Abstract
Background:
Many state and local health departments now promote and support the use of HIV pre-exposure prophylaxis (PrEP), yet monitoring use of the intervention at the population level remains challenging.
Methods:
We report the results of an online survey designed to measure PrEP use among men who have sex with men (MSM) in Washington State. Data on the proportion of men with indications for PrEP based on state guidelines and levels of awareness, interest, and use of PrEP are presented for 1,080 cisgender male respondents who completed the survey between January 1 and February 28, 2017. We conducted bivariate and multivariable logistic regression to identify factors associated with current PrEP use. To examine patterns of discontinuation, we conducted Cox Proportional Hazards regression and fit a Kaplan Meier curve to reported data on time on PrEP.
Results:
Eighty percent of respondents had heard of PrEP, 19% reported current use, and 36% of men who had never used PrEP wanted to start taking it. Among MSM for whom state guidelines recommend PrEP, 31% were taking it. In multivariable analysis, current PrEP use was associated with older age, higher education, and meeting indications for PrEP use. Our data suggest that 20% of PrEP users discontinue within 12 months, and men with lower educational attainment were more likely to discontinue.
Conclusions:
Despite high levels of use, there is significant unmet need for PrEP in Washington. Our experience indicates that internet surveys are feasible and informative for monitoring PrEP use in MSM.
Keywords: Pre-exposure prophylaxis, PrEP, HIV prevention, Men who have sex with men, Internet survey
Summary
Data from an internet-based survey indicate that use of HIV pre-exposure prophylaxis is high among Washington State men who have sex with men, though there remains substantial unmet need.
Introduction
Expanding access to HIV pre-exposure prophylaxis (PrEP) has become a pillar of the HIV prevention strategy in the United States,1 supported by strong evidence of the intervention’s efficacy and effectiveness from clinical trials and observational studies.2 The potential population-level impact of PrEP is particularly significant for men who have sex with men (MSM), who experienced 70% of new HIV diagnoses nationally in 2016.3 The U.S. Public Health Service has issued guidelines recommending PrEP for high-risk MSM and other priority populations,4 but large gaps have been reported between eligibility, interest, and use.5–7 To inform efforts to improve PrEP delivery, reliable data are needed to describe the populations at risk, monitor use, and characterize the barriers to uptake and retention in care.
Measuring PrEP use among MSM is methodologically challenging due to the lack of efficient and unbiased sampling methods for this population. In the U.S., data on MSM’s use of prevention interventions have primarily come from clinic samples,7,8 which are limited to persons who seek care in selected clinics or healthcare organizations, and venue- and event-based samples,9,10 which are often expensive and limited in geographic scope. Internet-based recruitment has gained popularity as an alternative strategy for sampling MSM,11–15 but this approach has not yet been widely adopted by state and local health departments for purposes of public health monitoring.
In this paper, we present the findings from the 2017 Washington HIV Prevention Project (WHPP), an internet-based survey developed to monitor the success of Washington State’s efforts to promote PrEP use among high-risk resident MSM. To evaluate the consistency of WHPP findings with data from offline samples, we compare our estimates of PrEP use to estimates from an in-person survey administered at the 2017 Seattle Pride parade.16
Methods
We recruited participants to complete an online cross-sectional survey between January 1 and February 28, 2017. Participants accessed the survey through banner and text-based pop-up advertisements on social media, male-male geosocial networking, and general LGBTQ-interest apps and websites. Upon clicking past a landing webpage with information on the purpose of the survey, participants were randomly shown one of three informed consent pages that differed only in the stated incentive: a $10 Amazon gift certificate, a $10 donation to charity, or no monetary incentive. Through daily monitoring of IP addresses and timestamps (described in Supplemental Digital Content 1), we identified a pattern of seemingly fraudulent responses that led us to discontinue the gift certificate incentive after nine days.
Consenting participants were shown a set of questions to screen for eligibility. Persons were ineligible if they were female sex at birth, age <16 years, lived outside of Washington, did not have oral or anal sex with a man in the past 12 months, reported ever testing positive for HIV, or had an Internet Protocol (IP) address outside the U.S. Additional details on survey methods are provided in Supplemental Digital Content 1. Because this work was conducted as a public health surveillance activity, it was determined not to be human subjects research by the University of Washington Institutional Review Board.
Key Measures
Prior to answering questions about PrEP, respondents were presented with the following description: “PrEP is a pill taken every day by HIV-negative people to reduce the risk of getting HIV. It is currently available under the brand name Truvada®.” Respondents who had heard of PrEP were asked if they were currently taking or had taken it in the past. Men who had never taken PrEP were asked if they were interested in taking it, with response options of “Yes, I want to start taking PrEP”, “I am not sure about PrEP, but I would like to learn more about it,” and “No, I am not interested in taking PrEP.” Follow-up questions asked why they were not interested or had not yet initiated (see Supplemental Digital Content 2 for response options). Current and past PrEP users reported the month and year they most recently started PrEP, and men who had discontinued additionally reported the month and year in which they last took PrEP. We measured self-reported adherence over the past 30 days and defined high adherence as taking ≥4 pills per week on average.17 Men who had discontinued PrEP indicated why they stopped their medication and whether they were interested in taking it again. All participants were asked how effective they thought PrEP is at preventing HIV infection if taken every day.
PrEP candidacy was defined according to guidelines developed by Public Health – Seattle and King County and the Washington State Department of Health (WADOH).18 These guidelines were adapted from those issued by the U.S. Public Health Service,4 the International Antiviral Society—USA,19 and the World Health Organization20 to reflect the local epidemic context, and were informed by analyses that identified factors associated with HIV acquisition. The guidelines define two tiers of risk: persons for whom medical providers should recommend PrEP, and persons with whom providers should discuss PrEP (Table 1).
Table 1:
PrEP candidacy categories based on Washington State PrEP implementation guidelines
| Recommend PrEP for MSM with any of the following risk factors: |
|
| Discuss PrEP with MSM who do not meet the above criteria for recommending PrEP and who report any of the followinga: |
|
The guidelines refer to diagnosis of early syphilis. Due to the difficulty of measuring stage of infection via self-report, for this analysis we included any diagnosis of syphilis as an indication for recommending PrEP;
Three indications for discussing PrEP with MSM were not measured in the survey: having an HIV-positive female partner with intentions to conceive, completing a course of post-exposure prophylaxis for non-occupational exposure, and seeking a prescription for PrEP;
Proxy measure for CAS outside of a long-term, mutually monogamous relationship with a partner who is HIV-negative.
