Abstract
Background
With the Wuhan pandemic spread to India, more than lakhs of population were affected with COVID-19 with varying severities. Physiotherapists participated as frontline workers to contribute to management of patients in COVID-19 in reducing morbidity of these patients and aiding them to road to recovery. With infrastructure and patient characteristics different from the West and lack of adequate evidence to existing practices, there was a need to formulate a national consensus.
Materials and methods
Recommendations were formulated with a systematic literature search and feedback of physiotherapist experiences. Expert consensus was obtained using a modified Delphi method.
Results
The intraclass coefficient of agreement between the experts was 0.994, significant at p < 0.001.
Conclusion
This document offers physiotherapy evidence-based consensus and recommendation to planning physiotherapy workforce, assessment, chest physiotherapy, early mobilization, preparation for discharge planning, and safety for patients and therapist in acutec are COVID 19 setup of India. The recommendations have been integrated in the algorithm and are intended to use by all physiotherapists and other stakeholders in management of patients with COVID-19 in acute care settings.
How to cite this article
Jiandani MP, Agarwal B, Baxi G, Kale S, Pol T, Bhise A, et al. Evidence-based National Consensus: Recommendations for Physiotherapy Management in COVID-19 in Acute Care Indian Setup. Indian J Crit Care Med 2020;24(10):905–913.
Keywords: Chest physiotherapy, Coronavirus, COVID-19, Early mobilization, Physiotherapy, Rehabilitation
Preamble
From Wuhan as the pandemic COVID-19 affected India, several buildings and open grounds were converted to major COVID-19 hospitals to meet the rising needs. By mid-March 2020, India saw more than a lakh active cases of COVID-19. With increasing literature and experiences from the globe, rapid changes have been incorporated in the management of COVID-19. Physiotherapists being an integral part of the intensive care team have come forward as frontline warriors to contribute in the management of COVID-19. However, due to lack of consensus and few guidelines from the West, there have been different protocols to deliver physiotherapy care to patients admitted with COVID-19.
Purpose
To prepare an evidence-based guideline through national consensus on physiotherapy management of COVID-19 for India.
Consensus-building exercise has been undertaken to develop and provide recommendation by putting together current experiences and available evidence to physiotherapists working in the various settings for treatment of confirmed and or suspected COVID-19 patients in India.
Introduction
Physiotherapy is as an integral part of critical care management. The aim of physiotherapy in critical care is to prevent and manage the pulmonary complications and focus on early rehabilitation by reducing the immobilization complications.
Patients diagnosed with COVID-19 have primarily respiratory symptoms with oxygen desaturation as the hallmark. Presence of associated comorbidities such as diabetes mellitus, hypertension, thyroid dysfunction, obesity, and renal dysfunction increases their mortality and morbidity. The ABCDEF bundle of care recommends respiratory therapy or chest physiotherapy and early mobilization as an integral part that helps reduce the morbidity and mortality;1 however, in relation to COVID-19 the approaches for the same need to be studied. All physiotherapeutic approaches are aerosol-generating procedures (AGPs) and require close contact, raising safety concerns for the therapists. Very little is known about best evidence physiotherapy practices that would derive benefit to the patient in COVID-19.
With the constant dilemma of benefit vs harm, this document attempts at providing recommendation based on the available data and literature for better implementation of services in these testing times of the COVID pandemic.
Materials and Methods
These recommendations have been prepared based on available literature evidence and expert consensus. A systematic literature search, available guidelines, recommendations, and expert opinions using the following search terms were conducted: physiotherapy, COVID-19, coronavirus 2019, chest physiotherapy, critical care physiotherapy, ICU rehabilitation, and early mobilization. Multiple combinations using Boolean operators were used. Retrieved studies were evaluated and summarized by three independent reviewers. Feedback was obtained from physiotherapists working in various hospitals, handling COVID-19 patients, through telephonic conversations and e-mails. A physiotherapy clinical decision-making algorithm and recommendation was developed through the modified Delphi method.
Expert Consensus Process
Physiotherapy experts in the cardiorespiratory field across India were approached (N = 19). The experts consisted of both clinicians and academicians.
The first author (MJ) conducted a virtual meeting in mid-march to introduce the need for consensus for developing a COVID-19 PT recommendation considering the emerging need. Experiences of physiotherapists treating patients with COVID-19 were gathered and noted.
The first draft of algorithm and the recommendations were e-mailed to panel members with a checklist. Experts were requested to record their comments and recommendations on the form prepared to obtain the consensus.
Based on the expert opinions, the consensus statement and recommendations were modified. The modified document was mailed to the experts for the second round of consensus.
A third round of consensus was carried out and the documents were finalized. Multiple virtual discussions were conducted to reach a consensus. Intraclass coefficient of agreement between the experts was 0.994, significant at p < 0.001.
The consensus document was then submitted to Maharashtra State Council for Occupational Therapy and Physiotherapy for approval, which was approved by the council on June 11, 2020.
ISCCM guidelines were used to grade the recommendations2 and where there was no evidence it is mentioned as useful practice point (UPP) (Table 1).
Table 1.
