Abstract
Purpose
To evaluate the efficacy of endovascular treatment of intractable nasopharyngeal hemorrhage after radiotherapy for nasopharyngeal carcinoma (NPC) and report the relevant endovascular therapeutic experience.
Patients and Methods
Records of patients who underwent endovascular treatment for intractable nasopharyngeal hemorrhage after irradiation for NPC from January 2007 to December 2019 were reviewed. The demographics, endovascular therapeutic details, and clinical outcomes were analyzed.
Results
Twenty-four consecutive patients were included in this study. Nineteen patients underwent embolization of the bilateral internal maxillary arteries; one patient underwent embolization of the right internal maxillary artery and the left external carotid artery; one patient underwent embolization of the left internal maxillary artery and the right internal carotid artery, and the other three patients underwent embolization of the unilateral internal carotid artery. During a mean follow-up of 600.9 days (range, 2–1658 days), twenty patients showed no recurrence of bleeding; one patient died of hemorrhagic shock; one patient had recurrent bleeding, and angiography revealed a pseudoaneurysm in the right internal carotid artery, which was then embolized with spring coil after a 30-min occlusion test. Two patients had recurrent bleeding on 2.5 months and 29.9 months respectively after the endovascular treatment, and angiography showed hypervascularity supplied by the bilateral internal maxillary arteries and then was embolized with polyvinyl alcohol particles. The three patients who received re-interventions showed no re-bleeding until the last follow-up.
Conclusion
Pseudoaneurysm and hypervascularity are the main angiographic characteristics of patients with intractable nasopharyngeal hemorrhage after radiotherapy for NPC, and endovascular treatment provides a safe and effective management approach.
Keywords: nasopharyngeal carcinoma, hemorrhage, radiotherapy, endovascular treatment
Introduction
Nasopharyngeal carcinoma (NPC) is the most common head and neck malignant tumor in Southern China and Southeast Asia, with an incidence between 15 and 50 cases per 100 000.1 Radical radiotherapy is the mainstay of curative therapy for NPC.2 However, radiotherapy can lead to undesirable complications including nasopharyngeal hemorrhage which is frequently torrential and catastrophic and is one of the most clinical challenging conditions.3 Conventional methods for the control of such hemorrhages such as packing and compression are often inefficient in many post-irradiation patients because the vessels are found deep in the tissue, and they usually appear post-irradiation trismus.4 Open surgical ligation is also not a suitable treatment choice because there often exists focal infection and abundant collateral vessels and a high risk of complications.5 With the progress of the endovascular therapeutic techniques, more patients are likely to receive this treatment. At present, reports on endovascular treatment of nasopharyngeal hemorrhage after radiotherapy for NPC are mostly case reports and case series, and most of them have a short follow-up. Therefore, this study aims to evaluate the long-term efficacy of endovascular treatment of intractable nasopharyngeal hemorrhage after radiotherapy for NPC and report the relevant endovascular therapeutic strategies based on a relatively large size of samples of 24 patients during a 12-year period.
Patients and Methods
Study Populations
This study was approved by the Ethics Committee of Wuhan Union Hospital, Wuhan, China, and conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from each patient.
Records of patients who underwent endovascular treatment for nasopharyngeal hemorrhage after irradiation for NPC from January 2007 to December 2019 were reviewed. The demographics, interval time of the completion of primary radiotherapy to nasopharyngeal hemorrhage, pre-bleeding symptoms, the volume of bleeding, endovascular therapeutic details, and outcomes were analyzed.
Treatment
Upon the emergence of nasopharyngeal hemorrhage, maintaining the upper airway patency is essential (mucus suction, endotracheal intubation, or tracheotomy). All patients had oronasal packing/intranasal balloon tamponade and intravenous fluids/blood transfusions to maintain the vital signs. And then the patients received digital subtraction angiography (DSA) to identify the bleeding vessels and performed endovascular treatment.
