Abstract
Objective
We aimed to conduct a systematic review of the available literature to determine the effects of confirmed cases of COVID-19 in pregnant women from the foetal perspective by estimation of mother to child transmission, perinatal outcome and possible teratogenicity.
Methods
Data sources: eligible studies between 1 November 2019 and 10 August 2020 were retrieved from PubMed, Embase, LitCovid, Google Scholar, EBSCO MEDLINE, CENTRAL, CINAHL, MedRXiv, BioRXiv and Scopus collection databases. English language case reports, case series and cohort studies of SARS-CoV-2 confirmed pregnant women with data on perinatal outcome, congenital anomalies and mother to child transmission were analysed.
Results
38 case reports, 34 cohort and case series describing 1408 neonates were included for evidence acquisition of mother to child transmission. 29 case reports and 31 case series and cohort studies describing 1318 foetuses were included for the evaluation of perinatal outcome and congenital anomalies. A pooled proportion of 3.67% neonates had positive SARS-CoV-2 viral RNA nasopharyngeal swab results and 7.1% had positive cord blood samples. 11.7% of the placenta, 6.8% of amniotic fluid, 9.6% of faecal and rectal swabs and none of the urine samples were positive. The rate of preterm labour was 26.4% (OR=1.45, 95% CI 1.03 to 2.03 with p=0.03) and caesarean delivery (CS) was 59.9% (OR=1.54, 95% CI 1.17 to 2.03 with p=0.002). The most common neonatal symptom was breathing difficulty (1.79%). Stillbirth rate was 9.9 per 1000 total births in babies born to COVID-19 mothers.
Conclusion
Chances of mother to child transmission of the SARS-CoV-2 virus is low. The perinatal outcome for the foetus is favourable. There is increased chances of CS but not preterm delivery. The stillbirth and neonatal death rates are low. There are no reported congenital anomalies in babies born to SARS CoV-2 positive mothers.
Keywords: data collection, microbiology, mortality, neonatology, virology
Key message.
What is known about the subject?
Studies specifically analysing all aspects of the foetus in SARS-CoV-2 positive mothers are not currently available. There are some systematic reviews reporting maternal outcomes, vertical transmission and neonatal outcomes involving a lesser number of pregnancies separately but aspects like foetal complications and teratogenicity are not adequately reported.
What this study adds?
The confirmed congenital transmission rate was found to be 9/1408 (0.63%). The risk of caesarean delivery is significantly higher in SARS-CoV-2 positive mothers but there is no significantly higher risk of prematurity. There is evidence of foetal distress, and neonatal respiratory symptoms in COVID-19 mothers but stillbirth is low.
Introduction
Novel coronavirus infection and associated coronavirus disease-2019 (COVID-19) pandemic has changed our lives forever and has compelled us to reconsider almost everything we have long taken for granted. Among the different coronaviruses severely affecting human species, Middle East respiratory syndrome coronavirus (MERS-CoV), severe acute respiratory syndrome coronavirus (SARS-CoV) and SARS-CoV-2 are significant, causing MERS, SARS and COVID-19, respectively. SARS-CoV-2 strains show significant sequence homology to SARS-CoV and MERS-CoV.1 As the pandemic evolved, there were significant advances in our knowledge about various aspects of the COVID-19 including epidemiology, clinical features, transmission, detection and management modalities. Discoveries along the process of evolution are still contributing to our management practices.
There were concerns regarding the maternal and foetal effects since the beginning of the pandemic. The earlier evidence of COVID-19 in pregnancy pointed towards pregnancy being considered as low risk for the disease and no difference in disease behaviour in pregnant and non-pregnant women was reported.2 On the contrary, a newer study involving pooled data from more than 8000 women in the USA pointed towards a significantly higher rate of intensive care unit (ICU) admission (adjusted relative risk (aRR)=1.5) and need for mechanical ventilation (aRR=1.7) in pregnant women as compared with non-pregnant women, even when adjusted for race/ethnicity and underlying comorbid conditions.3 Similar findings were reported from other studies from the USA and Sweden.4–6
However, these studies did not specify adequately foetal effects resulting from congenital or neonatal infection in SARS-CoV-2 positive mothers and consequent perinatal outcomes. Evidence of COVID-19 specifically focusing on foetal and neonatal outcomes are lacking. Most of the reported literature have smaller studies. Previous systematic reviews focusing on the outcomes of all coronaviruses have reported a higher risk of pre-eclampsia, preterm birth, miscarriage and perinatal death.
Through this article, we want to analyse the published evidence on the foetal perspective of COVID-19 infection concerning mother to child transmission (congenital or neonatal infection) and perinatal outcome through a systematic review. This will aid in alleviating uncertainties faced while doing patient counselling and help in subsequent management during these testing times.
Methods
Search strategy
A systematic search of PubMed, Embase, LitCovid, MedRxiv, BioRxiv, Google Scholar, EBSCO MEDLINE, CINAHL and Scopus electronic database was done. Medical subject handling terms (MeSH) and free-text term keywords like vertical transmission, perinatal outcome, foetal, neonate, newborn, pregnancy were used in combination with COVID-19, 2019-nCoV, SARS-CoV-2 to search for data from 1st November 2019 till 10th July 2020. Thereafter manual update was done on weekly basis till 10th August 2020. The references of relevant studies were also searched.
The keywords detail and full search strategy used in each of PubMed, Embase, LitCovid, MedRxiv, BioRxiv, Google Scholar, EBSCO MEDLINE, CINAHL and Scopus electronic database are as follows: both medical subject headings (MeSH) and keywords: “2019 novel coronavirus infection” OR “COVID-19” OR “COVID19” OR "coronavirus disease 2019” OR “nCoV infection” OR “2019-nCoV” OR “2019 novel coronavirus” OR “2019 coronavirus” OR “novel coronavirus” OR (2019 AND coronavirus) OR “SARS CoV-2” OR “SARS CoV2” AND “vertical transmission” OR “foetal outcome” OR “perinatal outcome” OR “neonatal outcome” OR “pregnancy” OR “congenital infection” OR “mother-to-child transmission” OR “(transmission AND vertical)” OR “(transmission AND fetomaternal)” OR “teratogenicity”.
Selection criteria
The search consisted of only English language articles (original English articles and other language articles with available English translation) including case reports, case series and letters to editors containing case information. After a thorough screening, no randomised clinical trials were found.
Inclusion criteria
The studies fulfilling all of the following criteria (1, 2 and 3) were included for review.
Studies reporting pregnant women with confirmed COVID-19 who had delivered.
Studies containing the results of the SARS-CoV-2 test (including reverse transcriptase-Polymerase Chain Reaction (RT-PCR) and serological tests) in both mother and newborn samples.
Studies that present the out-come of vertical transmission or congenital transmission or neonatal transmission or the perinatal outcome or congenital anomaly.
Exclusion criteria
Exclusions consisted of studies in pregnant women yet to deliver, duplicated studies, review articles, articles in languages other than English where translation was not possible, studies where infection in mothers is not confirmed, or where neonatal testing was not done. Conference abstracts, expert opinions and critical appraisals were also excluded.
Both the authors (RD, SSK) reviewed all titles independently. The potential relevance of the studies to be included for review were agreed on by discussion. Selected titles and abstracts were further screened between studies to reject overlap of cases.
Full-text copies of the selected papers were obtained and the relevant data regarding study characteristics, evidence of vertical transmission and perinatal outcomes were extracted by the same two reviewers independently. In the case of individual case reports, if the same patient was included in more than one study with similar characteristics and findings, only the report with a larger number of patients was included. As far as possible, single case reports were cross-checked with other reports from the same location and hospital. If a case series included multiple locations, the individual reports from the same centres were excluded. Similarly, if the time-frame of the reported cases matched from the same centre, the characteristics were compared to decide regarding the inclusion or exclusion from the study. Finally, studies were screened by assessing selection, comparability and exposure for inclusion into evidence acquisition of mother to child transmission (congenital or neonatal transmission) and/or perinatal outcome measures (online supplementary tables 1A, B).
bmjpo-2020-000859supp001.pdf (150KB, pdf)
Study outcomes
Mother to child transmission
Evidence of mother to child transmission (congenital or neonatal transmission) is indicated by positive RT-PCR status in different samples like the neonatal nasopharyngeal swab, cord blood, amniotic fluid, breast milk and placental tissue. Transmission of infection from mother to foetus generally includes transmission through germ cells or the placenta during pregnancy, via the birth canal during labour and delivery, and the postpartum period through breast feeding or close contact. The transfer of micro-organisms during pregnancy is seen with many of the common pathogens with resultant effects ranging from asymptomatic infection, intrauterine growth restriction (IUGR), intrauterine death and structural anomalies as a sequel of infection. Some pathogens like cytomegalovirus or Zika virus produce mild to no symptoms in the pregnant patient but can cause congenital infection with severe consequences.7 Viruses specifically can be transmitted to the foetus via the maternal blood when it enters the placental villus, containing the foetal blood vessels or by direct access to the placenta from the lower genital tract by ascending infection.8 Again even when transferred trans-placentally during the antenatal period, the specific timing of maternal infection can have different effects on the foetus. The first-trimester infection can cause severe structural anomalies whereas second and third-trimester infections are more likely to cause functional organ abnormalities.9
Several factors are contributing to the concerns of mother to child transmission in COVID-19. It is known that the SARS-CoV-2 uses Angiotensin converting enzyme-2 (ACE-2) receptors for entry into the cells. ACE-2 receptors are detected in various parts of the uterus, vagina, decidual cells and placenta.10–13 Recently, the case definition for SARS‐CoV‐2 infection in pregnant women, foetuses and neonates has been published with a categorisation of infection into confirmed, probable, possible, unlikely and not infected groups.14
Congenital infection with intrauterine foetal death (IUFD)/stillbirth is14:
Confirmed from foetal tissue or autopsy material if the virus is detected by PCR from foetal or placental tissue or electron microscopic detection of the viral particle in tissue or viral growth in culture from foetal or placental tissue.
A probable infection if the virus is detected by PCR in the surface swab from the foetus or placental swab on the foetal side.
Unlikely if it is positive in the maternal side of the placenta but foetal tissues are not tested and not present if it is not detected in foetal tissue in an autopsy.
Similarly, congenital infection in live-born symptomatic neonate is14:
Confirmed when the virus is detected by PCR in umbilical cord blood or neonatal blood collected within the first 12 hours of birth or amniotic fluid collected prior to the rupture of the membrane.
A probable infection when there is the detection of the virus by PCR in nasopharyngeal swab at birth (collected after cleaning baby) AND placental swab from the foetal side of the placenta in a neonate born via caesarean section (CS) before rupture of membrane or placental tissue.
Possible when there are anti-SARS-CoV-2 IgM antibodies in umbilical cord blood or neonatal blood collected within the first 12 hours of birth or placental tissue but nasopharyngeal swab test at birth is negative.
Unlikely or absent when samples are negative within 12 hours of birth (nasopharyngeal swab, umbilical cord blood or neonatal blood) and antibody testing is not done or negative, respectively.
If a live-born neonate has no clinical features of infection, congenital infection is14:
Confirmed by detection of the virus by PCR in cord blood or neonatal blood collected within the first 12 hours of birth.
Probable if the virus is detected by PCR in amniotic fluid collected prior to rupture of the membrane but no detection in umbilical cord blood or neonatal blood collected within the first 12 hours of birth.
Possible when there is anti-SARS-CoV-2 IgM in umbilical cord blood or detection of the virus by PCR in placental tissue but PCR in umbilical cord blood, amniotic fluid and neonatal blood (<12 hours of life) is negative.
Furthermore, infection acquired intrapartum in a symptomatic neonate is confirmed if the virus is detected by PCR in nasopharyngeal swab at birth (collected after cleaning the baby) AND at 24–48 hours of age AND alternate explanation for clinical features excluded.14
Intrapartum neonatal infection in asymptomatic neonate is confirmed by detection of the virus by PCR in nasopharyngeal swab at birth (collected after cleaning the baby) AND at 24–48 hours of age.14
Postpartum infection is confirmed if a neonate shows symptoms beyond 48 hours of life and the nasopharyngeal swab is positive beyond 48 hours which was negative at birth.14
If a neonate is born with a specific structural sequel of an infection, intrauterine infection is a probability. The probability of infection also depends on the presence of the agent in the genital tract and time taken from exposure to detection by definitive tests to differentiate between intrapartum and postpartum infection. Furthermore, the sensitivity of RT-PCR testing is different for detecting SARS-CoV-2 in different samples. Therefore, it is rational to test samples from multiple sites to improve detection and reduce false-negative cases.9 15
Perinatal outcome
Perinatal outcome measures included foetal outcomes like foetal complications in SARS-CoV-2 positive pregnant women, gestational age at delivery (preterm delivery), mode of delivery, birth weight and stillbirth. The neonatal period is defined as the time period from birth until the end of the first 28 days of life. Events in the early neonatal period (first 7 days) usually are related to the pregnancy more significantly and it is also included in the definition of the perinatal period. In this review, we have assessed the neonatal outcomes using the APGAR score at 1 min and 5 min of life, neonatal symptoms, admission into neonatal ICU, and neonatal death, as the parameters. An APGAR score of less than 7 at 1 min and 5 min after birth in a newborn is defined as a low APGAR score in this study.16 Any outcome measures not explicitly mentioned were considered not to have been reported.
