Highlights
-
•
This study examines the impact of COVID-19 on ERP outcome.
-
•
Rates of improvement that would be anticipated outside of a pandemic were attenuated during COVID-19.
-
•
Patients who endured financial distress or were medically at-risk had worse ERP outcomes.
-
•
Patients who were children or who had higher baseline doubt/uncertainty fared better in ERP during COVID-19 than adults on average or those with lower levels of doubt/uncertainity.
Keywords: Obsessive-compulsive disorder, Exposure and response prevention, Cognitive behavioral therapy, COVID-19, Pandemic, Yale-Brown obsessive-compulsive scale, Treatment
Abstract
The COVID-19 pandemic has created novel mental health challenges for those with pre-existing problems including obsessive-compulsive disorder (OCD). Our study reports on clinician perceptions regarding the effect of the COVID-19 pandemic on patients with OCD receiving exposure and response prevention treatment (ERP) prior to and during the pandemic. Participating clinicians completed a survey which included questions adapted from National Institute of Mental Health-Global Obsessive-Compulsive Scale (NIMH-GOCS) and Yale-Brown Obsessive-Compulsive Scale (Y-BOCS). Clinicians rated clinical features at treatment initiation, just prior to the pandemic, and mid-pandemic (July/August, 2020). Findings suggest that the COVID-19 pandemic was associated with attenuation of ERP progress from expected rates in most patients during first several months of the pandemic; clinicians estimated that 38% of their patients had symptoms worsen during the pandemic and 47% estimated that symptoms remained unchanged despite participating in ERP. Those who endured financial distress or were medically at-risk for severe COVID-19 disease had worse ERP course. Adults also had a worse ERP course during than pandemic than youth. Further research is needed to better understand the effect of the COVID-19 pandemic on OCD symptomatology and treatment trajectory post-pandemic.
1. Introduction
The novel SARS-CoV-2 coronavirus (and its clinical syndrome, COVID-19) has created lasting social, medical, and psychological consequences since its emergence in December 2019 (Lu et al., 2020). Individuals have taken measures to protect themselves by adhering to official safety guidelines outlined by governmental and public health bodies, which include social distancing, wearing face masks, practicing appropriate hygiene, and maintaining other preventative behaviors (CDC, 2020). Beyond its medical morbidities, the COVID-19 pandemic presents additional challenges for mental health. The pandemic has been associated with worsened mental health for those with pre-existing problems as well as new-onset mental health concerns (Asmundson et al., 2020; Haider et al., 2020; Plunkett et al., 2020).
The impact of psychosocial stressors on mental health problems during the COVID-19 pandemic is becoming better understood. The pandemic has been directly associated with psychological distress among the general population across numerous reports (e.g., (González-Sanguino et al., 2020; Moccia et al., 2020; Sønderskov et al., 2020; Wang et al., 2020b). People who lost jobs are among those who have suffered the strongest negative psychological impacts (Rodríguez-Rey et al., 2020), and concerns about employment and the economy have caused anxiety and uncertainty (Spoorthy et al., 2020). Those working in occupations with high-risk exposure, such as healthcare workers, are enduring increased levels of mental health concerns (Spoorthy et al., 2020).
While the consequences of the COVID-19 pandemic for general mental health are clear (Steardo et al., 2020), there has been particular interest in the potential effect of the pandemic on obsessive-compulsive disorder (OCD). Given how OCD may interact with pandemic-related fears, as well as substantial symptom heterogeneity (Thorsen et al., 2018), it is important to determine whether particular OCD clinical characteristics may be associated with worse mental health outcomes (Schneider et al., 2020). Concerns about harm to self or others and a heightened propensity towards disgust may result in excessive washing and cleaning in many with OCD (Akhtar et al., 1975; Cervin et al., 2020; Khanna et al., 1990; Wheaton et al., 2010). Indeed, fears of contamination and excessive washing or cleaning are among the most prevalent symptoms among individuals with OCD (Abramowitz et al., 2010). OCD is also associated with intolerance of uncertainty and an inflated sense of responsibility to prevent harm (Britton and Davey, 2017; Obsessive Compulsive Cognitions Working Group, 2005). As the COVID-19 pandemic has seen widespread calls for increased responsibility for each individual to keep oneself and others safe and increased cleaning behaviors, as well as ambiguity regarding the scope and impact of the disease, it is reasonable to expect that individuals with OCD may be at particularly high risk for adverse mental health consequences during the pandemic. Accordingly, the COVID-19 pandemic has been associated with worsening of OCD symptoms (Benatti et al., 2020; Davide et al., 2020; French and Lyne, 2020; Matsunaga et al., 2020; Tanir et al., 2020) as well as relapse from previously well-controlled OCD (Jassi et al., 2020; Kumar and Somani, 2020).
What remains unclear is the extent to which patients in active exposure and response prevention therapy (ERP) are progressing in treatment during the COVID-19 pandemic and, if so, whether this progress is impacted as a function of various clinical factors. Exposure and response prevention is the first line treatment of adults and children with OCD, demonstrating high acceptability (Lewin et al., 2014), low dropout rates (Johnco et al., 2020), large effect sizes relative to psychotherapy and placebo control conditions (McGuire et al., 2015; Skapinakis et al., 2016), and superiority to antidepressant medication monotherapy (Foa et al., 2005). There is value to examining both OCD-specific and COVID-specific predictors of ERP outcomes to better understand prognosis and treatment tailoring variables. Outside of the COVID-19 pandemic, several variables have been demonstrated to predict ERP outcome, including higher severity of OCD and depression (Denys et al., 2003; Mataix-Cols et al., 2002; Tibi et al., 2019; Kyrios et al., 2015; Hamatani et al., 2020; Ong et al., 2016), family accommodation (Garcia et al., 2010; Merlo et al., 2009), and poor insight (Nissen and Parner, 2018; Selles et al., 2020).
To date, no research has examined the impact of the COVID-19 pandemic on ERP outcomes for individuals with OCD, nor has any study explored potential predictors of outcomes. Therefore, the aim of this study was to evaluate clinicians’ perspectives regarding the impact of the COVID-19 pandemic on individuals with OCD receiving ERP under their care prior to and during the pandemic. On the basis of reports of worsening OCD during the pandemic as well as clinical experience, we predicted that OCD symptomatology would decrease from the start of ERP to pre-COVID-19; thereafter, we predicted that the trajectory of symptom improvement would flatten throughout the pandemic. Based on past findings regarding predictors of ERP outcome, we also predicted that the trajectory of outcomes would be different for those with poor insight (versus with good/excellent insight; Nissen and Parner, 2018; Selles et al., 2020) and greater pathological doubt (versus mild doubt; Kyrios et al., 2015; Martinelli et al., 2014). While primary contamination symptoms is not typically associated with attenuated outcome to ERP (Keeley et al., 2008; Storch et al., 2008), we explored if this factor may be predictive of outcome given that COVID-19 has exacerbated these symptoms among many individuals with OCD (Knowles et al., 2021). Finally, although few data have been reported regarding the impact of stressors on ERP outcome in those with OCD, some studies have documented that psychosocial stressors predict sustained or worsened OCD severity (Lin et al., 2007; Marquett et al., 2013). Accordingly, we predicted that elevated COVID-19-related life stressors, including financial stress, close contact with someone diagnosed with COVID-19, high-risk occupations, and the presence of high-risk medical comorbidities, would predict less positive ERP outcome.
