Abstract
Objective
The delays in elective surgery caused by the coronavirus disease 2019 (COVID-19) pandemic have resulted in a substantial backlog of cases. In the present study, we sought to determine the estimated time to recovery for vascular surgery procedures delayed by the COVID-19 pandemic in a regional health system.
Methods
Using data from a 35-hospital regional vascular surgical collaborative consisting of all hospitals performing vascular surgery in the state of Michigan, we estimated the number of delayed surgical cases for adults undergoing carotid endarterectomy, carotid stenting, endovascular and open abdominal aortic aneurysm repair, and lower extremity bypass. We used seasonal autoregressive integrated moving average models to predict the surgical volume in the absence of the COVID-19 pandemic and historical data to predict the elective surgical recovery time.
Results
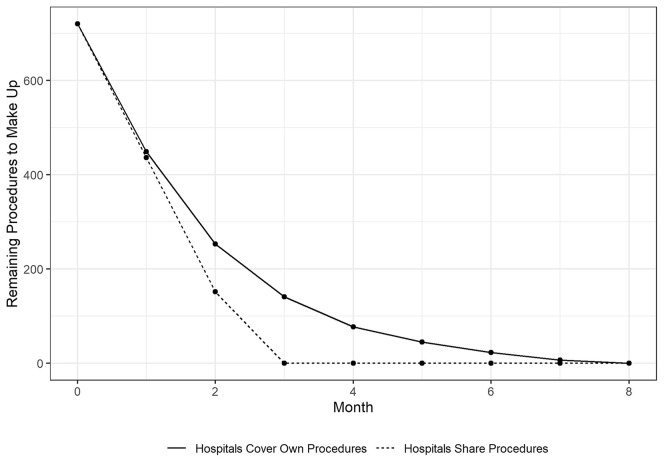
The median statewide monthly vascular surgical volume for the study period was 439 procedures, with a maximum statewide monthly case volume of 519 procedures. For the month of April 2020, the elective vascular surgery procedural volume decreased by ∼90%. Significant variability was seen in the estimated hospital capacity and estimated number of backlogged cases, with the recovery of elective cases estimated to require ∼8 months. If hospitals across the collaborative were to share the burden of backlogged cases, the recovery could be shortened to ∼3 months.
Conclusions
In the present study of vascular surgical volume in a regional health collaborative, elective surgical procedures decreased by 90%, resulting in a backlog of >700 cases. The recovery time if all hospitals in the collaborative were to share the burden of backlogged cases would be reduced from 8 months to 3 months, underscoring the necessity of regional and statewide policies to minimize patient harm by delays in recovery for elective surgery.
Keywords: COVID-19, Elective surgery, Health system
Article Highlights.
-
•
Type of Research: A retrospective analysis of prospectively collected registry data (Blue Cross Blue Shield of Michigan Cardiovascular Collaborative)
-
•
Key Findings: A substantial decrease occurred in elective surgery in response to the coronavirus disease 2019 pandemic, resulting in >700 delayed vascular surgical procedures in a regional health collaborative. Recovery will take an estimated 8 months to complete.
-
•
Take Home Message: The local, regional, and national response to elective surgical delays should focus on prioritizing patients at the greatest risk of morbidity owing to the prolonged delay and policy makers' need to consider incentivizing interfacility transfer of delayed cases to speed the recovery and minimize patient morbidity.
Coronavirus disease 2019 (COVID-19) has disrupted all facets of healthcare delivery worldwide, including the delivery of elective surgical care. Many hospitals reduced or even eliminated elective surgical care in an effort to preserve the resources necessary for delivering care to COVID-19 patients.1, 2, 3 Delays in treatment, especially for time-sensitive surgical diseases, such as malignancy or cardiovascular disease, can result in worse quality of life and disease severity and increased morbidity and mortality.4, 5, 6, 7
Estimates of surgical delays have been limited to surveys of providers at a national level. Additionally, the capacity of regional health systems to recover from the deferment of cases and the distribution of that variability has not been explored. Thus, we sought to examine the number of delayed cases in the state of Michigan using real-time and historical data and estimate the recovery trajectory using information from a statewide vascular surgical consortium.