Foetal distress (FD) is assessed during labour by non-reassuring or pathological cardiotocographic (CTG) findings and meconium-stained amniotic fluid.17 18 For this research, studies reporting FD, abnormal or non-reassuring or pathological CTG, foetal compromise, meconium-stained amniotic fluid are included under FD. Other foetal complications were prelabour rupture of membranes and preterm prelabour rupture of membranes.
Preterm delivery is defined as delivery of a viable product of conception before 37 completed weeks of gestation.
Delivery can be vaginal delivery (including instrumental) and by CS. For this research, instrumental vaginal deliveries (VDs) and normal VDs were considered together.
Both the Royal College of Obstetrics and Gynecology and the American College of Obstetricians and Gynecologists have adopted the definition of IUGR as an estimated foetal weight less than 10 percentile. The term IUGR has been used interchangeably with small for gestational age (SGA). SGA is a term commonly used for a neonate with birth weight less than 10th centile.19 20
For this research, stillbirth was considered as foetal death beyond 24 weeks of gestation, and stillbirth rate (SBR) is calculated as the number of stillbirths per 1000 total births.
Statistical analysis
Pooled proportions of categorical variables were calculated with percentage after obtaining the positive rates of each of the SARS-CoV-2 testing methods used, wherever applicable. Odds Ratio (OR) was calculated for the foetal outcome of preterm delivery and mode of delivery in the SARS-CoV-2 positive mothers from the pooled data (combining the studies where the control group of SARS-CoV-2 negative pregnant women was available) with 95% CI and p values. The percentage of the most common variables were also calculated.
Public and patient involvement statement
This research is not ‘coproduced’ with patients, carers or members of the public.
Results
Mother to child transmission
Search results
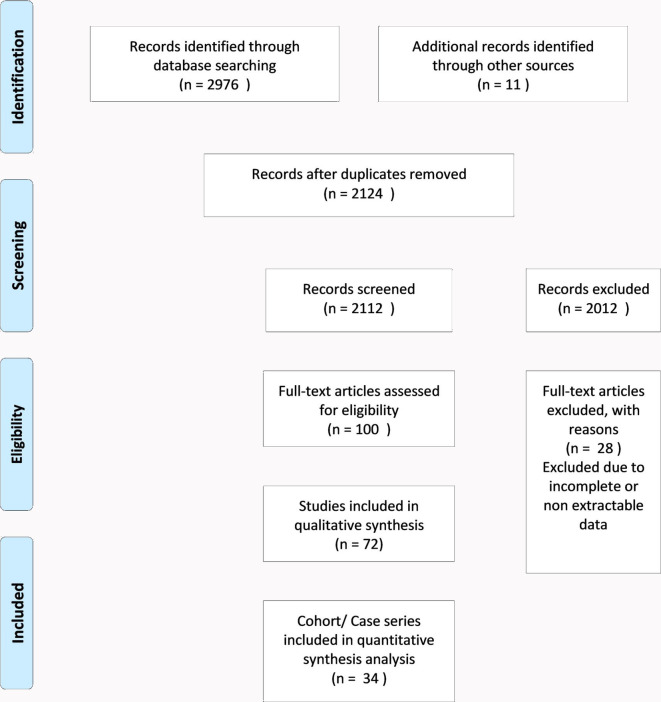
Out of 100 records selected for full-text review, 3 Chinese, 1 Italian, 1 Dutch and 1 Spanish studies were excluded due to non-availability of English translation. 72 studies fulfilled the eligibility criteria and were included in the qualitative synthesis. 38 studies were case reports containing 4 or fewer number of cases and 34 studies had 5 or more number of patients (figure 1).
Figure 1.
Image-PRISMA-1-Mother to child transmission.
Since evidence from randomised control trials were not available until the time of the search, 34 studies having 5 or more number of patients were considered for qualitative analysis.21 22 However, the findings from the case reports were also noted. The majority of earlier studies were from China but later studies contained cases from the rest of the world (online supplementary tables 1A, B).
Systematic review
Tests for diagnosis of SARS-CoV-2 were done in a total of 1408 neonates. The most common type of sample tested was neonatal nasopharyngeal samples (NP swab) (67 out of 72 studies) followed by the placenta, amniotic fluid and cord blood. In the majority, samples were taken from more than one site. In a few studies, the same type of sample was repeated at different intervals (eg, NP swab and breast milk samples) (table 1).
Table 1.
Studies and type of samples
| Serial number | Author (reference) | Number of neonates tested | Specimen tested | Results: neonatal and others | Positive/total tested |
| 1. | Chen et al 45 | 6 | NP, AF, cord blood, BM | Negative | |
| 2. | Cao et al 67 | 5 | NP | Negative | |
| 3. | Hu et al 42 | 7 | NP, urine, AF | NP +ve at 36 hours, others negative | 1/7 |
| 4. | Zhu et al 57 | 10 | NP | Negative(within 72 hours (8); between D7 and D9 (2)) | |
| 5. | Zhang et al 102 | 10 | NP | Negative | |
| 6. | Penfield C et al 103 | 11 | NP, placental and membrane | NP: negative (D1 and D5) Placenta and membrane +ve |
3/11 |
| 7. | Knight M et al 23 | 262 | NP (n=244), blood or aspirate | +ve at <12 hours +ve at >12 hours |
6/244 6/244 |
| 8. | Kayem G et al 25 | 181 | NP | +ve | 2/181 |
| 9. | Nayak A et al 26 | 134 | NP (n=131) | +ve on D1, −ve on D5 | 3/131 |
| 10. | Yan J et al 24 | 86 | NP (n=86); cord blood (n=10), AF (n=10) | Negative | |
| 11. | Khan S et al 64 | 17 | NP | +ve within 24 hours | 2/17 |
| 12. | Zeng L et al 41 | 33 | NP, anal swab | Both +ve D2 and D4, −ve on D6 | 3/33 |
| 13. | Breslin N et al 59 | 18 | NP | Negative | |
| 14. | Breslin N et al 114 | 7 | NP | Negative | |
| 15. | Qiancheng X et al 107 | 23 | NP | Negative | |
| 16. | Prabhu M et al 60 | 71 | NP | Negative at 24 hours | |
| 17. | Shanes E et al 36 | 16 | NP, placenta | Negative | |
| 18. | Savasi V et al 109 | 57 | NP | +ve | 4/57 |
| 19. | London V et al 27 | 48 | NP | Negative | |
| 20. | Pierce-Williams R et al 63 | 33 | NP | −ve at 24 hours, +ve at 48 hours | 1/33 |
| 21. | Martínez-Perez O et al 65 | 82 | NP | NP +ve at birth and negative at 48 hours (3); NP −ve at birth but +ve at D10 (2) | 5/82 |
| 22. | Nie R et al 68 | 26 | NP, Cord blood, Placenta | NP +ve at 36 hours, negative: all other samples, NP (D4, D8, D15) | 1/26 |
| 23. | Yin M et al 46 | 17 | NP (n=17), BM (n=14), AF (n=2), placenta (n=2), anal swab (n=5) | Negative | |
| 24. | Yang P et al 81 | 7 | NP, cord blood, AF | Negative | |
| 25. | Yang H et al 73 | 55 | NP | Negative | |
| 26. | Wu Y et al 47 | 5 | NP, anal swab, BM | Negative, BM +ve | 1/5 |
| 27. | Patane L et al 39 | 22 | NP, placenta | NP +ve, placenta- chronic intervillitis, PCR +ve in placenta | 2/22 |
| 28. | Ferrazzi E et al 28 | 42 | NP | NP +ve on D1, D3 (2) NP equivocal at birth but +ve on D3 (1) |
3/42 |
| 29. | Govind A et al 61 | 9 | NP, placenta, AF | NP +ve | 1/9 |
| 30. | Vintzileos W et al 113 | 29 | NP | Negative | |
| 31. | Baergen R et al 37 | 21 | NP | Negative | |
| 32. | Zeng H et al 54 | 6 | NP neonatal blood |
NP negative; elevated IgM and IgG (2); Elevated IgG, normal IgM (3) |
Cytokine IL-6 elevated in all infants |
| 33. | Liu Y et al 69 | 10 | Foetal blood | Negative | |
| 34. | Mulvey J et al 38 | 5 | Placenta | Negative | |
| 35. | Hantoushzadeh et al 75 | 4 | NP | −ve at D1; +ve at D7 | 1/4 |
| 36. | Buonsenso et al 53 | 2 | NP, AF, placenta, cord blood, rectal swab, BM | 1st: NP −ve on D1, D4 and +ve on D15, placenta, AF, rectal swab-negative, weak IgG +ve, IgM −ve 2nd: placenta, breast milk: +ve but cord blood negative in neonate with NP negative result |
1/2 |
| 37. | Fan C et al ()48 | 2 | NP, AF, cord blood, BM, placenta, vaginal swab | Negative | |
| 38. | Liu W et al ()56 | 3 | NP, cord blood, neonatal whole blood |
Negative (D2) | |
| 39. | Lowe B et al ()62 | 1 | NP | Negative | |
| 40. | Chen S et al ()104 | 3 | NP, placenta | Negative | |
| 41. | Chen Y et al ()58 | 4 | NP | Negative | |
| 42. | Gidlöf S et al ()76 | 2 | NP | Negative (34 hours and 4.5 days) | |
| 43. | Khan S et al ()85 | 3 | NP | Negative | |
| 44. | Schnettler W et al ()110 | 1 | NP, AF | AF −ve, NP −ve on D1, D2 | |
| 45. | Blauvelt C et al ()84 | 1 | NP, rectal swab D2 IgG and IgM |
NP −ve on D1, D2, D14 Rectal swab −ve on D2 IgG and IgM negative (D5) |
|
| 46. | Alzamora M et al ()78 | 1 | NP, cord blood | Negative for IgM and IgG; NP +ve at 16 hours and 48 hours | 1/1 |
| 47. | Vivanti A et al ()29 | 1 | NP, AF, vaginal swab, NBAL, neonatal blood and rectal swabs | NP +ve at 1 hour, D3, D18; rectal swab +ve at 1 hour, D3, D18; vaginal swab, NBAL, neonatal blood, AF +ve |
1/1 |
| 48. | Song L et al ()49 | 1 | NP, AF, cord blood, BM | NP −ve at D3, D7 All other negative |
|
| 49. | Zambrano L et al ()87 | 1 | NP | Negative | |
| 50. | Li Y et al ()44 | 1 | NP, neonatal blood, faeces and urine | NP negative at birth and 48 hours All other negative |
|
| 51. | Dong L et al ()55 | 1 | NP, serum vaginal swab |
IgM level elevated NP negative at 2 hours,16 hours |
1/1 |
| 52. | Baud D et al ()33 | 1 | NP, AF, placenta vaginal swabs |
Placenta +ve All other negative |
1/1; 2nd trimester spontaneous miscarriage |
| 53. | Wang X et al ()77 | 1 | NP, AF, placenta, cord blood, gastric juice, faeces | NP −ve at D1, D3, D7, D9 All other negative |
|
| 54. | Huang J et al ()86 | 1 | NP | Negative | |
| 55. | Iqbal S et al ()105 | 1 | NP | Negative | |
| 56. | Kalafat E et al ()79 | 1 | NP, cord blood, Placenta | Negative | |
| 57. | Lee D et al ()80 | 1 | NP, AF, cord blood, placenta, neonatal serum, anal swab | Negative | |
| 58. | Liao X et al ()106 | 1 | NP, AF, cord blood, placenta | Negative | |
| 59. | Xiong X et al ()50 | 1 | NP, AF, BM, rectal swab | Negative | |
| 60. | Wang S et al ()51 | 1 | NP, placenta, cord blood, BM | NP +ve at 36 hours −ve in all others |
1/1 |
| 61. | Zamaniyan M et al ()30 | 1 | NP, cord blood, AF, vaginal secretion | NP: −ve at 0 hour, +ve at D2, D4, D6 AF +ve, all others negative |
1/1 |
| 62. | Kirtsman M et al ()35 | 1 | NP, placental, stool, BM neonatal plasma D4 |
NP +ve at D1, D2, D7 Placenta +ve Stool +ve D7, BM +ve |
1/1 |
| 63. | Lyra J et al()74 | 1 | NP | Negative | |
| 64. | Algarroba G et al ()34 | 1 | NP | Negative at 0 hour, D2, D7 | |
| 65. | Peng Z et al ()43 | 1 | NP, NBAL fluid, sputum, urine | Negative | |
| 66. | Groß R et al ()52 | 2 | BM, NP | Both NP +ve (>D7), BM +ve (1) | 2/2,1/2 |
| 67. | Perrone S et al ()72 | 4 | NP (3), Placenta (1) | NP negative on D1, placenta-negative | |
| 68. | Hosier H et al ()32 | 1 | Placenta, cord blood | Both +ve | 1/1; D&E at 22 weeks |
| 69. | Pulinx B et al ()31 | 2 | AF, placental | Both +ve | 2/2, DCDA twin at 24 weeks |
| 70. | Yu N et al ()108 | 2 | AF in mid pregnancy | Negative | |
| 71. | Kulkarni et al ()117 | 1 | NP, placenta, cord stump, neonatal blood | All +ve at 12 hours of life; serology −ve on D10 but +ve on D21 | 1/1 |
| 72. | Sisman J et al ()70 | 1 | NP, placenta | NP +ve at 24 hours, 48 hours, D14; placenta +ve by electron microscopy | 1/1 |
D&E- dilatation and evacuation; AF, amniotic fluid; BM, breast milk; D1, 1st day of life; D4, 4th day of life; DCDA, dichorionic diamniotic; NBAL, non-bronchoscopic broncho-alveolar lavage fluid; NP, neonatal pharyngeal/throat swab.