2. Methods
2.1. Participants
This online survey was conducted from July 19 to August 2, 2020 using the Qualtrics survey platform (Seattle, WA). The survey was sent electronically over email to 595 clinicians who were registered in the International OCD Foundation (IOCDF) database from 2017-2018 and who regularly provide CBT to adults and children with OCD and anxiety.
The Institutional Review Board at Baylor College of Medicine approved the study protocol and procedures of informed consent before the survey's distribution. In the first page of the survey, participants were informed that their participation was completely voluntary and that their responses would be kept confidential. After reviewing the first page and providing consent, participants were directed to proceed to the second page to begin the survey.
2.2. Measures
Following the consent page, the questionnaire consisted of four sections: clinician demographics, client demographic characteristics, client clinical characteristics, and qualitative descriptions of client well-being. Each clinician was prompted to provide information for one to five patients who had begun treatment for OCD prior to the pandemic and are still receiving care. The clinician was instructed to think back to the most recent patients s/he has seen that fit this description. Clinicians were then asked to rate a series of questions described below based on their current understanding of the patient. A subset of clinician respondents (n = 50) were also asked about changes to frequency of therapy during the pandemic.
The demographic information collected about the clinicians themselves included gender, age, ethnicity/race, current status of mental health work (active/inactive), country of practice, student or trainee status, profession of employment or training (psychiatrist, psychologist, psychotherapist, etc.), and the number of patients with OCD whom they were actively treating at the time of the survey. Clinicians were also asked to report client demographic information, including age, gender, highest level of education, and employment status. Clinicians also reported any known psychiatric comorbidities in these patients.
To estimate the overall impact of the COVID-19 pandemic on OCD symptoms, clinicians were first each asked to estimate what percentage of their patients had symptoms: 1) worsen, 2) stay the same, or 3) improve since the COVID-19 pandemic began. Other questions in this portion of the survey were adapted from two validated scales to assess client clinical characteristics: National Institute of Mental Health-Global Obsessive-Compulsive Scale (NIMH-GOCS; Insel et al., 1983) and Yale-Brown Obsessive-Compulsive Scale (Y-BOCS; Goodman et al., 1989a, 1989b). For each of these ratings, clinicians were prompted to rate their patients’ symptoms: 1) at the beginning of treatment, 2) just prior to the pandemic, and 3) currently (i.e., at the time of the survey [July 17-August 4, 2020]).
The NIMH-GOCS is a single-item rating on a scale of 1 (minimal symptoms) to 15 (very severe) to evaluate the severity of OCD, with severity levels grouped into 5 categories that include: minimal severity (1-3), subclinical severity (4-6), clinical severity (7-9), severe clinical severity (10-12), and very severe clinical severity (13-15). In prior studies, NIMH-GOCS illustrated good short-term test-retest reliability (r = 0.87-0.98; Kim et al., 1992), excellent interrater reliability (ICC = 0.77-0.95; Kim et al., 1992), good convergent validity with other OCD severity measures (r = 0.63-0.77; Kim et al., 1992), and demonstrated treatment sensitivity (Flament et al., 1985; Insel et al., 1983).
The Y-BOCS is regarded as the gold standard assessment of OCD symptom severity, with well-established psychometric properties (Storch et al., 2010). We adapted 3 questions from the Y-BOCS and asked clinicians to assess each client's insight, pathological doubt/uncertainty, and sense of over-responsibility. Next, clinicians were asked to assess to what degree a client's family members accommodate his/her compulsive behaviors. Please see Supplement 1 for more details about the survey and the items adapted from the Y-BOCS.
2.3. Statistical analysis
A mixed within-between analysis of variance (ANOVA) was conducted to evaluated GOCS scores 1) at the beginning of treatment, 2) immediately prior to the pandemic, and 3) currently (i.e. at the time the survey was completed [July 17-August 4, 2020]). Linear and quadratic effects of time were evaluated to test the hypotheses that OCD symptoms would decrease overall from pretreatment (i.e. a significant negative linear effect) but maintain since immediately prior to the pandemic (i.e. reflected in a positive quadratic effect).
The model also tested a number of predictors of change in NIMH-GOCS scores. The interactions between each variable and the linear and quadratic effect of time were analyzed to evaluate how COVID-19-specific and pretreatment clinical variables impacted the trajectory of symptoms. COVID-19-specific variables included those described above (i.e. family/close contact diagnosed/treated, financial impact, at-risk medically, and at-risk occupation) and were included on the basis of emerging literature documenting the adverse impact of these variables on mental health during the pandemic. Pretreatment ratings of clinical variables hypothesized to be related to poorer outcomes during the pandemic included: insight, doubt/uncertainty, over-responsibility, family accommodation, and comorbid depression. A power analysis was conducted to determine adequate sample size to detect a significant difference if effect sizes were small (f = .141) or medium (f = .387) between comparison groups (e.g., those with or without financial impact, contamination symptoms, etc.) (Cohen, 1992), assuming power of .8 and α = .05. To evaluate a medium effect, a sample size of 34 was needed; to detect significant differences for a small effect, a sample size of 238 was needed.
3. Results
3.1. Participant information
Two-hundred twenty-seven people opened the survey and began completing it. Among those, 169 completed at least some information about at least one client. Of those 169, 137 (81%) provided complete clinical ratings for at least one of their patients (e.g., OCD severity, family accommodation, insight, etc.). Most respondents provided ratings for one client, with a maximum of five patients reported on from each participant. Respondents provided at least some demographic information about a total of 269 patients with OCD. Of those, 232 (86%) had complete clinical ratings, and 236 had at least partial clinical ratings completed (e.g., completed NIMH-GOCS but did not complete other ratings). Because only four patients (1%) had partial data completed, it was decided to conduct analyses with complete data only (n = 232). Thus, the final sample size was powered to detect most small predictor effects (target sample size for small effect detection of n = 238). No significant differences in NIMH-GOCS ratings or other clinical variables were found between respondents who rated only one client and those who rated more than one client (p > .16 for all comparisons).
See Table 1 for complete clinician and client demographic information. In summary, the majority of clinicians identified as female (77%), white (85%), and psychologists (78%). The mean number of adult patients with OCD whom clinicians were treating was 11.5 (19.3), and the mean number of child/adolescent patients with OCD was 4.9 (7.7). Approximately half of patients were reported to be female (51%), and over half had at least an undergraduate degree (38% college degree, 17% postgraduate). Forty-one percent were students, and the average age was 28.5 years, with a range from 4-77 years.
Table 1.
