Abstract
Objective:
A fully dimensional model of psychosis implies that psychotic-like experiences (PLEs) connect the entire psychosis spectrum. Three types of self-reported PLEs—persecutory ideation, bizarre experiences, and perceptual abnormalities—are commonly found in the general population. This study assessed the construct, predictive, and incremental validity of self-reported PLEs in youth at clinical high risk for psychotic disorders (CHR).
Methods:
Self-report data on PLEs (Community Assessment of Psychic Experiences; CAPE) were collected from 105 CHR youth (mage = 19.3). Interview measures of attenuated psychotic symptoms and self-report measures of psychosis-proneness, depression, and anxiety were collected at baseline and 12-month follow-up (n = 70 at follow-up). Factor, cross-sectional, and longitudinal analyses examined relationships between study variables.
Results:
Self-reported PLEs were best represented by the same three factors found in the general population: persecutory ideation, bizarre experiences, and perceptual abnormalities. Cross-sectionally, PLEs—particularly persecutory ideation—correlated with interview-rated attenuated psychotic symptoms and self-reported psychosis-proneness, depression, and anxiety. Longitudinally, baseline PLEs trended toward predicting 12-month change in positive attenuated psychotic symptoms (r = .29, pFDR = .058). Incrementally, baseline PLEs predicted 12-month change in positive and disorganized symptoms, when accounting for the effect of baseline positive symptoms and demographics.
Conclusion:
Three types of PLEs were valid in this CHR sample. Self-reported PLEs may be used not only to screen individuals for inclusion in the CHR classification, but also to characterize individuals within this population. Self-reported PLEs may help to forecast which CHR individuals will progress toward psychotic illness.
Keywords: Psychosis-risk, psychotic-like experiences (PLEs), dimensional, clinical high risk (CHR), longitudinal, confirmatory factor analysis (CFA)
Research has accrued over the past few decades to support a dimensional view of psychosis. For instance, 10–25% of adults in the general population have experienced hallucinations [1], 75–90% of psychotic experiences are transitory [2], and 17.5% of the population fit within a broad psychosis phenotype [3]. Moreover, recent reviews of genetic, neuropsychological, social, and environmental evidence have supported a “fully dimensional” model of psychosis [4–6]. In this model, the entire general population can be placed on the psychosis continuum, with the extent of an individual’s psychotic-like experiences (PLEs) classified as normative experience, non-clinical psychosis, attenuated psychotic symptoms, or clinical psychotic symptoms (see Figure 1).
Figure 1.
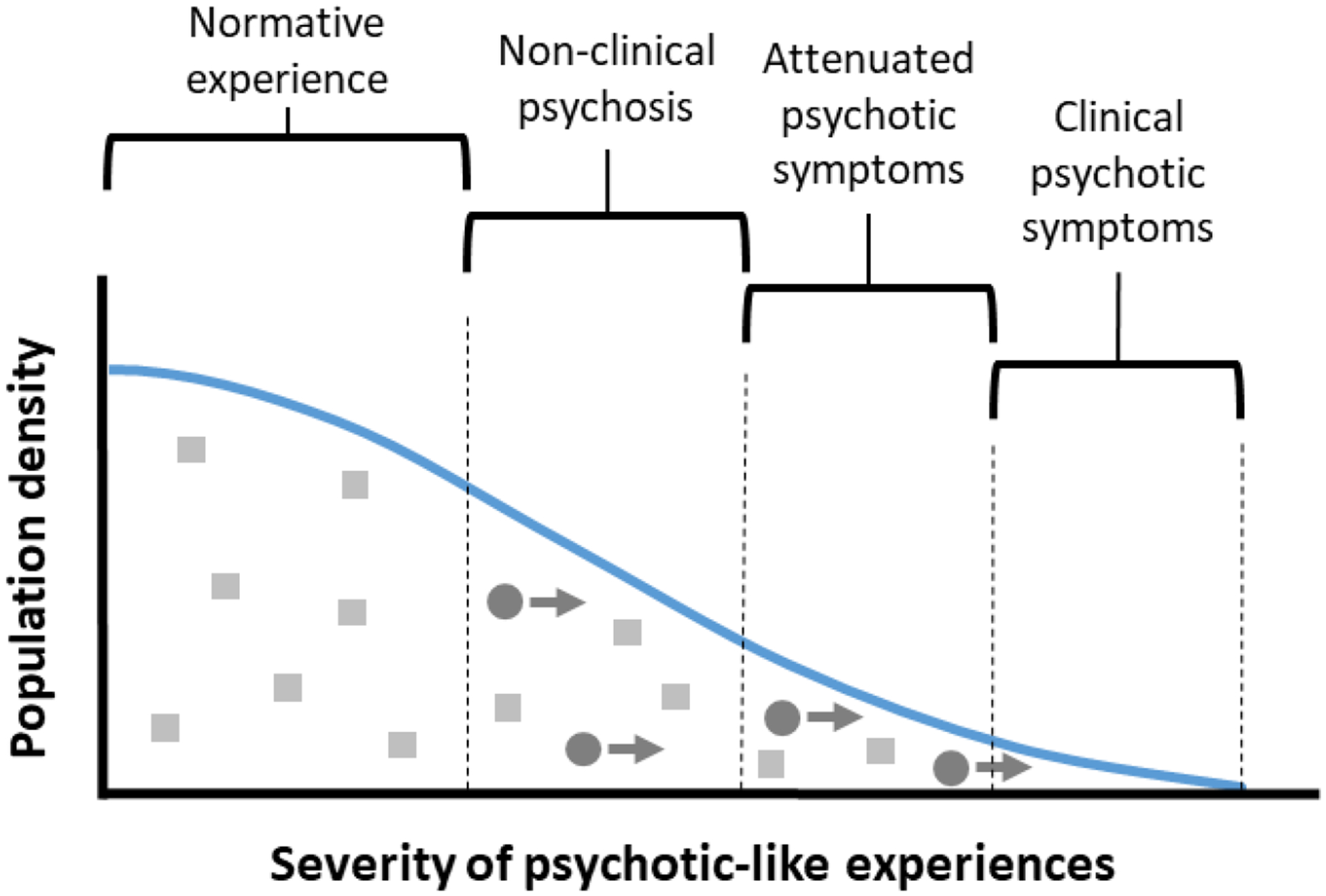
A hypothetical population distribution of psychotic-like experiences (PLEs) in a fully dimensional model of psychosis. In this model, PLEs are continuously distributed. As they become more severe, they are classified first as non-clinical psychosis, then as attenuated psychotic symptoms, and finally as clinical psychotic symptoms. Light-coloured squares represent individuals who experience stable, trait-like levels of PLEs; dark-coloured circles represent individuals who experience increasingly severe PLEs over time and are more likely to convert to a psychotic disorder.
This has important implications for individuals at clinical high-risk (CHR) for psychotic disorders. CHR individuals are those who are not diagnosed with a psychotic disorder, but are considered to be at high risk due to attenuated psychotic symptoms, brief intermittent psychotic symptoms, or genetic risk and functional decline [7]. CHR individuals have a greatly increased incidence of psychotic disorders, with 10 – 40% converting to psychotic disorders within 24 months [8–10]. Despite this alarming conversion rate, the inverse is also true: 60 – 90% of CHR individuals do not develop a psychotic disorder within this timeframe. This is in line with the fully dimensional model, which predicts that some individuals should experience persistent levels of subclinical PLEs without clinically significant impairment, due to high resilience factors and low environmental stressors [2, 4, 11]. Following this model, the CHR classification likely contains two groups: individuals experiencing persistent, trait-like levels of subclinical PLEs (represented by light squares in Figure 1), and individuals progressing toward a psychotic disorder (dark circles in Figure 1).