Criteria for quality of evidence levels and grading of strength of recommendations used in formulation of current recommendations
| Quality of evidence | Level |
|---|---|
| Evidence from ≥1 RCT good-quality and well-conducted randomized control trial(s) or meta-analysis of RCTs | 1 |
| Evidence from at least one RCT of moderate quality or well-designed clinical trial without randomization; or from cohort or case-controlled studies | 2 |
| Evidence from descriptive studies, or reports of expert committees, or opinion of respected authorities based on clinical experience | 3 |
| Not backed by sufficient evidence; however, a consensus reached by the working group, based on clinical experience and expertise | UPP |
| Strength of recommendation | Grade |
| Strong: To do or not to do where the benefits clearly outweigh the risk or vice versa for most if not all the patients | A |
| Weak recommendations where benefits and risk are more closely balanced or are more uncertain. | B |
Scope
This consensus statement provides recommendations for physiotherapy management of COVID-19 in acute care setup with focus on respiratory care and early mobilization. Statements on safety precautions and post-recovery rehabilitation also included. Algorithms for decision-making pathway and symptomatic patient treatment are developed.
Understanding COVID-19
The newly emergent SARS-CoV-2 was first recognized in Wuhan, China, in December 2019, having a genetic sequencing of the virus closely related to the SARC virus.
The transmission of virus mainly occurs from symptomatic people by close contact through droplet transmission, direct contact transmission with infected individual, or contact with contaminated objects and surfaces.3 SARS-CoV infects lung epithelial cells causing lung injury due to the associated inflammatory response. Patients may present with acute respiratory distress syndrome (ARDS), COVID pneumonia, or fibrosis. Lung CT scan findings found to have multiple mottling and ground-glass opacity in bilateral lungs. Autopsy studies have shown vascular changes and thromboembolic phenomenon causing shunt effect.4 Cardiac complications like arrhythmias and myocardial injury are seen in COVID-19 similar to other CoVs, which may be mediated by proinflammatory markers.5,6 It is found that cardiac biomarkers are highly elevated suggesting acute cardiac injury in those with increased mortality, severe disease, and those requiring ventilatory support.6
A varied presentation of the disease with multiple system involvement and failure is documented. People with comorbidities are found to have more severe presentation and increased mortality.7 As per available literature, 40% people with COVID-19 show only mild or moderate symptoms. About 15% develop severe symptoms requiring supplemental oxygen therapy. Five percent of them are critical.4,8
Patient Classification
Asymptomatic
These are individuals with COVID-19 nucleic acid test positive, who do not have any clinical signs and symptoms, and have normal chest radiograph. Oxygen saturation is normal at rest and may not desaturate on activity.
Symptomatic
These individuals may have symptoms of acute upper respiratory tract infection (fever, fatigue, myalgia, cough, sore throat, runny nose, sneezing) or digestive symptoms (nausea, vomiting, abdominal pain, diarrhea). They may have normal saturation at rest but may desaturate with exercise or mobility.
Symptomatic patients were further classified (Table 2) as per severity of respiratory symptoms from the physiotherapeutic perspective depending on oxygen requirement and taking into consideration severity classification for COVID-19-MoHFW.9
Table 2.
Classification of symptomatic COVID-19 patients
| Severity | O2 saturation (SpO2) | Hemodynamic stability | O2 support | Other symptoms | CT chest |
|---|---|---|---|---|---|
| Mild pneumonia | Mild or no change at rest (SpO2 of 92–94%) | Stable | Low-flow oxygen | No | Normal |
| Moderate pneumonia | Drop in SpO2 during activity | Tachycardia and hemodynamic variability | High-flow oxygen (HFO) system/venturi mask | Fever, cough, breathlessness | Ground glass opacities and bilateral lung mottling |
| Severe | Needs high FiO2 and PEEP to maintain oxygenation | Unstable/altered hemodynamics needs respiratory support | Mechanical ventilator (MV) or noninvasive ventilation (NIV) | Altered mental status, Signs of ARDS (mild to severe)8 | ARDS changes |
| Critical | Needs high FiO2 and PEEP to maintain oxygenation | Unstable/altered hemodynamics needs respiratory support | Mechanical ventilator or on extracorporeal membrane oxygenation (ECMO) | ARDS, multiorgan failure, sepsis, shock | ARDS changes bilateral ground glass appearance |
Recommendations for Workforce Planning and Deployment of Physiotherapist [Level 3B]10,11
Though many hospitals in India are declared as dedicated COVID-19 hospitals, major hospitals manage both COVID-19 and non-COVID-19 patients. The need for rehabilitation of patients in the non-COVID-19 area may not be less emphasized. Hence, it is important to delegate different teams of physiotherapists in COVID and non-COVID areas with reduced movement internally between teams. Deployment of staff to treat patients in various places from quarantine centers to COVID wards and COVID ICUs should be based on the expertise and skill required.
Staff with skill and expertise in treating patients in intensive care unit (ICU) should be deployed for the purpose of treating patients in COVID-19 ICU, for consultation and training of therapist and graduates in management of COVID-19.
Physiotherapists not confident of working in acute care setup should be trained for treating COVID-19 patients with mild to moderate involvement, facilitate rehabilitation, and discharge pathways.
Learning resources and training to staff in the form of e-Learning package from the World Health Organization and World Confederation of Physical Therapy (WCPT), Centre for Disease Control and Prevention, and resources related to updates on COVID-19 exclusively should be provided.
It is mandatory to train all therapists in proper technique and sequence of donning and doffing of personal protective equipment (PPE), six steps of the handwashing technique, and disposal of biomedical waste as per institutional policy and Centre of Disease Control and Prevention guidelines to protect transmission and infection.