Demographics.
| Clinician (respondent) information (n=137) | Reported patient information (n=232) | ||
|---|---|---|---|
| Gender N (%) | Gender N (%) | ||
| Male | 30 (22%) | Male | 108 (47%) |
| Female | 106 (77%) | Female | 118 (51%) |
| Other | 1 (1%) | Other | 6 (3%) |
| Hispanic or Latino/a ethnicity N (%) | 9 (7%) | Education N (%) | |
| Race N (%) | Elementary/middle school | 25 (11%) | |
| East Asian | 5 (4%) | High school or some college | 78 (34%) |
| South Asian or Indian-American | 3 (2%) | College degree (associate's, bachelor's, etc.) | 87 (38%) |
| Middle Eastern or North African | 2 (2%) | Postgraduate degree | 39 (17%) |
| White | 117 (85%) | Other | 3 (1%) |
| Other | 5 (4%) | Employment N (%) | |
| Multiracial | 6 (4%) | Student | 94 (41%) |
| Student or trainee N (%) | Part-time employed | 26 (11%) | |
| Yes | 7 (5%) | Full-time employed | 72 (31%) |
| No | 130 (95%) | Unemployed or not working | 32 (14%) |
| Profession N (%) | Stay-at-home parent | 6 (3%) | |
| Psychiatrist | 8 (6%) | Not applicable or unsure | 2 (1%) |
| Age M (range) | 28.5 (4-77) | ||
| Psychologist | 107 (78%) | Contamination symptoms N (%) | 131 (57%) |
| Psychotherapist (Social worker, counselor, marriage/family therapist) | 20 (15%) | Comorbidity N (%) | |
| Other | 2 (2%) | Anxiety disorder | 110 (48%) |
| Age M (range) | 44.4 (23-73) | Depressive disorder | 75 (32%) |
| Number of adult OCD patients M (SD) | 11.5 (19.3) | COVID-19 impact N (%) | |
| Number of youth OCD patients M (SD) | 4.9 (7.7) | Family member or close contact diagnosed with of treated for COVID-19 | 19 (8%) |
| COVID-19 began impacting region N (%) | Adverse financial impact (reduced work or financial pressure) | 36 (16%) | |
| January, 2020 | 2 (2%) | At-risk for severe COVID-19 illness | 21 (9%) |
| February, 2020 | 5 (4%) | At-risk occupation (e.g., healthcare, transportation) | 19 (8%) |
| March, 2020 | 118 (86%) | ||
| April, 2020 | 7 (5%) | ||
| May, 2020 | 1 (1%) | ||
| June, 2020 | 4 (3%) | ||
3.2. Change in OCD severity
Each clinician was prompted to provide an estimation of the percentage of patients with OCD they have seen whose symptoms had worsened, improved, or stayed the same. When averaging these estimations, it was found that clinicians estimated that 38% of their patients had symptoms worsen due to the COVID-19 pandemic (SD=30.4), 47% had symptoms stay the same (SD=31.8), and 10% had symptoms improve (SD=16.2). Of the subset of clinician respondents (n = 50) who were also asked about changes to frequency of therapy during the pandemic, 14% described less frequent treatment, 62% described no change in treatment frequency, 12% described more frequent treatment, and 12% reinitiated treatment.
The between-within ANOVA showed a significant multivariate effect of time on NIMH-GOCS scores, F (2, 220) = 7.37, p = .001, η2partial = .063. Mauchly's test of sphericity was significant, W (2) = .96, p = .009, and thus Greenhouse-Geisser corrections to main effects were used. A significant overall within-subjects effect of time was observed. Inspection of contrasts showed a significant linear effect, F (1) = 4.00, p = .047, η2partial = .02, though the quadratic effect was not significant, F (1) = 3.01, p = .080, η2partial = .01. Mean and standard deviations of NIMH-GOCS across time; NIMH-GOCSpretreatment = 9.39 (2.52), NIMH-GOCSCOVID-start = 6.86 (2.42), NIMH-GOCScurrent = 7.12 (3.02). Although this appears to reflect a linear and quadratic effect (i.e., slightly higher GOCS scores at the end point), this effect was not significant when controlling for other variables in the multivariate model. See a summary of multivariate effects in Table 2 , as well as predictor effects in Table 3 .
Table 2.
Multivariate effects of model predicting OCD severity.
| F | P | η2partial | |
|---|---|---|---|
| Main effects of time | 3.43 | 0.034 | 0.030 |
| COVID-19-specific factors | |||
| Family/close contact impact | 0.74 | 0.48 | 0.007 |
| Medically at risk | 3.53 | 0.031 | 0.031 |
| Occupationally at risk | 0.28 | 0.76 | 0.003 |
| Financial impact | 5.97 | 0.003 | 0.052 |
| Demographic/clinical factors | |||
| Comorbid depression | 0.77 | 0.46 | 0.007 |
| Age (adult vs. youth) | 4.80 | 0.009 | 0.042 |
| Insight | 1.10 | 0.33 | 0.010 |
| Doubt/uncertainty | 10.16 | <0.001 | 0.085 |
| Inflated perceptions of responsibility | 1.26 | 0.29 | 0.011 |
| Family accommodation | 2.26 | 0.11 | 0.020 |
| Contamination symptoms | 1.43 | 0.24 | 0.013 |
Note: OCD=Obsessive-compulsive disorder. Obsessive-compulsive disorder symptom severity was assessed with the Global Obsessive-Compulsive Scale. Family/close contact impact indicated that a family member or close contact (friend, colleague) of the client has been diagnosed with or treated for COVID-19. “Medically at risk” represented individuals who were at significant risk for severe COVID-19 illness (e.g., immunocompromised, chronic medical conditions, pregnant). “Occupationally at risk” represented individuals whose occupation involved significant risk of COVID-19 exposure (e.g., healthcare, transportation). Individuals were classified as experiencing financial impact if they 1) became unemployed or furloughed as a result of the COVID-19 pandemic, or 2) experienced significant new or worsened financial pressure related to the pandemic.
Table 3.
Linear and quadratic predictor effects.
| F | P | η2partial | |
|---|---|---|---|
| Time | |||
| Linear | 4.00 | 0.047 | 0.018 |
| Quadratic | 3.09 | 0.080 | 0.014 |
| COVID-19-specific factors | |||
| Family/close contact impact- linear | 0.38 | 0.54 | 0.002 |
| Family/close contact impact- quadratic | 0.20 | 0.66 | 0.001 |
| Medically at risk- linear | 2.30 | 0.13 | 0.010 |
| Medically at risk- quadratic | 4.99 | 0.027 | 0.022 |
| Occupationally at risk- linear | 0.93 | 0.33 | 0.004 |
| Occupationally at risk- quadratic | 0.50 | 0.48 | 0.002 |
| Financial impact- linear | 11.04 | 0.001 | 0.048 |
| Financial impact- quadratic | 1.17 | 0.28 | 0.005 |
| Demographic/clinical factors | |||
| Comorbid depression- linear | 0.0095 | 0.92 | 0.000 |
| Comorbid depression- quadratic | 1.55 | 0.21 | 0.007 |
| Age (adult vs. youth)- linear | 5.92 | 0.016 | 0.26 |
| Age (adult vs. youth)- quadratic | 4.01 | 0.046 | 0.018 |
| Insight- linear | 0.40 | 0.53 | 0.002 |
| Insight- quadratic | 1.87 | 0.17 | 0.008 |
| Doubt/uncertainty- linear | 23.25 | 0.000 | 0.096 |
| Doubt/uncertainty- quadratic | 0.01 | 0.94 | 0.000 |
| Inflated perceptions of responsibility- linear | 1.29 | 0.26 | 0.006 |
| Inflated perceptions of responsibility- quadratic | 1.32 | 0.25 | 0.006 |
| Family accommodation- linear | 0.29 | 0.59 | 0.001 |
| Family accommodation- quadratic | 4.17 | 0.042 | 0.019 |
| Contamination symptoms- linear | 2.51 | 0.11 | 0.011 |
| Contamination symptoms- quadratic | 0.43 | 0.51 | 0.002 |
Note: OCD=Obsessive-compulsive disorder. Obsessive-compulsive disorder symptom severity was assessed with the Global Obsessive-Compulsive Scale. Family/close contact impact indicated that a family member or close contact (friend, colleague) of the client has been diagnosed with or treated for COVID-19. “Medically at risk” represented individuals who were at significant risk for severe COVID-19 illness (e.g., immunocompromised, chronic medical conditions, pregnant). “Occupationally at risk” represented individuals whose occupation involved significant risk of COVID-19 exposure (e.g., healthcare, transportation). Individuals were classified as experiencing financial impact if they 1) became unemployed or furloughed as a result of the COVID-19 pandemic, or 2) experienced significant new or worsened financial pressure related to the pandemic.