Recently, self-reported PLEs have been suggested as a screening tool for psychosis-risk [12–15]. Two recent studies have used the Community Assessment of Psychic Experiences (CAPE[16], a fully dimensional measure of PLEs developed for the general population, as a screening tool for CHR [13, 14]. These studies find that cutoff points on the CAPE can identify individuals who are likely to be classified as CHR in a diagnostic interview. However, to date, no studies have examined clinical correlates of these self-reported PLEs within a CHR sample. This is particularly important because general population studies find PLEs to predict not only psychotic disorders, but also other forms of psychopathology including mood and anxiety disorders [17–22]. There is marked comorbidity with mood and anxiety disorders in CHR populations [23], and it is unclear to what extent high scores on self-reported PLEs in this population would reflect a specific vulnerability to psychosis, a general vulnerability to psychopathology, or both. To understand the role of self-reported PLEs in the CHR population, it is necessary to: (a) define relationships between specific types of PLEs and specific attenuated psychotic symptoms; (b) define relationships between PLEs and non-psychotic symptoms; and (c) determine whether PLEs predict symptom course over time.
Research in the general population has identified various types of self-reported PLEs. Early studies linked the positive subscale of the CAPE to psychopathology [24–26], and several studies have examined that subscale in the general population [17–19, 26–29]. Studies consistently find three factors resembling low levels of paranoia, delusions, and hallucinations, with some studies also finding one or two additional factors [18, 19, 26, 28]. The CAPE positive subscale has also been shortened to a 15-item version (CAPE-P15) with a consistent 3-factor structure of persecutory ideation (“paranoia”), bizarre experiences (“delusions”), and perceptual abnormalities (“hallucinations”; [27]. To date, one study has examined the factor structure of the CAPE-P15 in a CHR sample, replicating the three-factor structure and finding support for a general factor [14]. Because that study’s aim was to test the CAPE as a screening tool for CHR, the authors only analyzed the general factor [14]. This is appropriate when the CAPE is used as a screening tool. However, given the important conceptual links between PLEs in the normative population and the clinical psychotic population, it is crucial to understand the roles that types of PLEs play within the CHR population [30]. For instance, we would expect specific types of self-reported PLEs to map onto specific types of attenuated psychotic symptoms assessed by a diagnostic interview. Alternatively, if self-reported PLEs did not map onto specific types of attenuated psychotic symptoms, this would be a serious challenge to their construct validity in CHR populations. The current study’s first aim was to confirm the factor structure of the CAPE in a CHR sample and validate the factors through cross-sectional correlations with interview and self-report assessments of attenuated psychotic symptoms.
PLEs are associated not only with psychotic symptomatology, but also with non-psychotic symptomatology. They carry a three-fold increase in risk for any mental disorder, compared to a four-fold increase in risk for psychotic disorder [31]. In general population studies, PLEs—particularly persecutory ideation—are consistently associated with depression and anxiety [17–22]. Moreover, these types of PLEs have been found to decrease as depression remits over time [22]. In some cases, odd beliefs and suspiciousness are better understood not as the early stages of an emerging psychotic disorder, but as nonspecific markers of mental suffering [23]. PLEs thus seem to indicate two overlapping clinical dimensions: a general psychopathology dimension, and a specific psychotic disorder dimension [23]. This complicates their conceptual status in CHR populations, in which mood and anxiety disorders are also common [23, 32]. To what extent do PLEs in this population reflect a general vulnerability to psychopathology, a specific vulnerability to psychosis, or both? The current study’s second aim was to define relationships between self-reported PLEs, depression, and anxiety in a CHR sample.
Finally, the ultimate goals of psychosis-risk research are to predict, prevent, or postpone progression to psychosis [8]. One challenge is to identify individuals who are traveling through the “non-clinical psychosis” and “attenuated psychotic symptom” categories toward clinical psychosis (see Figure 1). Longitudinal studies have shown PLEs to predict progression toward psychotic disorders in the general population [25, 31, 33, 34]. Is this also the case within the CHR population? Prospectively, once an individual has been classified as CHR, are PLEs still relevant in predicting symptom course? If so, do they predict psychotic symptom course, nonpsychotic symptom course, or both? The current study’s third aim was to determine whether baseline PLEs predicted the course of psychotic, depressive, and anxious symptoms over 12 months.
In sum, the current study addressed three questions about psychotic-like experiences in 105 youth at clinical high risk for psychosis: first, were various types of psychotic-like experiences valid in this sample; second, cross-sectionally, how did these experiences relate to psychotic and nonpsychotic symptoms; and third, longitudinally, did these experiences predict change in psychotic and nonpsychotic symptoms over 12 months?
Method
Participants
Participants were 105 help-seeking community participants who were classified as CHR based on distressing and impairing experiences, assessed by the Structured Interview for Psychosis-Risk Syndromes [7]. Participants were recruited in two urban areas (Chicago, Illinois and Boulder, Colorado) by newspaper, transit, and Craigslist ads, e-mail postings, and community professional referrals. Participants were referred or self-referred based on unusual experiences such as suspiciousness, social withdrawal, or “mind tricks”, and distress associated with these experiences. It is important to note that they were recruited at a research clinic specializing in the psychosis prodrome, and not through any sort of speciality care system.
Participants included 48 females (45%) and 58 males (55%), with a mean age of 19.3 (SD = 2.12). Fifty-eight participants self-identified as white/Caucasian (54%), 26 as Hispanic/Latinx (24%), 9 as black/African American (8%), and 13 as interracial or other (12%). Participants had a mean of 13.01 (SD 1.97) years of education and participants’ parents had a mean of 16.01 (SD 2.31) years of education. Participants reported a median family income of $60,000 - $99,999 per year, with 31 participants (29%) reporting median family income of less than $40,000, and 32 participants (30%) reporting median family income of $100,000 or more. As is commonly found in CHR samples, there was significant comorbidity with symptoms of anxiety and depression. Fifty-five participants (51%) scored above the “moderate anxiety” cutoff on the BAI (≥16), while 38 participants (35%) scored above the “moderate depression” cutoff on the BDI-II (≥20).
Procedures
Self-report measures and clinical interviews were administered in person as part of a baseline assessment battery in ongoing research at two academic research clinic sites. Both sites were specialty research clinics within large universities, focused on early diagnosis and intervention for psychotic disorders. Clinical interviews were conducted by interviewers with multiple years of clinical experience who were blind to participants’ CAPE scores. Twelve-month follow-up data were available for a subset of participants (n = 70; 67%). Twenty participants (19%) were lost to follow-up, while 15 participants (14%) had not yet completed their follow-up assessments. The standard in the CHR field is to follow naturalistically treated patients [35], and participants were not enrolled in any treatment studies during this 12 month period and received treatment as usual from any pre-existing community providers. T-tests found no baseline differences in any study variables between participants who completed the 12-month follow-up and participants who were lost to follow-up. All procedures were approved by university Institutional Review Boards and all participants provided written informed consent.
Measures
Community Assessment of Psychic Experiences, Positive Scale (CAPE-P).
The CAPE is a 42-item self-report measure of psychotic-like experiences (PLEs), divided into positive, negative, and depressive dimensions [16]. The positive subscale contains 20 items, each of which is rated for frequency (1 = “Never” to 4 = “Nearly always”) and distress (1 = “Not distressed” to 4 = “Very distressed”). The CAPE positive frequency items have been used in previous research as a screening tool to identify CHR individuals, both in their original 20-item version and a reduced 15-item version (CAPE-P15;[13, 14]. The current study focused on the CAPE positive frequency items only.
Structured Interview for Psychosis-Risk Syndromes (SIPS).
