Highlights
-
•
Statewide vaping prevalence was significantly associated with COVID-19 cases on a state level.
-
•
Statewide vaping prevalence was significantly associated with COVID-19 death on a state level.
-
•
This study emphasizes the importance of studying the susceptibility of current vapers to COVID-19 cases and death.
Abstract
Existing literature indicated electronic cigarette users (vapers) have impaired immune response that might increase vulnerability to coronavirus disease 2019 (COVID-19) infection and death. However, whether vapers are more susceptible to COVID-19 is unknown.
Using integrated data in each US state from the 2018 Behavioral Risk Factor Surveillance System (BRFSS), United States Census Bureau and the 1Point3Acres.com website, generalized estimating equation (GEE) models with negative binomial distribution assumption and log link functions were used to examine the association of statewide e-cigarette use prevalence with number of COVID-19 cases and deaths in the US on a state level from January 21, 2020 to April 25, 2020.
The weighted proportion of vapers who used e-cigarettes every day or some days ranged from 2.86% to 6.42% for US states. Statistically significant associations were observed between the weighted proportion of vapers and number of COVID-19 cases as well as COVID-19 deaths in the US after adjusting for the weighted proportion of smokers and other significant covariates in the GEE models. With every one percent increase in weighted proportion of vapers in each state, the number of COVID-19 cases increase by 0.3139 (95% CI: 0.0554–0.5723) and the number of COVID-19 deaths increase by 0.3730 (95% CI: 0.0815–0.6646) in log scale in each US state.
The positive associations between the proportion of vapers and the number of COVID-19 cases and deaths in each US state in this ecological study suggest an increased susceptibility of vapers to COVID-19 on a state level and warrants further investigation.
1. Introduction
Novel coronavirus disease 2019 (COVID-19) outbreak was declared a global pandemic by the World Health Organization (WHO) on March 11, 2020 (Cucinotta and Vanelli, 2020). As of April 28, 2020, there were over three million COVID-19 cases and over 200,000 deaths globally (Dong et al., 2020). In the United States, the total number of COVID-19 cases exceeded one million, with over 57,000 deaths reported by April 28, 2020. COVID-19 presents with cough, dyspnea and fever among other systemic symptoms and can lead to pneumonia and acute hypoxemic respiratory failure (Ahn et al., 2020).
Electronic cigarettes (e-cigarettes), promoted as an alternative for cigarette smoking, rapidly gained popularity in recent years in the US. In 2018, the prevalence of current e-cigarette use (vaping) in US adults was 3.2% (Dai and Leventhal, 2019). Recent studies on the associations of vaping and health symptoms/diseases have observed associations between vaping and symptoms of wheezing and self-reported Chronic Obstructive Pulmonary Disease (COPD), along with increased inflammation in bronchial epithelial cells and alterations in the pulmonary immune response to infection (Gaurav, 2019, Gilpin et al., 2019, Muthumalage et al., 2019, Wu et al., 2014, Li et al., 2020, Xie et al., 2019). Tobacco control researchers have raised concerns that vapers may be more susceptible to COVID-19 and could develop more severe COVID-19 symptoms (Majmundar et al., 2020). However, there is very limited evidence on the association between vaping and COVID-19.
We examined the association of vaping with COVID-19 cases and deaths, using the integrated state-level weighted proportions of current e-cigarette users (vapers) from the 2018 Behavioral Risk Factor Surveillance System (BRFSS) survey data, the population size and land area in 2018 in each state from United States Census Bureau, and the daily number of COVID-19 cases and deaths in each state from the 1Point3Acres.com website during the time period from January 21, 2020 to April 25, 2020 in the United States (https://coronavirus.1point3acres.com). Our study is the first one to observe the association of vaping with COVID-19 at the US population level.