“Linear predictors” reflect the linear time*predictor interaction effect, while “quadratic predictors” reflect the linear.
3.3. Predictors of OCD trajectory during the pandemic
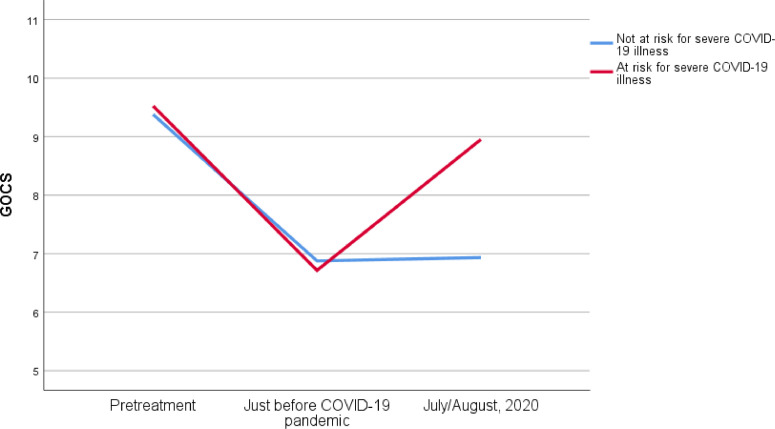
A summary of each predictor of linear and quadratic change in NIMH-GOCS is summarized in Table 3. The quadratic time*medically at-risk interaction was found to be significant; inspection of NIMH-GOCS scores among individuals who were and were not at medical risk showed that while individuals who were and were not at-risk did not appear to have different trajectories of improvement from pretreatment to just prior to the pandemic, the quadratic effect was much stronger among those who were at-risk, indicating a much more significant increase in OCD symptoms during the pandemic. In this group, symptoms were at similar levels pretreatment and currently. Please see Fig. 1 for a summary of NIMH-GOCS changes in those who were and were not at serious medical risk from COVID-19.
Fig. 1.
Course of OCD symptoms during COVID-19 pandemic among individuals who are medically at-risk for serious complications from COVID-19
Note: GOCS = Global Obsessive-Compulsive Scale. Examples of characteristics that would leave a client at risk for severe COVID-19 included being immunocompromised, having chronic medical conditions, or being pregnant.
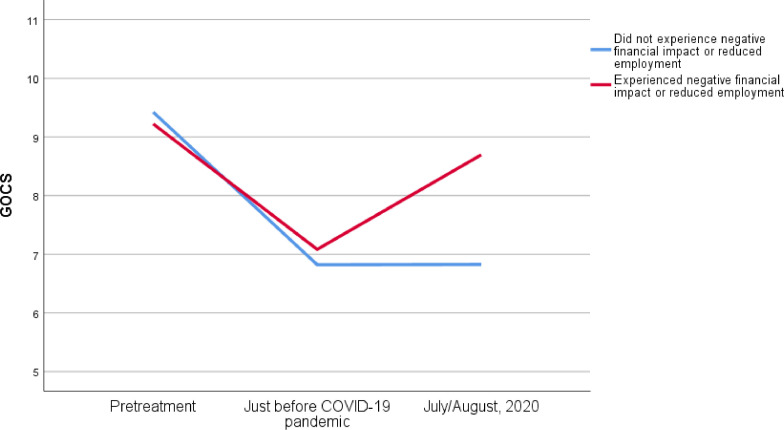
Significant linear time*financial impact and linear time*doubt/uncertainty interactions were also found. Specifically, those without financial impact from the COVID-19 pandemic showed a decline in GOCS scores from pretreatment to current, reflecting an improvement in OCD severity, while those with financial impacts showed minimal overall change, as presented in Fig. 2 . Further inspection of mean NIMH-GOCS scores showed similar improvements in OCD severity from pretreatment to just prior to the pandemic in both groups, though an increase in NIMH-GOCS scores was observed among those with increased financial strain or new unemployment, reflecting worsening OCD severity in this group. In contrast, individuals who did not experience financial impact showed relatively stable NIMH-GOCS from just prior to the pandemic to current (i.e. mid-pandemic).
Fig. 2.
Course of OCD symptoms during COVID-19 pandemic among individuals who experienced negative financial impact or reduced employment
Note: GOCS = Global Obsessive-Compulsive Scale.
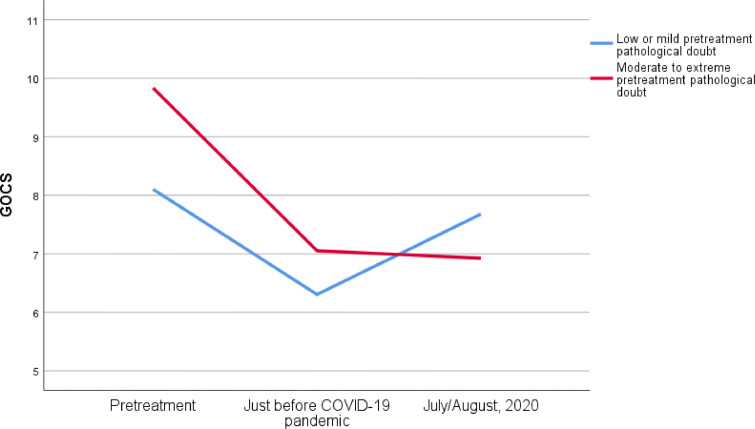
The pathological doubt*linear time interaction showed that those with more severe doubt/uncertainty issues experienced a decline in GOCS scores from pretreatment to current (i.e. mid-pandemic), whereas those with less severe doubt/uncertainty problems experienced less improvement. Further inspection showed that while those with more severe doubt symptoms had more severe OCD at baseline, symptoms declined from pretreatment to just prior to the pandemic and were maintained since then. Those without doubt issues also experienced improvements from pretreatment to just prior to the pandemic but experienced an increase in severity of symptoms since then. This interaction is displayed in Fig. 3 .
Fig. 3.