Neonatal nasopharyngeal swab
In our review, a total of 1388 neonates born to mothers with COVID-19 infection were tested by NP swabs. 51 neonates were found positive by the RT-PCR test constituting 3.67% of total pooled samples (table 2a).
Table 2a.
Mother to child transmission-test positive (pooled result)
| Sample tested by RT-PCR for SARS-CoV-2 | Number of studies | Number tested | Number positive |
Pooled percentage |
| Neonatal naso-pharyngeal swab | 67 (32 case series/cohort+35 case reports) | 1388 (1335 case series/cohort+53 case reports) | 51 (40 out of 1335 in case series/cohort+11 out of 53 case reports) | 3.67 (3% in case series/cohort; 2.07% in case reports) |
| Placenta±membranes | 22 | 111 | 13 | 11.7 |
| Amniotic fluid | 19 | 58 | 4 | 6.8 |
| Breast milk | 10 | 56 | 3 | 5.3 |
| Cord blood/plasma | 16 | 56 | 4 | 7.1 |
| Other neonatal samples | ||||
| Anal swab | 11 | 52 | 5 | 9.6 |
| Urine | 3 | 9 | 0 | |
| Neonatal serology | ||||
| IgM | 5 | 11 | (Elevated) 3 | 27 |
| IgG | 4 | 10 | (Elevated) 6 | 60 |
RT, reverse transcriptase.
The largest cohort study from the UK involved 427 pregnant women with COVID-19. 244 out of the 262 neonates were tested by NP swab. Six of the neonates were positive for SARS-CoV-2 within 12 hours of birth and six more were positive after 12 hours of birth (12 out of 244; 4.9%).23 Studies involving 181 women and 116 women in China showed two positive neonates out of 181 (2 out of 181; 1.1%) in the first study and no positive cases for SARS-CoV-2 in the other study.24 25 An analysis of 141 women from a hospital in India showed that 3 of the 131 neonates were tested positive for SARS-CoV-2 by NP swab.26 In another study in a New York Hospital, 48 neonates born to 55 women were all tested negative on day 0 of life.27 However, one Italian study found three infants positive by NP swab out of 42 tested within 48 hours after birth.28
One recent case report revealed that RT-PCR was positive for SARS-CoV-2 in all of the samples for amniotic fluid, vaginal swab, blood and non-bronchoscopic bronchoalveolar lavage fluid as well as NP swab and rectal swabs collected at 1 hour of life, and then repeated at 3 days and 18 days suggesting a trans-placental transmission.29
As stated earlier NP swab positivity at different neonatal ages plays an important role in confirming or ruling out the viral transmission from a SARS-CoV-2 positive mother.
On further analysis of the positive samples, the congenital infection was confirmed in five live-born neonates, possible in five neonates and probable in two neonates. Neonatal infection acquired intra partum was confirmed in two neonates, probable in five neonates and possible in 14 neonates. Similarly, neonatal infection acquired post partum was confirmed in seven neonates and infection was unlikely in one neonate (table 2b).
Table 2b.
Analysis of evidence of congenital/ intrapartum/postpartum transmission
| Author (reference) (samples positive/total tested) |
Samples +ve | Foetal/neonatal status | Alternate explanation for clinical features | Mother to child transmission (n) |
| Groß R et al(2/2)52 | NP >D7 | Respiratory symptoms (2), icterus (1) | Alternate explanation: excluded in 1; respiratory syncytial virus +ve in 1 | Neonatal infection acquired post partum: confirmed (1) unlikely (1) |
| Buonsenso et al(1/2)53 | 1st: NP −ve on D1, D4 and +ve on D15, placenta, AF, rectal swab:negative, weak IgG +ve, IgM −ve second - Placenta, Breast milk-+ve but cord blood negative in neonate with NP negative result |
Symptoms: absent | – | Neonatal infection acquired post partum: confirmed (asymptomatic) (1st) possible congenital infection (2nd) |
| Vivanti A et al(1/1)29 | NP +ve at 1 hour, D3, D18; rectal swab +ve at 1 hour, D3, D18; vaginal swab, NBAL, neonatal blood +ve |
Irritability, poor feeding, axial hypertonia and opisthotonos | Alternate explanation: excluded | Confirmed congenital infection |
| Kirtsman M et al(1/1)35 | NP +ve at birth, D2, D7 Placenta (foetal side) +ve Stool +ve D7, BM +ve |
Hypothermia, feeding difficulties, hypoglycaemic, neutropenia | Alternate explanation: excluded | Probable congenital infection |
| Zamaniyan M et al(1/1)30 | NP: −ve at 0 hours, +ve at D2, D4, D6 AF before rupture of membranes +ve cord blood and vaginal secretion: negative |
Fever (1) | Alternate explanation: not identified | Confirmed congenital infection |
| Wang S et al(1/1)51 | NP +ve at 36 hours placenta, cord blood, BM:−ve |
Vomiting, lymphopenia, abnormal liver enzyme levels | Alternate explanation: excluded | Neonatal infection acquired intra partum: possible |
| Khan S et al(2/17)64 | NP +ve within 24 hours | NNP | Alternate explanation: not identified | Neonatal infection acquired intra partum: possible |
| Zeng L et al(3/33)41 | NP +ve at D2, D4, −ve at D6 | RD (1); cyanosis, feeding intolerance (1); fever (2); NNP (3); lethargy, fever (1); lethargy, fever, NNP, vomiting leukocytosis, lymphocytopenia (1); preterm- neonatal RDS, NNP, lymphocytopenia (1) | Alternate explanation: excluded | Neonatal infection acquired intra partum: possible NP not done at birth, no other samples tested |
| Hu X et al(1/7)42 | NP +ve at 36 hours; foetal urine, AF are negative | Symptoms: absent | – | Neonatal infection acquired intra partum: possible NP not done at birth |
| Knight M et al(12/244)23 | NP +ve at <12 hours (6) NP +ve at >12 hours (6) |
Neonatal encephalopathy (1) | – | Congenital infection possible (1) Other evidences lacking |
| Alzamora M et al(1/1)78 | NP +ve at 16 hours and 48 hours Cord blood IgM and IgG negative at D1 and D5 |
Respiratory difficulty and cough | Alternate explanation: excluded | Neonatal infection acquired intra partum: confirmed NP not done at birth |
| Hantoushzadeh et al(1/4)75 | NP −ve on D1, +ve on D7 | NNP, lymphopenia (1) | – | Neonatal infection acquired post partum: confirmed |
| Pierce-Williams R et al(1/33)63 | Negative at 24 hours, +ve at 48 hours |
Symptoms: absent | – | Neonatal infection acquired post partum: confirmed |
| Nayak A et al(3/131)26 | NP +ve on D1; −ve on D5 | Neonatal seizures, MAS (1) | – | Probable neonatal infection acquired intra partum |
| Nie R et al(1/26)68 | NP +ve at 36 hours, negative: D4, D8, D15; cord blood, placenta:negative | Pulmonary infection (1) | Alternate explanation: not identified | Neonatal infection acquired intra partum: possible NP not done at birth |
| Savasi V et al(4/57)109 | Timing of NP test could not be ascertained (early postpartum period) | – | – | – |
| Kayem G et al(2/181)25 | Timing of test could not be ascertained | – | – | – |
| Patane L et al(2/22)39 | 1st: NP +ve at birth, >24 hours, >7 days 2nd: NP negative at birth, +ve on D7 Placenta: chronic intervillitis, PCR +ve in both placenta |
Mild feeding difficulty (2) | – | Probable congenital infection (1) Possible congenital infection (1) |
| Ferrazzi E et al(3/42)28 | NP +ve on D1, D3 (2) NP equivocal at birth but +ve on D3 (1) |
Gastrointestinal symptoms, RD (2) | Alternate explanation: not identified | Neonatal infection acquired post partum: confirmed (1) Neonatal infection acquired intra partum: possible (2) Other evidences lacking |
| Govind A et al(1/9)61 | NP at birth | NNP (1) | Alternate explanation: excluded | Neonatal infection acquired intra partum: confirmed? NP not done after 24 hours |
| Penfield C et al((3/11)103 | NP: Negative (D1 and D5) Placenta and membrane +ve |
Symptoms: absent | Neonatal infection acquired intra partum: possible | |
| Baud D et al(1/1)33 | NP, AF, vaginal swabs: negative Placenta +ve |
2nd trimester spontaneous miscarriage | Confirmed congenital infection | |
| Hosier H et al(1/1)32 | Placenta, cord blood: both +ve | D&E at 22 weeks | Confirmed congenital infection | |
| Pulinx B et al(2/2)31 | AF, placenta: both +ve | DCDA twin at 24 weeks expelled | Confirmed congenital infection | |
| Dong L et al(1/1)55 | IgM level elevated NP negative at 2 hours,16 hours |
Symptoms: absent | – | Possible congenital infection |
| Zeng H et al(1/1)54 | NP negative; elevated IgM and IgG (2); elevated IgG, normal IgM (3) |
Symptoms: absent | – | Possible congenital infection |
| Martínez-Perez O et al(5/82)65 | NP +ve at birth and negative at 48 hours (3); NP negative at birth but +ve at D10 (2) | RD (2) Symptoms: absent (3) |
Alternate explanation: not identified (2) | Neonatal infection acquired intra partum: probable (2) Neonatal infection acquired intra partum: possible (1) Neonatal infection acquired post partum: confirmed (2) |
| Kulkarni et al(1/1)117 | NP, placenta, cord stump RT PCR- All +ve at 12 hours of life NP at D5 and D10 +ve |
Fever, icterus and poor feeding | Alternate explanation:excluded | Confirmed congenital infection |
| Sisman J et al(1/1)70 | NP +ve at 24 hours, 48 hours, D14 placenta +ve by electron microscopy |
Fever, RD, icterus | Alternate explanation: excluded | Confirmed congenital infection |
AF, amniotic fluid; BM, breast milk; DCDA, dichorionic diamniotic; D&E, dilatation and evacuation; NBAL, non-bronchoscopic broncho-alveolar lavage fluid; NNP, neonatal pneumonia; NP, neonatal pharyngeal/throat swab; RD, respiratory distress.
However, in a larger study, out of 12 neonates with positive NP result (six within 12 hours of life and six at more than 12 hours of life), further analysis was not possible due to lack of follow-up swab results and unavailability of test results of other maternal samples like placenta and amniotic fluid.23
Amniotic fluid
In our review, 58 samples of amniotic fluid were tested in 19 studies with a positive result in four samples.29–31 Congenital infection is confirmed in two of the studies in live-born neonates.29 30 Congenital infection is also confirmed in a dichorionic, diamniotic (DCDA) twin expelled at 24 weeks by positive amniotic fluid result.31
Placenta
A total of 22 studies were identified in our review where the placenta was examined for the presence of SARS-CoV-2 or related pathological changes. A total of 111 placental samples were tested and 13 were found positive for SARS-CoV-2. PCR for SARS-CoV-2 RNA was positive from the placenta in two case reports where there were spontaneous miscarriage and dilatation and curettage, respectively confirming a congenital infection.32 33 In one of them, the umbilical cord was also positive for the virus, but the foetal organs were tested negative. The virus was confirmed to be localised mostly in the syncytiotrophoblastic cells of the placenta by immunohistochemistry for the SARS-CoV-2 spike protein as well as electron microscopy and it was identical to the typically locally isolated virus.32 In another study, electron microscopy showed the presence of the virus in the foetal side of the placenta. The virions were present in the mesenchymal core of the terminal villus and were demonstrated to be invading a syncytiotrophoblast and a microvillus. However, the neonate delivered at 28 weeks in this pregnancy was tested negative for the virus.34
Evidence of probable mother to child transmission was obtained in another case where the newborn was found positive for the virus by nasopharyngeal swab, plasma and stool samples along with the placenta.35 Similarly, confirmed congenital transmission of the virus was demonstrated by another study where SARS-CoV-2 was detected in amniotic fluid aspirated before the rupture of the membranes, vaginal swab, neonatal blood, bronchoalveolar lavage fluid and neonatal swabs on repeated occasions at 1 hour, 3rd day and 18th day of life. The trophoblastic cells showed SARS-CoV-2 N protein on immunostaining.29
Placental pathological examination showed an array of changes including vascular malperfusion, fibrin deposition, and chronic villitis, intervillositis, and villous infarctions in our review. Two of these studies showed vascular malperfusion in 10 out of 20 placentas and 12 out of 15 placentas, respectively but there were no assessments of placentas in these studies for the presence of SARS-CoV-2 infection. However, neonatal swabs were negative for the virus.36 37 Similar pathological changes were seen in another study involving five SARS-CoV-2 positive pregnant women but the placentas were negative for the virus on direct testing for SARS-CoV-2.38 Chronic intervillositis was also seen in the pathological examination of the placentas of two women where the neonates were positive for SARS-CoV-2 by nasopharyngeal swab testing.39 Examination showed severe chronic villitis in another case where there was a stillbirth at term but direct tests of foetal tissues and placenta did not show infection with the virus.40
Other samples
Various other samples were tested for SARS-CoV-2 by different studies. Anal swab, rectal swab or faecal sample was positive in 9.6% of neonates in our study. The stool sample was positive in two of the studies on day 2 and day 7 of life.35 41 The urine sample was tested in only three studies without any positive results.42–44 Breast milk was tested by RT-PCR in 10 of the studies with a pooled positive rate of 5.3% (3 out of 56).35 45–53 In one of the studies, the breast milk sample was positive in four consecutive days coinciding with the maternal symptoms in one woman but it was negative in milk samples of another woman. Both the babies were positive by the nasopharyngeal swab test and were symptomatic.52 A vaginal swab was tested in 23 women with one positive result (4.3%).29 Since IgM cannot cross the placenta, elevated IgM levels in the neonate indicate possible congenital infection, as seen in some of the neonates in this review.54 55 However, the assay of IgM for the detection of infection has significant false-positive results.
