Abstract
We use individual-level data to estimate the effects of long- and short-term exposure to air pollution (PM2.5) on the probability of dying from COVID-19. To the best of our knowledge, our study is the first to look at this relationship using individual-level data. We find that for Mexico City there is evidence of a positive relationship between pollution and mortality that significantly grows with age and that appears to be mostly driven by long- rather than short-term exposure. By using a rich set of individual- and municipal-level covariates we are able to isolate the effect of exposure to pollution from other crucial factors, thus alleviating endogeneity concerns related to selection. Our results provide yet another reason for the need to implement environmental strategies that will reduce the exposure to air pollution: it is a key element to improve the general population's health. In addition, and considering that at this moment we do not know when the pandemic will stop or if SARS-CoV-2 will become a recurrent threat, the relationship that we uncovered suggests that financial resources should be allocated to improve medical services in those areas where PM2.5 concentrations tend to be high.
Keywords: COVID-19, Health, Mexico, Mortality, PM2.5, SARS-CoV-2
Graphical abstract
Highlights
-
•
We find evidence that air pollution (PM2.5) increases the probability of dying from COVID-19
-
•
This effect is most likely driven by long-term exposure
-
•
Results are robust to controlling for individuals’ characteristics (including age and comorbidities)
-
•
The effect is increasing with age, especially within the population that is 40 years or older
1. Introduction
The COVID-19 pandemic has had devastating effects both in terms of human lives and health, and of economic and social costs. Given this challenging context, understanding the factors that might increase mortality risks from COVID-19 is essential so that policy makers can design and implement effective policies to protect individuals with high-risk characteristics and living in contexts that might enhance their vulnerability. While the global pandemic has spread across all regions, the death toll it has brought along has varied enormously between countries, plausibly due to a combination of population characteristics (i.e. age structure, comorbidity prevalence), public policies, and environmental factors. In this study, we focus on the impact of one important environmental factor, air pollution, which has been explored recently in academic studies as a factor contributing to COVID-19 mortality (Conticini et al., 2020; Copat et al., 2020). We analyze the case of Mexico which, as of October 28th, ranks fourth in the world in terms of total deaths (>90,000) and is among the 10 countries with the highest number of deaths per 100 thousand inhabitants (>70) (JH-CSSE, 2020). COVID-19 deaths are largely concentrated in the Mexico City Metropolitan Area (MCMA), where air pollution levels, in spite of no longer being at the historically high levels observed during the end of the last century, remain very high.
Polluted air gains access to the body through the respiratory tract but it has systemic effects that can damage many other organs (Schraufnagel et al., 2019). Therefore, air pollution is linked to many health problems and can lead to premature death in children and adults (Brunekreef and Holgate, 2002; Cohen et al., 2017; Burnett et al., 2018). In particular, air pollutants can cause a persistent inflammatory response and thus increase the risk of infection from viruses that target the respiratory tract (Brunekreef and Holgate, 2002; Travaglio et al., 2020). Hence, it has been argued that prolonged exposure to air pollution makes people more vulnerable to COVID-19 (Yao et al., 2020; Wu et al., 2020). Furthermore, although the role of air pollution in the airborne transmission of the virus is still uncertain, preliminary evidence confirms that SARS-CoV-2 might be present on particulate matter (Setti et al., 2020). If that is the case, current exposure to air pollution could contribute to the spread of the virus as it is potentially carried deep into the lungs on the surface of particulate matter (Schraufnagel et al., 2019). Results for China seem to confirm this as they show a positive relationship between ambient air pollutants and COVID-19 infection (Zhu et al., 2020).
Air pollution is a pressing issue for many megacities, in particular for those located in developing countries (Marlier et al., 2016). The MCMA, the fifth largest in the world (United Nations, 2018), is no exception as its pollution levels frequently exceed the limits suggested by the World Health Organization (WHO) (SEDEMA, 2017). Furthermore, the MCMA has been hit hard by the COVID-19 pandemic: as of October 28th, there have been more than 21,000 COVID-19 deaths in the MCMA—only 13 countries in the world have had more deaths.
Recent research has used aggregate data (e.g., county, municipal, etc.) to look at the relationship between air pollution and COVID-19 (e.g., Cole et al., 2020; Coker et al., 2020, and Wu et al., 2020). To the best of our knowledge, our study is the first to look at the relationship between air pollution and COVID-19 mortality at the individual level. By doing so, we are able to isolate the effect of exposure to air pollution from other crucial factors like age, sex, obesity, diabetes, and hypertension, thus partially alleviating endogeneity concerns. A second contribution of this paper is the use of both short- and long-term exposure to air pollution to disentangle the effects of each type of exposure on the probability of dying from COVID-19. Finally, the context of the countries analyzed in the available studies, with the exception of Vasquez-Apestegui et al. (2020), is very different from that of Mexico and other developing countries, in particular those in Latin America, where health systems have a limited capacity and where the share of the population without formal employment is high (López-Feldman et al., 2020). Our results can contribute to the design of public policies that are better focused to the realities of countries with such characteristics.
2. Materials and methods
2.1. Data
Data for confirmed COVID-19 cases and deaths come from the official statistics released daily by Mexico's Ministry of Health (SEDESA, 2020; SSA, 2020).1 Data for each individual is collected by medical personnel. The information collected and reported includes basic demographic characteristics, health variables (such as being diagnosed with diabetes, hypertension or obesity), smoking status, date when symptoms began, and whether the individual died. Additionally, individuals' municipality of residence is reported, thus allowing us to match each individual to municipal level covariates as well as different measures of pollution exposure.
The municipal level variables that we use in our analysis are population size, population density, hospital beds per capita, poverty measures (“health-service access deficiency” and “food insecurity”), and percentage of jobs that can be done at home. All the information comes directly from official sources (Coneval, 2017; INEGI, 2015) except the percentage of jobs that can be done from home which was estimated based on information from (INEGI, 2015) following Dingel and Neiman (2020).
