Highlights
-
•
Infectious disease outbreaks are associated with mental health symptoms and disorders.
-
•
Pooled prevalence of depression, anxiety, insomnia, PTSD, and psychological distress were 15.97%, 15.15%, 23,87%, 21.94%, and 13.29%, respectively.
-
•
No significant differences were observed for gender, geographical regions, and healthcare workers (except for insomnia, which was more prevalent among healthcare workers).
-
•
This study provides findings that will guide research and the development of better mental health programs during and after the pandemic.
Keywords: COVID-19, Depression, Anxiety, Insomnia, Posttraumatic stress disorder, Psychological distress, Systematic review with meta-analysis
Abstract
Objective
We conducted a systematic review and meta-analysis to estimate the pooled prevalence of depression, anxiety, insomnia, PTSD, and Psychological distress (PD) related to COVID-19 among affected populations.
Methods
We searched articles in Medline, Embase, APA PsycInfo, CINAHL, Scopus, and Web of Science. Random-effects meta-analyses on the proportions of individuals with symptoms of depression, anxiety, insomnia, PTSD, and PD were generated and between-group differences for gender, healthcare workers (HCWs), and regions where studies were conducted.
Results
A total of 2189 articles were screened, 136 full-text articles were assessed for eligibility. Fifty-five peer-reviewed studies met inclusion criteria for the meta-analysis (N=189,159). The prevalence of depression (k=46) was 15.97% (95%CI, 13.24-19.13). The prevalence of anxiety (k=54) was 15.15% (95%CI, 12.29-18.54). The prevalence of insomnia (k=14) was 23.87% (95%CI, 15.74-34.48). The prevalence of PTSD (k=13) was 21.94% (95%CI, 9.37-43.31). Finally, the prevalence of psychological distress (k=19) was 13.29% (95%CI, 8.80-19.57). Between-group differences were only found in HCWs (z=2.69, p < 0.05) who had a higher prevalence of insomnia than others.
Conclusions
Findings suggest that the short-term mental health consequences of COVID-19 are equally high across affected countries, and across gender. However, reports of insomnia are significantly higher among HCWs than the general population.
1. Introduction
On March 11, 2020, the World Health Organization (WHO) officially declared the Coronavirus disease 2019 (COVID-19, also known as SARS-CoV-2) outbreak as a pandemic (World Health Organization, 2020). This pandemic provoked unprecedented public health measures aimed at preventing the spread of the virus: confinement of more than half of the world's population, closure of schools and universities, social and physical distancing, and the declaration of health emergencies in many countries (Jernigan, 2020; Prem et al., 2020; Qiu et al., 2020). On November 14, 2020, more than 53,78 million confirmed cases of COVID-19 were identified worldwide, causing more than 1,3 million deaths (John Hopkins University, 2020).
Previous studies have shown that infectious disease outbreaks are associated with mental health symptoms and disorders (e.g., depression, anxiety, posttraumatic stress disorder, insomnia) in survivors, family members, healthcare workers (HCW), and members of affected communities (Cénat et al., 2020b, 2020d; Keita et al., 2017; Lehmann et al., 2015; Mohammed et al., 2015). A meta-analysis has shown the major consequences of Ebola disease on mental health (Cénat et al., 2020b). Although having a lower fatality case rate than Ebola, this pandemic is associated with considerable deaths worldwide and studies conducted among affected populations have shown major risk factors for the mental health of affected populations (Cénat et al., 2021; Lai et al., 2020; Lee et al., 2020; Lei et al., 2020; Li et al., 2020a, 2020b, 2020d, 2020c; Liu et al., 2020a; Lu et al., 2020; Mazza et al., 2020; Moccia et al., 2020a; Moghanibashi-Mansourieh, 2020; Nguyen et al., 2020). These factors include anxiety and stress associated with the risk of being infected, death of loved ones, infection of loved ones, containment measures, social isolation and loneliness, physical and emotional fatigue of HCW, massive job loss, financial insecurity and poverty, excessive consumption of information from the media, and the vulnerability of certain groups in high-income countries (HICs) and low- and middle-income countries (LMICs) (Ahmed et al., 2020; Al-Rabiaah et al., 2020; Bo et al., 2020; Cai et al., 2020; Cao et al., 2020; Cénat, 2020a; Cénat et al., 2021; Chen et al., 2020; Chew et al., 2020; Du et al., 2020; Gao et al., 2020; Hao et al., 2020a, 2020b; Huang and Zhao, 2020; Lai et al., 2020; Lee et al., 2020; Lei et al., 2020; Moccia et al., 2020a; Moghanibashi-Mansourieh, 2020; Nguyen et al., 2020; Pappa et al., 2020a; Rogers et al., 2020). These studies and others also revealed that all these elements constitute risk factors that can contribute to mental health problems such as anxiety, depression, insomnia, somatization, social phobia, PTSD, OCD, self-harm, and suicidal ideations and behaviors (Cao et al., 2020; Cénat, 2020a; Cénat et al., 2021; Du et al., 2020; Gao et al., 2020; Hao et al., 2020a, 2020b; Huang and Zhao, 2020; Lai et al., 2020; Lee et al., 2020; Lei et al., 2020; Moghanibashi-Mansourieh, 2020; Nguyen et al., 2020; Pappa et al., 2020a; Rogers et al., 2020).
A systematic review and meta-analysis on different coronaviruses (SARS, MERS, and SARS-Cov2) showed that 14 to 61% of infected individuals face serious psychiatric and neuropsychiatric problems (such as depression, impaired memory, insomnia and sleep disorders, anxiety, and PTSD, etc.) during the illness, and 14.8 to 76.9% experience these problems afterwards (Rogers et al., 2020). On May 8, 2020, a meta-analytic review conducted on COVID-19 HCW in Asian countries examined anxiety, depression, and insomnia (Pappa et al., 2020a). Estimates of the pooled prevalence was 23.20% for anxiety, 22.8% for depression, and 34.32% for insomnia. These results can be explained by the stressors and anxieties faced by HCW in their work environment, including the fear of being infected and of infecting their loved ones or colleagues, the rapid deaths of patients, as well as emotional and physical fatigue. It also showed the need for systematic reviews on the general population to develop and implement both prevention and intervention mental health programs based on initial evidence. Another systematic review showed that relatively high rate of anxiety, depression, posttraumatic stress disorder and psychological distress symptoms among population affected by COVID-19 in multiple countries (Xiong et al., 2020).
Conducted in a global mental health perspective, the main objective of this systematic review and meta-analysis is to analyze the impacts of the COVID-19 pandemic on the mental health of affected populations to help develop and implement mental health programs based on initial evidence. Specifically, it aims to (1) analyze the pooled prevalence of depression, anxiety, insomnia, PTSD, and psychological distress (PD) in the general population; (2) examine differences in the pooled prevalence of these problems among HCW compared to the general population; (3) analyze gender-based differences in the pooled prevalence of investigated mental health problems; and (4) as the pandemic has disproportionately affected different parts of the world, this systematic review also aims to analyze differences in mental health problems according to the geographical regions in which the studies were conducted.
2. Methods
This meta-analysis follows methods described in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2019) as well as guidelines presented in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Moher et al., 2009).
2.1. Protocol and registration
We registered this meta-analysis with PROSPERO (CRD42020185613) to avoid unnecessary replication.
2.2. Identification and selection of studies
This meta-analysis focuses on mental health consequences of the COVID-19 pandemic. Scholarly journal articles that reported prevalence for mental health disorders or symptoms were selected. A social sciences research librarian with experience in planning systematic reviews assisted in drafting, developing, and implementing a search strategy to find pertinent published articles in APA PsycInfo (Ovid), Medline (Ovid), Embase (Ovid), CINAHL (Ebsco), Scopus, and Web of Science. The search strategy itself was designed, in part, by examining reviews related to COVID-19 (Lalonde, 2020; Nussbaumer-Streit et al., 2020) and reviews focused on psychological distress (Thekkumpurath et al., 2008; Wade et al., 2016), by consulting COVID-19 search strategies used by other information professionals and compiled by the Medical Library Association (Nussbaumer-Streit et al., 2020), and through discussions with members of the research team. The final search strategy includes pertinent keywords and was executed on May 12, 2020. No limits or restrictions were used in any of the database searches (the complete search strategy is available as supplementary material). Some authors were contacted by email to obtain clarifications or additional information on their article.
2.3. Inclusion and exclusion criteria
Published peer-reviewed journal articles were included if they met the following criteria: (1) were published in either French or English, (2) had empirical data on the prevalence of mental health symptoms or disorders collected during the COVID-19 pandemic. There were no restrictions in terms of age or the type of population studied (e.g., HCW, patients, non-patients).