To assess heterogeneity in PrEP uptake across the state, we categorized respondents as residing in one of three regions based on reported ZIP codes: King County (which includes Seattle), other counties in western Washington, and eastern Washington (see Figure, Supplemental Digital Content 3, for a regional map).
Analyses
Duplicate and invalid responses were flagged and removed using a modified version of a published protocol,21 described in Supplemental Digital Content 1. Data are presented from respondents who completed the survey at least through initial questions about PrEP awareness and use. To identify factors associated with current PrEP use, we conducted logistic regression. We first examined associations for a base model including the following covariates, which were defined a priori: region, age, race/ethnicity, sexual orientation, education, income, and PrEP candidacy. In an exploratory analysis, we examined bivariate associations with other factors measured in our survey, including health insurance, perceived effectiveness of PrEP, and specific HIV risk indicators. Our multivariable exploratory model included base model social and demographic variables and additional factors that were significant in bivariate analyses.
We estimated time to PrEP discontinuation by fitting a Kaplan Meier curve to reported data on dates of first and last PrEP use. Current users’ time on PrEP was censored at the date of survey completion. Time-invariant predictors of discontinuation (age at PrEP initiation, race/ethnicity, education, and region of residence) were explored using multivariable Cox Proportional Hazards regression, employing the exact marginal method to adjust for ties.
To assess the consistency of WHPP findings with data from sources using offline (in-person) recruitment, we compared estimates of PrEP awareness and use with those from a sample of MSM who completed a self- or interviewer-administered paper questionnaire at the Seattle Pride Parade in June 2017.16 In this analysis, both samples were restricted to cisgender males living in the Seattle metropolitan area. To account for differences in the HIV risk profile of the two samples, we tabulated the proportion reporting PrEP use among high-risk men for whom state guidelines recommend the intervention. Because the Pride survey did not measure current partnerships with HIV-positive partners, this indication was not included when defining risk groups for this comparison. Analyses were conducted using Stata version 13.1 (StataCorp, College Station, TX). An alpha of 0.05 was used for significance testing.
Results
Recruitment, response rates, and cost
In the two-month recruitment period, 2,767 unique individuals consented to the survey, 44% of whom (1,225) met inclusion criteria. Seventy-nine percent (973) of eligible participants completed the survey. The costs of recruitment, survey administration, and incentives totaled $23.69 per complete response (see Appendix, Supplementary Digital Content 1, for details on response rates and expenses). For this analysis, we excluded respondents who reported a gender other than male (n=32), resulting in 1,080 responses from cisgender males who completed the survey through initial questions about PrEP, of whom 924 completed the entire survey.
Sample characteristics
The median age in the sample was 30 (range: 16–82), and 61% of respondents were below the age of 35 (Table 2). Two-thirds of the sample (68%) identified as non-Hispanic white, and 49% reported a 4-year college degree or higher education. Fifty-six percent of respondents reported residence in King County. Based on reported behaviors and experiences within the past 12 months, 33% of men met criteria indicating that medical providers should recommend PrEP initiation. Another 30% of men met criteria indicating that a medical provider should discuss PrEP with them.
Table 2:
Sample characteristics
| n/Na | % | |
|---|---|---|
| Recruitment platform | ||
| Social media | 806/1,080 | 74.6% |
| Geosocial networking | 211/1,080 | 19.5% |
| General LGBTQ interest | 63/1,080 | 5.8% |
| Demographic and social characteristics | ||
| Region | ||
| King County | 610/1,080 | 56.5% |
| Other counties in western Washington | 308/1,080 | 28.5% |
| Eastern Washington | 162/1,080 | 15.0% |
| Age | ||
| 16 to 24 | 313/1,080 | 29.0% |
| 25 to 34 | 351/1,080 | 32.5% |
| 35 to 44 | 167/1,080 | 15.5% |
| 45 to 54 | 128/1,080 | 11.9% |
| 55 and older | 121/1,080 | 11.2% |
| Race/ethnicity | ||
| Hispanic | 198/1,067 | 18.6% |
| Non-Hispanic white | 725/1,067 | 67.9% |
| Non-Hispanic black | 42/1,067 | 3.9% |
| Non-Hispanic other | 102/1,067 | 9.6% |
| Gay/homosexual identity | 889/1,076 | 82.6% |
| Education | ||
| High school or less | 176/1,065 | 16.5% |
| Some college/vocational school | 364/1,065 | 34.2% |
| 4-year college or higher | 525/1,065 | 49.3% |
| Income | ||
| Less than $15,000 | 110/930 | 11.8% |
| $15,000 to $29,999 | 111/930 | 11.9% |
| $30,000 to $49,999 | 167/930 | 18.0% |
