Abstract
Acute kidney injury (AKI) is a frequent complication of traumatic injury; however, long-term outcomes such as mortality and end-stage kidney disease (ESKD) have been rarely reported in this important patient population. We compared the long-term outcome of vehicle-traumatic and non-traumatic AKI requiring renal replacement therapy (AKI-RRT). This nationwide cohort study used data from the Taiwan National Health Insurance Research Database. Vehicle-trauma patients who were suffered from vehicle accidents developing AKI-RRT during hospitalization were identified, and matching non-traumatic AKI-RRT patients were identified between 2000 and 2010. The incidences of ESKD, 30-day, and long-term mortality were evaluated, and clinical and demographic associations with these outcomes were identified using Cox proportional hazards regression models. 546 vehicle-traumatic AKI-RRT patients, median age 47.6 years (interquartile range: 29.0–64.3) and 76.4% male, were identified. Compared to non-traumatic AKI-RRT, vehicle-traumatic AKI-RRT patients had longer length of stay in hospital [median (IQR):15 (5–34) days vs. 6 (3–11) days; p < 0.001). After propensity matching with non-traumatic AKI-RRT cases with similar demographic and clinical characteristics. Vehicle-traumatic AKI-RRT patients had lower rates of long-term mortality (adjusted hazard ratio (HR), 0.473; 95% CI, 0.392–0.571; p < 0.001), but similar rates of ESKD (HR, 1.166; 95% CI, 0.829–1.638; p = 0.377) and short-term risk of death (HR, 1.134; 95% CI, 0.894–1.438; p = 0.301) as non-traumatic AKI-RRT patients. In competing risk models that focused on ESKD, vehicle-traumatic AKI-RRT patients were associated with lower ESKD rates (HR, 0.552; 95% CI, 0.325–0.937; p = 0.028) than non-traumatic AKI-RRT patients. Despite severe injuries, vehicle-traumatic AKI-RRT patients had better long-term survival than non-traumatic AKI-RRT patients, but a similar risk of ESKD. Our results provide a better understanding of long-term outcomes after vehicle-traumatic AKI-RRT.
Subject terms: Haemodialysis, Outcomes research
Introduction
Background
Acute kidney injury (AKI) has been studied in a wide range of populations and has been consistently associated with increased risk of future morbidity and mortality1,2. The in-hospital mortality associated with AKI ranges from 9.1% to 21.9% in the United States3, and amounts to as high as 62% in the critical care setting in patients requiring renal replacement therapy (RRT)4,5. As AKI is a clinical syndrome it treatment should be tailored to its underlying etiology. While considerable data exist on the epidemiology, outcomes and suggested management of AKI in settings such as sepsis or nephrotoxin exposure, comparatively less data is available to guide clinicians on the clinical course of AKI after major trauma.
Trauma is a leading cause of hospitalization worldwide, which mainly affects a young and previously healthy population both in the developed and developing world. The incidence of AKI among major traumatic injuries has been reported to be 6.0–36.8%6,7, and traumatic AKI has been associated with a mortality rate of 14.9–57.0%7–10. Overall around 5% of trauma patients admitted to the intensive care unit (ICU) require RRT10. In a recent systematic review the pooled incidence of AKI after trauma was 20.4% with an associated 3.6-fold increase in the relative risk of death, commonly reported associations of AKI after trauma include older age, higher severity of injury, volume of blood transfusion, abdominal site of injury and presence of comorbid disease including diabetes mellitus11. Prior studies of traumatic AKI-RRT have focused mainly on short-term outcomes12,13 and detailed comparisons of outcomes between traumatic-AKI and AKI of differing etiologies that have not been made.
Given the paucity of studies concerning traumatic AKI-RRT, we sought to describe its epidemiology and associated short and long-term outcomes in a large epidemiological database.
Results
Temporal change in in-hospital mortality
Among 123,470 hospitalized AKI-RRT patients in the past decade, we identified 546 vehicle-traumatic AKI-RRT patients who survived to index discharge (Fig. 1). The annual number of trauma cases decreased gradually; however, the proportions of vehicle-traumatic AKI-RRT patients tended to increase over time, especially in the elderly group (aged ≥ 65 years) (Fig. 2). In our cohort, young patients (aged ≤ 44 years) were less likely to be admitted because of trauma; however, they had the highest incidence of vehicle-traumatic AKI-RRT (Fig. 2) during hospitalization. On the other hand, soft tissue injury from trauma had the lowest incidence of AKI-RRT (Fig. 3).
Figure 1.
