Abstract
Study Objective
The purpose of this study was to assess the impact of the coronavirus disease 2019 (COVID-19) pandemic on surgical volume and emergency department (ED) consults across obstetrics-gynecology (OB-GYN) services at a New York City hospital.
Design
Retrospective cohort study.
Setting
Tertiary care academic medical center in New York City.
Patients
Women undergoing OB-GYN ED consults or surgeries between February 1, 2020 and April 15, 2020.
Interventions
March 16 institutional moratorium on elective surgeries.
Measurements and Main Results
The volume and types of surgeries and ED consults were compared before and after the COVID-19 moratorium. During the pandemic, the average weekly volume of ED consults and gynecology (GYN) surgeries decreased, whereas obstetric (OB) surgeries remained stable. The proportions of OB-GYN ED consults, GYN surgeries, and OB surgeries relative to all ED consults, all surgeries, and all labor and delivery patients were 1.87%, 13.8%, 54.6% in the pre–COVID-19 time frame (February 1–March 15) vs 1.53%, 21.3%, 79.7% in the COVID-19 time frame (March 16–April 15), representing no significant difference in proportions of OB-GYN ED consults (p = .464) and GYN surgeries (p = .310) before and during COVID-19, with a proportionate increase in OB surgeries (p <.002). The distribution of GYN surgical case types changed significantly during the pandemic with higher proportions of emergent surgeries for ectopic pregnancies, miscarriages, and concern for cancer (p <.001). Alternatively, the OB surgery distribution of case types remained relatively constant.
Conclusion
This study highlights how the pandemic has affected the ways that patients in OB-GYN access and receive care. Institutional policies suspending elective surgeries during the pandemic decreased GYN surgical volume and affected the types of cases performed. This decrease was not appreciated for OB surgical volume, reflecting the nonelective and time-sensitive nature of obstetric care. A decrease in ED consults was noted during the pandemic begging the question “Where have all the emergencies gone?” Although the moratorium on elective procedures was necessary, “elective” GYN surgeries remain medically indicated to address symptoms such as pain and bleeding and to prevent serious medical sequelae such as severe anemia requiring transfusion. As we continue to battle COVID-19, we must not lose sight of those patients whose care has been deferred.
Keywords: Coronavirus disease 2019, Emergency department consults, Gynecologic surgeries, Obstetric surgeries
On March 1, 2020 the first patient in New York was diagnosed with severe acute respiratory syndrome coronavirus 2, the virus responsible for the coronavirus disease 2019 (COVID-19) pandemic [1]. New York City quickly became the epicenter as infection rates soared and hospital leaders instituted policy changes to limit exposures, preserve personal protective equipment, repurpose hospital space, and redeploy staff in the anticipation of increased COVID-19 admissions [2].
One such change was the halting of elective surgeries. On March 16, the American College of Obstetrics and Gynecology, jointly with other associations, released a statement concurring with the United States Surgeon General calling for a moratorium on surgeries if delay would not cause harm [3]. On March 20, the governor of New York issued a stay-at-home order to minimize transmission. The Centers for Disease Control and Prevention announced that most with COVID-19 have “mild illness and are able to recover at home without medical care,” instructing only those with “trouble breathing” or “other emergency warning signs” to seek care [4].
Because of these unprecedented measures, we wanted to evaluate how these circumstances affected our obstetrics-gynecology (OB-GYN) department. The objective of this study was to assess the volume and indications of emergency department (ED)–consults and surgeries for the OB-GYN service at Columbia University Irving Medical Center in New York City before and after the elective surgery moratorium during the COVID-19 pandemic.
Materials and Methods
Patient Selection
This was an observational retrospective cohort study. All OB-GYN consults and surgeries, including pediatric and adult patients, that took place at New York Presbyterian (NYP)–Columbia University Irving Medical Center (CUIMC) from February 1, 2020 to April 15, 2020 were included. NYP-CUIMC is a tertiary care academic medical center located in New York City with a broad referral network of patients with complex cases and those who are high risk. It consists of 2 teaching hospitals, Milstein Hospital and Morgan Stanley Children's Hospital. Consults or surgeries performed at other New York Presbyterian hospitals and satellite locations were not included.
On March 13, 2020, NYP-CUIMC announced a moratorium on all nonemergent elective surgeries starting March 16. All patients who had ED consults or surgery between February 1 and March 15 (44-day period) were categorized into the pre–COVID-19 group, and all patients between March 16 and April 15 (31-day period) were categorized into the COVID-19 group. All patients during the defined pre–COVID-19 and COVID-19 time frames were included for analysis. Although the New York stay-at-home order did not go into effect until March 20, we measured the change in ED consultations after March 16 to coincide with the moratorium on elective surgery for consistency. It is likely that behavior change throughout New York had already begun before the stay-at-home order was made, although perhaps not as drastically.
