Abstract
Objective:
The objective of this study was to evaluate the long-term predictive value of the Danish Whiplash Group Risk Assessment Score (DWGRAS) with 7 risk strata.
Design:
E-questionnaire-based follow-up study (n=927) combining 2 cohorts of whiplash-injured patients, 1 observational (n=187) and 1 interventional randomized controlled trial (n=740).
Methods:
Nine hundred twenty-seven previously healthy persons exposed to acute whiplash injury during motor vehicle collision were sent letter by postal service asking the addressee if they would respond to an E-questionnaire. Outcome measures were: whiplash-related disability, pain, use of medication/nonmedical treatment, work capacity.
Results:
The response rate was 37%. Fifty-five percent reported whiplash-related disability. Fourteen percent reported daily symptoms. A strong relationship was found between risk strata and impact of event and between risk strata and disabling symptoms.
Conclusions:
Internal and long-term validation of DWGRAS was performed, but a low response rate indicates that results should be interpreted with caution. Furthermore, external validation needs to be done in long-term studies. An receiver operating characteristics curve of 0.73 (95% confidence interval 0.67; 0.79) predicting daily or weekly whiplash-related disability after 12 to 14 years was found using the DWGRAS risk score.
Key Words: prospective study, whiplash injuries, headache, neck pain, work disability
It is estimated that ∼50% of persons sustaining a whiplash injury will continue to report persistent symptoms and present with persistent signs.1,2 There is a need for better identification of the factors predicting the outcome to plan future interventional studies and to improve the treatment after whiplash injury. So far, grading systems used in whiplash injuries have not been successful.3–5 One reason may be the complexity of an apparently mild neck injury and the multifaceted appearance of the so-called whiplash syndrome6,7 with a range of biological, psychological, and social factors involved. In whiplash injuries, there is a lack of information about the combined effect of biological, psychological, and social factors for long-term prognosis.
We have previously developed and validated8,9 a risk assessment score: The Danish Whiplash Group Risk Assessment Score (DWGRAS) and the 7 derived Risk Strata have shown a capability of predicting a 1-year pain disability and work disability. DWGRAS was reported to reflect biological factors, including a 1-year development in neck strength and endurance10 using a control group sustaining an acute ankle injury, and to reflect changes in pain response. Neck disability, using the Copenhagen Disability Functioning Scale,11 was correlated to the DWGRAS Score.
DWGRAS has been used to reflect differences in social performance including factors related to work, for example, predicting a 1-year work disability8 and also the changes in daily life functioning.12 From a psychological point of view, factors like impact of event, intrusion and avoidance related to cognitive psychological impact of the exposure to whiplash injury, are significantly different after 1 year in risk strata derived from the DWGRAS score.8
The Quebec Task Force Grading system is considered the gold standard for describing whiplash patients and was introduced by the Quebec Task Force in 1995,5 but has not been helpful in predicting long-term pain and disability after whiplash injuries.3 One reason could be an underlying biologically oriented explanation of the traumatic event.
Recently, Sterling and colleagues have developed a clinical prediction rule, which included: initial neck disability index, initial neck pain (visual analogue scale), cold pain threshold, range of neck movement, age, sex, presence of headache, and posttraumatic stress symptoms. Hyperarousal and hypervigilance have been of particular interest.13,14 This prediction rule is similar to the DWGRAS score. Long-term observations have not been reported, but external validation studies have been published.13 A +15-year follow-up on whiplash injury was published by Squires and colleagues.15,16 The initial group was heterogeneous, not followed up from early after injury, and more severely affected in comparison to other cohorts. A Norwegian study17,18 reported nonpainful symptoms, depression, and anxiety in the HUNT 1 and II studies in persons, who in questionnaires claimed to be experiencing whiplash injury. However, otherwise injuries were not documented early after injury. A recent cross-sectional survey of 12,000 persons of either between 40 and 42 years of age or between 60 and 62 years of age (The 6th Tromsø Study) found chronic pain in almost one-third of the participants. Four percent related their chronic pain to whiplash injury. But, in general there is a lack of knowledge regarding the roles of biological, psychological, and social risk factors for the long-term prognosis after a whiplash injury.17 Grading systems that are easy to use are needed early after whiplash injury. The grading system should possess a long-term predictive value and high internal and external validity.
The aim of this study was to examine the long-term capacity of the DWGRAS risk score for predicting whiplash-related disability, and painful and nonpainful symptoms and the use of medication and nonmedical treatment based on initial risk stratification.
HYPOTHESIS
The DWGRAS risk score and DWGRAS risk strata predict long-term whiplash-related disability, pain, nonpainful symptoms, and psychological cognitive problems.
MATERIALS AND METHODS
Participants in this prospective follow-up study were included from 2 previously conducted 1-year prospective studies on acute whiplash injury.19–23 The DWGRAS classification was derived from these 2 studies.8,9
Study 1 was an observational prospective study of consecutively included (n=187) acute whiplash patients during 1997-1999 with an age-matched and sex-matched control group of 40 patients exposed to an ankle sprain. The patients were all recruited from the hospital units in Aarhus County covering a population of ∼400,000 inhabitants. All patients were seen and examined within 10 days after injury by the same researcher (H.K.).19,20
Study 2 was planned based on study 1, and used the same methods for examining the main parameters from study 1. Study 2 was designed as a multicenter interventional, randomized control study with 3 treatment arms for high-risk whiplash patients and 2 treatment arms for low-risk patients (n=740 acute whiplash patients during 2002-2004). No ankle-injured control group or healthy control group was used in this study. This study covered several counties, and a population of 2.5 million inhabitants. A study nurse and a study physiotherapist located at the 2 centers contacted the hospital units to recruit eligible participants for the study. In study 2 the first examination took place within 10 days after injury.
Inclusion criteria were: whiplash injury due to rear-end car collision in study 1 (rear-end or frontal collision in study 2), preservation of consciousness during the time of collision, no direct head trauma, and no sign of amnesia or concussion, contact with the unit within 2 days after injury presenting with injury-related symptoms, and range of age between 18 and 70 years. Participants in both studies fulfilled criteria for whiplash associated disorders (WAD) grades from I to III. Exclusion criteria were previous severe neck or back disorder, known wide-spread pain or fibromyalgia, previous severe headaches including severe migraines, previous head injuries, record of severe psychiatric disease, and alcohol or medical/substance abuse. The WAD grades 0 and IV were excluded21,23,24 (Fig. 1).