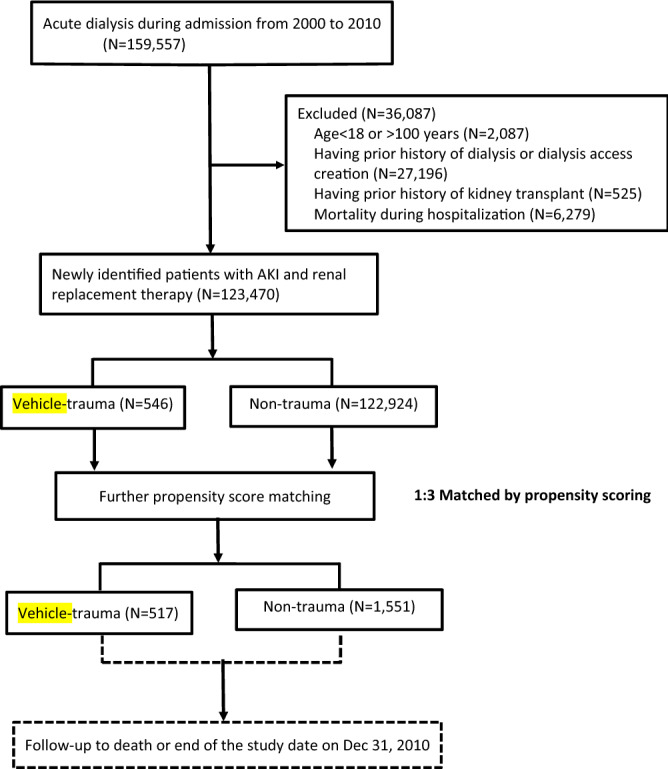
Flow chart of the participants.
Figure 2.
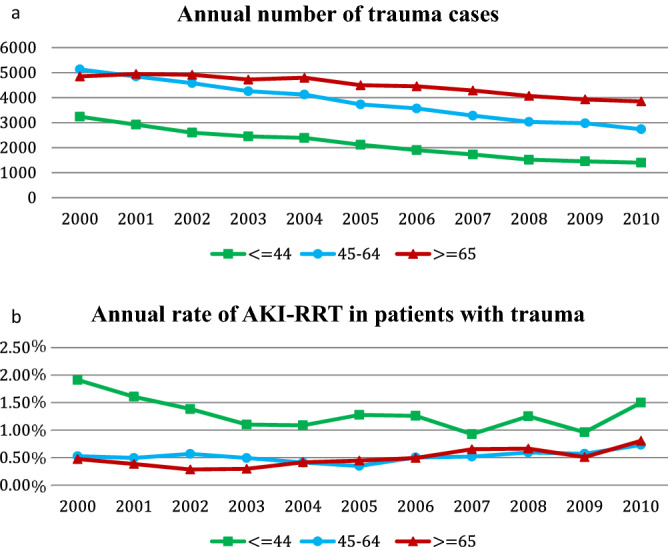
Temporal patterns of annual number of trauma cases (a) and annual rate of vehicle-traumatic AKI-RRT (b) stratified by age groups (annual rate of vehicle-traumatic AKI-RRT = annual number of vehicle-traumatic AKI-RRT/ annual number of trauma cases). (b) p for trend, age ≦ 44: 0.073, 45 < age < 65: 0.183, age ≧ 65: 0.004).
Figure 3.
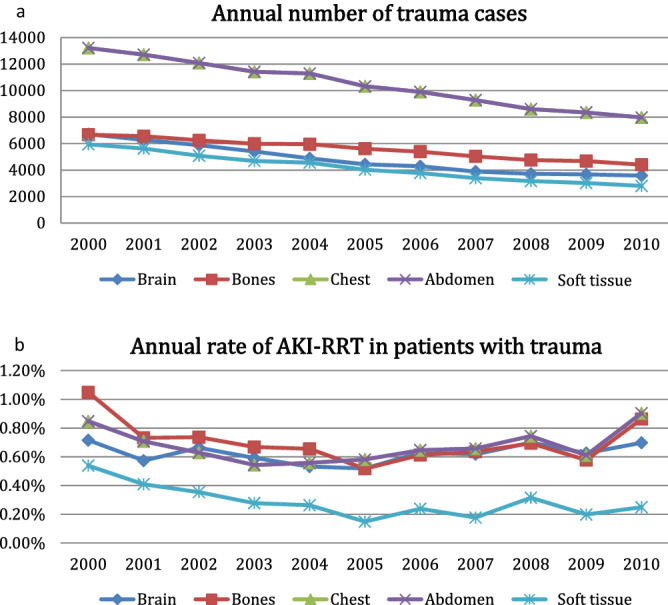
Temporal patterns of annual number of trauma cases (a) and annual rate of traumatic AKI-RRT (b) stratified by injured body part (annual rate of vehicle-traumatic AKI-RRT = annual number of vehicle-traumatic AKI-RRT/ annual number of trauma cases). (b) p for trend, brain: 0.697, bones: 0.186, chest: 0.484, abdomen: 0.484, Skin: 0.024).
Patient characteristics before and after propensity score matching
Compared to patients with other causes of AKI-RRT, vehicle-traumatic AKI-RRT patients were younger [median IQR: 47.6 (29.0–64.3) vs. 65.9 (53.7–74.5), p < 0.001) and more of them were male (77.1% vs. 54.2%, p < 0.001). Vehicle-traumatic AKI-RRT patients also had a lower rate of cerebrovascular disease, COPD, diabetes, liver disease, and advanced chronic kidney disease (CKD) which was defined as the presence of CKD coding and concomitant reimbursement coding of erythropoiesis-stimulating agents without copayment. More pulmonary and cardiac complications occurred in AKI-RRT patients than non-traumatic AKI-RRT patients during hospitalization. Among them, 517 vehicle-traumatic AKI-RRT patients were successfully matched with 1,551 non-traumatic AKI-RRT patients (Table 1).