2. Methods
2.1. Study population
We integrated the 2018 Behavioral Risk Factor Surveillance System (BRFSS) survey data at state level (https://www.cdc.gov/brfss/annual_data/annual_2018.html), the population size and land area in each state from the United States Census Bureau (https://www.census.gov/newsroom/press-kits/2018/pop-estimates-national-state.html), and the COVID-19 infected cases and deaths data from the 1Point3Acres.com website (https://coronavirus.1point3acres.com) at available dates from each state through the unique two letter state abbreviations for this ecological study. From the 2018 BRFSS survey, 34 states provided information on the vaping status variable. The population size in each state in 2018 and land area in each state were obtained from the United States Census Bureau website. The COVID-19 infected cases and deaths counts were available for each state from January 21, 2020 to April 25, 2020. Reports of negative numbers of infected cases and deaths were excluded from the COVID-19 data. After integrating the BRFSS data and the census data with the COVID-19 cases and deaths from different dates at the state level, there were 1607 observations in the final analysis data.
2.2. Vaping status
The vaping status variable was defined by the answers to the question “Do you now use e-cigarettes, every day, some days, or not at all?” in the 2018 BRFSS survey. Subjects who now use e-cigarettes every day or some days were classified as vapers and subjects who responded that they use e-cigarettes “not at all” or “not applicable” were classified as non-vapers. The weighted frequency of vapers in each state was obtained using the proc surveyfreq procedure in SAS version 9.4 (SAS Institute Inc., Cary, NC), considering the complex sampling design of the BRFSS survey. The weighted proportion of vapers in each US state was calculated using the ratio of weighted frequency of vapers and weighted frequency of total number of subjects in each state.
2.3. Outcomes and covariates
The outcomes used in current analysis were the number of COVID-19 cases and deaths in US states. Covariates considered in the current investigation included population size, population density (calculated using population size divided by land area) from the United States Census Bureau, age, gender, race/ethnicity, education, income, mental health, physical health, obesity, respiratory disease (including asthma and COPD), heart disease, cancer, stroke, diabetes, kidney disease, and smoking (currently smoke every day or some days) from the 2018 BRFSS survey data. The number of COVID-19 cases was also used as a covariate when modeling the COVID-19 deaths. All the covariates were state-level variables. The covariates included in the GEE model for COVID-19 cases were state population size in log scale, male, less than high school education, poor physical health, cancer, obese, and smoker. The covariates in the GEE model for COVID-19 deaths included the number of daily confirmed cases in each state, state population size in log scale, proportion of people aged 35–44, proportion of White, Black, and Hispanic, proportion of people having respiratory disease, cancer, being obese, and being smokers.
2.4. Statistical analysis
Generalized estimating equation (GEE) models with negative binomial distribution assumptions and log link functions were used to examine the association of weighted proportion of vapers with the number of COVID-19 cases and deaths, after adjusting for the confounding effects from significant covariates (Johnson and Kim, 2004, Vagenas and Totsika, 2018). The correlations of number of COVID-19 cases and deaths from different dates within the same state were considered through the autoregressive 1 (AR (1)) variance–covariance structure within the GEE model framework. The purposeful covariates selection method was used to select significant covariates for the GEE models (Bursac et al., 2008). Variance inflation factor (VIF) was used to examine the multicollinearities among the predictor variables in the GEE models (Lambrinos, 1984). A VIF value of five or less was considered to indicate no multicollinearity in the fitted GEE model. All statistical analyses were conducted using statistical analysis software SAS version 9.4 (SAS Institute Inc., Cary, NC) and R (R Core Team, 2017). Significance levels for all tests were set at 5% for two-sided tests.