FIGURE 1.
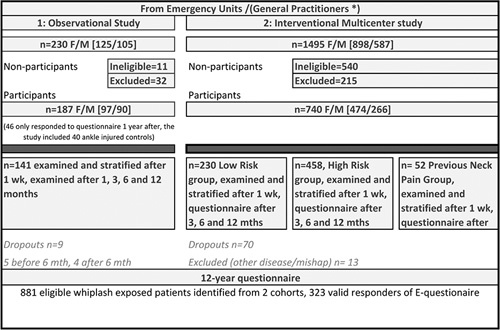
Flowchart of initial prospective whiplash studies and the prospective follow-up by E-questionnaire after 12 to 14 years. *Denotes referral from units in Study 1 and from units and GPs in Study 2. GPs indicates general practitioners.
In both studies all participants completed the patient reported questionnaires and underwent a physical neurological examination at median 5 days after exposure to a motor vehicle collision.19–21,24 The obtained 11-point numeric rating scale (NRS) pain scores, the number-of-nonpainful symptoms, and the total cervical range of motion25,26 were merged into an algorithm, which was used to calculate the individual risk scores. From an early point after injury all whiplash-exposed patients were divided into 7 risk strata8,9 (Table 1).
TABLE 1.
Danish Whiplash Group Risk Assessment Score Risk Score and Stratification (0-19 Points)
| Points | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (A) CROM | >280 | 261-280 | 241-260 | 221-240 | 200-220 | <200 | |||||||
| (B) Neck/head NRS-11 | 0-2 | 3-4 | 5-8 | 9-10 | |||||||||
| (C) No. nonpain symptoms | 3-5 | 6-11 | |||||||||||
| Stratum 1 | =0 points | (A) CROM measured as total score of cervical range of motion in 6 directions, neck flexion (during jaw retraction), neck extension, neck lateroflexion dxt/sin, and neck rotation dxt/sin | |||||||||||
| Stratum 2 | =1-3 points | ||||||||||||
| Stratum 3 | =4-6 points | ||||||||||||
| Stratum 4 Stratum 5 Stratum 6 Stratum 7 | =7-9 points =10-12 points =13-15 points =16-19 points | (B) Maximum value of the obtained NRS-11 score (0-10) of present neck pain and present headache (C) Sum of nonpainful symptoms related to injury | |||||||||||
CROM indicates cervcal range of motion; NRS, numeric rating scale.
The E-based questionnaire which was fulfilled after 12 to 14 years is shown in Table 2, including the Impact of Event Questionnaire (first version of IES is applied as in previous reports).27,28 The Impact of Event Questionnaire covered the impact of previous exposure to whiplash injury; also subscales on intrusion and avoidance related to the injury are covered by this measure. In this study, we did not use the revised IES questionnaire (IES-R) which also measures hyperarousal.29 For further details on the content of the E-Questionnaire refer to Table 2.
TABLE 2.
Content of E-questionnaire Posed 12 to 14 Years After Acute Whiplash Injury
| Do you currently experience health-related problems caused by the car mishap, you were exposed to? (yes/no) | |
| Do you often experience following nonpainful problems/symptoms after the car mishap? | A checklist of nonpainful symptoms/problems related to the car mishap with following options: no symptoms or yes, 1 or more of each of following symptoms: prickling/sleeping sensation, fatigue, sleep disorders, balance problems, hyperacusis, visual disturbances, anxiety/depression, irritability, dizziness, forgetfulness, concentration problems, nausea, globulus/dysphagia, jaw pain/ jaw disability, stiffness or reduced neck mobility, and finally, yes describe other problems (several choices available) |
| Do you experience pain after the car mishap? | NRS-11 average neck pain during the last week; NRS-11 average headache during the last week; NRS-11 average shoulder-arm pain during the last week; NRS-11 average low back pain during last week |
| Do you receive nonmedical treatment because of the previous car mishap today | Several choices, none; perform instructed neck exercises, chiropractic treatment, physiotherapy, acupuncture, yes other nonmedical treatment, describe other treatments |
| Do you receive medical treatment because of the car mishap today | Several choices, none, acetylsalicylic acid, acetaminophen, NSAIDs, tramadol, morphine or morphine-like drugs, migraine medication (eg, triptans, ergotalkaloids), epilepsy drugs (eg, gabapentin, pregabalin, topiramate), depression medication (eg, amitriptyline, nortriptyline, imipramine, mirtazapine, other), yes other medication, describe other medications |
| Have your employment status changed due to the mishap today | No change, yes changed function, but similar working hours due to mishap, yes, reduced working hours due to mishap, yes, I receive disability pension due to mishap, I was retired before mishap, Other change not related to whiplash mishap, describe |
| The Impact of Event Questionnaire | All questions regarding impact of the initial whiplash injury as event were posed |
NRS indicates numeric rating scale; NSAID, non-steroidal anti-inflammatory drugs.
Primary Outcome Measures at a 12-Year Follow-up
Presence of Whiplash Health Related Symptoms (WAD symptoms).5,30 Patients were asked, “Do you, as of today, experience problems due to the car-collision you were exposed to” (0: no, never; 1: yes, now and then, but less than once a week; 2: yes, regularly, once or more times during a week; 3: yes daily problems).
Secondary Outcome Parameters
The secondary outcome parameters were: neck pain intensity (NRS 0 to 10) due to previous whiplash injury; headache intensity (NRS 0 to 10) due to previous whiplash injury, posttraumatic stress reaction (Impact of Event Scale,27,28 15 questions rated from 0 to 5, range of total scores, from 0 to 45, with subscales of intrusion and avoidance) due to previous whiplash injuries. Furthermore, the frequency of nonpainful symptoms due to previous whiplash injury and the use of medication and nonmedical treatment due to previous whiplash injury. Actual work capacity was reported by the patient.