Table 1.
Clinical characteristics after propensity score matching (NHIR database).
| Variables | Before matching | After matching | ||||
|---|---|---|---|---|---|---|
| Non-trauma group (n = 122,924) |
Trauma group (n = 546) |
p Value | Non-trauma group (n = 1,551) |
Trauma group (n = 517) |
p Value | |
| Gender (Male) | 66,595 (54.2%) | 421 (77.1%) | < 0.001 | 1183 (76.3%) | 395 (76.4%) | 0.952 |
| Age (year) (IQR) | 65.9 (53.7–74.5) | 47.6 (29.0–64.3) | < 0.001 | 48.7 (34.2–64.9) | 48.7 (31.5–65.3) | 0.469 |
| Pre-admission Comorbidities | ||||||
| Charlson comorbidity index (IQR) | 0 (0–0) | 0 (0–1) | < 0.001 | 0 (0–1) | 0 (0–1) | 0.075 |
| Myocardial infarction | 988 (0.8%) | 3 (0.6%) | 0.51 | 10 (0.6%) | 3 (0.6%) | 0.872 |
| Congestive heart failure | 5410 (4.4%) | 22 (4.0%) | 0.67 | 80 (5.1%) | 22 (4.3%) | 0.412 |
| Cerebrovascular disease | 9742 (7.9%) | 13 (2.4%) | < 0.001 | 41 (2.6%) | 13 (2.5%) | 0.874 |
| Dementia | 1384 (1.1%) | 1 (0.2%) | 0.04 | 6 (0.4%) | 1 (0.2%) | 0.512 |
| Chronic obstructive pulmonary disease | 12,042 (9.8%) | 30 (5.5%) | < 0.001 | 90 (5.8%) | 30 (5.8%) | 0.999 |
| Peptic ulcer disease | 12,025 (9.8%) | 28 (5.1%) | < 0.001 | 99 (6.4%) | 28 (5.4%) | 0.428 |
| Diabetes mellitus | 42,643 (34.7%) | 77 (14.1%) | < 0.001 | 209 (13.4%) | 77 (14.9%) | 0.419 |
| Moderate or severe liver disease | 7229 (5.9%) | 24 (4.4%) | 0.14 | 91 (5.8%) | 24 (4.6%) | 0.293 |
| Chronic kidney disease | 92,238 (75.0%) | 130 (23.8%) | < 0.001 | 388 (24.9%) | 130 (25.2%) | 0.953 |
| Advanced chronic kidney disease* | 51,628 (42.0%) | 41 (7.51%) | < 0.001 | 119 (7.6%) | 41 (7.9%) | 0.849 |
| In-hospital Acute Comorbidities | ||||||
| Pulmonary complications | ||||||
| Prolonged mechanical ventilation** | 10,506 (8.6%) | 416 (76.2%) | < 0.001 | 1184 (76.0%) | 387 (74.9%) | 0.494 |
| Re-intubation | 5989 (4.9%) | 228 (41.8%) | < 0.001 | 688 (44.2%) | 217 (42.0%) | 0.344 |
| Acute respiratory distress syndrome | 509 (0.4%) | 7 (1.3%) | 0.002 | 35 (2.3%) | 7 (1.4%) | 0.208 |
| Pleural effusion | 376 (0.3%) | 3 (0.6%) | 0.30 | 11 (0.7%) | 3 (0.6%) | 0.753 |
| Chest tube insertion | 1041 (0.9%) | 111 (20.3%) | < 0.001 | 247 (15.9%) | 90 (17.4%) | 0.429 |
| Hemodynamic complications | ||||||
| Hypovolemic shock | 668 (0.5%) | 12 (2.2%) | < 0.001 | 32 (2.1%) | 10 (1.9%) | 0.856 |
| ECMO use | 147 (0.1%) | 17 (3.1%) | < 0.001 | 44 (2.8%) | 12 (2.3%) | 0.532 |
| Main cause of infection | ||||||
| Pneumonia | 2346 (1.9%) | 5 (0.9%) | 0.09 | 14 (0.9%) | 5 (1.0%) | 0.894 |
| Urinary tract infection | 2984 (2.4%) | 4 (0.7%) | 0.01 | 19 (1.2%) | 4 (0.8%) | 0.397 |
| Severe sepsis | 6041 (4.9%) | 72 (13.2%) | < 0.001 | 243 (15.6%) | 68 (13.2%) | 0.166 |
| Outcomes | ||||||
| Index hospital stay (day) (IQR) | 6 (3–11) | 15 (5–34) | < 0.001 | 12 (5–28) | 15 (5–35) | 0.007 |
| Follow-up duration (year) (IQR) | 3.32 (0.1–8.85) | 2.49 () | ||||
| 30-day mortality | 2490 (2.0%) | 99 (18.1%) | < 0.001 | 248 (15.9%) | 95 (18.4%) | 0.207 |
| Long-term mortality | 73,777 (60.0%) | 134 (24.5%) | < 0.001 | 729 (46.8%) | 129 (25.0%) | < 0.001 |
| ESKD | 32,445 (26.4%) | 45 (8.2%) | < 0.001 | 208 (13.4%) | 55 (10.6%) | 0.892 |
ECMO, extracorporeal membrane oxygenation; ESKD, end stage kidney disease; IQR, interquartile range.