Course of OCD symptoms during COVID-19 pandemic among individuals with pathological doubt
Note: GOCS=Global Obsessive-Compulsive Scale.
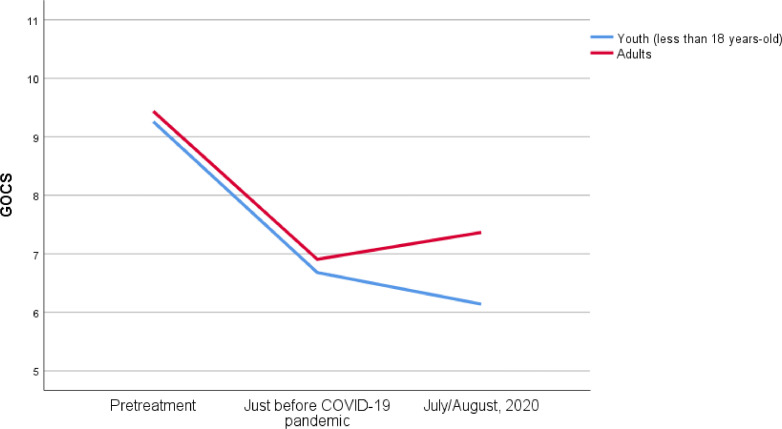
Age also showed significant linear and quadratic effects. Inspection of these interactions showed that both youth and adults experienced relatively similar symptom from pretreatment to immediately prior to the pandemic. From just prior to the pandemic to mid-pandemic, however, youth continued to show improvement in symptoms, while adults, on average, experienced a slight increase. See Fig. 4 for a depiction of this interaction.
Fig. 4.
Course of OCD symptoms during COVID-19 pandemic among youth and adults
Note: GOCS=Global Obsessive-Compulsive Scale.
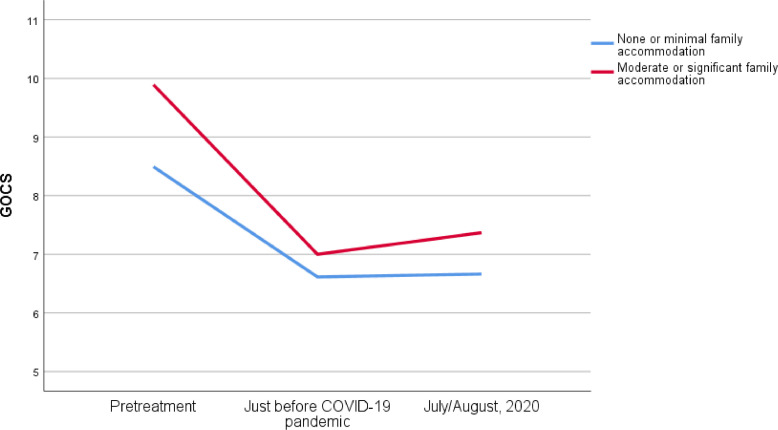
Finally, although family accommodation did not show a significant multivariate effect, the quadratic effect was positive and significant. Individuals with higher family accommodation had higher pretreatment symptoms, and subsequently experienced steeper initial improvement, followed by a steeper increase in symptom severity, reflected in a stronger positive quadratic effect. The linear effect was not significant. See Fig. 5 for a visual display of mean GOCS scores across follow among those with low and moderate-to-high family accommodation.
Fig. 5.
Course of OCD symptoms during COVID-19 pandemic with different levels of family accommodation
Note: GOCS=Global Obsessive-Compulsive Scale.
No other variables showed a significant impact on NIMH-GOCS trajectories during the pandemic, including clinical (inflated responsibility, depression, insight, contamination symptoms) and pandemic-specific factors (having a high-risk occupation and having family member or close contact with direct COVID-19 impact).
4. Discussion
We report on clinician perceptions of the impact of the COVID-19 pandemic on individuals with OCD receiving ERP prior to and during the pandemic. Overall, clinicians estimated that over one-third of their patients’ symptoms worsened during the initial period of the COVID-19 pandemic despite continuing in active treatment. Only 10% were reported to be doing better since the onset of the pandemic, while 47% remained stable. These findings suggest that the COVID-19 pandemic represents a significant stressor for most patients with OCD, exerting a deleterious effect on many. The overall stressful nature of the pandemic, which is well documented across individuals (Asmundson et al., 2020; Qiu et al., 2020; Wang et al., 2020a), may impact overall treatment progress, as one would expect higher rates of improvement during active treatment over this time interval in the absence of the pandemic. Results suggest that financial stress and being medically at-risk for significant complications from COVID-19 are two stressors that have been particularly detrimental for individuals with OCD in treatment. Findings also highlighted that progress in OCD treatment has been attenuated moreso in adults relative to youth. Although clinicians have articulated clear guidelines for conducting effective ERP via telehealth and with public health precautions in place (Fontenelle and Miguel, 2020; McKay et al., 2020; Storch et al., 2020), it is unclear to what extent telehealth delivery may also affect outcomes.
Across the sample as a whole, OCD symptoms were reported to improve from pretreatment to the time immediately prior to the onset of the COVID-19 pandemic. Thereafter, however, gains tended to level off, on average, and even worsened for some. Individuals with negative financial impacts from the COVID-19 pandemic and those at risk for serious medical complications from COVID-19 had increases in OCD severity since the beginning of the pandemic compared to those without these clinician-identified stressors whose symptom progress remained flat (on average). Both stressors may interfere with treatment provision (e.g., reduced access to sessions, less intense exposure tasks) or serve as a general stressor countering treatment progress. Indeed, economic anxiety is robust during the COVID-19 pandemic (Bareket-Bojmel et al., 2020), and those who lost jobs have suffered significant negative psychological impacts (Rodríguez-Rey et al., 2020). While ERP presents an ideal forum for addressing unrealistic fears in treatment, high levels of life stressors and practical barriers to treatment are expected to interfere with outcome.
Youth appear to have fared better in ERP during the pandemic relative to adults, with continued improvements in symptoms reported among children and adolescents. Although the pandemic has been a major stressor for youth as well as adults (Signh et al., 2020), it may be that the COVID-19 pandemic has brought more adjustment difficulties, such as trouble coping with social and academic changes, rather than OCD-specific stress. It is possible that stay-at-home orders allowed them youth to continue to focus on completing ERP exercises since they had fewer competing “extracurricular” activities during this time, especially during the first few months of the pandemic when activities were more stringently limited. Alternatively, youth may have had less exposure to real-world triggers (e.g., school stressors) during confinement. In contrast, adults may have had more competing occupational, family, child-educational duties, and financial tasks with which to cope.
Family accommodation has also played a role in the course of symptoms during the pandemic; individuals with higher family accommodation experienced steeper symptom improvement prior to the pandemic, followed by a slightly steeper increase in symptoms during the pandemic. This suggests that there may have been slightly more “bounce-back” in OCD severity among individuals with greater family accommodation during the pandemic, potentially due to more family interaction during stay-at-home orders. It is also worth noting the steeper decline prior to the pandemic for individuals with greater family accommodation, potentially due to greater statistical opportunity for change in this group, as individuals with greater family accommodation also began with higher OCD severity. This steeper pre-pandemic decline appeared to contribute more to the quadratic effect than post-pandemic symptom changes.