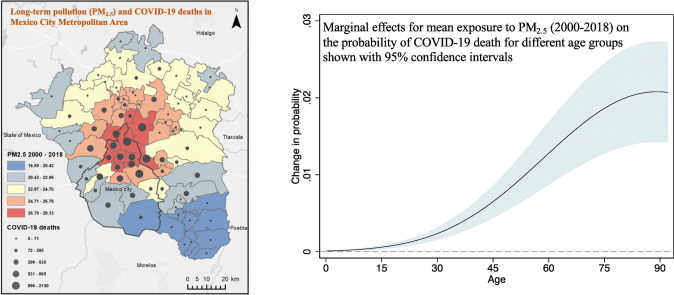
We rely on two sources of information for air pollution, one for long-term exposure and the other for short-term exposure. The average annual concentrations of particulate matter finer than 2.5 micrograms per cubic meter (PM2.5 μg/m3) were obtained from Hammer et al. (2020). Their global dataset, estimated from NASA's satellite products combined with ground level observations from the WHO, has been widely used to analyze the impact of air pollution on health outcomes. Wu et al. (2020) and Knittel and Knittel and Ozaltun (2020) use their data to study the relationship between PM2.5 exposure and COVID-19 deaths in the US. Our analogous municipality-averaged measure was obtained after averaging 1.1 × 1.1 km2 grid-cells (0.01 × 0.01 degrees) within each municipality each year. The mean exposure between 2000 and 2018 is shown in Fig. 1 ; although all 76 municipalities comprised in the MCMA (which encompasses Mexico City) exceed the WHO's standard of annual 10 μg/m3, variability in exposure across the territory is comparable to other recent studies focusing in small countries or specific regions within a country (e.g., Cole et al., 2020; Coker et al., 2020). In the MCMA, the highest exposure is observed in central and northeastern municipalities close to the boundaries between Mexico City and the State of Mexico where most economic activity occurs, and most people inhabit. Fig. 1 suggest that such areas are also experiencing high numbers of COVID-19 deaths.
Fig. 1.
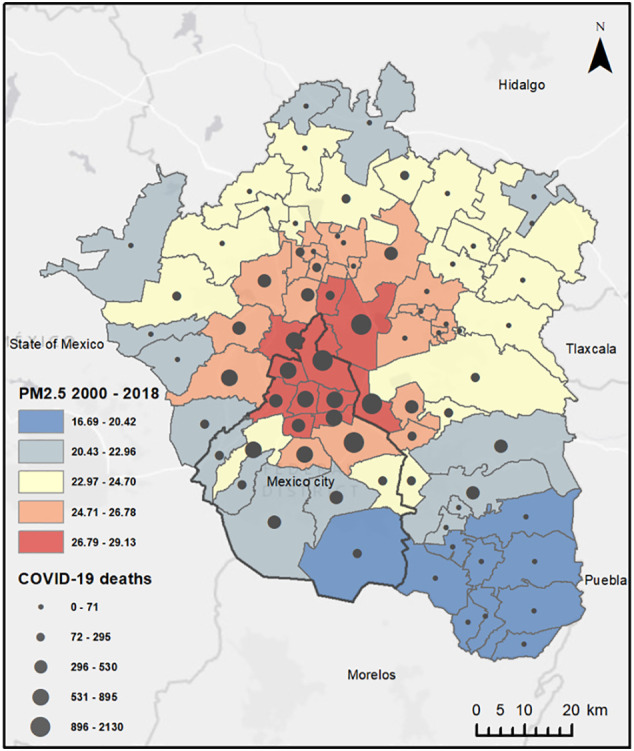
Distribution of long-term pollution (PM2.5) and COVID-19 deaths in Mexico City and the Mexico City Metropolitan Area. Own estimation with data from Hammer et al. (2020) and SSA, 2020.
Our contemporaneous PM2.5 exposure variables are estimated using information published by Mexico City's Secretary of Environment from ground-based air quality monitors (SEDEMA, 2020). Their Automatic Network of Atmospheric Monitoring comprises 34 monitors that report hourly measures of concentrations of different pollutants throughout the MCMA, but that are more densely distributed within Mexico City and bordering municipalities from the State of Mexico. In order to assign more accurately pollution concentrations to each municipality, we restrict our analysis to those municipalities whose centroid is at most 7 km away from a monitoring station. Therefore, given data availability and the geographic location of the air quality monitors, we can measure short-term exposure for 14 out of 16 of the MCMA municipalities in Mexico City using 18 out of the 21 stations that measure PM2.5.2 With the information available, we calculate the weighted average of daily concentrations of PM2.5 based on the readings from all monitors located within a 7 km radius from each municipality centroid (the average municipality had 2 monitoring stations located within this radius).3 Weights are given by the inverse of the distance between the municipality centroid and each monitor. Using this information, we calculate alternative versions of our short-term exposure measure that we use as robustness checks.
We also calculate an alternative version of the long-term exposure variable based on ground-based pollution concentrations during 2019. Temporally, this variable could be considered a more accurate measure of the actual exposure of the average inhabitant of a given municipality if there is a concern of people changing residential locations from one municipality to another between 2018 and 2020. Spatially, however, the satellite-based measures are constructed from finer-grid cells within a municipality and thus could be considered to more accurately represent exposure of inhabitants in a given municipality.
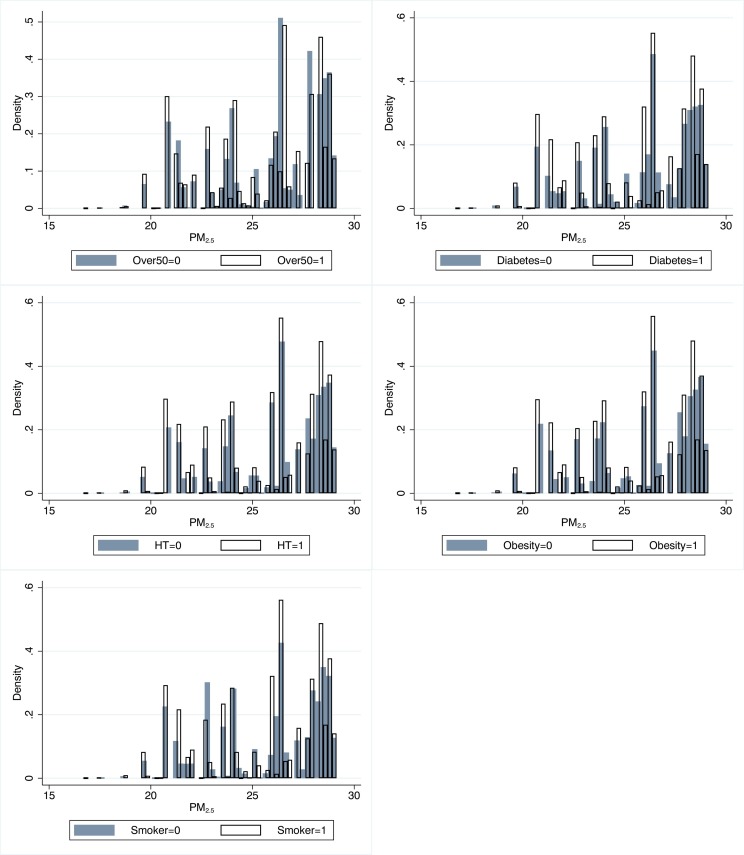
It is worth noting that, in addition to the substantial geographic variation in PM2.5 concentrations within the MCMA that is shown in Fig. 1, we also observe ample variation in the exposure to air pollution across individuals with different characteristics and comorbidities. In particular, Fig. 2 shows variation in PM2.5 long-term exposure across age, diagnoses for diabetes, hypertension, obesity, and smoking status for individuals living in the MCMA. These characteristics and comorbidities have been found to be important modifiers of the risk of dying from COVID-19; it is therefore particularly important to have variation in exposure to air pollution across them.