| $50,000 to $99,999 | 278/930 | 29.9% |
| $100,000 or more | 215/930 | 23.1% |
| Prefer not to answer | 49/930 | 5.3% |
| Has health insurance | 929/1,037 | 89.6% |
| HIV and STI testing | ||
| HIV testing history | ||
| Never tested | 219/1,074 | 20.4% |
| Tested in the past 12 months | 657/1,074 | 61.2% |
| Tested >12 months ago | 198/1,074 | 18.4% |
| STI diagnosis (past 12 months) | ||
| Rectal gonorrhea | 47/1,025 | 4.6% |
| Syphilis | 57/1,025 | 5.6% |
| Any bacterial STIb | 189/1,025 | 18.4% |
| Sexual behaviors and drug use (past 12 months) | ||
| Anal sex role | ||
| No anal sex | 103/1,000 | 10.3% |
| Exclusively bottom | 197/1,000 | 19.7% |
| Versatile | 578/1,000 | 57.8% |
| Exclusively top | 122/1,000 | 12.2% |
| ≥10 anal sex partners | 162/1,013 | 16.0% |
| Current main/primary male partner | 443/998 | 44.4% |
| Current HIV-positive male partner | 79/979 | 8.1% |
| CAS with a non-main partner | 476/980 | 48.6% |
| CAS with an unknown status partner | 280/975 | 28.7% |
| CAS with an HIV-positive partner | 145/979 | 14.8% |
| Injection drug use | 57/938 | 6.1% |
| Methamphetamine use | 81/926 | 8.7% |
| Poppers use | 211/926 | 22.8% |
| History of exchange sex | 36/935 | 3.9% |
| PrEP awareness and use | ||
| PrEP awareness | 852/1,080 | 78.9% |
| Perceived effectiveness of PrEP | ||
| Less than 75% | 260/1,036 | 25.1% |
| 75% to 89% | 174/1,036 | 16.8% |
| 90% or higher | 524/1,036 | 50.6% |
| Unsure/Prefer not to answer | 78/1,036 | 7.5% |
| Use of PrEP | ||
| Never | 832/1,080 | 77.0% |
| Current | 200/1,080 | 18.5% |
| Past | 48/1,080 | 4.4% |
| WA State PrEP guideline category | ||
| Recommendc | 303/912 | 33.2% |
| Discussd | 271/912 | 29.7% |
| Not indicated | 338/912 | 37.1% |
Acronyms: STI, sexually transmitted infection; CAS, condomless anal sex; PrEP, pre-exposure prophylaxis
Includes data from 924 complete and 156 partial responses that completed the survey at least through questions about PrEP use. Denominators may vary due to missing data;
Diagnosis of gonorrhea (pharyngeal, urethral, or rectal), chlamydia (pharyngeal, urethral, or rectal), or syphilis;
MSM who reported a diagnosis of rectal gonorrhea or syphilis, use of methamphetamine or poppers, or history of exchange sex in the prior 12 months, and those in ongoing sexual relationships with HIV-positive male partners who are not on ART, on ART <6 months, or not virologically suppressed;
MSM who do not meet criteria for recommending PrEP and who reported CAS with a partner who is not main/primary, CAS with an HIV-positive or unknown status partner, diagnosis of urethral gonorrhea or rectal chlamydia, or injection drug use in the past 12 months, and those in ongoing sexual relationships with HIV-positive male partners who have been on ART ≥6 months and who are virologically suppressed.
Awareness, interest, and use of PrEP
Eight in ten respondents (79%) had heard of PrEP, 19% reported current use, and 4% had used PrEP in the past (Table 2). By Washington State PrEP candidacy category, 31% of men for whom PrEP is recommended and 25% of those with whom it should be discussed reported current use, compared to only 4% of those for whom PrEP is not indicated. Among men in the “recommend” category, current PrEP use was reported by 37% in King County, 20% in other western Washington counties, and 22% in eastern Washington.
More than one third (36%) of men who had never used PrEP indicated that they wanted to start taking it, and 33% weren’t sure but wanted to learn more. Among never-users for whom PrEP is recommended, 56% wanted to start PrEP and 23% weren’t sure; among those with whom PrEP should be discussed, 51% wanted to start and 32% weren’t sure. Reported reasons for not using or not being interested in PrEP are presented in Figure 1, stratified by PrEP candidacy category and interest. Overall, the most common barriers to uptake among PrEP-naïve men for whom PrEP is recommended were a perception of being at low risk for HIV (29%), concern about side-effects (26%), and cost or insurance coverage issues (23%).
Figure 1: Reasons for not taking or not being interested in PrEP among PrEP-naïve MSM who meet local indications for PrEP being recommendeda (top panel) or discussedb (bottom panel), by reported interest in starting PrEP (N=373).
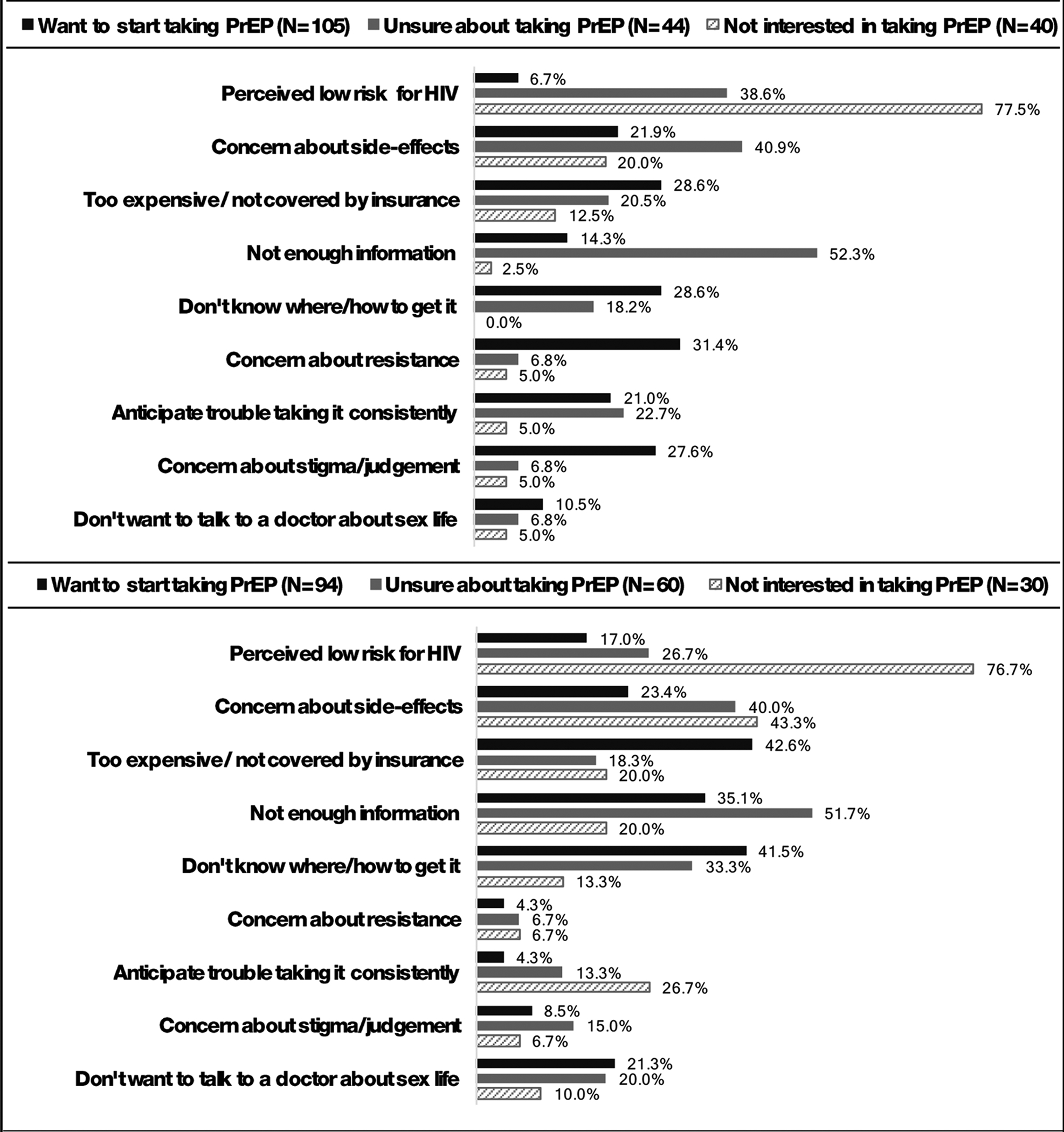
aMSM who reported a diagnosis of rectal gonorrhea or syphilis, use of methamphetamine or poppers, or history of exchange sex in the prior 12 months, and those in ongoing sexual relationships with HIV-positive male partners who are not on ART, on ART <6 months, or not virologically suppressed; bMSM who do not meet criteria for recommending PrEP and who reported CAS with a partner who is not main/primary, CAS with an HIV-positive or unknown status partner, diagnosis of urethral gonorrhea or rectal chlamydia, or injection drug use in the past 12 months, and those in ongoing sexual relationships with HIV-positive male partners who have been on ART ≥6 months and who are virologically suppressed.