Unexpectedly, individuals who had more severe problems with doubt/uncertainty pretreatment fared better during the pandemic compared to those with lower levels of baseline doubt/uncertainty. One possibility is that these issues were addressed more directly in treatment before the pandemic, and thus these patients were better prepared to address the current circumstances (Satici et al., 2020). Another possibility is that COVID-19 represents a genuine threat and that the presence of such a real-world danger does not impact symptoms of pathological doubt/uncertainty.
There are several study limitations. First, we relied on retrospective clinician report rather than addressing patients directly in a prospective manner. The data reported reflects trajectories for individuals with OCD who continued to receive treatment during the COVID-19 pandemic; outcomes for those who terminated treatment may look very different. Second, our sample sizes for subgroup analyses were small. For example, we had n=21 for the “at-risk for severe COVID-19 illness” subgroup and n=36 for the “adverse financial impact” subgroup. Thus, the comparisons were based on unequal sample sizes and may have been biased due to the relatively smaller number of people endorsing these risk factors. Third, clinicians were sampled during the initial phase of the COVID-19 pandemic; it is unclear how findings will play out as the pandemic continues. Finally, clinicians possessed expertise in OCD treatment and were asked to select up to 5 patients (although most reported on 1); findings may not be representative of all OCD patients and/or those seen by this group of expert clinicians.
In summary, our study is one of the first reports to assess the impact of the COVID-19 pandemic on patients with OCD receiving ERP from the perspective of treating clinicians. Overall, progress in ERP seems to be attenuated from expected rates for most adult patients (but less so for youth) during the initial months of the pandemic. Results also suggest that the pandemic is associated with worsening of symptoms in patients who endured financial distress, who are medically at-risk, or had greater baseline family accommodation. Surprisingly, individuals with greater pretreatment doubt/uncertainty progressed more favorably in treatment during the pandemic, on average, compared with individuals with less pretreatment doubt/uncertainty issues. While this study represents an initial effort to understand the impact of the COVID-19 pandemic and associated stressors on ERP outcomes, further research is needed to better understand the effect of the COVID-19 pandemic on OCD symptomatology and treatment trajectory post-pandemic.
Authors’ statement
Role of Funding Source: No funding was sought or obtained for this manuscript.
Disclosure
Dr. Storch reports personal fees from Elsevier, personal fees from Wiley, personal fees from Springer, personal fees from American Psychological Association, personal fees from Jessica Kingsley, personal fees from Lawrence Erlbaum, personal fees from Oxford, grants from Greater Houston Community Foundation, grants from ReBuild Texas, grants from NIH, grants from Texas Higher Education Coordinating Board, personal fees from Levo Therapeutics, personal fees from International OCD Foundation, outside the submitted work. Ms. Sheu, Ms. Rombado, Mr. Gupta, Dr. Hoch, Dr. Schneider, and Dr. Guzick reports no disclosures. Dr Dr. Goodman has received research support from Brainsway, Biohaven Pharmaceutics and the NIH; Medtronic donated devices to a research project; and he received consulting fees from Biohaven and Neurocrine Biosciences.
CRediT authorship contribution statement
Eric A. Storch: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Writing - original draft, Writing - review & editing. Jessica C. Sheu: Conceptualization, Data curation, Investigation, Methodology, Project administration, Writing - original draft, Writing - review & editing. Andrew G. Guzick: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing - original draft, Writing - review & editing. Sophie C. Schneider: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Supervision, Writing - review & editing. Sandra L. Cepeda: Data curation, Investigation, Methodology, Project administration, Supervision, Writing - review & editing. Bianca R. Rombado: Conceptualization, Data curation, Methodology, Project administration, Writing - review & editing. Rohit Gupta: Conceptualization, Data curation, Methodology, Project administration, Writing - review & editing. Connor T. Hoch: Conceptualization, Data curation, Methodology, Project administration, Writing - review & editing. Wayne K. Goodman: Methodology, Project administration, Supervision, Writing - review & editing.
References
- Abramowitz J.S., Deacon B.J., Olatunji B.O., Wheaton M.G., Berman N.C., Losardo D., Timpano K.R., McGrath P.B., Riemann B.C., Adams T., Björgvinsson T., Storch E.A., Hale L.R. Assessment of obsessive-compulsive symptom dimensions: development and evaluation of the Dimensional Obsessive-Compulsive Scale. Psychol. Assess. 2010;22:180–198. doi: 10.1037/a0018260. [DOI] [PubMed] [Google Scholar]
- Akhtar S., Wig N.N., Varma V.K., Pcrshad D., Verma S.K. A phenomenological analysis of symptoms in obsessive-compulsive neurosis. Br. J. Psychiatry. 1975;127:342–348. doi: 10.1192/bjp.127.4.342. [DOI] [PubMed] [Google Scholar]
- Asmundson G.J.G., Paluszek M.M., Landry C.A., Rachor G.S., McKay D., Taylor S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bareket-Bojmel L., Shahar G., Margalit M. COVID-19-related economic anxiety is as high as health anxiety: findings from the USA, the UK, and Israel. Int. J. Cogn. Ther. 2020:1–9. doi: 10.1007/s41811-020-00078-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benatti B., Albert U., Maina G., Fiorillo A., Celebre L., Girone N., Fineberg N., Bramante S., Rigardetto S., Dell'Osso B. What happened to patients with obsessive compulsive disorder during the COVID-19 pandemic? A multicentre report from tertiary clinics in Northern Italy. Front. Psychiatry. 2020:11. doi: 10.3389/fpsyt.2020.00720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Britton G.I., Davey G.C.L. Negative mood and obsessive-compulsive related clinical constructs: an examination of underlying factors. Front. Psychol. 2017;8 doi: 10.3389/fpsyg.2017.01570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC . Centers for Disease Control and Prevention; 2020. Coronavirus Disease 2019 (COVID-19)–Prevention & Treatment [WWW Document]https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html URL. (accessed 9.1.20) [Google Scholar]
- Cervin M., Perrin S., Olsson E., Claesdotter-Knutsson E., Lindvall M. Involvement of fear, incompleteness, and disgust during symptoms of pediatric obsessive-compulsive disorder. Eur. Child Adolesc. Psychiatry. 2020 doi: 10.1007/s00787-020-01514-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychol. Bulletin. 1992;112(1):155–159. doi: 10.1037//0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Davide P., Andrea P., Martina O., Andrea E., Davide D., Mario A. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020;291 doi: 10.1016/j.psychres.2020.113213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denys D., Burger H., van Megen H., de Geus F., Westenberg H. A score for predicting response to pharmacotherapy in obsessive-compulsive disorder. Int. Clin. Psychopharmacol. 2003;18:315–322. doi: 10.1097/00004850-200311000-00002. [DOI] [PubMed] [Google Scholar]