Fig. 2.
Distribution of long-term exposure to PM2.5 in the MCMA by individual characteristics. Each panel shows a histogram of the average concentration of PM2.5 to which individuals grouped by a given category were exposed. The categories are: Over50 (a variable equal to one if an individual is at least 50 years old); Diabetes (=1 if the individual was diagnosed with type-2 diabetes); HT (=1 if the individual was diagnosed with hypertension); Obesity(=1 if the individual was diagnosed as obese); and Smoker (=1 if the individual smokes).
As Table 1 shows, the MCMA and the Mexico City sub-sample are very similar in terms of individual characteristics, with slightly less than half of the cases being female, a mean age of 45, and comorbidity rates between 10% and 18%. In terms of pollution exposure and socioeconomic characteristics, the Mexico City sub-sample lives in slightly denser and more polluted areas but has larger access to hospital beds, health care, food security, and telework. Importantly, the death rate among confirmed cases is respectively 10% and 11%. Worth mentioning is that in Mexico the number of total COVID-19 tests performed per capita is very low (Roser et al., 2020). This implies that the number of COVID-19 deaths is likely to be underestimated. The low level of testing is the result of an explicit decision made by the federal government to not perform widespread testing. This policy is being applied in the whole country and there is no evidence that suggests that testing levels vary inside the MCMA.4 Therefore, we argue that underestimation is not correlated to municipal pollution levels and hence should not bias our estimations in any meaningful way.5 As is the case in many other countries, there are instances where deaths are not immediately attributed to COVID-19 due to lack of testing. These deaths remain classified as suspicious until a committee decides if they should be attributed to COVID-19. Our estimations use the most up-to-date information, which includes deaths that were originally classified as suspicious and later on were attributed to COVID-19. There is no evidence to suggest that in the MCMA the number of deaths classified as suspicious varies with pollution levels.
Table 1.
Summary statistics—MCMA and Mexico City samples.
| Variable | Mexico City Metropolitan Area (MCMA) |
Mexico City |
||
|---|---|---|---|---|
| Mean | Standard deviation | Mean | Standard deviation | |
| Death (1 if the person died from COVID19) | 0.10 | 0.31 | 0.11 | 0.31 |
| Female (1 if person's sex is female) | 0.49 | 0.50 | 0.48 | 0.50 |
| Age (person's age) | 44.64 | 16.73 | 44.98 | 16.79 |
| Obesity (1 if person diagnosed with obesity) | 0.17 | 0.37 | 0.18 | 0.38 |
| Smoking (1 if person had the habit of smoking) | 0.10 | 0.31 | 0.11 | 0.31 |
| Diabetes (1 if person diagnosed with diabetes) | 0.14 | 0.35 | 0.14 | 0.35 |
| Hypertension (1 if person diagnosed with hypertension) | 0.17 | 0.37 | 0.17 | 0.38 |
| PM2.5 (2000–2018 average daily mean in μg/m3) | 25.72 | 2.25 | 26.70 | 2.02 |
| PM2.5–2019 (2019 average annual mean in μg/m3) | 24.92 | 2.65 | ||
| PM2.5–14 (2-week average mean before onset of symptoms in μg/m3) | 20.79 | 5.77 | ||
| Temperature (2-week average daily mean before onset of symptoms in °C) | 20.70 | 2.21 | ||
| Population density (inhabitants per km2) | 9.10 | 5.44 | 11.34 | 4.85 |
| Population (100,000) | 0.74 | 0.51 | 0.83 | 0.54 |
| Hospital beds (per 10,000 inhabitants) | 17.87 | 16.59 | 23.29 | 18.00 |
| Lack access to health care (% of population) | 19.81 | 3.34 | 19.03 | 2.76 |
| Lack access to food security (% of population) | 12.57 | 5.27 | 9.53 | 2.54 |
| Can work from home (% of labor force) | 24.69 | 8.71 | 29.26 | 7.48 |
| Individual observations | 196,273 | 71,620 | ||
| Municipalities | 76 | 14 | ||
Sources: Own estimation with data from Coneval (2017), SEDESA (2020), SSA (2020), Dingel and Neiman (2020), INEGI (2015), SEDEMA (2020) and Hammer et al. (2020). The MCMA is comprised of 76 municipalities in the states of Hidalgo, Mexico, and Mexico City. All municipalities (16) from Mexico City are part of the MCMA and are included in the MCMA sample. The Mexico City sample only considers the 14 municipalities for which we have PM2.5 for 2019 and 2020. PM2.5–2019 and PM2.5–14 are calculated from the weighted average of the daily concentrations from 7:00 am to 7:00 pm based on all monitors located within a 7 km radius from each municipality centroid, with weights given by the inverse of the distance between the municipality centroid and each monitor.
2.2. Econometric specification
We specify the following probit model to estimate the effect that pollution has on the probability of dying from COVID-19:
| (1) |
where Φ is the standard normal cumulative distribution function, Death im is a dummy variable equal to one if individual i from municipality m who has been infected by COVID-19 dies and zero otherwise, pollution m is a measure of air pollution at municipality m, and X im is a vector of individual- and municipal-level variables that control for potential confounding factors.6 Based on the literature on air pollution and health, and on the results available for the relationship between exposure to PM2.5 and COVID-19, we expect β to be positive. In addition to testing this hypothesis, we are interested in estimating the effect that an increase of 1 μg/m3 in PM2.5 has on the probability that an individual will die after having contracted COVID-19. To do so, we take the derivative of the right-hand side of Eq. (1) with respect to pollution and estimate the average marginal effect of PM2.5 pollution on the probability of dying (for more on the average marginal effect of the probit model see Wooldridge (2002), p. 467).