The SIPS is a structured clinical interview assessing positive, negative, disorganized, and general attenuated psychotic symptoms [7]. This study analyzed the positive, negative, and disorganized SIPS subscales, as well as individual symptom scores for positive symptoms.
Psychosis-risk questionnaires.
To further validate the CAPE, the Prodromal Questionnaire-Brief Version (PQ-B) assessed self-reported psychosis-risk [36], while the Launay-Slade Hallucination Scale (LSHS) assessed predisposition toward hallucinations [37].
Depression and anxiety.
Two scales were administered to assess symptoms of depression and anxiety. The Beck Depression Inventory (BDI-II) assessed depressive symptoms [38], and the Beck Anxiety Inventory (BAI) assessed anxiety symptoms [39].
Data Analysis
This was an observational study with cross-sectional and longitudinal components. All analyses were carried out in the R statistical programming language (v3.5.1; [40], primarily using the psych (v. 1.8.10; [41] and lavaan packages (v. 0.6–3; [42]. A confirmatory factor analysis with maximum likelihood estimation compared 10 factor models which have previously been proposed for the CAPE. Model fit was compared via root mean square error of approximation (RMSEA), standardized root mean of the residual (SRMR), the comparative fit index (CFI), the Tucker-Lewis Index (TLI), the Akaike Information Criterion (AIC), and the Bayesian Information Criterion (BIC). Because models were not nested, we did not compare the models’ chi-squared statistics. Although fit statistics are most useful for comparing various models’ relative fit, rather than evaluating objective fit, traditional objective fit cutoffs are as follows: RMSEA < .08; SRMR < .08; CFI > .90; TLI > .95.
Sample size recommendations for CFA vary by the number of items, number of factors, and item communalities [43]. Nine out of the ten tested CFA models had 5 or more items per factor and 4 or fewer factors. With a realistic assumption of wide communality, the sample size of 105 is at the low end of the “good precision” range for these nine models [43]. The tenth model [26] was included for completeness, although its fit statistics are likely to be less reliable than those of the other models. To obtain stable estimates given the sample size, fit statistics were bootstrapped over 1,000 bootstrap samples using the Bollen-Stine method [44].
After determining the best-fitting factor model, we obtained scores for subtypes of PLEs by calculating the mean of the CAPE items that loaded onto each factor. The Shapiro-Wilkes test indicated that two of the PLE subtypes (Bizarre Experiences and Perceptual Abnormalities) were non-normally distributed. These variables were transformed via a rank-based inverse normal transformation, which has been shown to be more robust than nonparametric tests such as Spearman’s correlation [45].
We examined Pearson correlations between PLEs (full-scale scores and subtype scores), attenuated psychotic symptoms (SIPS-Positive symptoms and full-scale scores for the SIPS Positive, Negative, and Disorganized scales), psychosis-risk questionnaires (PQ-B, LSHS), depression (BDI), and anxiety (BAI). A sensitivity analysis indicated that the sample size of 105 would be powered at .80 to detect a correlation of |.192| or larger. All p-values were corrected for the false discovery rate using the Benjamini-Hochberg method [46]. As a supplemental analysis, we used Steiger’s Z-test of dependent correlations to test pairwise differences in the magnitude of correlations for the three types of PLEs.
All study variables were analyzed as continuous symptom severity scores, although individual SIPS symptoms were rated on ordinal scales ranging from 0 to 5. SIPS symptom ratings are commonly analyzed using parametric statistics, including by the SIPS’s authors [7]. Moreover, empirical analyses and simulations have shown that parametric tests are robust to ordinal data, and that differences between parametric and nonparametric tests are often trivial [47]. In this study, the choice of parametric vs. nonparametric tests did not substantially affect SIPS symptoms score analyses or interpretation. For simplicity, our main analyses of symptom data use parametric statistics to match the rest of our analyses. For completeness, corresponding nonparametric tests are provided in the supplemental material, Table S1.
To assess predictive validity, we first examined Pearson correlations between PLEs and difference scores in symptoms from baseline to 12-month follow-up. To assess incremental predictive validity, we then computed residualized change score analyses to examine the incremental effects of PLEs when holding SIPS attenuated positive symptom scores, age, sex, income, and education constant.
Results
Confirmatory Factor Analysis
Which of the CAPE factor models in the literature best fit this CHR sample? Bootstrapped fit statistics for 10 factor models appear in Table 1. Overall, the best-fitting model was the CAPE-P15 model derived from Capra et al. [27] with 15 items and three correlated factors for Persecutory Ideation, Bizarre Experiences, and Perceptual Abnormalities. Two modifications of this model, one which added correlated errors for several items [27] and another which used a bifactor framework to estimate a general factor and three orthogonal group factors [14], did not substantially improve model fit. A hierarchical omega analysis suggested the presence of a general factor (ωhierarchical = .59), although this general factor accounted for less variance than the general factors in previous bifactor studies of the CAPE-P15 (ωhierarchical > .80; [14, 48]. Because our primary research aim was a detailed analysis of PLEs in the CHR population, we analyzed both full-scale scores (representing a general factor) and subscale scores (representing correlated factors). Descriptive statistics for the full-scale CAPE-P15 (mean = 1.64, SD = 0.43) and the three subscales (Persecutory Ideation mean = 1.94, SD = 0.53; Bizarre Experiences mean = 1.48, SD = 0.46; Perceptual Abnormalities mean = 1.50, SD = 0.64) were similar to those previously reported for a sample of 256 youth seeking assessment for psychosis-risk [14].
Table 1.
CAPE Confirmatory Factor Analysis Fit Statistics (Bootstrapped Estimates)
| Reference | Items | Factors | RMSEA | TLI | CFI | SRMR | AIC | BIC |
|---|---|---|---|---|---|---|---|---|
| Capra, 2013 | 15 | 3 | .039 (.029) | .957 (.063) | .958 (.044) | .062 (.009) | 2,832 (89) | 2,919 (89) |
| Capra, 2013 | 15 | 3 + correlated errors | .039 (.029) | .959 (.061) | .961 (.039) | .061 (.009) | 2,834 (93) | 2.931 (93) |
| Bukenaite, 2017 | 15 | 3 specific + 1 general | .037 (.029) | .957 (.069) | .955 (.048) | .087 (.014) | 2,855 (87) | 2,937 (87) |
| Bukenaite, 2017 | 15 | 1 | .040 (.029) | .943 (.079) | .943 (.056) | .062 (.008) | 2,930 (84) | 3,009 (84) |
| Yung, 2006 | 18 | 3 | .044 (.028) | .928 (.081) | .931 (.061) | .067 (.009) | 3.805 (98) | 3.906 (98) |
| Wigman, 2011 | 20 | 5 | .045 (.027) | .930 (.071) | .936 (.053) | .066 (.008) | 3.920 (105) | 4,050 (105) |
| Yung, 2009 | 20 | 4 | .044 (.027) | .930 (.075) | .934 (.056) | .070 (.009) | 3,963 (101) | 4,083 (101) |
| Armando, 2012 [19] | 20 | 4 | .045 (.027) | .926 (.074) | .931 (.055) | .069 (.008) | 3,967 (103) | 4,089 (101) |
| Mark, 2016 | 20 | 3 | .044 (.027) | .928 (.075) | .931 (.058) | .068 (.008) | 3,986 (104) | 4,098 (104) |
| Stefanis, 2002 | 20 | 1 | .046 (.027) | .905 (.095) | .909 (.074) | .067 (.008) | 4,091 (101) | 4,195 (101) |
Note: N = 105. Bootstrapped estimates are means of r = 1000 bootstrap samples using the Bollen-Stine method, with standard deviations in parentheses. Best fit for each fit statistic indicated in bold. AIC and BIC are only comparable for models with the same number of items; best fit on AIC and BIC are indicated in bold for 15 items and 20 items. This test of the Wigman, 2011 model violated recommendations for minimum sample size in CFA, and its fit statistics should be considered less reliable than the other models’.