Perinatal outcome
Search results
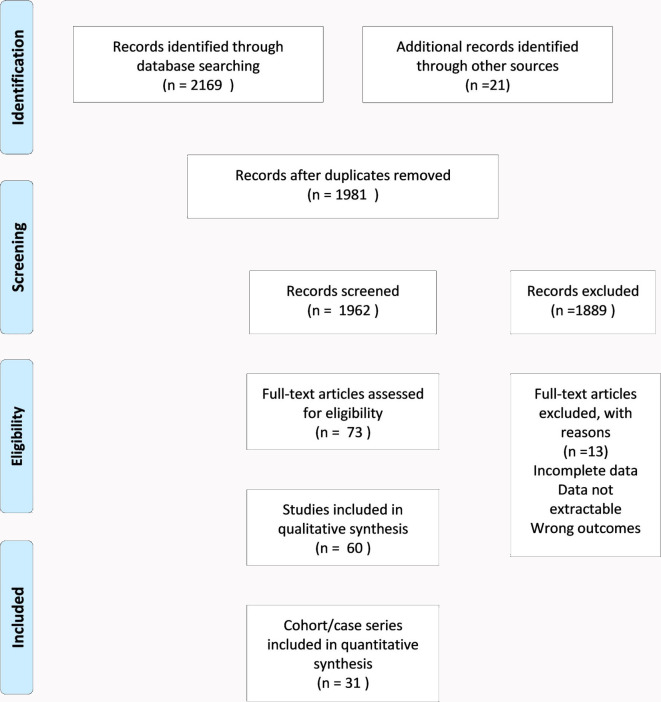
Out of 73 records selected for full-text review, 1 Chinese and 1 Spanish study were excluded due to unavailability of English translation. A total of 60 studies fulfilled the eligibility criteria and were included in the qualitative synthesis. Thirty-one studies qualified as case series/cohort and 29 studies contained four or fewer cases in our review (figure 2). No randomised control trials were available until the time of the search.
Figure 2.
Image-PRISMA-2-Perinatal outcome.
Systematic review
Foetal outcomes
Foetal complications in SARS-CoV-2 positive pregnant women
In our review, a total of 30 studies reported any foetal effects excluding all pregnancy losses or IUFDs (table 3). The most commonly reported effect was foetal distress in 36 out of 1311 pregnancies (2.74%). In addition to foetal distress, some studies have reported non-reassuring or pathological cardiotocography (CTG) (11 out of 1311; 0.83 %), and some have mentioned meconium-stained amniotic fluid (3 out of 1311; 0.22%), both findings can also be considered as evidence of foetal distress.29 56–62 In another study involving 262 deliveries, the foetal compromise was seen in 37 foetuses and an emergency CS was done in 9 of them.23 Thus, the cumulative chance of foetal distress in pregnant women with a positive test for SARS-CoV-2 is 6.63%.
Table 3.
Foetal outcome
| Serial number | Author (reference) | Number of neonates from SARS CoV-2 +ve pregnancies | Foetal complications (n) |
Mode of delivery (n) | Birth weight (g) | Preterm delivery (n) | Stillbirth (n) | Comments |
| 1. | Chen H et ai45 | 9 | FD (2) PROM (1) |
CS (9) | 1880–3730 | Yes (2) | – | |
| 2. | Romagano M et al 82 | 7 | – | CS (7) | 1290–2580 (AGA) | Yes (7) | ||
| 3. | Zeng H et al 54 | 6 | CS (6) | – | ||||
| 4. | Zhu H et al 57 | 10 | FD (6), PROM (3), MSA (2) | CS (7) VD (2) |
SGA-2 LGA/normal-8 |
Yes (6) | – | 1 twin delivery |
| 5. | Khan S et al 64 | 17 | PROM | CS (17) | 2300–3750 <2700(3) |
Yes (5) | – | |
| 6. | Zeng L et al 41 | 33 | PROM (3); FD (1) | VD (7); CS (26) |
SGA (3) 1580–3360 |
Yes (4) | – | |
| 7. | Breslin N et al 59 | 18 | Ab.CTG (3) | CS (8); VD (10) |
Yes (1) | – | ||
| 8. | Qiancheng X et al 107 | 23 | – | CS (17) VD (5) |
3130 (2915–3390) | Yes (1) | – | 1 twin delivery |
| 9. | Hantoushzadeh S et al 75 | 5 | IUFD (3) | CS (4) | 1180–3200 | Yes (3) | Yes (1) | 1 twin delivery |
| 10. | Martínez-Perez O et al 65 | 82 | PROM (18) PPROM (7) IUGR (1) |
VD (41) CS (41) |
1450–3210 | Yes (25) | – | |
| 11. | Savasi V et al 109 | 57 | – | VD (34) CS (22) |
3160 (840–4350) | Yes (12) | – | 1 twin delivery |
| 12. | London V et al 27 | 56 | DFM (1) IUFD (17 weeks) (1) |
CS (22) VD (33) |
– | Yes (12) | – | |
| 13. | Lokken E et al 40 | 8 | FD (3) | CS (3) VD (5) |
– | Yes (1) | Yes(1) | |
| 14. | Yan J et al 24 | 99 | FD (9); IUGR (2) PPROM (6) |
CS (85) VD (14) |
3108±526 | Yes (21) | – | |
| 15. | Pierce-Williams R et al 63 | 32 | IUGR(2), PPROM (1) | CS (24) VD (8) |
2403.3±858 | Yes (19) | – | |
| 16. | Knight M et al 23 | 262 | Miscarriage (4) Foetal compromise (37) |
CS (156) VD (106) |
– | Yes (66) | Yes (3) | |
| 17. | Kayem G et al 25 | 176 | Foetal loss <21 weeks (5) | CS (87) VD (89) |
– | Yes (50) | Yes (2) | |
| 18. | Nayak A et al 26 | 134 | Miscarriage (6) | CS (67) VD (67) |
>2500 (92) <2500 (39) |
Yes (38) | Yes (3) | |
| 19. | Prabhu M et al 60 | 70 | PROM and Ab.CTG (4) |
CS (32) VD (38) |
3060.9–3149.6 | Yes (11) | Yes (1) | |
| 20. | Li N et al 66 | 17 | FD (1); PROM (1) | CS (14) VD (2) |
3078.2±565.0 | Yes (4) | – | 1 twin delivery |
| 21. | Cao D et al 67 | 11 | FD (3); PROM (4) | CS (8) VD (2) |
2050–3800 | Yes (4) | – | 1 twin delivery |
| 22. | Hu X et al 42 | 7 | PROM (1) | CS (6) VD (1) |
3180–3670 | – | – | |
| 23. | Yang P et al 81 | 7 | – | CS (7) | 2096±660 | Yes (4) | – | |
| 24. | Yang H et al 73 | 13 | – | CS (9) VD (4) |
3063.2±536.4 | – | – | |
| 25. | Ferrazzi E et al 28 | 42 | – | CS (18) VD (24) |
2730–3226 | Yes (11) | – | |
| 26. | Govind A et al 61 | 9 | Ab.CTG (1) | CS (8) VD (1) |
1200–4300 | Yes (2) | – | |
| 27. | Nie R et al 68 | 28 | FD (4); IM (1); PROM (3) |
VD (5); CS (22) |
2988 (502) | Yes (10) | – | 1 twin delivery |
| 28. | Yin M et al 46 | 17 | IM (3) | VD (4); CS (13) |
2580–3035 | Yes (5) | – | |
| 29. | Qadri F115 | 10 | CS (2) VD (8) |
Yes (1) | ||||
| 30. | Dória M et al 71 | 10 | IUGR (6) | CS (6) VD (4) |
2350–3380 | – | – | |
| 31. | Liu Y et al 69 | 10 | FD(3), PROM (1) | CS (10) | Yes (6) | Yes (1) | ||
| 32. | Perrone S et al 72 | 4 | IUGR (1) | VD (4) | 2290–3790 | – | – | |
| 33. | Patane L et al 39 | 2 | – | VD (1) CS (1) |
2660–2686 | Yes (1) | – | |
| 34. | Fan C et al 48 | 2 | – | CS (2) | 3440–2890 | Yes (1) | – | |
| 35. | Pulinx B et al 31 | 2 | IUFD (1) | VD (2) | Yes (1) | Yes (1) | DCDA twins | |
| 36. | Liu W et al 56 | 3 | FD (1); MSA; chorioamnionitis | CS (2) VD (1) |
3250–3670 | – | – | |
| 37. | Cooke W et al 83 | 2 | – | CS (2) | 1530, 1400 | Yes (2) | – | |
| 38. | Chen Y et al 58 | 4 | DFM (1) Ab.CTG (1) |
CS (3) VD (1) |
3050–3550 | – | – | |
| 39. | Gildof S et al 76 | 2 | – | CS (2) | 2680, 2160 | Yes (2) | – | |
| 40. | Khan S et al 85 | 3 | – | VD (3) | 2890–3750 | Yes (1) | – | |
| 41. | Zambrano L et al 87 | 1 | – | VD (1) | 1500 | Yes(1) | – | |
| 42. | Lowe B et al 62 | 1 | Ab.CTG (1) | VD (1) | – | – | ||
| 43. | Blauvelt C84 | 1 | – | CS (1) | 1880 | Yes (1) | – | |
| 44. | Kirtsman M et al 35 | 1 | – | CS (1) | 2930 | Yes (1) | – | |
| 45. | Lyra J et al 74 | 1 | – | CS (1) | 3110 | – | – | |
| 46. | Li Y et al 44 | 1 | FD(1) | CS (1) | Yes (1) | – | ||
| 47. | Dong L et al 55 | 1 | – | CS (1) | 3120 | Yes (1) | – | |
| 48. | Wang X et al 77 | 1 | FD (1) | CS (1) | 1830 | Yes (1) | – | |
| 49. | Alzamora M et al 78 | 1 | – | CS (1) | 2970 | – | – | |
| 50. | Huang J et al 86 | 1 | – | VD (1) | – | – | ||
| 51. | Kalafat E et al 79 | 1 | – | CS (1) | 2790 | Yes (1) | – | |
| 52. | Xiong S et al 50 | 1 | PROM | VD (1) | 3070 | – | – | |
| 53. | Wang S et al 51 | 1 | FD (1) | CS (1) | 3205 | – | – | |
| 54. | Zamaniyan M et al 30 | 1 | – | CS (1) | 2350 | Yes (1) | – | |
| 55. | Song L et al 49 | 1 | – | CS (1) | 3630 | Yes (1) | – | |
| 56. | Lee D et al 80 | 1 | – | CS (1) | 3130 | – | – | |
| 57. | Iqbal S et al 105 | 1 | VD (1) | |||||
| 58. | Vivanti A et al 29 | 1 | Ab.CTG (1) | CS (1) | 2540 | Yes (1) | – | |
| 59. | Kulkarni et al 117 | 1 | – | VD (1) | 3200 | – | – | |
| 60. | Sisman J et al 70 | 1 | PROM | VD (1) | 3280 | Yes (1) |
Ab.CTG, non-reassuring/pathological foetal cardio-tocography; AGA, appropriate for gestational age; CS, caesarean section; DFM, Decreased foetal movement; FD, foetal distress; IM, induced miscarriage; IUFD, intrauterine fetal deaths; IUGR, intrauterine growth restriction; LGA, Large for gestational age; MSA, meconium-stained amniotic fluid; PROM, prelabour rupture of membrane; SGA, small for gestational age; VD, vaginal delivery.
