Abstract
Malaria in the Amazon is often perceived as an exclusively rural disease, but transmission has been increasingly documented within and near urban centers. Here we explore patterns and causes of urban-to-rural mobility, which places travelers at risk of malaria in Mâncio Lima, the main malaria hotspot in northwestern Brazil. We also analyze rural-to-urban mobility caused by malaria treatment seeking, which poses an additional risk of infection to urban residents. We show that the rural localities most frequently visited by urban residents–typically farming settlements in the vicinity of the town–are those with the most intense malaria transmission and also the most frequent source localities of imported malaria cases diagnosed in the town. The most mobile urban residents are typically poor males 16 to 60-years old from multi-sited households who lack a formal job. Highly mobile residents represent a priority target for more intensive and effective malaria control interventions, that cannot be readily delivered to the entire community, in this and similar urbanized endemic settings across the Amazon.
Introduction
Although the overall burden of malaria in Latin America and the Caribbean has decreased dramatically over the past two decades, transmission persists in 21 countries in the region, where 120 million people are estimated to be currently exposed to some risk of infection [1]. The Amazon Basin, a vast territory that extends over Bolivia, Brazil, Colombia, Ecuador, Guyana, French Guiana, Peru, Suriname, and Venezuela, contributes approximately 90% of the region’s malaria burden [2].
Malaria in the Amazon has traditionally been perceived as a disease affecting poor rural communities, with most reported infections acquired in remote riverine villages [3,4], frontier farming settlements [5,6], gold mining [7,8], and Amerindian reserves [9–11]. Indeed, malaria rates tend to be lower in cities and towns, compared to surrounding rural settings, due to multiple factors such as improved housing and access to healthcare and limited availability of mosquito vector habitats [12]. Nevertheless, since the mid-1990s malaria cases have been increasingly reported within and near urban centers in the Amazon, consistent with sustained transmission in or around towns across the region [13–20].
The Amazon Basin of Brazil is facing an accelerated urban growth–estimated at 2.4% per year between 2000 and 2010 [21] and characterized by massive rural-to-urban migration, unplanned housing, and inadequate infrastructure–that challenges its conventional representation as a densely forested territory interspersed by small and isolated human settlements [22]. Urban residents now account for 72.5% of the region′s population and large cities with >500,000 inhabitants are home to almost 20% of the 24.4 million Amazonians [21]. Urbanized spaces ranging from metropolitan areas to small towns sprawling into the rainforest gradually became more tightly articulated to the surrounding farming settlements, riverine villages, and even indigenous communities [23,24]. This process extends to rural spaces some socioeconomic and spatial relations that are typical of urban centers, blurring the traditional rural-urban boundary, and fosters human mobility across the rural-urban interface as a key component of new livelihood and income diversification strategies [25,26]. Rural families typically travel to the nearest town or city at least once a month to sell their crops, purchase goods, and receive social benefits from conditional cash transfer programs and rural retirement programs [27]. Conversely, newly arrived urban families often maintain both urban and rural residences and rely on agricultural production for subsistence or additional income [26–28]. These factors leading to increased human mobility are key drivers of urban malaria risk, as parasites from rural villages are introduced and may spread in densely populated and receptive urban spaces, potentially leading to explosive epidemics or sustained endemic propagation of parasites [16,20,29].
Malaria transmission rates in Brazil are nowadays greatest in the upper Juruá Valley, next to the border with Peru [30]. With <0.5% of the Amazon's population, the region contributes 18% of the overall country's malaria burden, estimated at 186,485 cases in 2018 [1]. Malaria transmission spreads to some urbanized spaces in the Juruá Valley region, where large population of anopheline mosquito vectors that thrive in locally abundant natural and artificial water habitats, mainly fish farming ponds, renders these areas receptive to malaria transmission [16,17,29,31].
Here we combine epidemiological surveillance data and travel histories to explore human mobility patterns in Mâncio Lima, the main urban malaria hotspot of Brazil. We found that the localities that are most frequently visited by urban residents are typically those with the most intense malaria transmission. These localities also contribute the vast majority of imported malaria infections diagnosed in the urban area. Importantly, source communities with more intense transmission, which are likely to drive most urban malaria risk, are not hard-to-reach riverine villages; instead, they are situated in the vicinity of the town, where effective public health interventions are easier to implement.
Methods
Study site
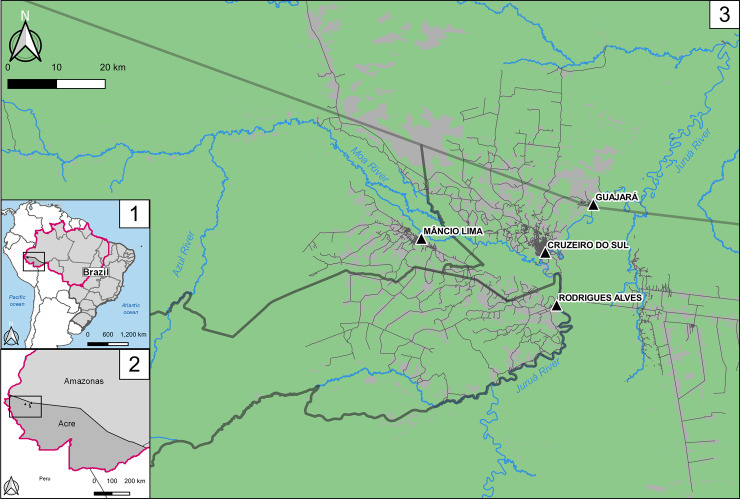
The study site, the municipality of Mâncio Lima, covers a surface area of 5,453 km2 in the upper Juruá Valley region of Acre State, westernmost Brazil (Fig 1). Half of its 18,638 inhabitants reside in the town of Mâncio Lima, the only urban area in the municipality (07°36'51" S, 72°53'45" W). We note that urban areas in Brazil are defined according to relatively arbitrary administrative rules that do not necessarily consider population density and other internationally adopted criteria [32]. Here we delimitate the town of Mâncio Lima essentially as done by the Brazilian Institute of Geography and Statistics (IBGE) but extend the urban area to two urbanized neighborhoods (Iracema to the Northwest and Pé da Terra to the Southeast), which are situated along the main road that crosses the town, following the “urbanicity” criteria developed by Dal’Asta and colleagues [33] for use in this setting. These two neighborhoods had been originally classified as rural by IBGE.
Fig 1. Location of the study site, the municipality of Mâncio Lima, Acre state, Brazil.
1: Brazilian Federal Units and the Amazon, also known as Legal Amazonia (magenta line in the map); 2: Acre and Amazonas states in dark and light gray, respectively, with the municipalities convered in this study highlighted in the weastern portion of the Fig 3: The municipalities of the upper Juruá Valley region: Mâncio Lima, Rodrigues Alves and Cruzeiro do Sul in Acre state and Guajará in Amazonas state. Dark thick lines represent the municipalities’ borders. The triangles show the town of each municipality, and in light green the forest cover in contrast with gray representing mostly deforested areas. Roads and streets are represented. Figure created with QGIS software version 3.14, an open source Geographic Information System (GIS) licensed under the GNU General Public License (https://bit.ly/2BSPB2F). Publicly available shape files provided from the Brazilian Institute of Geography and Statistics (IBGE) website (https://bit.ly/34gMq0S). Vegetated areas retrieved from Brazilian Institute for Space Research (2018) PRODES Project (https://bit.ly/33Q6wBD.) Roads and streets obtained from the Open Street Map Foundation website (https://bit.ly/36T2n1A). All utilized geographical data are under the Creative Commons Attribution License (CC BY 4.0).