*Advanced chronic kidney disease: presence of CKD coding and concomitant reimbursement coding of erythropoiesis-stimulating agents without copayment.
**Prolonged mechanical ventilation: the use of mechanical ventilation ≥ 21 days.
To evaluate the potential etiology of AKI in our cohort (Supplemental Table 1), we collected the data of in-hospital acute comorbidities, including hypovolemic shock, cardiogenic shock, and severe sepsis which may relate to AKI. In addition, we also collected the data of contrast exposure and nephrotoxicity medications exposure before AKI-RRT after propensity score matching. Non-trauma patients had higher risk of cardiogenic shock (17.4% vs. 1.2%, p < 0.001) and nephrotoxicity medications exposure (18.6% vs. 2.9%, p < 0.001).
The overall median (IQR) follow-up duration is 2.65 (0.14–7.04) years. The vehicle-traumatic group follow-up duration is 3.32 (0.10–8.85) years and the non-traumatic group follow-up duration is 2.49 (0.16–6.39) years.
Outcomes in patients with AKI-RRT after discharge
After propensity score matching, the follow-up period was 2.98 years. The 30-day mortality was similar between two groups (18.4% vs. 15.9%, p = 0.207). Although the baseline comorbidities and acute medical problems before index hospitalization were similar in both groups after matching, vehicle-traumatic AKI-RRT patients had a longer length of stay in hospital [median IQR 15 (5–35) vs. 12 (5–28) days, p = 0.007). The long-term incidence of ESKD was similar between groups (10.6% vs. 13.4%, p = 0.832) (Table 1).
The risk of developing ESKD (HR, 1.166, p = 0.377) and 30-day mortality after discharge (HR, 1.134, p = 0.301) among the vehicle-traumatic AKI-RRT patients relative to non-traumatic AKI-RRT were similar. However, vehicle-traumatic AKI-RRT patients had a lower risk of long-term mortality than non-traumatic group (adjust HR: 0.473, p < 0.001) (Table 2). In addition, vehicle-traumatic AKI-RRT patients was associated with lower ESKD rates (HR, 0.552; 95% CI, 0.325–0.937; p = 0.028) than non-traumatic AKI-RRT patients in multivariable competing risk models which set death as a competing risk. Furthermore, this lower mortality rate after vehicle-traumatic AKI-RRT persisted after adjusting for age, gender and Charlson score Cox proportional analysis (p < 0.001) (Fig. 3).
Table 2.
Incidence and risks for outcome of interest in AKI patients with renal replacement therapy during hospitalization, between vehicle-traumatic patients and their matches.
| Incidence | Crude | Adjust* | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Events | Person-years | Incidence rate per 1000 person-years | Events | Person-years | Incidence rate per 1000 person-years | Hazard ratio (95% CI) |
p | Hazard ratio (95% CI) |
p | |
| Trauma | Non-trauma | Trauma vs. non-trauma | ||||||||
| Long-term ESKD | 45 | 3614.99 | 12.45 | 132 | 11068.44 | 11.93 |
1.039 (0.741–1.457) |
0.825 |
1.166 (0.829–1.638) |
0.377 |
| 30-day mortality | 95 | 36.94 | 2571.74 | 248 | 111.68 | 2220.63 |
1.154 (0.911–1.462) |
0.234 |
1.134 (0.894–1.438) |
0.301 |
| Long-term mortality | 129 | 2453.31 | 52.58 | 769 | 5946.12 | 129.33 |
0.434 (0.360–0.523) |
< 0.001 |
0.473 (0.392–0.571) |
< 0.001 |
ESKD, end-stage kidney disease; CI, confidence interval.
*The multivariable Cox regression model selected covariates from all variables in Table 1 and cardiogenic shock and exposure to nephrotoxic medications by a stepwise procedure.
After stratified vehicle-traumatic AKI-RRT patients by injured body part (Supplemental Table 2), the risk of developing ESKD and 30-day mortality after discharge among the vehicle-traumatic AKI-RRT patients relative to non-traumatic AKI-RRT were similar except for soft tissue injury from trauma which had lower incidence of 30-day mortality (HR, 0.714, p = 0.003). Bones (adjust HR: 0.580, p < 0.001) and abdomen injury (adjust HR: 0.607, p < 0.001) from trauma had lower risk of long-term mortality than non-traumatic group.
After stratified AKI-RRT patients by age (Supplemental Table 3), vehicle-traumatic AKI-RRT patients had lower risk of long-term mortality in elder (adjust HR: 0.793, p = 0.042) and younger (adjust HR: 0.580, p < 0.001) subgroup than non-trauma cohorts. However, vehicle-traumatic AKI-RRT patients had higher incidence of 30-day mortality in the elder subgroup (adjust HR: 1.441, p = 0.016).
