of Preventive Medicine, 51, 833–842. 10.1016/j.amepre.2016.06.015 [DOI] [PubMed] [Google Scholar]
- Yin, R. K. (2014). Case study research. Design and methods. Washington, DC: Sage. [Google Scholar]
- Zaagsma, M. , Volkers, K. M. , Schippers, A. P. , Wilschut, J. A. , & van Hove, G. (2019). An exploratory study of the support needs in 24/7 online support for people with mild intellectual disabilities. Journal of Policy and Practice in Intellectual Disabilities, 16, 78–87. 10.1111/jppi.12275 [DOI] [Google Scholar]