2.4. Steps for selection
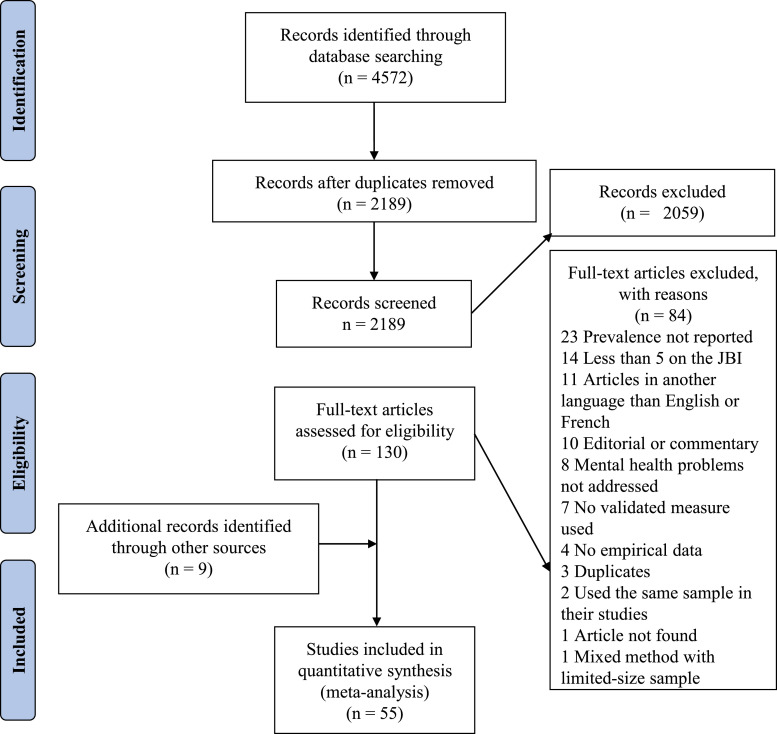
A total of 4572 references were identified across all six databases and were imported into CovidenceTM. Pairs of coders (CKKK, PGN, JNM, RDD, SEM, JMC) were involved in all selection steps (e.g., sorting of articles, data extraction, assessment of quality). Each pair of coders was responsible for half of the articles at each step of the process. Disagreements in screening and coding within a team were resolved by discussion between the two coders. Once duplicates were removed after importing references in CovidenceTM, the titles and abstracts of 2189 references were screened. Of these 2189, 130 full-text references were screened. Following this step, a total of 60 articles were included and 46 articles passed the quality evaluation step. Four additional articles that were published after the initial search were added to the final pool of articles. Five articles were found in the reference list of a previous meta-analysis on COVID-19 (Pappa et al., 2020b). The present meta-analysis is based on a total of 55 articles. From these, 68 independent samples or sub-samples were kept for the meta-analysis. The screening process is recorded in the PRISMA chart (Fig. 1 ).
Fig. 1.
PRISMA chart for the meta-analysis search process.
2.5. Data extraction and management
Sample characteristics of the 68 independent samples included in the meta-analysis are summarized in Table 1 and were the following: author names, month of publication (all articles were submitted or published in 2020, except for the samples that were sent by email to the team), gender, country, type of sample (general population or HCW), assessment tools used for depression, anxiety, insomnia, psychological distress, and PTSD.
Table 1.
Key Characteristics and Quality Evaluation of the Included Studies.
| Authors | Month of publication | Total sample size | Gender | Country | Sample | Depression assessment | Anxiety assessment | Insomnia assessment | PTSD assessment | Psychological distress assessment | Quality evaluation |
| Ahmed et al. | April | 1074 | 46.8% | China | General Population | Beck Depression Inventory (BDI) | Beck Anxiety Inventory (BAI) | 9 | |||
| Al-Rabiaah et al. | January | 174 | 53.2% | China | General Population | General Anxiety Disorder 7-item (GAD-7) | 8 | ||||
| Bo et al. | March | 714 | 50.9% | China | General Population | PTSD Checklist– Civilian Version (PCL-C) | 6 | ||||
| Cai et al. | April | 1521 | 75.5% | China | HCW | Symptom Check-List 90 (SCL-90) | 8 | ||||
| Cao et al. | March | 7143 | 69.65% | China | General Population | General Anxiety Disorder 7-item (GAD-7) | 9 | ||||
| Casagrande et al. | May | 2291 | 74.6% | Italy | General Population | Generalized Anxiety Disorder scale (GAD-7) | Pittsburgh Sleep Quality Index (PSQI) | PTSD Checklist for DSM-5; PCL-5 | Psychological General Well-Being questionnaire (PGWB) | 9 | |
| Chen et al. | March | 105 | 90.5% | China | HCW | Self-Rating Depression Scale (SDS) | Self-Rating Anxiety Scale (SAS) | 7 | |||
| Chew et al. | April | 906 | 64.3% | India & Singapore | HCW | Depression Anxiety Stress Scales (DASS-21) | Depression Anxiety Stress Scales (DASS-21) | Impact of Events Scale-Revised (IES-R) | 9 | ||
| Du et al. (a) | March | 134 | 60.5% | China | HCW | Beck Depression Inventory (BDI) | Beck Anxiety Inventory (BAI) | 7 | |||
| Du et al. (b) | April | 134 | 60.5% | China | HCW | Beck Depression Inventory-II (BDI-II) | Beck Anxiety Inventory (BAI) | 8 | |||
| Gao et al. | April | 4872 | 67.7% | China | General Population | WHO-Five Well-Being Index (WHO-5) | General Anxiety Disorder 7-item (GAD-7) | 9 | |||
| Guo et al. | March | 11118 | 74.8% | China | HCW | Self-Rating Depression Scale (SDS) | Self-Rating Anxiety Scale (SAS) | 9 | |||
| Hao, J. et al. | February | 504 | 52.4% | China | General Population | Kessler 6-Item (K-6) Psychological Distress Scale | 7 | ||||
| Hao, F. et al. | April | 185 | 64.3% | China | HCW | Depression, Anxiety and Stress Scale (DASS-21) | Depression, Anxiety and Stress Scale (DASS-21) | Insomnia Severity Index (ISI) | Impact of Event Scale-Revised (IES-R) | 9 | |
| Huang & Zhao | March | 7236 | 54.6% | China | General Population | Pittsburgh Sleep Quality Index (PSQI) | 9 | ||||
| Kokou-Kpolou et al. | May | 556 | 75.5% | France | General Population | Insomnia Severity Index | 9 | ||||
| Lai et al. | March | 1257 | 76.7% | China | General Population | 9-item Patient Health Questionnaire (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 7-item Insomnia Severity Index | Impact of Event Scale-Revised (IES-R) | 9 | |
| Lee, Jobe, & Mathis | April | 1237 | 45.1% Women, 0.3% Other | United-States | General Population | 9-item Patient Health Questionnaire (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 8 | |||
| Lei et al. | April | 1593 | 61.3% | China | General Population | Self-Rating Depression Scale (SDS) | Self-Rating Depression Scale (SDS) | 9 | |||
| Li, G. et al. | May | 4369 | 100% | China | HCW | 9-item Patient Health Questionnaire (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 9 | |||
| Li, X. et al. | May | 948 | 76.8% | China | HCW | Athens Insomnia Scale (AIS) | 9 | ||||
| Li, Yuchen et al. | May | 1442 | N/A | China | General Population | Kessler 6-Item (K-6) Psychological Distress Scale | 9 | ||||
| Li, Yun et al. | May | 3637 | 63% | China | General Population | 9-item Patient Health Questionnaire (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | Insomnia Severity Index (ISI) | 9 | ||
| Liu, N. et al. | March | 285 | 54.4% | China | General Population | PTSD Checklist for DSM-5 (PCL-5) | 9 | ||||
| Liu, C. et al. | March | 512 | 84.6% | China | HCW | Zung Self-rating Anxiety Scale (SAS) | 9 | ||||
| Liu, Z. et al. | May | 4679 | 82.3% | China | HCW | Zung Self-rating Depression Scale (SDS) | WHO 20-item Self-Reporting Questionnaire (SRQ-20) | 9 | |||
| Lu et al. (A) | April | 2042 | 77.9% | China | HCW | Hamilton Depression Scale | Hamilton Anxiety Scale | 7 | |||
| Lu et al. (B) | April | 257 | 75.5% | China | HCW | Hamilton Depression Scale | Hamilton Anxiety Scale | 7 | |||
| Mazza et al. | May | 2766 | 71.6% | Italy | General Population | Depression, Anxiety and Stress Scale-21 (DASS-21) | Depression, Anxiety and Stress Scale-21 | 8 | |||
| Moccia et al. | April | 500 | 59.6% | Italy | General Population | Kessler 10-item Psychological Distress Scale (K-10) | 7 | ||||
| Moghanibashi-Mansourieh | April | 10754 | 65.8% | Iran | General Population | Depression, Anxiety and Stress Scale-21 | 8 | ||||
| Nguyen et al. | March | 3947 | 55.7% | Vietnam | General Population | Patient Health Questionnaire 9-item (PHQ-9) | 9 | ||||
| Ni et al. (A) | May | 214 | 68.8% | China | HCW | Patient Health Questionnaire 2-item (PHQ-2) | General Anxiety Disorder 2-item (GAD-2) | 8 | |||
| Ni et al. (B) | May | 1577 | 60.8% | China | General Population | Patient Health Questionnaire 2-item (PHQ-2) | General Anxiety Disorder 2-item (GAD-2) | 8 | |||
| Ozamiz-Etxebarria | April | 976 | 81.1% | Spain | General Population | Depression, Anxiety and Stress Scale-21 (DASS-21) | 8 | ||||
| Ozdin et al. | May | 343 | 49.2% | Turkey | General Population | Hospital Anxiety and Depression Scale (HADS) | Hospital Anxiety and Depression Scale (HADS) | 8 | |||
| Qi et al. | March | 1306 | 80.4% | China | HCW | Athens Insomnia Scale (AIS) | 9 | ||||
| Qiu et al. | March | 52730 | 64.73% | China | General Population | COVID-19 Pertitraumatic Distress Index (CPDI) | 7 | ||||
| Rossi et al. | May | 18147 | 79.6% | Italy | General Population | 9-item Patient Health Questionnaire (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 7-item Insomnia Severity Index (ISI) | Global Psychotrauma Screen, post-traumatic stress symptoms subscale (GPS-PTSS) | 9 | |
| Shacham et al. | April | 338 | 58.6% | Israel | HCW | Kessler 6-item Psychological Distress Scale (K-6) | 6 | ||||
| Tan et al. (a) | April | 470 | 68.3% | Singapore | HCW | Depression, Anxiety and Stress Scale-21 (DASS-21) | Depression, Anxiety and Stress Scale-21 (DASS-21) | Impact of Events Scale-Revised (IES-R) | 8 | ||