Premature rupture of membrane (PROM) was reported in 42 pregnancies from 13 studies and Preterm PROM (PPROM) was reported in 14 pregnancies.24 41 42 45 50 57 60 63–70 IUGR was reported in 12 foetuses in five studies.24 63 65 71 72 The highest number of IUGR foetuses was reported in 6 out of 10 foetuses in another study.71 Besides, SGA was reported in another study in 2 out of 10 foetuses.57 Chorioamnionitis was reported only in one study involving three foetuses.5
Mode of delivery
Mode of delivery was available for a total of 1311 out of which 8 were twin pregnancies. 761 (60%) were delivered by CS and 506 (40%) by VD out of 1267 pregnancies from case series. In case reports, out of 44 deliveries, 25 were CS (56.8%) and 19 (43.2%) were VD bringing the percentage of CS to 59.9% and VD to 40.1% in the pooled data (table 4). Few studies in our data compared the CS in the SARS-CoV-2 positive pregnant women to negative controls comprising of 122 CS in the positive group out of 233 and 650 CS in the control group out of 1562 in the pooled data. OR for CS in SARS-CoV-2 positive mothers is 1.5421 (95% CI 1.1701 to 2.0324) and p=0.0021 which is statistically significant.26 60 66 73
Table 4.
Perinatal outcome (pooled data)
| Foetal outcome | ||||
| Outcome | Number of studies | Results | Indications | Remarks |
| Preterm birth | 43 studies (26 case series/cohort and 17 case reports) |
|
|
Pooled preterm birth in 26.4% of total births Spontaneous preterm birth: 1.8% of total births |
| Mode of delivery | 59 studies (30 case series/cohort and 29 case reports) |
|
Maternal COVID-19 related conditions most common indication | Pooled data: CS=786 (59.9%) VD=525 (40.1%) |
| Stillbirth Miscarriage |
Stillbirth=8 studies Miscarriage=5 studies |
Stillbirth=13 Spontaneous miscarriage=15 Induced miscarriage=4 |
All induced miscarriages were due to maternal request | Stillbirth rate=9.9 |
| Feral complications | FD=21 studies PROM and PPROM=15 studies |
Foetal distress (87 out of 1311 pregnancies) (6.63%) PROM and PPROM (56 out of 1311 pregnancies) (4.27%) |
– | – |
| IUGR and SGA | IUGR: 5 studies SGA: 2 studies |
12 foetuses had IUGR (0.9%) 5 neonates had SGA (0.38%) |
– | – |
| Neonatal outcomes | ||||
| Outcome | Results | |||
| Neonatal symptoms | Respiratory symptoms=23 neonates (1.79%) Neonatal pneumonia and pulmonary infection=14 neonates (1.1%) Fever=12 neonates (0.9%) |
Most common symptom is respiratory distress in (1.17%) | ||
| APGAR score | Score of less than 7 at 1 min and 5 minutes=neonates | Most common reason is preterm birth | ||
| ICU admissions | In 276 neonates (21.5%) | Most common reason was for observation and isolation (32.6 %) Prematurity is second most common reason ICU admissions for suspected or confirmed neonatal sepsis was reported in 6 neonates (0.46%) |
||
| Neonatal death | 7 neonates | Neonatal death rate=5.46 per 1000 live births | ||
Ab.CTG, non-reassuring/pathological foetal cardio-tocography; CS, caesarean section; FD, foetal distress; ICU, intensive care unit; IM, induced miscarriage; IUGR, intrauterine growth restriction; MSA, meconium-stained amniotic fluid; PROM, prelabour rupture of membrane; SGA, small for gestational age; VD, vaginal delivery.
CS was the only mode of delivery in the majority of early published case reports as in the early days of the pandemic, elective CS delivery was the mode preferred by most of the countries for maternal indications.29 30 35 44 45 48 49 51 54 55 64 74–84 As the pandemic progressed, favourable outcomes were reported from vaginal delivery by many studies.50 62 72 85–87 It was also demonstrated that the chances of the virus being present in the vaginal fluid is very remote. In the later and larger case series, CS deliveries were only done for obstetrical indications.26 In a study involving 134 deliveries, there were 67 CS and 67 VDs. The rate of CS was not statistically different in women with positive SARS-CoV-2 as compared with negative pregnancies.26 In yet another study, there were significantly higher rates of CS deliveries in cases (14 out of 16) as compared with the control group (57 out of 121) (p<0.001) but there was no difference in the groups with regards to chronic illnesses or pregnancy complications.66 However, when done for maternal COVID-19 indications, the rate of caesarean was found to increase with the severity of the disease.25 In another study, out of 41 CS deliveries, 12 were for COVID-19 symptoms without other obstetrical indications (four with severe symptoms and eight with mild/moderate symptoms).65
In the largest study in the UK, the CS delivery was seen in 156 women and vaginal birth was seen in 106 women from a total of 262 births. The indications of CS were maternal compromise (27%), foetal compromise (24%), failed induction of labour or failure to progress (19%), other obstetric reasons (16%), prior CS (10%) and maternal request (4%).23 Maternal COVID-19 related conditions were predominant indications in another larger study reporting CS for COVID-19 pneumonia in (33 out of 85), previous CS (16 out of 85), foetal distress (9 out of 85) and failure to progress in 5 out of 85 patients.24 Many other studies similarly reported maternal condition requiring delivery as the most common indication for CS.25 28 81
Preterm delivery
In our study, the outcome of preterm delivery was reported in a total of 43 studies involving 1318 foetuses out of which 330 out of 1273 neonates in the case series and cohort (25.9%) and 19 out of 45 neonates in the case reports (42.2%) were delivered preterm. The pooled preterm birth was seen in 26.4% of total births (table 4). However, the majority of them were elective deliveries to improve maternal respiratory conditions related to COVID-19. Spontaneous preterm delivery was only seen in 1.8% of neonates. The other indications included the preterm prelabour rupture of membranes. In a substantial number of studies, data regarding the indications were not found. Few studies in our data compared the preterm delivery in the SARS-CoV-2 positive pregnant women to negative controls comprising 52 preterm deliveries in the positive group out of 220 and 267 preterm deliveries in the control group out of 1520 in the pooled data. OR for preterm delivery in SARS-CoV-2 positive mothers is 1.4526 (95% CI 1.0360 to 2.0366) and p=0.0304.26 60 66
In a study involving 134 deliveries in COVID-19 patients, preterm delivery was reported in 38 pregnancies with positive SARS-CoV-2 and 239 out of 836 SARS-CoV-2 negative deliveries, which was not significantly different.26 A similar report was seen in another study where 4 preterm deliveries were seen out of 17 SARS-CoV-2 confirmed group as compared with 7 out of 121 in the control group.66 In another study, out of a total of 25 preterm deliveries, iatrogenic preterm delivery was done in 12 and 13 were spontaneous preterm deliveries.65
Furthermore, comparing the outcomes of COVID-19 pregnancies with different disease severity involving 181 pregnant women, preterm delivery was seen in 13 out of 123 (10.6%), 14 out of 29 (48.3%) and 23 out of 29 (79.3%) in women with non-severe, oxygen-requiring and critical COVID-19, respectively. Delivery before 32 weeks was highest in 48.3% of women in the critical COVID-19 group. In severe disease, urgent delivery is required to stabilise the maternal condition, even when it results in iatrogenic preterm delivery.25
Birth weight
In our review, birth weight was missing in many studies and only the mean weight of the babies was mentioned in some of the series. IUGR was reported in 4 studies in 11 babies.24 63 71 72 Also, SGA was found in two studies in five babies.41 57 A maximum of six babies had IUGR in one study but they were described as mild.71
Miscarriage and stillbirth
Stillbirth was seen in 13 foetuses in 8 studies in our review and seven were second-trimester miscarriages23 25 26 31 40 60 69 75 (table 4). Three intrauterine deaths were observed in one of the studies which reported maternal deaths due to COVID-19.75 Similarly, we found 15 spontaneous miscarriages, and 4 induced miscarriages reported in 5 studies.23 25 26 46 68 Induced miscarriages were done on maternal request in both studies.46 68 Among the spontaneous miscarriages, 6 were seen in 141 pregnancies in one study and 5 in 181 pregnancies in another study.25 26 In one of the studies, there were three stillbirths. However, the causes of these three stillbirths reported, were not related to COVID-19 in the mother.23
Neonatal outcomes
Neonatal symptoms
The most common neonatal symptoms were respiratory problems reported as respiratory distress, shortness of breath, respiratory difficulty, dyspnoea and breathing problems.28 41 52 57–59 65 70 76 78 81 82 84 Respiratory distress was the most common symptom reported in 14 neonates but the test for SARS-CoV-2 was positive in only 4 neonates and negative in 8.28 41 59 65 81 82 84 Pneumonia was seen in five neonates who were positive for SARS-CoV-2 and four neonates who were negative.41 48 61 64 75 Although usually respiratory symptoms are seen more in preterm babies due to pulmonary immaturity, in a single case report there were no neonatal complications in a SARS-CoV-2 positive mother who delivered a preterm baby at 29 weeks 5 days by emergency CS for maternal indications.88
Diffuse bilateral granular and hazy opacities in chest radiograph and thickened lungs on X-ray were found in two neonates but the neonatal test for SARS-CoV-2 was negative in both of them.51 84 In another SARS-CoV-2 positive, newborn chest X-ray was consistent with pulmonary infection, 53 hours after birth.68 In another study, neonatal symptoms are extensively described. The most common first clinical symptom in the neonates of SARS-CoV-2 positive women was shortness of breath (n=6), followed by gastrointestinal symptoms like feeding intolerance, bloating, refusing milk and gastric bleeding (n=4). Other symptoms included fever, rapid heart rate and vomiting. Chest radiographic abnormalities included infections (n=4), neonatal respiratory distress syndrome (n=2) and pneumothorax (n=1). Another preterm baby suffered from frequent oxygenation fluctuations and thrombocytopenia and was cured 15 days later.57 It was reported in yet another study that most of the complications in neonates were a result of prematurity (often iatrogenic) rather than SARS-CoV-2 infection.41 Other presentations in SARS-CoV-2 positive neonates included fever, cyanosis, lethargy, irritability, poor feeding, axial hypertonia, opisthotonus and feeding difficulties.29 39 41
APGAR score
In our review, a total of nine studies have reported a low APGAR score among babies born to SARS-CoV-2 positive mothers.26 28 29 41 61 78 82–84 Seven of the neonates were very preterm or preterm and were SARS-CoV-2 negative. The APGAR score in these is likely to be due to pulmonary immaturity.26 28 29 78 82–84 Two other babies were term deliveries and tested positive for SARS-CoV-2.41 61 However, another study reported low APGAR scores of 0–3 in 2 babies of COVID-19 positive mothers and 15 babies in COVID-19 negative mothers, indicating no statistically significant difference.26
ICU admissions
Admission to the neonatal ICU was done for various reasons. The majority of admissions were for observation and isolation. Neonates admitted due to complications of prematurity constitute another higher portion of the neonates. In a study, out of a total of 24 ICU admissions, it was found that 16 babies were admitted due to low birth weight, 2 for low APGAR score and 6 others for other uncommon reasons like ABO blood group incompatibility.26 In another study, it was found that rates of admission to ICU increased with the severity of the disease in the mother.25 In our review, ICU admissions for suspected or confirmed neonatal sepsis was reported in six neonates out of which enterobacter and respiratory syncytial virus was found in two neonates. The culture was negative for four others.35 41 51 52 59 70
Neonatal death
Neonatal death was reported among seven neonates in five studies.23–25 57 75 It was unclear whether COVID-19 in mothers contributed to the deaths in two neonates in one of the studies.23 In another study, neonatal death occurred in a preterm baby on the ninth day of life who was admitted with shortness of breath and moaning and later developed refractory shock, multiple organ failure and disseminated intravascular coagulation.57 The calculated neonatal death rate is 5.47 per 1000 live births (table 5).
Table 5.