3. Results
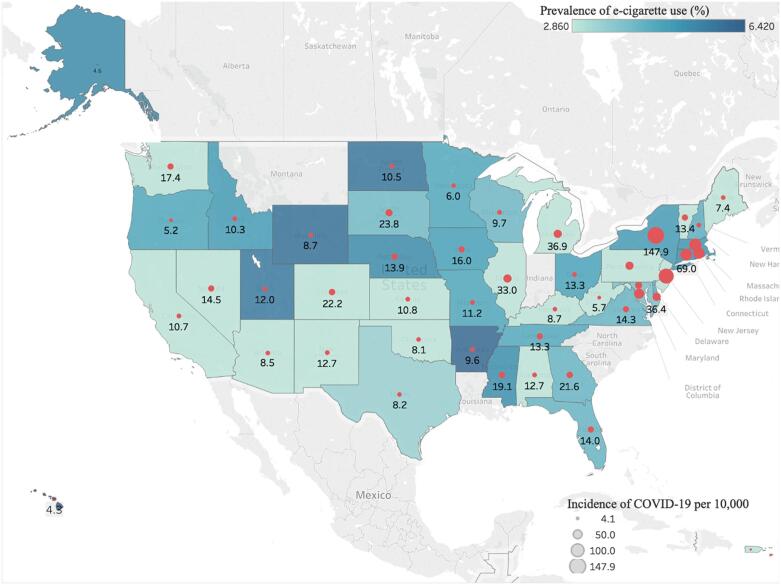
The weighted proportion of vapers ranged from 2.86% to 6.42% for US states. The daily number of infected COVID-19 cases ranged from 0 to 11,743 with an average of 362 daily cases and a median of 69 daily cases across all states in the US during the time period from January 21, 2020 to April 25, 2020. Fig. 1 showed the US map for vaping prevalence and incidence of COVID-19 per 10,000. The map indicated a positive association between vaping prevalence and incidence of COVID-19 per 10,000 on a state level. During the same time period, the daily number of deaths ranged from 0 to 4556 with the mean number of daily deaths at 20 and the median number of daily deaths at 1 across all US states.
Fig. 1.
US map for vaping prevalence and incidence of COVID-19 per 10,000.
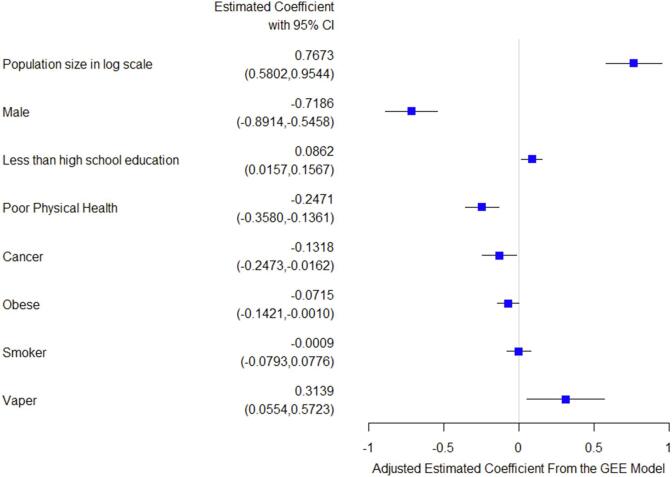
Fig. 2 showed the estimated coefficients and their 95% confidence intervals from the GEE model on daily number of COVID-19 cases. States that had a higher proportion of vapers also had a larger number of daily COVID-19 cases. For every one percent increase in vaping prevalence, the prevalence of COVID-19 cases increased by 0.3139 fold (95% CI: 0.0554–0.5723) on average in log scale. Both population size in log scale in each state and proportion of less than high school education had a positive association with the daily COVID-19 cases. Male gender, poor physical health, cancer, and obesity had a negative association with the daily COVID-19 cases. Proportion of current smokers in each state was not significantly associated with the daily COVID-19 cases in each state.
Fig. 2.
Adjusted estimated coefficients from the GEE model on number of COVID-19 cases.