- Flament M.F., Rapoport J.L., Berg C.J., Sceery W., Kilts C., Mellström B., Linnoila M. Clomipramine treatment of childhood obsessive-compulsive disorder. A double-blind controlled study. Arch. Gen. Psychiatry. 1985;42:977–983. doi: 10.1001/archpsyc.1985.01790330057007. [DOI] [PubMed] [Google Scholar]
- Foa E.B., Liebowitz M.R., Kozak M.J., Davies S., Campeas R., Franklin M.E., Huppert J.D., Kjernisted K., Rowan V., Schmidt A.B., Simpson H.B., Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. AJP. 2005;162:151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Fontenelle L.F., Miguel E.C. The impact of coronavirus (COVID-19) in the diagnosis and treatment of obsessive-compulsive disorder. Depress. Anxiety. 2020;37:510–511. doi: 10.1002/da.23037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- French I., Lyne J. Acute exacerbation of OCD symptoms precipitated by media reports of COVID-19. Ir. J. Psychol. Med. 2020:1–4. doi: 10.1017/ipm.2020.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia A.M., Sapyta J.J., Moore P.S., Freeman J.B., Franklin M.E., March J.S., Foa E.B. Predictors and moderators of treatment outcome in the pediatric obsessive compulsive treatment study (POTS I) J. Am. Acad. Child Adolesc. Psychiatry. 2010;49:1024–1033. doi: 10.1016/j.jaac.2010.06.013. quiz 1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M.Á., Saiz J., López-Gómez A., Ugidos C., Muñoz M. Mental health consequences during the initial stage of the 2020 coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020;87:172–176. doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman W.K., Price L.H., Rasmussen S.A., Mazure C., Delgado P., Heninger G.R., Charney D.S. The Yale-Brown Obsessive Compulsive Scale. II. Validity. Arch. Gen. Psychiatry. 1989;46:1012–1016. doi: 10.1001/archpsyc.1989.01810110054008. [DOI] [PubMed] [Google Scholar]
- Goodman W.K., Price L.H., Rasmussen S.A., Mazure C., Fleischmann R.L., Hill C.L., Heninger G.R., Charney D.S. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch. Gen. Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- Haider I.I., Tiwana F., Tahir S.M. Impact of the COVID-19 pandemic on adult mental health. Pak. J. Med. Sci. 2020;36:S90–S94. doi: 10.12669/pjms.36.COVID19-S4.2756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamatani S., Tsuchiyagaito A., Nihei M., Hayashi Y., Yoshida T., Takahashi J., Okawa S., Arai H., Nagaoka M., Matsumoto K., Shimizu E., Hirano Y. Predictors of response to exposure and response prevention-based cognitive behavioral therapy for obsessive-compulsive disorder. BMC Psychiatry. 2020;20 doi: 10.1186/s12888-020-02841-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Insel T.R., Murphy D.L., Cohen R.M., Alterman I., Kilts C., Linnoila M. Obsessive-compulsive disorder. A double-blind trial of clomipramine and clorgyline. Arch. Gen. Psychiatry. 1983;40:605–612. doi: 10.1001/archpsyc.1983.04390010015002. [DOI] [PubMed] [Google Scholar]
- Jassi A., Shahriyarmolki K., Taylor T., Peile L., Challacombe F., Clark B., Veale D. OCD and COVID-19: a new frontier. Cogn. Behav. Ther. 2020;13 doi: 10.1017/S1754470X20000318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnco C., McGuire J.F., Roper T., Storch E.A. A meta-analysis of dropout rates from exposure with response prevention and pharmacological treatment for youth with obsessive compulsive disorder. Depress. Anxiety. 2020;37:407–417. doi: 10.1002/da.22978. [DOI] [PubMed] [Google Scholar]
- Keeley M.L., Storch E.A., Merlo L.J., Geffken G.R. Clinical predictors of response to cognitive-behavioral therapy for obsessive-compulsive disorder. Clin. Psychol. Rev. 2008;28:118–130. doi: 10.1016/j.cpr.2007.04.003. [DOI] [PubMed] [Google Scholar]
- Khanna S., Kaliaperumal V.G., Channabasavanna S.M. Clusters of obsessive-compulsive phenomena in obsessive-compulsive disorder. Br. J. Psychiatry. 1990;156:51–54. doi: 10.1192/bjp.156.1.51. [DOI] [PubMed] [Google Scholar]
- Kim S.W., Dysken M.W., Kuskowski M. The symptom checklist-90: obsessive-compulsive subscale: a reliability and validity study. Psychiatry Res. 1992;41:37–44. doi: 10.1016/0165-1781(92)90016-v. [DOI] [PubMed] [Google Scholar]
- Knowles K.A., Olatunji B.O. Anxiety and safety behavior usage during the COVID-19 pandemic: the prospective role of contamination fear. J. Anxiety Disord. 2021;77 doi: 10.1016/j.janxdis.2020.102323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A., Somani A. Dealing with coronavirus anxiety and OCD. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyrios M., Hordern C., Fassnacht D.B. Predictors of response to cognitive behaviour therapy for obsessive-compulsive disorder. Int. J. Clin. Health Psychol. 2015;15:181–190. doi: 10.1016/j.ijchp.2015.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewin A.B., McGuire J.F., Murphy T.K., Storch E.A. The importance of considering parent's preferences when planning treatment for their children–the case of childhood obsessive-compulsive disorder. J. Child Psychol. Psychiatry. 2014;55:1314–1316. doi: 10.1111/jcpp.12344. [DOI] [PubMed] [Google Scholar]
- Lin H., Katsovich L., Ghebremichael M., Findley D.B., Grantz H., Lombroso P.J., King R.A., Zhang H., Leckman J.F. Psychosocial stress predicts future symptom severities in children and adolescents with Tourette syndrome and/or obsessive-compulsive disorder. J Child Psychol Psychiatry. 2007 Feb;48(2):157–166. doi: 10.1111/j.1469-7610.2006.01687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu H., Stratton C.W., Tang Y.-W. Outbreak of pneumonia of unknown etiology in Wuhan, China: the mystery and the miracle. J. Med. Virol. 2020;92:401–402. doi: 10.1002/jmv.25678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marquett R.M., Thompson L.W., Reiser R.P., Holland J.M., O'Hara R.M., Kesler S.R., Stepanenko A., Bilbrey A., Rengifo J., Majoros A., Thompson D.G. Psychosocial predictors of treatment response to cognitive-behavior therapy for late-life depression: an exploratory study. Aging Ment. Health. 2013;17:830–838. doi: 10.1080/13607863.2013.791661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli M., Chasson G., Wetterneck C.T., Hart J.M., Björgvinsson T. Perfectionism dimensions as predictors of symptom dimensions of obsessive-compulsive disorder. Bull. Menn. Clin. 2014;78:140–159. doi: 10.1521/bumc.2014.78.2.140. [DOI] [PubMed] [Google Scholar]
- Mataix-Cols D., Marks I.M., Greist J.H., Kobak K.A., Baer L. Obsessive-compulsive symptom dimensions as predictors of compliance with and response to behaviour therapy: results from a controlled trial. Psychother. Psychosom. 2002;71:255–262. doi: 10.1159/000064812. [DOI] [PubMed] [Google Scholar]