Neonatal outcome
| Serial number | Author (reference) | Number of neonates | APGAR score (1 min, 5 min) | Neonatal symptoms (n) | Neonatal ICU admission (n) | Neonatal death | Neonatal RTPCR status |
| 1. | Alzamora M et al 78 | 1 | 6–8 | Respiratory difficulty Cough on D6 |
(1) (due to maternal sedation) | – | +ve |
| 2. | Chen H et al 45 | 9 | 8–10 | – | – | – | |
| 3. | Fan C et al 48 | 2 | 9–10 | Fever, abdominal distension, lymphopenia (1) Mild NNP, lymphopenia (1) |
– | – | Negative |
| 4. | Dong L et al 55 | 1 | 9–10 | – | – | – | |
| 5. | Zeng H et al 54 | 6 | 9–10 | – | – | ||
| 6. | Liu W et al 56 | 3 | 8–10 | Decreased responsiveness and decreased muscle tone | – | – | Negative |
| 7. | Zhu H et al 57 | 10 | 8–10 in all 7–8 in 1 |
Shortness of breath (6), vomiting (1), rash (1), fever (3) | Yes (2) | Yes (1) | Negative |
| 8. | Wang X et al 77 | 1 | 9–10 | – | Yes (1) | – | |
| 9. | Liu Y et al 69 | 10 | 10 | – | – | – | |
| 10. | Chen Y et al 58 | 4 | 8–9 (3) 7–8 (1) |
Oedema (1), rash (2), dyspnoea and TTN (1) | Yes (2) | – | Negative |
| 11. | Gidlöf S et al 76 | 2 | 9–10 | Breathing problem, cyanotic attack (1) | Negative | ||
| 12. | Huang J et al 86 | 1 | 8–9 | – | – | – | |
| 13. | Iqbal S et al 105 | 1 | 9 | – | – | – | |
| 14. | Lee D et al 80 | 1 | 9–10 | – | Yes (1) | – | |
| 15. | Khan S et al 85 | 3 | 9–10 | – | – | – | |
| 16. | Khan S et al 64 | 17 | 9–10 (16) 7–9 (1) |
NNP (5) | – | – | 2 out of 5 with pneumonia were +ve |
| 17. | Xiong S et al 50 | 1 | 9–10 | – | – | – | |
| 18. | Wang S et al 51 | 1 | 8–9 | Vomiting, lymphopenia, abnormal liver enzyme levels | Yes (1) | – | Negative |
| 19. | Zeng L et al 41 | 33 | Preterm newborn: 3, 4 Term: normal |
RD (4=3 ve, 1+ve). Cyanosis, feeding intolerance (3=2 ve,1+ve) Fever in 2, NNP in 3 of the 3+ve Lethargy, fever (1) lethargy, fever, NNP, leucocytosis, lymphocytopenia, vomiting (1) Preterm: neonatal RDS, NNP, lymphocytopenia (1) |
Yes (3) | – | +ve |
| 20. | Zamaniyan M et al 30 | 1 | 8, 9 | Fever (1) | – | – | +ve |
| 21. | Breslin N et al 59 | 18 | >7, >9 | RD/sepsis (1) | Yes (3) | – | Negative |
| 22. | Qiancheng X et al 107 | 23 | 10, 10 | – | – | ||
| 23. | Hantoushzadeh S et al 75 | 5 | 7 (2), 9–10 | NNP, lymphopenia (1) | Yes (1) | Yes (2) | Negative |
| 24. | Shanes E et al 36 | 15 | 7 (8), 8 (7); 9 | ||||
| 25. | Zambrano L et al 87 | 1 | – | – | Yes (1) | – | |
| 26. | Martínez-Perez O et al 65 | 82 | <5 (3) | RD (2) | Yes (19) | +ve | |
| 27. | Savasi V et al 109 | 57 | 10 | – | Yes (9) | – | |
| 28. | Song L et al 49 | 1 | 8, 9 | – | – | – | |
| 29. | Lokken E et al 40 | 8 | |||||
| 30. | Yan J et al 24 | 99 | 9, 10 | Neonatal asphyxia (1) | Yes (47) | Yes (1) | Negative |
| 31. | Pierce-Williams R et al 63 | 32 | 7.9±1.7 | – | Yes (21) | – | |
| 32. | Knight M et al 23 | 262 | Neonatal encephalopathy (1) | Yes (67) | Ys (2) | Unclear whether symptomatic neonate was +ve | |
| 33. | Kayem G et al 25 | 181 | – | Yes (37) | Yes (1) | ||
| 34. | Nayak A et al 26 | 131 | 7–10 (128) <7 (6) |
Neonatal seizures (1), MAS (1) | Yes (24) | Unclear whether symptomatic neonates were +ve | |
| 35. | Prabhu et al 60 | 73 | 9 | – | Yes (13) | – | Negative |
| 36. | Vivanti A et al 29 | 1 | 4,7 | Irritability, poor feeding, axial hypertonia and opisthotonos | Yes (1) | – | +ve |
| 37. | Li N et al 66 | 17 | 9.6±0.5, 10 | – | – | – | |
| 38. | Cao D et al 67 | 11 | 8–9, 10 | – | – | – | |
| 39. | Hu X et al 42 | 7 | 7–8, 8-9 | – | – | – | |
| 40. | Yang P et al 81 | 7 | 8–9,9-10 | Vomiting (1), RD (2), moaning (2) | Yes (5) | – | Negative |
| 41. | Yang H et al 73 | 13 | 9, 10 | Fever (1) | – | – | |
| 42. | Patane L et al 39 | 2 | 9, 10 | Mild feeding difficulty (2) | Yes (1) | – | +ve |
| 43. | Ferrazzi E et al 28 | 42 | <7 (2) | Gastrointestinal symptoms, RD (2) | Yes (3) | – | +ve |
| 44. | Govind A et al 61 | 9 | <7 (2) | NNP (1) | Yes (1) | – | +ve |
| 45. | Nie R et al 68 | 28 | 8–10, 10 | Pulmonary infection (1) | Yes (1) | – | +ve |
| 46. | Yin M et al 46 | 17 | 8, 9 | – | – | – | |
| 47. | Dória M et al 71 | 10 | 9, 10 | – | – | – | |
| 48. | Perrone S et al 72 | 4 | 9, 10 | – | – | – | |
| 49. | Romagano M et al 82 | 7 | 1–7, 4–9 | RD | Yes (7) | – | Negative |
| 50. | Cooke W et al 83 | 2 | 1–6, 3–8 | Bowel perforation D6 (1) | Yes (2) | – | Negative |
| 51. | Lowe B et al 62 | 1 | 9, 9 | – | – | – | |
| 52. | Blauvelt C et al 84 | 1 | 4, 8 | RD | Yes (1) | – | Negative |
| 53. | Kirtsman M et al 35 | 1 | 9,9 | Neutropenia, hypothermia, feeding difficulties, hypoglycaemic | Yes (1) | – | +ve |
| 54. | Lyra J et al 74 | 1 | 8, 9 | – | – | – | Negative |
| 55. | Groß R et al 52 | 2 | – | Respiratory symptoms (2), icterus (1) | – | – | +ve |
| 56. | Kulkarni et al 117 | 1 | 6, 9 | Fever, icterus and poor feeding | Yes (1) | – | +ve |
| 57. | Sisman J et al 70 | 1 | 7, 9 | Fever, RD, icterus | Yes (1) | – | +ve |
RD, Respiratory distress; MAS, Meconium aspiration syndrome; TTN, Transient Tachypnea of Newborn; NNP, Neonatal Pneumonia.
Congenital anomaly
We could not find any studies describing structural anomalies in the foetus associated with COVID-19. Due to an evolving pandemic, the teratogenicity of the virus has not yet been explored adequately. However, in few of the studies, the findings of anomaly scans during pregnancy were included and they did not show any difference between foetuses of SARS-CoV-2 positive and negative women.46 57 In two case reports, a multicystic dysplastic kidney was detected by antenatal ultrasound in one and after delivery in the other.36 59 In another study bilateral gliosis of the deep white periventricular and subcortical matter was detected in an 11 days old neonate born to SARS-CoV-2 positive mother by MRI.29 However, these cannot be attributed to SARS-CoV-2. Furthermore, autopsy finding in a stillborn baby born to COVID-19 mother did not show any abnormality in another report.40
Discussion and conclusion
We wanted to analyse the published evidence on the foetal perspective of COVID-19 infection concerning mother to child transmission, perinatal outcome and congenital anomalies through a systematic review.
The present available data do not provide a clear conclusion into the foetal outcomes and its clinical implications. Few other reviews have explored the evidence of vertical transmission. There is varied positivity rate of different samples. The positivity of NP swab in this study is 3.67% which is in accordance with other reviews reporting 3.2% (22/936), 2% (9/493) and 3.48% (3/86), respectively.89–91 In a couple of other reviews, however, the NP samples were negative ((0/113) and (0/9)).92 93 No evidence of vertical transmission was found in other reviews.2 94 95
The placental sample was positive in our review in 11.7% of pregnancies. It is similar to the review by Kotlyar et al reporting 9.7% (3/31) sample positivity.89 The placenta was extensively studied in another review where it was shown that there is a low likelihood of placental infection and vertical transmission of SARS-CoV-2 since the receptors and proteases, are only minimally expressed by the human placenta throughout pregnancy.96 Placenta was also negative for 54 samples in another review.90
Amniotic fluid collected before the rupture of membranes was positive in 6.8% of pregnancies in our review, in contrast to the review by Kotlyar et al (0/51) and Ashraf et al (1/16).89 91
The serological analysis was found in some studies within our review showing IgM positive results at birth indicating possible congenital transmission. Using the criteria by Shah et al, we found that there is confirmed congenital transmission in five live-born neonates and two DCDA twins expelled at 24 weeks.14. Similarly, the possible congenital transmission was found in five neonates and probable in two neonates. These analyses were not reported in earlier reviews involving more than 1300 pregnancies in total.
The chance for CS is more in women with COVID-19 and in most instances for maternal indications. Preterm delivery is also high (26.4%) most commonly due to adverse maternal condition, although spontaneous preterm labour is low (1.8%). This is in accordance with another systematic review with regards to the indication but they found a trend towards spontaneous preterm labour.97 In contrast, an earlier review reported 6.4% of preterm deliveries as spontaneous.98
FD (6.63%) was the most common complication seen in the foetus followed by PROM and PPROM (4.27%) in our review. Similar findings were seen in other reviews.91 94 One earlier review did not report any foetal complications.92 PPROM was reported in 14 pregnancies in our review. While PROM and PPROM are unlikely to contribute to mother to child transmission as the SARS-CoV-2 has not been positive in the vaginal swab, PPROM is a significant cause of preterm labour. Through our review, it was not possible to ascertain whether COVID-19 in mothers increases the risk for PROM. IUGR was reported in 12 foetuses in 5 studies (0.9%). IUGR can be multifactorial and need to be analysed with the presence of maternal risk factors. SARS-CoV-2 has not been associated with IUGR and it was not possible to ascertain whether COVID-19 in mother increases the risk for IUGR in our study.
The rates of stillbirth and neonatal death in our study were 9.9 and 5.46, respectively. In another study, it was found that stillbirth was significantly higher during the pandemic compared with the non-pandemic period due to reasons non-associated with COVID-19 (difference, 6.93 (95% CI 1.83 to 12.0) per 1000 births; p=0.01).99 So it is unlikely that the stillbirth and neonatal death rate are increased in COVID-19 mothers. The symptoms when present in the infected neonates were most often mild and neonatal outcomes were found to be good.100 101There is no reported teratogenicity or congenital anomalies associated with SARS-CoV-2 infection. Although maternal parameters were reported in previous studies, maternal outcomes were not included in our review.102–115
The outcome so far is favourable for the foetus despite the risks to the mother for ICU admissions and mechanical ventilation seen in other studies.3 116 There is no significant increase in preterm birth but there is a significantly increased risk of CS in mothers with COVID-19.
Though the foetal perspective seems good in the case of maternal COVID-19, it will be reasonable to consider these findings with caution. Prospective studies and randomised control trials were missing from the evidence due to the recent nature of the infection. Therefore, larger and better quality studies are required to address the knowledge gaps and to reach at a definite guideline for management.
There are many strengths to this study. The studies included in the review contained only confirmed maternal cases by RT-PCR and not the suspected cases or clinically diagnosed cases. The studies contained the results of neonatal testing. Studies included in this review were from countries across the world and not restricted to a specific region, making the findings from the study globally applicable. The case series/cohorts were chosen only when the total number of cases was more than four. Moreover, various aspects of vertical transmission as well as foetal and neonatal outcomes were analysed from the chosen studies.
Nonetheless, there are many limitations to our study. Only a limited number of available case series and cohorts were included in this review as high-quality evidence involving a higher number of subjects is lacking dues to the new kind of infection and still evolving nature of the pandemic. In our review, studies in languages other than English were excluded due to unavailability of English translation. Almost all of the reports are retrospective reviews showing incomplete data with significant heterogeneity within the included studies with a chance of selection or recall bias. Different types of samples were used for the diagnosis of SARS-CoV-2 in different studies. Though nasopharyngeal swab was used for diagnosis in most studies, there were different types of kits used. Again the same kit may have different sensitivity and specificity in different types of samples. Universal testing of pregnant women was not done in many studies, resulting in missing foetal and perinatal effects in asymptomatic women. As maternal outcomes were not studied, the effects of the severity of maternal disease on the foetal outcomes could not be looked into.
Future implications
Whether there is an intrauterine infection of the foetus with respect to SARS-CoV-2 needs to be studied. What are the effects of intrauterine infection, whether there is different susceptibility at different stages of pregnancy, and whether susceptibility depends on disease severity in the mother, needs to be explored. Follow-up studies are required to see long-term effects of neonatal infection with SARS-CoV-2.
Supplementary Material
Footnotes
Collaborators: NA.
Contributors: Conception and design of the study: RD, SSK. Acquisition of data: SSK, RD. Analysis and/or interpretation of data: SSK, RD. Drafting the manuscript: RD, SSK. Revising the manuscript critically for important intellectual content: RD, SSK. Approval of the version of the manuscript to be published (the names of all authors must be listed): SSK, RD.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1. Rasmussen SA, Smulian JC, Lednicky JA, et al. . Coronavirus disease 2019 (COVID-19) and pregnancy: what obstetricians need to know. Am J Obstet Gynecol 2020;222:415–26. 10.1016/j.ajog.2020.02.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Muhidin S, Behboodi Moghadam Z, Vizheh M. Analysis of maternal coronavirus infections and neonates born to mothers with 2019-nCoV; a systematic review. Arch Acad Emerg Med 2020;8:e49. [PMC free article] [PubMed] [Google Scholar]
- 3. Ellington S, Strid P, Tong VT, et al. . Characteristics of women of reproductive age with Laboratory-Confirmed SARS-CoV-2 infection by pregnancy status — United States, January 22–June 7, 2020. MMWR Morb Mortal Wkly Rep 2020;69:769–75. 10.15585/mmwr.mm6925a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rajewska A, Mikołajek-Bedner W, Lebdowicz-Knul J, et al. . COVID-19 and pregnancy – where are we now? A review. J Perinat Med 2020;48:428–34. 10.1515/jpm-2020-0132 [DOI] [PubMed] [Google Scholar]
- 5. Woodward A. A pregnant mother infected with the coronavirus gave birth, and her baby tested positive 30 hours later. Available: https://www.businessinsider.com/wuhan-coronavirus-in-infant-born-from-infected-mother-2020-2 [Accessed June 15, 2020].