Methods
Data source and study population
We collected data for all adult patients who had undergone elective carotid endarterectomy, carotid stenting, endovascular and open abdominal aortic aneurysm repair, and lower extremity bypass included in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium. The Blue Cross Blue Shield of Michigan Cardiovascular Consortium is a longitudinal multicenter statewide registry of vascular surgery and carotid interventions in Michigan, which has been described in detail previously.8 , 9 In brief, the registry is composed of a consortium of 35 hospitals within the state of Michigan that was designed as a regional collaborative effort to assess and improve the quality of care and outcomes. Data from consecutive patients undergoing a variety of cardiovascular surgeries and procedural care at participating hospitals are included. The data quality, accuracy, and completeness are assessed by ad hoc queries, random record review, and a series of diagnostic routines included in the database. All sites are audited twice annually by a nurse investigator from the coordinating center, with a random sampling of 5% of cases audited for accuracy. Data from each hospital are reported within 1 month of the performance of surgical procedures. Owing to the use of retrospective deidentified data, the institutional review board at the University of Michigan (Ann Arbor, Mich) exempted the present cohort study from approval and the requirement for written informed consent. The present study followed the STROBE (strengthening reporting of observational studies in epidemiology) guidelines.10
Outcomes and statistical modeling
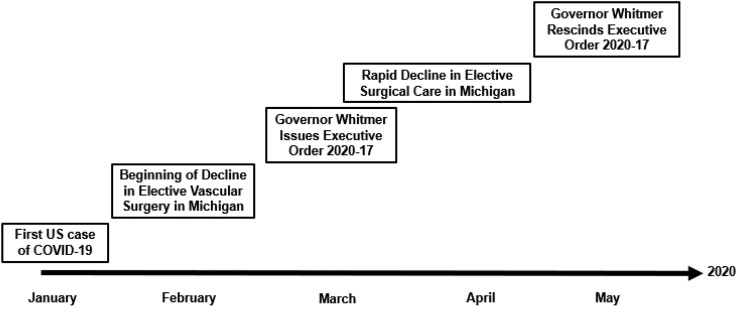
Our analysis was conducted from May 28 to June 5, 2020 and included data from January 1, 2017 to April 30, 2020. On March 20, 2020, Michigan Governor Whitmer issued Executive Order 2020-17 (COVID-19), which directed all “covered” healthcare facilities to halt elective surgical procedures.11 This continued until approximately the second week of May 2020, when many hospitals began to increase their elective volume. No specific guidance was provided by the executive order regarding the definition of elective vs urgent/emergent but, rather, included the following statement: “For purposes of this order, ‘non-essential procedure’ means a medical or dental procedure that is not necessary to address a medical emergency or to preserve the health and safety of a patient, as determined by a licensed medical provider.” Our dataset included only data for procedures that the clinician had deemed elective according to their clinical expertise. A visual representation of the timeline of relevant events is shown in Fig 1 . All variables had complete data available, and no imputation was performed.
Fig 1.
Timeline of events affecting surgical volume in Michigan during the pandemic.
We calculated the mean and maximum monthly vascular surgical volumes for all hospitals within the registry. To estimate the number of forecasted procedures in the absence of COVID-19, we used two standard forecasting methods: (1) seasonal autoregressive integrated moving average and (2) carrying forward the historical mean.12 Both forecasting methods produced similar predictions. The number of delayed cases was calculated as the difference between the forecasted value for each month after February 2020 and the actual number of cases completed according to the registry data for that month. To estimate the time to recovery, we set the maximum monthly capacity of each hospital system in the state as the maximum monthly case volume that individual hospital had achieved in the 3 years before the decrease in elective surgical volume in March 2020. This procedure was repeated for each hospital within the collaborative. All analyses were performed using R, version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).13
Results
The summary statistics for the individual hospitals are reported in the Table . Data from 35 hospitals were included in the present analysis, with an overall statewide mean of 437.62 total procedures per month. The historical median was similar at 439 total procedures per month, with a statewide historical maximum monthly volume of 506 procedures. In April 2020, a total of 40 elective vascular surgical procedures were completed, representing a 90.0% reduction in the overall volume of 443 forecasted procedures.
Table.