We are also interested in the effects that short-term exposure might have on the probability of dying from COVID-19. We use the air pollution data that is available for Mexico City to analyze this. This allows us to estimate a modified version of Eq. (1) where, in addition to long-term exposure, we include additional measures of exposure to PM2.5. In particular, in addition to our long-term exposure variable, we include a variable that captures the cumulative average concentration of PM2.5 during the 14 days before the onset of symptoms (PM2.5–14). Additionally, in some of the models we use the variable that measures average concentrations in Mexico City during 2019 (PM2.5–2019).
Addressing endogeneity concerns is crucial in order to establish a causal relationship between exposure to pollution and health. In particular, the evidence suggests that environmental quality is an important dimension for choosing residential location, which is likely to lead to a correlation between higher pollution levels and both observable and unobservable characteristics correlated with health—potentially leading to omitted variable bias. Additionally, avoidance behavior may similarly lead to nonrandom assignment of pollution exposure (Currie et al., 2014). In order to partially address these concerns, we include a rich set of municipal- and individual-level covariates that we use to control for factors that may be correlated to pollution exposure and simultaneously affect mortality. In our preferred specification we include population size, population density, hospital beds per capita, poverty measures (“health-service access deficiency” and “food insecurity”), and percentage of jobs that can be done at home, all measured at the municipal level, as covariates. We also include individual indicators for sex, obesity, smoking status, diabetes, hypertension, age, age squared, and the day in which symptoms started to control for time effects. The inclusion of these covariates is likely to alleviate endogeneity concerns—Cole et al. (2020) and Wu et al. (2020) point out that individual-level data, which they cannot include in their analyses since their COVID-19 data is at the county or municipal levels, is crucial to establish a rigorous statistical link between long-term exposure to pollution and COVID-19. Our standard errors are clustered at the municipality level in order to correct for spatial correlation of the individuals' unobserved variation that may remain after including covariates.
3. Results
To begin the econometric analysis, we use the full sample for the MCMA and estimate a version of Eq. (1) that only includes long-term exposure to PM2.5 as the explanatory variable. Our results (Model 1, Table 2 ) show that there is a positive and statistically significant relationship between exposure and the probability of dying from COVID-19. The relationship remains valid when we include municipal level covariates in Model 2. The last column (Model 3) shows the results of including individual level covariates in our analysis and is our preferred specification. The positive relationship between long-term exposure to PM2.5 and the probability of dying from COVID-19 is robust to the inclusion of covariates at both the individual and municipal levels.7
Table 2.
The relationship between long-term exposure to pollution and the probability of dying from COVID-19 in the MCMA.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| PM2.5 (μg/m3) | 0.0424⁎⁎⁎ | 0.0733⁎⁎⁎ | 0.0571⁎⁎⁎ |
| [0.0143] | [0.0096] | [0.0093] | |
| Municipal-level covariates included | No | Yes | Yes |
| Individual-level covariates included | No | No | Yes |
| N | 196,273 | 196,273 | 196,273 |
| Municipalities | 76 | 76 | 76 |
| Pseudo-R2 | 0.006 | 0.027 | 0.265 |
Notes: The dependent variable is a dummy equal to one if an individual diagnosed with COVID-19 dies and zero otherwise. Estimations are done using a probit model. Cluster robust standard errors at the municipal-level are shown in brackets. Municipal-level covariates are: Population density, population, density of hospital beds, percentage of population without access to health care, percentage of population with moderate or severe food insecurity, and percentage of labor force with jobs that can be done from home. Individual-level covariates are: gender, age and age squared, obesity, diabetes, hypertension, smoking status, and day in which symptoms started. MCMA is comprised of 76 municipalities in the states of Hidalgo, Mexico, and Mexico City. All municipalities (16) from Mexico City are part of the MCMA and are included in this sample.
p < 0.01.
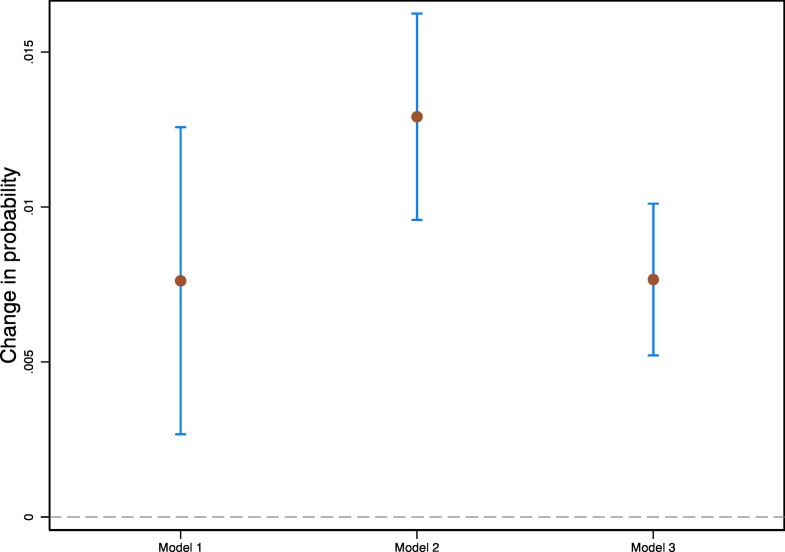
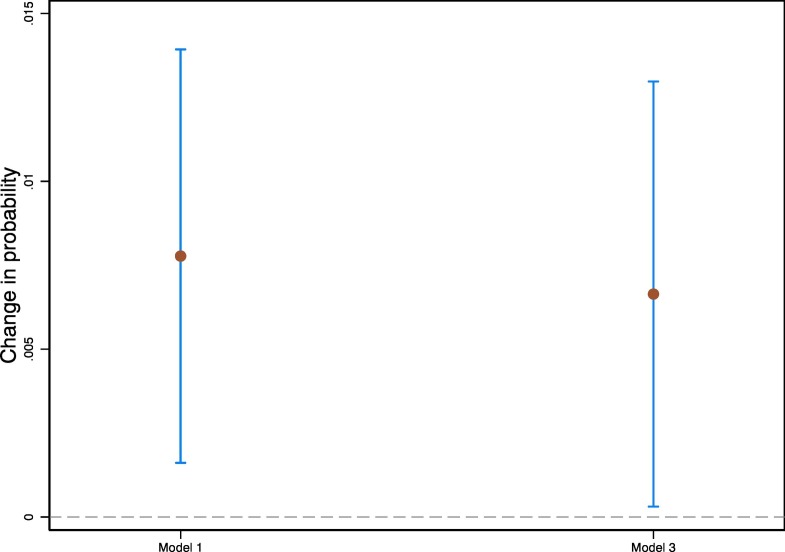
In order to better interpret our results, we estimate marginal effects for the three versions of the model, which are shown in Fig. 3 . For the version without covariates (Model 1, Table 2) we estimate an average marginal effect of 0.0076, which implies that for an increase of 1 μg/m3 in PM2.5 the probability of dying from COVID-19 increases on average by 0.76 percentage points. For the model with municipal-level covariates (Model 2) the marginal effect is 0.0129. Our preferred specification is the one that takes into account age, obesity, diabetes, hypertension, smoking, and municipal level covariates, as in Model 3. For that model we estimate that on average the probability of dying from COVID-19 increases by 0.77 percentage points with an increase of 1 μg/m3 in PM2.5. Given that the average mortality rate for our sample is of approximately 10.4%, our estimates suggest that an increase of 1 μg/m3 in PM2.5 may increase mortality risk by approximately 7.4%.