Data Collection
OB-GYN consults and surgeries were identified through electronic data extraction from the electronic medical record (EMR). Both hospital sites included in this study, Milstein Hospital and Morgan Stanley Children's Hospital, share the same EMR system. Data were generated from EMR queries by a data analytic expert and confirmed by 2 of the authors who were clinical members on the OB-GYN team. Obstetric (OB) and gynecology (GYN) surgical cases were additionally confirmed with an internal departmental patient list used for quality improvement review. When necessary, a manual chart review was conducted to verify data abstraction and to extract certain variables of interest.
Data Classification
ED Consults
All consult requests from the ED to the GYN, GYN oncology, or OB services were included. The consult requests were classified by the indication for the consult, examples including pregnancy of unknown location, pelvic pain, abnormal vaginal bleeding, among others outlined in Table 1 . Inpatient OB-GYN consults for patients who were hospitalized and patients who were seen in labor and delivery triage were not included in this analysis.
Table 1.
Indications and disposition of emergency department consultations to OB-GYN before and after March 16 moratorium on nonemergent surgery
| ED consults | Pre–COVID-19 n = 275 | COVID-19 n = 79 | p-value |
|---|---|---|---|
| Consult indication | |||
| Pelvic pain* | 65 (23.6) | 25 (31.6) | .317 |
| Pregnancy of unknown location/ectopic pregnancy | 55 (20.0) | 10 (12.7) | |
| Pregnancy concerns and second trimester losses | 37 (13.5) | 11 (13.9) | |
| Spontaneous abortion | 27 (9.8) | 6 (7.6) | |
| Postpartum concerns† | 18 (6.5) | 3 (3.8) | |
| Abnormal uterine bleeding | 17 (6.2) | 9 (11.4) | |
| Cancer | 17 (6.2) | 4 (5.1) | |
| Postoperative concern | 13 (4.7) | 3 (3.8) | |
| Bartholin's cyst/labial abscess or laceration | 12 (4.4) | 6 (7.6) | |
| Other | 14 (5.1) | 1 (1.3) | |
| Disposition after emergency department evaluation | |||
| n = 275 | n = 79 | ||
| Operating room | 31 (11.3) | 7 (8.9) | .171 |
| Transfusion | 10 (3.6) | 7 (8.9) | |
| Admission to OB or GYN service | 34 (12.4) | 13 (16.5) | |
COVID-19 = coronavirus disease 2019; ED = emergency department; GYN = gynecology; OB = obstetric.
Values are given in number (%).
Pelvic pain includes adnexal masses, rule-out torsion, pelvic inflammatory disease, tubo-ovarian abscess.
Postpartum concerns include postcesarean section concerns.
GYN Surgery
GYN surgeries were classified by service (benign GYN vs GYN oncology), case acuity (scheduled vs emergent), and surgical approach (vaginal, hysteroscopic, laparoscopic, abdominal, or other). The surgeries were also classified by case types, which were defined by the primary indication for surgery (Tables 2 and 3 ). For example, if a patient had symptomatic myomas and an incidental ovarian cyst, the case type was assigned as “fibroid surgery” to reflect the primary reason for surgery. Please see Supplemental Table 1 for a detailed breakdown of cases by all indications, symptoms and conditions.
Table 2.
GYN surgical characteristics
| Cases | Pre–COVID-19 N = 212 | COVID-19 N = 32 | p-value |
|---|---|---|---|
| Benign GYN surgeon | 134 (63.2) | 19 (59.4) | .825 |
| GYN oncologist surgeon | 78 (36.8) | 13 (40.6) | |
| Scheduled case | 187 (88.2) | 20 (62.5) | <.01 |
| Emergent case | 25 (11.8) | 12 (37.5) | |
| Vaginal | 21 (9.9) | 9 (28.1) | .022 |
| Hysteroscopic | 34 (16.0) | 1 (3.1) | |
| Laparoscopic | 117 (55.2) | 18 (56.3) | |
| Abdominal | 33 (15.6) | 3 (9.4) | |
| Other | 7 (3.3) | 1 (3.1) |
COVID-19 = coronavirus disease 2019; GYN = gynecology.
Values are given in number (%).
Table 3.