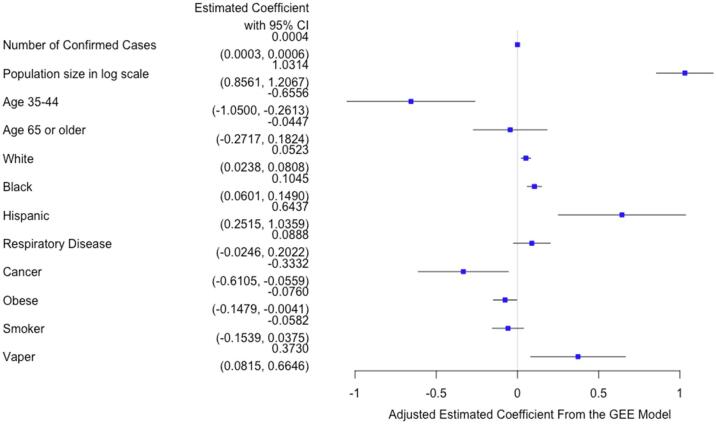
The estimated coefficients and their 95% confidence intervals from the GEE model on daily number of COVID-19 deaths were shown in Fig. 3. States that had a higher proportion of vapers also had a higher number of daily COVID-19 deaths. With a one percent increase in vaping prevalence, the prevalence of COVID-19 deaths increased by 0.3730 fold (95% CI: 0.0815–0.6646) on average in log scale. Daily confirmed cases, state population size in log scale, proportion of White, Black, and Hispanic were positively associated with the daily number of COVID-19 deaths in each state. The proportion of people aged 35–44, having cancer, and being obese all were negatively associated with daily number of COVID-19 deaths in each state. The proportion of people aged 65 years or older, proportion of people having respiratory disease, and proportion of current smokers in each state were not significantly associated with the daily number of COVID-19 deaths in each state.
Fig. 3.
Adjusted estimated coefficients from the GEE model on number of COVID-19 deaths.
4. Discussion
Using integrated state level data obtained from the 2018 BRFSS survey, the United States Census Bureau and the 1Point3Acres.com website, we were able to investigate the association of weighted proportion of vapers with COVID-19 cases and deaths in the United States. We found a significant positive association of vaping prevalence with COVID-19 cases and deaths at the state level controlling for sociodemographic and health related covariates. This finding further supports the need for future research into the potential susceptibility of vapers to COVID-19. Additional findings include the expected positive association between population size and COVID-19 cases and death. Finally we also observed a positive association between a low education level and COVID-19 cases and a negative association between male sex and COVID-19 cases, as well as negative associations of obesity with COVID-19 cases and death.
Though we identified a positive association between the weighted proportion of vapers and the number of COVID-19 cases and deaths at state level, we did not have data on what proportion of those who actually contracted COVID-19 or died from COVID-19 were vapers. Thus, we cannot determine causality between vaping and COVID-19 cases and deaths. However, prior research supports the biological plausibility of a relationship between vaping and an increased susceptibility to respiratory infection (Eaton et al., 2018). Multiple mouse models have observed an increased severity in respiratory infection associated with vaping exposure related to dysregulation of lung epithelial cells and an impaired immune response to both viral (Madison et al., 2019); and bacterial infection (Hwang et al., 2016). Bacterial superinfection of viral illnesses like influenza and COVID-19 is especially dangerous, as this leads to an increased severity in illness (Rynda-Apple et al., 2015) A human cell based model of exposure to nicotine-free flavored e-liquid observed immunosuppressive effects and impaired respiratory innate immune cell function (alveolar macrophages, neutrophils, and natural killer cells) (Clapp et al., 2017). In humans, bronchoalveolar lavage samples from the airways of active vapers also revealed dysregulation of the airway’s innate immune response including neutrophilic response and mucin (Reidel et al., 2018). A wide variety of flavorings are used by vapers, many of which, such as diacetyl, acetoin, pentanedione, o-vanillin, maltol, and coumarin in nicotine-free e-liquid, could also trigger inflammatory responses in human monocytes (Muthumalage et al., 2019). Previous human studies found vaping is associated with increased risk of chronic bronchitis symptoms (chronic cough or phlegm) (Gotts et al., 2019, Wang et al., 2016, McConnell et al., 2017) and epidemiologic studies observed an increased risk of self-reported wheezing and COPD (Li et al., 2020, Xie et al., 2019). In addition, social behaviors associated with vaping could also enhance the risk of infection. For example, vapers who were not wearing a mask inside confined areas or even outside in a non-distanced group would be at an increased risk for contracting COVID-19. With the ongoing COVID-19 pandemic, particular health concerns have been raised regarding vaping, such as whether vapers have higher risk for COVID-19 and could develop more severe symptoms once contracted COVID-19 (Majmundar et al., 2020). To our best knowledge, this is the first ecological study to empirically examine and observe an association between vaping and COVID-19.