Mâncio Lima has currently the highest annual parasite incidence (API; number of new laboratory-confirmed malaria cases per 1,000 population per year) for a municipality in Brazil, estimated at 422.8 in 2018 [34]. With a typical equatorial humid climate, the area receives most rainfall between November and April, but malaria transmission occurs year-round. Streams, wetlands rich in moriche palm trees, and natural and human-made fish farming ponds are widespread across the town of Mâncio Lima and serve as breeding habitats for malaria vectors [31]. The epidemiology of urban malaria in Mâncio Lima has been described in detail elsewhere [19].
Sociodemographic data and travel histories
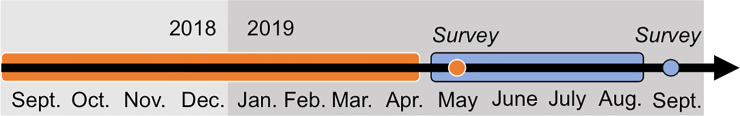
A population census performed by our field team between November 2015 and April 2016 enumerated 9,124 permanent residents in the urban area of Mâncio Lima, with ages ranging between <1 month and 105 years (mean, 27.0; median, 22.0; SD, 20.0 years) and distributed into 2,329 households [19]. Our study sample comprises all members of randomly selected households that correspond to approximately 20% of all households enumerated and mapped during a census survey. Simple probability sampling was carried out using a list of households generated during the census survey to select 25% of all households in Mâncio Lima, allowing for empty houses and those we were unable to locate. Structured questionnaires applied to study participants were used to obtain sociodemographic data and travel histories. To this end, two consecutive cross-sectional surveys were carried out in the study site and targeted the same population sample (Fig 2). The first survey, between May and June 2019, comprised 2,015 subjects aged <1–105 years (mean, 28.2; median, 24.0; SD, 20.1 years) distributed into 522 households. The originally selected households were revisited during the second survey, between September and October 2019, which comprised 2,130 subjects aged <1–105 years (mean, 28.4; median, 24.5; SD, 20.1 years) distributed into 562 households. Demographic, socioeconomic and occupational/behavioral information was obtained. We note, however, that the population sample was dynamic such that residents joining the household were enrolled and residents leaving the household between the two cross-sectional surveys were withdrawn. Since this is an exploratory observational study was originally designed to evaluate several sociodemographic, clinical, and laboratory outcomes, including human mobility-related outcomes, in the same population, no formal sample size and power calculations were made. The study was not originally intended to have statistical power to detect small differences between comparison groups and across different exposure strata, which are unlikely to be of public health significance.
Fig 2. Timeline of the cross-sectional surveys of urban residents in Mâncio Lima, Brazil, during which mobility data were collected.
In the May-June 2019 survey (orange circle in the figure), we collected information about overnight trips from September 2018 to April 2019; while in September-October 2019 survey (blue circle in the figure), we collected information about overnight trips from May to August 2019, then obtaining travel histories for the entire period of 12 months (September 2018 to August 2019).
To measure the spatial mobility of urban residents, individual reports of overnight trips within the past 6 months were collected during two consecutive cross-sectional surveys carried out 6 months apart. Reports included the total duration of each trip and its destination, allowing us to calculate the total number of days each individual spent in each destination between September 2018 and August 2019. Only trips for which the destination, resolved at the locality level (as defined below), was situated in the upper Juruá Valley region were considered (77.1% of all overnight trips). Original anonymized data are available in S1 Dataset.
Additional data sources
We retrieved all malaria case notifications from the upper Juruá Valley region (combined 2020 population estimate, 144,671 inhabitants) that were entered into the electronic malaria notification system of the Ministry of Health of Brazil between January 2016 and December 2018. Because malaria is a notifiable disease in Brazil and diagnostic testing and treatment are not available outside the network of government-run health care facilities, the database comprises the vast majority of laboratory-confirmed malaria episodes countrywide [35].
The upper Juruá Valley has been divided, for operational malaria control purposes, into smaller geographic units, or “localities”, with shared epidemiological and ecological characteristics [36]. The central points of the localities (typically a health post or school) were georeferenced using hand-held GPS receivers, all dwellings were identified and given a unique identifier, and all residents were enumerated during periodic census surveys carried out by the local malaria control program staff. We retrieved from the electronic malaria notification system the following locality-related information: (a) GPS coordinates, (b) population size, (c) number of locally acquired, laboratory-confirmed malaria episodes that were diagnosed and treated in the locality between 2016 and 2018, and (d) number of malaria episodes reportedly acquired in other localities that were diagnosed, treated and notified in the town of Mâncio Lima between 2016 and 2018 (i.e., imported infections [37]). An infection is routinely notified as imported when the patient reports overnight stays in an endemic site, within 15 days prior to diagnosis, which is different from the place where the infection has been diagnosed and notified [37].
From these data retrieved from the electronic malaria notification system we estimated the average API between 2016 and 2018 for every locality in the region and quantified rural-to-urban mobility caused by malaria-treatment seeking during this period, which determines the frequency of influx of infected individuals into the town (i.e., its vulnerability [37]). The numerator of API is the average number of locally acquired malaria cases between 2016 and 2018 and the denominator is the estimated population size for each locality in 2017 (based on the most recent census survey and adjusted for projections of population growth provided by the Brazilian Institute of Geography and Statistics). We note that the vast majority of imported infections in the study site are acquired in rural localities where malaria diagnosis facilities are not available, motivating treatment seeking in the town.
Data analysis
Field-collected data, entered using tablets programed with REDCap [38], were cleaned and exported to Stata SE 15.0 (StataCorp, TX, USA) for statistical analysis. Proportions were compared with χ2 tests and correlations were investigated using the Pearson′s correlation test.
Multivariate regression models with either dichotomic or continuous outcome variables were run to identify correlates of urban-to-rural mobility. The dichotomic outcomes analyzed with logistic regression models were: (1) overnight trip outside the town within the past 12 months (no/yes) and (2) overnight trip to high-risk localities–i.e., those with an API greater than that of the town of Mâncio Lima (442 cases per 1,000 inhabitants)–within the past 12 months (no/yes). Given the nested structure of the data (individuals clustered into households), we used the “meqrlogit” STATA command to build mixed-effects logistic regression models that included the grouping variable “household” as a random factor. These models performed better than their Poisson counterparts, as judged by Akaike’s and Bayesian information criteria; therefore, only logistic regression results are presented here. The continuous outcome variables analyzed with negative binomial models were: (3) total number of overnights outside the town within the past 12 months and (4) total number of overnights in high-risk localities. Models were built with the “menbreg” STATA command, including the grouping variable “household” as random factor. For each outcome we ran two separate regression models: (a) one for the entire population and (b) one for economically active males (i.e. aged 16–60 years old), who tend to be more mobile due to occupational activities and behavior. For each analysis we present both adjusted and unadjusted coefficients.
Variable selection for the final models followed the hierarchical approach based on conceptual frameworks as suggested by Victora and colleagues [39]; hierarchical levels are shown in S1 Fig. Variables available were: age group (0–5; 6–15; 16–40; 41–60; 41–60; > 60 years); gender (female, male); literacy (illiterate; literate); terciles of a household wealth index (poorest; intermediate; least poor) that considers housing characteristics and assets, such as vehicles and home appliances, and was computed as described by Filmer and Pritchett [40]; if anyone in the household receives benefits from the federal Bolsa Família conditional cash transfer program [41] (no; yes); individual work status (does not work; formal employee; informal employee; employer); family head workstatus (does not work; formal employee; informal employee; employer); regular fishing (no/yes) and presence of a second residence outside the urban area (no, yes). All estimates are provided along with 95% confidence intervals.