Cross-Sectional Analyses
How did PLEs relate to psychotic and nonpsychotic symptoms? Correlations between PLEs and clinical variables are shown in Table 2.
Table 2.
Pearson Correlations with 95% Confidence Intervals for Psychotic-Like Experiences and Clinical Variables
| Types of PLEs | |||||||
|---|---|---|---|---|---|---|---|
| Variable | M | SD | CAPE-P15 Full Scale | Pers. Id. | Biz. Exp. | Perc. Ab. | Steiger’s Z-test |
| SIPS Symptom Domains | |||||||
| Positive | 11.89 | 4.24 |
.38*** [.20, .53] |
.48*** [.32, .62] |
.21* [.02, .39] |
.32** [.14, .48] |
PI > BE** PI > PA* |
| Negative | 9.51 | 6.77 |
29** [.11, .46] |
.33** [.15, .49] |
.15 [−.04, .33] | .21* [.02, .39] |
PI > BE* |
| Disorganized | 5.02 | 3.49 |
.31** [.13, .47] |
.33** [.15, .49] |
.28** [.09, .45] |
.14 [−.06, .32] |
- |
| SIPS Positive Symptomsa | |||||||
| P1: Unusual thought content | 3.32 | 1.12 | .35** [.17, .51] |
.45*** [.28, .59] |
.26* [.07, .43] |
.17 [−.03, .35] |
PI > PA** PI > BE* |
| P2: Suspiciousness | 2.61 | 1.54 | .16 [−.04, .34] |
.25* [.07, .43] |
.01 [−.18, .20] |
.19 [−.01, .37] |
PI > BE** |
| P3: Grandiose ideas | 1.53 | 1.44 |
.22* [.03, .39] |
.34** [.16, .50] |
.14 [−.06, .32] |
.09 [−.10, .28] |
PI > PA* |
| P4: Perceptual abnormalities | 2.63 | 1.35 |
.37*** [.20, .53] |
.33** [.15, .49] |
.20 [.00, .37] |
54*** [.39, .66] |
PA > BE*** PA > PI* |
| P5: Disorganized communication | 1.80 | 1.34 | .11 [−.08, .30] |
.17 [−.03, .35] |
.10 [−.10, .28] |
.02 [−.17, .21] |
- |
| Psychosis-risk questionnaires | |||||||
| Psychosis-proneness | 20.88 | 23.46 |
.42*** [.25, .57] |
.41*** [.23, .56] |
.30** [.11, .46] |
.30** [.11, .46] |
- |
| Hallucination-Proneness | 21.02 | 10.45 |
.64*** [.51, .74] |
.45*** [.29, .59] |
.53*** [.37, .65] |
.63*** [.50, .74] |
PA > PI* |
| Depression and anxiety | |||||||
| Depression | 16.62 | 11.82 |
.43*** [.25, .57] |
.51*** [.35, .64] |
.23* [.04, .41] |
29** [.10, .46] |
PI > BE*** PI > PA* |
| Anxiety | 17.78 | 12.08 |
.31** [.12, .47] |
.30** [.12, .47] |
.26* [.07, .43] |
.17 [−.03, .35] |
- |
Note: N = 105. CAPE Biz. Exp. and Perc. Ab. were transformed via rank-based inverse-normal transformation to correct nonnormality. CAPE = Community Assessment of Psychic Experiences; SIPS = Structured Interview for Psychosis-Risk Syndromes; Psychosis-proneness = Psychosis Questionnaire-Brief Version; Hallucination-proneness = Launay-Slade Hallucination Scale; Depression = Beck Depression Inventory-II; Anxiety = Beck Anxiety Inventory. 95% confidence intervals shown in brackets.
SIPS symptom scores are ordinal data. For consistency, they are presented here with parametric statistics. We also tested them with non-parametric statistics (Spearman’s correlations). Results did not meaningfully differ. Nonparametric results with medians and IQRs are provided in the supplemental material, Table S1.
FDR-corrected p < .05;
FDR-corrected p < .01;
FDR-corrected p < .001.
Attenuated psychotic symptoms.
PLEs related to SIPS positive, negative, and disorganized symptom domains as well as three of five SIPS positive symptoms (unusual thought content, grandiose ideas, and perceptual abnormalities). There was also significant variability between the three types of PLEs. Follow-up tests (Steiger’s Z-test of dependent correlations) found that CAPE persecutory ideation preferentially related to SIPS positive and negative symptom domains. At the level of specific positive symptoms, CAPE persecutory ideation preferentially related to SIPS unusual thought content, suspiciousness, and grandiose ideas, while CAPE perceptual abnormalities preferentially related to SIPS perceptual abnormalities.
Psychosis-risk questionnaires.
PLEs related to measures of psychosis-proneness and hallucination-proneness. There was some variability between types of PLEs, with CAPE perceptual abnormalities preferentially relating to LSHS hallucination-proneness.
Depression and anxiety.
PLEs related to measures of depression and anxiety. There was some variability between types of PLEs, with CAPE persecutory ideation preferentially relating to depression.
Longitudinal Analyses
Did PLEs predict symptom course, defined as symptom change from baseline to 12-month follow up? Follow up data was available for a subset of participants (n = 70). Two outliers were excluded based on inspection of scatterplots and extreme values, leaving 68 participants. Longitudinal data were analyzed in two ways. First, we examined PLEs’ simple effects on symptom change through their correlations with 12-month difference scores. As shown in Table 3 and Figure 2, baseline PLEs may have predicted an increase in positive attenuated psychotic symptoms over 12 months, although this effect was at the trend level after FDR-correction, r(66) = .29, pFDR = .058. Baseline PLEs did not predict change in any other symptoms.
Table 3.
Pearson Correlations for Baseline Psychotic-Like Experiences and Symptom Course Over 12 Months (As Difference Scores)
| Types of PLEs | |||||||
|---|---|---|---|---|---|---|---|
| Variable | N | M | SD | CAPE-P15 Full Scale | Pers. Id. | Biz. Exp. | Perc. Ab. |
| Δ SIPS Positive | 66 | −1.34 | 4.00 |
.29† [.05, .50] |
.21 [−.03, .43] |
.21 [−.03, .43] |
.20 [−.04, .42] |
| Δ SIPS Negative | 68 | −1.41 | 5.73 | .07 [−.17, .30] |
−.01 [−.25, .23] |
.08 [−.16, .31] |
.12 [−.12, .35] |
| Δ SIPS Disorganized | 68 | −1.13 | 2.92 | .15 [−.09, .37] |
.06 [−.18, .30] |
.09 [−.15, .32] |
.19 [−.06, .41] |
| Δ Depression | 68 | −3.89 | 8.95 | .00 [−.24, .24] |
.00 [−.24, .24] |
.07 [−.17, .30] |
−.15 [−.37, .09] |
| Δ Anxiety | 68 | −2.31 | 11.16 | .09 [−.15, .31] |
.14 [−.10, .36] |
.03 [−.20, .26] |
.02 [−.21, .25] |
Note: CAPE Biz. Exp. and Perc. Ab. were transformed via rank-based inverse-normal transformation to correct non-normality. N is slightly different for different correlations due to missing data, which was removed by pairwise deletion. CAPE = Community Assessment of Psychic Experiences; SIPS = Structured Interview for Psychosis-Risk Syndromes; PQ-B = Psychosis Questionnaire-Brief Version; LSHS = Launay-Slade Hallucination Scale; Depression = Beck Depression Inventory-II; Anxiety = Beck Anxiety Inventory. 95% confidence intervals shown in brackets.