- 6. Collin J, Byström E, Carnahan A, et al. . Public Health Agency of Sweden’s brief report: pregnant and postpartum women with SARS‐CoV‐2 infection in intensive care in Sweden. Acta Obstet Gynecol Scand 2020;99:819–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rogan SC, Beigi RH. Treatment of viral infections during pregnancy. Clin Perinatol 2019;46:235–56. 10.1016/j.clp.2019.02.009 [DOI] [PubMed] [Google Scholar]
- 8. Racicot K, Mor G. Risks associated with viral infections during pregnancy. J Clin Invest 2017;127:1591–9. 10.1172/JCI87490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lamouroux A, Attie-Bitach T, Martinovic J, et al. . Evidence for and against vertical transmission for severe acute respiratory syndrome coronavirus 2. Am J Obstet Gynecol 2020;223:91.e1–91.e4. 10.1016/j.ajog.2020.04.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Li M, Chen L, Zhang J, et al. . The SARS-CoV-2 receptor ACE2 expression of Maternal-Fetal interface and fetal organs by single-cell transcriptome study. PLoS One 2020;15:e0230295 https://doi.org/ 10.1371/journal.pone.0230295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jing Y, Run-Qian L, Hao-Ran W, et al. . Potential influence of COVID-19/ACE2 on the female reproductive system. Mol Hum Reprod 2020:gaaa030 https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Levy A, Yagil Y, Bursztyn M, Barkalifa R, et al. . Ace2 expression and activity are enhanced during pregnancy. Am J Physiol Regul Integr Comp Physiol 2008;295:R1953–61. 10.1152/ajpregu.90592.2008 [DOI] [PubMed] [Google Scholar]
- 13. Valdés G, Neves LAA, Anton L, et al. . Distribution of Angiotensin-(1-7) and ACE2 in Human Placentas of Normal and Pathological Pregnancies. Placenta 2006;27:200–7. 10.1016/j.placenta.2005.02.015 [DOI] [PubMed] [Google Scholar]
- 14. Shah PS, Diambomba Y, Acharya G, et al. . Classification system and case definition for SARS‐CoV‐2 infection in pregnant women, fetuses, and neonates. Acta Obstet Gynecol Scand 2020;99:565–8. 10.1111/aogs.13870 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wang W, Xu Y, Gao R, et al. . Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–4. 10.1001/jama.2020.3786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Razaz N, Cnattingius S, Persson M, et al. . One-Minute and five-minute Apgar scores and child developmental health at 5 years of age: a population-based cohort study in British Columbia, Canada. BMJ Open 2019;9:e027655 10.1136/bmjopen-2018-027655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Desai D, Chauhan K, Chaudhary S. A study of meconium stained amniotic fluid, its significance and early maternal and neonatal outcome. Int J Reprod Contracept Obstet Gynecol 2013;2:190–3. 10.5455/2320-1770.ijrcog20130616 [DOI] [Google Scholar]
- 18. Ajah LO, Ibekwe PC, Onu FA, et al. . Evaluation of clinical diagnosis of fetal distress and perinatal outcome in a low resource Nigerian setting. J Clin Diagn Res 2016;10:QC08–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Royal College of Obstetricians and Gynaecologists , Published November 1,2002. Available: http://www.rcog.org.uk/womens-health/investigation-and-managementsmall-gestational-age-fetus-green-top-31 [Accessed 9 Oct 2020].
- 20. American College of Obstetricians and Gynecologists Intrauterine growth restriction. practice Bulletin No. 12, 2000, Washington DC. Available: http://www.acog.org [Accessed 9 Oct 2020].
- 21. Abu-Zidan FM, Abbas AK, Hefny AF. Clinical "case series": a concept analysis. Afr Health Sci 2012;12:557–62. [PMC free article] [PubMed] [Google Scholar]
- 22. Murad MH, Sultan S, Haffar S, et al. . Methodological quality and synthesis of case series and case reports. Bmj Ebm 2018;23:60–3. 10.1136/bmjebm-2017-110853 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Knight M, Bunch K, Vousden N, et al. . Characteristics and outcomes of pregnant women hospitalized with confirmed SARS-CoV- 2 infection in the UK: a national cohort study using the UK obstetric surveillance system (UKOSS). BMJ 2020;369:m2107 https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yan J, Guo J, Fan C, et al. . Coronavirus disease 2019 in pregnant women: a report based on 116 cases. Am J Obstet Gynecol 2020;223:111.e1–111.e14. 10.1016/j.ajog.2020.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kayem G, Lecarpentier E, Deruelle P, Alessandrini V, Azria E, et al. . A snapshot of the Covid-19 pandemic among pregnant women in France. Journal of Gynecology Obstetrics and Human Reproduction 2020;49:101826 10.1016/j.jogoh.2020.101826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nayak AH, Kapote DS, Fonseca M, et al. . Impact of the coronavirus infection in pregnancy: a preliminary study of 141 patients. J Obstet Gynecol India 2020;70:256–61 https://doi.org/ 10.1007/s13224-020-01335-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. London V, McLaren R, Atallah F, et al. . The relationship between status at presentation and outcomes among pregnant women with covid-19. Am J Perinatol 2020;37:991–4. 10.1055/s-0040-1712164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ferrazzi E, Frigerio L, Savasi V, et al. . Vaginal delivery in SARS‐CoV‐2‐infected pregnant women in northern Italy: a retrospective analysis. BJOG 2020;127:1116–21 https://doi.org/ 10.1111/1471-0528.16278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Vivanti AJ, Vauloup-Fellous C, Prevot S, et al. . Transplacental transmission of SARS-CoV-2 infection. Nat Commun 2020;11:3572 10.1038/s41467-020-17436-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Zamaniyan M, Ebadi A, Aghajanpoor Mir S, et al. . Preterm delivery, maternal death, and vertical transmission in a pregnant woman with COVID-19 infection [published online ahead of print, 2020 Apr 17]. Prenat Diagn 2020. 10.1002/pd.5713.10.1002/pd.5713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Pulinx B, Kieffer D, Michiels I, et al. . Vertical transmission of SARS-CoV-2 infection and preterm birth. Eur J Clin Microbiol Infect Dis 2020;382 https://doi.org/ 10.1007/s10096-020-03964-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hosier H, Farhadian S, Morotti RA, et al. . First case of placental infection with SARS CoV-2. medRxiv 2020. https://doi.org/ [Google Scholar]
- 33. Baud D, Greub G, Favre G, et al. . Second-Trimester miscarriage in a pregnant woman with SARS-CoV-2 infection. JAMA 2020;323:2198–200. 10.1001/jama.2020.7233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Algarroba GN, Rekawek P, Vahanian SA, et al. . Visualization of SARS-CoV-2 virus invading the human placenta using electron microscopy. Am J Obstet Gynecol 2020;223:275–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Kirtsman M, Diambomba Y, Poutanen S, et al. . Probable congenital SARS-CoV-2 infection in a neonate born to a woman with active SARS-CoV-2 infection. CMAJ 2020;628:E647–E5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shanes ED, Mithal LB, Otero S, et al. . Placental pathology in COVID-19. Am J Clin Pathol 2020;154:23–32. 10.1093/ajcp/aqaa089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Baergen RN, Heller DS. Placental pathology in Covid-19 positive mothers: preliminary findings. Pediatr Dev Pathol 2020;23:177–80. 10.1177/1093526620925569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Mulvey JJ, Magro CM, Ma LX, et al. . Analysis of complement deposition and viral RNA in placentas of COVID-19 patients. Ann Diagn Pathol 2020;46:151530. 10.1016/j.anndiagpath.2020.151530 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Patane L, Morotti D, Giunta MS, et al. . Vertical transmission of COVID-19: SARS-CoV-2 RNA on the fetal side of the placenta in pregnancies with COVID-19 positive mothers and neonates at birth. AJOG-MFM 2020;100145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Lokken EM, Walker CL, Delaney S, et al. . Clinical characteristics of 46 pregnant women with as sars-cov-2 infection in Washington state. Am J Obstet Gynecol 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Zeng L, Xia S, Yuan W, et al. . Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr 2020;174:722–5. 10.1001/jamapediatrics.2020.0878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Hu X, Gao J, Luo X, et al. . Severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) vertical transmission in neonates born to mothers with coronavirus disease 2019 (COVID-19) pneumonia. Obstet Gynecol 2020;136:65–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Peng Z, Wang J, Mo Y, et al. . Unlikely SARS-CoV-2 vertical transmission from mother to child: a case report. J Infect Public Health 2020;13:818–20 https://doi.org/ 10.1016/j.jiph.2020.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Li Y, Zhao R, Zheng S, et al. . Lack of vertical transmission of severe acute respiratory syndrome coronavirus 2, China. Emerg Infect Dis 2020;26:1335–6 https://dx.doi.org/ 10.3201/eid2606.200287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Chen H, Guo J, Wang C, et al. . Clinical characteristics and intrauterine vertical transmission potential of COVID-19 infection in nine pregnant women: a retrospective review of medical records. The Lancet 2020;395:809–15. 10.1016/S0140-6736(20)30360-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Yin M, Zhang L, Deng G, et al. . Severe acute respiratory syndrome coronavirus 2 (SARS CoV-2) infection during pregnancy in China: a retrospective cohort study. medRxiv 2020. [Google Scholar]
- 47. Wu Y, Liu C, Dong L, et al. . Coronavirus disease 2019 among pregnant Chinese women: case series data on the safety of vaginal birth and breastfeeding. BJOG: Int J Obstet Gy 2020;127:1109–15. 10.1111/1471-0528.16276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Fan C, Lei D, Fang C, et al. . Perinatal transmission of COVID-19 associated SARS-CoV-2: should we worry? Clin Infect Dis 2020:ciaa226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Song L, Xiao W, Ling K, et al. . Anesthetic management for emergent cesarean delivery in a parturient with recent diagnosis of coronavirus disease 2019 (COVID-19): a case report. Transl Perioper & Pain Med 2020;7:234–7. [Google Scholar]
- 50. Xiong X, Wei H, Zhang Z, et al. . Vaginal delivery report of a healthy neonate born to a convalescent mother with COVID19. J Med Virol 2020. 10.1002/jmv.25857.10.1002/jmv.25857. [E-pub ahead of print].. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Wang S, Guo L, Chen L, et al. . A case report of neonatal 2019 coronavirus disease in China. Clin Infect Dis 2020;71:853–7. 10.1093/cid/ciaa225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Groß R, Conzelmann C, Müller JA, et al. . Detection of SARS-CoV-2 in human breastmilk. The Lancet 2020;395:1757–8. 10.1016/S0140-6736(20)31181-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Buonsenso D, Costa S, Sanguinetti M, et al. . Neonatal late onset infection with severe acute respiratory syndrome coronavirus 2. Am J Perinatol 2020;37:869–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Zeng H, Xu C, Fan J, et al. . Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA 2020;323:1848–9. 10.1001/jama.2020.4861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Dong L, Tian J, He S, et al. . Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA 2020;323:1846–8. 10.1001/jama.2020.4621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Liu W, Wang Q, Zhang Q, et al. . Coronavirus disease 2019 (COVID-19) during pregnancy: a case series.. Preprints 2020:2020020373. [Google Scholar]
- 57. Zhu H, Wang L, Fang C, et al. . Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl Pediatr 2020;9:51–60. 10.21037/tp.2020.02.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Chen Y, Peng H, Wang L, et al. . Infants born to mothers with a new coronavirus (COVID-19). Front. Pediatr. 2020;8:104 10.3389/fped.2020.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Breslin N, Baptiste C, Gyamfi-Bannerman C, et al. . Coronavirus disease 2019 infection among asymptomatic and symptomatic pregnant women: two weeks of confirmed presentations to an affiliated pair of new York City hospitals. American Journal of Obstetrics & Gynecology MFM 2020;2:100118 10.1016/j.ajogmf.2020.100118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Prabhu M, Cagino K, Matthews KC, et al. . Pregnancy and postpartum outcomes in a universally tested population for SARS‐CoV‐2 in New York City: a prospective cohort study. BJOG 2020;00:1–9 https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Govind A, Essien S, Karthikeyan A, et al. . Re: novel coronavirus COVID-19 in late pregnancy: outcomes of first nine cases in an inner City London Hospital. Eur J Obstet Gynecol Reprod Biol 2020;251:272–4. 10.1016/j.ejogrb.2020.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Lowe B, Bopp B. COVID‐19 vaginal delivery – a case report. Aust N Z J Obstet Gynaecol 2020;60:465–6 https://doi.org/ 10.1111/ajo.13173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Pierce-Williams RAM, Burd J, Felder L, et al. . Clinical course of severe and critical COVID-19 in hospitalized pregnancies: a US cohort study. Am J Obstet Gynecol MFM 2020;100134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Khan S, Jun L, Siddique R, et al. . Association of COVID-19 with pregnancy outcomes in health-care workers and general women. Clinical Microbiology and Infection 2020;26:788–90. 10.1016/j.cmi.2020.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Martínez-Perez O, Vouga M, Cruz Melguizo S, et al. . Association between mode of delivery among pregnant women with COVID-19 and maternal and neonatal outcomes in Spain. JAMA 2020;324:296 https://doi.org/ 10.1001/jama.2020.10125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Li N, Han L, Peng M, et al. . Maternal and neonatal outcomes of pregnant women with COVID-19 pneumonia: a case-control study. Clinical Infectious Diseases 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Cao D, Yin H, Chen J, et al. . Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: a retrospective study. International Journal of Infectious Diseases 2020;95:294–300 https://doi.org/ 10.1016/j.ijid.2020.04.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Nie R, Wang S, Qiong Y, et al. . Clinical features and the maternal and neonatal outcomes of pregnant women with coronavirus disease 2019. medRxiv 2020. https://doi.org/ [Google Scholar]