Discussion
Our study is, to our knowledge, the first to describe the short-term and long-term outcomes of vehicle-traumatic AKI-RRT patients from a large national database. Our study demonstrated that vehicle-traumatic AKI-RRT patients had lower long-term mortality than non-traumatic AKI-RRT patients. However, incident ESKD and short-term mortality were similar between vehicle-traumatic and non-traumatic AKI-RRT patients.
The trend of vehicle-traumatic AKI-RRT
In an observational study in the United States, the incidence of AKI-RRT increased at an average of 10% per year from 2000 to 20099. In the NHIRD, we found that the proportions of patients with AKI-RRT among vehicle-traumatic patients also increased throughout the years. The older the patients, the higher annual number of trauma cases was found; however, the oldest vehicle-traumatic group had the lowest incidence of AKI-RRT (Fig. 2). These results may indicate that young people had higher severity of trauma and the consequent risk of AKI-RRT. There seemed to be no difference in body distribution of injury on the incident vehicle-traumatic AKI-RRT except for the lowest incidence of soft tissue injury related AKI-RRT.
ESKD and long-term mortality in patients with vehicle-traumatic AKI-RRT
AKI in traumatic patients is a common complication and associated with significantly higher 30-day and 1-year mortality than traumatic patients without AKI12. Although trauma-related risk factors for kidney injury (e.g., direct lesions to the kidneys, shock, ischemia–reperfusion, rhabdomyolysis, exposure to nephrotoxic substances, abdominal compartment syndrome, hemorrhagic shock and sepsis), The rate of long term incident ESKD in patients after AKI-RRT in our study did not significantly differ vehicle-trauma and non-trauma populations. However, compared to non-traumatic AKI-RRT patients, traumatic patients had lower risk of long-term mortality after survival in our cohort. The above results may indicate that the etiology of AKI-RRT may be associated with long-term mortality. On the other hand, the risk of ESKD existed if renal damage happened regardless of trauma or non-trauma. If we consider death as a competing risk, vehicle-traumatic AKI-RRT patients were associated with lower ESKD rates than non-traumatic AKI-RRT patients, which may indicate that vehicle-traumatic AKI-RRT patients had better renal recovery potential. In addition, the vehicle-traumatic AKI-RRT patients with soft tissue injuries may have lower severity trauma which may contribute to better 30-day mortality.
The observed decreased long-term mortality and long-term ESKD in vehicle-traumatic AKI-RRT patients after 30 days can be related to the overall better health status of these patients before the traumatic injury and that perhaps a greater burden of co-morbidity and complications in the more non-traumatic AKI-RRT population with greater baseline debility. This cannot be fully addressed with propensity score-matching involving cross-sectional comorbidity data at the time of or before index admission.
One of the few other studies examining long term-outcomes after traumatic AKI examined 40 soldiers who survived traumatic AKI-RRT in that study there was a lower incidence of ESKD (2.5% vs. 10.6%) and a lower long-term mortality (2.5% vs. 25%) rate over a median follow-up of 2.7 years than in our cohort14. These differences might be attributed to low incidence rates, younger age (26 ± 6 years), and fewer baseline comorbidities in the military study14.
The management of vehicle-traumatic AKI
Management of AKI should be considered in the context of the underlying etiology; for instance, sepsis-associated AKI will focus on source control of infection hemodynamic support and secondary injury prevention15, while nephrotoxic will focus on identification removal of the offending agent16.
However, the management of traumatic AKI is complicated because it commonly involves multiple risk factors for AKI, including direct traumatic injury to the kidneys, hypovolemic shock, ischemia–reperfusion injury, exposure to endogenous and exogenous nephrotoxic substances, and secondary infection. Accordingly an understanding of the underlying cause of traumatic AKI is required to enable its optimal management. In addition, we have demonstrated that that traumatic AKI-RRT patients had lower long-term rates of death or ESKD in competing risk analsysis compared to non-traumatic AKI-RRT patients; this might indicate that severe traumatic AKI has a generally good prognosis justifying aggressive treatment including the use of RRT where indicated.
Follow-up strategy in patients of AKI-RRT
AKI-RRT has been shown to be associated with an increased incidence of ESKD, mortality17, coronary events13, stroke18, and bone fracture19 among those who survived to hospital discharge. Although guidelines published by kidney disease: improving global outcomes (KDIGO) Clinical Practice Guideline recommend that survivors of AKI be followed up by a nephrologist within 90 days20, reports in the literature suggest only a small proportion of patients after severe AKI are followed-up by a nephrologist after survival discharge21–23. Given their young age, relative lack or comorbidity, and still significant risk of developing ESKD, AKI-RRT is a neglected population where focused medical follow-up could address the progression of CKD and development of other complications over a long expected lifespan. These results further provide the outcome information for patient care and rational health resource allocation.