The existing literature on the increased risk of respiratory infection in combustible cigarette smokers was summarized by a prior meta-analysis finding an increased risk of current smokers for influenza infection compared to non-smokers (Lawrence et al., 2019). As COVID-19 is a novel condition, the literature examining the risk of smokers for COVID-19 is scant. A recent study based on 1099 COVID-19 patients found smoking history was associated with COVID-19 severity (Guan et al., 2020). A recent systematic review on COVID-19 and smoking concludes that smoking is likely associated with worse outcomes in COVID-19 (Vardavas and Nikitara, 2020). However, other studies indicate that smoking might not be associated with the incidence and severity of COVID-19 (Cai, 2020), including a recent meta-analysis based on Chinese patients suggests that active smoking is not associated with severity of COVID-19 (Lippi and Henry, 2020). It remains unclear whether nicotine has a role in the either the increased or decreased severity of illness for smokers with COVID-19. Our study did not find a significant association between the weighted proportion of smokers and the number of COVID-19 infections and deaths at state level. Due to the incomplete testing and tracking of home deaths, it is possible that a percentage of older smokers with comorbidities are dying at home from COVID-19 and therefore are not captured into the reported COVID-19 cases and death data (Appleby, 2020, Simons et al., 2020). Additionally, it is unknown whether or not COVID-19 could be transmitted to those surrounding smokers through passive smoking and vaping. More epidemiological and clinical studies are needed to investigate the association of smoking with COVID-19 cases and deaths.
We found states that had a larger weighted proportion of subjects who had less than high school education had a higher number of COVID-19 cases. Researchers from the University of Southern California found that Americans who had less than high school education had a lower perceived risk of exposure to COVID-19 and a higher perceived risk of deaths than those who have college or higher degrees (Healthpolicy, n.d.). This might explain, in part, the positive association between the weighted proportion of less than high school education with the number of COVID-19 cases. We also found states that had a larger proportion of non-Hispanic Blacks and Hispanics had a larger number of COVID-19 deaths. The COVID-19 deaths rate data from Washington D.C. and 36 US states reported through April 27, 2020 showed that non-Hispanic Blacks (28.4%) and Hispanics (11.3%) had the highest COVID-19 deaths rate (Apmresearchlab, n.d.). This could be related to the higher proportion of chronic conditions such as hypertension, heart disease and diabetes in non-Hispanic Blacks and Hispanics (Al Kibria, 2019, Al Kibria et al., 2019). In addition, COVID-19 deaths could also be affected by availability and access to care as well as the level of care, which could contribute to the ethnic disparities in COVID-19 deaths. Interestingly, we found that states with a higher proportion of males had lower number of COVID-19 cases than states with higher proportion of females. Previous investigation in Chinese COVID-19 patients found a larger proportion of males admitted to hospital and males also had more severe symptoms and higher mortality rate (Guan et al., 2020, Epidemiology Working Group for Ncip Epidemic Response CCfDC, 2020, Jin et al., 2020, Xie et al., 2020). This observation of a gender difference in COVID-19 cases and death and the role of gender in COVID-19 cases and death in the US is worth further investigation. In addition, we observed that states with a higher proportion of obesity had reduced COVID-19 cases and death. One possible explanation could be that people who are obese have a decreased exposure to COVID-19 due to being relatively home-bound due to disability or mobility issues. Although recent studies indicate obesity might be a risk factor for severe COVID-19 symptoms, the evidence base detailing the association of obesity with COVID-19 cases and death is still limited and need further investigation (Caussy et al., 2020).