Ethics statement
The study protocol was approved by the Institutional Review Board of the Institute of Biomedical Sciences, University of São Paulo, Brazil, and by the National Committee of Ethics in Research (CONEP) of the Ministry of Health of Brazil (CAAE number 64767416.6.0000.5467). Written informed consent and assent were obtained from all study participants.
Results
Characteristics of the study population
Complete mobility information was available from 1,903 individuals, distributed into 504 households, who participated in both cross-sectional surveys. This total corresponds to 94.4% of individuals interviewed in May-June 2019 and 89.3% of those interviewed in September-October 2019. Sociodemographic characteristics of the study population are shown in S1 Table. Participants have a mean age of 28.3 years (range, <1–105 years; median, 24.0; standard deviation [SD], 20.2), with a male:female ratio of 0.95. Adults ≥25 years old reported 7.3 years of schooling on average, which corresponds to incomplete elementary school; 19.2% of study participants ≥15 years old are illiterate. Only 53.0% of individuals ≥18 years old reported to be currently working; of those, 8.6% are formally employed and the majority (55.7%) are informal employees who engage in seasonal farming in the surroundings of the town. Multi-sited households are common in Mâncio Lima– 16.8% (85 out of 504) of the families maintain both urban and rural residences. The 370 subjects living in multi-sited households were aged <1–92 years (mean, 27.3; median, 21.5; SD, 20.3), with a sex ratio close to 1:1 (186 females and 184 males). A total of 170 (45.9%) individuals live in households in the first (poorest) wealth index tercile. Moreover, 214 (57.8%) of the members of multi-sited households were directly of indirectly beneficiaries of the main conditional cash transfer program in Brazil (Bolsa Família), which targets the most socially vulnerable groups of the population. S2 Table provides the reported locations of second residences.
Malaria rates in the town of Mâncio Lima and surrounding localities
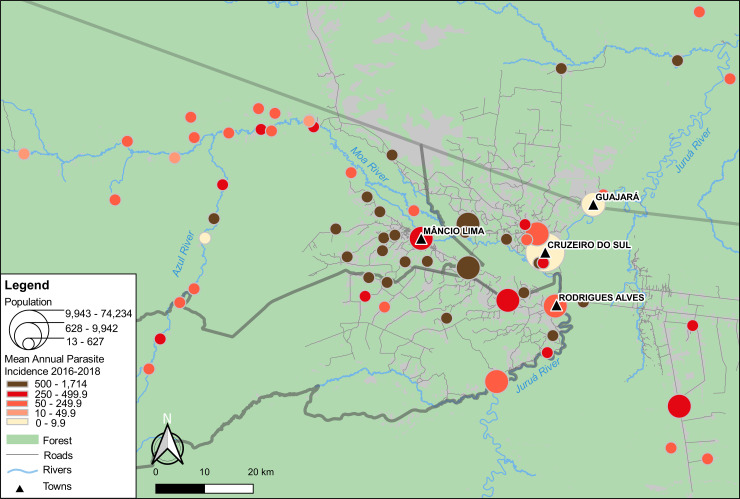
Fig 3 shows that average APIs vary widely among the 65 localities in the upper Juruá Valley that were reported as destinations of overnight trips by urban residents in Mâncio Lima. The names of all destinations are provided in S2 Fig; separate IPA averages for P. vivax and P. falciparum are given in S3 and S4 Figs. Average API between 2016 and 2018 ranges across localities from 1 to 1,714 laboratory-confirmed malaria cases, regardless of the species, per 1,000 population per year; estimates for each locality are listed in S3 Table.
Fig 3. Map showing the location of the town of Mâncio Lima and the 65 localities in the upper Juruá Valley region that were mentioned as travel destinations by study participants.
Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light yellow to dark brown that are proportional to malaria transmission intensity, using the average annual parasite incidences (APIs) for both P. vivax and P. falciparum between 2016 and 2018 as a proxy (higher APIs in darker tones).
The average API for the town of Mâncio Lima during the same period was 442 cases per 1,000 population per year, which is surprisingly high for an urban setting. For comparison, the three other urban centers in the upper Juruá Valley region–namely, Cruzeiro do Sul (estimated urban population, 63,800 inhabitants), Rodrigues Alves (population, 13,200), and Guajará (population, 8,800), whose locations are indicated in Fig 3 –sustain substantially lower malaria transmission compared with Mâncio Lima, with mean APIs of 1, 50, and 8 malaria cases per 1,000 population between 2016 and 1018, respectively. Of note, three fourths of the 24 localities with very intense malaria transmission (API ≥ 500) are periurban farming settlements situated within a 20-km radius of the town of Mâncio Lima. Only three high-risk localities are remote riverine villages along the main local rivers (Juruá, Moa, and Azul).
Contrary to the commonly held perception of malaria as a disease of isolated communities deep in the rainforest in the Amazon, periurban agricultural settlements contribute most of the malaria burden in the upper Juruá Valley, what is especially apparent for the municipality of Mâncio Lima (Fig 3). Somewhat surprisingly, this pattern is even more marked for P. falciparum infections, which mostly cluster in the vicinity of the town, being much less frequent in more remote sites (S3 Fig). Locally transmitted malaria remains relatively infrequent in the towns of Rodrigues Alves and Guajará and the city of Cruzeiro do Sul (S4 Table).
Urban-to-rural mobility and its determinants
Over one third (35.5%) of the study participants reported at least one overnight trip between September 2018 and August 2019, with a total of 34,150 overnights outside the town, corresponding to approximately 5% of their nights during the study period. Nearly half (47.0%) of the study participants who reported overnights outside the town were away for ≥1 month during the study period (one or more trips); 24.4% of them were away for ≥3 months.
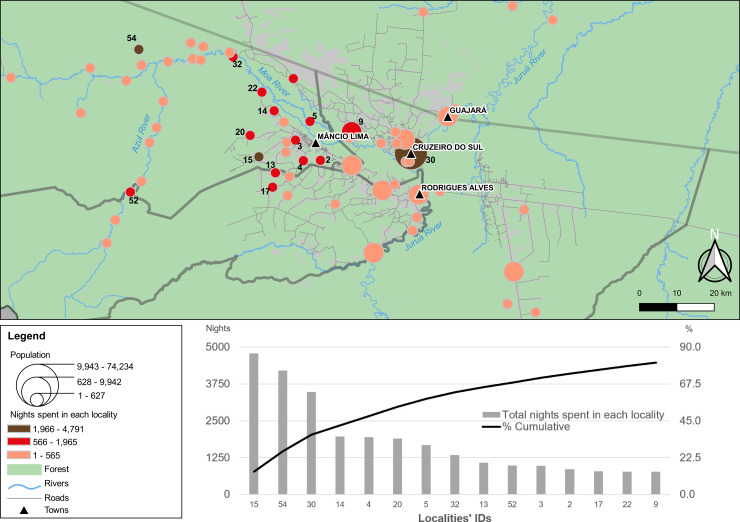
The three most frequent destinations are two small rural settlements (Tonico and Timbauba, #15 and #54 in Fig 4, respectively) and the nearest city (Cruzeiro do Sul, #30 in Fig 4). In contrast, the towns of Rodrigues Alves and Guajará attract relatively few visitors from Mâncio Lima. Tonico, the most visited locality, displays the highest API in the region, estimated at 1,714 cases per 1,000 inhabitants between 2016 and 2018 (S3 Table). Fifteen localities (14 of them rural) account for over 80% of overnights (Fig 4, lower panel; see also S5 Table). Importantly, the localities within 20 km of Mâncio Lima (32.3% of those shown in Fig 1) account for 58.1% of the total overnights outside the town. In addition, 48.7% of the reported overnights were in rural localities with API ≥ 500 (compare Figs 1 and 4), exposing urban visitors to substantial malaria risk. In other words, during the study period participants reportedly spent, on average, 2.4% of the their nights in high-risk localities, mostly in the vicinity of the town.