FDR-corrected p = .058
Figure 2.
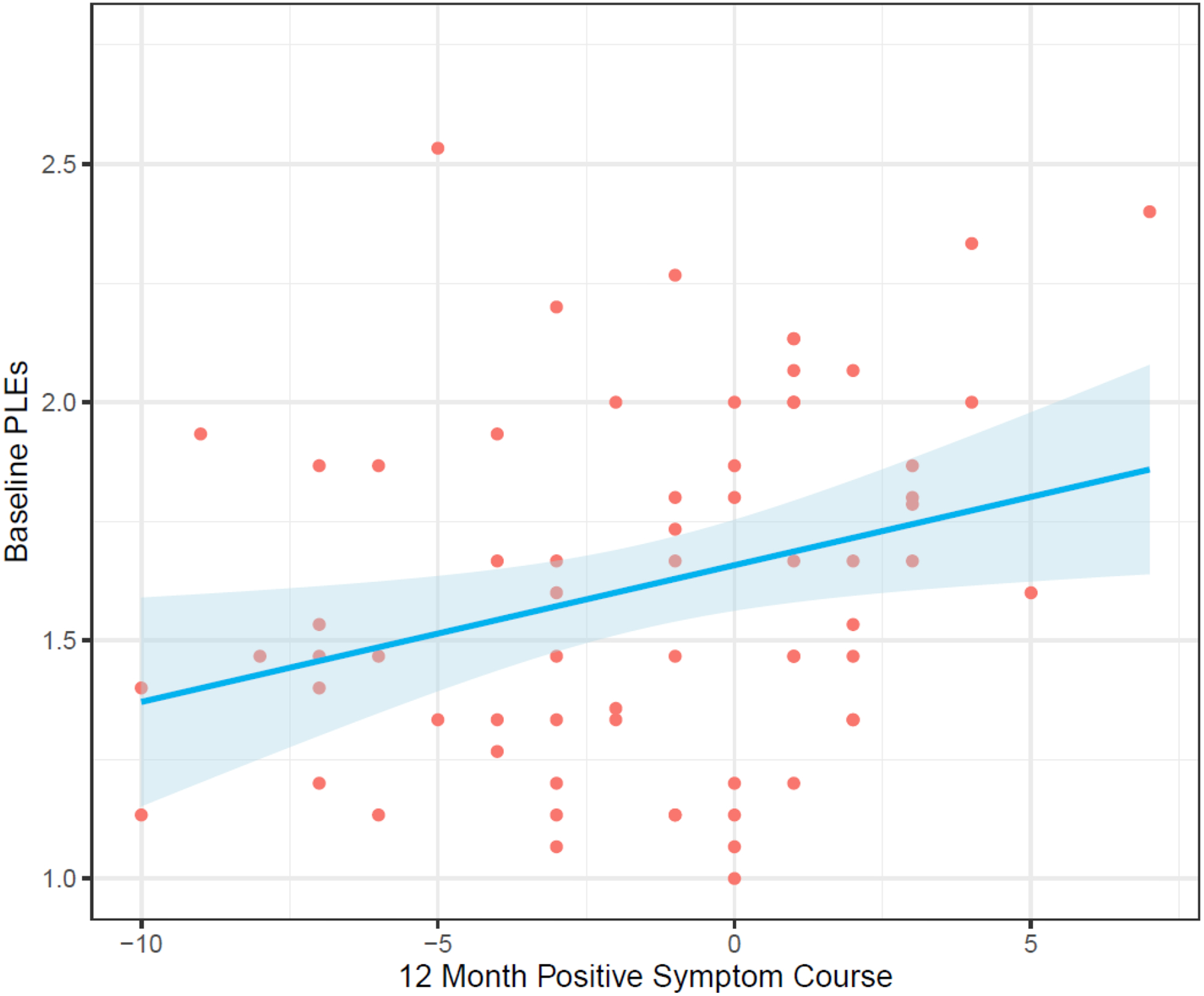
Baseline psychotic-like experience (PLEs) predicting progression of attenuated positive psychotic symptoms (12 month difference scores) in CHR youth, r(64) = .29, p = .018, pFDR = .058 (see Table 3). The shaded area indicates the standard error.
Given the substantial content overlap between types of PLEs and SIPS attenuated positive symptoms, we also tested whether PLEs would predict symptom change when statistically accounting for the effect of SIPS positive symptoms. In other words, did PLEs provide incremental predictive validity, above and beyond the predictive validity of SIPS positive symptoms? To answer this question, we computed simultaneous multiple regressions with 12-month follow up symptom scores as dependent variables, and baseline symptom scores, PLEs, SIPS positive scores, and demographics as predictors. * See Table 4 for details of each model. PLEs provided incremental validity in predicting SIPS positive symptoms and disorganized symptoms at 12-month follow up. The effect on positive symptoms was driven primarily by persecutory ideation PLEs, while the effect on disorganized symptoms was driven primarily by bizarre experiences PLEs. As shown in Table 5, persecutory ideation PLEs also provided incremental validity in predicting anxiety at 12-month follow up. To further validate these results, we re-ran longitudinal analyses excluding the top quartile of CAPE scorers, whose high scores on the CAPE could reflect the presence of attenuated psychotic symptoms (see Supplemental Material, Tables S2 and S3). In this analysis, point estimates were reduced, and PLEs still incrementally predicted positive symptoms, suggesting that attenuated psychotic symptoms did not drive the results.
Table 4.
Standardized Coefficients from Simultaneous Multiple Regressions Predicting Attenuated Psychotic Symptoms at 12-Month Follow Up
| Dependent Variable (12-Month Follow Up) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|
| Predictors (Baseline) |
SIPS Positive | SIPS Disorganized | SIPS Negative | ||||||
| CAPE Full scale | .27** | .35*** | .14 | ||||||
| CAPE Pers. Id. | .27** | .20† | |||||||
| CAPE Biz. Exp. | .15† | .31** | |||||||
| CAPE Perc. Ab. | .19* | .21* | |||||||
| SIPS Positive | .62*** | .62*** | .71*** | .67*** | .27* | .31* | .35** | .30* | .24* |
| SIPS Disorganized | .32** | .37** | .31** | .41*** | |||||
| SIPS Negative | .44*** | ||||||||
| Adj. R2 | .63 | .62 | .58 | .60 | .55 | .48 | .54 | .49 | .49 |
| F | 18.9 | 18.2 | 16.0 | 16.8 | 12.4 | 9.71 | 11.9 | 10.1 | 10.0 |
| DF | 6, 58 | 6, 58 | 6, 58 | 6, 58 | 7, 59 | 7, 59 | 7, 59 | 7, 59 | 7, 59 |
Note: All regression equations adjusted for age, sex, income, and education. CAPE Biz. Exp. and Perc. Ab. were transformed via rank-based inverse-normal transformation to correct non-normality. CAPE = Community Assessment of Psychic Experiences; SIPS = Structured Interview for Psychosis-Risk Syndromes.
p < .10,
p < .05,
p < .01,
p < .001.
All F-statistics, p < .001.
Table 5.