Correlates of current PrEP use
In bivariate analyses, current PrEP use was associated with residence in King County, older age (relative to 18–24), identifying as gay or homosexual, higher education, higher income, and meeting criteria for PrEP being recommended or discussed (Table 3). In the base multivariable model adjusting for a priori covariates, only age, education, and PrEP candidacy remained significantly associated with current use. In a multivariable exploratory model, older age, having health insurance, diagnosis with rectal gonorrhea or syphilis, reporting ≥10 anal sex partners in the past 12 months, having a current HIV-positive male partner, CAS with a partner who was not main/primary or whose HIV status was positive or unknown, poppers use, and perceiving PrEP to be ≥90% effective were positively associated with current PrEP use.
Table 3:
Correlates of current PrEP use (N=850)a
| Using PrEP | Unadjusted associations | Adjusted associations | ||||||
|---|---|---|---|---|---|---|---|---|
| Base modelb | Exploratory modelc | |||||||
| n | % | OR (95% CI) | p-value | aOR (95% CI) | p-value | aOR (95% CI) | p-value | |
| A priori covariates | ||||||||
| Region of residence | <0.001 | 0.260 | 0.676 | |||||
| King County | 123 | 25.2% | Reference | Reference | Reference | |||
| Other western Washington | 32 | 13.4% | 0.46 (0.30, 0.70) | 0.67 (0.41, 1.09) | 0.80 (0.45, 1.44) | |||
| Eastern Washington | 18 | 14.5% | 0.50 (0.29, 0.86) | 0.82 (0.44, 1.53) | 1.13 (0.53, 2.42) | |||
| Age | <0.001 | <0.001 | 0.043 | |||||
| 16 to 24 | 18 | 7.2% | Reference | Reference | Reference | |||
| 25 to 34 | 70 | 25.4% | 4.36 (2.51, 7.57) | 3.97 (2.19, 7.18) | 2.99 (1.43, 6.25) | |||
| 35 to 44 | 44 | 33.1% | 6.34 (3.48, 11.57) | 5.23 (2.66, 10.27) | 3.09 (1.33, 7.23) | |||
| 45 to 54 | 29 | 28.7% | 5.17 (2.71, 9.85) | 4.17 (2.03, 8.57) | 3.34 (1.32, 8.41) | |||
| 55 and older | 12 | 13.2% | 1.95 (0.90, 4.23) | 2.06 (0.87, 4.88) | 2.31 (0.83, 6.41) | |||
| Race/ethnicity | 0.717 | 0.784 | 0.858 | |||||
| Non-Hispanic white | 125 | 21.3% | Reference | Reference | Reference | |||
| Hispanic | 26 | 17.4% | 0.78 (0.49, 1.25) | 0.76 (0.45, 1.29) | 0.96 (0.50, 1.84) | |||
| Non-Hispanic black | 7 | 21.9% | 1.03 (0.44, 2.45) | 0.86 (0.32, 2.33) | 0.60 (0.19, 1.91) | |||
| Non-Hispanic other | 15 | 18.3% | 0.83 (0.46, 1.50) | 0.95 (0.47, 1.90) | 0.98 (0.44, 2.17) | |||
| Gay/homosexual identity | 160 | 22.3% | 2.68 (1.47, 4.87) | 0.001 | 1.90 (0.96, 3.75) | 0.063 | 1.50 (0.67, 3.39) | 0.326 |
| Education | <0.001 | 0.002 | 0.126 | |||||
| High school or less | 7 | 5.2% | Reference | Reference | Reference | |||
| Some college/vocational school | 41 | 15.0% | 3.23 (1.41, 7.41) | 2.00 (0.82, 4.89) | 1.50 (0.52, 4.33) | |||
| 4-year college or higher | 125 | 28.3% | 7.21 (3.28, 15.86) | 3.66 (1.55, 8.66) | 2.34 (0.83, 6.55) | |||
| Income | <0.001 | 0.319 | 0.534 | |||||
| Less than $15,000 | 7 | 7.1% | Reference | Reference | Reference | |||
| $15,000 to $29,999 | 13 | 12.6% | 1.90 (0.72, 4.98) | 2.07 (0.73, 5.86) | 1.76 (0.53, 5.87) | |||
| $30,000 to $49,999 | 34 | 23.1% | 3.95 (1.68, 9.33) | 2.80 (1.09, 7.14) | 2.84 (0.98, 8.29) | |||
| $50,000 to $99,999 | 59 | 22.8% | 3.88 (1.71, 8.82) | 2.37 (0.96, 5.86) | 1.96 (0.68, 5.62) | |||
| $100,000 or more | 54 | 27.3% | 4.93 (2.15, 11.30) | 2.90 (1.13, 7.46) | 1.84 (0.62, 5.50) | |||
| I prefer not to answer | 6 | 13.6% | 2.08 (0.65, 6.58) | 1.94 (0.54, 7.01) | 1.77 (0.39, 8.12) | |||
| WA State PrEP guidelines category | <0.001 | <0.001 | ||||||
| Not indicated | 13 | 4.1% | Reference | Reference | ||||
| Discussd | 69 | 27.2% | 8.81 (4.74, 16.37) | 10.14 (5.31, 19.37) | ||||
| Recommende | 91 | 33.0% | 11.62 (6.32, 21.36) | 13.91 (7.35, 26.34) | ||||
| Exploratory covariates | ||||||||
| Has health insurance | 170 | 21.9% | 6.74 (2.10, 21.67) | 0.001 | 6.16 (1.57, 24.14) | 0.009 | ||
| Diagnosis with rectal gonorrhea or syphilis | 27 | 41.5% | 3.11 (1.84, 5.26) | <0.001 | 3.35 (1.49, 7.49) | 0.003 | ||