Primary indications for surgeries
| Cases | Pre–COVID-19 | COVID-19 | p-value |
|---|---|---|---|
| Total | 212 | 32 | |
| Concern for cancer | 50 (23.6) | 12 (37.5) | <.001 |
| Myomas (hysterectomy or myomectomy) | 45 (21.2) | 0 | |
| Postmenopausal bleeding or thickened endometrium | 17 (8.0) | 1 (3.1) | |
| Adnexal mass | 16 (7.5) | 1 (3.1) | |
| Ectopic pregnancy | 12 (5.7) | 6 (18.8) | |
| Endometriosis | 15 (7.1) | 0 | |
| Pelvic organ prolapse or incontinence | 14 (6.6) | 0 | |
| Abnormal uterine bleeding | 10 (4.7) | 2 (6.2) | |
| Other GYN indications* | 8 (3.8) | 2 (6.2) | |
| Infertility† | 9 (4.2) | 0 | |
| Adnexal torsion | 6 (2.8) | 2 (6.2) | |
| Pelvic pain | 7 (3.3) | 2 (6.2) | |
| Spontaneous abortion (D&C) | 3 (1.4) | 4 (12.5) | |
| Total | 237 | 181 | |
| Required cesarean section | 211 (89.0) | 164 (90.6) | .366 |
| Required cesarean hysterectomy for placenta accreta spectrum | 5 (2.1) | 3 (1.7) | |
| Required cerclage and cerclage removal | 10 (4.2) | 8 (4.4) | |
| Required fetal procedure | 2 (0.8) | 4 (2.2) | |
| Other OB indications‡ | 9 (3.8) | 2 (1.1) |
COVID-19 = coronavirus disease 2019; D&C = dilation and curettage; GYN = gynecology; OB = obstetric.
Values are given in number (%).
Other GYN includes family planning procedures, labial abscesses, hematocolpos, risk-reducing gonadectomy.
Infertility includes tubal disease, intrauterine adhesions, septum, or submucosal myomas.
Other OB includes examination under anesthesia, D&C for postpartum hemorrhage and tubal ligation after vaginal delivery.
Supplemental Table 1.
Indications for GYN Surgeries: Breakdown by symptoms and conditions
| Clinical Indication & Diagnoses | PRE-COVID-19 N= 212 | COVID-19 N=32 |
|---|---|---|
| Pain | 79 | 13 |
| Myoma | 34 | 1 |
| Ectopic pregnancy | 12 | 6 |
| Endometriosis | 14 | 1 |
| Adnexal mass | 16 | 0 |
| Adnexal Torsion | 5 | 3 |
| Ruptured ovarian cyst | 2 | 0 |
| Other | 4 | 2 |
| Vaginal Bleeding | 29 | 6 |
| Myoma | 14 | 1 |
| Endometrial Polyp | 7 | 0 |
| Spontaneous abortion | 3 | 4 |
| Other | 5 | 1 |
| Infertility | 14 | 0 |
| Intrauterine disease | 10 | 0 |
| Tubal disease | 3 | 0 |
| Endometriosis | 2 | 0 |
| Postmenopausal pathology | 19 | 1 |
| Postmenopausal bleeding | 15 | 1 |
| Endometrial polyp | 8 | 0 |
| Thickened Endometrium | 3 | 0 |
| Family Planning* | 3 | 1 |
| Sterilization | 2 | 0 |
| Abortion | 1 | 1 |
| Urogynecology | 15 | 0 |
| Prolapse | 12 | 0 |
| Incontinence | 3 | 0 |
| Cancer or Concern for malignancy | 57 | 12 |
| Endometrial cancer | 18 | 6 |
| Ovarian Cancer | 24 | 2 |
| Cervical Cancer | 7 | 1 |
| Other | 8 | 3 |
| Other | 6 | 1 |
Family planning procedures are generally performed at satellite locations.
Note: All surgical indications recorded, thus 1 case may fall into multiple categories.
Finally, surgeries were separated into categories of required surgical cases defined by the Accreditation Council for Graduate Medical Education (ACGME) for OB-GYN residency graduation requirements [5]. Given the limitations of data extraction, cystourethroscopy and abortions were not included in this analysis because cystourethroscopies were not captured as the primary surgeries performed, and most abortion procedures are done at satellite locations not analyzed in this study.
Data Analysis
To capture the change in case types before and after the COVID-19 mandate, comparisons between groups were made on the basis of proportions (i.e., percent distribution) for different indications for ED consults and different case types for GYN and OB surgeries because the time period between groups were different. A weekly case volume and weekly percentage change and its 95% confidence interval were calculated for each case type of OB-GYN consults on the basis on 2 independent binomial distributions between the pre–COVID-19 and COVID-19 groups. Each ED consult was only assigned 1 indication for consult, and each surgery was assigned only 1 case type to accurately calculate proportions by using multinomial distributions.
Comparative statistical analysis was performed using independent samples t tests for age and body mass index. The proportions of OB-GYN consults and surgeries were compared by unpooled 2-sided z test. Categoric variables were compared by chi-square tests. Statistical significance was defined as p-value <.05. All analyses were performed using Python (Python Software Foundation, Wilmington, DE) and R (Bell Labs, Murray Hill, NJ) .