Standardized Coefficients from Simultaneous Multiple Regressions Predicting Non-Psychotic Symptoms at 12-Month Follow Up
| Dependent Variable (12-Month Follow Up) |
|||||
|---|---|---|---|---|---|
| Predictors (Baseline) |
Depression | Anxiety | |||
| CAPE Full scale | .17 | .23† | |||
| CAPE Pers. Id. | .28* | ||||
| CAPE Biz. Exp. | .17 | ||||
| CAPE Perc. Ab. | .04 | ||||
| SIPS Positive | .10 | .04 | −.01 | .09 | .12 |
| Depression | .51*** | ||||
| Anxiety | .45*** | .46*** | .47*** | .52*** | |
| Adj. R2 | .37 | .35 | .36 | .34 | .31 |
| F | 6.57 | 6.36 | 6.67 | 5.99 | 5.51 |
| DF | 7, 59 | 7, 62 | 7, 62 | 7, 62 | 7, 62 |
Note: All regression equations adjusted for age, sex, income, and education. CAPE Biz. Exp. and Perc. Ab. were transformed via rank-based inverse-normal transformation to correct non-normality. CAPE = Community Assessment of Psychic Experiences; SIPS = Structured Interview for Psychosis-Risk Syndromes; Depression = Beck Depression Inventory-II; Anxiety = Beck Anxiety Inventory.
p < .10,
p < .05,
p < .01,
p < .001.
All F-statistics, p < .001.
Finally, a smaller-than-expected proportion of CHR individuals had converted to a psychotic disorder at 12-month follow-up (n = 7, 10%). This very small sample size made statistical tests of converters vs. nonconverters impractical in this sample.
Discussion
Psychotic-like experiences (PLEs) connect the entire psychosis dimension, from normative experiences to clinical psychotic symptoms. However, until recently, little has been known about these experiences’ relevance for individuals at clinical high-risk for psychosis (CHR). Strong preliminary work has indicated that self-reported PLEs are a useful diagnostic screening tool for identifying CHR individuals [13–15]. Yet our understanding of PLEs in the CHR population has been incomplete without a clear picture of their relationships to clinical symptoms, both cross-sectionally and longitudinally. The current study addressed this need, finding that three types of PLEs were valid in a CHR sample, that PLEs cross-sectionally correlated with psychotic as well as non-psychotic symptoms, and that PLEs longitudinally primarily predicted 12-month course in positive psychotic symptoms.
Three types of psychotic-like experiences were valid in a clinical high-risk sample
Of various factor models in the literature, the best-fitting model for the CAPE positive subscale was the 15-item version (CAPE-P15) with three correlated factors: persecutory ideation, bizarre experiences, and perceptual abnormalities. Although the sample size was at the low end of the acceptable range for CFA analysis, these three types of PLEs are robustly supported in the literature on PLEs in the general population [27, 30, 48–50]. There has been some recent debate as to whether bifactor models are more appropriate for PLEs [14, 48]. A bifactor model did not improve model fit over a correlated-factors model in the current study. Some variance was accounted for by a common factor, but this was less than has been reported in previous bifactor studies of this scale (ωhierarchical = .59, compared to ωhierarchical > .80 in the prior studies; [14, 48]. This could be related to the higher proportion of CHR individuals in this sample compared to those prior samples, one of which was a non-clinical sample, and the other of which was 51% CHR and 49% low psychosis-risk. PLEs may be more homogeneous at lower intensities and more differentiated at higher intensities.
Cross-sectional relationships to self-report and interview measures confirmed the three PLE subscales’ convergent and discriminant validity. All three subscales correlated with positive attenuated psychotic symptoms assessed by the SIPS interview (rs = .21 to .48). Bizarre experiences specifically correlated with SIPS unusual thought content, and perceptual abnormalities specifically correlated with SIPS perceptual abnormalities. Persecutory ideation was the only subscale to correlate with SIPS suspiciousness. PLEs—particularly persecutory ideation—also correlated with negative and disorganized symptoms. Finally, all three subscales also correlated with self-report measures of psychosis-risk (PQ-B) and hallucination-proneness (LSHS). Perceptual abnormalities were the type of PLE most associated with hallucination-proneness. Overall, effect sizes were in the moderate range, around r = .30 [51]. Effect sizes were smallest for bizarre experiences PLEs. Effect sizes were largest for persecutory ideation PLEs or when PLE type aligned with the content of clinical measures, e.g., perceptual abnormalities PLEs with self-reported hallucination-proneness. The clinical variables in this study were related in a nomological network in theoretically meaningful patterns, showing good convergent validity, although bizarre experiences PLEs had the weakest links within the nomological network.
The persecutory ideation subscale correlated with four out of five SIPS positive symptoms (all except disorganized communication), suggesting that it may capture more than suspiciousness and incipient paranoia. Three of the six items on the persecutory ideation subscale seem to capture perplexed mood or non-persecutory ideas of reference (“have you ever felt as if people seem to drop hints about you or say things with a double meaning”, “have you ever felt as if some people are not what they seem to be”, and “have you ever felt that people look at you oddly because of your appearance”). This subscale may capture more general ideas of reference in addition to persecutory ideation.
Psychotic-like experiences related to depression and anxiety
Self-reported PLEs were cross-sectionally correlated with depression and anxiety, as well as attenuated psychotic symptoms. Of the three types of PLEs, persecutory ideation was most associated with depression. This mirrors several general population studies [17–22], but is somewhat surprising in a CHR sample, given the substantial content overlap between the SIPS and the CAPE. For instance, the content of the CAPE “persecutory ideation” factor and the SIPS “suspiciousness” section clearly overlap with one another. Yet the CAPE “persecutory ideation” factor was more closely associated with depression than with SIPS “suspiciousness” (r = .49 vs. r = .25, Z = −2.29, p = .022). CHR youth who reported higher levels of baseline PLEs reported higher levels not only of attenuated psychotic symptoms, but also of depression and anxiety. Cross-sectionally, self-report measures of PLEs in this population appear to capture experiences on a general psychopathology dimension as well as a specific psychosis dimension.
Psychotic-like experiences primarily predicted 12-month change in positive psychotic symptoms
The most important role for any CHR assessment tool is prospective. Whether used as a unidimensional screener or a multidimensional assessment tool, the most important question is whether CAPE scores predict symptom change over time. Longitudinal analyses of difference scores suggested that baseline PLEs likely predicted 12-month change in SIPS positive symptoms (see Table 3 and Figure 2). CHR youth who scored higher on self-reported PLEs at baseline seemed more likely to report increased positive attenuated psychotic symptoms 12 months later, but not increased negative, disorganized, depression, or anxiety symptoms.
Moreover, incremental validity analyses—statistically adjusting for the effect of demographics and attenuated positive symptoms—found that baseline PLEs predicted progression of attenuated positive and disorganized symptoms over 12 months. These analyses showed some specificity, with persecutory ideation PLEs predicting positive symptom course, bizarre experiences PLEs predicting disorganized symptom course, and perceptual abnormalities PLEs predicting both. In CHR populations, it is important to disentangle general vulnerabilities to psychopathology from specific vulnerabilities to psychosis. Self-report measures of PLEs may be a small piece of this puzzle, giving researchers and clinicians one more avenue to predict the progression of psychotic symptoms within CHR samples.
Strengths and Limitations
This study’s main strength is its combination of factor, cross-sectional, and longitudinal analyses. This allowed us to test PLEs’ construct, predictive, and incremental validity, and distinguish relationships to psychotic and nonpsychotic symptoms. The study’s main limitation is its sample size. Unique recruitment challenges tend to suppress sample sizes in CHR research [52], and the current sample size compares favourably to the one other sample which two previous studies have used to examine CAPE scores in CHR (N = 84 CHR and 81 non-CHR help-seeking individuals[13, 14]. Nevertheless, culture, cohort, or recruitment effects, or other idiosyncratic features of the current sample, could affect the study’s results. This study relied on widely used self-report and interview measures, and its findings should be straightforward to test in other participant samples. We would welcome direct replications in other samples—particularly samples drawn from other contexts (e.g., different cultures, different kinds of assessment settings). Other notable limitations are that were unable to control for effects of any treatment which participants may have received outside the current study during the 12-month follow-up, and that follow-up data were not available for the entire participant sample. We did not find baseline differences between participants who completed 12-month follow-up and participants who were lost to follow-up. Nevertheless, selection bias or treatment effects could have affected the longitudinal results.