| Tan et al. (b) | April | 673 | 25.6% | China | General Population | Depression, Anxiety and Stress Scale-21 (DASS-21) | Depression, Anxiety and Stress Scale-21 (DASS-21) | Insomnia Severity Index (ISI) | Impact of Events Scale-Revised (IES-R) | 8 | |
| Tang et al. | May | 2485 | 61.4% | China | General Population | Patient Health Questionnaire 9-item (PHQ-9) | PTSD Checklist Civilian (PCL-C) | 8 | |||
| Wang, Y. et al. | March | 600 | 55.5% | China | General Population | Self-rating anxiety scale (SAS) | 9 | ||||
| Wang, C. et al. (a) | April | 1304 | 67.3% | China | General Population | Depression, Anxiety and Stress Scale (DASS-21) | Depression, Anxiety and Stress Scale (DASS-21) | 8 | |||
| Wang, C. et al. (b) | March | 1210 | 67.3% | China | General Population | Depression, Anxiety and Stress Scale-21 (DASS-21) | Depression, Anxiety and Stress Scale-21 (DASS-21) | Impact of Events Scale-Revised (IES-R) | 7 | ||
| Wang, S. et al. | May | 123 | 90% | China | HCW | Self-rating anxiety scale (SAS) | Pittsburgh sleep quality index (PSQI) | 9 | |||
| Xie et al. | April | 1784 | 43.3% | China | General Population | Screen for Child Anxiety Related Emotional Disorders | 9 | ||||
| Zhang, S. (Bolivia) | Unpublished sample sent by author | 240 | Bolivia | HCW | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | |||||
| Zhang, S. (Ecuador) | Unpublished sample sent by author | 252 | Ecuador | HCW | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | |||||
| Zhang, S. (Iran) | Unpublished sample sent by author | 521 | Iran | General Population | Patient Health Questionnaire 9-item (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | ||||
| Zhang, S. (Iran2) | Unpublished sample sent by author | 304 | Iran | HCW | Patient Health Questionnaire 9-item (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | ||||
| Zhang, S. (Iran3) | Unpublished sample sent by author | 139 | Iran | General Population | Patient Health Questionnaire 9-item (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | ||||
| Zhang, S.(Malaysia) | Unpublished sample sent by author | 655 | Malaysia | General Population | General Anxiety Disorder 7-item (GAD-7) | Unpublished sample sent by author | |||||
| Zhang, S. (middle) | Unpublished sample sent by author | 474 | Multi-countries | General Population | Patient Health Questionnaire 9-item (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 0 | Unpublished sample sent by author | |||
| Zhang, S. (Pakistan) | Unpublished sample sent by author | 629 | Pakistan | HCW | General Anxiety Disorder 7-item (GAD-7) | 0 | Unpublished sample sent by author | ||||
| Zhang, S. (Peru) | Unpublished sample sent by author | 220 | Peru | HCW | General Anxiety Disorder 7-item (GAD-7) | 0 | Unpublished sample sent by author | ||||
| Zhang, S. (senior) | Unpublished sample sent by author | 182 | Multi-countries | General Population | Patient Health Questionnaire 9-item (PHQ-9) | General Anxiety Disorder 7-item (GAD-7) | 0 | Unpublished sample sent by author | |||
| Zhang, S. et al. (a) | May | 304 | 58.6% | Iran | HCW | Patient Health Questionnaire 4-item (PHQ-4) | Patient Health Questionnaire 4-item (PHQ-4) | Kessler 6-item Psychological Distress Scale (K-6) | 6 | ||
| Zhang, Y. et al. | March | 263 | 59.7% | China | General Population | Impact of Events Scale-Revised (IES-R) | 7 | ||||
| Zhang, W.-R. et al. | April | 2182 | 64.2% | China | HCW | Patient Health Questionnaire 4-item (PHQ-4) | Insomnia Severity Index (ISI) | 8 | |||
| Zhang, C. et al. | April | 1563 | 82.73% | China | HCW | General Anxiety Disorder 2-item (GAD-2) | Insomnia Severity Index (ISI) | Impact of Events Scale-Revised (IES-R) | 9 | ||
| Zhang, J. et al. | April | 205 | 56.1% | China | General Population | Patient Health Questionnaire 9-item (PHQ-9) | Generalized Anxiety Disorder scale (GAD-7) | 6 | |||
| Zhang, S. et al. (b) | May | 369 | 45% | China | General Population | Kessler 6-item Psychological Distress Scale (K-6) | 7 | ||||
| Zhou, J. et al. | April | 2065 | N/A | China | General Population | Generalized Anxiety Disorder scale (GAD-7) | Insomnia Severity Index (ISI) | 6 | |||
| Zhou, S.-J. et al. | April | 8079 | 53.5% | China | General Population | Generalized Anxiety Disorder scale (GAD-7) | 9 | ||||
| Zhu, S. et al. | April | 2279 | 59.7% | China | General Population | Generalized Anxiety Disorder scale (GAD-7) | 9 | ||||
| Zhu, Z. et al. | February | 5062 | 85% | China | HCW | Patient Health Questionnaire-9 (PHQ-9) | Generalized Anxiety Disorder Scale (GAD-7) | 6 | |||
Note. All articles were published or submitted in 2020, except for the unpublished data.
2.6. Quality assessment
We used the Joanna Briggs Institute (JBI) checklist for prevalence studies (Martin, 2017) to evaluate the quality of the 68 retained independent samples. The evaluation criteria were: (1) appropriateness of the sample frame; (2) recruitment procedure; (3) adequacy of the sample size; (4) description of subjects and setting; (5) coverage of the identified sample; (6) validity of the methods used to identify the mental health symptoms or disorders; (7) reliability of the methods used to identify mental health symptoms or disorders; (8) adequacy of statistical analyses; and (9) response rate. Articles were assigned one point per criterion met, for a maximum of 9 points. Articles were excluded if their total score was less than 5 points (no included articles received a rating lower than 5). There were 55 articles remaining after this step and 14 articles were removed because they had less than 5 out of 9 on the JBI checklist.
2.7. Meta-analysis
Random effects meta-analyses were generated based on the proportions of individuals with symptoms or disorders (depression, anxiety, insomnia, psychological distress, and PTSD) among samples of people affected by the COVID-19 pandemic using the “9etaphor” package in R Version 4 (Viechtbauer, 2010). Random effects account for the heterogeneity among the studies. Logit transformed proportions were used and transformed back for ease of interpretation into a forest plot. The binomial-normal model was indicated as it gives unbiased estimates and a good coverage of confidence intervals for meta-analyses with proportions (Hamza et al., 2008; Stijnen et al., 2010).
3. Results
The prevalence of mental health symptoms/disorders (depression, anxiety, insomnia, PTSD, psychological distress) were analyzed in 68 independent samples (N=189,159). Most studies were conducted in China (k= 45) and on the general population (k=41), the rest of the studies were on other countries and on HCW, respectively. The data allowed for comparisons between the general population and HCW for all the mental health symptoms and for comparisons between male and female genders and geographical regions (China and other countries) for depression and anxiety.
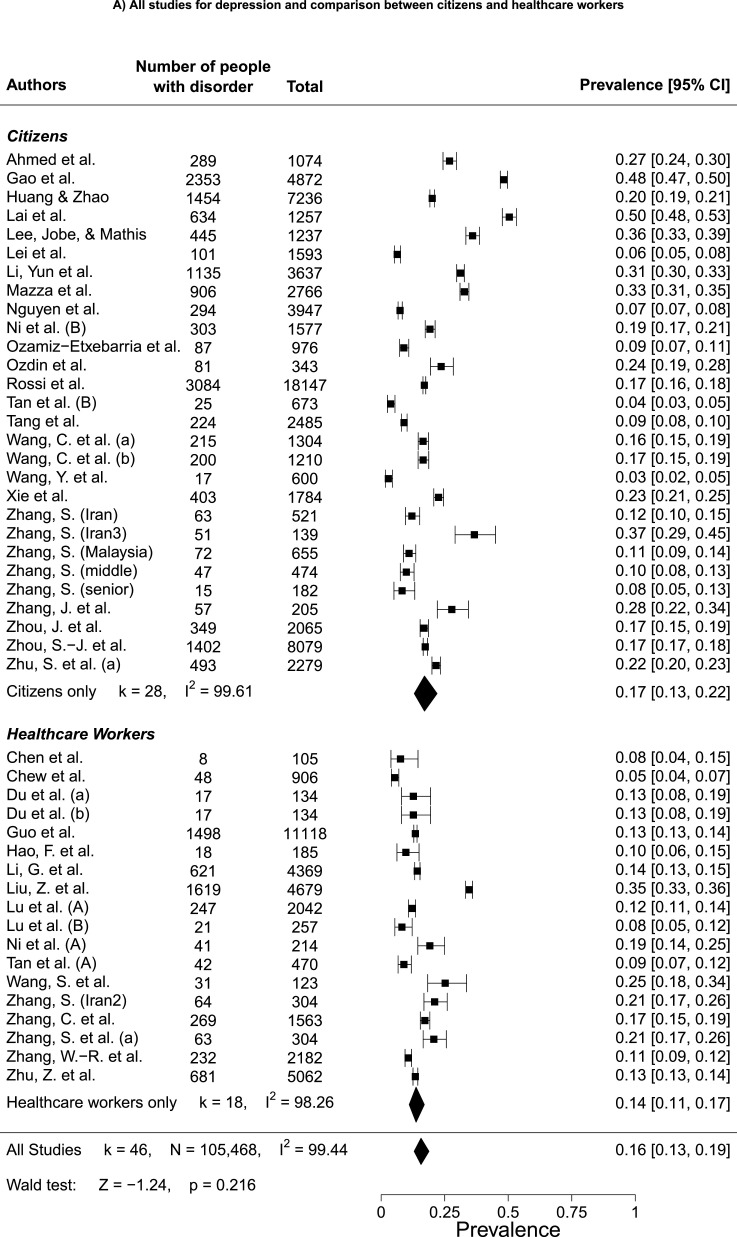
3.1. Depression
Fig. 2 A shows a forest plot of the pooled prevalence of depression in people during the COVID-19 pandemic (k=46, N=105,468). The pooled prevalence of depression among participants is 15.97% CI 95% [13.24%;19.13%]. The Kendall's tau rank order correlation is not significant (r τ= -.01, p>0.05), indicating an absence of asymmetry in the funnel plot. This result provides evidence that there is no publication bias in the present meta-analysis. There is heterogeneity in the results (I2 = 99.44) (Higgins et al., 2003). Fig. 2A shows that there are no differences in the prevalence of depression between citizens (k=28, 17.05, 95% CI [13.03;22.01]) and HCW (k=18,13.75, 95% CI [11.04;16.96]), (z = -1.24, p > 0.05). Fig. 2B shows that there is no difference in the prevalence of depression in studies conducted in China (k=34, 16.23, 95% CI [13.02;20.04]) compared to studies conducted in other countries (k=12, 16.92, 95% CI [11.78;23.70]), (z = .20, p > 0.05). Fig. 2C indicates that there are no differences in the prevalence of depression between males (k=9,19.05, 95% CI [11.17;30.57]) and females (k=9, 22.93, 95% CI [15.16;33.14]), (z = -0.57, p > 0.05).