Limitation
Our study has certain limitations. Firstly, as all observational studies, we could not exclude the possibility of residual confounding. To decrease the effect of potential confounding factors, we developed a 3:1 propensity score. We were able to construct a comparison cohort with balanced covariates between the two groups. Second, with some administrative databases, detailed in-hospital parameters, and laboratory results were not available in our cohort. Therefore, we could not examine whether classifying patients into different severity scoring systems, such as the Injury Severity Score (ISS) and Acute Physiology and Chronic Health Evaluation score. The severity of trauma and illness has been found to be associated with AKI8,24, and thus could be potential predictors of clinical outcome. To attenuate the effect of the limitations, we did adjust by Charlson comorbidity index (pre-admission comorbidities) and in-hospital acute comorbidities, including pulmonary and hemodynamic complications, to evaluate the disease severity of each patient in our database. We further stratify our trauma patients based upon injured body regions as proxies to evaluate the traumatic severity. Third, we did not analyze the effect of duration and modality of RRT which may be the predictors of disease severity and the confounding factors of long-term outcomes in our study. To attenuate the effect of the limitations, we did adjust by Charlson comorbidity index (pre-admission comorbidities) and in-hospital acute comorbidities, including pulmonary and hemodynamic complications, to evaluate the disease severity of each patient in our database.
Conclusion
In our study, we found that the vehicle-traumatic AKI-RRT patients had better long-term survival than non-traumatic counterparts with AKI-RRT. However, there were similar outcomes of ESKD and short-term mortality. Our findings are pertinent to civilian populations with similar demographics and may inform care in real-world practice.
Methods
Study design and setting
National Health Insurance registration database (NHIRD)
The Taiwan National Health Insurance (NHI) program is mandatory and universal, offering comprehensive medical care coverage to more than 99% of the country’s population of 23 million people. This nationwide compulsory healthcare program that covers outpatient visits, hospital admissions, prescriptions, interventional procedures, disease profiles, and vital statuses. Taiwan’s NHI records are regularly inspected, and physicians are subject to statutory regulation13,19,25–28. The National Health Insurance Research Database (NHIRD) thus represents a comprehensive, high-quality record of healthcare episodes provided to the Taiwanese population.
Selection of participants
We enrolled patients aged ≥ 18 years who were admitted because of major trauma and developed AKI-RRT during their index admission as recognized by RRT-related procedure codes and survived to hospital discharge. All diagnoses, including trauma-related injuries and baseline comorbidities, were obtained by the codes of International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM). Those that were related to vehicle-related accidents, defined as any of ICD-9-CM E-Code E800 to E844 included in the diagnosis codes, were aggregated to individuals and were enrolled as study subjects25. When more than one accident was encountered by a single person, only the first event was counted for analysis. We identified baseline comorbidities from at least three outpatient visits or one inpatient claim within a one-year antecedent to the index admission with first dialysis. This rule was constructed based on a relatively strict criterion and was well validated with good predictive power13,19,25,26,29.
Dialysis patients who underwent renal transplantation, vascular access creation, or peritoneal-dialysis catheter implantation for chronic dialysis and those who had received chronic dialysis prior to the index admissions were excluded. To compare the long-term outcomes of interest, we constructed a comparator group of non-traumatic AKI-RRT patients matched to vehicle-traumatic AKI-RRT patients in a 3:1 ratio based on age, gender, and propensity scores. (Supplemental Table 4).
As all personal information is de-identified in the research database to protect privacy, no informed consent was required, and this study was deemed exempt from a full ethical review by the institutional review board of the National Taiwan University Hospital (201212021RINC).
Outcomes
Our primary outcome was long-term all-cause mortality after hospital discharge. The secondary outcomes were 30-day all-cause mortality and de novo end-stage kidney disease (ESKD) defined as the requirement of dialysis for at least three months after hospital discharge. We used a selection period of 90 days to define ESKD because all patients receiving dialysis for more than 90 days in Taiwan can apply to the NHI for catastrophic illness registration cards30. Each patient was monitored from the date of discharge and was censored at either death, dialysis, or the end of the study (December 31, 2010), whichever occurred first.
We also stratified trauma patients by injured body part and age to evaluate the outcomes comparing to their matches in the subgroup analysis.
Research variables
We recorded the disease severity and patient condition during index hospitalization. Disease severity and patient condition are estimated by the ICU procedure and complications with acute pulmonary [prolonged mechanical ventilation (the use of mechanical ventilation ≥ 21 days), re-intubation, acute respiratory distress syndrome, pleural effusion, and chest tube insertion], cardiovascular [hemopericardium, hypovolemic shock, cardiac arrest, heart block, atrial fibrillation, extracorporeal membrane oxygenation (ECMO) and intra-aortic balloon pumping (IABP)] and infectious (pneumonia, urinary tract infection and severe sepsis) and other (delirium, stroke and gastrointestinal bleeding) disorders31.
The Charlson comorbidity index32 was computed using baseline comorbidities. Additional adjustments in these models included control for direct effects from age, gender, and comorbidities that are listed in Table 1.
Analysis
Baseline characteristics were described as the percentages for categorical variables and median with interquartile range (IQR) for continuous variables. Differences between the trauma and non-trauma related groups were compared by the independent t-test or χ2 test where appropriate.