All operations were performed by experienced doctors in the interventional operating room. Patients were put in a supine position. Firstly, the right femoral artery was punctured under local anesthesia and a 5F vascular sheath (Terumo, Tokyo, Japan) was inserted into the puncture site. Secondly, angiography of the bilateral internal and external carotid arteries was performed by a 5-F angiographic catheter (Cordis) through the 5F vascular sheath which aims to identify the bleeding vessels. Thirdly, in case of external carotid artery branch vessel bleeding, a microcatheter (Terumo, Tokyo, Japan) was used to insert the vessel superselectively, and then embolization was performed with polyvinyl alcohol particles, spring coils, gelfoam sponge, or a combination of these (Figure 1 and Supplementary Videos S1 and S2); In case of internal carotid artery bleeding, a 30-min occlusion test should be performed, which is helpful to evaluate the competency of collateral circulation. If the compensation of collateral circulation is good, the internal carotid artery can be occluded immediately by spring coils (Figure 2); if the compensation of collateral circulation is poor, the internal carotid artery can be occluded after a bypass operation or implanted with the covered stent according to the situation of the internal carotid artery. Fourthly, angiography was performed again to evaluate the embolization effect.
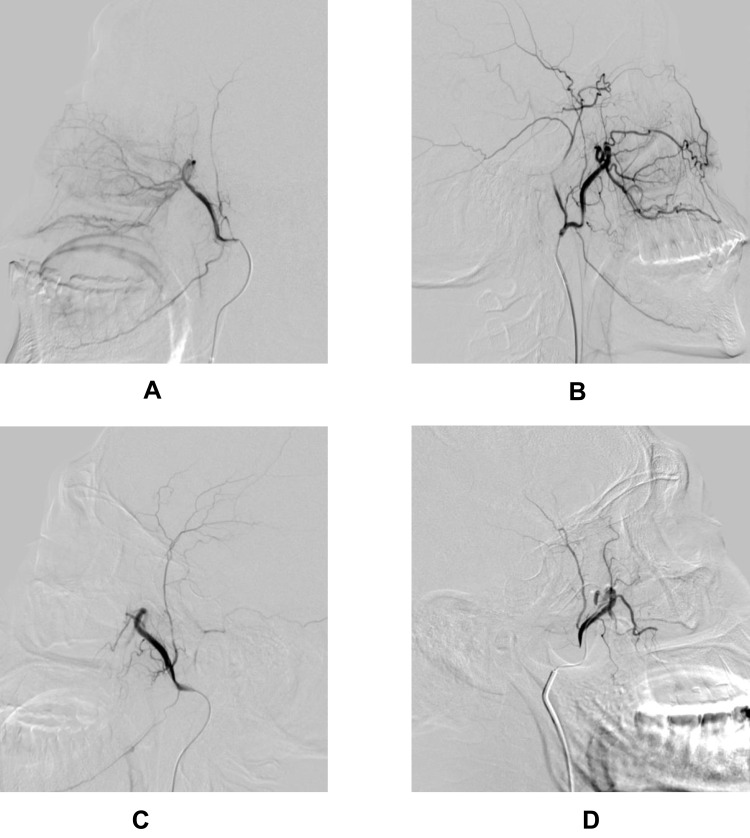
Figure 1.
(A and B) Digital subtraction angiography showed hypervascularity supplied by the cavernous bilateral internal maxillary arteries. (C and D) Postembolization internal maxillary arteries angiograms revealed total occlusion of the internal maxillary arteries and the hypervascularity did not appear.
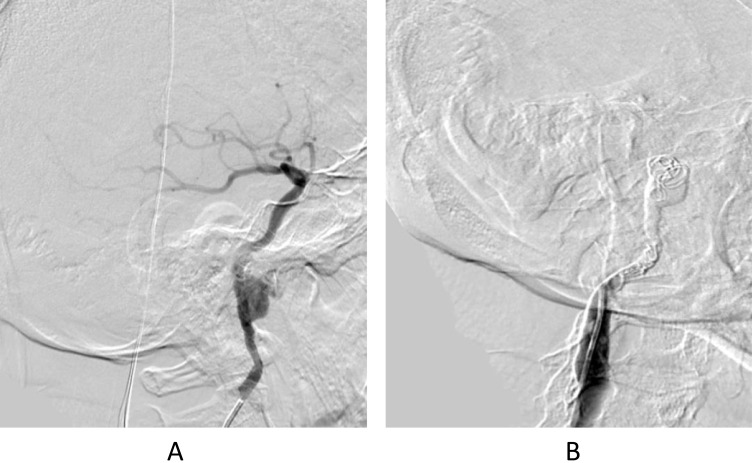
Figure 2.