Fig. 3.
The effects of long-term exposure to PM2.5 on probability of COVID-19 death in the MCMA. Estimates of marginal effects to exposure to PM2.5 (2000–2018) shown with 95% cluster-robust confidence intervals. The models behind each estimation are those described in Table 2.
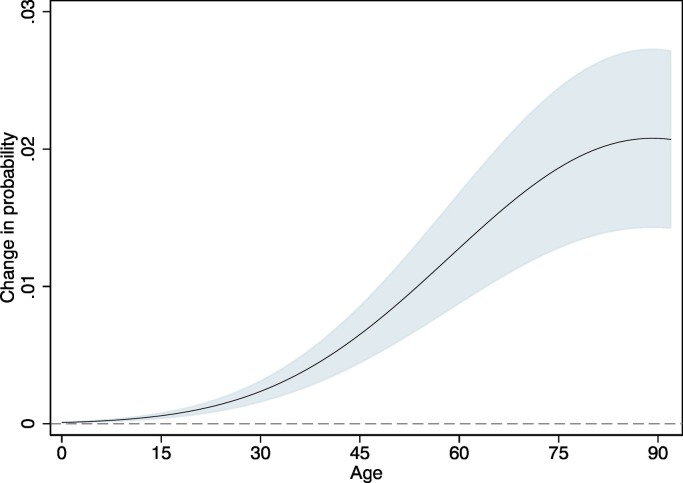
Fig. 4 presents the average marginal effects of pollution across age. It shows that the effects of long-term exposure on the probability of dying are heterogeneous and increasing with age. Long-term exposure to air pollution has a very small effect on children (0.02 percentage points from one additional μg/m3 of PM2.5 for 5-year-old children). At first, the magnitude of the effect increases slowly—individuals with 20 years of age have a marginal effect of 0.09 percentage points—but starts increasing faster gradually—the marginal effect is 0.45 percentage points for individuals that are 40 years old and 1.23 percentages points for those that are 60 years old, until it plateaus around 2 percentage points for individuals aged 80 years or older.8
Fig. 4.
The effects of exposure to PM2.5 air pollution on probability of COVID-19 death by age in the MCMA. Estimates of marginal effects to exposure to PM2.5 (2000–2018) shown with 95% cluster-robust confidence intervals. The model behind the estimation (Model 3 in Table 2) includes municipal-level covariates (population density, population, density of hospital beds, percentage of population without access to health care, percentage of population with moderate or severe food insecurity, and percentage of labor force with jobs that can be done from home), and individual-level covariates (gender, age and age squared, obesity, diabetes, hypertension, smoking status, and day in which symptoms started).
Table 3 shows the results of using the data from air pollution monitors that is available for Mexico City. With these data we are able to, in addition to our long-term exposure variable, include short-term PM2.5 cumulative average concentration during the 14 days before the onset of symptoms. Model 1 shows that the coefficient of short-term pollution is significant only at the 10% level. In Model 2, we use PM2.5 concentrations during 2019 instead of using the long-term variable. We only find weak evidence to support that there is an effect of short-term exposure on the probability of dying (Model 2, Table 3). The effect of long-term exposure seems to be partially captured with the variable PM2.5–2019, which is weakly statistically significant. This is reassuring; both variables (PM2.5–2019 and PM2.5) seem to be in fact capturing the same phenomenon. As a way to test that this is in fact the case, the last column shows the results of estimating the model with the three pollution variables simultaneously (Model 3). The two long-term exposure variables appear to be substitutes of each other, while once again we only find a slightly statistically significant effect for short-term exposure.9 As a robustness check, we also estimate all the models presented in Table 3 using cumulative average concentrations during 2, 7, 5 and 10 days instead of 14 days (results are presented in Table A4 of the Appendix). While the results for long-term exposure are similar to those presented in Table 3, results for short-term exposure are not statistically significant for any of the alternative exposure windows. Finally, as shown in Fig. 5 , the marginal effects for changes in long-term PM2.5 exposure estimated for Mexico City are very similar to those estimated for the MCMA (Fig. 3). Marginal effects for short-term exposure are very small and only weakly significant (90% CI: 0.00006, 0.00099).
Table 3.
The relationship between long- and short-term exposure to pollution and the probability on dying from COVID-19 in Mexico City.
| Model 1 | Model 2 | Model 3 | |
|---|---|---|---|
| PM2.5 (μg/m3) | 0.0566⁎⁎ | 0.0484⁎⁎ | |
| [0.0227] | [0.0234] | ||
| PM2.5–2019 (μg/m3) | 0.0260⁎ | 0.0170 | |
| [0.0149] | [0.0132] | ||
| PM2.5–14 (μg/m3) | 0.0038⁎ | 0.0035⁎ | 0.0037⁎ |
| [0.0021] | [0.0020] | [0.0021] | |
| Municipal-level covariates included | Yes | Yes | Yes |
| Individual-level covariates included | Yes | Yes | Yes |
| N | 71,620 | 71,620 | 71,620 |
| Municipalities | 14 | 14 | 14 |
| Localities | 380 | 380 | 380 |
| Pseudo R2 | 0.260 | 0.260 | 0.260 |
Notes: The dependent variable is a dummy equal to one if an individual diagnosed with COVID-19 dies and zero otherwise. Estimations are done using a probit model. Cluster robust standard errors at the municipal-level shown in brackets. Municipal-level covariates are: Population density, population, density of hospital beds, percentage of population without access to health care, percentage of population with moderate or severe food insecurity, and percentage of labor force with jobs that can be done from home. Individual-level covariates are: gender, age and age squared, obesity, diabetes, hypertension, smoking status, and day in which symptoms started. The Mexico City sample only considers the 14 municipalities for which, in addition to long-term exposure to PM2.5, we know PM2.5 for 2019 and 2020.
p < 0.1.
p < 0.05.