| Anal sex role | <0.001 | 0.364 | ||||||
| No anal sex | 1 | 1.0% | 0.03 (0.00, 0.24) | 0.28 (0.03, 2.33) | ||||
| Exclusively bottom | 20 | 12.1% | 0.41 (0.21, 0.78) | 0.74 (0.31, 1.74) | ||||
| Versatile | 127 | 25.9% | 1.04 (0.63, 1.70) | 1.13 (0.58, 2.20) | ||||
| Exclusively top | 25 | 25.3% | Reference | Reference | ||||
| ≥10 anal sex partners | 83 | 60.6% | 10.64 (7.08, 16.00) | <0.001 | 2.99 (1.73, 5.14) | <0.001 | ||
| Current HIV-positive male partner | 30 | 41.1% | 3.09 (1.88, 5.10) | <0.001 | 3.63 (1.52, 8.69) | 0.004 | ||
| CAS with a partner who was not main/primary or whose HIV status was positive or unknown | 153 | 33.8% | 9.61 (5.89, 15.69) | <0.001 | 4.78 (2.63, 8.70) | <0.001 | ||
| Injection drug use | 5 | 9.3% | 0.38 (0.15, 0.97) | 0.044 | 0.33 (0.09, 1.19) | 0.092 | ||
| Methamphetamine use | 10 | 13.5% | 0.59 (0.30, 1.17) | 0.130 | ||||
| Poppers use | 77 | 41.4% | 4.18 (2.91, 6.01) | <0.001 | 1.91 (1.17, 3.13) | 0.010 | ||
| History of exchange sex | 1 | 3.1% | 0.12 (0.02, 0.89) | 0.038 | 0.32 (0.03, 3.02) | 0.321 | ||
| Perceived effectiveness of PrEP ≥90% | 153 | 36.0% | 11.39 (6.97, 18.61) | <0.001 | 4.83 (2.62, 8.89) | <0.001 | ||
Acronyms: OR, odds ratio; CI, confidence interval; aOR, adjusted odds ratio; CAS, condomless anal sex; PrEP, pre-exposure prophylaxis
This analysis is restricted to respondents who have never or are currently using PrEP and provided responses to all covariates;
The base model includes only a priori covariates (region, age, education, race/ethnicity, sexual orientation, income, and PrEP candidacy based on Washington state guidelines);
The exploratory model includes base model social and demographic variables and exploratory variables that were significant in biviariate analyses. The Washington state PrEP guideline category variable was not included in the exploratory model because it is derived from the specific HIV risk indicators included as exploratory covariates;
MSM who do not meet criteria for recommending PrEP and who reported CAS with a partner who is not main/primary, CAS with an HIV-positive or unknown status partner, diagnosis of urethral gonorrhea or rectal chlamydia, or injection drug use in the past 12 months, and those in ongoing sexual relationships with HIV-positive male partners who have been on ART ≥6 months and who are virologically suppressed;
MSM who reported a diagnosis of rectal gonorrhea or syphilis, use of methamphetamine or poppers, or history of exchange sex in the prior 12 months, and those in ongoing sexual relationships with HIV-positive male partners who are not on ART, on ART <6 months, or not virologically suppressed.
PrEP adherence and discontinuation
Current PrEP users reported high adherence, with 93% having taken an average of 4 or more pills per week in the past 30 days and 66% reporting perfect adherence. Current users reported having started PrEP a median of 12 months prior to survey completion (interquartile range (IQR): 5–20), and past users reported a median of 5 months of use (IQR: 2–8.5). The most common reasons for stopping PrEP were a perception of no longer being at high risk for HIV (52%), concern about long-term health effects (27%), not being able to afford PrEP or having lost insurance (23%), and side-effects (20%). In a Kaplan-Meier analysis (Figure 2), we estimated that 20% of men discontinue PrEP within 12 months of initiation (95% CI: 15%-26%). Discontinuation was associated with having a high school education or lower (adjusted hazard ratio (aHR): 4.86, 95% CI: 1.77–13.38) or having completed some college or vocational school (aHR: 2.08, 95% CI: 1.02–4.25), relative to having a 4-year college degree or higher, but was not significantly associated with age, race/ethnicity, or region. Fifty-three percent of men who had discontinued PrEP wanted to start taking it again, and 28% were unsure about taking PrEP again.
Figure 2: Time to PrEP discontinuationa.