Fig. 2.
Forest plot of pooled depression prevalence and comparisons between citizens and healthcare workers, geographical regions, and gender.
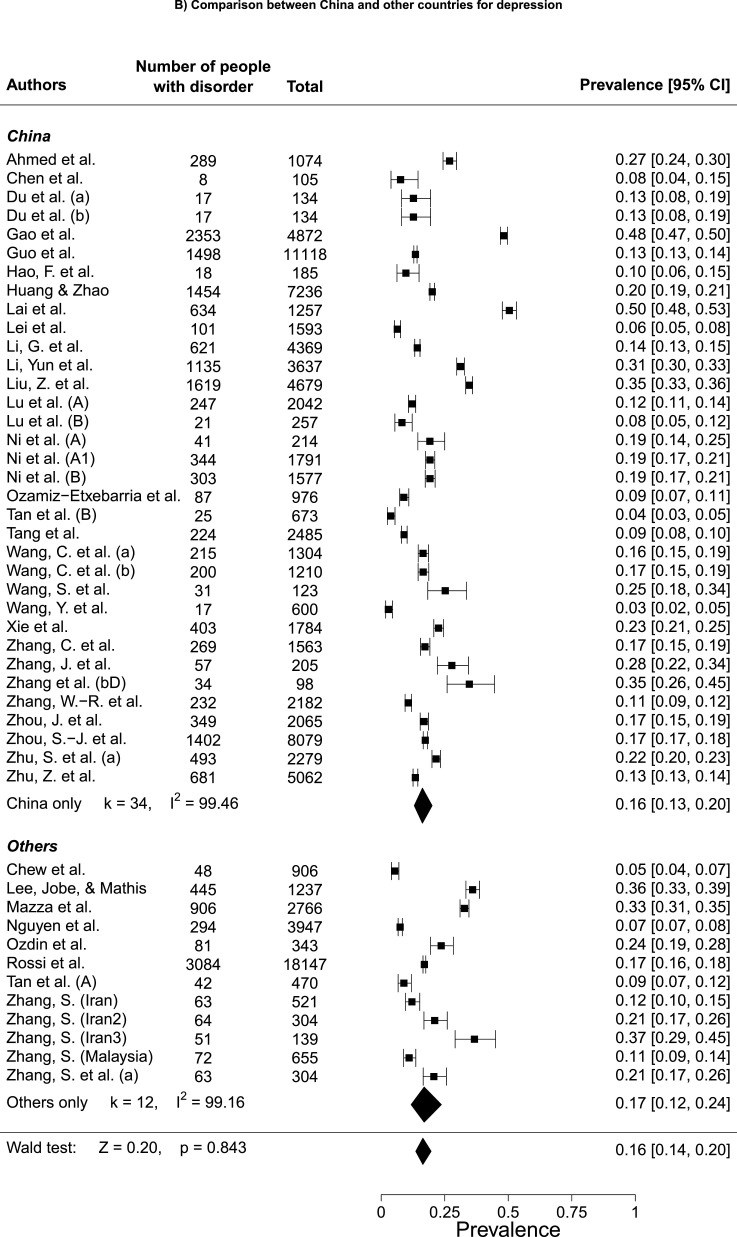
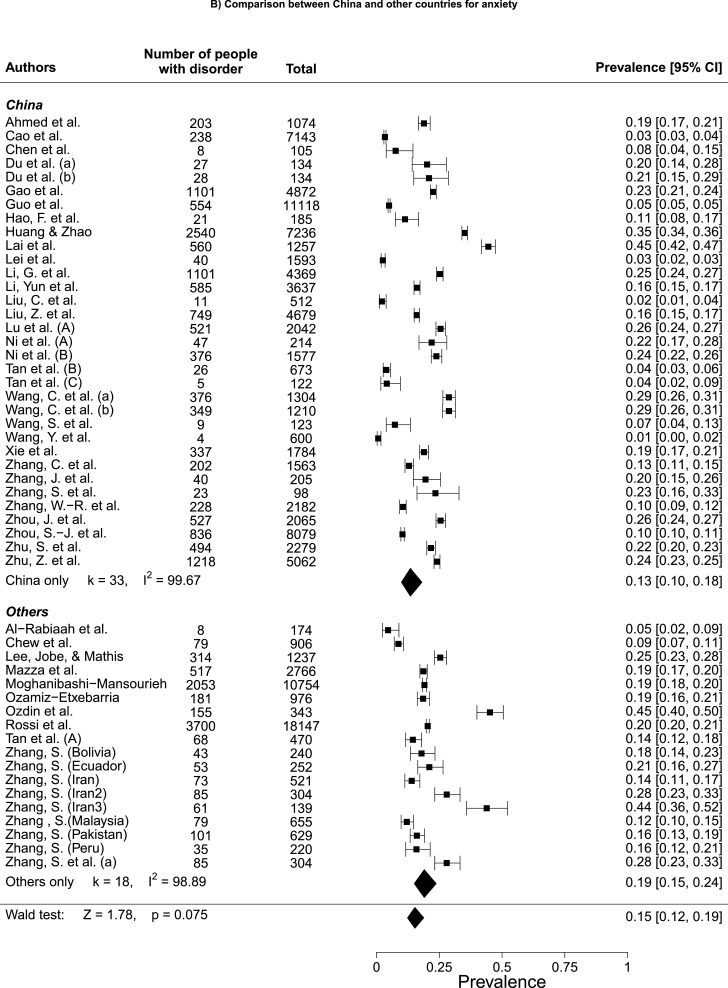
3.2. Anxiety
Fig. 3 A shows a forest plot of the pooled prevalence of anxiety in people during the COVID-19 pandemic (k=54, N= 121,373). The pooled prevalence of anxiety among participants is 15.15% CI 95% [12.29%;18.54%]. The Kendall's tau rank order correlation is not significant (r τ= -.20, p<0.05), indicating the presence of asymmetry in the funnel plot. This result provides evidence of publication bias in the present meta-analysis. There is heterogeneity in the results (I2 = 99.58) (Higgins et al., 2003). Fig. 3A indicates that there are no differences in the prevalence of anxiety between citizens (k=31, 14.62, 95% CI [10.69;19.69]) and HCW (k=23, 15.86, 95% CI [12.22;20.33]), (z = 0.40, p > 0.05). Fig. 3B shows that there is no difference in the prevalence of anxiety in studies conducted in China (k=33, 13.49, 95% CI [9.90;18.11]) compared to studies conducted in other countries (k=18, 19.02, 95% CI [15.01;23.80]), (z = 1.78, p > 0.05). However, we might lack statistical power to detect a difference between the two groups. Fig. 3C shows that there are no differences in the prevalence of anxiety between males (k=6, 14.19, 95% CI [7.14;26.23]) and females (k=6, 17.87, 95% CI [9.64;30.73]), (z = -0.51, p > 0.05).
Fig. 3.
Forest plot of pooled depression prevalence and comparisons between citizens and healthcare workers, geographical regions, and gender.