Fig. 5.
The effects of long-term exposure to PM2.5 on probability of COVID-19 death in Mexico City. Estimates of marginal effects to exposure to PM2.5 (2000–2018) shown with 95% cluster-robust confidence intervals. The models behind each estimation are those described in Table 3.
4. Discussion
Given the magnitude of the health crisis caused by SARS-CoV-2 and the amount of research that it has spurred across many fields, many researchers have looked at the relationship between exposure to particulate matter and morbi-mortality by COVID-19, perhaps unsurprisingly. Many of these studies have analyzed the relationship between exposure and infection and have shown that there is in fact a positive association between high levels of PM10 and PM2.5 and confirmed cases (Coccia, 2020; Zhu et al., 2020). Consistent with results for the SARS 2003 outbreak (Cui et al., 2003), the research that looks at the effects on mortality has found, as we do, that there is a positive relationship between exposure to PM2.5 and COVID-19 mortality.
Our results cannot be directly compared to other results for COVID-19 as ours is, to the best of our knowledge, the first study to estimate the effects of air pollution on the probability of dying at the individual level.10 Nonetheless, a natural point of comparison are the results from Wu et al. (2020) for the U.S., as we use similar covariates in our analysis and the long-term exposure variable that we use comes from the same source, although they look at exposure from 2000 to 2016 while we use 2000 to 2018. Their reported estimate that a 1 μg/m3 increase in PM2.5 is associated to an 8% increase in the death rate, is consistent with our estimation of an increase in the COVID-19 mortality rate of 0.77 percentage points, which is equivalent to an increase in the probability of dying from COVID-19 of 7.4%. Our results are in line with those published by Petroni et al. (2020) who find that a 1 μg/m3 increase in PM2.5 is correlated with a 7% increase in the mortality rate ratio in the U.S.
Cole et al. (2020) and Coker et al. (2020) also look at long-term exposure to PM2.5 and mortality. They use municipal-level data for Netherlands and Italy, respectively, and find evidence of a positive relationship. Coker et al. (2020) use excess mortality as dependent variable and estimate that a one-unit increase in PM2.5 concentration (μg/m3) is associated with a 9% increase in mortality. Meanwhile, Cole et al. (2020) find that the same increase in PM2.5 will lead to 2.3 more deaths at the municipality level. Although not directly comparable, our results are similar in magnitude to those form Coker et al. (2020) and higher than those from Cole et al. (2020). This is consistent with the fact that Mexico's per-capita COVID-19 mortality is similar to Italy's and much higher to that of the Netherlands.
The work of Yao et al. (2020) for 49 cities in China is also related to ours as it uses short-term and long-term exposure indicators, average PM concentrations from January 15, 2020 to February 29, 2020 and average concentrations of PM annual mean levels in years 2015–2019. Using data at the city-level they show, like we do, that the association between short- and long-term exposure and fatality is positive.
Contrary to all these studies that use data at an aggregate level, by using individual-level information we are able to estimate how exposure to PM2.5 can have a differential effect on the probability of dying according to the age of the infected individual. We show that the effect of PM2.5 is monotonically increasing with age and reaches a maximum at around 80 years of age, a finding that is consistent with the available evidence that clearly shows that COVID-19 fatality rates vary with age (Roser et al., 2020). Furthermore, although the effects are small, according to our results exposure to PM2.5 can actually increase the probability that infants and small children die from COVID-19. This is consistent with evidence showing that exposure to PM2.5 can lead to systemic inflammation and suppress early immune responses to infections even in young people (Conticini et al., 2020; Wu et al., 2020).
This study is subject to some limitations. First, although we include a rich set of municipal- and individual-level covariates, available information does not allow us to directly control for individuals' residential choice or avoidance behavior. Both factors could lead to nonrandom assignment of pollution exposure and hence represent a threat to establishing a causal relationship. Second, we are implicitly assuming that air pollution is evenly distributed within each municipality (locality). If that is not the case and the distribution of PM2.5 inside a municipality (locality) is correlated to some individual characteristics that also affect the probability of dying, then our results could be biased. Third, although we know the residence of all the individuals in our sample, we do not know for how long they have been living there or how much of their time they actually spend at home. In our estimations, individuals' long-term exposure to PM2.5 is based on residence. Nonetheless, if an individual recently moved to a municipality, their true exposure to air pollution would be different to the one that we are attributing. Although we partially control for this by using exposure during 2019 as an alternative measure to exposure during 2000–2018, it is still possible for our results to be biased because of this. Fourth, we do not find robust evidence of an effect of short-term PM2.5 exposure on the probability of dying from COVID-19. We had expected to find a statistically significant relationship because pollution exposure could be expected to generate an acute deterioration of the immunological system and to facilitate transportation of the virus. However, due to heterogeneous changes in daily activities and mobility across the population during the pandemic, measured PM2.5 concentrations may be less indicative of actual exposure and thus become a bad predictor of the probability of dying from COVID-19. In spite of these limitations, our study makes relevant contributions to the literature.
5. Concluding remarks
We find evidence of a positive relationship between PM2.5 air pollution and the probability that an individual will die after contracting COVID-19; this relationship increases with age, especially for individuals that are 40 years old or more. Although our results suggest that this is mainly driven by long-term exposure, we cannot rule out that short-term exposure also has an effect. These results are robust to model specification and inclusion of confounders at the municipal- and individual-level. The last is the most important contribution of this paper as, in contrast to the previous literature, we are able to explicitly include in our estimations not only the age and gender of the person affected by COVID-19 but also if she has underlying health conditions. By doing this, we reduce the likelihood that unobservables could explain away the effects that we report. In spite of these efforts, our robust statistical evidence cannot be fully interpreted as causal as we do not have experimental or quasi-experimental data. Furthermore, although in our estimations we use cluster-robust standard errors, there might be spatial autocorrelation issues that cannot be fully accounted for by our empirical strategy that is based on individual-level data.