(A) Digital subtraction angiography showed a pseudoaneurysm in the right internal carotid artery and the proximal wall of the internal carotid artery was rough. (B) The right internal carotid artery was embolized with spring coils after a 30-min occlusion test. Postembolization right internal carotid artery angiogram revealed total occlusion of the right internal carotid artery and the pseudoaneurysm was completely obliterated.
Results
Demographics and Clinical Features
A total of 24 consecutive patients who underwent endovascular treatment of nasopharyngeal hemorrhage after irradiation for NPC from January 2007 to December 2019 were included in this study. The median age was 61 years (range, 37–76 years). There were eighteen men (75.0%) and six women (25.0%). Thirteen patients (54.2%) received one-course radiotherapy, and eleven patients (45.8%) received second-course radiotherapy due to the local recurrence of NPC. The mean interval time of the completion of primary radiotherapy to nasopharyngeal hemorrhage was 90.3 months (range, 9–191 months). Before nasopharyngeal hemorrhage, thirteen patients (54.2%) complained of recurrent headaches, six patients (25%) presented with repeated little nasal bleeding, and the other five patients (20.8%) were asymptomatic. The cumulative total bleeding volume ranged between 300 and 1500 mL. (Table 1)
Table 1.
The Demographics and Clinical Features of Irradiated Patients Presenting with Intractable Nasopharyngeal Hemorrhage
| No | Sex | Age (Year) | Number of Radiotherapy | Pre-Bleeding Symptoms | NPC Recurrence at the Time of Bleeding | Bleeding Volume (mL) |
|---|---|---|---|---|---|---|
| 1 | M | 61 | 2 | Recurrent headaches | Yes | 1000 |
| 2 | F | 39 | 1 | Recurrent headaches | Yes | 1500 |
| 3 | M | 60 | 1 | Recurrent headaches | No | 450 |
| 4 | M | 55 | 2 | Repeated little nasal bleeding | Yes | 600 |
| 5 | M | 37 | 2 | No | Yes | 600 |
| 6 | M | 71 | 1 | Repeated little nasal bleeding | No | 550 |
| 7 | M | 76 | 1 | Recurrent headaches | No | 350 |
| 8 | M | 68 | 1 | Recurrent headaches | Yes | 300 |
| 9 | F | 65 | 2 | No | No | 450 |
| 10 | M | 40 | 2 | Recurrent headaches | No | 800 |
| 11 | F | 51 | 1 | Recurrent headaches | No | 450 |
| 12 | M | 55 | 2 | Repeated little nasal bleeding | No | 1200 |
| 13 | M | 46 | 1 | Repeated little nasal bleeding | No | 350 |
| 14 | M | 60 | 2 | No | No | 850 |
| 15 | M | 62 | 1 | Recurrent headaches | No | 500 |
| 16 | F | 42 | 2 | Repeated little nasal bleeding | No | 800 |
| 17 | F | 61 | 2 | Recurrent headaches | No | 750 |
| 18 | M | 66 | 2 | Recurrent headaches | No | 850 |
| 19 | M | 63 | 1 | No | No | 300 |
| 20 | M | 56 | 2 | Recurrent headaches | Yes | 650 |
| 21 | F | 70 | 1 | No | No | 300 |
| 22 | M | 65 | 2 | Recurrent headaches | No | 750 |
| 23 | M | 67 | 1 | Recurrent headaches | No | 750 |
| 24 | M | 62 | 2 | Repeated little nasal bleeding | No | 600 |
Abbreviation: NPC, nasopharyngeal carcinoma.
Treatment
The angiographic findings showed that nineteen patients with hypervascularity supplied by the cavernous bilateral internal maxillary arteries, one patient with hypervascularity supplied by the right internal maxillary artery and with the left external carotid artery occluded in the segment of the facial artery, one patient with hypervascularity supplied by the left internal maxillary artery and with the right internal carotid artery stenosis, and three patients with contrast extravasation from the internal carotid artery or pseudoaneurysm in the internal carotid artery.
In total, nineteen patients were managed with polyvinyl alcohol particles of various sizes or combined with gelfoam sponge embolization of the bilateral internal maxillary artery; one patient was managed with polyvinyl alcohol particles and spring coils embolization of the right internal maxillary artery and the left external carotid artery; one patient was managed with polyvinyl alcohol particles and spring coils embolization of the left internal maxillary artery and the right internal carotid artery, and the other three patients were managed with spring coils embolization of the internal carotid artery. (Table 2)
Table 2.