To estimate each patient’s propensity score for vehicle-traumatic AKI-RRT, we fitted a separate multivariable logistic regression model with the factors predicting vehicle trauma as admitting diagnosis in patients with AKI-RRT during index hospitalization33 (further seen in Supplemental Table 4). The caliper distance is 0.25 and subjects are matched without replacement in this propensity score matching. The estimated propensity score was also added to adjusting the Cox regression model as a single covariate for controlling selection bias. Multivariable logistic regression models before and after propensity-scored matching were applied to estimate odds ratio (OR) of study outcomes after adjusting all the confounders predicting trauma (Supplemental Table 4).
We evaluated the association of vehicle-traumatic AKI-RRT with the risks of long-term ESKD, 30-day mortality and long-term mortality among our cohort using Cox regression models with time-dependent covariates. To assess multivariate Cox regression models in mortality and ESKD analysis, the relationship between scaled Schoenfeld residuals and time was examined, with no significant evidence for non-proportionality (p value > 0.05), therefore we accepted the assumption in the Cox model of constant hazard ratios over time.
The significance levels for entry and stay were set to 0.15 to be conservative. Then, with the aid of substantive knowledge, the best candidate final logistic model was identified manually by dropping the covariates with p value > 0.05 one at a time until all regression coefficients were significantly different from 0.
All the analyses were conducted with R software, version 2.8.1 (Free Software Foundation, Inc., Boston, MA, USA); competing-risk analysis was performed using Stata/MP version 12 (Stata Corporation). A two-sided p-value < 0.05 was considered to be statistically significant.
Supplementary information
Acknowledgments
The study was partly based on data provided by the National Health Insurance Administration, Ministry of Health and Welfare, Taiwan. The interpretation and conclusions shown in this paper do not represent those of the National Health Insurance Administration, Ministry of Health and Welfare, National Health Research Institutes, or National Taiwan University Hospital. We also express our sincere gratitude to all staff of the Taiwan Clinical Trial Consortium, TCTC.
Author contributions
N.-K.C. and Y.-P.H. prepared the data, V.-C.W. analysed the data, C.-K.C. wrote the manuscript. J.R.P. and V.-C.W. supervised. C.-Y.C., T.-S.L., Y.-P.H. and Y.-M.C. collected and analyzed the data. All authors reviewed the manuscript.
Funding
This study was supported by Ministry of Science and Technology (MOST) of the Republic of China (Taiwan) [Grant Number, MOST 106-2321-B-182-002, MOST 108-2314-B-002-058, 109-2314-B-002-174-MY3].
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
John R. Prowle, Email: j.prowle@qmul.ac.uk
Vin-Cent Wu, Email: q91421028@ntu.edu.tw.
Supplementary information
is available for this paper at 10.1038/s41598-020-77556-3.
References
- 1.Shiao CC, et al. Long-term remote organ consequences following acute kidney injury. Crit. Care. 2015;19:438. doi: 10.1186/s13054-015-1149-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doyle JF, Forni LG. Acute kidney injury: short-term and long-term effects. Crit. Care. 2016;20:188. doi: 10.1186/s13054-016-1353-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brown JR, Rezaee ME, Marshall EJ, Matheny ME. Hospital mortality in the United States following Acute Kidney Injury. Biomed. Res. Int. 2016;2016:4278579. doi: 10.1155/2016/4278579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uchino S, et al. Acute renal failure in critically ill patients: a multinational, multicenter study. JAMA J. Am. Med. Assoc. 2005;294:813–818. doi: 10.1001/jama.294.7.813. [DOI] [PubMed] [Google Scholar]
- 5.Chang CH, et al. Acute kidney injury enhances outcome prediction ability of sequential organ failure assessment score in critically ill patients. PLoS ONE. 2014;9:e109649. doi: 10.1371/journal.pone.0109649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Podoll AS, Kozar R, Holcomb JB, Finkel KW. Incidence and outcome of early acute kidney injury in critically-ill trauma patients. PLoS ONE. 2013;8:e77376. doi: 10.1371/journal.pone.0077376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shashaty MG, et al. African American race, obesity, and blood product transfusion are risk factors for acute kidney injury in critically ill trauma patients. J. Crit. Care. 2012;27:496–504. doi: 10.1016/j.jcrc.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Skinner DL, Hardcastle TC, Rodseth RN, Muckart DJ. The incidence and outcomes of acute kidney injury amongst patients admitted to a level I trauma unit. Injury. 2014;45:259–264. doi: 10.1016/j.injury.2013.07.013. [DOI] [PubMed] [Google Scholar]