Fig 4. Trip destinations of residents in the town of Mâncio Lima according to number of overnight stays.
As in Fig 1, the map shows the location of the town of Mâncio Lima and the 65 localities in the upper Juruá Valley region with overnigths reported by study participants. Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light orange to dark brown that are proportional to the number of overnights in each locality between September 2018 and August 2019 (larger number of overnights in darker tones). The lower panel shows the cumulative number and proportion of overnights in the top-15 localities; their identification codes (IDs) are shown in the map.
The number of overnights in each locality is not significantly correlated with its distance from the town of Mâncio Lima (Pearson´s r = -0.22, P = 0.09). We note, however, that the three most visited localities (Tonico, Cruzeiro do Sul and Timbauba) are outliers in the regression analysis, being disproportionately more visited than expected from their distance from the town of Mâncio Lima (S5 Fig). Because the city of Cruzeiro do Sul (4,204 overnights), situated at Euclidian distance of 26 km southeast from Mâncio Lima, is the largest urban center in the region, its attractiveness is easily understood. Moreover, as discussed below, Tonico and Timbauba are common sites for second residences of urban families. When these three outliers are removed from the regression analysis, a significant negative correlation is observed between the number of overnights and distance from the town (Pearson’s r = -0.36, P = 0.004), suggesting that study participants tend to spend more overnights in proximate localities, with the exceptions noted above.
Not surprisingly, members of multi-sited households display increased mobility. Indeed, 55.4% of study participants whose families have a second residence reported at least one overnight trip in the previous 12 months, compared with only 30.7% of those with no second residence (P < 0.01, χ2 test). The riverine village of Timbauba, along the Moa river (54 km northwest of the town in Euclidian distance), is the second most frequent site for a second residence and also the second most visited locality (4,204 overnights). Likewise, the farming settlement of Tonico (16 km west of the town by road), the most visited locality (4,791 overnights) and the highest API in the region, is among the top-five locations where study participants have a second residence.
Mixed-effects multiple logistic regression analysis identified five significant correlates of overall urban-to-rural mobility and four correlates of mobility to high-risk areas (Table 1). Common risk factors associated with both outcomes were: (a) male gender; (b) regular fishing; and (c) a second residence outside the urban area. Age bewteen 16 and 40 years was a statistically significant risk factor for overall mobility, while people older than 60 years old were less likely to spend their nights in high-risk areas. Informal employees were more likely to travel, but not necessarily to high-risk localities.
Table 1. Mixed-effects logistic regression analysis of correlates of urban-to-rural overall mobility (left columns) and mobility to high-risk areas (right columns) in the study population of Mâncio Lima, northwestern Brazil (n = 1,903).
| Overall mobility (overnight trip outside the town within the past 12 months) | Mobility to high-risk areas (overnight trip outside the town within the past 12 months to localities with an API greater than that of the town of Mâncio Lima) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted model | Adjusted model | Unadjusted model | Adjusted model | |||||||||
| ORa | (95% CI)b | P | ORa | (95% CI)b | P | ORa | (95% CI)b | P | ORa | (95% CI)b | P | |
| Age | ||||||||||||
| 0–5 | Reference | Reference | Reference | Reference | ||||||||
| 06–15 | 1.19 | (0.7–2.0) | 0.506 | 1.06 | (0.6–1.8) | 0.837 | 1.01 | (0.5–2.0) | 0.968 | 0.93 | (0.5–1.9) | 0.846 |
| 16–40 | 2.64 | (1.6–4.2) | <0.0001 | 1.97 | (1.2–3.3) | 0.009 | 1.47 | (0.8–2.7) | 0.210 | 1.08 | (0.5–2.1) | 0.815 |
| 41–60 | 2.49 | (1.4–4.4) | 0.001 | 1.60 | (0.8–3.0) | 0.146 | 1.18 | (0.6–2.5) | 0.657 | 0.72 | (0.3–1.7) | 0.452 |
| > 60 | 0.81 | (0.4–1.6) | 0.543 | 0.63 | (0.3–1.3) | 0.198 | 0.32 | (0.1–0.9) | 0.029 | 0.22 | (0.1–0.6) | 0.006 |
| Gender | ||||||||||||
| Female | Reference | Reference | Reference | Reference | ||||||||
| Male | 1.82 | (1.4–2.4) | <0.0001 | 1.46 | (1.1–2.0) | 0.011 | 2.01 | (1.4–2.9) | <0.0001 | 1.61 | (1.1–2.4) | 0.017 |
| Work status | ||||||||||||
| Does not work | Reference | Reference | Reference | Reference | ||||||||
| Formal employee | 1.38 | (0.8–2.3) | 0.198 | 0.90 | (0.5–1.6) | 0.709 | 1.38 | (0.7–2.6) | 0.312 | 1.15 | (0.6–2.4) | 0.695 |
| Informal employee | 3.13 | (2.2–4.4) | <0.0001 | 1.61 | (1.1–2.4) | 0.022 | 2.21 | (1.5–3.4) | <0.0001 | 1.44 | 0.8–2.5) | 0.192 |
| Employer | 0.36 | (0.0–4.2) | 0.414 | 0.22 | (0.0–2.6) | 0.231 | 3.90 | (0.1–105.5) | 0.419 | 3.74 | (0.1–108.8) | 0.444 |
| Wealth indexc | ||||||||||||
| Poorest | Reference | Reference | Reference | Reference | ||||||||
| Intermediate | 0.70 | (0.4–1.2) | 0.223 | 0.77 | (0.43–1.4) | 0.385 | 1.90 | (0.8–4.4) | 0.132 | 2.33 | (1.0–5.5) | 0.054 |
| Least poor | 0.76 | (0.4–1.3) | 0.336 | 0.75 | (0.4–1.4) | 0.368 | 1.29 | (0.6–3.0) | 0.554 | 1.35 | (0.6–3.3) | 0.515 |
| Fishing | ||||||||||||
| No | Reference | Reference | Reference | Reference | ||||||||
| Yes | 3.3 | (2.3–4.7) | <0.0001 | 2.40 | (1.6–3.5) | <0.0001 | 2.52 | (1.58–4.0) | <0.0001 | 2.13 | (1.3–3.6) | 0.004 |
| Second residence | ||||||||||||
| No | Reference | Reference | Reference | Reference | ||||||||
| Yes | 5.05 | (2.8–9.1) | <0.0001 | 5.59 | (3.0–10.6) | <0.0001 | 6.8 | (2.9–16.0) | <0.0001 | 7.58 | (3.1–18.6) | <0.0001 |
aOR = odds ratio.
bCI = confidence interval.
cWealth Index terciles.
Mixed-effects negative binomial regression models identified the following factors independently associated with increased number of overnights outside the town: (a) male gender, (b) age between 16 and 60 years, (c) informal employment, (d) regular fishing, and (e) second residence outside the urban area (Table 2). We note that the least poor study participants reported less overnights outside the town, compared with the lowest wealth stratum. The analysis limited to overnights in high-risk areas identified only two significant positive associations: (a) male gender and (b) second residence outside the town. Taken together, these results allow to identify high-mobility study participants as typically males aged 16 to 60 years old in the lowest wealth stratum, with informal jobs, who have a second residence outside the town and fish regularly. Further multivariate analyses limited to male participants aged between 16 and 60 years (n = 535), who comprise the main economically active segment of the population, essentially confirmed these findings (S6 and S7 Tables). Of note, individuals in the intermediate (but not highest) wealth stratum were found to be significantly less mobile in this curtailed dataset.