Treatments and Outcomes of Irradiated Patients Presenting with Intractable Nasopharyngeal Hemorrhage
| No | Angiographic Findings | Embolic Agent | Embolized Vessels | Death Time (Days)/Cause | Re-Bleeding Time (Days) | Re-Intervention | Re-Bleeding After the Second Intervention |
|---|---|---|---|---|---|---|---|
| 1 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | 2/massive hemorrhage | 2 | No | N/A |
| 2 | Hypervascularity supplied by the right IMA and the left ECA occluded in the segment of the FA | PVA + coils | Right IMA and left ECA | N/A | 75 | Yes | No |
| 3 | Hypervascularity supplied by bilateral IMA | PVA + gelfoam sponge | Bilateral IMA | N/A | N/A | No | No |
| 4 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | 3 | Yes | No |
| 5 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | 897 | Yes | No |
| 6 | Hypervascularity supplied by the left IMA and the right ICA stenosis | PVA | Left IMA and right ICA | N/A | N/A | No | N/A |
| 7 | Contrast extravasation from the right stenotic ICA | Coils | Right ICA | N/A | N/A | No | N/A |
| 8 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 9 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 10 | Hypervascularity supplied by bilateral IMA | PVA + gelfoam sponge | Bilateral IMA | N/A | N/A | No | N/A |
| 11 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 12 | Pseudoaneurysm in right the ICA | Coils | Right ICA | N/A | N/A | No | N/A |
| 13 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 14 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 15 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 16 | Hypervascularity supplied by bilateral IMA | PVA + gelfoam sponge | Bilateral IMA | N/A | N/A | No | N/A |
| 17 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 18 | Hypervascularity supplied by bilateral IMA | PVA + gelfoam sponge | Bilateral IMA | N/A | N/A | No | N/A |
| 19 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 20 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 21 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
| 22 | Hypervascularity supplied by bilateral IMA | PVA + gelfoam sponge | Bilateral IMA | N/A | N/A | No | N/A |
| 23 | Pseudoaneurysm in the left ICA | Coils | Left ICA | N/A | N/A | No | N/A |
| 24 | Hypervascularity supplied by bilateral IMA | PVA | Bilateral IMA | N/A | N/A | No | N/A |
Abbreviations: IMA, internal maxillary artery; PVA, polyvinyl alcohol particles; ECA, external carotid artery; FA, facial artery; N/A, not applicable; ICA, internal carotid artery.
Outcomes
The mean follow-up was 600.9 days (range, 2–1658 days). After the endovascular treatment, one patient had bilateral maxillofacial pain, and the symptom was entirely resolved in half a month.
During the follow-up period, twenty patients (83.3%) showed no recurrence of bleeding; one patient (4.2%) died of hemorrhagic shock 2 days after the endovascular treatment (case 1); one patient (4.2%) had recurrent bleeding after the endovascular treatment, and angiography was performed on the third day of post-operation, which revealed a pseudoaneurysm in the right internal carotid artery and the proximal wall of the internal carotid artery was rough which be impaired by radiotherapy, and then the right internal carotid artery was embolized with spring coils after a 30-min occlusion test (case 4); Two patients (8.3%) had recurrent bleeding on 2.5 months (case 2) and 29.9 months (case 5) respectively after the endovascular treatment, and angiography showed hypervascularity supplied by the bilateral internal maxillary arteries and then were embolized with polyvinyl alcohol particles. The three patients who received re-interventions showed no recurrence of bleeding until the last follow-up. (Table 2)
Discussion