Mexico is still in the midst of the pandemic; health conditions are continuously evolving, and data related to COVID-19 cases and mortality is being updated regularly. In the coming months we should have better data and a cleaner picture of the full extent of the effects of the pandemic both in the MCMA and in the country. Meanwhile, our results provide yet another reason for the need to implement more stringent controls to air pollution. In addition, and considering that at this moment we do not know when the pandemic will stop or if SARS-CoV-2 will become a recurrent threat, the relationship that we uncovered suggests that financial resources should be allocated to improve medical services in those areas where PM2.5 concentrations tend to be high; long-term exposure has made people living in those areas more vulnerable to the disease. Additionally, policy makers and governments should rethink and reinforce environmental strategies that will reduce levels of air pollution as a key element of public health policies.
In our analysis we focus on the MCMA because of its high levels of air pollution and high rate of COVID-19 mortality. Nonetheless, it is not clear if our results are valid for other big metropolitan areas in the world or even for other parts of Mexico. The fact that our results are in general consistent with other studies on the relation between air pollution and COVID-19 mortality gives us greater confidence that our findings are externally valid—at least to some extent. Finally, our findings suggest that there are groups that, given their exposure to PM2.5, could be particularly vulnerable to COVID-19 in developing countries with characteristics similar to Mexico. Notorious among these groups are users of public transportation, street vendors, and households that use solid fuels for all or part of their cooking or heating needs. Understanding how COVID-19 affects these groups will be essential for the design of public policies that can successfully decrease the toll that this pandemic is exerting on the population.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Alejandro López-Feldman: Conceptualization, Methodology, Formal analysis, Investigation, Writing - original draft, Writing - review & editing, Supervision, Project administration. David Heres: Conceptualization, Formal analysis, Investigation, Writing - original draft, Writing - review & editing. Fernanda Marquez-Padilla: Conceptualization, Methodology, Formal analysis, Writing - original draft, Writing - review & editing.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Editor: Philip K. Hopke
Footnotes
We use the data update available on October 7th, 2020. For all our estimations we restrict the sample to those individuals for which the symptoms started at least 14 days before that date.
Incorporating the two remaining municipalities in Mexico City, representing 6% percent of the city's population, required the maximum distance from a municipality to a monitor to be increased to 15 km. This distance is particularly unlikely to provide reliable pollution exposure measures for these two municipalities given that the weighted-average would be estimated based on a single and relatively remote monitoring station.
We also restricted our measure to consider only readings from 7:00 am-7:00 pm which we consider to better represent daily exposure due to economic and social activities that mostly takes place during those hours. Nonetheless, all the estimations presented in the paper were also done using 24-hour readings, the results (available upon request) are very similar to those obtained using 12-hour readings.
This is different to what happens in other countries, like Italy, where testing policies vary among regions and therefore measurement error is non-randomly distributed (Coker et al., 2020).
In order to empirically test this, we regress the share of positive COVID-19 tests at the municipality-month level on a linear time trend and municipal-level covariates (population size, population density, hospital beds per capita, poverty measures, and percentage of jobs that can be done from home) and obtain residuals. We then regress the residuals on the mean PM2.5 municipal variable and find no statistically significant associations (95% CI: −0.006, 0.002) between residuals and air pollution, suggesting that undermeasurement is indeed uncorrelated to PM2.5 levels. Intuitively, this shows that being above or below the general trend for MCMA in terms of the share of positive tests is uncorrelated with pollution levels conditional on municipal-level covariates. This relation can be seen graphically in Figure A1 of the Appendix.
In some of the estimations for Mexico City we take advantage of the fact that for that sub-sample we have information at the locality level (a smaller administrative area than a municipality) and hence use pollution concentrations at that level.
The relationship is also robust to the way in which the probability function is modeled; our results remain valid when we estimate a linear probability model instead of a probit model (Table A1 of the Appendix).
We do not find evidence that the magnitude of the effect of air pollution on COVID-19 mortality risk varies according to comorbidities (hypertension, type 2 diabetes, obesity) or smoking status—although these factors do affect the probability of death from COVID-19 directly (Figure A2 of the Appendix).
All models presented in Table 3 were also estimated using linear probability models. The results, shown in Table A2 of the Appendix, are very similar to those presented in Table 3. As an additional robustness check, we also included the average temperature that the individual experienced in the 14 days before the onset of symptoms as an additional variable in all the models presented in Table 3. Results for PM2.5 and PM2.5–2019 remain virtually identical, while PM2.5–14 ceases to be statistically significant (Table A3 of the Appendix).
Travaglio et al. (2021) use individual-level data for England but they estimate the probability of being infected, not the probability of dying.
Supplementary material to this article can be found online at https://doi.org/10.1016/j.scitotenv.2020.143929.
Appendix A. Supplementary material
Supplementary material
References
- Brunekreef B., Holgate S.T. Air pollution and health. Lancet. 2002;360(9341):1233–1242. doi: 10.1016/S0140-6736(02)11274-8. [DOI] [PubMed] [Google Scholar]
- Burnett R., Chen H., Szyszkowicz M., Fann N., Hubbell B., Pope C.A.…Coggins J. Global estimates of mortality associated with long-term exposure to outdoor fine particulate matter. Proc. Natl. Acad. Sci. 2018;115(38):9592–9597. doi: 10.1073/pnas.1803222115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coccia M. Factors determining the diffusion of COVID-19 and suggested strategy to prevent future accelerated viral infectivity similar to COVID. Sci. Total Environ. 2020;729:1–20. doi: 10.1016/j.scitotenv.2020.138474. (138474) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen A.J., Brauer M., Burnett R., Anderson H.R., Frostad J., Estep K.…Feigin V. Estimates and 25-year trends of the global burden of disease attributable to ambient air pollution: an analysis of data from the Global Burden of Diseases Study 2015. Lancet. 2017;389(10082):1907–1918. doi: 10.1016/S0140-6736(17)30505-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coker E.S., Cavalli L., Fabrizi E., Guastella G., Lippo E., Parisi M.L.…Vergalli S. The effects of air pollution on COVID-19 related mortality in northern Italy. Environ. Resour. Econ. 2020:1–24. doi: 10.1007/s10640-020-00486-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole M.A., Ozgen C., Strobl E. Air pollution exposure and COVID-19 in Dutch municipalities. Environ. Resour. Econ. 2020:1–30. doi: 10.1007/s10640-020-00491-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coneval Anexo estadístico de pobreza a nivel municipio 2010 y 2017. 2017. https://www.coneval.org.mx/Medicion/Paginas/AE_pobreza_municipal.aspx Available from.