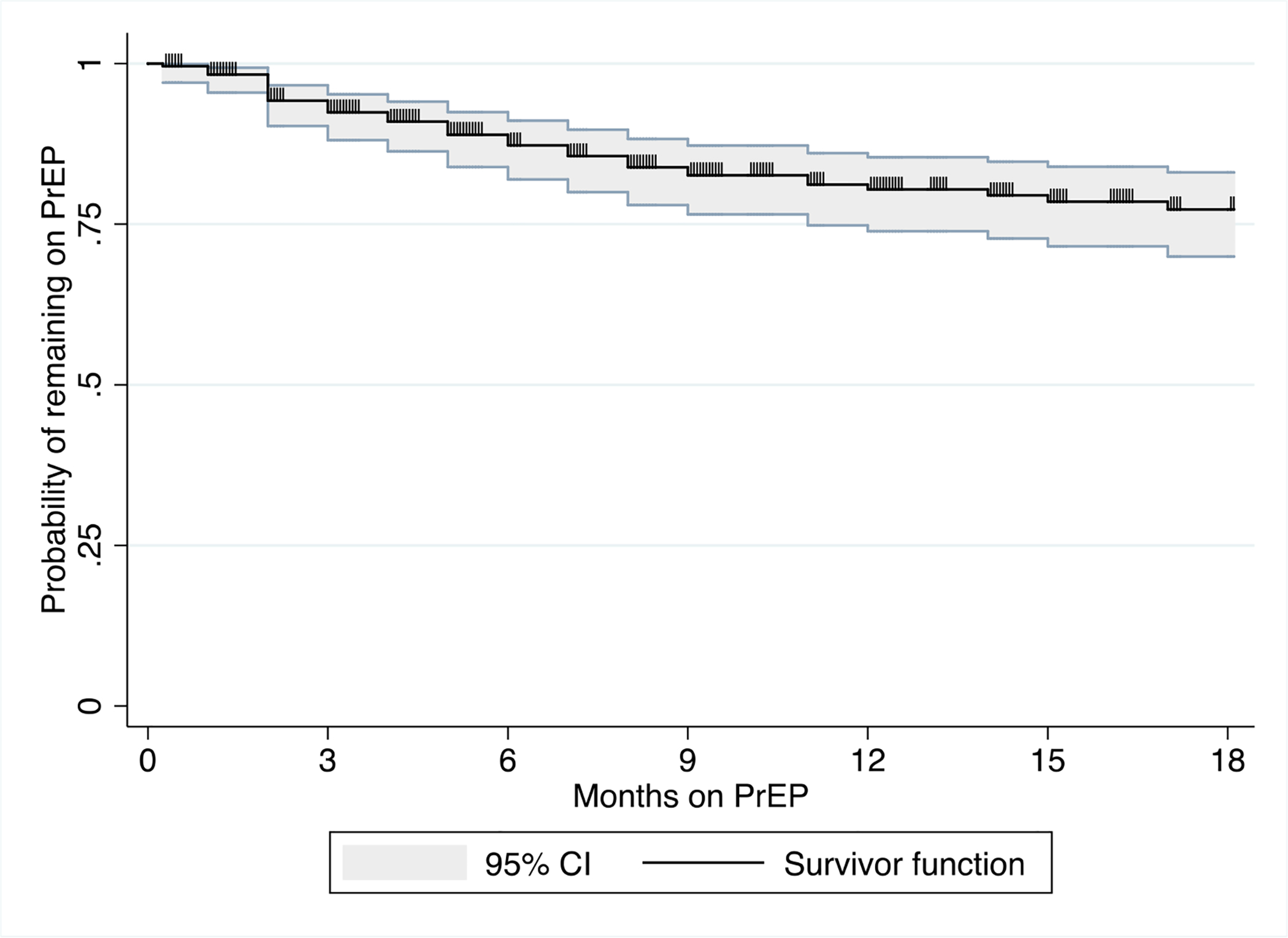
aIncludes data from 194 current and 44 past PrEP users who provided data on their dates of PrEP use. Tic marks indicate censoring times for current PrEP users. The graph is truncated at 18 months; 60 men reported having taken PrEP for 18 months or longer.
Comparison with the 2017 Seattle Pride Parade survey
Awareness of PrEP was similar among the 739 Seattle-area WHPP respondents (82%) and the sample of 297 HIV-negative cisgender MSM who completed the 2017 Seattle Pride Parade survey (86%; chi-square p=0.073). In both samples, 26% of men reported lifetime use of PrEP, with 21% of WHPP and 22% of Pride survey respondents reporting current use (p=0.853). A higher proportion of men in the WHPP sample reported behaviors indicating that PrEP should be recommended (33% vs. 19%; p<0.001). Among those in this high-risk category, 39% of WHPP respondents and 36% of Pride survey respondents reported lifetime use of PrEP (p=0.739), and 33% and 27% reported current use, respectively (p=0.398).
Discussion
In this sample of internet-recruited Washington State MSM, awareness and interest in PrEP were high, with more than half of high-risk men who had never used PrEP indicating that they wanted to start taking it. Current PrEP use was associated with sexual and drug-related HIV risk indicators in multivariable regression, and nearly one-third of men classified by state guidelines as having the strongest indication for PrEP reported current use. However, the gaps between reported interest and use of PrEP reveal substantial unmet need, and our analyses indicate sociodemographic disparities in uptake.
Previous surveys of MSM in the United States, conducted between 2014 and 2016, have reported 4%-10% current or past-12-month use of PrEP5,6,22 and 10%-15% lifetime use.23,24 Among higher risk men, these studies have found that 6%-13% report current or past-12-month use.5,6 The differences between these estimates and our findings are likely partially attributable to increased PrEP uptake in the years over which these data were collected. However, the 23%-26% lifetime and 19%-22% current use of PrEP reported by men in the WHPP and Seattle Pride survey samples suggest that PrEP use is higher in Washington State than in many other parts of the country.
Despite the high uptake of PrEP reported by men at high risk for HIV, many respondents reported barriers to PrEP initiation. Thirty percent of PrEP-naïve men who met indications for PrEP being recommended or discussed perceived themselves to be at low risk. Although Washington State guidelines may misclassify some individuals, our findings suggest a potential disconnect between perceived and actual risk. Among men recommended to initiate PrEP who wanted to start taking it, reported barriers suggest that many men face real or perceived financial barriers to PrEP, lack sufficient information about the intervention or how to receive it, or live somewhere where access is inadequate.
In particular, PrEP use was lower among younger, less educated, and uninsured men. Of note, we did not observe disparities in PrEP use by race/ethnicity, though our sample of black respondents was small. Some previous surveys of MSM have similarly reported no significant differences in PrEP use by race/ethnicity,5,23 but others have reported lower use among black and other minority MSM.6,24,25 In light of the high incidence of HIV among black and Hispanic MSM,26 concerted efforts are needed to ensure that PrEP reaches these at-risk populations.