Table 2. Mixed-effects negative binomial regression analysis of correlates of urban-to-rural overall mobility (left columns) and mobility to high-risk areas (right columns), in the study population of Mâncio Lima, northwestern Brazil (n = 1,903).
| Overall mobility (total number of overnights outside the town within the past 12 months) | Mobility to high-risk areas (total number of overnights in localities with an API greater than that of the town of Mâncio Lima) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unadjusted model | Adjusted model | Unadjusted model | Adjusted model | |||||||||
| IRRa | (95% CI)b | P | IRRa | (95% CI)b | P | IRRa | (95% CI)b | P | IRRa | (95% CI)b | P | |
| Age | ||||||||||||
| 0–5 | Reference | Reference | Reference | Reference | ||||||||
| 06–15 | 1.31 | (0.7–2.3) | 0.362 | 1.24 | (0.7–2.2) | 0.463 | 1.01 | (0.4–2.3) | 0.990 | 0.91 | (0.4–2.0) | 0.821 |
| 16–40 | 3.52 | (2.1–6.0) | <0.0001 | 2.73 | (1.5–4.8) | 0.001 | 2.06 | (1.0–4.3) | 0.052 | 1.61 | (0.7–3.6) | 0.243 |
| 41–60 | 4.14 | (2.2–7.8) | <0.0001 | 2.42 | (1.2–4.9) | 0.015 | 1.75 | (0.7–4.4) | 0.237 | 1.06 | (0.4–2.9) | 0.911 |
| > 60 | 1.27 | (0.6–2.8) | 0.566 | 0.97 | (0.4–2.2) | 0.938 | 0.72 | (0.2–2.4) | 0.595 | 0.48 | (0.1–1.7) | 0.256 |
| Gender | ||||||||||||
| Female | Reference | Reference | Reference | Reference | ||||||||
| Male | 2.43 | (1.8–3.3) | <0.0001 | 1.94 | (1.4–2.7) | <0.0001 | 3.04 | (2.00–4.7) | <0.0001 | 2.76 | (1.7–4.6) | <0.0001 |
| Work status | ||||||||||||
| Does not work | Reference | Reference | Reference | Reference | ||||||||
| Formal employee | 1.59 | (0.9–2.8) | 0.114 | 0.97 | (0.5–1.8) | 0.917 | 1.87 | (0.8–4.6) | 0.175 | 1.55 | (0.6–4.0) | 0.363 |
| Informal employee | 4.26 | (2.9–6.2) | <0.0001 | 1.70 | (1.0–2.8) | 0.031 | 3.32 | (1.9–5.7) | <0.0001 | 1.46 | (0.7–3.0) | 0.302 |
| Employer | 1.66 | (0.1–22.0) | 0.702 | 0.65 | (0.0–9.4) | 0.751 | 4.65 | (0.2–130.1) | 0.366 | 2.85 | (0.1–102.2) | 0.566 |
| Wealth indexc | ||||||||||||
| Poorest | Reference | Reference | Reference | Reference | ||||||||
| Intermediate | 0.53 | (0.3–1.0) | 0.041 | 0.60 | (0.3–1.1) | 0.103 | 3.03 | (1.0–9.4) | 0.056 | 2.76 | (1.0–7.8) | 0.055 |
| Least poor | 0.53 | (0.3–1.0) | 0.047 | 0.51 | (0.3–1.0) | 0.037 | 1.74 | (0.6–5.4) | 0.335 | 1.14 | (0.4–3.2) | 0.805 |
| Fishing | ||||||||||||
| No | Reference | Reference | Reference | Reference | ||||||||
| Yes | 3.60 | (2.4–5.4) | <0.0001 | 1.93 | (1.3–3.0) | 0.003 | 2.62 | (1.4–4.9) | 0.003 | 1.39 | (0.7–2.7) | 0.322 |
| Second residence | ||||||||||||
| No | Reference | Reference | Reference | Reference | ||||||||
| Yes | 13.3 | (7.3–24.4) | <0.0001 | 15.46 | (8.3–28.8) | <0.0001 | 60.18 | (18.3–197.8) | <0.0001 | 60.99 | (19.7–188.4) | <0.0001 |
aIRR = incidence rate ratio. Note that “incidence” here refers to the total number of overnights over 12 months.
bCI = confidence interval.
cWealth Index terciles.
Malaria treatment seeking and rural-to-urban mobility
Overall, 19,847 laboratory-confirmed malaria cases–including 16,347 P. vivax infections (82.4%) and 3,500 P. falciparum infections (17.6%)–were diagnosed, treated, and notified in the town of Mâncio Lima between January 2016 and December 2018. Of them, 5,389 (33.0%) P. vivax infections and 1,545 (44.1%) P. falciparum infections were classified as imported during routine case investigation (S8 Table). The ratio between locally transmitted and imported infections in the town is 2.0:1 for P. vivax and 1.3:1 for P. falciparum. These data indicate that a large number of subjects, either urban residents or not, who acquired malaria outside of the town regularly seek treatment in Mâncio Lima and expose their inhabitants to some risk of infection, given the malaria receptivity of the urban area.
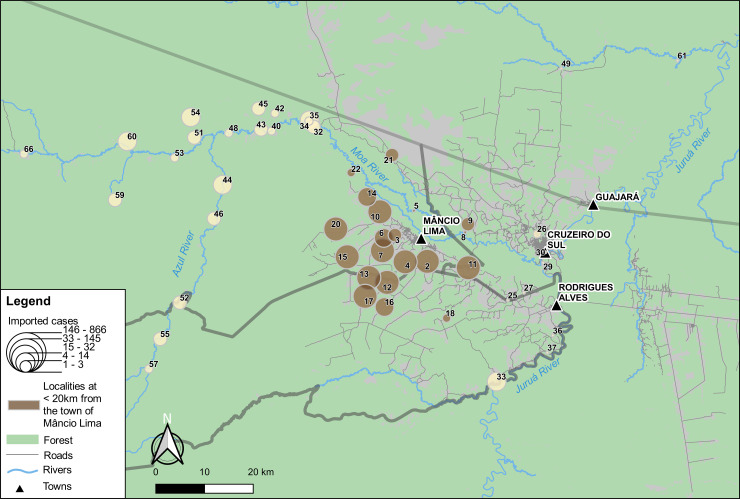
We next investigated the geographic origin of imported malaria infections notified in Mâncio Lima. The vast majority of them (77.8% for P. vivax and 78.3% for P. falciparum infections) had one of the 65 localities shown in Fig 1 recorded as the most likely origin during routine case investigation (S8 Table). The most common putative source localities of imported cases are shown in Fig 5. Importantly, the top-10 source localities, none of them more than 20 km away from the urban area, account for 64.5% of P. vivax and 69.3% of P. falciparum infections imported into the town of Mâncio Lima. Permanent malaria diagnosis outposts are not available in these localities. Importantly, the number of imported cases correlates negatively with the distance between the putative source locality and the town (Pearson’s r = -0.45, P = 0.001).
Fig 5. Map showing the localities recorded as source of imported malaria cases diagnosed and treated in Mâncio Lima between 2016 and 2018.
Localities are represented by circles with size proportional to the total number of malaria cases acquired in each locality that were diagnosed and treated in the town of Mâncio Lima between 2016 and 2018 (quintiles). Localities situated at < 20km from the town (Euclidian distance) are shown in bown. The numbers of infections per locality that were imported to the town are shown in S8 Table.