- Conticini E., Frediani B., Caro D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in northern Italy? Environ. Pollut. 2020;261 doi: 10.1016/j.envpol.2020.114465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Copat C., Cristaldi A., Fiore M., Grasso A., Zuccarello P., Santo Signorelli S.…Ferrante M. The role of air pollution (PM and NO2) in COVID-19 spread and lethality: a systematic review. Environ. Res. 2020;191:1–9. doi: 10.1016/j.envres.2020.110129. 110129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui Y., Zhang Z.F., Froines J., Zhao J., Wang H., Yu S.Z., Detels R. Air pollution and case fatality of SARS in the People's Republic of China: an ecologic study. Environ. Health. 2003;2(1):1–5. doi: 10.1186/1476-069X-2-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Currie J., Zivin J.G., Mullins J., Neidell M. What do we know about short-and long-term effects of early-life exposure to pollution? Annu. Rev. Resour. Econ. 2014;6(1):217–247. [Google Scholar]
- Dingel J.I., Neiman B. How many jobs can be done at home? J. Public Econ. 2020;189 doi: 10.1016/j.jpubeco.2020.104235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammer M.S., van Donkelaar A., Li C., Lyapustin A., Sayer A.M., Hsu N.C.…Brauer M. Global estimates and long-term trends of fine particulate matter concentrations (1998-2018) Environmental Science & Technology. 2020;54:7879–7890. doi: 10.1021/acs.est.0c01764. [DOI] [PubMed] [Google Scholar]
- INEGI . Instituto Nacional de Estadística y Geografía; 2015. Encuesta Intercensal 2015.https://www.inegi.org.mx/programas/intercensal/2015/ Available from. [Google Scholar]
- JH-CSSE COVID-19 data repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. 2020. https://github.com/CSSEGISandData/COVID-19
- Knittel C.R., Ozaltun B. NBER Working Paper Series. vol. 27391. 2020. What does and does not correlate with covid-19 death rates; pp. 1–25.http://www.nber.org/papers/w27391 [Google Scholar]
- López-Feldman A., Chávez C., Vélez M.A. Environmental impacts and policy responses to Covid-19: a view from Latin America. Environ. Resour. Econ. 2020 doi: 10.1007/s10640-020-00460-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlier M.E., Jina A.S., Kinney P.L., DeFries R.S. Extreme air pollution in global megacities. Current Climate Change Reports. 2016;2(1):15–27. [Google Scholar]
- Petroni M., Hill D., Younes L., Barkman L., Howard S., Howell I.B.…Collins M.B. Hazardous air pollutant exposure as a contributing factor to COVID-19 mortality in the United States. Environ. Res. Lett. 2020;15(9) [Google Scholar]
- Roser M., Ritchie H., Ortiz-Ospina E., Hasell J. "Coronavirus Pandemic (COVID-19)". Published online at OurWorldInData.org. 2020. https://ourworldindata.org/coronavirus Retrieved from: [Online Resource]
- Schraufnagel D.E., Balmes J.R., Cowl C.T., De Matteis S., Jung S.-H., Mortimer K., Perez-Padilla R., Rice M.B., Riojas-Rodriguez H., Sood A., Thurston G.D., To T., Vanker A., Wuebbles D.J. Air pollution and noncommunicable diseases. Chest. 2019;155(2):409–416. doi: 10.1016/j.chest.2018.10.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SEDEMA . Secretaria de Medio Ambiente de la Ciudad de México; 2017. Calidad del aire en la Ciudad de México, informe 2016, Dirección general de Gestión de la Calidad del Aire, Dirección de Monitoreo Atmosférico. [Google Scholar]
- SEDEMA Bases de datos - Red Automática de Monitoreo Atmosférico (RAMA). Sistema de Monitoreo Atmosférico, Secretaría de Medio Ambiente de la Ciudad de México. 2020. http://www.aire.cdmx.gob.mx/dfault.php?opc=%27aKBh%27 Available from.
- SEDESA (2020). Covid-19 SINAVE Ciudad de México. Sistema Nacional de Vigilancia Epidemiológica, Secretaría de Salud de la Ciudad de México. Available from https://datos.cdmx.gob.mx/explore/dataset/base-covid-sinave/information/. Accessed July 18, 2020.
- Setti L., Passarini F., De Gennaro G., Baribieri P., Perrone M.G., Borelli M., Palmisani J., Di Gilio A., Torboli V., Pallavicini A., Ruscio M., Piscitelli P., Miani A. MedRxiv; 2020. SARS-Cov-2 RNA Found on Particulate Matter of Bergamo in Northern Italy: First Preliminary Evidence; pp. 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SSA Casos diarios por municipio. Dirección General de Epidemiología, Secretaría de Salud. 2020. https://coronavirus.gob.mx/datos/#DownZCSV Available from.
- Travaglio M., Yu Y., Popovic R., Selley L., Leal N.S., Martins L.M. 2020. Links between Air Pollution and COVID-19 in England. MedRxiv; pp. 1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations . Department of Economic and Social Affairs, Population Division; 2018. The World's Cities in 2018 – Data Booklet. (ST/ES/SER.A/417) [Google Scholar]
- Vasquez-Apestegui V., Parras-Garrido E., Tapia V., Paz-Aparicio V.M., Rojas J.P., Sánchez-Ccoyllo O.R., Gonzales G.F. Association between air pollution in Lima and the high incidence of COVID-19: findings from a post hoc analysis. Research Square. 2020:1–22. doi: 10.21203/rs.3.rs-39404/v1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu X., Nethery R.C., Sabath B.M., Braun D., Dominici F. 2020. Exposure to Air Pollution and COVID-19 Mortality in the United States: A Nationwide Cross-Sectional Study. MedRxiv; pp. 1–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldridge J. MIT press; 2002. Econometric Analysis of Cross Section and Panel Data. [Google Scholar]
- Yao Y., Pan J., Wang W., Liu Z., Kan H., Qiu Y.…Wang W. Association of particulate matter pollution and case fatality rate of COVID-19 in 49 Chinese cities. Sci. Total Environ. 2020;741 doi: 10.1016/j.scitotenv.2020.140396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu Y., Xie J., Huang F., Cao L. Association between short-term exposure to air pollution and COVID-19 infection: evidence from China. Sci. Total Environ. 2020;727 doi: 10.1016/j.scitotenv.2020.138704. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material