- 69. Liu Y, Chen H, Tang K, et al. . Withdrawn: clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. Journal of Infection 2020. Online ahead of print 10.1016/j.jinf.2020.02.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Sisman J, Jaleel M, Moreno W, et al. . Intrauterine transmission of SARS-CoV-2 infection in a preterm infant. Pediatr Infect Dis J 2020;002815 https://doi.org/ [DOI] [PubMed] [Google Scholar]
- 71. Dória M, Peixinho C, Laranjo M, et al. . Covid-19 during pregnancy: a case series from an universally tested population from the North of Portugal. Eur J Obstet Gynecol Reprod Biol 2020;250:261–2. 10.1016/j.ejogrb.2020.05.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Perrone S, Deolmi M, Giordano M, et al. . Report of a series of healthy term newborns from convalescent mothers with COVID-19. Acta Bio Med [Internet] 2020;91:251–5 https://mattioli1885journals.com/index.php/actabiomedica/article/view/9743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. yang H, Sun G, Tang F, et al. . Clinical features and outcomes of pregnant women suspected of coronavirus disease 2019. Journal of Infection 2020;81:e40–4. 10.1016/j.jinf.2020.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Lyra J, Valente R, Rosário M, et al. . Cesarean section in a pregnant woman with COVID-19: first case in Portugal. Acta Med Port 2020;33:429–31 10.20344/amp.13883 10.20344/amp.13883 [DOI] [PubMed] [Google Scholar]
- 75. Hantoushzadeh S, Shamshirsaz AA, Aleyasin A, et al. . Maternal death due to COVID-19. Am J Obstet Gynecol 2020;223:109.e1–109.e16. 10.1016/j.ajog.2020.04.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Gidlöf S, Savchenko J, Brune T, et al. . COVID‐19 in pregnancy with comorbidities: more liberal testing strategy is needed. Acta Obstet Gynecol Scand 2020;99:948–9. 10.1111/aogs.13862 [DOI] [PubMed] [Google Scholar]
- 77. Wang X, Zhou Z, Zhang J, et al. . A case of 2019 novel coronavirus in a pregnant woman with preterm delivery. Clin Infect Dis 2020;71:844–6. 10.1093/cid/ciaa200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Alzamora MC, Paredes T, Caceres D, et al. . Severe COVID-19 during pregnancy and possible vertical transmission. Am J Perinatol 2020;37:861–5. 10.1055/s-0040-1710050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Kalafat E, Yaprak E, Cinar G, et al. . Lung ultrasound and computed tomographic findings in pregnant woman with COVID‐19. Ultrasound Obstet Gynecol 2020;55:835–7 https://doi.org/ 10.1002/uog.22034 [DOI] [PubMed] [Google Scholar]
- 80. Lee DH, Lee J, Kim E, et al. . Emergency cesarean section on severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) confirmed patient. Korean J Anesthesiol 2020;73:347–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Yang P, Wang X, Liu P, et al. . Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. Journal of Clinical Virology 2020;127:104356 10.1016/j.jcv.2020.104356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Romagano MP, Guerrero K, Spillane N, et al. . Perinatal outcomes in critically ill pregnant women with covid-19. Am J Obstetr Gynecol MFM 2020;100151 https://doi.org/ [Google Scholar]
- 83. Cooke WR, Billett A, Gleeson S, et al. . SARS-CoV-2 infection in very preterm pregnancy: experiences from two cases. Eur J Obstet Gynecol Reprod Biol 2020;250:259–60. 10.1016/j.ejogrb.2020.05.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Blauvelt CA, Chiu C, Donovan AL, et al. . Acute respiratory distress syndrome in a preterm pregnant patient with coronavirus disease 2019 (COVID-19). Obstet Gynecol 2020;136:46–51. [DOI] [PubMed] [Google Scholar]
- 85. Khan S, Peng L, Siddique R, et al. . Impact of COVID-19 infection on pregnancy outcomes and the risk of maternal-to-neonatal intrapartum transmission of COVID-19 during natural birth. Infect. Control Hosp. Epidemiol. 2020;41:748–50. 10.1017/ice.2020.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Huang J-W, Zhou X-Y, Lu S-J, et al. . Dialectical behavior therapy-based psychological intervention for woman in late pregnancy and early postpartum suffering from COVID-19: a case report. J Zhejiang Univ Sci B 2020;21:394–9. 10.1631/jzus.B2010012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Zambrano LI, Fuentes-Barahona IC, Bejarano-Torres DA, et al. . A pregnant woman with COVID-19 in central America. Travel Med Infect Dis 2020;36:101639 Online ahead of print 10.1016/j.tmaid.2020.101639 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. González Romero D, Ocampo Pérez J, González Bautista L, et al. . Pronóstico perinatal Y de la paciente embarazada Con infección POR COVID-19. Rev Clin Esp 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89. Kotlyar A, Grechukhina O, Chen A, et al. . Vertical transmission of COVID-19: a systematic review and meta-analysis. American Journal of Obstetrics and Gynecology 2020:S0002–9378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90. Lopes de Sousa Álvaro Francisco, Carvalho HEFde, Oliveira LBde, Lopes de Sousa AF, Félix de Carvalho HE, Braz de Oliveira L, et al. . Effects of COVID-19 infection during pregnancy and neonatal prognosis: what is the evidence? Int J Environ Res Public Health 2020;17:4176 Available at www.mdpi.com/journal/ijerph 10.3390/ijerph17114176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Ashraf MA, Keshavarz P, Hosseinpour P, et al. . Coronavirus disease 2019 (COVID-19): a systematic review of pregnancy and the possibility of vertical transmission. J Reprod Infertil 2020;21:157–68. [PMC free article] [PubMed] [Google Scholar]
- 92. Juan J, Gil MM, Rong Z, et al. . Effect of coronavirus disease 2019 (COVID‐19) on maternal, perinatal and neonatal outcome: systematic review. Ultrasound Obstet Gynecol 2020;56:15–27. 10.1002/uog.22088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Irani M, Pakfetrat A, Mask MK, et al. . And perinatal outcomes. J Edu Health Promot 2019;2020:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Akhtar H, Patel C, Abuelgasim E, et al. . COVID-19 (SARS-CoV-2) infection in pregnancy: a systematic review. Gynecol Obstet Invest 2020;85:295–306. 10.1159/000509290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Karimi-Zarchi M, Neamatzadeh H, Dastgheib SA, et al. . Vertical transmission of coronavirus disease 19 (COVID-19) from infected pregnant mothers to neonates: a review, fetal and pediatric pathology 2020;39:246–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Pique-Regi R, Romero R, Tarca AL, et al. . Does the human placenta express the canonical cell entry mediators for SARS-CoV-2? eLife 2020;9:e58716 10.7554/eLife.58716 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Della Gatta AN, Rizzo R, Pilu G, et al. . Coronavirus disease 2019 during pregnancy: a systematic review of reported cases. Am J Obstet Gynecol 2020;223:36–41. 10.1016/j.ajog.2020.04.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Huntley BJF, Huntley ES, Di Mascio D, et al. . Rates of maternal and perinatal mortality and vertical transmission in pregnancies complicated by severe acute respiratory syndrome coronavirus 2 (SARS-Co-V-2) infection. Obstet Gynecol 2020;136:303–12. 10.1097/AOG.0000000000004010 [DOI] [PubMed] [Google Scholar]
- 99. Khalil A, von Dadelszen P, Draycott T, et al. . Change in the incidence of stillbirth and preterm delivery during the COVID-19 pandemic. JAMA 2020;324:705–6. 10.1001/jama.2020.12746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Wei M, Yuan J, Liu Y, et al. . Novel coronavirus infection in hospitalized infants under 1 year of age in China. JAMA 2020;323:1313–4. 10.1001/jama.2020.2131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Dumpa V, Kamity R, Vinci AN, et al. . Neonatal coronavirus 2019 (COVID-19) infection: a case report and review of literature. Cureus 2020;12:e8165. 10.7759/cureus.8165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Zhang I, Jiang Y, Wei M, et al. . Analysis of the pregnancy outcomes in pregnant women with COVID-19 in Hubei Province [in Chinese]. Zhonghua Fu Chan Ke Za Zhi 2020;55:166–71. [DOI] [PubMed] [Google Scholar]
- 103. Penfield CA, Brubaker SG, Limaye MA, et al. . Detection of SARS-CoV-2 in placental and fetal membrane samples. Am J Obstet Gynecol MFM 2020;2:100133 https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Chen S, Chen S, Huang B, et al. . Pregnant women with new coronavirus infection: a clinical characteristics and placental pathological analysis of three cases. Zhonghua Bing Li Xue Za Zhi 2020;49:418–23. [DOI] [PubMed] [Google Scholar]
- 105. Iqbal SN, Overcash R, Mokhtari N, et al. . An uncomplicated delivery in a patient with Covid-19 in the United States. N Engl J Med 2020;382:e34. 10.1056/NEJMc2007605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Liao X, Yang H, Kong J, et al. . Chest CT findings in a pregnant patient with 2019 novel coronavirus disease. Balkan Med J 2020;37:226–8. 10.4274/balkanmedj.galenos.2020.2020.3.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Qiancheng X, Jian S, Lingling P, et al. . Sixth batch of Anhui medical team Aiding Wuhan for COVID-19. coronavirus disease 2019 in pregnancy. Int J Infect Dis 2020;95:376–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108. Yu N, Li W, Kang Q, et al. . No SARS-CoV-2 detected in amniotic fluid in mid-pregnancy. Lancet Infect Dis 2020:S1473–3099. 10.1016/S1473-3099(20)30320-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109. Savasi VM, Parisi F, Patanè L, et al. . Clinical findings and disease severity in hospitalized pregnant women with coronavirus disease 2019 (covid-19). Obstet Gynecol 2020;136:252–8. 10.1097/AOG.0000000000003979 [DOI] [PubMed] [Google Scholar]
- 110. Schnettler WT, Al Ahwel Y, Suhag A. Severe acute respiratory distress syndrome in coronavirus disease 2019–infected pregnancy: obstetric and intensive care considerations. AJOG-MFM 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Lang G-J, Zhao H. Can SARS-CoV-2-infected women breastfeed after viral clearance? J Zhejiang Univ Sci B 2020;21:405–7. 10.1631/jzus.B2000095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Buonsenso D, Raffaelli F, Tamburrini E, et al. . Clinical role of lung ultrasound for the diagnosis and monitoring of COVID19 pneumonia in pregnant women [published online ahead of print, 2020 Apr 26]. Ultrasound Obstet Gynecol 2020. 10.1002/uog.22055.10.1002/uog.22055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Vintzileos WS, Muscat J, Hoffmann E, et al. . Screening all pregnant women admitted to labor and delivery for the virus responsible for coronavirus disease 2019. Am J Obstet Gynecol 2020;223:284–6. 10.1016/j.ajog.2020.04.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Breslin N, Baptiste C, Miller R, et al. . COVID-19 in pregnancy: early lessons. Am J Obstet Gynecol MFM 2020;2:100111 https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Qadri F, Mariona F. Pregnancy affected by SARS-CoV-2 infection: a flash report from Michigan. J Matern Fetal Neonatal Med 2020;13:1–3. 10.1080/14767058.2020.1765334 [DOI] [PubMed] [Google Scholar]
- 116. Sentilhes L, De Marcillac F, Jouffrieau C, et al. . Coronavirus disease 2019 in pregnancy was associated with maternal morbidity and preterm birth. Am J Obstet Gynecol 2020. 10.1016/j.ajog.2020.06.022. [Epub ahead of print: 15 Jun 2020]. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Kulkarni R, Rajput U, Dawre R, et al. . Early-Onset symptomatic neonatal COVID-19 infection with high probability of vertical transmission. Infection 2020. 10.1007/s15010-020-01493-6. [Epub ahead of print: 02 Aug 2020] https://doi.org/ [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjpo-2020-000859supp001.pdf (150KB, pdf)