Ethics
Study 1 was approved by The Scientific Committee for Aarhus County, Project number 1996/3799. Study 2 was approved by The Scientific Committee for the counties of Vejle and Funen, project number 20000268. Patients gave consent to being contacted by the researcher/research team. Informed verbal and written consent was obtained for study participation. The 2 studies were conducted in accordance with the Helsinki II Declaration. This follow-up study was approved by The Regional Scientific Committee (The Region of Central Jutland, Denmark) project number 1-10-72-130-13.
Statistics
Nonparametric tests were applied. Kruskal-Wallis (KW) test was used for comparison of multiple samples (eg, 7 risk strata). Mann-Whitney U was applied comparing 2 samples of discrete variables. When reporting fractions (binomial distribution) proportions were given with exact 95% confidence intervals (CIs) as in Tables 3–6. P-values <0.05 were considered significant, and α=0.05 was set for type 1 error. Figures 3–5 are presented as mean values with a 95% CI; the statistics in the figures are based on KW test. The Dunn Pairwise Comparison was applied to test for and avoid mass-significance. Statistical Software package Stata/IC 15 (StataCorp LP, TX). χ2 statistics was applied to test for both the worst-case and the best-case scenarios of nonresponders (835 [eligible]-325 [responders]) having either no whiplash-related symptoms or whiplash-related symptoms similar to responders. TabOdds and receiver operating characteristics (ROC) curves were used to identify the predictive capacity of the risk score and stratification.
TABLE 3.
Initial Properties of Whiplash Patients Based on Stratification
| Participants in Primary Studies | Responders to Questionnaire-study at 12-14 y Follow-up | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Risk Strata | n | Sex Female/Male Ratio | Age at Injury (Mean±SD) | Initial Marital Status Married/Single/Other | Education Level at Injury | n | Sex Female/Male Ratio | Age (Mean±SD) | Marital status Married/Single/Other | Education White Collar |
| 1 | 105 | 0.48 (0.38, 0.58) | 35.86±11.17 | 0.74/0.18/0.08 (0.64, 0.81) (0.11, 0.29) (0.03, 0.18) | 0.57/0.43 (0.46, 0.66) (0.33, 0.54) | 49 | 0.49 (0.34, 0.64) | 34.63±10.25 | 0.71/0.22/0.07 (0.56, 0.82) (0.11, 0.41) (0.01, 0.32) | 0.52/0.48 (0.37, 0.67) (0.32, 0.64) |
| 2 | 281 | 0.59 (0.51, 0.63) | 34.65±11.17 | 0.73/0.18/0.10 (0.67, 0.77) (0.14, 0.23) (0.06, 0.14) | 0.52/0.48 (0.46, 0.58) (0.42, 0.54) | 103 | 0.64 (0.54, 0.73) | 34.14±11.22 | 0.70/0.19/0.11 (0.60, 0.77) (0.12, 0.30) (0.06, 0.22) | 0.46/0.54 (0.36, 0.56) (0.44, 0.64) |
| 3 | 138 | 0.62 (0.52, 0.69) | 35.12±11.92 | 0.74/0.17/0.09 (0.66, 0.81) (0.11, 0.26) (0.05, 0.17) | 0.60/0.40 (0.51, 0.68) (0.31, 0.49) | 57 | 0.59 (0.45, 0.71) | 37.31±11.66 | 0.78/0.17/0.05 (0.65, 0.86) (0.09, 0.33) (0.01, 0.26) | 0.56/0.44 (0.42, 0.69) (0.30, 0.58) |
| 4 | 120 | 0.68 (0.59, 0.76) | 34.10±10.54 | 0.60/0.24/0.16 (0.51, 0.69) (0.17, 0.34) (0.10, 0.25) | 0.51/0.49 (0.42, 0.61) (0.39, 0.58) | 38 | 0.74 (0.57, 0.85) | 34.62±10.79 | 0.54/0.27/0.19 (0.37, 0.70) (0.14, 0.48) (0.08, 0.41) | 0.46/0.54 (0.29, 0.64) (0.37, 0.70) |
| 5 | 75 | 0.65 (0.53, 0.75) | 37.69±12.31 | 0.59/0.28/0.13 (0.47, 0.69) (0.18, 0.41) (0.07, 0.27) | 0.54/0.46 (0.42, 0.66) (0.34, 0.58) | 23 | 0.78 (0.56, 0.90) | 37.69±10.98 | 0.70/0.26/0.04 (0.47, 0.85) (0.10, 0.55) (0.00, 0.78) | 0.43/0.57 (0.23, 0.67) (0.34, 0.76) |
| 6 | 98 | 0.76 (0.66, 0.83) | 32.95±10.76 | 0.72/0.18/0.10 (0.62, 0.80) (0.11, 0.29) (0.05, 0.20) | 0.70/0.30 (0.60, 0.78) (0.21, 0.41) | 36 | 0.81 (0.64, 0.90) | 33.67±10.10 | 0.78/0.17/0.06 (0.61, 0.88) (0.06, 0.40) (0.01, 0.42) | 0.69/0.31 (0.51, 0.82) (0.17, 0.52) |
| 7 | 62 | 0.66 (0.53, 0.77) | 36.50±11.75 | 0.75/0.19/0.06 (0.63, 0.84) (0.10, 0.34) (0.02, 0.24) | 0.70/0.30 (0.57, 0.80) (0.19, 0.45) | 15 | 0.53 (0.26, 0.78) | 38.03±13.00 | 0.73/0.13/0.13 (0.45, 0.89) (0.02, 0.66) (0.02, 0.66) | 0.73/0.27 (0.45, 0.89) (0.08, 0.64) |
| Total | 881 | 0.62 (0.59, 0.65) | 34.99±11.33 | 0.70/0.19/0.10 (0.66, 0.73) (0.17, 0.22) (0.08, 0.12) | 0.54/0.46 (0.50, 0.57) (0.42, 0.49) | 322 | 0.64 (0.58, 0.69) | 35.22±11.06 | 0.71/0.19/0.09(0.66, 0.75) (0.15, 0.24) (0.06, 0.14) | 0.50/0.50 (0.45, 0.56) (0.44, 0.55) |
TABLE 6.