Due to fear of pandemic and anxiety over personal and family safety, adequate counseling and psychological support should be provided to improve the morale of therapists appointed in treating patients with COVID-19.
Physiotherapists who are judged to be at high risk should not be encouraged to enter the COVID-19 isolation area. This includes those who are older than 55 years of age, pregnant, immune-compromised, and having associated comorbidities of diabetes, cardiac disease, renal involvement, malignancy, respiratory disease, and anemia.
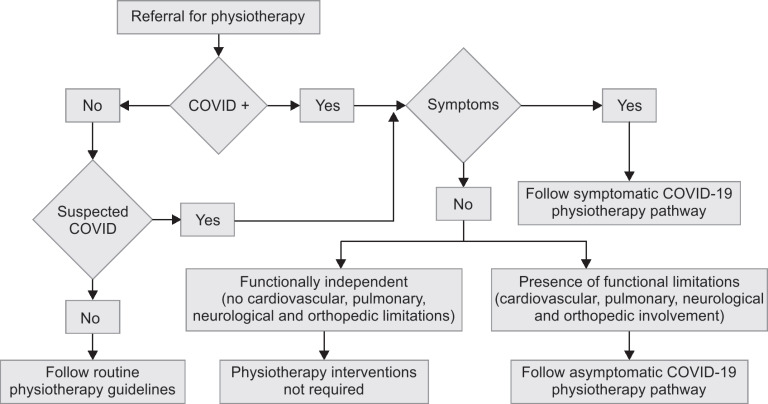
Recommendations for Physiotherapy Decision-Making [UPP]
- Upon getting the physiotherapy referral, a physiotherapist may follow the physiotherapy decision-making process flow (Flowchart 1) to categorize the patient and to determine the physiotherapy intervention process.
- COVID-19 physiotherapy decision-making process map categorized the patients depending up on the stage and the symptoms.
- Institution-based routine physiotherapy guidelines should be followed for patients who are not suspected of COVID-19.
- Suspected and diagnosed COVID-19 individuals should follow the positive process flow.12
Flowchart 1.
COVID-19 physiotherapy decision-making process
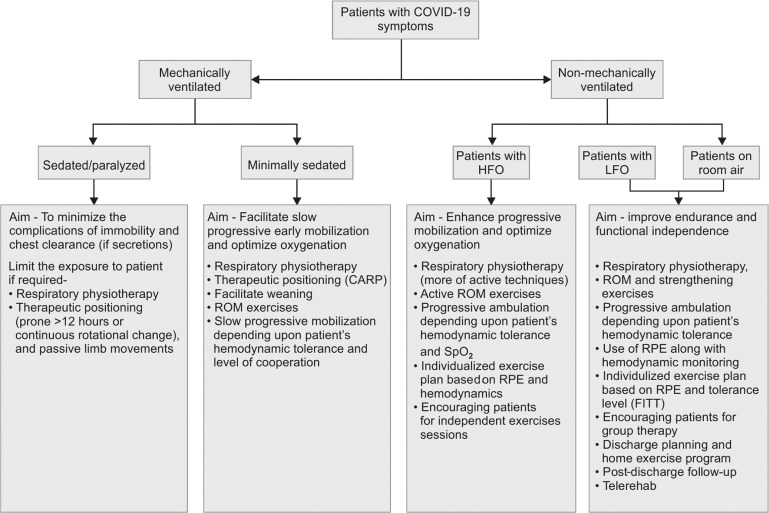
COVID-19 Physiotherapy (PT) Pathway [UPP]
The COVID-19 PT pathway is classified according to the symptoms.
COVID-19 PT Pathway (asymptomatic)
Patients diagnosed as COVID-19-positive without symptoms but having functional limitations due to any cardiovascular, pulmonary, neurological, or orthopedic dysfunctions (stroke, fractures, postsurgical, etc.) are considered in this category.
Patients in this category should follow institutional-based routine physiotherapy guidelines with complete comprehensive COVID-19 precautions (PPEs).
COVID-19 PT Pathway (symptomatic)
This pathway (Flowchart 2) categorized the patients to nonmechanically ventilated and mechanically ventilated.
Flowchart 2.
Physiotherapy pathway for symptomatic COVID-19 patients
- Nonmechanical ventilated
- Patient with HFO
- Patients with LFO
- Patients on room air
- Mechanical ventilated or on noninvasive ventilation
- Sedated/paralyzed
- Minimally sedated
Recommendations for Assessment and Screening
It is important that all patients be continuously monitored and assessed before, during, and after physiotherapy sessions [UPP].
- Physiotherapy screening [Level 3B]10,13–15
- All patients should be screened for presence of comorbidities like obesity, diabetes, hypertension, thyroid dysfunction, and associated musculoskeletal or neurological impairments.
- Screening for hemodynamic stability: Symptoms and signs of associated chest pain, presence of tachycardia or irregular rhythm, edema feet, and breathlessness suggestive of associated cardiac sequelae and myocarditis should be screened.
- Screening for respiratory distress: Signs of increased respiratory rate (>30), altered breathing pattern (increased use of accessory muscles) at rest, with change of position or with activity, should be observed.
- Screening for activity-induced desaturation: Physiotherapists working with COVID-19 patients have reported a drop in oxygen saturation even with patients having normal saturation at rest. As per unpublished observations based on experiences reported by physiotherapists, simple activities in bed or edge of bed have been reported to cause desaturation in patients with moderate to severe involvement. Hence, all patients should be screened for desaturation with activity. Patients with a fall of more than 3% in saturation or saturation of <96% at rest should be observed closely. Patients with HFO therapy are observed to desaturate rapidly. Need for oxygen titration should be assessed and discussed with the physician.