Institutional Review Board Approval
This study was approved by the institutional review board (AAAS9860) of CUIMC and was granted a waiver of consent.
Results
Basic demographics for patients receiving OB-GYN ED consults and surgeries before and after the March 16 moratorium on elective surgeries are presented in Table 4 . Overall demographics among the patients in the pre–COVID-19 and COVID-19 groups were similar.
Table 4.
Demographic characteristics of emergency department consults, gynecology surgeries, and obstetric surgeries
| Patients | Pre–COVID-19* | COVID-19† | p-value |
|---|---|---|---|
| Emergency department consults | n = 275 | n = 79 | |
| Age, yrs, mean (SD) | 31.80 (12.3) | 32.05 (15.02) | .883 |
| BMI, kg/m2, mean (SD)‡ | 27.86 (6.1) | 29.46 (7.4) | .170 |
| Race, n (%) | |||
| White | 91 (33.1) | 23 (29.1) | .667 |
| Black or African American | 55 (20.0) | 22 (27.8) | |
| Asian | 8 (2.9) | 2 (2.5) | |
| Other | 84 (30.5) | 21 (26.6) | |
| Declined/not available | 37 (13.5) | 11 (13.9) | |
| Gynecologic surgeries | n = 212 | n = 32 | |
| Age, yrs, mean (SD) | 46.9 (16.2) | 45.7 (21.1) | .701 |
| BMI, kg/m2, mean (SD) | 28.3 (6.3) | 29.0 (7.5) | .584 |
| Race, n (%) | |||
| White | 89 (42.0) | 18 (56.2) | .190 |
| Black or African American | 46 (21.7) | 6 (18.8) | |
| Asian | 9 (4.2) | 2 (6.2) | |
| Other | 32 (15.1) | 5 (15.6) | |
| Declined/not available | 36 (17.0) | 1 (3.1) | |
| Obstetric surgeries | n = 237 | n = 181 | |
| Age, yrs, mean (SD) | 33.4 (5.1) | 33.0 (6.4) | .399 |
| BMI, kg/m2, mean (SD) | 32.8 (21.2) | 31.9 (5.4) | .575 |
| Race, n (%) | |||
| White | 100 (42.2) | 59 (32.6) | .022 |
| Black or African American | 47 (19.8) | 26 (14.4) | |
| Asian | 11 (4.6) | 6 (3.3) | |
| Other | 46 (19.4) | 52 (28.7) | |
| Declined/not available | 33 (13.9) | 38 (21.0) | |
BMI = body mass index; COVID-19 = coronavirus disease 2019; SD = standard deviation.
Pre–COVID group included all patients from February 1, 2020 to March 15, 2020.
COVID-19 group included all patients from March 16, 2020 to April 15, 2020.
There was missing data for BMI in the consult group: *pre–COVID-19 group n=200, ‡COVID-19 group n= 41. The BMI was unknown for 75 of patients in the pre–COVID-19 group (n = 200) and 38 of the COVID-19 group (n = 41).
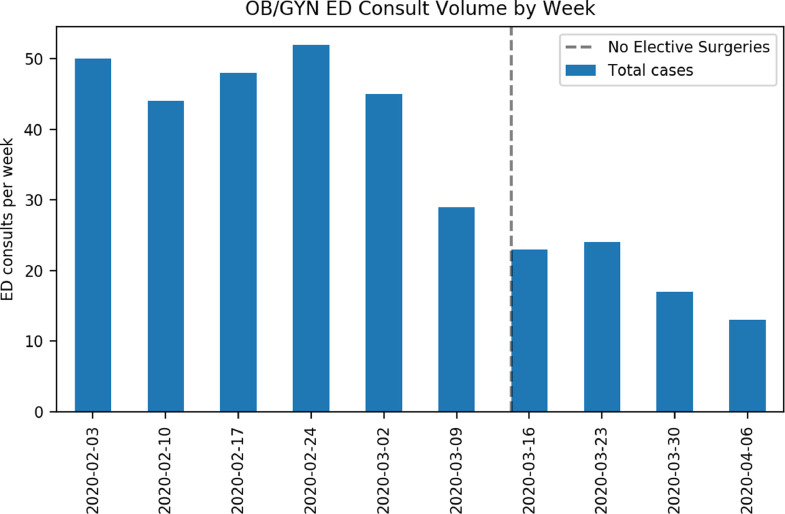
There were 275 OB-GYN ED consults among a total of 14 719 ED consults in the pre–COVID-19 group compared with 79 OB-GYN ED consults among 5150 ED consults in the COVID-19 group. The average number of OB-GYN ED consults per week decreased from 44.8 to 17.8 between groups, demonstrating a 60.3% decrease in weekly OB-GYN ED consult volume (Fig. 1 ). When comparing pre–COVID-19 and COVID-19 time frames, the proportions of OB-GYN ED consults to total ED consults were 1.87% vs 1.53%, which was not significant (p = .464) (Table 5 ). As shown in Table 1, the 3 most common indications for OB-GYN ED consults remained the same in both time periods. There was no significant difference in the distribution of the consult indications and their dispositions for the pre–COVID-19 vs COVID-19 groups. Although a greater percentage of ED consult requests for the evaluation of pelvic pain, abnormal uterine bleeding, and labial/perineal conditions were noted in the COVID-19 group compared with the pre–COVID-19 group, these differences were not significant (p = .317). Overall treatment plans, particularly surgical, for patients receiving OB-GYN consults in the ED did not differ significantly pre–COVID-19 or COVID-19 (p = .171). Pre–COVID-19, 31 patients (11.3%) evaluated in the ED required surgical management for diagnoses including ectopic pregnancy, hemorrhage requiring dilation and curettage, and ovarian torsion. During the COVID-19 period, 7 (8.9%) were surgically managed for any reason. The number of patients presenting with bleeding that was significant enough to require a blood transfusion decreased from 10 to 7 (Table 1).