Work Capacity 12 to 14 Years After Whiplash Injury in Risk Strata
| Stratum | n | No Change in Work Ability Due to Whiplash Injury | Change in Duties at Work or Less Hours Due to Whiplash Injury | Early Retirement (Disability Pension) Due to Whiplash Injury | Other Disease or Previously Retired |
|---|---|---|---|---|---|
| 1 | 49 | 0.92 (0.80, 0.98) | 0.04 (0.004, 0.03) | 0.02 (0.0005, 0.11) | 0.02 (0.0005, 0.11) |
| 2 | 103 | 0.92 (0.85, 0.97) | 0.08 (0.03, 0.15) | 0.00 (0.0, 0.04) | 0.00 (0.0, 0.04) |
| 3 | 60 | 0.78 (0.65, 0.88) | 0.10 (0.04, 0.21) | 0.07 (0.02, 0.16) | 0.10 (0.04, 0.21) |
| 4 | 38 | 0.61 (0.43, 0.76) | 0.29 (0.15, 0.46) | 0.078 (0.02, 0.21) | 0.026 (0.0005, 0.11) |
| 5 | 23 | 0.57 (0.34, 0.77) | 0.30 (0.13, 0.53) | 0.09 (0.01, 0.28) | 0.04 (0.001, 0.22) |
| 6 | 36 | 0.53 (0.35, 0.70) | 0.36 (0.21, 0.54) | 0.11 (0.03, 0.26) | 0.00 (0.0, 0.097) |
| 7 | 15 | 0.53 (0.27, 0.79) | 0.33 (0.12, 0.61) | 0.14 (0.02, 0.40) | 0.00 (0.0, 0.22) |
| Total | 324 | 0.77 (0.72, 0.82) | 0.16 (0.12, 0.21) | 0.049 (0.028, 0.079) | 0.019 (0.007, 0.039) |
Data presented as frequencies with 95% confidence intervals (binomial exact) in brackets.
FIGURE 3.
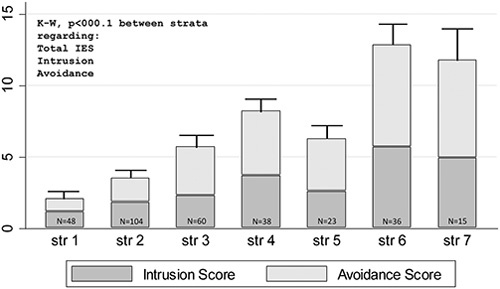
Impact of event score, total, intrusion, and avoidance in risk strata from the Danish Whiplash Group Risk Assessment Score after 12 to 14 years (mean±SEM).
FIGURE 5.
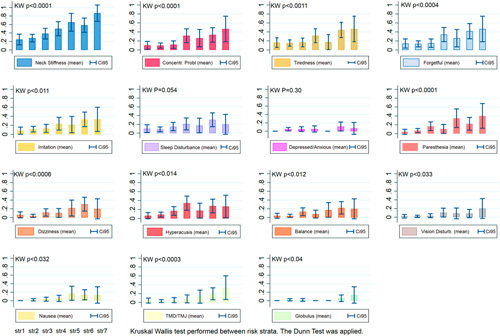
Nonpainful symptoms in risk strata from the Danish Whiplash Group Risk Assessment Score after 12 to 14 years (mean±SEM). CI indicates confidence interval.
TABLE 5.
Nonmedical Treatment in Risk Strata After 12 to 14 Years
| Risk Strata | No Nonpharmacological Treatment | Active Neck Exercise | Chiropractor | Physiotherapy | Acupuncture |
|---|---|---|---|---|---|
| 1 | 0.79 (0.65, 0.88) | 0.10 (0.03, 0.31) | 0.06 (0.01, 0.30) | 0.10 (0.03, 0.31) | 0.02 (0.00, 0.63) |
| 2 | 0.75 (0.66, 0.82) | 0.18 (0.11, 0.29) | 0.12 (0.06, 0.22) | 0.10 (0.05, 0.20) | 0.07 (0.03, 0.17) |
| 3 | 0.62 (0.48, 0.73) | 0.18 (0.10, 0.34) | 0.07 (0.02, 0.25) | 0.15 (0.07, 0.31) | 0.08 (0.03, 0.26) |
| 4 | 0.55 (0.38, 0.71) | 0.21 (0.10, 0.42) | 0.05 (0.01, 0.41) | 0.21 (0.10, 0.42) | 0.03 (0.00, 0.68) |
| 5 | 0.48 (0.27, 0.70) | 0.35 (0.16, 0.61) | 0.26 (0.10, 0.55) | 0.35 (0.16, 0.61) | 0.13 (0.03, 0.50) |
| 6 | 0.58 (0.41, 0.74) | 0.25 (0.12, 0.46) | 0.11 (0.03, 0.37) | 0.22 (0.10, 0.44) | 0.22 (0.10, 0.44) |
| 7 | 0.47 (0.21, 0.74) | 0.33 (0.12, 0.67) | 0.00 (0.00, 0.22) | 0.27 (0.08, 0.64) | 0.27 (0.08, 0.64) |
| Total | 0.66 (0.60, 0.71) | 0.2 (0.16, 0.25) | 0.10 (0.07, 0.13) | 0.16 (0.12, 0.20) | 0.09 (0.06, 0.12) |
| * | NS | NS | * | † |
Data presented as frequencies with 95% confidence intervals (binomial exact) in brackets.
NS indicates nonsignificant.
K-W: *P<0.05.
†P<0.01.
RESULTS
A total of 325 (36.9%) eligible participants completed the online questionnaire (Fig. 1). A minor proportion had died after we had checked the national register, some had moved and were living abroad; furthermore, return-to-sender letters with unknown address were abundant, and a majority did receive the letter of invitation by postal service but did not follow the link submitted. It was possible for participants to ask for a mailed questionnaire if internet access was not available and a few participants replied by letter.
Table 3 provides the distribution of sex, age-at-injury, initial marital status, and the initial educational level for each of the 7 risk strata, and for the whole group. The distribution is outlined for the original cohort and for the subgroup of responders to the 12 to 14 years follow-up E-questionnaires.
The responders did not differ from nonresponders regarding sex, initial age, initial marital status ([formally] married or common law[-married]/single/other).