- Screening for readiness to mobilization: The sedation level and awakening should be evaluated for patients on mechanical ventilation or noninvasive ventilation to assess readiness for early mobilization. Safety parameters for mobilization should be considered (refer Section “Safety for patients”).
- Assessing for mobility and function: Ambulatory stable patients should be assessed for musculoskeletal impairments of mobility, strength, endurance, and balance during recovery from the acute phase and for rehabilitation. Physiotherapists working with COVID patients have observed excessive lower extremity weakness and fatigue in patients recovering from the illness [UPP].
- Quick assessment of functions like 30-second chair sit and rise, isometric grip strength, and one-leg stance can be done in patients with mild severity and/or during the discharge phase. It is recommended to do a predischarge functional test as timed up and go, L-test, or 6-minute walk test depending on patients’ parameters and ambulation to guide planning of home program and rehabilitation [Level 2B].16,17
- As many patients have complained of fatigue, it is recommended that fatigue or level of exertion can be evaluated using the Borgs scale or visual analog scale (VAS) [Level 2B].18
- It is recommended to screen all patients on mechanical ventilation for agitation and delirium, cognitive impairment, and impairments of integumentary system, as these can occur in patients with prolonged ICU stay. Acute respiratory distress syndrome, Sepsis, increased age, prior cognitive deficit, and delirium can lead to increased risk of cognitive impairment and post-ICU stress disorder.19 Hence, it is recommended to use the Richmond Agitation Sedation Scale (RASS)20 for decision making of active mobility within safety limits. Pressure areas should be screened for developing of pressure sores, if any [Level 2A].
Recommendations for Physiotherapeutic Interventions
Physiotherapeutic maneuvers include body positioning to improve ventilation-perfusion ratio and oxygenation, airway clearance to clear secretions in the airway, and alveoli and early mobilization to combat ill effects of deconditioning and prevent critical care illness and myopathy and improve function and quality of life.21 A clear need for clinical indication of physical therapy intervention should be established following screening and evaluation.
Therapeutic Positioning
It is recommended to encourage awake active prone positioning “COVID awake repositioning proning protocol” called as “CARP” (Table 3)22 in mild to moderate severity as it can help in improving oxygen saturation, delay, or reduce the need for intubation and intensive care in pneumonia due to COVID-19 [Level 2B].23,24
An extended semi-sitting or sitting position is favorable when proning not possible due to patient discomfort or obesity [Level 2B].25,26
It has been observed that not all patients benefit in prone; hence, the best saturation position should be accordingly advised [UPP].
When possible and in close collaboration with the team, a 24-hour position rotation chart can be provided, which favors alternations of the lateral decubitus, to semi-prone to prone position [UPP].
For maximum benefit, position is to be maintained at least for 30 minutes to an hour. Cushions/aids can be used during prone positioning that supports the body and avoid excessive active muscles work that causes undue fatigue [Level 3B].27
Dyspnea-relieving positions for patients with mild to moderate symptoms in sitting with fixation of upper extremity to facilitate breathing may be of help in patients with increased respiratory rate and distress [Level 2B].28
In severe and critical patients that are sedated, proning is a mode of therapy for 12–16 hours. Safe application of the prone position during ventilation requires sufficient human resources and expertise [Level 3B].27 In absence of continuous rotation beds and poor resource, a best possible position should be attained.
The ventilator tubing should be prevented from getting disconnected accidentally and causing aerosol liberation. In such a scenario, the physiotherapist plays a role in recommending a continuous rotational positional change. Chest physiotherapy may not be indicated in patients who are critical on mechanical ventilator with high PEEP [Level 1A].29
Table 3.
COVID awake repositioning/prone protocol (CARP)22
| 30 minutes to 2 hours full prone |
| 30 minutes to 2 hours right side lying |
| 30 minutes to 2 hours propped-up sitting |
| 30 minutes to 2 hours left side lying |
| 30 minutes to 2 hours prone |
CARP-Janus General Medicine Resuscitation and Acute Critical Care
Respiratory Physiotherapy
Patients Likely to Benefit from Respiratory Physiotherapy [Level 2B]10,13,14,30,31
Productive cough and presence of airway secretions.
Associated respiratory morbidity or diabetes
Secretions with ineffective cough
Improved saturation response to positioning, reduced fatigue, and dyspnea
Being weaned from ventilator support
Prolonged bedrest and immobile
Any functional limitation
Patients with Minimum Benefit from Respiratory Physiotherapy
Patients having acute ARDS infection with a respiratory rate > 30 beats/minute; SpO2 < 90% despite oxygen support, a FiO2 of >50% on a noninvasive mechanical ventilator, and PEEP/CPAP > 10 cm H2O, and already proning for 12 hours and deeply sedated.32
Diagnosed of COVID-19 with severe hypoxemia and increased distress requiring intubation [Level 3B].32
Breathing Exercises
In patients with mild to moderate symptoms, breathing control and deep breathing exercises with diaphragm activation are recommended [Level 3B].33 It is important to recruit and expand basal alveoli to prevent atelectasis [Level 3B].34 Diaphragm activation with scoop technique using patients own hand for proprioceptive feedback can be encouraged [UPP]. Similarly, diaphragm activation to expand posterior lung segments should be encouraged. Charts and audiovisual aids are found facilitatory in educating patients regarding breathing techniques [UPP].