Summary of hospital characteristics
| Characteristic | No. (%) |
|---|---|
| Monthly vascular surgery volume | |
| <10 | 14 (40.0) |
| 10-20 | 15 (42.9) |
| >20 | 6 (17.1) |
| Beds, No. | |
| <300 | 7 (20.0) |
| 300-500 | 19 (54.3) |
| >500 | 9 (25.7) |
| Annual admissions, No. | |
| <15,000 | 9 (26.5) |
| 15,000-30,000 | 17 (50.0) |
| >30,000 | 8 (23.5) |
| Teaching hospital | 11 (31.4) |
| Hospital locale | |
| Urban | 30 (88.2) |
| Rural | 4 (11.8) |
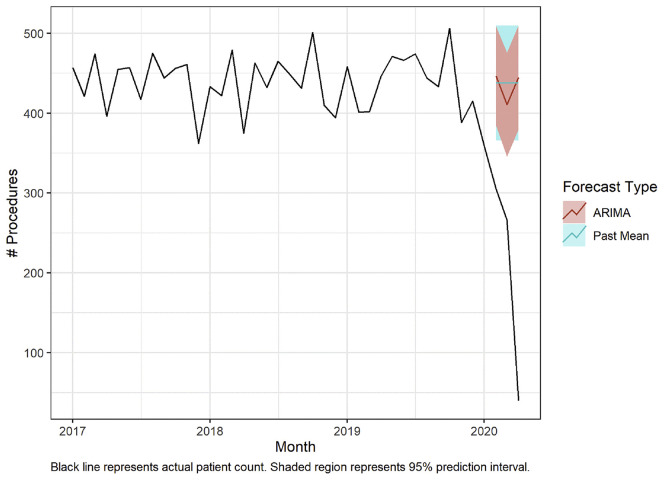
The statewide historical monthly surgical volumes, in addition to the forecasted volumes with the absence of the COVID-19 effect, are shown in Fig 2 . The estimated backlog of vascular surgical procedures from February to April 2020 was 702 procedures. The statewide capacity for these vascular procedures, defined as the difference between the statewide maximum monthly surgical volume and the statewide mean monthly surgical volume for the study period, was 81.38 cases. Thus, the estimated recovery time was 8.62 months.
Fig 2.
Actual and forecasted surgical case volume. Solid black line indicates actual case volumes. Forecasted surgical case volumes in the absence of the effect from coronavirus disease 2019 (COVID-19) are shown, with shaded areas representing 95% confidence intervals. ARIMA, Autoregressive integrated moving average.
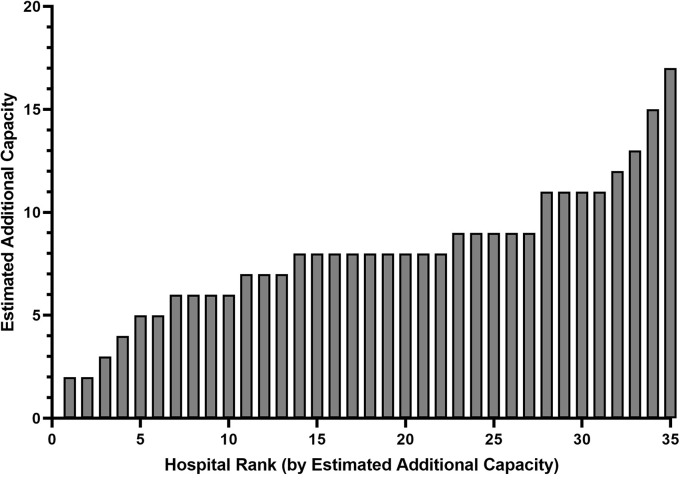
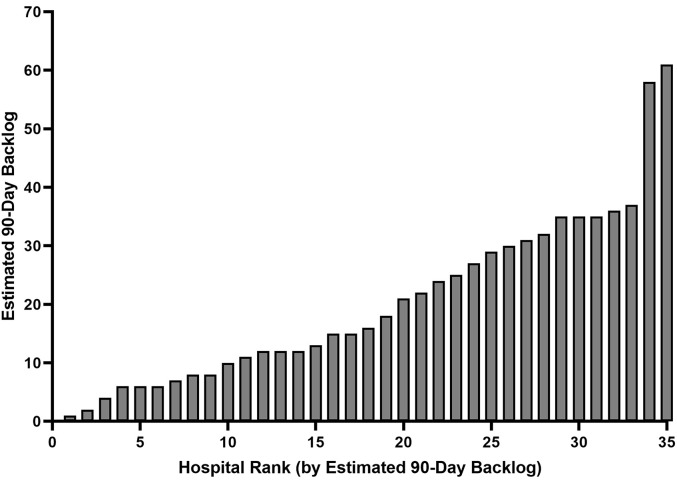
The hospital level capacity estimates revealed significant variability across institutions (Supplementary Fig 1, online only). Significant variation was found in the 3-month backlog volumes across the hospitals in the collaborative (Supplementary Fig 2, online only).
Supplementary Fig 1 (online only).
Estimated hospital-specific additional elective vascular surgery capacity. The hospitals were ranked according to the estimated capacity, and these ranks do not necessarily correlate with the hospital ranks of Supplementary Fig 2 (online only).