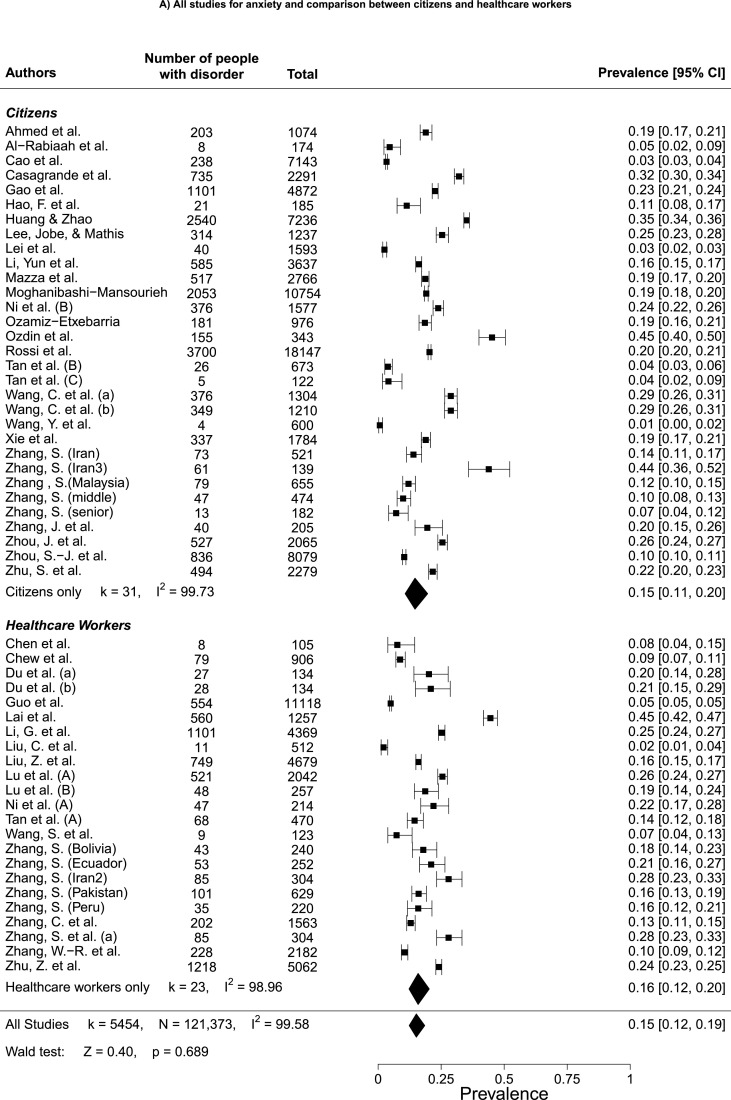
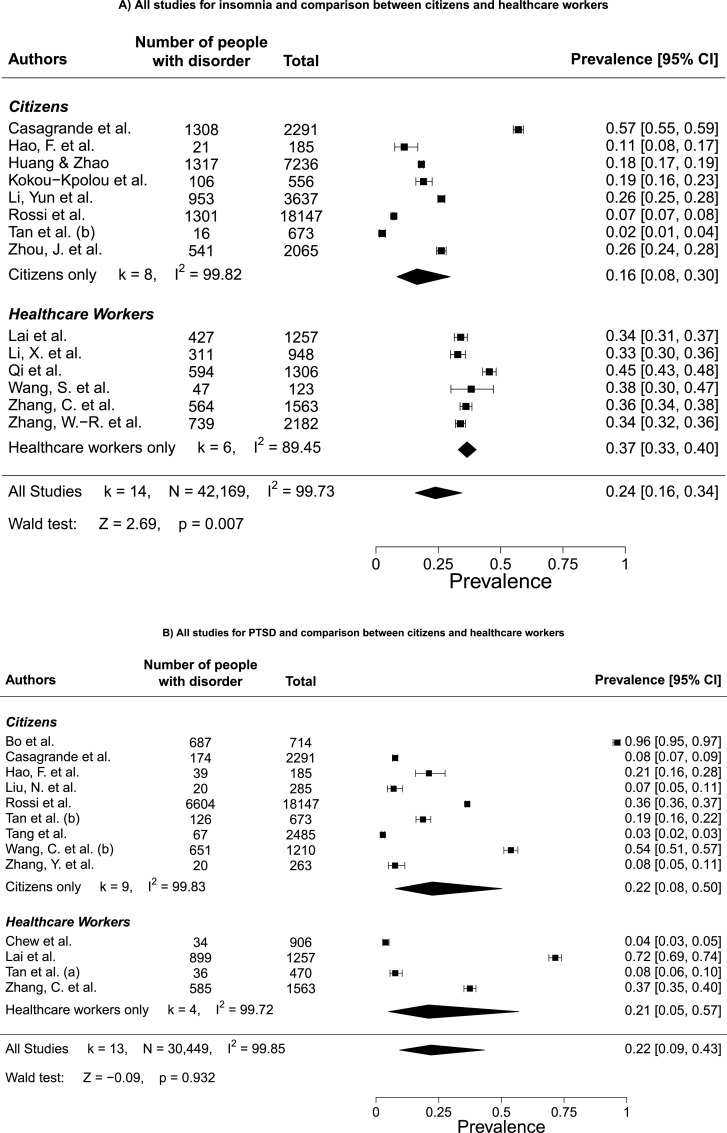
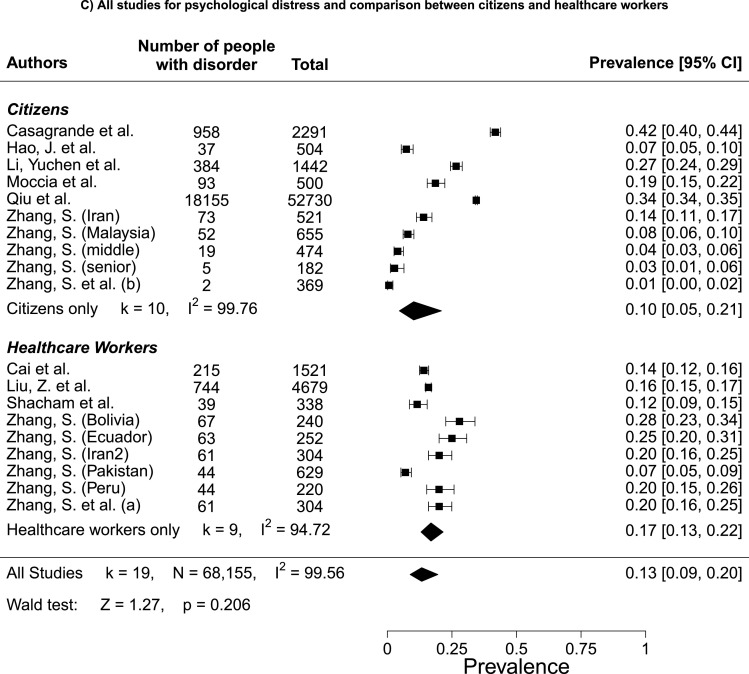
3.3. Insomnia
Fig. 4 A shows a forest plot of the pooled prevalence of insomnia in people during the COVID-19 pandemic (k=14, N= 42,169). The pooled prevalence of insomnia among participants is 23.87% CI 95% [15.74%;34.48%]. The Kendall's tau rank order correlation is not significant (r τ= -.12, p>0.05), which indicates that there is no asymmetry in the funnel plot. This result provides evidence that there is no publication bias in the present meta-analysis. There is heterogeneity in the results (I2 = 99.73) (Higgins et al., 2003). Fig. 4A indicates a difference in the prevalence of insomnia between citizens (k=8, 16.45, 95% CI [8.39;29.74]) and HCW (k=6, 36.52, 95% CI [32.99;40.20]), (z = 2.69, p < 0.05). HCW have a higher prevalence of insomnia than citizens.
Fig. 4.
Forest plot of pooled prevalence of insomnia, PTSD, and psychological distress and distress, and comparisons between citizens and healthcare workers.
3.4. Posttraumatic stress disorder (PTSD)
Fig. 4B shows a forest plot of the pooled prevalence of PTSD in people during the COVID-19 pandemic (k=13, N=30,449). The pooled prevalence of PTSD among participants is 21.94% CI 95% [9.37%;43.31%]. The Kendall's tau rank order correlation is not significant (r τ= -.08, p>0.05), which indicates that there is no asymmetry in the funnel plot. This result provides evidence that there is no publication bias in the present meta-analysis. There is heterogeneity in the results (I2 = 99.85) (Higgins et al., 2003). Fig. 4B shows no difference in the prevalence of PTSD between citizens (k=9, 22.43, 95% CI [7.62;50.32]) and HCW (k=4, 20.91, 95% CI [5.01;57.00]), (z = -.09, p > 0.05).
3.5. Psychological distress
Fig. 4C shows a forest plot of the pooled prevalence of psychological distress in people during the COVID-19 pandemic (k=19, N=68,155). The pooled prevalence of psychological distress among participants is 13.29% CI 95% [8.80%;19.57%]. The Kendall's tau rank order correlation is not significant (r τ= -.08, p>0.05), indicating an absence of asymmetry in the funnel plot. This result provides evidence that there is no publication bias in the present meta-analysis. There is heterogeneity in the results (I2 = 99.60) (Higgins et al., 2003). Fig. 4C indicates no difference in the prevalence of psychological distress between citizens (k=10, 10.19, 95% CI [4.63;20.96]) and HCW (k=9, 16.88, 95% CI [13.02;21.61]), (z = 1.27, p > 0.05).
4. Discussion
Conducted with a global mental health perspective, the objective of this systematic review and meta-analysis was to analyze the impacts of COVID-19 on the mental health of affected populations to help implement programs based on initial evidence. The results showed that the most studied mental health problems during COVID-19 are depression, anxiety, insomnia, PTSD, and PD. We conducted meta-analyses on the prevalence of these five mental health problems. This meta-analysis includes 68 independent samples and sub-samples that indicate that pandemic-affected populations have significantly higher prevalence of depression, anxiety, insomnia, PTSD, and PD compared to the general population under normal circumstances. First, compared to what was observed in the latest WHO study on common mental health disorders, prevalence of depression in populations affected by COVID-19 is more than three times higher (15.97%) than in the general population (4.4%); while it is four times higher for anxiety (15.15% vs. 3.6%); and five times higher for PTSD (21.94% vs. 4%) (Kessler et al., 2017; Liu et al., 2017; World Health Organization, 2017). These prevalence rates are also higher than those usually observed in the general population (Atwoli et al., 2015; Dorrington et al., 2014; Grove et al., 2011; Guo et al., 2016; Kessler et al., 2017; Liu et al., 2017; Slade et al., 2011; Stein et al., 2017; Vilagut et al., 2016; Weinberger et al., 2018; World Health Organization, 2017). Results also showed significantly higher prevalence of insomnia and PD in populations affected by COVID-19 compared to the general population (Cao et al., 2017; Ford et al., 2015; Jiang et al., 2015; Mojtabai and Jorm, 2015; Nishi et al., 2018; Slade et al., 2011). These high prevalence rates can be explained by the fear associated with the pandemic, containment measures, high numbers of people infected, and deaths (Moghanibashi-Mansourieh, 2020; Ohayon, 2002; Rogers et al., 2020). Additionally, the pandemic is associated with a lack of control among infected people, job losses, wage losses, and uncertainty about the future (Nicola et al., 2020).