Nasopharyngeal hemorrhage is described as a sudden hemorrhage of >100 mL or continuous bleeding of more than 300 mL in the nasopharyngeal area within a short period and represents a particular subtype of epistaxis after radiotherapy for NPC.4,6 The condition is usually lethal and the main causes are as following: firstly, there is an abundant blood supply around the nasopharynx, including the ascending pharyngeal artery, pharyngeal artery, pterygoid artery, ascending palatine artery, and internal carotid artery. Meanwhile, the growth of tumor and radiotherapy result in the extensive development of the collateral vessels in the nasopharynx.7 Therefore, the patients with NPC after radiotherapy are likely to appear intractable hemorrhage; Secondly, the glossopharyngeal nerve is located in the radiotherapy field of NPC. After radiotherapy, the glossopharyngeal nerve is damaged, resulting in a decrease of pharyngeal sensation and atrophy of muscles.8 Once a massive hemorrhage occurs, the patients cannot swallow or cough up the blood in time, resulting in much blood flowing into the trachea quickly and causing asphyxia; Thirdly, the patients irradiated for NPC usually appear post-irradiation trismus and adhesion of the nasal cavity. Therefore, the traditional hemostasis methods, such as packing and balloon tamponade, are ineffective, resulting in hemorrhagic shock.9 Multiple factors had been reported contribute to such nasopharyngeal hemorrhage, including high dose radiotherapy which makes the vessels hard and fibrotic, the mucosa of the nasopharynx is damaged and ulcerated, and the surrounding tissue is necrotic, which promotes local infection and inflammation, and aggravates vascular damage.6,10,11 Additionally, the recurrence of the tumor and the second-course radiotherapy is also the relevant causes.5,12
Various hemostasis methods, including anterior and posterior nostril packing, carotid artery ligation, and endovascular treatment, were used in clinical practice. Nasal packing could often be ineffective because the hemorrhage usually results from a residual or recurrent tumor, pseudoaneurysm formation as well as osteonecrosis and soft tissue inflammation, and the patients usually appear post-irradiation trismus and adhesion of the nasal cavity.9 Surgical ligation of the feeding artery might be unsuccessful because of the presence of extensive collateral vessels and performing the surgical operation in patients at low blood volume increases the risk of complications.5 Endovascular treatment has been recommended as the first-line treatment modality by some doctors because angiography can detect the bleeding vessels quickly and accurately and endovascular embolization has a high success rate, especially for patients with a ruptured pseudoaneurysm in the internal carotid which is a significant catastrophic condition.7,13–15 In our study, twenty-three patients (95.8%) were successfully treated by one-time or two-time endovascular embolization, which showed a great efficacy of endovascular treatment of nasopharyngeal hemorrhage after radiotherapy for NPC. One patient died of abrupt massive hemorrhage (case 1) and three patients had re-bleeding (case 2, case 4, case 5). All of them had a recurrence of NPC, so the cause of re-bleeding may be the advanced disease and these patients should be close surveillance. In our cases, 66.7% (4/6) patients suffering from a recurrence of NPC had re-bleeding after international embolization. Similarly, Low and Goh reported that 66.7% (4/6) suffering from a recurrence of NPC had re-bleeding after international embolization and 75% of them (3/4) died.9 Therefore, the recurrence of NPC may be a potential risk factor for re-bleeding after international embolization. In our cases, 3 patients (3/13, 23.1%) receiving second-course radiotherapy had re-bleeding and 1 patient (1/11, 9.1%) receiving one-course had re-bleeding. It seems that the patients receiving one-course radiotherapy had a better endovascular treatment efficacy of nasopharyngeal hemorrhage than that receiving second-course radiotherapy, but the result still needs a large size of samples to confirm.
According to the reports in the literature, angiographic features of nasopharyngeal hemorrhage in patients irradiated for NPC included the overflow of contrast medium from the bleeding artery, abnormal or dysplastic irregular vessels in and around the nasal cavity segmental, arterial stenosis, arterial ballooning, and pseudoaneurysm formation.9,16 Importantly, rotational angiography is necessary which may be a great help in identifying those small lesions superimposed on carotid branches. In our cases, the angiographic findings included hypervascularity supplied by internal maxillary arteries, carotid artery stenosis, pseudoaneurysm, and contrast extravasation from the stenotic internal carotid artery, which is consistent with the reports above.