Fig. 1.
This figure shows the total volume of OB-GYN consults per week over the course of the early coronavirus disease 2019 pandemic. The dotted line indicates the date of the mandated ban on elective cases. ED = emergency department; GYN = gynecology; OB = obstetric.
Table 5.
Comparison of OB-GYN consults and surgical volumes pre–COVID-19 vs COVID-19 period
| Patients | Pre–COVID-19 February 1, 2020–March 15, 2020, 44 d | COVID-19 March 16, 2020–April 15, 2020, 31 d | Weekly percentage `change (95% CI) % | p-value |
|---|---|---|---|---|
| All ED consults | 14 719 | 5150 | –0.33 (–1.23 to 0.56) | .464 |
| Total OB-GYN consults, rate | 275 (1.87%) | 79 (1.53%) | ||
| Average OB-GYN consults/wk | 44.8 | 17.8 | ||
| All surgeries | 1531 | 150 | 7.4 (–6.98 to 21.9) | .310 |
| Total GYN surgeries, rate | 212 (13.8%) | 32 (21.3%) | ||
| Average GYN surgeries/wk | 34.8 | 7.2 | ||
| All patients in labor and delivery | 434 | 227 | 25.1 (9.0 to 41.2) | .002 |
| Total OB surgeries, rate | 237 (54.6%) | 181 (79.7%) | ||
| Average OB surgeries/wk | 38.6 | 40.9 |
CI = confidence interval; COVID-19 = coronavirus disease 2019; ED = emergency department; GYN = gynecology; OB = obstetric.
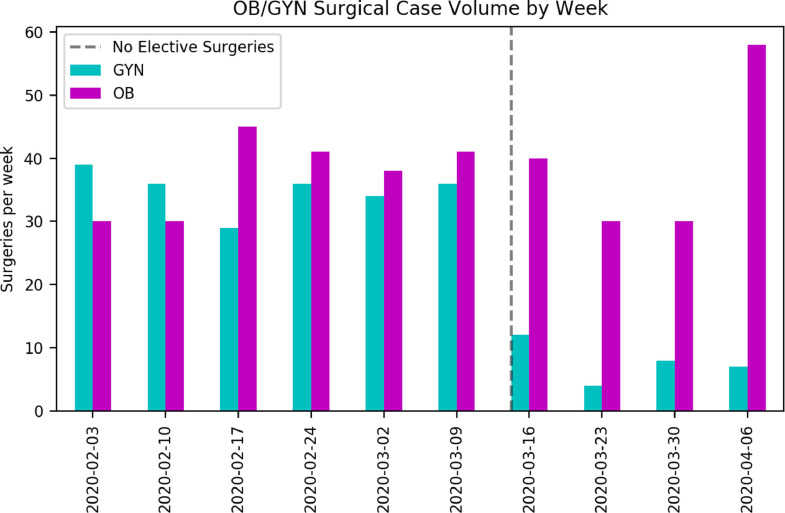
Regarding GYN surgeries, there was a significant decrease in surgical volume when comparing the pre–COVID-19 group with the COVID-19 group. There were 212 GYN cases performed during the pre–COVID-19 time frame with an average of 34.8 surgeries per week vs only 79 GYN cases in the COVID-19 period with an average of 7.2 surgeries per week, demonstrating a 79.3% decrease in GYN surgical volume (Fig. 2 ; Table 5). When comparing pre–COVID-19 time frames with COVID-19 time frames, the proportions of GYN surgeries to all surgeries were 13.8% and 21.3%, respectively, which was not significant (p = .310) (Table 5). The distribution of cases performed by benign GYN surgeons vs GYN oncologists was comparable between the pre–COVID-19 and COVID-19 periods; however, a significant difference was noted in the case acuity between groups (Table 2). In comparing scheduled with emergent cases, there was a greater proportion of emergent cases performed in the COVID-19 time frame with an increase in emergency surgeries from 11.8% to 37.5% (p <.01) (Table 2). The distribution of surgical approach demonstrated a significant change (p = .022), consistent with the types of surgeries that were being performed or deferred during the COVID-19 period, with a smaller proportion of diagnostic hysteroscopies for postmenopausal bleeding or polypectomies/myomectomies for abnormal uterine bleeding (16.0% pre–COVID-19 vs 3.1% COVID-19), fewer large abdominal incisions for open hysterectomies or myomectomies for enlarged myoma uteri (15.6% pre–COVID-19 vs 9.4% COVID-19), and a greater proportion of suction dilation and curettage's for hemorrhage during COVID-19 (9.9% vaginal procedures pre–COVID-19 vs 28.1% COVID-19) (Table 2).