Purse lip breathing can help alleviate dyspnea and prevent bronchospasm.35,36 On oxygen support with rebreathing bag or NIV patient may find difficult to use Purselip breathing [Level 3B].
Airway Clearance Techniques
Active cycle of the breathing technique is recommended as a method of airway clearance for patients with secretion.10,13,31 In patients with mild to moderate severity in presence of exudative pneumonia, it would help to clear secretions [Level 3B].
Suctioning should be performed using a closed inline suction system [Level 1B]37.
Nebulization
Inhaled therapy using a pneumatic jet nebulizer is not recommended [Level 3A].38 A preferred option is to use dry inhalers or ultrasonic nebulizers connected to the mechanical ventilator in a closed circuit, without removing the antimicrobial filter on the expiratory branch of the circuit [Level 3B].39
Early Mobilization
It is recommended to begin with an early passive or active assisted mobilization program based on patients level of cooperation/orientation, oxygen saturation, and hemodynamic stability [Level 3A].10,14,15,40,41 As COVID-19 induces inflammatory response, due care and caution has to be exercised while planning any exercises [UPP].
Gradual progression with very low intensity depending on saturation, symptoms, permissible level of oxygen therapy, and hemodynamic response should be encouraged [Level 3B].42
Exercises to progress from assisted to active mobilization at the edge of bed and out of bed. Progression of the exercise should depend on level of cooperation, hemodynamic stability, exercise tolerance, and neuromuscular parameters. Allow adequate rest during exercises till discharge and stabilization [Level 3B].10,14,15,40
Graded Mobilization
With very mild symptoms due to COVID-19, it is recommended to consider limiting activity to light activity within functional requirement of metabolic equivalents but limit sedentary periods. If needed, oxygen therapy may be initiated in consultation with the physician if patient desaturates. Increase rest periods if symptoms deteriorate. Prolonged exhaustive or high-intensity training should be avoided [Level 3B].43
Asymptomatic patients may be encouraged to achieve at least 10 minutes of continuous physical activity or structured exercise without fatigue or desaturation below 90% [Level 3B].44 Adequate rest periods should be encouraged to avoid undue fatigue.
Exercises may progress to 20 minutes applying principles of frequency, intensity, time, and type after 3 weeks of acute episode and once patient is asymptomatic to allow adequate recovery [Level 3B].42
Mobility aids used should be disinfected. Use of light thera-bands depending on the muscle strength is recommended during the predischarge phase provided there is no desaturation [UPP].
Use of Respiratory Devices
Various devices for facilitation in inspiratory and expiratory exercises are available. However, their use in COVID-19 is not known. There is no evidence so far on the use of below-mentioned devices in treating patients with COVID-19. All devices are single patient use and a strict protocol of biomedical hazardous waste disposal should be maintained. These devices cannot be shared between patients [Level 3A].11
Incentive spirometer that facilitates inspiration can be used for contactless therapy in patients with oxygen via nasal prong or cannula or off oxygen [Level 3B].36 If it stimulates or precipitates cough, it is to be discontinued. Single-use device not to be shared within patients [Level 3A].11
For patients with oxygen support through face mask, it is not recommended to remove the support for use of devices as it is observed to lead to desaturation [UPP].
In patients with secretions, oscillatory PEP device to mobilize secretions can be used as contactless mode of therapy three to four times in a day [Level 3B].36 For patients with oxygen support through face mask, it is not recommended to remove the support for use of devices as it may lead to desaturation. Patient affordability and ease of use have to be considered before prescription of devices [UPP].
In patients on ventilator with copious secretions, high-frequency chest wall compression (HFCC) or mechanical vibrator can be applied as contactless mode after ensuring hemodynamic stability [Level 3B].36
Inspiratory muscle trainer may be used after ensuring hemodynamic stability for improving respiratory muscle strength for contactless training and ensuring oxygen support [Level 3B].36
Recommendation for Relaxation
A general body relaxation may help patients to reduce anxiety and stress related to disease and isolation. Relaxation should be given in position of comfort without undue breathlessness. Audio recordings and soothing music can be used for the same in the isolation facility and quarantine area [Level 2B].45
Recommendations for Group Therapy
Patients with mild to moderate severity on LFO, NRBM or room air should be encouraged for group therapy. Patients on room air should use a three ply mask during therapy sessions. Group therapy sessions provide encouragement and motivation to perform exercise and save on therapist contact time. Monitoring of oxygen saturation can be carried out using a finger probe pulse oximeter [UPP].
Safety Recommendations for Patients and Physiotherapists
Safety for Patients
Physiotherapist should perform a safety screening to determine whether the patient is fit for activities and mobilization and the factors should include:
- Cardiovascular and respiratory factors [Level 3A]14,15,46
- No new onset of cardiac arrhythmia or myocardial ischemia
- No new or increase in ionotropic infusion
- Heart rate >40 or <120 bpm
- Systolic blood pressure >90 or <180 mm Hg
- Mean arterial pressure ≥60
- Respiratory rate >10 or <40 bpm
- Oxygen saturation ≥90%
- Other factors
- Pain: NRS <3
- GCS score >13
- Hemoglobin level >7 g/dL
- Platelet count level >21 × 103/uL
- Oral body temperature <38.5°C
- Blood glucose level 3.5–20 mmol/L
- Potassium level 3.5–5.5 mEq/L
- No lines that makes mobilization unsafe
- Safe environment and appropriate staffing
Assess patient's response during activity and mobilization to know whether the patient is tolerating the intervention [Level 3A].15
- Signs of intolerance include [Level 3A]:14,15
- Pain: NRS ≥ 3
- Reduced level of consciousness
- Increase in patient's heart rate of 30 bpm over baseline with an upper limit ≤ 120 bpm
- Decrease systolic blood pressure >10 mm Hg during exercise
- Diastolic blood pressure ≥110 mm Hg
- No rise in systolic blood pressure and heart rate
- Increasing ectopic beats
- Arrhythmias
- Signs and symptoms of myocardial infarction
- Symptoms of respiratory distress
- Patient appears distressed
All invasive lines, ventilator tubings, to be taken care of during positioning [UPP].