5. Limitations
There are several limitations in current study. First, the weighted proportions of vapers, smokers, and other demographic and chronic diseases are from the 2018 BRFSS data, which might differ from the 2020 estimates. The outbreak of e-cigarette, or vaping product use-associated lung injury (EVALI) occurred in September 2019 might change the vaping pattern on state levels as CDC issued guidance against the use of e-cigarettes. The reported COVID-19 cases and deaths obtained from 1Point3Acres.com website could be subject to some reporting errors as we noticed some negative number of COVID-19 cases and deaths, which we excluded from further analysis. However, we compared the COVID-19 data obtained from 1Point3Acres.com website with the COVID-19 data from the New York Times (Github, n.d.) and Centers for Disease Control and Prevention (CDC) website (CDC, n.d.) and found consistent numbers of COVID-19 cases and deaths, which increased the robustness and reliability of the data sources. Second, our current analysis is on state level instead of individual level. We don’t know the individual status of vaping and COVID-19 cases or deaths, thus estimated coefficients of association could be different from epidemiological or clinical studies on individual subjects. Third, this ecological study at a group-level is also subject to limitations such as ecological bias, confounding, and misclassifications. The group-level data did not include information on whether vapers were strictly following social/physical distancing guidelines to reduce their risks for COVID-19. Fourth, the study period did not cover the whole duration in the US as the pandemic is still ongoing. The analysis of the daily number of cases and deaths over the first period of the pandemic could be biased as the spread of the virus was unequally across states in the US during the first three months and our ecological study was not able to account for outbreak dynamics (e.g. size of outbreak, public health guidelines). Finally, the number of reported cases could be impacted by testing strategies and reporting system that might be different from one state to another.
6. Conclusions
There are positive associations between the weighted proportion of vapers in each US state and the daily number of COVID-19 cases and deaths in each US state. These positive associations suggest vapers may have an increased susceptibility to COVID-19 cases and deaths. Systematic assessment of vaping among patients, along with additional studies on the associations of vaping with COVID-19 infections and deaths at individual level are needed to further explore this positive association between vaping and COVID-19 cases and deaths.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health (NIH) and the Food and Drug Administration (FDA) Center for Tobacco Products under Award Number U54CA228110.
Author contributions
DL, ZX: conceived and designed the study. DL: analyzed the data. DL wrote the manuscript. DL, DC, DO, ZX: assisted with interpretation of analyses and edited the manuscript.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA.
Data sharing statement
The 2018 Behavioral Risk Factor Surveillance System (BRFSS) survey data are publicly available from the Centers for Disease Control and Prevention website (https://www.cdc.gov/brfss/annual_data/annual_2018.html). The state population in 2018 and the land area in each state were obtained from the United States Census Bureau website (https://www.census.gov/). The COVID-19 cases and deaths data were requested and obtained from the 1Point3Acres.com website (https://coronavirus.1point3acres.com/en).