Discussion
The association between circular population movement and urban malaria risk has long been recognized in South America [42, 17] as well as in other endemic settings worldwide [e.g., 43–45]. Although public health policies cannot prevent directly human mobility, which is “driven mostly by need rather than choice” [46], they can proactively address some of the underlying causes and consequences of movements that contribute to malaria transmission.
Here we characterize patterns of spatial mobility in the main urban malaria hotspot of Brazil and their main determinants. We focus on the urban-to-rural mobility that places travelers at risk for malaria and rural-to-urban mobility caused by treatment seeking that poses a risk to urban residents, especially if rural visitors extend their stay in the town for selling crops, purchasing goods, or fully recovering from the current malaria episode. Importantly, the most common travel destinations are typically those with the most intense malaria transmission–essentially farming settlements situated within 20 km of Mâncio Lima, accessible to public health interventions, rather than remote riverine communities. These findings have clear implications for implementing effective malaria control policies in potential source communities that may fuel urban malaria transmission. The most mobile urban residents are poor males 16 to 60-years old from multi-sited households who lack a formal job in the town. Likewise, the most frequent source localities of imported cases diagnosed in Mâncio Lima are also situated within 20 km radius of the town.
The presence of multi-sited households in the Amazon [28] is part of a broader process called extended urbanization [23–25]. The traditional rural-urban divide in the region has been gradually replaced by a continuous gradient of “urbanicity”–typically urban features are extended to rural communities while towns and cities retain some “rurality” [33]. Our findings suggest that human mobility across the rural-urban gradient, mostly motivated by subsistence or commercial farming in peri-urban settlements, poses a continuous risk of malaria introduction into more urbanized and densely populated spaces.
These results can inform public health responses to prevent mobility-related urban and peri-urban malaria transmission across the Amazon, including large cities such as Manaus [18] and Porto Velho [15] in Brazil and Iquitos in Peru [14]. The first challenge consists in identifying the most mobile population strata who may contribute a large proportion of infections in the community [19]. Once identified, mobile individuals may be targeted with more intensive and effective interventions that cannot be readily delivered to the entire community. Importantly, the high-risk individuals in Mâncio Lima will acquire clinical immunity faster, after repeated infections [47], and eventually constitute a large clinically silent reservoir that carries malaria parasites across the rural-urban interface. Delivering personal protection measures, such as bed nets, and adequate access to diagnosis and treatment are examples of strategies to mitigate mobility-associated malaria risk.
Second, human mobility fuels malaria transmission in urban centers in the Amazon that are receptive–i.e., whose environmental conditions allow for malaria transmission from a human through a vector mosquito to another human [37]. Indeed, molecular analyses of parasite isolates provide evidence for sustained malaria transmission in the town of Mâncio Lima [20]. Vectors are increasingly abundant in this and other urbanized spaces in the Amazon and can sustain local malaria transmission. Typical larval habitats are natural water bodies in unplanned peri-urban settlements adjacent to forested areas [22] and natural and human-made fish farming ponds, now widespread in towns and cities across the region [16,29,31,48–50]. Extensive deforestation and environmental degradation may further displace vectors to more urbanized areas where suitable larval habitats are found [29]. Interestingly, highly productive larval habitants have also been increasingly found in areas dedicated to urban farming in tropical Africa (e.g., [51]). Larval source management with biological larvicides represents a logical approach to malaria control in urbanized spaces where breeding sites are relatively few, easy to find and readily accessible. It has been successful in African cities [52,53] and can drastically reduce anopheline larval density in fish farming ponds in the Amazon [54].
Third, imported infections diagnosed in urban communities across the Amazon do not necessarily originate in hard-to-reach traditional settlements. Instead, our results indicate that they are mostly acquired in farming settlements in the vicinity of the city or town, where farmers usually sell their crops and purchase goods. These findings imply that more intensive control interventions and better infrastructure for laboratory diagnosis and prompt treatment in nearby rural localities might drastically reduce the number of cases imported into the urban area. Moreover, as malaria transmission has been clearly linked to deforestation [29], environmental policies are also likely to contribute to malaria control in this and similar settings across the Amazon.
This study has some limitations. One is the possible recall bias in travel histories obtained at approximately six-month intervals, given the long time elapsed between the event and the interview. Alternatives to travel histories include the use of mobile phone data, which have been increasingly used to track human movements over time [55]. To this end, individuals are assigned to a primary cell phone tower based on the most frequently used tower at night. Travel to another tower catchment area is inferred if their location is recorded at that tower for more than one night. However, this strategy depends on relatively good mobile phone coverage, typically found in cities and towns [56] but absent in most rural sites in the Amazon. Recall bias may also affect the inference of the most likely site of infection, which was also self-reported, in the investigation of imported malaria cases. Finally, the use of routine malaria surveillance data, which are limited to clinical cases detected by conventional diagnostic methods such as microscopy or rapid diagnostic tests, is also a limitation. Routine surveillance typically overlooks chronic asymptomatic carriers of submicroscopic parasitemias who may seed infections in urban spaces over extended periods of time [57].
Despite these potential study limitations, we show that surveillance data combined with additional sociodemographic and mobility information from population-based surveys provides valuable information that can be explored for evidence-based planning and deployment of interventions aimed to reduce urban malaria risk across the Amazon.
Supporting information
(DOC)
(PDF)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(TIFF)
(TIF)
Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light yellow to dark brown that are proportional to malaria transmission intensity, using the APIs as a proxy (higher APIs in darker tones).
(TIF)
Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light yellow to dark brown that are proportional to malaria transmission intensity, using the APIs as a proxy (higher APIs in darker tones).
(TIF)
(TIFF)
Acknowledgments
We thank Juliana Tonini, Lais C. Salla, Thaís C. de Oliveira, Vanessa C. Nicolete, Madson L. de Oliveira, and Rodrigo M. Corder for their help in field work, and Maria José Menezes for her excellent administrative support.
Data Availability
Primary data used in our analyses are published with the manuscript as S1 Dataset.
Funding Statement
This work was supported by the Fundação de Amparo à Pesquisa do Estado de São Paulo (FAPESP; http://www.fapesp.br/en/), Brazil (grant 2016/18740-9), and by the National Institute of Allergy and Infectious Diseases, National Institutes of Health (https://www.niaid.nih.gov/), United States of America (grant U19 AI089681), which also provides a post-doctoral fellowship to ICJ. The Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq; http://cnpq.br/), Brazil, provides a senior research scholarship to MUF, while FAPESP provides a post-doctoral fellowship to PTR (2018/03902-9). The funders had no role in study design, data collection and analysis, preparation of the manuscript, or decision to publish.