Patient should not be disconnected from the circuit at any point of time [UPP].
Group therapy in mild to moderate should be with safe distancing and patients with mask [UPP].
As all physiotherapy procedures are aerosol generating, physiotherapists should weigh the risk vs benefit during application of interventions [UPP].
Safety Recommendations for Therapists
Healthcare workers performing aerosol-generating procedures on patients with COVID-19 should wear fitted respirator masks (N-95) instead of surgical masks along with other PPE and eye protection [Level 3A].11
Aerosol-generating procedures include chest percussion, vibration, prone positioning, high-flow nasal oxygen, noninvasive ventilation, nebulization, open suctioning, cuff inflation deflation, ventilator tube changing, breathing exercise, airway clearance/lung reexpansion techniques, incentive spirometer, and any activities that can result in expectoration of sputum or facilitate cough like exercise training and mobilization. Since airway clearance causes massive droplet dispersion, airway clearance procedures should be administered only when considered strictly needed for clinical improvement of the patient [Level 3A].33
The contactless mode of therapy should be encouraged where feasible. Physiotherapists preferably use posterior approach and maintain a distance >2 m and away from the “blast zone” or line of cough [Level 3A].32
Tools for patient education such as charts in language understood, audio-visual aids, and mike systems should be used to encourage contactless therapy [UPP].
It is essential that cough etiquettes (covering mouth with hands, handkerchief, coughing in sleeves with folded elbows) are taught to all the patients. Patient should be wearing a mask during all physiotherapeutic maneuvers [Level 3A].10
The PPE should not be removed or adjusted and correctly worn for the duration of exposure to potentially contaminated areas [UPP].
All personal accessory items like rings, earrings, phone, and writing material should be removed before donning and entering the COVID zone. Dedicated stethoscopes and pulse oximeters should be used within isolation areas. Reusable PPE items, i.e., goggles and face shields, must be cleaned and disinfected using guidelines for CDC [Level 3A].12
Recommendations for Discharge Planning Following Recovery
COVID-19 mimics other Co-V outbreaks, hence evidences and experiences of the past having demonstrated an impaired quality of life associated with emotional distress may be expected as long-term sequelae in COVID 19 survivors. A prolonged critical care stay associated with lung changes would need rehabilitation to improve quality of life.36,47 Most patients with COVID-19 would need pulmonary rehabilitation approach and follow-up. Home program with education, counseling, tailored exercise program, and healthy nutrition along with telerehabilitation should be encouraged accordingly [UPP].
Summary
The current pandemic being a challenge in itself, it is necessary that utmost precautions are taken while delivering the best therapy after adequate clinical reasoning. The intention of these recommendations is to deliver safe care to the patient with holistic approach to prevent morbidity as well as protect the physiotherapist by adhering to safety guidelines. The therapist needs to weigh the benefit achieved vs harm to optimize treatment with a holistic approach. The recommendations are subject to update with more available literature.
Footnotes
Source of support: Nil
Conflict of interest: None
References
- 1.Castro AAM, Calil SR, Freitas SA, Oliveira AB, Porto EF. Chest physiotherapy effectiveness to reduce hospitalization and mechanical ventilation length of stay, pulmonary infection rate and mortality in ICU patients. Respir Med. 2013;107(1):68–74. doi: 10.1016/j.rmed.2012.09.016. DOI: [DOI] [PubMed] [Google Scholar]
- 2.Khilnani GC, Zirpe K, Hadda V, Mehta Y, Madan K, Kulkarni A, et al. Guidelines for antibiotic prescription in intensive care unit. Indian J Crit Care Med Peer-Rev Off Publ Indian Soc Crit Care Med. 2019;23(Suppl 1:):S1–S63. doi: 10.5005/jp-journals-10071-23101. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Clinical management of COVID-19. https://www.who.int/publications-detail-redirect/clinical-management-of-covid-19 https://www.who.int/publications-detail-redirect/clinical-management-of-covid-19 Accessed June 28, 2020.
- 4.Lodigiani C, Iapichino G, Carenzo L, Cecconi M, Ferrazzi P, Sebastian T, et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9–14. doi: 10.1016/j.thromres.2020.04.024. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophy. 2020;31(5):1003–1008. doi: 10.1111/jce.14479. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Siddamreddy S, Thotakura R, Dandu V, Kanuru S, Meegada S. Corona virus disease 2019 (COVID-19) presenting as acute ST elevation myocardial infarction. Cureus J Med Sci. 2020;12(4) doi: 10.7759/cureus.7782. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293–1304. doi: 10.1056/NEJMoa1011802. DOI: [DOI] [PubMed] [Google Scholar]
- 8.Team TNCPERE. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) — china, 2020. China CDC Wkly. 2020;2(8):113–122. doi: 10.46234/ccdcw2020.032. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.MoHFW | Home. https://www.mohfw.gov.in/ https://www.mohfw.gov.in/ Accessed July 10, 2020.