The initial educational level (low/moderate/high) was a predictor for willingness to participate (KW, P<0.02), and to a larger degree the well- educated from the original cohort responded to the E-based questionnaire. The distribution of strata was slightly skewed, showing more responders confined to stratum 1 (low risk) and fewer than expected confined to stratum 7 (high risk) (KW, P<0.01). Number of participants in each stratum is reported for the 2 primary studies and for the 12-year follow-up of respondents in Table 1.
Main Outcome
Whiplash-related health disability was reported by 24.0% of the responders whose problems occurred less than once a week, and 16.3% of responders had problems once or on several occasions per week. Furthermore, 14.5% of the responders reported daily problems related to previous whiplash injury >12 years postinjury. More than 80% in stratum 7 complained of frequent health disability associated with previous whiplash injury (KW, P<0.01) (Fig. 2).
FIGURE 2.
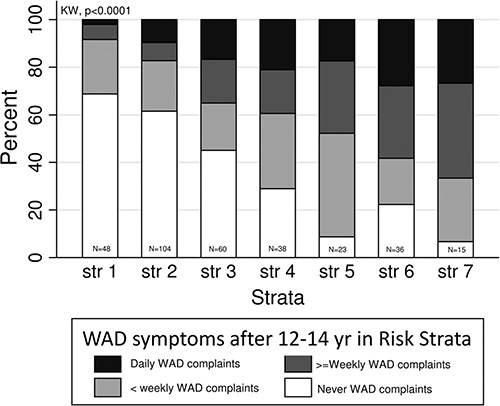
Whiplash-related symptoms after 12 to 14 in risk strata from Danish Whiplash Group Risk Assessment Score. Stacked bar.
In 45.2% of the responders, no health-related problems due to previous injury were reported. A best case post hoc analysis found 5.4% having daily WAD symptoms as opposed to 73.8% if nonresponders from the eligible cohort were regarded as being nonrecovered/having daily symptoms. A roctab analysis showed an ROC area of 0.73 (95% CI 0.67; 0.79) using the DWGRAS stratification to predict long-term daily and to predict weekly disability. If cutoff was set to predicting only daily WAD disability after 12 to 14 years, it was lowered to an ROC area of 0.68 (95% CI 0.60; 0.75).
Posttraumatic Stress
Results from the assessment of the Impact of Event Scale 12 years after whiplash injury are reported in Figure 3. For both the total IES score and score of the subscales (subscales: intrusion and avoidance) the burden of posttraumatic stress was greater in high-risk strata (KW, P<0.01, Fig. 3).
Pain Perception and Pain Distribution
The long-term report of present pain was confined to the head, neck, shoulder-arm, and low back as depicted in Figure 4, which showed a general burden of pain in both the low and the high-risk strata. As shown in Figure 4, in the higher stratum the more intense pain is reported in the different regions (KW, P<0.01).
FIGURE 4.
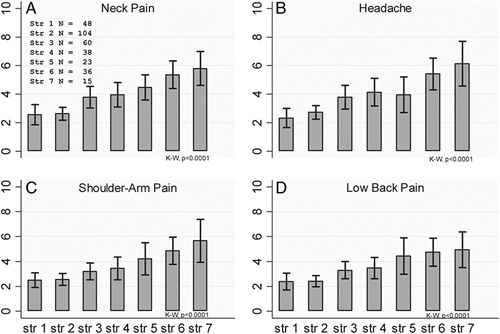
Reported pain (11-point numerical rating scale [mean±SEM]) due to previous whiplash injury in risk strata (str 1 to str 7) from the Danish Whiplash Group Risk Assessment Score after 12 to 14 years. A, Neck pain. B, Headache. C, Shoulder-arm pain. D, Low back pain.
Nonpainful Symptoms Revisited After 12 to 14 Years
Frequencies of the number of nonpainful symptoms were significantly raised in higher risk strata (KW, P<0.01) as shown in Figure 5.
In high-risk strata (strata 5 to 7) 25% to 45% of responders complained of cognitive difficulties, for example, concentration problems, forgetfulness, and fatigue. Paresthesia and hyperacusis were also commonly encountered as symptoms in the high-risk strata. Neck stiffness and reduced neck mobility was reported in >50% in risk strata 5, 6, and 7.
Use of Medication
The use of weak analgesics, acetaminophen, and non-steroidal anti-inflammatory drugs, but not acetylsalicylic acid was significantly more commonly used in the high-risk strata (KW, P<0.001) and the use of weak (P<0.05) and strong opioids (P<0.01) was more commonly prescribed in the high-risk strata (refer to Table 4).
TABLE 4.
Use of Medication 12 to 14 Years After Whiplash Injury in Risk Strata
| Weak Analgesics | Opioids | Prophylactic Medications | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Risk Strata | Acetylsalicylic Acid | Acetaminophen | NSAIDs | Weak Opioid | Strong Opioid | Triptans/Migraine | Anticonvulsants | Antidepressants | Other Medication |
| 1 | 0.07 (0.01, 0.31) | 0.07 (0.01, 0.31) | 0.04 (0.01, 0.36) | 0.00 (0.00, 0.08) | 0.00 (0.00, 0.08) | 0.00 (0.00, 0.08) | 0.00 (0.00, 0.08) | 0.00 (0.00, 0.08) | 0.02 (0.00, 0.64) |
| 2 | 0.03 (0.01, 0.16) | 0.15 (0.09, 0.26) | 0.08 (0.04, 0.19) | 0.01 (0.00, 0.43) | 0.01 (0.00, 0.43) | 0.04 (0.01, 0.16) | 0.01 (0.00, 0.43) | 0.02 (0.00, 0.20) | 0.02 (0.00, 0.20) |
| 3 | 0.00 (0.00, 0.06) | 0.24 (0.14, 0.39) | 0.1 (0.04, 0.27) | 0.05 (0.01, 0.26) | 0.00 (0.00, 0.06) | 0.02 (0.00, 0.58) | 0.00 (0.00, 0.06) | 0.05 (0.01, 0.26) | 0.00 (0.00, 0.06) |
| 4 | 0.00 (0.00, 0.09) | 0.39 (0.24, 0.58) | 0.26 (0.13, 0.47) | 0.05 (0.01, 0.41) | 0.08 (0.02, 0.36) | 0.08 (0.02, 0.36) | 0.00 (0.00, 0.09) | 0.00 (0.00, 0.09) | 0.05 (0.01, 0.41) |
| 5 | 0.00 (0.00, 0.15) | 0.43 (0.23, 0.67) | 0.35 (0.16, 0.61) | 0.13 (0.03, 0.50) | 0.13 (0.03, 0.50) | 0.00 (0.00, 0.15) | 0.04 (0.00, 0.78) | 0.00 (0.00, 0.15) | 0.04 (0.00, 0.78) |
| 6 | 0.00 (0.00, 0.10) | 0.44 (0.28, 0.63) | 0.25 (0.12, 0.46) | 0.06 (0.01, 0.42) | 0.08 (0.02, 0.37) | 0.11 (0.03, 0.37) | 0.00 (0.00, 0.10) | 0.06 (0.01, 0.42) | 0.03 (0.00, 0.69) |
| 7 | 0.07 (0.00, 0.85) | 0.33 (0.12, 0.67) | 0.47 (0.21, 0.74) | 0.13 (0.02, 0.66) | 0.13 (0.02, 0.66) | 0.07 (0.00, 0.85) | 0.07 (0.00, 0.85) | 0.00 (0.00, 0.22) | 0.07 (0.00, 0.85) |
| Total | 0.02 (0.009, 0.04) | 0.25 (0.20, 0.30) | 0.15 (0.12, 0.20) | 0.04 (0.02, 0.07) | 0.04 (0.02, 0.06) | 0.04 (0.02, 0.06) | 0.009 (0.002, 0.03) | 0.02 (0.009, 0.04) | 0.03 (0.01, 0.05) |
| NS | *** | *** | * | ** | NS | NS | NS | NS | |
Data presented as frequencies with 95% confidence intervals (binomial exact) in brackets.