The second objective of this study was to compare mental health problems between HCW and other populations affected by COVID-19. Results showed that there were no significant differences in depression, anxiety, PTSD, and PD. These results are consistent with previous studies that have shown that during epidemics and crises (e.g., SARS, Ebola), HCW generally have the same level or fewer mental health problems than community members (Cénat et al., 2020b, 2020d, 2020c; Lancee et al., 2008; Lehmann et al., 2015; Pappa et al., 2020b). However, longitudinal studies need to be conducted to determine whether this non-differentiation between HCW and the general population is related to temporary coping strategies associated with being on the front lines. After the pandemic ends, HCW may develop more severe mental health problems. For example, the prevalence of insomnia that is more than two times higher among HCW is a predictor of depression and suicidal ideation (Cukrowicz et al., 2006).
The third objective of this study was to test for gender differences in the prevalence of mental health problems. The data allowed comparisons for depression and anxiety. While a higher prevalence of anxiety and depression was expected in females, surprisingly, there were no gender differences. Available data have not always allowed for the evaluation of gender differences during past epidemics (Cénat et al., 2020d). Studies conducted during this pandemic have shown that males and females experience stressors in similar ways (Cao et al., 2020). Studies conducted in China, both with very large and small samples, have also found no gender differences (Cao et al., 2020; Chen et al., 2020; Huang and Zhao, 2020). However, studies in the Middle East and the West have shown that women are at greater risk of developing mental health problems during COVID-19 (Mazza et al., 2020; Moccia et al., 2020b; Moghanibashi-Mansourieh, 2020). These observations should be investigated longitudinally because confirmation of this pattern could lead to questions about the association between cultural gender roles and the development of mental health problems.
As the pandemic has disproportionately affected different parts of the world, the final objective of this study was to analyze differences in mental health problems according to the regions in which the studies were conducted. We wanted to compare studies from Asia, Europe, and North America. Since most of the studies were from China, we were only able to analyze differences between China and other countries as a whole, and only for depression and anxiety. The global nature of this pandemic offers the possibility of analyzing the phenomenology of psychopathology between countries.
5. Limitations
While this study provides findings that will guide research and the development of better mental health programs during and after the pandemic, it has some limitations. The first is that the pandemic is still ongoing. Articles are written quickly and do not always document essential aspects that would allow us to analyze differences between groups. In addition, new publications are published daily, but this study was necessary to allow mental health programs to be developed based on early evidence. The second limitation of this study is that most of the published research comes from China. This is because China is the first country to have faced the pandemic. Also, although we only retained studies with high cut-off scores and valid measures, a large heterogeneity was found in the results. A recent meta-analysis on mental health problems in populations affected by Ebola disease and others on HCW during the COVID-19 pandemic had a similar finding (Cénat et al., 2020b; Pappa et al., 2020b; Xiong et al., 2020). The disproportionate spread of COVID-19, associated consequences, and differences between scales used to measure mental health problems are all factors that may explain this heterogeneity. Moreover, very few studies have been conducted among survivors of COVID-19, especially those who developed severe symptoms. These studies could have allowed for an analysis of probable differences within groups affected by COVID-19. Finally, the lack of studies in low- and middle-income countries prevents a more global perspective in this study.
6. Future directions
The greatest strength of this study is that it identifies a range of avenues for future research. First, this article shows the need for longitudinal studies to better understand the impacts of COVID-19 on survivors, gender, geographical regions, etc. Second, these studies should also analyze socio-demographic characteristics to highlight the differences that may exist between groups, and identify those most at risk to facilitate the development of programs based on their specific needs. Also, studies should explore mental health problems specifically among HCW on a longitudinal basis, while comparing with the rest of the population. This will allow us to observe whether being in the heat of the moment acts as a protective factor in the short term as in the long term, HCW present more health problems than the rest of the population. Future studies should also pay special attention to survivors, especially those who have developed severe symptoms or who have been on artificial ventilators. Finally, studies should also analyze whether differences exist depending on the measures used to assess mental health problems. This will help identify the best tools to accurately measure mental health problems.
7. Conclusions
This study shows that regardless of gender, group or region, the current pandemic is impacting the mental health of affected populations. Indeed, all groups have a high prevalence of depression, anxiety, insomnia, PTSD, and PD. Thus, this study provides initial evidence for the implementation of mental health prevention and intervention programs that provide holistic care to affected individuals. Special attention must be paid to infected individuals and those who have developed severe symptoms to make healthcare as minimally traumatic as possible for them and their families, while respecting measures to prevent the spread of the virus. Also, programs must be developed quickly for HCW to address the mental health problems associated with the pandemic and to prevent them in the long term.
Finally, research is necessary to identify and document all aspects of the pandemic that impact mental health including social inequalities, the vulnerability of children and adolescents, the resilience of LMICs, confinement, traumatic characteristics of COVID-19-related deaths (Bhopal, 2020; Cénat, 2020a, Cénat, 2020b; Cénat et al., 2020a; Cénat and Dalexis, 2020; Dalexis and Cénat, 2020; Holmes et al., 2020; Kokou-Kpolou et al., 2020; Li et al., 2020e; Xiong et al., 2020). Research must help build more resilient populations and healthcare systems in the face of epidemics by providing sufficient evidence to develop both surveillance, prevention and intervention programs during and after this worldwide crisis (Cénat, 2020c; Collin-Vézina et al., 2020; Holmes et al., 2020; Liu et al., 2020b).
Funding
None
Declaration of Competing Interest
No conflict of interest for any author.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2020.113599.
Appendix. Supplementary materials
References
- Ahmed M.Z., Ahmed O., Aibao Z., Hanbin S., Siyu L., Ahmad A. Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Rabiaah A., Temsah M.H., Al-Eyadhy A.A., Hasan G.M., Al-Zamil F., Al-Subaie S., Alsohime F., Jamal A., Alhaboob A., Al-Saadi B., Somily A.M. Middle East respiratory syndrome-corona virus (MERS-CoV) associated stress among medical students at a university teaching hospital in Saudi Arabia. J. Infect. Public Health. 2020;13:687–691. doi: 10.1016/j.jiph.2020.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atwoli L., Stein D.J., Koenen K.C., McLaughlin K.A. Epidemiology of posttraumatic stress disorder: prevalence, correlates and consequences. Curr. Opin. Psychiatry. 2015 doi: 10.1097/YCO.0000000000000167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhopal R.S. COVID-19: Immense necessity and challenges in meeting the needs of minorities, especially asylum seekers and undocumented migrants. Public Health. 2020 doi: 10.1016/j.puhe.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bo H.X., Li W., Yang Y., Wang Y., Zhang Q., Cheung T., Wu X., Xiang Y.T. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol. Med. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai W., Lian B., Song X., Hou T., Deng G., Li H. A cross-sectional study on mental health among health care workers during the outbreak of corona virus disease 2019. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., Zheng, J., 2020. The psychological impact of the COVID-19 epidemic on college students in China. DOI: 10.1016/j.psychres.2020.112934. [DOI] [PMC free article] [PubMed]
- Cao X.-L., Wang S.-B., Zhong B.-L., Zhang L., Ungvari G.S., Ng C.H., Li L., K Chiu H.F., I Lok G.K., Lu J.-P., Jia F.-J., Xiang Y.-T. The prevalence of insomnia in the general population in China: a meta-analysis. PLoS ONE. 2017;12 doi: 10.1371/journal.pone.0170772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M. The vulnerability of low-and middle-income countries facing the COVID-19 pandemic: the case of Haiti. Travel Med. Infect. Dis. 2020 doi: 10.1016/j.tmaid.2020.101684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M. US deportation policies in the time of COVID-19: a public health threat to the Americas. Public Health. 2020 doi: 10.1016/j.puhe.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M. How to provide anti-racist mental health care. Lancet Psychiatry. 2020;7:929–931. doi: 10.1016/S2215-0366(20)30309-6. [DOI] [PubMed] [Google Scholar]