Fig. 2.
This figure shows the total volume of OB-GYN surgeries per week over the course of the early coronavirus disease 2019 pandemic. The dotted line indicates the date of the mandated ban on elective cases. GYN = gynecology; OB = obstetric.
The breakdown of the case types for GYN surgeries is presented in Table 3. A significant difference was noted in the GYN surgery case types when comparing pre–COVID-19 and COVID-19 cases (p <.001). There were increases in proportions for concern for cancer (from 23.6% to 37.5%), ectopic pregnancy (from 5.7% to 18.8%), and spontaneous abortions (from 1.4% to 12.5%), respectively, whereas there were decreases in proportions for surgeries for myomas (from 21.2% to 0%), endometriosis (from 7.1% to 0%), and pelvic organ prolapse/incontinence (from 6.6% to 0%), respectively (Table 3).
OB surgical volume remained unchanged in the pre–COVID-19 and COVID-19 groups with 237 OB surgeries in the pre–COVID-19 time frame with an average of 38.6 cases per week vs 181 cases in the COVID-19 time period with an average of 40.9 cases per week. Fig. 2 shows that whereas the volume of OB surgeries remained relatively constant over the course of the early pandemic, the GYN surgical volume drastically decreased as outlined in earlier text. When comparing pre–COVID-19 time frames with COVID-19 time frames, the proportions of OB surgeries to all patients in labor and delivery were 54.6% vs 79.7%, which was a significant increase (p = .002) (Table 5). Table 3 demonstrates that there was a comparable breakdown in the case types among the OB surgeries with no significant differences noted between the pre–COVID-19 and COVID-19 groups (p = .366).
Finally, GYN surgeries were analyzed by the ACGME categories for resident surgical training [5]. In each category, there was a notable decrease in the number of cases performed pre–COVID-19 and COVID-19 periods (Table 6 ).
Table 6.
ACGME graduation surgical case requirements for OB-GYN residency training
| Cases | Pre–COVID-19 | COVID-19 | Minimum cases required for graduation*[4] |
|---|---|---|---|
| GYN | |||
| Hysterectomy, total | 62 | 10 | 85 |
| Minimally invasive hysterectomy | 38 | 5 | 70 |
| Abdominal hysterectomy† | 24 | 5 | 15 |
| Hysteroscopy | 43 | 1 | 40 |
| Laparoscopy | 66 | 14 | 60 |
| Surgery for invasive cancer | 57 | 12 | 25 |
| Incontinence and pelvic floor procedures | 15 | 0 | 25 |
| OB | |||
| Cesarean section | 211 | 164 | 145 |
ACGME = Accreditation Council for Graduate Medical Education; COVID-19 = coronavirus disease 2019; GYN = gynecology; OB = obstetric.
Vaginal deliveries, abortions, cystoscopy, and ultrasound procedures were not included in this table as they were not specifically addressed in this study.
Abdominal hysterectomy includes cesarean hysterectomies.
Discussion
The COVID-19 pandemic has had a devastating impact on our community. As of August 25, 2020, there have been more than 176 000 deaths and 5.7 million individuals diagnosed with COVID-19 in the United States [6]. In the wake of this pandemic, hospitals have encountered new challenges with an increase in high-acuity patient admissions, scarce resources, and a significant change in practice patterns. Early in the pandemic, hospitals combated these issues by postponing all elective procedures, making operating rooms readily available to be transformed into intensive care units and preserving personal protective equipment. These changes, among other factors, have altered the way patients access and receive care. Presented in this study were observations from a hospital in New York during the peak of the COVID-19 pandemic in our area, which may not be immediately generalizable to the United States population but may inform anticipated changes as the pandemic continues to spike across the country.