References
- 1.World Health Organization. World Malaria Report 2018. Geneva, World Health Organization, 2019. Available at: http://www.who.int/malaria/publications/world-malaria-report-2019/en/ [Google Scholar]
- 2.Ferreira MU, Castro MC. Malaria situation in Latin America and the Caribbean: residual and resurgent transmission and challenges for control and elimination. Methods Mol Biol. 2019;2013:57–70. 10.1007/978-1-4939-9550-9_4 [DOI] [PubMed] [Google Scholar]
- 3.Alves FP, Durlacher RR, Menezes MJ, Krieger H, Silva LH, Camargo EP. High prevalence of asymptomatic Plasmodium vivax and Plasmodium falciparum infections in native Amazonian populations. Am J Trop Med Hyg. 2002;66:641–648. 10.4269/ajtmh.2002.66.641 [DOI] [PubMed] [Google Scholar]
- 4.Ladeia-Andrade S, Ferreira MU, de Carvalho ME, Curado I, Coura JR. Age-dependent acquisition of protective immunity to malaria in riverine populations of the Amazon Basin of Brazil. Am J Trop Med Hyg. 2009;80:452–459. [PubMed] [Google Scholar]
- 5.de Castro MC, Monte-Mór RL, Sawyer DO, Singer BH. Malaria risk on the Amazon frontier. Proc Natl Acad Sci USA. 2006;103:2452–2457. 10.1073/pnas.0510576103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.da Silva-Nunes M, Codeço CT, Malafronte RS, da Silva NS, Juncansen C, Muniz PT, et al. Malaria on the Amazonian frontier: transmission dynamics, risk factors, spatial distribution, and prospects for control. Am J Trop Med Hyg. 2008;79:624–635. [PubMed] [Google Scholar]
- 7.Pommier de Santi V, Dia A, Adde A, Hyvert G, Galant J, Mazevet M, et al. Malaria in French Guiana linked to illegal gold mining. Emerg Infect Dis. 2016;22:344–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sánchez JF, Carnero AM, Rivera E, Rosales LA, Baldeviano GC, Asencios JL, et al. Unstable malaria transmission in the southern Peruvian Amazon and its association with gold mining, Madre de Dios, 2001–2012. Am J Trop Med Hyg. 2017;96:304–311. 10.4269/ajtmh.16-0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Laserson KF, Wypij D, Petralanda I, Spielman A, Maguire JH. Differential perpetuation of malaria species among Amazonian Yanomami Amerindians. Am J Trop Med Hyg. 1999;60:767–773. 10.4269/ajtmh.1999.60.767 [DOI] [PubMed] [Google Scholar]
- 10.Bevilacqua M, Rubio-Palis Y, Medina DA, Cárdenas L. Malaria control in Amerindian communities of Venezuela: Strengthening ecohealth practice throughout conservation science and capability approach. Ecohealth. 2015;12:253–266. 10.1007/s10393-015-1026-3 [DOI] [PubMed] [Google Scholar]
- 11.Robortella DR, Calvet AA, Amaral LC, Fantin RF, Guimarães LFF, França Dias MH, et al. Prospective assessment of malaria infection in a semi-isolated Amazonian indigenous Yanomami community: Transmission heterogeneity and predominance of submicroscopic infection. PLoS One. 2020;15:e0230643 10.1371/journal.pone.0230643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wilson ML, Krogstad DJ, Arinaitwe E, Arevalo-Herrera M, Chery L, Ferreira MU, et al. Urban malaria: Understanding its epidemiology, ecology, and transmission across seven diverse ICEMR network sites. Am J Trop Med Hyg. 2015;93(3 Suppl):110–123. 10.4269/ajtmh.14-0834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Camargo LM, dal Colletto GM, Ferreira MU, Gurgel Sde M, Escobar AL, Marques A, et al. Hypoendemic malaria in Rondonia (Brazil, western Amazon region): seasonal variation and risk groups in an urban locality. Am J Trop Med Hyg. 1996;55:32–38. 10.4269/ajtmh.1996.55.32 [DOI] [PubMed] [Google Scholar]
- 14.Branch O, Casapia WM, Gamboa DV, Hernandez JN, Alava FF, Roncal N, et al. Clustered local transmission and asymptomatic Plasmodium falciparum and Plasmodium vivax malaria infections in a recently emerged, hypoendemic Peruvian Amazon community. Malar J. 2005;4:27 10.1186/1475-2875-4-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tada MS, Marques RP, Mesquita E, Dalla Martha RC, Rodrigues JA, Costa JD, et al. Urban malaria in the Brazilian Western Amazon Region I: high prevalence of asymptomatic carriers in an urban riverside district is associated with a high level of clinical malaria. Mem Inst Oswaldo Cruz. 2007;102:263–269. 10.1590/s0074-02762007005000012 [DOI] [PubMed] [Google Scholar]
- 16.Costa KM, de Almeida WA, Magalhães IB, Montoya R, Moura MS, de Lacerda MV. Malaria in Cruzeiro do Sul (Western Brazilian Amazon): analysis of the historical series from 1998 to 2008 [in Portuguese]. Rev Panam Salud Publica. 2010;28:353–360. 10.1590/s1020-49892010001100005 [DOI] [PubMed] [Google Scholar]
- 17.Lana RM, Riback TIS, Lima TFM, da Silva-Nunes M, Cruz OG, Oliveira FGS, et al. Socioeconomic and demographic characterization of an endemic malaria region in Brazil by multiple correspondence analysis. Malar J. 2017;16:397 10.1186/s12936-017-2045-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Almeida ACG, Kuehn A, Castro AJM, Vitor-Silva S, Figueiredo EFG, Brasil LW, et al. High proportions of asymptomatic and submicroscopic Plasmodium vivax infections in a peri-urban area of low transmission in the Brazilian Amazon. Parasit Vectors. 2018;11:194 10.1186/s13071-018-2787-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Corder RM, Paula GA, Pincelli A, Ferreira MU. Statistical modeling of surveillance data to identify correlates of urban malaria risk: A population-based study in the Amazon Basin. PLoS One. 2019;14:e0220980 10.1371/journal.pone.0220980 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salla LC, Rodrigues PT, Corder RM, Johansen IC, Ladeia-Andrade S, Ferreira MU. Molecular evidence of sustained urban malaria transmission in Amazonian Brazil, 2014–2015. Epidemiol Infect. 2020;148:e47 10.1017/S0950268820000515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.IBGE (Instituto Brasileiro de Geografia e Estatística). Censo Demográfico 2010. Resultados preliminares da amostra. Rio de Janeiro: IBGE, 2011.
- 22.Browder JO. The urban-rural interface: urbanization and tropical forest cover change. Urban Ecosyst. 2002;6:21–41. [Google Scholar]
- 23.Monte-Mór R. Modernities in the jungle: extended urbanization in the Brazilian Amazon. Ph.D. thesis. Los Angeles, University of California, Los Angeles, 2004.
- 24.Castriota R, Tonucci J. Extended urbanization in and from Brazil. Environ Plan D Soc Space. 2018; 36:512–528. [Google Scholar]
- 25.Barbieri A, Monte-Mór R, Bilsborrow, R. Towns in the jungle: exploring linkages between rural-urban mobility, urbanization and development in the Amazon. In: de Sherbinin A, Rahman A, Barbieri A, Fotso JC, Zhu Y (eds.). Urban population-environment dynamics in the developing world: case studies and lessons learned Paris, Committee for International Cooperation in National Research in Demography (CICRED), 2009. Available at http://www.populationenvironmentresearch.org/workshops.jsp#W2007
- 26.Barbieri A, Guedes GR, dos Santos RO. Migration, livelihoods and development in the post-frontier: evidences from the Brazilian Amazonia. Paper presented at the Meeting of the Population Association of America, Austin, Texas, 2019. Available at: http://paa2019.populationassociation.org/uploads/192149.