We estimated that in our population, 20% of men who initiate PrEP will discontinue by 12 months. This estimate is similar to that derived from a cohort study of patients in northern California,27 but substantially lower than estimates from studies focusing on STD clinic patients and other high-risk populations.28,29 As in prior studies,23,28 the primary reasons for discontinuation reported by WHPP participants included no longer being at high risk, concern about long-term health effects, and financial barriers. While discontinuation may be indicated for some men, these findings point to a need for more consistent follow-up to encourage patients to discuss their concerns before discontinuing their medication. More than half of men who had discontinued PrEP expressed interest in starting it again, highlighting the need for clinicians and public health staff to serially discuss the intervention with men whose risks may be dynamic.
Our approach to PrEP monitoring has implications for diverse public health HIV programs. To inform implementation and evaluate the success of efforts to promote PrEP and other interventions, state and local health departments need to establish systems to monitor patterns of utilization and related behaviors at the population level. Alongside data from general population probability samples, event-based surveys, partner services interviews, and in-person surveys of high-risk groups (i.e., the National HIV Behavioral Surveillance System), internet-based surveys can be a valuable component of a comprehensive HIV surveillance strategy. Internet-based surveys have several advantages over other methods, particularly for recruitment of MSM: they can efficiently collect data over broad geographic areas; avoid linking PrEP monitoring to STI surveillance activities, which likely results in biased estimates since persons on PrEP are screened for asymptomatic STIs as part of their care; and are relatively inexpensive, at approximately $24 per completed response. Collaboration between public health and academic partners could facilitate expansion of internet-based public health monitoring to jurisdictions with limited time or expertise, a factor that was key to the success of this project.
Our findings have several limitations. First, our sample may not be representative of all Washington State MSM. As with other internet-based samples,13,14,30 WHPP participants were young, highly educated, and reported high engagement in HIV risk behaviors. The fact that the prevalence of PrEP use was similar in the WHPP and Pride samples lends credibility to the estimates, though the representativeness of the Pride survey sample is also uncertain. Second, the relative anonymity afforded to participants in online surveys makes it difficult to verify their eligibility and prevent duplicate responses. Through monitoring of IP addresses, time stamps, and response patterns, we detected 851 apparently invalid entries, but this approach is not foolproof. Third, our analyses of time to PrEP discontinuation assumed uninformative censoring (i.e. that current and past PrEP users were comparably likely to complete the survey), and used data on dates of PrEP use during a period of increasing awareness and uptake. These data may not be generalizable to men starting PrEP now or in the future. Additionally, our estimates of time to discontinuation might overestimate the duration of PrEP use, since our cross-sectional design may be more likely to collect data on longer periods of PrEP use among respondents who have gone on and off PrEP multiple times (length time bias).
The 2017 WHPP survey suggests high use of PrEP among MSM in Washington State, particularly among those at highest risk for HIV. Despite this success, there is substantial unmet need for PrEP; many men – particularly young, less educated MSM – require additional information or assistance to access PrEP, and our region has not yet achieved our defined 2020 objective of 50% PrEP use among MSM at highest risk.16 Our experience indicates that internet-based monitoring to measure PrEP utilization is feasible, relatively low cost, and allows for collection of statewide data which may not otherwise be available. Particularly if they are repeated at regular intervals, the data such surveys generate can play a critical role in monitoring the uptake of public health interventions over time and in identifying populations with disproportionate unmet need.
Supplementary Material
Supplemental Digital Content 1. Appendix with additional details on survey methodology and response rates.pdf
Supplemental Digital Content 2. Text that presents the survey measures of reasons for not using, not being interested in, or stopping PrEP.pdf
Supplemental Digital Content 3. Figure that shows a map indicating the regions of Washington State defined for analyses.pdf
Acknowledgements
This work was funded by the University of Washington STD/AIDS Research Training Program (NIH T32 AI07140) and the Washington State Department of Health. With the Washington State Department of Health, Tom Jaenicke and Elizabeth Crutsinger-Perry provided management and contract support, and April Gilreath and Lori Delaney helped translate survey materials into Spanish. Tanya Avoundjian contributed to the design of survey advertisements, and the University of Washington / Fred Hutch Center for AIDS Research Community Action Board (funded by P30 AI27757) provided feedback on advertisement design. Thanks to Patrick Sullivan, Jeremy Grey, Nicole Luisi, Travis Sanchez, Maria Zlotorzynska, Eric Hall, and Adam Vaughan of PRISM Health at the Emory University Rollins School of Public Health for their technical support, whose contributions were partly supported by grants 1R01DA038196 and 5P30AI050409, the Emory Center for AIDS Research. We would also like to thank the participants who took the time to complete this survey.
Sources of Funding: This work was funded by the University of Washington STD/AIDS Research Training Program (NIH T32 AI07140) and the Washington State Department of Health.
Footnotes
Conflict of Interest: MRG receives research support from Hologic and has consulted for GSK. All other authors declare that they have no conflict of interest.