- Cénat J.M., Dalexis R.D. The complex trauma spectrum during the COVID-19 pandemic: a threat for children and adolescents’ physical and mental health. Psychiatry Res. 2020:293. doi: 10.1016/j.psychres.2020.113473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Dalexis R.D., Guerrier M., Noorishad P.-G., Derivois D., Bukaka J., Birangui J.-P., Adansikou K., Clorméus L.A., Kokou-Kpolou C.K., Ndengeyingoma A., Sezibera V., Auguste R.E., Rousseau C. Frequency and correlates of anxiety symptoms during the COVID-19 pandemic in low- and middle-income countries: a multinational study. J. Psychiatr. Res. 2021:132. doi: 10.1016/j.jpsychires.2020.09.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Dalexis R.D., Kokou-Kpolou C.K., Mukunzi J.N., Rousseau C. Social inequalities and collateral damages of the COVID-19 pandemic: when basic needs challenge mental health care. Int. J. Public Health. 2020 doi: 10.1007/s00038-020-01426-y. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cénat J.M., Felix N., Blais-Rochette C., Rousseau C., Bukaka J., Derivois D., Noorishad P.-G., Birangui J.-P. Prevalence of mental health problems in populations affected by Ebola virus disease: a systematic review and meta-analysis. Psychiatry Res. 2020;289 doi: 10.1016/j.psychres.2020.113033. [DOI] [PubMed] [Google Scholar]
- Cénat J.M., McIntee S.E., Blais-Rochette C. Symptoms of posttraumatic stress disorder, depression, anxiety and other mental health problems following the 2010 earthquake in Haiti: a systematic review and meta-analysis. J. Affect. Disord. 2020;273:55–85. doi: 10.1016/j.jad.2020.04.046. [DOI] [PubMed] [Google Scholar]
- Cénat J.M., Mukunzi J.N., Noorishad P.-G., Rousseau C., Derivois D., Bukaka J. A systematic review of mental health programs among populations affected by the Ebola virus disease. J. Psychosom. Res. 2020;131 doi: 10.1016/j.jpsychores.2020.109966. [DOI] [PubMed] [Google Scholar]
- Chen Y., Zhou H., Zhou Y., Zhou F. Prevalence of self-reported depression and anxiety among pediatric medical staff members during the COVID-19 outbreak in Guiyang, China. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew N.W.S., Lee G.K.H., Tan B.Y.Q., Jing M., Goh Y., Ngiam N.J.H., Yeo L.L.L., Ahmad A., Ahmed Khan F., Napolean Shanmugam G., Sharma A.K., Komalkumar R.N., Meenakshi P.V., Shah K., Patel B., Chan B.P.L., Sunny S., Chandra B., Ong J.J.Y., Paliwal P.R., Wong L.Y.H., Sagayanathan R., Chen J.T., Ying Ng A.Y., Teoh H.L., Tsivgoulis G., Ho C.S., Ho R.C., Sharma V.K. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin-Vézina D., Brend D., Beeman I. When it counts the most: trauma-informed care and the COVID-19 global pandemic. Dev. Child Welf. 2020 doi: 10.1177/2516103220942530. 251610322094253. [DOI] [Google Scholar]
- Cukrowicz K.C., Otamendi A., Pinto J.Y., Bernert R.A., Krakow B., Joiner T.E. The impact of insomnia and sleep disturbances on depression and suicidality. Dreaming. 2006;16:1–10. doi: 10.1037/1053-0797.16.1.1. [DOI] [Google Scholar]
- Dalexis R.D., Cénat J.M. Asylum seekers working in Quebec (Canada) during the COVID-19 pandemic: risk of deportation, and threats to physical and mental health. Psychiatry Res. 2020 doi: 10.1016/j.psychres.2020.113299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorrington S., Zavos H., Ball H., McGuffin P., Rijsdijk F., Siribaddana S., Sumathipala A., Hotopf M. Trauma, post-traumatic stress disorder and psychiatric disorders in a middle-income setting: prevalence and comorbidity. Br. J. Psychiatry. 2014;205:383–389. doi: 10.1192/bjp.bp.113.141796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Du J., Dong L., Wang T., Yuan C., Fu R., Zhang L., Liu B., Zhang M., Yin Y., Qin J., Bouey J., Zhao M., Li X. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry. 2020 doi: 10.1016/j.genhosppsych.2020.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford E.S., Cunningham T.J., Giles W.H., Croft J.B. Trends in insomnia and excessive daytime sleepiness among US adults from 2002 to 2012. Sleep Med. 2015;16:372–378. doi: 10.1016/j.sleep.2014.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao J., Zheng P., Jia Y., Chen H., Mao Y., Chen S., Wang Y., Fu H., Dai J. Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE. 2020;15 doi: 10.1371/journal.pone.0231924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grove R., Associate R., Slade T., Mcevoy P.M. Epidemiology of anxiety disorders in the Australian general population: findings of the 2007 Australian National Survey of Mental Health and Wellbeing. Aust. N. Z. J. Psychiatry. 2011;45:957–967. doi: 10.3109/00048674.2011.624083. [DOI] [PubMed] [Google Scholar]
- Guo X., Meng Z., Huang G., Fan J., Zhou W., Ling W., Jiang J., Long J., Su L. Meta-analysis of the prevalence of anxiety disorders in mainland China from 2000 to 2015 open. Sci. Rep. 2016 doi: 10.1038/srep28033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamza T.H., van Houwelingen H.C., Stijnen T. The binomial distribution of meta-analysis was preferred to model within-study variability. J. Clin. Epidemiol. 2008;61:41–51. doi: 10.1016/j.jclinepi.2007.03.016. [DOI] [PubMed] [Google Scholar]
- Hao F., Tan W., Jiang L., Zhang L., Zhao X., Zou Y., Hu Y., Luo X., Jiang X., McIntyre R.S., Tran B., Sun J., Zhang Z., Ho R., Ho C., Tam W. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao X., Zhou D., Li Z., Zeng G., Hao N., Li E., Li W., Deng A., Lin M., Yan B. Severe psychological distress among patients with epilepsy during the COVID‐19 outbreak in southwest China. Epilepsia. 2020:16544. doi: 10.1111/epi.16544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Thomas J., Chandler J., Cumpston M., Li T., Page M. Cochrane; 2019. Cochrane Handbook for Systematic Reviews of Interventions, Version 6. ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins J.P.T., Thompson S.G., Jonathan J.D., Douglas G.A. Measuring inconsistency in meta-analyses. Br. Med. J. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., Tracey I., Wessely S., Arseneault L., Ballard C., Christensen H., Cohen Silver R., Everall I., Ford T., John A., Kabir T., King K., Madan I., Michie S., Przybylski A.K., Shafran R., Sweeney A., Worthman C.M., Yardley L., Cowan K., Cope C., Hotopf M., Bullmore E. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang Y., Zhao N. Mental health burden for the public affected by the COVID-19 outbreak in China: who will be the high-risk group? Psychol. Health Med. 2020:1–12. doi: 10.1080/13548506.2020.1754438. [DOI] [PubMed] [Google Scholar]
- Jernigan D.B. Update: public health response to the coronavirus disease 2019 outbreak–United States, February 24, 2020. Morb. Mortal. Wkly. Rep. 2020 doi: 10.15585/MMWR.MM6908E1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang X.L., Zheng X.Y., Yang J., Ye C.P., Chen Y.Y., Zhang Z.G., Xiao Z.J. A systematic review of studies on the prevalence of Insomnia in university students. Public Health. 2015 doi: 10.1016/j.puhe.2015.07.030. [DOI] [PubMed] [Google Scholar]
- John Hopkins University, 2020. Coronavirus COVID-19 (2019-nCoV) [WWW Document]. John Hopkins Univ. URL https://gisanddata.maps.arcgis.com/apps/opsdashboard/index.html#/bda7594740fd40299423467b48e9ecf6 (accessed 11.5.20).
- Keita M.M., Taverne B., Sy Savané S., March L., Doukoure M., Sow M.S., Touré A., Etard J.F., Barry M., Delaporte E. Depressive symptoms among survivors of Ebola virus disease in Conakry (Guinea): preliminary results of the PostEboGui cohort. BMC Psychiatry. 2017;17:127. doi: 10.1186/s12888-017-1280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler R.C., Aguilar-Gaxiola S., Alonso J., Benjet C., Bromet E.J., Cardoso G., Degenhardt L., de Girolamo G., Dinolova R.V., Ferry F., Florescu S., Gureje O., Haro J.M., Huang Y., Karam E.G., Kawakami N., Lee S., Lepine J.P., Levinson D., Navarro-Mateu F., Pennell B.E., Piazza M., Posada-Villa J., Scott K.M., Stein D.J., Ten Have M., Torres Y., Viana M.C., Petukhova M.V., Sampson N.A., Zaslavsky A.M., Koenen K.C. Trauma and PTSD in the WHO World Mental Health Surveys. Eur. J. Psychotraumatol. 2017 doi: 10.1080/20008198.2017.1353383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kokou-Kpolou C.K., Fernández-Alcántara M., Cénat J.M. Prolonged grief related to COVID-19 deaths: do we have to fear a steep rise in traumatic and disenfranchised griefs? Psychol. Trauma: Theory, Research, Practice, and Policy. 2020;12(S1):S94. doi: 10.1037/tra0000798. [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., Wu J., Du H., Chen T., Li R., Tan H., Kang L., Yao L., Huang M., Wang H., Wang G., Liu Z., Hu S. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.3976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lalonde K. Med. Libr. Assoc; 2020. COVID-19 Literature Searching. [Google Scholar]
- Lancee W.J., Maunder R.G., Goldbloom D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008;59:91–95. doi: 10.1176/ps.2008.59.1.91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S.A., Jobe M.C., Mathis A.A. Mental health characteristics associated with dysfunctional coronavirus anxiety. Psychol. Med. 2020 doi: 10.1017/S003329172000121X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehmann M., Bruenahl C.A., Löwe B., Addo M.M., Schmiedel S., Lohse A.W., Schramm C. Ebola and psychological stress of health care professionals. Emerg. Infect. Dis. 2015;21:913–914. doi: 10.3201/eid2105.141988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei L., Huang X., Zhang S., Yang J., Yang L., Xu M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in Southwestern China. Med. Sci. Monit. 2020:26. doi: 10.12659/msm.924609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li G., Miao J., Wang H., Xu S., Sun W., Fan Y., Zhang C., Zhu S., Zhu Z., Wang W. Psychological impact on women health workers involved in COVID-19 outbreak in Wuhan: a cross-sectional study. J. Neurol. Neurosurg. Psychiatry. 2020 doi: 10.1136/jnnp-2020-323134. [DOI] [PubMed] [Google Scholar]