References
- Cucinotta D., Vanelli M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020;91(1):157–160. doi: 10.23750/abm.v91i1.9397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong E., Du H., Gardner L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020 doi: 10.1016/S1473-3099(20)30120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn D.G., Shin H.J., Kim M.H. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19) J. Microbiol. Biotechnol. 2020;30(3):313–324. doi: 10.4014/jmb.2003.03011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H.Y., Leventhal A.M. Prevalence of e-cigarette use among adults in the United States, 2014–2018. JAMA-J. Am. Med. Assoc. 2019;322(18):1824–1827. doi: 10.1001/jama.2019.15331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaurav R. Vaping Away Epithelial Integrity. Am. J. Respir. Cell Mol. Biol. 2019;61(2):127–129. doi: 10.1165/rcmb.2019-0016ED. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin D.F., McGown K.A., Gallagher K. Electronic cigarette vapour increases virulence and inflammatory potential of respiratory pathogens. Respir. Res. 2019;20(1):267. doi: 10.1186/s12931-019-1206-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthumalage T., Lamb T., Friedman M.R., Rahman I. E-cigarette flavored pods induce inflammation, epithelial barrier dysfunction, and DNA damage in lung epithelial cells and monocytes. Sci. Rep. 2019;9(1):19035. doi: 10.1038/s41598-019-51643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu Q., Jiang D., Minor M., Chu H.W. Electronic cigarette liquid increases inflammation and virus infection in primary human airway epithelial cells. PLoS One. 2014;9(9) doi: 10.1371/journal.pone.0108342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li D., Sundar I.K., McIntosh S. Association of smoking and electronic cigarette use with wheezing and related respiratory symptoms in adults: cross-sectional results from the Population Assessment of Tobacco and Health (PATH) study, wave 2. Tob. Control. 2020;29(2):140–147. doi: 10.1136/tobaccocontrol-2018-054694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie Z., Ossip D.J., Rahman I., Li D. Use of electronic cigarettes and self-reported chronic obstructive pulmonary disease diagnosis in adults. Nicotine Tob. Res. 2019:ntz234. doi: 10.1093/ntr/ntz234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Majmundar A., Allem J.P., Cruz T.B., Unger J.B. Public health concerns and unsubstantiated claims at the intersection of vaping and COVID-19. Nicotine Tob. Res. 2020 doi: 10.1093/ntr/ntaa064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson T.R., Kim J.S. A generalized estimating equations approach to mixed-effects ordinal probit models. Br. J. Math. Stat. Psychol. 2004;57(Pt 2):295–310. doi: 10.1348/0007110042307177. [DOI] [PubMed] [Google Scholar]
- Vagenas D., Totsika V. Modelling correlated data: Multilevel models and generalized estimating equations and their use with data from research in developmental disabilities. Res. Dev. Disabil. 2018;81:1–11. doi: 10.1016/j.ridd.2018.04.010. [DOI] [PubMed] [Google Scholar]
- Bursac Z., Gauss C.H., Williams D.K., Hosmer D.W. Purposeful selection of variables in logistic regression. Source Code Biol. Med. 2008;3:17. doi: 10.1186/1751-0473-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lambrinos, J., 1984. Applied Linear-Regression Models - Neter, J, Wasserman, W, Kutner, Mh. Technometrics. 26(4),415–6.
- Eaton D.L., Kwan L.Y., Stratton K., editors. Public Health Consequences of E-Cigarettes. Washington, (DC); 2018. [Google Scholar]
- Madison M.C., Landers C.T., Gu B.H. Electronic cigarettes disrupt lung lipid homeostasis and innate immunity independent of nicotine. J. Clin. Invest. 2019;129(10):4290–4304. doi: 10.1172/JCI128531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang J.H., Lyes M., Sladewski K. Electronic cigarette inhalation alters innate immunity and airway cytokines while increasing the virulence of colonizing bacteria. J. Mol. Med. (Berl). 2016;94(6):667–679. doi: 10.1007/s00109-016-1378-3. [DOI] [PubMed] [Google Scholar]