NS indicates not statistically significant difference between strata; NSAID, non-steroidal anti-inflammatory drugs.
K-W: *P<0.05.
**P<0.01.
***P<0.001.
Use of Nonmedical Treatment After 12 to 14 Years
Nonpharmacological treatment was overall (KW, P<0.05) significantly more abundant in the high-risk groups, as more reported the use of physiotherapy (KW, P<0.05) and acupuncture (KW, P<0.01), but we did not encounter more extensive use of chiropractic treatment or use of active neck exercise 12 to 14 years after whiplash in high-risk strata.
Work Capacity After 12 to 14 Years
Ninety-two percent of responders from strata 1 and 2 had no change in work capacity as opposed to 53% to 57% in strata 5, 6, and 7. A significant difference in work capacity was observed between strata (KW, P<0.01).
Nineteen participants were older than 65 years of age when answering the questionnaire. In the remaining 304 participants now aged from 28.3 to 64.8 years of age, 25 patients reported between 1 and 14 days sick leave in the past year, 4 participants reported 15 to 30 days, and 3 participants from 31 to 90 days of sick leave, and 13 reported >3 months of sick leave due to disability related to previous whiplash injury.
DISCUSSION
The main finding of this long-term prospective study of previously whiplash-exposed patients is that the applied DWGRAS and the risk stratification to determine persons at risk within 5 days after whiplash injury were clinically meaningful in predicting long-term pain, the burden of nonpainful symptoms, the use of pain medication, and work absenteeism/changed work capacity. Fifty-five percent in this cohort report a series of symptoms they relate to a previous whiplash injury exposure 12 to 14 years ago, which is in accordance with other prospective studies.31 Fourteen percent reported daily WAD symptoms. However, only 37% of the initially examined cohort patients were available after 12 to 14 years for the follow-up. Neck stiffness was by far the most prominent symptom after 12 to 14 years. We found that active neck strength and endurance were severely affected 1 year after whiplash injury as compared with ankle sprain.10 The frequencies of cognitive symptoms (concentration problems, tiredness and forgetfulness, and irritation) were moderate, but more common in high-risk groups. Less commonly encountered symptoms were dizziness and balance problems. Nausea and vision disturbance, hyperacusis, jaw dysfunction, globulus/dysphagia, and paresthesia were almost only reported in the high-risk strata. Depression and anxiety were rarely reported and did not differ between strata in this study. We could therefore identify some common whiplash-associated main problems being stiffness of the neck and bodily pain mainly confined to the head and the neck. In the high-risk strata, however, we encountered a more multifaceted symptom complex,32 but with remarkably more neck stiffness and neck pain, and with more headache as well. The so-called concussion-related symptoms are more prone in nonrecovered whiplash patients as well, which we have previously reported.12
Posttraumatic stress seems to be important for long-term recovery in whiplash.33,34 Both intrusion and avoidance scores and total IES differed significantly between risk strata. However, IES scores were lowered after 12 to 14 years compared with values in risk strata from study 2 from after 3 months and 1 year.28 The present study applied the original Horowitz version of IES, but other researchers have applied the IES-R version by Weiss and Marmar in whiplash studies, and a correlation between pain and hyperarousal and hypervigilance has been reported.29,35,36 In this study, we did not include the subscale on hyperarousal, due to the lack of validated cutoff levels at the time of the study initiation.
In previous prospective whiplash studies, there has been reported time-dependent initial fluctuations using the IES score and the subscores of avoidance and intrusion. Also, our present findings should lead to a more cautious observation of both psychological, biological, and social factors.28,37
Strengths and Weaknesses of the Study
Previously, we made an internal validation of DWGRAS prediction capacities in the observational study with ROC curves of 0.87 (95% CI 0.75; 1.00) and of 0.78 (95% CI 0.73; 0.84) in the multicenter study when using the risk score after 1 week to predict 1-year work disability after a whiplash injury.8,9 External validation of the DWGRAS has to our knowledge not been performed or published. The recently developed clinical prediction rule by Ritchie et al13,14 has shown satisfactory results in an external validation study, but long-term results have not been published.
Bannister and Gordon reported follow-ups after 1, 7.5, and 15 years in their cohort. Fluctuations in recovery were seen.15,16,38 The Gargan Bannister Grades A-D (designated from 1 to 4 in some publications) were based on symptom severity from patient reports with positive correlation to the Neck Disability Index39; however, based on a sample of more severely affected whiplash-injured patients and unspecific inclusion and exclusion criteria. The Gargan Bannister grading is similar to a previously proposed patient reporting the based grading system by Parmer and Raymakers.40 In this study, an initial 1-year follow-up was followed by >10 years that we have not come across until this last E-questionnaire based follow-up. It is obviously a weakness that we could not obtain follow-up data for >37% of eligible cases. This raises the question if the responder group was representative for the entire group.