References
- 1.White House Office of National AIDS Policy. National HIV/AIDS Strategy for the United States: Updated to 2020. Washington, DC: The White House, 2015. Available at: https://www.aids.gov/federal-resources/national-hiv-aids-strategy/nhas-update.pdf [Google Scholar]
- 2.Riddell J Iv, Amico K, et al. HIV preexposure prophylaxis: A review. Jama 2018;319(12):1261–8. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention. HIV Surveillance Report, 2016. 2017. November 2017 Report No. Available at: http://www.cdc.gov/hiv/library/reports/hiv-surveillance.html
- 4.US Public Health Service. Preexposure Prophylaxis for the Prevention of HIV Infection in the United States - 2014: A Clinical Practice Guideline. Department of Health and Human Services and Centers for Disease Control and Prevention, 2014. Available at: http://www.cdc.gov/hiv/pdf/PrEPguidelines2014.pdf [Google Scholar]
- 5.Parsons JT, Rendina HJ, Lassiter JM, et al. Uptake of HIV Pre-Exposure Prophylaxis (PrEP) in a National Cohort of Gay and Bisexual Men in the United States. J Acquir Immune Defic Syndr 2017;74(3):285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hoots BE, Finlayson T, Nerlander L, et al. Willingness to Take, Use of, and Indications for Pre-Exposure Prophylaxis among Men Who Have Sex with Men - 20 U.S. Cities, 2014. Clin Infect Dis 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan PA, Glynn TR, Oldenburg CE, et al. Implementation of Preexposure Prophylaxis for Human Immunodeficiency Virus Prevention Among Men Who Have Sex With Men at a New England Sexually Transmitted Diseases Clinic. Sex Transm Dis 2016;43(11):717–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Helms DJ, Weinstock HS, Mahle KC, et al. HIV testing frequency among men who have sex with men attending sexually transmitted disease clinics: implications for HIV prevention and surveillance. J Acquir Immune Defic Syndr 2009;50(3):320–6. [DOI] [PubMed] [Google Scholar]
- 9.Wejnert C, Raymond HF, Robbins T, et al. Achieving Greater HIV Prevention Impact Through CDC’s National HIV Behavioral Surveillance System. J Acquir Immune Defic Syndr 2017;75 Suppl 3:S249–s52. [DOI] [PubMed] [Google Scholar]
- 10.Hood JE, Buskin SE, Dombrowski JC, et al. Dramatic increase in preexposure prophylaxis use among MSM in Washington state. Aids 2016;30(3):515–9. [DOI] [PubMed] [Google Scholar]
- 11.Grov C, Breslow AS, Newcomb ME, et al. Gay and bisexual men’s use of the Internet: research from the 1990s through 2013. J Sex Res 2014;51(4):390–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sanchez T, Smith A, Denson D, et al. Developing a Web-Based HIV Behavioral Surveillance Pilot Project Among Men Who Have Sex with Men. Open AIDS J 2012;6:224–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stack C, Oldenburg C, Mimiaga M, et al. Sexual Behavior Patterns and PrEP Dosing Preferences in a Large Sample of North American Men Who Have Sex With Men. J Acquir Immune Defic Syndr 2016;71(1):94–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holloway I, Dougherty R, Gildner J, et al. PrEP Uptake, Adherence, and Discontinuation among California YMSM Using Geosocial Networking Applications. J Acquir Immune Defic Syndr 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sanchez TH, Zlotorzynska M, Sineath RC, et al. National Trends in Sexual Behavior, Substance Use and HIV Testing Among United States Men Who have Sex with Men Recruited Online, 2013 Through 2017. AIDS Behav 2018. [DOI] [PubMed] [Google Scholar]
- 16.HIV/AIDS Epidemiology Unit, Public Health – Seattle & King County, Infectious Disease Assessment Unit, Washington State Department of Health. HIV/AIDS Epidemiology Report 2017. 2017. Available at: http://www.kingcounty.gov/depts/health/communicable-diseases/hiv-std/patients/epidemiology/annual-reports.aspx [Google Scholar]
- 17.Anderson PL, Glidden DV, Liu A, et al. Emtricitabine-tenofovir concentrations and pre-exposure prophylaxis efficacy in men who have sex with men. Sci Transl Med 2012;4(151):151ra25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Golden MR, Lindquist S, Dombrowski JC. Public Health-Seattle & King County and Washington State Department of Health Preexposure Prophylaxis Implementation Guidelines, 2015. Sex Transm Dis 2016;43(4):264–5. [DOI] [PubMed] [Google Scholar]
- 19.Marrazzo JM, del Rio C, Holtgrave DR, et al. HIV prevention in clinical care settings: 2014 recommendations of the International Antiviral Society–USA panel. Jama 2014;312(4):390–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Guildeline on When to Start Antiretroviral Therapy and on Pre-Exposure Prophylaxis for HIV. Geneva, Switzerland: World Health Organization, 2015. Available at: http://www.who.int/hiv/pub/guidelines/earlyrelease-arv/en/ [PubMed] [Google Scholar]
- 21.Grey JA, Konstan J, Iantaffi A, et al. An updated protocol to detect invalid entries in an online survey of men who have sex with men (MSM): how do valid and invalid submissions compare? AIDS Behav 2015;19(10):1928–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen YH, Snowden JM, McFarland W, et al. Pre-exposure Prophylaxis (PrEP) Use, Seroadaptation, and Sexual Behavior Among Men Who Have Sex with Men, San Francisco, 2004–2014. AIDS Behav 2016. [DOI] [PubMed] [Google Scholar]
- 23.Holloway IW, Dougherty R, Gildner J, et al. Brief Report: PrEP Uptake, Adherence, and Discontinuation Among California YMSM Using Geosocial Networking Applications. J Acquir Immune Defic Syndr 2017;74(1):15–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mayer KH, Biello KB, Novak D, et al. PrEP uptake disparities in a diverse on-line sample of US men who have sex with men. Conference on Retroviruses and Opportunistic Infections; February 13–16, 2017; Seattle, Washington 2017. [Google Scholar]
- 25.Katz DA, Dombrowksi JC, Bell T, et al. STD partner services to monitor and promote PrEP use among men who have sex with men. Conference on Retroviruses and Opportunistic Infections; February 13–16, 2017; Seattle, WA 2017. [Google Scholar]
- 26.Singh S, Song R, Johnson A, et al. HIV incidence, HIV prevalence, and undiagnosed HIV infections in men who have sex with men, United States. Ann Intern Med 2018. [DOI] [PubMed] [Google Scholar]
- 27.Marcus JL, Hurley LB, Hare CB, et al. Preexposure prophylaxis for HIV prevention in a large integrated healthcare system: adherence, renal safety, and discontinuation. J Acquir Immune Defic Syndr 2016;73(5):540–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chan PA, Mena L, Patel R, et al. Retention in care outcomes for HIV pre-exposure prophylaxis implementation programmes among men who have sex with men in three US cities. J Int AIDS Soc 2016;19(1):20903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dombrowski JC, Golden MR, Barbee LA, et al. Patient Disengagement from an HIV Pre-Exposure Prophylaxis Program in a Sexually Transmitted Disease Clinic. Sex Transm Dis 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Sanchez T, Smith A, Denson D, et al. Internet-based methods may reach higher-risk men who have sex with men not reached through venue-based sampling. Open AIDS J 2012;6:83–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content 1. Appendix with additional details on survey methodology and response rates.pdf
Supplemental Digital Content 2. Text that presents the survey measures of reasons for not using, not being interested in, or stopping PrEP.pdf
Supplemental Digital Content 3. Figure that shows a map indicating the regions of Washington State defined for analyses.pdf