- Rynda-Apple A., Robinson K.M., Alcorn J.F. Influenza and bacterial superinfection: illuminating the immunologic mechanisms of disease. Infect. Immun. 2015;83(10):3764–3770. doi: 10.1128/IAI.00298-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clapp P.W., Pawlak E.A., Lackey J.T. Flavored e-cigarette liquids and cinnamaldehyde impair respiratory innate immune cell function. Am. J. Physiol. Lung Cell Mol. Physiol. 2017;313(2):L278–L292. doi: 10.1152/ajplung.00452.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reidel B., Radicioni G., Clapp P.W. E-Cigarette Use Causes a Unique Innate Immune Response in the Lung, Involving Increased Neutrophilic Activation and Altered Mucin Secretion. Am. J. Respir. Crit. Care Med. 2018;197(4):492–501. doi: 10.1164/rccm.201708-1590OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotts J.E., Jordt S.E., McConnell R., Tarran R. What are the respiratory effects of e-cigarettes? BMJ. 2019;366 doi: 10.1136/bmj.l5275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang M.P., Ho S.Y., Leung L.T., Lam T.H. Electronic Cigarette Use and Respiratory Symptoms in Chinese Adolescents in Hong Kong. JAMA Pediatr. 2016;170(1):89–91. doi: 10.1001/jamapediatrics.2015.3024. [DOI] [PubMed] [Google Scholar]
- McConnell R., Barrington-Trimis J.L., Wang K. Electronic Cigarette Use and Respiratory Symptoms in Adolescents. Am. J. Respir. Crit. Care Med. 2017;195(8):1043–1049. doi: 10.1164/rccm.201604-0804OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrence H., Hunter A., Murray R., Lim W.S., McKeever T. Cigarette smoking and the occurrence of influenza - Systematic review. J. Infect. 2019;79(5):401–406. doi: 10.1016/j.jinf.2019.08.014. [DOI] [PubMed] [Google Scholar]
- Guan W.J., Ni Z.Y., Hu Y. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl. J. Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vardavas C.I., Nikitara K. COVID-19 and smoking: A systematic review of the evidence. Tob. Induc. Dis. 2020;18:20. doi: 10.18332/tid/119324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai H. Sex difference and smoking predisposition in patients with COVID-19. Lancet Respir. Med. 2020;8(4) doi: 10.1016/S2213-2600(20)30117-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lippi G., Henry B.M. Active smoking is not associated with severity of coronavirus disease 2019 (COVID-19) Eur. J. Intern. Med. 2020;75:107–108. doi: 10.1016/j.ejim.2020.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appleby J. What is happening to non-covid deaths. BMJ. 2020;369 doi: 10.1136/bmj.m1607. [DOI] [PubMed] [Google Scholar]
- Simons D., Shahab L., Brown J., Perski O. The association of smoking status with SARS-CoV-2 infection, hospitalisation and mortality from COVID-19: A living rapid evidence review. Qeios. 2020 doi: 10.1111/add.15276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://healthpolicy.usc.edu/evidence-base/individuals-with-low-incomes-less-education-report-higher-perceived-financial-health-threats-from-covid-19/.
- https://www.apmresearchlab.org/covid/deaths-by-race.
- Al Kibria G.M. Racial/ethnic disparities in prevalence, treatment, and control of hypertension among US adults following application of the 2017 American College of Cardiology/American Heart Association guideline. Prev. Med. Rep. 2019;14 doi: 10.1016/j.pmedr.2019.100850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Kibria G.M., Nemirovsky A., Sharmeen A., Day B. Age-stratified prevalence, treatment status, and associated factors of hypertension among US adults following application of the 2017 ACC/AHA guideline. Hypertens. Res. 2019;42(10):1631–1643. doi: 10.1038/s41440-019-0275-x. [DOI] [PubMed] [Google Scholar]
- Epidemiology Working Group for Ncip Epidemic Response CCfDC, 2020. Prevention. [The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China]. Zhonghua Liu Xing Bing Xue Za Zhi. 41(2),145–151. [DOI] [PubMed]
- Jin J.M., Bai P., He W. Gender Differences in Patients With COVID-19: Focus on Severity and Mortality. Front. Public Health. 2020;8:152. doi: 10.3389/fpubh.2020.00152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie J., Tong Z., Guan X., Du B., Qiu H. Clinical Characteristics of Patients Who Died of Coronavirus Disease 2019 in China. JAMANetw Open. 2020;3(4) doi: 10.1001/jamanetworkopen.2020.5619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caussy C., Pattou F., Wallet F. Prevalence of obesity among adult inpatients with COVID-19 in France. Lancet Diabetes Endocrinol. 2020 doi: 10.1016/S2213-8587(20)30160-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- https://github.com/nytimes/covid-19-data.
- https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/previouscases.html.