In terms of performing the endovascular treatment, the following suggestions are summed based on our experiences: (1) before endovascular treatment, angiography including bilateral internal and external carotid arteries must be performed in multiple directions to detect small lesions and collateral vessels. (2) For nasopharynx bleeding caused by the rupture of branches of the external carotid artery, it is necessary to use a microcatheter to insert the bleeding vessels as much as possible; if the bleeding vessels are seriously tortuous or narrow, which make it difficult to insert the vessels in a short time, the main trunk of the external carotid artery should be selected for embolization to control the lethal hemorrhage. Common embolic materials include polyvinyl alcohol particles, spring coil, NBCA (isobutyl cyanoacrylate), and gelatin sponge, and gelatin sponge cannot be used alone because of the risk of vascular recanalization. (3) For nasopharynx bleeding caused by pseudoaneurysm rupture of the internal carotid artery, a 30-min occlusion test should be performed. If the compensation of collateral circulation is good, using the spring coils to embolize the proximal and distal ends of the pseudoaneurysm after the non-detachable balloon blocks the proximal blood flow of the internal carotid artery; If the compensation of collateral circulation is poor, the internal carotid artery can be occluded after a bypass operation or implanted the covered stent according to the situation of the internal carotid artery. He et al reported that detachable balloons can be used to occlude the pseudoaneurysm.7 In our experience of embolizing bleeding vessels after radiotherapy, we do not recommend using the detachable balloon because the tension of the balloon may result in the rupture of the fragile vessels and the balloon can migrate after placement. It has been reported that stents can be used to embolize pseudoaneurysm.15 However, He et al reported that concerning stent erosion and infection because of local inflamed and necrotic tissue, as well as a lack of antiplatelet preparation, the main trunk occlusion should be thought as the preferred treatment toward, if feasible.7 In our experience, we agree with He’s opinion because most of the lesion vessels are significantly poor and the coils are the common embolized agents that can be used in emergent situations. But in some situations where the patients’ hemodynamics are stable and the lesion vessels are not so much poor, the covered stents can be considered to be used. (4) It has been reported that spontaneous occlusion of the internal carotid artery can be seen on angiography, which may occur under the conditions of nasal packing, hemostatic drugs, and hypotension, etc. The author thought that there is a possibility of recanalization, so the internal carotid artery should be embolized by spring coils.17 (5) The extent of embolization should be long enough to include all abnormal vessels such as vascular rough, vascular serious tortuosity, vascular stenosis et al, because all these image characteristics are indicated for fragile vessels. (6) After embolization, multi-directional angiography is needed again to detect the re-bleeding caused by collateral vessels.
It has been reported that some complications occurred after endovascular treatment, which includes hemiparesis, blindness, aphasia, and other symptoms of nervous system ischemia.9 However, the incidence of complications is low and most of them are curable. Luo et al reported endovascular treatment was successful in all 14 patients with radiation carotid blowout syndromes with the cessation of hemorrhage and only one patient had hemiparesis after embolization.16 He et al reported that three patients experienced headaches and two patients experienced low fever after the embolization, and the above symptoms recovered normal in 24–48h.7 In our cases, one patient had bilateral maxillofacial pain after the endovascular treatment, and the symptom was entirely resolved after hormone-assisted supportive therapy in half a month. Therefore, endovascular treatment is a safe method for NPC patients after radiotherapy with intractable nasopharyngeal hemorrhage.
Conclusion
Pseudoaneurysm and hypervascularity are the main angiographic characteristics of patients with intractable nasopharyngeal hemorrhage after radiotherapy for NPC, and endovascular treatment provides a safe and effective management approach.
Disclosure
This work was funded by grants from National Natural Science Foundation of China [81873917] and China Health Promotion Foundation [XM_2018_011_0006_01] and there is no other funding or financial relationships to disclose. The authors report no potential conflicts of interest for this work.