- 10.Thomas P, Baldwin C, Bissett B, Boden I, Gosselink R, Granger CL, et al. Physiotherapy management for COVID-19 in the acute hospital setting: clinical practice recommendations. J Physiother. 2020;66(2):73–82. doi: 10.1016/j.jphys.2020.03.011. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rao B, Singh S, Chacko J, Mani R, Wattal C, Mehta Y, et al. Critical care for COVID-19 affected patients: position statement of the Indian society of critical care medicine. Indian J Crit Care Med. 2020;24(4):222–241. doi: 10.5005/jp-journals-10071-23395. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CDC, Coronavirus Disease 2019 (COVID-19). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html https://www.cdc.gov/coronavirus/2019-ncov/hcp/framework-non-COVID-care.html Published February 11, 2020. Accessed June 28, 2020.
- 13.Stiller K. Physiotherapy in intensive care. Chest. 2013;144(3):825–847. doi: 10.1378/chest.12-2930. DOI: [DOI] [PubMed] [Google Scholar]
- 14.Sommers J, Engelbert RH, Dettling-Ihnenfeldt D, Gosselink R, Spronk PE, Nollet F, et al. Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin Rehabil. 2015;29(11):1051–1063. doi: 10.1177/0269215514567156. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hodgson CL, Stiller K, Needham DM, Tipping CJ, Harrold M, Baldwin CE, et al. Expert consensus and recommendations on safety criteria for active mobilization of mechanically ventilated critically ill adults. Crit Care. 2014;18(6) doi: 10.1186/s13054-014-0658-y. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lau HM-C, Lee EW-C, Wong CN-C, Ng GY-F, Jones AY-M, Hui DS-C. The impact of severe acute respiratory syndrome on the physical profile and quality of life. Arch Phys Med Rehabil. 2005;86(6):1134–1140. doi: 10.1016/j.apmr.2004.09.025. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dechman G, Hernandez P, Camp PG. Exercise prescription practices in pulmonary rehabilitation programs. Can J Respir Crit Care Sleep Med. 2017;1(2):77–83. doi: 10.1080/24745332.2017.1328935. DOI: [DOI] [Google Scholar]
- 18.Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health. 1990;16(Suppl 1:):55–58. doi: 10.5271/sjweh.1815. DOI: [DOI] [PubMed] [Google Scholar]
- 19.Rawal G, Yadav S, Kumar R. Post-intensive care syndrome: an overview. J Transl Intern Med. 2017;5(2):90–92. doi: 10.1515/jtim-2016-0016. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sessler CN, Gosnell MS, Grap MJ, Brophy GM, O'Neal PV, Keane KA, et al. The richmond agitation-sedation scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med. 2002;166(10):1338–1344. doi: 10.1164/rccm.2107138. DOI: [DOI] [PubMed] [Google Scholar]
- 21.Needham DM, Korupolu R, Zanni JM, Pradhan P, Colantuoni E, Palmer JB, et al. Early physical medicine and rehabilitation for patients with acute respiratory failure: a quality improvement project. Arch Phys Med Rehabil. 2010;91(4):536–542. doi: 10.1016/j.apmr.2010.01.002. DOI: [DOI] [PubMed] [Google Scholar]
- 22.COVID-19: Awake Repositioning/Proning. emDOCs.net - Emergency Medicine Education.; Published May 4, 2020. Accessed July 10, 2020. [Google Scholar]
- 23.Ng Z, Tay WC, Ho CHB. Awake prone positioning for non-intubated oxygen dependent COVID-19 pneumonia patients. Eur Respir J. 2020;56(1):2001198. doi: 10.1183/13993003.01198-2020. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bamford P, Bentley A, Dean J, David Whitmore D, Wilson-Baig N. Guidance for prone positioning of the conscious COVID Patient. https://emcrit.org/wp-content/uploads/2020/04/2020-04-12-Guidance-for-conscious-proning.pdf. Int Care Soc. 2020:1–6. Accessed August 31, 2020. [Google Scholar]
- 25.Sharp JT, Drutz WS, Moisan T, Foster J, Machnach W. Postural relief of dyspnea in severe chronic obstructive pulmonary disease. Am Rev Respir Dis. 1980;122(2):201–211. doi: 10.1164/arrd.1980.122.2.201. DOI: [DOI] [PubMed] [Google Scholar]
- 26.Kim K, Byun M, Lee W, Cynn H, Kwon O, Yi C. Effects of breathing maneuver and sitting posture on muscle activity in inspiratory accessory muscles in patients with chronic obstructive pulmonary disease. Multidiscip Respir Med. 2012;7(1):9. doi: 10.1186/2049-6958-7-9. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ghelichkhani P, Esmaeili M. Prone position in management of COVID-19 patients; a commentary. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7158870/ Arch Acad Emerg Med. 2020;8(1):e48. Accessed June 28, 2020. [PMC free article] [PubMed] [Google Scholar]
- 28.Mesquita Montes A, Tam C, Crasto C, Argel de Melo C, Carvalho P, Santos R, et al. Forward trunk lean with arm support affects the activity of accessory respiratory muscles and thoracoabdominal movement in healthy individuals. Hum Mov Sci. 2018;61:167–176. doi: 10.1016/j.humov.2018.07.011. DOI: [DOI] [PubMed] [Google Scholar]