While the pandemic continues to affect the United States, some suspect that many are suffering at home of causes unrelated to COVID-19 [7], and physicians across the country are reporting decreases in patients in EDs for other emergency medical conditions, prompting the recent New York Times article, “Where Have All the Heart Attacks Gone?” [8]. A correspondence in the New England Journal noted a decrease in hospitalizations of patients with myocardial infarction during the COVID-19 pandemic in the California Kaiser Permanente system [9]. Similar observations have been made abroad in Spain, China, and Italy noting fewer emergency procedures performed for conditions such as myocardial infarction and patients presenting later in their course during the pandemic 10, 11, 12.
Our study showed a 60% decrease in OB-GYN ED consults during the pandemic (Fig. 1; Table 5), similarly raising concerns about where patients with urgent OB-GYN conditions have gone. Although our overall OB-GYN ED consult volume decreased, the percentage of patients in the ED needing OB-GYN consults remained unchanged, suggesting the decreased OB-GYN ED consult volume reflects a total decrease in ED patient volume. Furthermore, among the patients with OB-GYN ED consults, the hospital admission, blood transfusion, or emergent surgery rates stayed relatively similar (Table 1). It is difficult to determine whether the decreased ED volume reflects the volume of “true emergencies” in which ED resources are being appropriately used vs a decreased clinical volume owing to patients fleeing New York to seek care elsewhere. In the previous scenario, wherein patients choose to stay home, either as a result of public directives to shelter in place or the fear of contracting the illness, patients may be appropriately managing nonurgent issues by turning to non-ED options, such as telehealth services that have become more readily available for patients who are insured [13]. In our institution telehealth has been rapidly adopted with approximately half of outpatient visits transitioned to telehealth during the pandemic. Patients may also be choosing hospitals less publicly associated with COVID-19 such as ours. We suspect the decreased ED volume is a combination of both scenarios.
Regarding surgical volume, OB surgical volume remained relatively unchanged during the pandemic as obstetric care cannot be deferred, whereas GYN surgical volume decreased by 80% (Fig. 2; Table 5). A significant portion of the family planning and infertility procedures at our institution are performed at satellite hospitals and were not included in our study owing to limitations of data extraction. This may have underestimated the decline in surgical volume. In addition, the COVID-19 pandemic affected the type of GYN cases being performed with marked growth in the proportion of emergency cases. Surgeries performed for common indications such as myomas or incontinence became almost nonexistent. (Table 3).
Although the moratorium on elective procedures was necessary, we fear the profound impact it may have had. Even “elective” GYN surgeries remain medically indicated to address symptoms such as pain and bleeding that may interfere with one's daily function or to prevent serious medical sequelae such as severe anemia requiring transfusion. In addition, patients awaiting infertility treatments experience a distinct loss and anxiety [14,15]. As we prepare for judicious reopening of our operating rooms, we must prioritize carefully. Patients may have greater pain, worse anemia, and/or more advanced pathology as a result of deferred care. As the pandemic lingers or we confront a second wave, we must continue to be thoughtful about the allocation of resources and remain vigilant not to delay originally elective cases that could progress to more urgent conditions with time.
Finally, we must consider the impact of COVID-19 on resident and fellow training. Consolidated and telehealth clinics sometimes no longer involve residents, and there are fewer inpatients and consults. Residents may be redeployed to work in emergency departments or intensive care units. Overall specialty-specific training has decreased domestically and internationally and across specialties 16, 17, 18, 19. GYN surgical volume across the country had already been declining [20,21] and has now plummeted. The ACGME has assured residents that case logs will be evaluated judiciously considering the pandemic [22]. Yet, the fact remains that trainees will graduate with less surgical experience. Educators must prioritize creative solutions to increase surgical exposure, increase simulation time, and make concerted efforts, with revamped schedules and clinical coverage models, to increase trainee time in the operating room.
The long-term effects of the COVID-19 pandemic are yet to be fully understood; however, the short-term findings illustrate an overall decrease in consults for emergency care and a marked reduction in patients receiving surgical care. As we continue to battle COVID-19, we must not lose sight of those patients whose care has been deferred, those who may be too afraid to seek care, and the trainees who care for them.
Footnotes
The authors declare that they have no conflict of interest.
An abstract of this manuscript was accepted for presentation at American Association of Gynecologic Laparoscopists Global Congress November 6–14, 2020.
This study was approved by the institutional review board (AAAS9860) of Columbia University Irving Medical Center on March 27, 2020 and was granted a waiver of consent.
To protect patient confidentiality, the data generated and/or reviewed during the above publication are not publicly available but available from the corresponding author by reasonable request.
References
- 1.New York State. Governor Cuomo issues statement regarding novel coronavirus in New York. Available at: https://www.governor.ny.gov/news/governor-cuomo-issues-statement-regarding-novel-coronavirus-new-york. Accessed May 23, 2020.