Supplementary Fig 2 (online only).
Estimated 90-day hospital-specific backlog of elective vascular surgical cases. Hospitals were ranked according to the estimated backlogged cases, and these ranks do not necessarily correlate with hospital ranks of Supplementary Fig 1 (online only).
To model the effect of the optimal interfacility referral of cases to hospitals with excess capacity within the collaborative, we estimated the time to recovery with each hospital only treating the backlogged cases within that hospital and compared this against the time to recovery if the backlogged cases were transferred to hospitals with excess capacity. The recovery curves are shown in Fig 3 . With hospitals only completing their own backlogged cases, the recovery would require ∼8 months. In contrast, the recovery would be reduced to 3 months if the hospitals were to share the burden of backlogged cases across the collaborative.
Fig 3.
Projected surgical case recovery trajectories. Solid black line indicates predicted recovery trajectory if all hospitals only performed their own backlogged cases; dotted black line indicates predicted recovery trajectory if all hospitals were to share the burden of backlogged cases until all cases were completed.
Conclusions
In the present study from a statewide collaborative, we found a rapid decrease in elective vascular surgical procedures and that this decreased elective surgical volume led to a large pool of deferred cases. Our models suggest that if hospital systems worked at the maximum capacity they had achieved for their vascular surgical volume during the previous 3 years, it would require 8 months to complete these delayed cases and also care for the normal flux of surgical patients. This recovery period could be dramatically shortened if the hospitals within the state were to share the burden of delinquent cases across the 35-hospital collaborative.
Completing backlogged cases in the order in which they were delayed could result in unnecessary harm to patients whose cases were delayed later in the pandemic but who might have more time-sensitive underlying diagnoses or might have a greater risk of experiencing harm from the delay. The cases should be prioritized according to each patient's probability of harm rather than strictly by the patient's position in the queue.
In the pre-COVID-19 era, interfacility referrals for surgical procedures capable of being completed at either hospital were uncommon. Our data suggest that the variability in surgical capacity across hospitals is substantial. With the large delay many patients are facing for vascular surgical care, coupled with the likely misalignment of backlogged and future hospital surgical capacity, healthcare systems should consider the redistribution of procedures to optimize the delivery of care and minimize the wait time. Although we are unable to capture the procedure volume for hospitals outside the state, especially given the dramatic regional variation in COVID-19 cases, considering the interfacility transfer of cases to hospitals outside the regional health system could be another mechanism to improve the time to treatment for patients on the backlog. State and national policy might need to incentivize referrals to minimize the financial losses from deferred patients and offset the financial incentive of hospitals to keep patients on the backlog when surrounding hospitals might have the capacity to treat them.
These results must be interpreted within the context of several limitations. The estimates presented in the present study are dependent on several assumptions, which are difficult to verify at the current stage of the pandemic. First, these data reflect any unmeasured relationships between hospital capacity and the characteristics of the Michigan vascular surgery patient population and its health systems. This might limit the generalizability of these findings to other regions or hospital systems with differing populations, geography, or other elements that could affect capacity and the recovery. Although previous studies have suggested that many hospitals operate near capacity with respect to surgical volume, it might be that either significant additional capacity is available that was not used in the 3-year study period or that the single month of data did not represent a sustainable monthly rate. The Executive Order affecting elective surgical care in the state of Michigan did not provide any guidance beyond what we described to help hospitals determine which surgical cases should be deferred and which should continue. Rather, hospitals and the surgeons operating within them were tasked with making this determination based on their clinical expertise. Thus, the indications for the elective procedures completed during the study period are not known and significant heterogeneity could be present across systems and surgeons with respect to what they consider elective. This has implications for the application of our findings to other states or regions, and our results should be interpreted within this context. Additionally, vascular surgical care occurs at most hospitals within the context of a broader scope of surgical care delivery, and hospitals might have even less capacity for vascular surgical procedures when considering the likely backlog of all other surgical care that must be delivered. Finally, the projections for recovery if hospitals were to share the backlog of cases is dependent on the “receiving” hospital having the capability of performing the backlogged operations and the assumption that the reintroduction of elective surgery does not occur over a prolonged interval. This assumption is difficult to verify and, in fact, is likely to be a dynamic property of the hospital, even for those hospitals with the physical capability of performing the procedure. Thus, our projections represent a “best case” scenario in which all hospitals in the collaborative are capable of caring for any of the backlogged patients and that hospitals return immediately to performing elective surgery at capacity.