- 27.Eloy L, Brondízio E, Pateo R. New perspectives on mobility, urbanisation and resource management in riverine Amazonia. Bull Latin Am Res 2015;34:3–18. [Google Scholar]
- 28.Padoch C, Brondízio E, Costa S, Piñedo-Vásquez M, Sears RR, Siqueira A. Urban forest and rural cities: multi-sited households, consumption patterns, and forest resources in Amazonia. Ecol Soc. 2008;13:2. [Google Scholar]
- 29.Olson SH, Gangnon R, Silveira GA, Patz JA. Deforestation and malaria in Mâncio Lima County, Brazil. Emerg Infect Dis. 2010;16:1108–1115. 10.3201/eid1607.091785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ferreira MU, Castro MC. Challenges for malaria elimination in Brazil. Malar J. 2016;15:284 10.1186/s12936-016-1335-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.dos Reis IC, Codeço CT, Degener CM, Keppeler EC, Muniz MM, de Oliveira FG et al. Contribution of fish farming ponds to the production of immature Anopheles spp. in a malaria-endemic Amazonian town. Malar J. 2015;14:452 10.1186/s12936-015-0947-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Bueno MCD, Lima RNS. The degree of urbanisation in Brazil. Regional Stat. 2019; 9: 72–84. [Google Scholar]
- 33.Dal’Asta AP, Lana RM, Amaral S, Codeço CT, Monteiro AMV. The urban gradient in malaria-endemic municipalities in Acre: Revisiting the role of locality. Int J Environ Res Publ Health. 2018;15:1254 10.3390/ijerph15061254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ministry of Health of Brazil. List of municipalities belonging to areas at risk or endemic for malaria [in Portuguese]. Brasília, Ministry of Health of Brazil, 2019. Available at: https://www.saude.gov.br/images/pdf/2019/junho/25/Lista-de-municipios-pertencentes-as-areas-de-risco-ou-endemicas-para-malaria.pdf [Google Scholar]
- 35.Daher A, Silva JCAL, Stevens A, Marchesini P, Fontes CJ, Ter Kuile FO, et al. Evaluation of Plasmodium vivax malaria recurrence in Brazil. Malar J. 2019. January 22;18(1):18 10.1186/s12936-019-2644-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization. A framework for malaria elimination. Geneva, World Health Organization, 2017. Available at: https://www.who.int/malaria/publications/atoz/9789241511988/en/ [Google Scholar]
- 37.World Health Organization. WHO malaria terminology. Geneva, World Health Organization, 2018. (WHO reference number: WHO/HTM/GMP/2016.6). Available at: https://www.who.int/malaria/publications/atoz/malaria-terminology/en/ [Google Scholar]
- 38.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)–A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Victora CG, Huttly SR, Fuchs SC, Olinto MT. The role of conceptual frameworks in epidemiological analysis: a hierarchical approach. Int J Epidemiol. 1997;26:224–227. 10.1093/ije/26.1.224 [DOI] [PubMed] [Google Scholar]
- 40.Filmer D, Pritchett LH. Estimating wealth effects without expenditure data—or tears: an application to educational enrollments in states of India. Demography. 2001;38:115–132. 10.1353/dem.2001.0003 [DOI] [PubMed] [Google Scholar]
- 41.Rasella D, Aquino R, Santos C, Paes-Sousa R, Barreto ML. Effect of a conditional cash transfer programme on childhood mortality: a nationwide analysis of Brazilian municipalities. Lancet 2013;382: 57–64 10.1016/S0140-6736(13)60715-1 [DOI] [PubMed] [Google Scholar]
- 42.Osorio L, Todd J, Bradley DJ. Travel histories as risk factors in the analysis of urban malaria in Colombia. Am J Trop Med Hyg. 2004;71:380–386. [PubMed] [Google Scholar]
- 43.Lowa M, Sitali L, Siame M, Musonda P. Human mobility and factors associated with malaria importation in Lusaka district, Zambia: a descriptive cross sectional study. Malar J. 2018;17:404 10.1186/s12936-018-2554-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guerra CA, Kang SY, Citron DT, Hergott DEB, Perry M, Smith J, et al. Human mobility patterns and malaria importation on Bioko Island. Nat Commun. 2019;10:2332 10.1038/s41467-019-10339-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Saita S, Pan-Ngum W, Phuanukoonnon S, Sriwichai P, Silawan T, White LJ, et al. Human population movement and behavioural patterns in malaria hotspots on the Thai-Myanmar border: implications for malaria elimination. Malar J. 2019;18:64 10.1186/s12936-019-2704-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Martens P, Hall L. Malaria on the move: human population movement and malaria transmission. Emerg Infect Dis. 2000;6:103–109. 10.3201/eid0602.000202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Corder RM, Ferreira MU, Gomes MGM. Modelling the epidemiology of residual Plasmodium vivax malaria in a heterogeneous host population: A case study in the Amazon Basin. PLoS Comput Biol. 2020;16:e1007377 10.1371/journal.pcbi.1007377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Maheu-Giroux M, Casapía M, Sotto-Calle VE, Ford LB, Buckeridge DL, Coomes OT, et al. Risk of malaria transmission from fish ponds in the Peruvian Amazon. Acta Trop 2010; 115:112–118. 10.1016/j.actatropica.2010.02.011 [DOI] [PubMed] [Google Scholar]
- 49.Barros FS, Honório NA. Deforestation and malaria on the Amazon frontier: larval clustering of Anopheles darlingi (Diptera: Culicidae) determines focal distribution of malaria. Am J Trop Med Hyg. 2015;93:939–953. 10.4269/ajtmh.15-0042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Martins LMO, David MR, Maciel-de-Freitas R, Silva-do-Nascimento TF. Diversity of Anopheles mosquitoes from four landscapes in the highest endemic region of malaria transmission in Brazil. J Vector Ecol. 2018;43: 235–244. 10.1111/jvec.12307 [DOI] [PubMed] [Google Scholar]
- 51.Matthys B, Vounatsou P, Raso G, Tschannen AB, Becket EG, Gosoniu L, et al. Urban farming and malaria risk factors in a medium-sized town in Cote d'Ivoire. Am J Trop Med Hyg. 2006;75:1223–31. [PubMed] [Google Scholar]
- 52.Fillinger U, Lindsay SW. Larval source management for malaria control in Africa: myths and reality. Malar J. 2011;10:353 10.1186/1475-2875-10-353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Maheu-Giroux M, Castro MC. Impact of community-based larviciding on the prevalence of malaria infection in Dar es Salaam, Tanzania. PLoS One. 2013;8:e71638 10.1371/journal.pone.0071638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fontoura PS, da Costa AS, Ribeiro FS, Ferreira MS, Castro MC, Ferreira MU. Field efficacy of VectoMax FG and VectoLex CG biological larvicides for malaria vector control in northwestern Brazil. J Med Entomol. 2020;57:942–946. 10.1093/jme/tjz220 [DOI] [PubMed] [Google Scholar]
- 55.Wesolowski A, Buckee CO, Engø-Monsen K, Metcalf CJE. Connecting mobility to infectious diseases: the promise and limits of mobile phone data. J Infect Dis. 2016;214(suppl 4):S414–S420. 10.1093/infdis/jiw273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Fornace KM, Surendra H, Abidin TR, Reyes R, Macalinao MLM, Stresman G, et al. Use of mobile technology-based participatory mapping approaches to geolocate health facility attendees for disease surveillance in low resource settings. Int J Health Geogr. 2018;17:21 10.1186/s12942-018-0141-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Lindblade KA, Steinhardt L, Samuels A, Kachur SP, Slutsker L. The silent threat: asymptomatic parasitemia and malaria transmission. Expert Rev Anti Infect Ther. 2013;11:623–639. 10.1586/eri.13.45 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOC)
(PDF)
(XLSX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(DOCX)
(TIFF)
(TIF)
Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light yellow to dark brown that are proportional to malaria transmission intensity, using the APIs as a proxy (higher APIs in darker tones).
(TIF)
Georeferenced localities are represented by circles with size proportional to their population size and filled with tones from light yellow to dark brown that are proportional to malaria transmission intensity, using the APIs as a proxy (higher APIs in darker tones).
(TIF)
(TIFF)
Data Availability Statement
Primary data used in our analyses are published with the manuscript as S1 Dataset.