References
- 1.Hui EP, Ma BBY, King AD, et al. Hemorrhagic complications in a Phase II study of sunitinib in patients of nasopharyngeal carcinoma who has previously received high-dose radiation. Ann Oncol. 2011;22(6):1280–1287. doi: 10.1093/annonc/mdq629 [DOI] [PubMed] [Google Scholar]
- 2.Pastor M, Lopez Pousa A, Del Barco E, et al. SEOM clinical guideline in nasopharynx cancer (2017). Clin Transl Oncol. 2018;20(1):84–88. doi: 10.1007/s12094-017-1777-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Agulnik M, Epstein JB. Nasopharyngeal carcinoma: current management, future directions and dental implications. Oral Oncol. 2008;44(7):617–627. doi: 10.1016/j.oraloncology.2007.08.003 [DOI] [PubMed] [Google Scholar]
- 4.Chen HY, Ma XM, Bai YR. Repeated massive epistaxis after re-irradiation in recurrent nasopharyngeal carcinoma. Contemp Oncol (Pozn). 2014;18(5):371–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lam JWK, Chan JYW, Lui WM, Ho WK, Lee R, Tsang RKY. Management of pseudoaneurysms of the internal carotid artery in postirradiated nasopharyngeal carcinoma patients. Laryngoscope. 2014;124(10):2292–2296. doi: 10.1002/lary.24721 [DOI] [PubMed] [Google Scholar]
- 6.Zhan J, Zhang S, Wei X, Fu Y, Zheng J. Etiology and management of nasopharyngeal hemorrhage after radiotherapy for nasopharyngeal carcinoma. Cancer Manag Res. 2019;11:2171–2178. doi: 10.2147/CMAR.S183537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.He C, Si Y, Xie Y, Yu L. Management of intractable epistaxis in patients who received radiation therapy for nasopharyngeal carcinoma. Eur Arch Otorhinolaryngol. 2013;270(10):2763–2767. doi: 10.1007/s00405-013-2598-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Au KH, Ngan RKC, Ng AWY, et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: a report of 3328 patients (HKNPCSG 1301 study). Oral Oncol. 2018;77:16–21. doi: 10.1016/j.oraloncology.2017.12.004 [DOI] [PubMed] [Google Scholar]
- 9.Low YM, Goh YH. Endovascular treatment of epistaxis in patients irradiated for nasopharyngeal carcinoma. Clin Otolaryngol Allied Sci. 2003;28(3):244–247. doi: 10.1046/j.1365-2273.2003.00699.x [DOI] [PubMed] [Google Scholar]
- 10.Li JH, Peh WC, Sham JS. Maxillary osteonecrosis after radiotherapy for nasopharyngeal carcinoma. Clin Oncol (R Coll Radiol). 1994;6(2):135–136. doi: 10.1016/S0936-6555(05)80118-9 [DOI] [PubMed] [Google Scholar]
- 11.Bedwlnek JM, Shukovsky LJ, Fletcher GH, Daley TE. Osteonecrosis in patients treated with definitive radiotherapy for squamous cell carcinomas of the oral cavity and naso- and oropharynx. Ther Radiol. 1976;119:665–667. doi: 10.1148/119.3.665 [DOI] [PubMed] [Google Scholar]
- 12.Han F, Zhao C, Huang S, et al. Long-term outcomes and prognostic factors of re-irradiation for locally recurrent nasopharyngeal carcinoma using intensity-modulated radiotherapy. Clin Oncol-UK. 2011;24(8):569–576. doi: 10.1016/j.clon.2011.11.010 [DOI] [PubMed] [Google Scholar]
- 13.Mok JSW, Marshall JN, Chan M, van Hasselt CA. Percutaneous embolization to control intractable epistaxis in nasopharyngeal carcinoma. Head Neck. 1999;21:211–216. doi: [DOI] [PubMed] [Google Scholar]
- 14.Wong GKC, Chan KK, Yu SCH, Tsang RKY, Poon WS. Treatment of profuse epistaxis in patients irradiated for nasopharyngeal carcinoma. ANZ J Surg. 2007;77(4):270–274. doi: 10.1111/j.1445-2197.2007.04032.x [DOI] [PubMed] [Google Scholar]
- 15.Cheng KM, Chan CM, Cheung YL, Chiu HM, Tang KW, Law CK. Endovascular treatment of radiation-induced petrous internal carotid artery aneurysm presenting with acute haemorrhage. A report of two cases. Acta Neurochir (Wien). 2001;143(4):351–356. doi: 10.1007/s007010170089 [DOI] [PubMed] [Google Scholar]
- 16.Luo C, Teng MM, Chang F, Chang C, Guo W. Radiation carotid blowout syndrome in nasopharyngeal carcinoma: angiographic features and endovascular management. Otolaryngol Head Neck Surg. 2008;138(1):86–91. [DOI] [PubMed] [Google Scholar]
- 17.Chen R, Chen J, Bai X, et al. Endovascular embolization of nasopharyngeal hemorrhage in patients irradiated for nasopharyngeal carcinoma. J Fujian Med Univ. 2018;52(01):57–59. [Google Scholar]