Therefore, data presented from this study should be interpreted cautiously. Similar arguments could be posed in the long-term follow-up studies from Norway, the HUNT studies with response rates of 51% after 10 years.18,41 It could be argued that a fluctuation in disability related to whiplash injury in the cohort represents a change in the perception and recognition of the whiplash injury at different timepoints in the general population, more than a change in the burden of the total of symptoms and disability as such.42,43 The participants of the present follow-up groups were similar to the original cohorts in terms of sex, age, and marital status but not with consideration of educational level, where a larger proportion of well-educated participants responded in this follow-up as compared with the original cohort. The present data are based on risk strata and without a corresponding control group after 12 to 14 years, thus specific causal conclusions about the role of risk factors cannot be drawn.
CONCLUSIONS
DWGRAS has long-term predictive value regarding the prediction of long-term whiplash-related disability, but long-term external validation of the grading system is needed. Precaution should be taken due to a significant loss to follow-up in the initial cohort. Nevertheless, the strong and consistent relationship between the a priori defined risk factors and the outcome with an ROC curve of 0.73 (95% CI 0.67; 0.79) predicting daily or weekly whiplash-associated disability after 12 to 14 years suggests that the present findings do reflect the risk for subsequent disability. DWGRAS can be easily performed in the unit or by the general practitioner if cervcal range of motion measurement equipment is available.
ACKNOWLEDGMENTS
The authors thank the units in Aarhus and the former counties of Viborg, Vejle, Funen, and Southern Jutland for participating in data collection. The authors would also like to thank other members of the DWGRAS group for their valuable contribution: Professor Flemming W. Bach, DMSc, Aarhus University Hospital and Department of Clinical Medicine Aarhus University, Denmark; Professor Emeritus Tom Bendix, DMSc, University of Copenhagen, Denmark and Associate Professor, Erisela Qerama, PhD, Department of Neurophysiology, Aarhus University Hospital, Denmark. The initial studies were funded by financial support received from the Danish Medical Research Council, the Danish Society of Polio and Accident Victims, the Danish Rheumatism Association, and an unrestricted grant from The Danish Insurance Association. The present paper was not externally funded.
Footnotes
The authors declare no conflict of interest.
REFERENCES
- 1.Carroll LJ, Hogg-Johnson S, Cote P, et al. Course and prognostic factors for neck pain in workers: results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33(suppl):S93–S100. [DOI] [PubMed] [Google Scholar]
- 2.Sterling M, Carroll LJ, Kasch H, et al. Prognosis after whiplash injury: where to from here? Discussion paper 4. Spine (Phila Pa 1976). 2011;36(suppl):S330–S334. [DOI] [PubMed] [Google Scholar]
- 3.Kivioja J, Jensen I, Lindgren U. Neither the WAD-classification nor the Quebec Task Force follow-up regimen seems to be important for the outcome after a whiplash injury. A prospective study on 186 consecutive patients. Eur Spine J. 2008;17:930–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kivioja J, Jensen I, Lindgren U. A prospective study on the Quebec Classification as a predictor for the outcome after whiplash injury. Proceedings from whiplash associated disorders. World Congress 99. Vancouver, Canada: Conference Proceedings; 1999.
- 5.Spitzer WO, Skovron ML, Salmi LR, et al. Scientific monograph of the Quebec Task Force on whiplash-associated disorders: redefining ‘whiplash’ and it’s management. Spine (Phila Pa 1976). 1995;20:1S–73S. [PubMed] [Google Scholar]
- 6.McLean SA, Ulirsch JC, Slade GD, et al. Incidence and predictors of neck and widespread pain after motor vehicle collision among US litigants and nonlitigants. Pain. 2014;155:309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kasch H, Turk DC, Jensen TS.Kasch H. Whiplash injury. Perspectives on the Development of Chronic Pain. Philadelphia: IASP Press; 2016. [Google Scholar]
- 8.Kasch H, Kongsted A, Qerama E, et al. A new stratified risk assessment tool for whiplash injuries developed from a prospective observational study. BMJ Open. 2013;3:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kasch H, Qerama E, Kongsted A, et al. The risk assessment score in acute whiplash injury predicts outcome and reflects biopsychosocial factors. Spine (Phila Pa 1976). 2011;36(suppl):S263–S267. [DOI] [PubMed] [Google Scholar]
- 10.Krogh S, Kasch H. Whiplash injury results in sustained impairments of cervical muscle function: a one-year prospective, controlled study. J Rehabil Med. 2018;50:548–555. [DOI] [PubMed] [Google Scholar]
- 11.Jordan A, Manniche C, Mosdal C, et al. The Copenhagen Neck Functional Disability Scale: a study of reliability and validity. J Manipulative Physiol Ther. 1998;21:520–527. [PubMed] [Google Scholar]
- 12.Kasch H, Jensen L. Minor head injury symptoms and recovery from whiplash injury: a 1-year prospective study. Rehab Process & Outcome. 2019;8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ritchie C, Hendrikz J, Jull G, et al. External validation of a clinical prediction rule to predict full recovery and ongoing moderate/severe disability following acute whiplash injury. J Orthop Sports Phys Ther. 2015;45:242–250. [DOI] [PubMed] [Google Scholar]
- 14.Ritchie C, Hendrikz J, Kenardy J, et al. Derivation of a clinical prediction rule to identify both chronic moderate/severe disability and full recovery following whiplash injury. Pain. 2013;154:2198–2206. [DOI] [PubMed] [Google Scholar]