Conclusion
Psychotic-like experiences theoretically connect the entire psychosis spectrum, ranging from normative experience to clinical psychotic symptoms. Yet little has been known about their status in individuals at clinical high risk for developing psychotic disorders. The current study characterized self-reported PLEs in a CHR sample in detail, showing that three types of PLEs were valid, that PLEs cross-sectionally related to psychotic and nonpsychotic symptoms, and that PLEs primarily predicted positive psychotic symptom progression over 12 months. PLEs are useful variables to track within CHR samples, and they may aid in efforts to identify those CHR individuals who are progressing toward psychosis.
Supplementary Material
Acknowledgements:
The authors wish to express their gratitude to the study participants. This work was supported in part by the Canadian Institutes of Health Research (DFS-152268 to HRC) and by the National Institutes of Health (R01MH112545-01, R01MH116039-01A1, and R01MH094650 to VAM).
Funding
This work was supported in part by the Canadian Institutes of Health Research (DFS-152268 to HRC) and by the National Institutes of Health (R01MH112545-01, R01MH116039-01A1, and R01MH094650 to VAM). The funding sources were not involved in study design, analysis, or manuscript writing.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Ethical Statement
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Availability of Data, Code, and Material
The data and analysis code that support the findings of this study are available from the corresponding author upon reasonable request. All measures are widely available online.
Demographics included age, sex, income, and education.
References
- 1.Johns LC, van Os J (2001) The continuity of psychotic experiences in the general population. Clinical Psychology Review 21:1125–1141. 10.1016/S0272-7358(01)00103-9 [DOI] [PubMed] [Google Scholar]
- 2.van Os J, Linscott RJ, Myin-Germeys I, et al. (2009) A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness–persistence–impairment model of psychotic disorder. Psychological Medicine 39:179–195. 10.1017/S0033291708003814 [DOI] [PubMed] [Google Scholar]
- 3.van Os J, Hanssen M, Bijl RV, Ravelli A (2000) Strauss (1969) revisited: a psychosis continuum in the general population? Schizophrenia Research 45:11–20. 10.1016/S0920-9964(99)00224-8 [DOI] [PubMed] [Google Scholar]
- 4.DeRosse P, Karlsgodt KH (2015) Examining the Psychosis Continuum. Curr Behav Neurosci Rep 2:80–89. 10.1007/s40473-015-0040-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson MT, Seal ML, Pantelis C, Phillips LJ (2013) Evidence of a dimensional relationship between schizotypy and schizophrenia: A systematic review. Neuroscience & Biobehavioral Reviews 37:317–327. 10.1016/j.neubiorev.2013.01.004 [DOI] [PubMed] [Google Scholar]
- 6.Claridge G, Beech T (1995) Fully and quasi-dimensional constructions of schizotypy. In: Raine A, Lencz T, Mednick SA (eds) Schizotypal personality. Cambridge University Press, Cambridge, pp 192–216 [Google Scholar]
- 7.Miller TJ, McGlashan TH, Woods SW, et al. (1999) Symptom Assessment in Schizophrenic Prodromal States. Psychiatr Q 70:273–287. 10.1023/A:1022034115078 [DOI] [PubMed] [Google Scholar]
- 8.Fusar-Poli P, Borgwardt S, Bechdolf A, et al. (2013) The Psychosis High-Risk State: A Comprehensive State-of-the-Art Review. JAMA Psychiatry 70:107–120. 10.1001/jamapsychiatry.2013.269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fusar-Poli P, Cappucciati M, Borgwardt S, et al. (2016) Heterogeneity of Psychosis Risk Within Individuals at Clinical High Risk: A Meta-analytical Stratification. JAMA Psychiatry 73:113–120. 10.1001/jamapsychiatry.2015.2324 [DOI] [PubMed] [Google Scholar]
- 10.Fusar-Poli P, Bonoldi I, Yung AR, et al. (2012) Predicting Psychosis: Meta-analysis of Transition Outcomes in Individuals at High Clinical Risk. Arch Gen Psychiatry 69:220–229. 10.1001/archgenpsychiatry.2011.1472 [DOI] [PubMed] [Google Scholar]
- 11.Yung AR, Stanford C, Cosgrave E, et al. (2006) Testing the Ultra High Risk (prodromal) criteria for the prediction of psychosis in a clinical sample of young people. Schizophrenia Research 84:57–66. 10.1016/j.schres.2006.03.014 [DOI] [PubMed] [Google Scholar]
- 12.Hanssen MSS, Bijl RV, Vollebergh W, van Os J (2003) Self-reported psychotic experiences in the general population: a valid screening tool for DSM-III-R psychotic disorders? Acta Psychiatr Scand 107:369–377. 10.1034/j.1600-0447.2003.00058.x [DOI] [PubMed] [Google Scholar]
- 13.Mossaheb N, Becker J, Schaefer MR, et al. (2012) The Community Assessment of Psychic Experience (CAPE) questionnaire as a screening-instrument in the detection of individuals at ultra-high risk for psychosis. Schizophrenia Research 141:210–214. 10.1016/j.schres.2012.08.008 [DOI] [PubMed] [Google Scholar]
- 14.Bukenaite A, Stochl J, Mossaheb N, et al. (2017) Usefulness of the CAPE-P15 for detecting people at ultra-high risk for psychosis: Psychometric properties and cut-off values. Schizophrenia Research 189:69–74. 10.1016/j.schres.2017.02.017 [DOI] [PubMed] [Google Scholar]
- 15.Addington J, Stowkowy J, Weiser M (2015) Screening tools for clinical high risk for psychosis. Early Intervention in Psychiatry 9:345–356. 10.1111/eip.12193 [DOI] [PubMed] [Google Scholar]
- 16.Stefanis NC, Hanssen M, Smirnis NK, et al. (2002) Evidence that three dimensions of psychosis have a distribution in the general population. Psychological medicine 32:347–358. 10.1017/S0033291701005141 [DOI] [PubMed] [Google Scholar]
- 17.Yung AR, Buckby JA, Cotton SM, et al. (2006) Psychotic-Like Experiences in Nonpsychotic Help-Seekers: Associations With Distress, Depression, and Disability. Schizophr Bull 32:352–359. 10.1093/schbul/sbj018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yung AR, Nelson B, Baker K, et al. (2009) Psychotic-Like Experiences in a Community Sample of Adolescents: Implications for the Continuum Model of Psychosis and Prediction of Schizophrenia. Aust N Z J Psychiatry 43:118–128. 10.1080/00048670802607188 [DOI] [PubMed] [Google Scholar]
- 19.Armando M, Nelson B, Yung AR, et al. (2012) Psychotic experience subtypes, poor mental health status and help-seeking behaviour in a community sample of young adults. Early Intervention in Psychiatry 6:300–308. 10.1111/j.1751-7893.2011.00303.x [DOI] [PubMed] [Google Scholar]
- 20.Armando M, Nelson B, Yung AR, et al. (2010) Psychotic-like experiences and correlation with distress and depressive symptoms in a community sample of adolescents and young adults. Schizophrenia Research 119:258–265. 10.1016/j.schres.2010.03.001 [DOI] [PubMed] [Google Scholar]
- 21.Barragan M, Laurens KR, Navarro JB, Obiols JE (2011) Psychotic-like experiences and depressive symptoms in a community sample of adolescents. European Psychiatry 26:396–401. 10.1016/j.eurpsy.2010.12.007 [DOI] [PubMed] [Google Scholar]