- Li X., Yu H., Bian G., Hu Z., Liu X., Zhou Q., Yu C., Wu X., Yuan T.F., Zhou D. Prevalence, risk factors, and clinical correlates of insomnia in volunteer and at home medical staff during the COVID-19. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Qin Q., Sun Q., Sanford L.D., Vgontzas A.N., Tang X. Insomnia and psychological reactions during the COVID-19 outbreak in China. J. Clin. Sleep Med. 2020 doi: 10.5664/jcsm.8524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y., Wang Y., Jiang J., Valdimarsdóttir U.A., Fall K., Fang F., Song H., Lu D., Zhang W. Psychological distress among health professional students during the COVID-19 outbreak. Psychol. Med. 2020:1–12. doi: 10.1017/S0033291720001555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Z., Ge J., Yang M., Feng J., Qiao M., Jiang R., Bi J., Zhan G., Xu X., Wang L., Zhou Q., Zhou C., Pan Y., Liu S., Zhang H., Yang J., Zhu B., Hu Y., Hashimoto K., Jia Y., Wang H., Wang R., Liu C., Yang C. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain. Behav. Immun. 2020;88:916–919. doi: 10.1016/j.bbi.2020.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Petukhova M.V., Sampson N.A., Aguilar-Gaxiola S., Alonso J., Andrade L.H., Bromet E.J., De Girolamo G., Haro J.M., Hinkov H., Kawakami N., Koenen K.C., Kovess-Masfety V., Lee S., Medina-Mora M.E., Navarro-Mateu F., O'Neill S., Piazza M., Posada-Villa J., Scott K.M., Shahly V., Stein D.J., Ten Have M., Torres Y., Gureje O., Zaslavsky A.M., Kessler R.C., Al-Hamzawi A., Al-Kaisy M.S., Benjet C., Borges G., Bruffaerts R., Bunting B., De Almeida J.M.C., Cardoso G., Chatterji S., Cia A.H., Degenhardt L., De Jonge P., Demyttenaere K., Fayyad J., Florescu S., He Y., Hu C.Y., Huang Y., Karam A.N., Karam E.G., Kiejna A., Lepine J.P., Levinson D., McGrath J., Moskalewicz J., Pennell B.E., Slade T., Stagnaro J.C., Viana M.C., Whiteford H., Williams D.R., Wojtyniak B. Association of DSM-IV posttraumatic stress disorder with traumatic experience type and history in the World Health Organization World Mental Health surveys. JAMA Psychiatry. 2017 doi: 10.1001/jamapsychiatry.2016.3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu N., Zhang F., Wei C., Jia Y., Shang Z., Sun L., Wu L., Sun Z., Zhou Y., Wang Y., Liu W. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psychiatry Res. 2020;287 doi: 10.1016/j.psychres.2020.112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S., Yang L., Zhang C., Xiang Y.T., Liu Z., Hu S., Zhang B. Online mental health services in China during the COVID-19 outbreak. Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu W., Wang H., Lin Y., Li L. Psychological status of medical workforce during the COVID-19 pandemic: a cross-sectional study. Psychiatry Res. 2020;288 doi: 10.1016/j.psychres.2020.112936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin J. Joanna Briggs Inst.; 2017. The Joanna Briggs Institute Critical Appraisal tools for use in JBI Systematic Reviews Checklist for Prevalence Studies; pp. 1–7. [Google Scholar]; Accessed May 11, 2020. https://joannabriggs.org/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Prevalence_Studies2017_0.pdf.
- Mazza C., Ricci E., Biondi S., Colasanti M., Ferracuti S., Napoli C., Roma P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health. 2020;17:3165. doi: 10.3390/ijerph17093165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moccia L., Janiri D., Pepe M., Dattoli L., Molinaro M., De Martin V., Chieffo D., Janiri L., Fiorillo A., Sani G., Di Nicola M. Affective temperament, attachment style, and the psychological impact of the COVID-19 outbreak: an early report on the Italian general population. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.04.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moghanibashi-Mansourieh A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohammed A., Sheikh T.L., Gidado S., Poggensee G., Nguku P., Olayinka A., Ohuabunwo C., Waziri N., Shuaib F., Adeyemi J., Uzoma O., Ahmed A., Doherty F., Nyanti S.B., Nzuki C.K., Nasidi A., Oyemakinde A., Oguntimehin O., Abdus-Salam I.A., Obiako R.O. An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: a cross sectional study–2014. BMC Public Health. 2015;15:824. doi: 10.1186/s12889-015-2167-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann. Intern. Med. 2009;151:264–269. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- Mojtabai R., Jorm A.F. Trends in psychological distress, depressive episodes and mental health treatment-seeking in the United States: 2001-2012. J. Affect. Disord. 2015;174:556–561. doi: 10.1016/j.jad.2014.12.039. [DOI] [PubMed] [Google Scholar]
- Nguyen H.C., Nguyen M.H., Do B.N., Tran C.Q., Nguyen T.T.P., Pham K.M., Pham L.V., Tran K.V., Duong T.T., Tran T.V., Duong T.H., Nguyen T.T., Nguyen Q.H., Hoang T.M., Nguyen K.T., Pham T.T.M., Yang S.-H., Chao J.C.-J., Duong T.V. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J. Clin. Med. 2020;9:965. doi: 10.3390/jcm9040965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicola M., Alsafi Z., Sohrabi C., Kerwan A., Al-Jabir A., Iosifidis C., Agha M., Agha R. The socio-economic implications of the coronavirus and COVID-19 pandemic: a review. Int. J. Surg. 2020;78:185–193. doi: 10.1016/j.ijsu.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nishi D., Susukida R., Usuda K., Mojtabai R., Yamanouchi Y. Trends in the prevalence of psychological distress and the use of mental health services from 2007 to 2016 in Japan. J. Affect. Disord. 2018;239:208–213. doi: 10.1016/j.jad.2018.07.016. [DOI] [PubMed] [Google Scholar]
- Nussbaumer-Streit B., Mayr V., Dobrescu A.I., Chapman A., Persad E., Klerings I., Wagner G., Siebert U., Christof C., Zachariah C., Gartlehner G. Quarantine alone or in combination with other public health measures to control COVID‐19: a rapid review. Cochrane Database Syst. Rev. 2020;2020:1–46. doi: 10.1002/14651858.CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ohayon M.M. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med. Rev. 2002 doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V.G., Papoutsi E., Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain. Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prem K., Liu Y., Russell T.W., Kucharski A.J., Eggo R.M., Davies N., Flasche S., Clifford S., Pearson C.A.B., Munday J.D., Abbott S., Gibbs H., Rosello A., Quilty B.J., Jombart T., Sun F., Diamond C., Gimma A., van Zandvoort K., Funk S., Jarvis C.I., Edmunds W.J., Bosse N.I., Hellewell J., Jit M., Klepac P. The effect of control strategies to reduce social mixing on outcomes of the COVID-19 epidemic in Wuhan, China: a modelling study. Lancet Public Health. 2020;5:e261–e270. doi: 10.1016/S2468-2667(20)30073-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiu J., Shen B., Zhao M., Wang Z., Xie B., Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatry. 2020 doi: 10.1136/gpsych-2020-100213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers J.P., Chesney E., Oliver D., Pollak T.A., McGuire P., Fusar-Poli P., Zandi M.S., Lewis G., David A.S. Psychiatric and neuropsychiatric presentations associated with severe coronavirus infections: a systematic review and meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry. 2020 doi: 10.1016/S2215-0366(20)30203-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slade T., Grove R., Burgess P. Kessler Psychological Distress Scale: normative data from the 2007 Australian National Survey of Mental Health and Wellbeing. Aust. N. Z. J. Psychiatry. 2011;45:308–316. doi: 10.3109/00048674.2010.543653. [DOI] [PubMed] [Google Scholar]
- Stein, D.J., Scott, K.M., Peter De Jonge, Kessler, R.C., 2017. Epidemiology of anxiety disorders: from surveys to nosology and back. [DOI] [PMC free article] [PubMed]
- Stijnen T., Hamza T.H., Özdemir P. Random effects meta-analysis of event outcome in the framework of the generalized linear mixed model with applications in sparse data. Stat. Med. 2010;29:3046–3067. doi: 10.1002/sim.4040. [DOI] [PubMed] [Google Scholar]
- Thekkumpurath P., Venkateswaran C., Kumar M., Bennett M.I. Screening for psychological distress in palliative care: a systematic review. J. Pain Symptom Manage. 2008;36:520–528. doi: 10.1016/j.jpainsymman.2007.11.010. [DOI] [PubMed] [Google Scholar]
- Viechtbauer W. Conducting meta-analyses in R with the metafor package. J. Stat. Softw. 2010:36. doi: 10.18637/jss.v036.i03. [DOI] [Google Scholar]
- Vilagut G., Forero C.G., Barbaglia G., Alonso J. Screening for depression in the general population with the center for epidemiologic studies depression (ces-d): a systematic review with meta-analysis. PLoS ONE. 2016;11:1–17. doi: 10.1371/journal.pone.0155431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wade D.F., Moon Z., Windgassen S.S., Harrison A.M., Morris L., Weinman J.A. Non-pharmacological interventions to reduce ICU-related psychological distress: a systematic review. Minerva Anestesiol. 2016;82:465–478. [PubMed] [Google Scholar]
- Weinberger A.H., Gbedemah M., Martinez A.M., Nash D., Galea S., Goodwin R.D. Trends in depression prevalence in the USA from 2005 to 2015: widening disparities in vulnerable groups. Psychol. Med. 2018;48:1308–1315. doi: 10.1017/S0033291717002781. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2020. WHO Director-General's opening remarks at the media briefing on COVID-19 - 11 March 2020 [WWW Document]. World Heal. Organ. URL https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19—11-march-2020 (accessed 5.24.20).
- World Health Organization . Geneva; 2017. Depression and Other Common Mental Disorders: Global Health Estimates. [Google Scholar]
- Xiong J., Lipsitz O., Nasri F., Lui L.M.W., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R.S. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020 doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.