- 15.Squires B, Gargan MF, Bannister GC. Soft-tissue injuries of the cervical spine 15 year follow up. J Bone Joint Surg. 1996;78B:955–957. [DOI] [PubMed] [Google Scholar]
- 16.Gargan MF, Bannister GC. The rate of recovery following whiplash injury. Eur Spine J. 1994;3:162–164. [DOI] [PubMed] [Google Scholar]
- 17.Myrtveit SM, Skogen JC, Petrie KJ, et al. Factors related to non-recovery from whiplash. The Nord-Trondelag Health Study (HUNT). Int J Behav Med. 2014;21:430–438. [DOI] [PubMed] [Google Scholar]
- 18.Myrtveit SM, Skogen JC, Wenzel HG, et al. Somatic symptoms beyond those generally associated with a whiplash injury are increased in self-reported chronic whiplash. A population-based cross sectional study: the Hordaland Health Study (HUSK). BMC Psychiatry. 2012;12:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kasch H, Bach FW, Jensen TS. Handicap after acute whiplash injury: a 1-year prospective study of risk factors. Neurology. 2001;56:1637–1643. [DOI] [PubMed] [Google Scholar]
- 20.Kasch H, Bach FW, Stengaard-Pedersen K, et al. Development in pain and neurologic complaints after whiplash: a 1-year prospective study. Neurology. 2003;60:743–749. [DOI] [PubMed] [Google Scholar]
- 21.Kongsted A, Qerama E, Kasch H, et al. Neck collar, “act-as-usual” or active mobilization for whiplash injury? A randomized parallel-group trial. Spine (Phila Pa 1976). 2007;32:618–626. [DOI] [PubMed] [Google Scholar]
- 22.Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, et al. Pain thresholds and tenderness in neck and head following acute whiplash injury: a prospective study. Cephalalgia. 2001;21:187–197. [DOI] [PubMed] [Google Scholar]
- 23.Kasch H, Qerama E, Kongsted A, et al. Clinical assessment of prognostic factors for long-term pain and handicap after whiplash injury: a 1-year prospective study. Eur J Neurol. 2008;15:1222–1230. [DOI] [PubMed] [Google Scholar]
- 24.Kongsted A, Qerama E, Kasch H, et al. Education of patients after whiplash injury: is oral advice any better than a pamphlet? Spine (Phila Pa 1976). 2008;33:E843–E848. [DOI] [PubMed] [Google Scholar]
- 25.Capuano-Pucci D, Rheault W, Aukai J, et al. Intratester and intertester reliability of the cervical range of motion device. Arch Phys Med Rehab. 1991;72:338–340. [PubMed] [Google Scholar]
- 26.Kasch H, Stengaard-Pedersen K, Arendt-Nielsen L, et al. Headache, neck pain, and neck mobility after acute whiplash injury: a prospective study. Spine (Phila Pa 1976). 2001;26:1246–1251. [DOI] [PubMed] [Google Scholar]
- 27.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41:209–218. [DOI] [PubMed] [Google Scholar]
- 28.Kongsted A, Bendix T, Qerama E, et al. Acute stress response and recovery after whiplash injuries. A one-year prospective study. Eur J Pain. 2008;12:455–463. [DOI] [PubMed] [Google Scholar]
- 29.Buitenhuis J, Jong PJD, Jaspers JPC, et al. Relationship between posttraumatic stress disorder symptoms an the course of whiplash complaints. J Psychosom Res. 2006;61:681–689. [DOI] [PubMed] [Google Scholar]
- 30.Sturzenegger M, DiStefano G, Radanov BP, et al. Presenting symptoms and signs after whiplash injury: the influence of accident mechanisms. Neurology. 1994;44:688–693. [DOI] [PubMed] [Google Scholar]
- 31.Carroll LJ, Holm LW, Hogg-Johnson S, et al. Course and prognostic factors for neck pain in whiplash-associated disorders (WAD): results of the Bone and Joint Decade 2000-2010 Task Force on Neck Pain and Its Associated Disorders. Spine (Phila Pa 1976). 2008;33(suppl):S83–S92. [DOI] [PubMed] [Google Scholar]
- 32.Gehrt TB, Wisbech Carstensen TB, Ornbol E, et al. The role of illness perceptions in predicting outcome after acute whiplash trauma: a multicenter 12-month follow-up study. Clin J Pain. 2015;31:14–20. [DOI] [PubMed] [Google Scholar]
- 33.Dikmen S, Machamer J, Temkin N. Mild head injury: facts and artifacts. J Clin Exp Neuropsychol. 2001;23:729–738. [DOI] [PubMed] [Google Scholar]
- 34.Dikmen S, McLean A, Temkin N. Neuropsychological and psychosocial consequenses of minor head injury. J Neurol Neurosurg Psychiatry. 1986;49:1227–1232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buitenhuis J, Jaspers JP, Fidler V. Can kinesiophobia predict the duration of neck symptoms in acute whiplash? Clin J Pain. 2006;22:272–277. [DOI] [PubMed] [Google Scholar]
- 36.Sterling M, Kenardy J, Jull G, et al. The development of psychological changes following whiplash injury. Pain. 2003;106:481–489. [DOI] [PubMed] [Google Scholar]
- 37.Sterling M. Physical and psychological aspects of whiplash: important considerations for primary care assessment, part 2—case studies. Man Ther. 2009;14:e8–e12. [DOI] [PubMed] [Google Scholar]
- 38.Tomlinson PJ, Gargan MF, Bannister GC. The fluctuation in recovery following whiplash injury 7.5-year prospective review. Injury. 2005;36:758–761. [DOI] [PubMed] [Google Scholar]
- 39.Lankester BJA, Garneti N, Bannister GC. The classification of outcome following whiplash injury—a comparison of methods. Eur Spine J. 2004;13:605–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parmer HV, Raymakers R. Neck injuries from rear impact road traffic accidents: prognosis in persons seeking compensation. Injury. 1997;24:75–78. [DOI] [PubMed] [Google Scholar]
- 41.Myrtveit SM, Wilhelmsen I, Petrie KJ, et al. What characterizes individuals developing chronic whiplash?: The Nord-Trondelag Health Study (HUNT). J Psychosom Res. 2013;74:393–400. [DOI] [PubMed] [Google Scholar]
- 42.Stovner LJ. The nosologic status of the whiplash syndrome: a critical review based on a methodological approach. Spine (Phila Pa 1976). 1996;21:2735–2746. [DOI] [PubMed] [Google Scholar]
- 43.Ferrari R, Kwan O, Russel AS, et al. The best approach to the problem of whiplash? One ticket to Lithuania, please. Clin Exp Rheum. 1999;17:321–326. [PubMed] [Google Scholar]