- 22.Yung AR, Buckby JA, Cosgrave EM, et al. (2007) Association between psychotic experiences and depression in a clinical sample over 6 months. Schizophrenia Research 91:246–253. 10.1016/j.schres.2006.11.026 [DOI] [PubMed] [Google Scholar]
- 23.Fusar-Poli P, Nelson B, Valmaggia LR, et al. (2014) Comorbid Depressive and Anxiety Disorders in 509 Individuals With an At-Risk Mental State: Impact on Psychopathology and Transition to Psychosis. Schizophrenia bulletin 10.1093/schbul/sbs136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welham J, Scott J, Williams G, et al. (2009) Emotional and behavioural antecedents of young adults who screen positive for non-affective psychosis: a 21-year birth cohort study. Psychol Med 39:625–634. 10.1017/S0033291708003760 [DOI] [PubMed] [Google Scholar]
- 25.Chapman LJ, Chapman JP, Kwapil TR, et al. (1994) Putatively psychosis-prone subjects 10 years later. J Abnorm Psychol 103:171–183. 10.1037//0021-843x.103.2.171 [DOI] [PubMed] [Google Scholar]
- 26.Wigman JTW, Vollebergh WAM, Raaijmakers QAW, et al. (2011) The Structure of The Extended Psychosis Phenotype in Early Adolescence—A Cross-sample Replication. Schizophr Bull 37:850–860. 10.1093/schbul/sbp154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Capra C, Kavanagh DJ, Hides L, Scott J (2013) Brief screening for psychosis-like experiences. Schizophrenia Research 149:104–107. 10.1016/j.schres.2013.05.020 [DOI] [PubMed] [Google Scholar]
- 28.Wigman JTW, Vollebergh WAM, Jacobs N, et al. (2012) Replication of the five-dimensional structure of positive psychotic experiences in young adulthood. Psychiatry Research 197:353–355. 10.1016/j.psychres.2011.09.015 [DOI] [PubMed] [Google Scholar]
- 29.Mark W, Toulopoulou T (2016) Psychometric Properties of “Community Assessment of Psychic Experiences”: Review and Meta-analyses. Schizophr Bull 42:34–44. 10.1093/schbul/sbv088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Therman S, Ziermans TB (2016) Confirmatory factor analysis of psychotic-like experiences in a general population sample. Psychiatry Research 235:197–199. 10.1016/j.psychres.2015.12.023 [DOI] [PubMed] [Google Scholar]
- 31.Healy C, Brannigan R, Dooley N, et al. (2019) Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychological Medicine 49:1589–1599. 10.1017/S0033291719000485 [DOI] [PubMed] [Google Scholar]
- 32.Cowan HR, McAdams DP, Mittal VA (2019) Core beliefs in healthy youth and youth at ultra high-risk for psychosis: Dimensionality and links to depression, anxiety, and attenuated psychotic symptoms. Development and Psychopathology 31:379–392. 10.1017/S0954579417001912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Poulton R, Caspi A, Moffitt TE, et al. (2000) Children’s Self-Reported Psychotic Symptoms and Adult Schizophreniform Disorder: A 15-Year Longitudinal Study. Arch Gen Psychiatry 57:1053. 10.1001/archpsyc.57.11.1053 [DOI] [PubMed] [Google Scholar]
- 34.Krabbendam L, Myin-Germeys I, Hanssen M, et al. (2004) Hallucinatory experiences and onset of psychotic disorder: evidence that the risk is mediated by delusion formation. Acta Psychiatr Scand 110:264–272. 10.1111/j.1600-0447.2004.00343.x [DOI] [PubMed] [Google Scholar]
- 35.Addington J, Cadenhead KS, Cornblatt BA, et al. (2012) North American Prodrome Longitudinal Study (NAPLS 2): Overview and recruitment. Schizophrenia Research 142:77–82. 10.1016/j.schres.2012.09.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Loewy RL, Pearson R, Vinogradov S, et al. (2011) Psychosis Risk Screening with the Prodromal Questionnaire – Brief version (PQ-B). Schizophr Res 129:42–46. 10.1016/j.schres.2011.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Launay G, Slade P (1981) The measurement of hallucinatory predisposition in male and female prisoners. Personality and Individual Differences 2:221–234. 10.1016/0191-8869(81)90027-1 [DOI] [Google Scholar]
- 38.Beck AT, Steer RA, Brown GK (1996) Beck depression inventory. The Psychological Corporation [Google Scholar]
- 39.Beck AT, Epstein N, Brown G, Steer RA (1988) An inventory for measuring clinical anxiety: psychometric properties. Journal of consulting and clinical psychology 56:893. [DOI] [PubMed] [Google Scholar]
- 40.R Core Team (2018) R: A language and environment for statistical computing. R Foundation for Statistical Computing [Google Scholar]
- 41.Revelle W (2018) psych: Procedures for Psychological, Psychometric, and Personality Research. Northwestern University, Evanston, Illinois [Google Scholar]
- 42.Rosseel Y (2012) lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software 48:1–36 [Google Scholar]
- 43.Mundfrom DJ, Shaw DG, Ke Tian Lu (2005) Minimum Sample Size Recommendations for Conducting Factor Analyses. International Journal of Testing 5:159–168. 10.1207/s15327574ijt0502_4 [DOI] [Google Scholar]
- 44.Bollen KA, Stine RA (1992) Bootstrapping Goodness-of-Fit Measures in Structural Equation Models. Sociological Methods & Research 21:205–229. 10.1177/0049124192021002004 [DOI] [Google Scholar]
- 45.Bishara AJ, Hittner JB (2012) Testing the significance of a correlation with nonnormal data: comparison of Pearson, Spearman, transformation, and resampling approaches. Psychological methods 17:399–417. 10.1037/a0028087 [DOI] [PubMed] [Google Scholar]
- 46.Benjamini Y, Hochberg Y (1995) Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. Journal of the Royal Statistical Society Series B (Methodological) 57:289–300 [Google Scholar]
- 47.Norman G (2010) Likert scales, levels of measurement and the “laws” of statistics. Adv in Health Sci Educ 15:625–632. 10.1007/s10459-010-9222-y [DOI] [PubMed] [Google Scholar]
- 48.Núñez D, Arias V, Vogel E, Gómez L (2015) Internal structure of the Community Assessment of Psychic Experiences—Positive (CAPE-P15) scale: Evidence for a general factor. Schizophrenia Research 165:236–242. 10.1016/j.schres.2015.04.018 [DOI] [PubMed] [Google Scholar]
- 49.Capra C, Kavanagh DJ, Hides L, Scott JG (2017) Current CAPE-15: a measure of recent psychotic-like experiences and associated distress: A measure of recent PLEs. Early Intervention in Psychiatry 11:411–417. 10.1111/eip.12245 [DOI] [PubMed] [Google Scholar]
- 50.Capra C, Kavanagh DJ, Hides L, Scott JG (2015) Subtypes of psychotic-like experiences are differentially associated with suicidal ideation, plans and attempts in young adults. Psychiatry Research 228:894–898. 10.1016/j.psychres.2015.05.002 [DOI] [PubMed] [Google Scholar]
- 51.Cohen J (1992) A power primer. Psychological Bulletin 112:135–159 [DOI] [PubMed] [Google Scholar]
- 52.Addington J, Epstein I, Reynolds A, et al. (2008) Early detection of psychosis: finding those at clinical high risk. Early Intervention in Psychiatry 2:147–153. 10.1111/j.1751-7893.2008.00078.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