- 9.Hsu RK, McCulloch CE, Dudley RA, Lo LJ, Hsu CY. Temporal changes in incidence of dialysis-requiring AKI. J. Am. Soc. Nephrol. JASN. 2013;24:37–42. doi: 10.1681/ASN.2012080800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Haines RW, et al. Acute kidney injury in trauma patients admitted to critical care: development and validation of a diagnostic prediction model. Sci. Rep. 2018;8:3665. doi: 10.1038/s41598-018-21929-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haines RW, Fowler AJ, Kirwan CJ, Prowle JR. The incidence and associations of acute kidney injury in trauma patients admitted to critical care: a systematic review and meta-analysis. J. Trauma Acute Care Surg. 2018 doi: 10.1097/ta.0000000000002085. [DOI] [PubMed] [Google Scholar]
- 12.Eriksson M, Brattstrom O, Martensson J, Larsson E, Oldner A. Acute kidney injury following severe trauma: Risk factors and long-term outcome. J. Trauma Acute Care Surg. 2015;79:407–412. doi: 10.1097/ta.0000000000000727. [DOI] [PubMed] [Google Scholar]
- 13.Wu VC, et al. Long-term risk of coronary events after AKI. J. Am. Soc. Nephrol. JASN. 2014;25:595–605. doi: 10.1681/ASN.2013060610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bolanos JA, et al. Outcomes after post-traumatic AKI requiring RRT in United States military service members. Clin. J. Am. Soc. Nephrol. 2015;10:1732–1739. doi: 10.2215/CJN.00890115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Prowle JR. Sepsis-associated AKI. Clin. J. Am. Soc. Nephrol. 2018;13:339–342. doi: 10.2215/cjn.07310717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guo, X. & Nzerue, C. How to prevent, recognize, and treat drug-induced nephrotoxicity. Clevel. Clin. J. Med. 69, 289–290, 293–284, 296–287 passim, 10.3949/ccjm.69.4.289 (2002). [DOI] [PubMed]
- 17.Wu VC, et al. Long-term outcomes after dialysis-requiring acute kidney injury. Biomed. Res. Int. 2014;2014:365186. doi: 10.1155/2014/365186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wu VC, et al. The impact of acute kidney injury on the long-term risk of stroke. J. Am. Heart Assoc. 2014;3:e000933. doi: 10.1161/JAHA.114.000933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang WJ, et al. The impact of acute kidney injury with temporary dialysis on the risk of fracture. J. Bone Miner. Res. Off. J. Am. Soc. Bone Miner. Res. 2013;29:676–684. doi: 10.1002/jbmr.2061. [DOI] [PubMed] [Google Scholar]
- 20.KDIGO KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2012;4:1–138. [Google Scholar]
- 21.Karsanji DJ, et al. Disparity between nephrologists' opinions and contemporary practices for community follow-up after AKI hospitalization. Clin. J. Am. Soc. Nephrol. 2017 doi: 10.2215/CJN.01450217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pan HC, et al. A nationwide survey of clinical characteristics, management, and outcomes of acute kidney injury (AKI)—patients with and without preexisting chronic kidney disease have different prognoses. Medicine (Baltimore) 2016;95:e4987. doi: 10.1097/MD.0000000000004987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siew ED, et al. Outpatient nephrology referral rates after acute kidney injury. J. Am. Soc. Nephrol. JASN. 2012;23:305–312. doi: 10.1681/ASN.2011030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bihorac A, et al. Incidence, clinical predictors, genomics, and outcome of acute kidney injury among trauma patients. Ann. Surg. 2010;252:158–165. doi: 10.1097/SLA.0b013e3181deb6bc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wu CS, Lai MS, Gau SS, Wang SC, Tsai HJ. Concordance between patient self-reports and claims data on clinical diagnoses, medication use, and health system utilization in Taiwan. PLoS ONE. 2014;9:e112257. doi: 10.1371/journal.pone.0112257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheng CL, Kao YH, Lin SJ, Lee CH, Lai ML. Validation of the national health insurance research database with ischemic stroke cases in Taiwan. Pharmacoepidemiol. Drug Saf. 2011;20:236–242. doi: 10.1002/pds.2087. [DOI] [PubMed] [Google Scholar]
- 27.Lin CC, Lai MS, Syu CY, Chang SC, Tseng FY. Accuracy of diabetes diagnosis in health insurance claims data in Taiwan. J. Formos Med. Assoc. 2005;104:157–163. [PubMed] [Google Scholar]
- 28.Cheng CL, et al. Validation of acute myocardial infarction cases in the national health insurance research database in taiwan. J. Epidemiol. 2014;24:500–507. doi: 10.2188/jea.JE20140076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chu YT, Wu SC, Lee YC, Lai MS, Tam SC. Assessing measures of comorbidity using National Health Insurance Databases. Taiwan J. Public Health. 2010;29:191–200. [Google Scholar]
- 30.Lin YF, et al. The 90-day mortality and the subsequent renal recovery in critically ill surgical patients requiring acute renal replacement therapy. Am. J. Surg. 2009;198:325–332. doi: 10.1016/j.amjsurg.2008.10.021. [DOI] [PubMed] [Google Scholar]
- 31.van Diepen S, Graham MM, Nagendran J, Norris CM. Predicting cardiovascular intensive care unit readmission after cardiac surgery: derivation and validation of the Alberta Provincial Project for Outcomes Assessment in Coronary Heart Disease (APPROACH) cardiovascular intensive care unit clinical prediction model from a registry cohort of 10,799 surgical cases. Crit. Care. 2014;18:651. doi: 10.1186/s13054-014-0651-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J.Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 33.Uchino S, et al. Diuretics and mortality in acute renal failure. Crit. Care Med. 2004;32:1669–1677. doi: 10.1097/01.ccm.0000132892.51063.2f. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