- Matsunaga H., Mukai K., Yamanishi K. The acute impact of the pandemic of COVID‐19 on the phenomenological features in the full or partial remitted patients with obsessive–compulsive disorder (OCD) Psychiatry Clin. Neurosci. 2020 doi: 10.1111/pcn.13119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGuire J.F., Piacentini J., Lewin A.B., Brennan E.A., Murphy T.K., Storch E.A. A meta-analysis of cognitive behavior therapy and medication for child obsessive compulsive disorder: moderators of treatment efficacy, response, and remission. Depress. Anxiety. 2015;32:580–593. doi: 10.1002/da.22389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay D., Minaya C., Storch E.A. Conducting exposure and response prevention treatment for contamination fears during COVID-19: the behavioral immune system impact on clinician approaches to treatment. J. Anxiety Disord. 2020;74 doi: 10.1016/j.janxdis.2020.102270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merlo L.J., Lehmkuhl H.D., Geffken G.R., Storch E.A. Decreased family accommodation associated with improved therapy outcome in pediatric obsessive–compulsive disorder. J. Consult. Clin. Psychol. 2009;77:355–360. doi: 10.1037/a0012652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain Behav. Immun. 2020;87:75–79. doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nissen J.B., Parner E. The importance of insight, avoidance behavior, not-just-right perception and personality traits in pediatric obsessive-compulsive disorder (OCD): a naturalistic clinical study. Nord. J. Psychiatry. 2018;72:489–496. doi: 10.1080/08039488.2018.1486454. [DOI] [PubMed] [Google Scholar]
- Obsessive Compulsive Cognitions Working Group Psychometric validation of the obsessive belief questionnaire and interpretation of intrusions inventory–part 2: factor analyses and testing of a brief version. Behav. Res. Ther. 2005;43:1527–1542. doi: 10.1016/j.brat.2004.07.010. [DOI] [PubMed] [Google Scholar]
- Ong C.W., Clyde J.W., Bluett E.J., Levin M.E., Twohig M.P. Dropout rates in exposure with response prevention for obsessive-compulsive disorder: what do the data really say? J. Anxiety Disord. 2016;40:8–17. doi: 10.1016/j.janxdis.2016.03.006. [DOI] [PubMed] [Google Scholar]
- Plunkett R., Costello S., McGovern M., McDonald C., Hallahan B. Impact of the COVID-19 pandemic on patients with pre-existing anxiety disorders attending secondary care. Ir. J. Psychol. Med. 2020:1–9. doi: 10.1017/ipm.2020.75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatry. 2020;33 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodríguez-Rey R., Garrido-Hernansaiz H., Collado S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020:11. doi: 10.3389/fpsyg.2020.01540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satici B., Saricali M., Satici S.A., Griffiths M.D. Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 2020:1–12. doi: 10.1007/s11469-020-00305-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider S.C., Storch E.A., Goodman W.K. New Oxford Textbook of Psychiatry. third ed. Oxford University Press; 2020. Core dimensions of obsessive-compulsive disorder. [Google Scholar]
- Selles R.R., Højgaard D.R.M.A., Ivarsson T., Thomsen P.H., McBride N.M., Storch E.A., Geller D., Wilhelm S., Farrell L.J., Waters A.M., Mathieu S., Stewart S.E. Avoidance, insight, impairment recognition concordance, and cognitive-behavioral therapy outcomes in pediatric obsessive-compulsive disorder. J. Am. Acad. Child Adolesc. Psychiatry. 2020;59:650–659. doi: 10.1016/j.jaac.2019.05.030. e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh S., Roy D., Sinha K., Parveen S., Sharma G., Joshi G. Impact of COVID-19 and lockdown on mental health of children and adolescents: a narrative review with recommendations. Psychiatry Res. 2020:293. doi: 10.1016/j.psychres.2020.113429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skapinakis P., Caldwell D.M., Hollingworth W., Bryden P., Fineberg N.A., Salkovskis P., Welton N.J., Baxter H., Kessler D., Churchill R., Lewis G. Pharmacological and psychotherapeutic interventions for management of obsessive-compulsive disorder in adults: a systematic review and network meta-analysis. Lancet Psychiatry. 2016;3:730–739. doi: 10.1016/S2215-0366(16)30069-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sønderskov K.M., Dinesen P.T., Santini Z.I., Østergaard S.D. The depressive state of Denmark during the COVID-19 pandemic. Acta Neuropsychiatr. 2020;32:226–228. doi: 10.1017/neu.2020.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy M.S., Pratapa S.K., Mahant S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic–a review. Asian J. Psychiatry. 2020;51 doi: 10.1016/j.ajp.2020.102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steardo L., Steardo L., Verkhratsky A. Psychiatric face of COVID-19. Transl. Psychiatry. 2020;10:261. doi: 10.1038/s41398-020-00949-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storch E.A., Larson M.J., Price L.H., Rasmussen S.A., Murphy T.K., Goodman W.K. Psychometric analysis of the Yale-Brown Obsessive-Compulsive Scale second edition symptom checklist. J. Anxiety Disord. 2010;24:650–656. doi: 10.1016/j.janxdis.2010.04.010. [DOI] [PubMed] [Google Scholar]
- Storch E.A., Merlo L.J., Larson M.J., Bloss C.S., Geffken G.R., Jacob M.L., Murphy T.K., Goodman W.K. Symptom dimensions and cognitive-behavioural therapy outcome for pediatric obsessive-compulsive disorder. Acta Psychiatr Scand. 2008;117(1):67–75. doi: 10.1111/j.1600-0447.2007.01113.x. [DOI] [PubMed] [Google Scholar]
- Storch E.A., Schneider S.C., Guzick A., McKay D., Goodman W.K. Impact of COVID-19 on exposure and response prevention for obsessive-compulsive disorder: present and post-pandemic considerations. Psychiatry Res. 2020;292 doi: 10.1016/j.psychres.2020.113310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanir Y., Karayagmurlu A., Kaya İ., Kaynar T.B., Türkmen G., Dambasan B.N., Meral Y., Coşkun M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020;293 doi: 10.1016/j.psychres.2020.113363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorsen A.L., Kvale G., Hansen B., van den Heuvel O.A. Symptom dimensions in obsessive-compulsive disorder as predictors of neurobiology and treatment response. Curr. Treat. Options Psychiatry. 2018;5:182–194. doi: 10.1007/s40501-018-0142-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tibi L., van Oppen P., van Balkom A.J.L.M., Eikelenboom M., Emmelkamp P.M.G., Anholt G.E. Predictors of treatment outcome in OCD: an interpersonal perspective. J. Anxiety Disord. 2019;68 doi: 10.1016/j.janxdis.2019.102153. [DOI] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C.S., Ho R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health. 2020;17:1729. doi: 10.3390/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang C., Pan R., Wan X., Tan Y., Xu L., McIntyre R.S., Choo F.N., Tran B., Ho R., Sharma V.K., Ho C. A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 2020;87:40–48. doi: 10.1016/j.bbi.2020.04.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wheaton M.G., Abramowitz J.S., Berman N.C., Riemann B.C., Hale L.R. The relationship between obsessive beliefs and symptom dimensions in obsessive-compulsive disorder. Behav. Res. Ther. 2010;48:949–954. doi: 10.1016/j.brat.2010.05.027. [DOI] [PubMed] [Google Scholar]