- 29.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. The Lancet. 2009;373(9678):1874–1882. doi: 10.1016/S0140-6736(09)60658-9. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee AL, Burge AT, Holland AE. Airway clearance techniques for bronchiectasis. Cochrane Database Syst Rev. 2015;2015(11):CD008351. doi: 10.1002/14651858.CD008351.pub3. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bott J, Blumenthal S, Buxton M, Ellum S, Falconer C, Garrod R, et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax. 2009;64(Suppl 1:):i1–i52. doi: 10.1136/thx.2008.110726. DOI: [DOI] [PubMed] [Google Scholar]
- 32.Vitacca M, Carone M, Clini EM, Paneroni M, Lazzeri M, Lanza A, et al. Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration. 2020;(6):1–7. doi: 10.1159/000508399. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kiekens C, Boldrini P, Andreoli A, Avesani R, Gamna F, Grandi M, et al. Rehabilitation and respiratory management in the acute and early post- acute phase. “Instant paper from the field” on rehabilitation answers to the COVID-19 emergency. Eur J Phys Rehabil Med. 2020;56(3):323–326. doi: 10.23736/S1973-9087.20.06305-4. DOI: [DOI] [PubMed] [Google Scholar]
- 34.Mols G, Priebe H-J, Guttmann J. Alveolar recruitment in acute lung injury. Br J Anaesth. 2006;96(2):156–166. doi: 10.1093/bja/aei299. DOI: [DOI] [PubMed] [Google Scholar]
- 35.Sakhaei S, Sadagheyani HE, Zinalpoor S, Markani AK, Motaarefi H. The impact of pursed-lips breathing maneuver on cardiac, respiratory, and oxygenation parameters in COPD patients. Open Access Maced J Med Sci. 2018;6(10):1851–1856. doi: 10.3889/oamjms.2018.407. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kurtaiş Aytür Y. Pulmonary rehabilitation principles in SARS-COV-2 infection (COVID-19): a guideline for the acute and subacute rehabilitation. Turk J Phys Med Rehabil. 2020;66(2):104–120. doi: 10.5606/tftrd.2020.6444. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Overend TJ, Anderson CM, Brooks D, Cicutto L, Keim M, McAuslan D, et al. Updating the evidence base for suctioning adult patients: a systematic review. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2706678/ Can Respir J J Can Thorac Soc. 2009;16(3):e6–e17. doi: 10.1155/2009/872921. DOI: Accessed July 29, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ari A. Practical strategies for a safe and effective delivery of aerosolized medications to patients with COVID-19. Respir Med. 2020;167:105987. doi: 10.1016/j.rmed.2020.105987. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Acquah A. Guidelines for the rehabilitation of patients with COVID-19 in African settings. WCPT Afr Region 2020. http://www.wcptafrica.org/guidelines-for-the-rehabilitation-of-patients-with-covid-19-in-african-settings/ http://www.wcptafrica.org/guidelines-for-the-rehabilitation-of-patients-with-covid-19-in-african-settings/ Accessed June 29, 2020.
- 40.Jacob P, Surendran PJ, E M MA, et al. Early mobilization of patients receiving vasoactive drugs in critical care units: a systematic review. J Acute Care Phys Ther. 2020 doi: 10.1097/JAT.0000000000000140. Publish Ahead of Print. [DOI] [Google Scholar]
- 41.Swaminathan N, Praveen R, Surendran P. The role of physiotherapy in intensive care units: a critical review. 2019;27(15) doi: 10.5114/pq.2019.87739. DOI: [DOI] [Google Scholar]
- 42.Barker-Davies RM, O'Sullivan O, Senaratne KPP, Baker P, Cranley M, Dharm-Datta S, et al. The Stanford Hall consensus statement for post-COVID-19 rehabilitation. Br J Sports Med. 2020;54(16):949–959. doi: 10.1136/bjsports-2020-102596. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chinese association of rehabilitation medicine, respiratory rehabilitation committee of Chinese association of rehabilitation medicine, cardiopulmonary rehabilitation group of Chinese Society of Physical Medicine and Rehabilitation [Recommendations for respiratory rehabilitation of coronavirus disease 2019 in adult]. Zhonghua Jie He He Hu Xi Za Zhi. 2020;43(4):308–314. doi: 10.3760/cma.j.cn112147-20200228-00206. DOI: [DOI] [PubMed] [Google Scholar]
- 44.ResearchGate.; (15) ACPICR Standards for Physical Activity and Exercise in the Cardiovascular Population | Request PDF. Accessed June 29, 2020. [Google Scholar]
- 45.Jackson JC, Pandharipande PP, Girard TD, Brummel NE, Thompson JL, Hughes CG, et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369–379. doi: 10.1016/S2213-2600(14)70051-7. DOI: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tompkins J, Norris T, Levenhagen K, et al. Academy of Acute Care Physical Therapy – APTA Task Force on Lab Values. p. 42.
- 47.Candan SA, Elibol N, Abdullahi A. Consideration of prevention and management of long-term consequences of post-acute respiratory distress syndrome in patients with COVID-19. Physiother Theory Pract. 2020;36(6):663–668. doi: 10.1080/09593985.2020.1766181. DOI: [DOI] [PubMed] [Google Scholar]