- 2.Center for Disease Control and Prevention. Interim guidance for healthcare facilities: preparing for community transmission of COVID-19 in the United States. Available at: https://stacks.cdc.gov/view/cdc/85502. Accessed April 27, 2020.
- 3.American College of Obstetricians and Gynecologists. Joint statement on elective surgeries. Available at:https://www.acog.org/news/news-releases/2020/03/joint-statement-on-elective-surgeries. Accessed April 27, 2020.
- 4.Center for Disease Control and Prevention. Coronavirus disease 2019: what to do if you are sick. Available at: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/steps-when-sick.html. Accessed May 4, 2020.
- 5.Accreditation Council for Graduate Medical Education. Case log information: obstetrics and gynecology. Available at: https://www.acgme.org/Portals/0/PFAssets/ProgramResources/OBGYNCaseLogInfo.pdf?ver=2020-11-20-163905-143. Accessed December 7, 2020.
- 6.Center for DiseaseControl and Prevention. Coronavirus disease 2019: United States COVID-19 cases and deaths by state. Available at:https://www.cdc.gov/coronavirus/2019-ncov/cases-updates/cases-in-us.html. Accessed August 25, 2020.
- 7.Hermann P. More people in district dying outside of hospitals during pandemic. Washington Post. Available at:https://www.washingtonpost.com/local/more-people-in-district-dying-outside-of-hospitals-during-pandemic/2020/05/04/cd6e7ea6-8cdf-11ea-8ac1-bfb250876b7a_story.html. Accessed May 5, 2020.
- 8.Krumholz HM. Where have all the heart attacks gone? New York Times. Available at:https://www.nytimes.com/2020/04/06/well/live/coronavirus-doctors-hospitals-emergency-care-heart-attack-stroke.html?searchResultPosition=1. Accessed May 4, 2020.
- 9.Solomon MD, McNulty EJ, Rana JS. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383:691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 10.De Filippo O, D'Ascenzo F, Angelini F. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383:88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rodriguez-Leor O, Cid-Alvarez B, Ojeda S. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol. 2020;2:82–89. [Google Scholar]
- 12.Tam CF, Cheung KS, Lam S. Impact of COVID-19 outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13 doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hollander JE, Carr BG. Virtually perfect? Telemedicine for Covid-19. N Engl J Med. 2020;382:1679–1681. doi: 10.1056/NEJMp2003539. [DOI] [PubMed] [Google Scholar]
- 14.Turocy JM, Robles A, Hercz D, D'Alton M, Forman EJ, Williams Z. The emotional impact of the ASRM guidelines on fertility patients during the COVID-19 pandemic. Fertil==76== Steril. 2020;114:E63. [Google Scholar]
- 15.Greater New York Hospital Association. DOH guidance on essential COVID-19 sexual and reproductive health services. Available at: https://www.gnyha.org/news/doh-guidance-on-essential-covid-19-sexual-and-reproductive-health-services/. Accessed May 4, 2020.
- 16.Amparore D, Claps F, Cacciamani GE. Impact of the COVID-19 pandemic on urology residency training in Italy. Minerva Urol Nefrol. 2020;72:505–509. doi: 10.23736/S0393-2249.20.03868-0. [DOI] [PubMed] [Google Scholar]
- 17.Bambakidis NC, Tomei KL. Editorial. Impact of COVID-19 on neurosurgery resident training and education. J Neurosurg. 2020 Apr 17 doi: 10.3171/2020.3.JNS20965. [Epub ahead of Print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Crosby DL, Sharma A. Insights on otolaryngology residency training during the COVID-19 pandemic. Otolaryngol Head Neck Surg. 2020;163:38–41. doi: 10.1177/0194599820922502. [DOI] [PubMed] [Google Scholar]
- 19.Liang ZC, Ooi SBS, Wang W. Pandemics and their impact on medical training: lessons from Singapore. Acad Med. 2020;95:1359–1361. doi: 10.1097/ACM.0000000000003441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hall EF, Raker CA, Hampton BS. Variability in gynecologic case volume of obstetrician-gynecologist residents graduating from 2009 to 2017. Am J Obstet Gynecol. 2020;222 doi: 10.1016/j.ajog.2019.11.1258. 617.e1–617.e8. [DOI] [PubMed] [Google Scholar]
- 21.Wright JD, Herzog TJ, Tsui J. Nationwide trends in the performance of inpatient hysterectomy in the United States. Obstet Gynecol. 2013;122:233–241. doi: 10.1097/AOG.0b013e318299a6cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Accreditation Council for Graduate Medical Education. ACGME response to the coronavirus (COVID-19). Available at:https://www.acgme.org/Newsroom/Newsroom-Details/articleId/10111. Accessed May 4, 2020.