To the best of our knowledge, the present study represents the first analysis of backlogged vascular surgical cases due to the COVID-19 pandemic and provides the first estimates for a recovery trajectory within a regional health system. These results should inform case prioritization efforts and local, regional, and national policy to maximize safe and equitable surgical care during the post–COVID-19 recovery.
Author contributions
Conception and design: CB, PH, NO
Analysis and interpretation: CB, JA, PH, MM, MW, NO
Data collection: Not applicable
Writing the article: CB, JA, PH, MM, MW, NO
Critical revision of the article: CB, JA, PH, MM, MW, NO
Final approval of the article: CB, JA, PH, MM, MW, NO
Statistical analysis: CB, JA, NO
Obtained funding: Not applicable
Overall responsibility: CB
Footnotes
C.S.B. is supported by the Ruth L. Kirschstein Postdoctoral Research Fellowship Award administered from the National Institute on Drug AbuseF32-DA050416.
Author conflict of interest: none.
Additional material for this article may be found online at www.jvascsurg.org.
The editors and reviewers of this article have no relevant financial relationships to disclose per the JVS policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
Additional material for this article may be found online at www.jvascsurg.org.
Appendix (online only).
References
- 1.COVIDSurg Collaborative Elective surgery cancellations due to the COVID-19 pandemic: global predictive modelling to inform surgical recovery plans. Br J Surg. 2020 May 12 doi: 10.1002/bjs.11746. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.American College of Surgeons COVID-19: Elective Case Triage Guidelines for Surgical Care. https://www.facs.org/covid-19/clinical-guidance/elective-case Available at:
- 3.Søreide K., Hallet J., Matthews J.B., Schnitzbauer A.A., Line P.D., Lai P.B.S., et al. Immediate and long-term impact of the COVID-19 pandemic on delivery of surgical services. Br J Surg. 2020 Apr 30 doi: 10.1002/bjs.11670. [E-pub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shin D.W., Cho J., Kim S.Y., et al. Delay to curative surgery greater than 12 weeks is associated with increased mortality in patients with colorectal and breast cancer but not lung or thyroid cancer. Ann Surg Oncol. 2013;20:2468–2476. doi: 10.1245/s10434-013-2957-y. [DOI] [PubMed] [Google Scholar]
- 5.Ho P.J., Cook A.R., Binte Mohamed Ri N.K., Liu J., Li J., Hartman M. Impact of delayed treatment in women diagnosed with breast cancer: a population-based study. Cancer Med. 2020;9:2435–2444. doi: 10.1002/cam4.2830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brott T.G., Halperin J.L., Abbara S., Bacharach J.M., Barr J.D., Bush R.L., et al. 2011 ASA/ACCF/AHA/AANN/AANS/ACR/ASNR/CNS/SAIP/SCAI/SIR/SNIS/SVM/SVS guideline on the management of patients with extracranial carotid and vertebral artery disease: executive summary. Circulation. 2011;124:489–532. [Google Scholar]
- 7.Ricotta J.J., AbuRahma A., Ascher E., Eskandari M., Faries P., Lal B.K. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease. J Vasc Surg. 2011;54:e1–e31. doi: 10.1016/j.jvs.2011.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Mukherjee D., Munir K., Hirsch A.T., Chetcuti S., Grossman P.M., Rajagopalan S., et al. Development of a multicenter peripheral arterial interventional database: the PVD-QI2. Am Heart J. 2005;149:1003–1008. doi: 10.1016/j.ahj.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 9.Krishnamurthy V., Munir K., Rectenwald J.E., Mansour A., Hans S., Eliason J.L., et al. Contemporary outcomes with percutaneous vascular interventions for peripheral critical limb ischemia in those with and without poly-vascular disease. Vasc Med. 2014;19:491–499. doi: 10.1177/1358863X14552013. [DOI] [PubMed] [Google Scholar]
- 10.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The strengthening the reporting of observational studies in epidemiology (STROBE) statement. Epidemiology. 2007;18:800–804. doi: 10.1097/EDE.0b013e3181577654. [DOI] [PubMed] [Google Scholar]
- 11.The Office of Governor Gretchen Whitmer Executive Order 2020-17 (COVID-19) https://www.michigan.gov/whitmer/0,9309,7-387-90499_90705-522451--,00.html Available at:
- 12.Box G.E.P., Jenkins G.M. Holden-Day; San Francisco, CA: 1970. Time Series Analysis: Forecasting and Control. [Google Scholar]
- 13.R: The R Project for Statistical Computing. https://www.r-project.org/ Available at: