Abstract
Background
The reverse total shoulder arthroplasty has become the most common method of arthroplasty of the shoulder. The complication of acromial or scapular stress fracture deserves consideration to describe incidence and determine whether prosthetic design or patient factors act as risk factors.
Methods
A systematic review of the literature was performed including the EMBASE, Medline and the Cochrane Library in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.
Results
The search returned 565 articles. After exclusion, 25 papers remained. In total, 208 fractures were reported in the literature, with an overall incidence of 5% and stress fractures were more common than post-traumatic ones; 24 fractures underwent osteosynthesis and there were nine revision arthroplasty surgeries. Outcomes worsened after fracture – whether treated with surgery or not. In patients with scapular base fractures, there was an improvement in functional outcome scores after surgery. Heterogeneous reporting of the risk factors prior to fractures, treatment methods and outcomes made recommendations weak.
Discussion
Acromial stress fracture after reverse total shoulder arthroplasty occurs relatively commonly but is poorly reported in the literature. It is unclear whether immobilisation, fixation or revision arthroplasty is the best treatment, although fixation may offer a better outcome. In future, reports should aim for greater consistency to allow a better understanding of this condition.
Keywords: acromial, fracture, complication, reverse shoulder arthroplasty, stress, fatigue
Introduction
The reliable treatment of cuff tear arthropathy (CTA) with a reversed prosthesis was first proposed by Grammont in 1987.1 The reversed configuration allowed for alterations in the biomechanics of the cuff-deficient shoulder to provide greater function and pain relief. The changed centre of rotation increased the tension placed onto the deltoid to allow recruitment of more muscle fibres for abduction and elevation.2,3 Since its implementation, reverse total shoulder arthroplasty (RTSA) has become a mainstay in the treatment of CTA. Despite its popularity, complications exist. Farshad and Gerber published a review, ranking complications from most to least common and these included scapular notching (most common), haematoma formation, infection, instability and acromial fracture.3 Furthermore, Zumstein et al. published a systematic review of all complications related to RTSA. In this paper, post-operative fractures of the scapula or acromion were identified as a rare occurrence with 12 instances (incidence of 1.5%) in the literature, and treatment was either conservative or osteosynthesis.2 Given the diversity of literature regarding fractures of the acromion and scapular spine after RTSA, the goals of this study were to explore the aetiology of acromial fracture, risk factors and fracture patterns in greater detail. Before commencing our literature review, we established a study protocol with specific objectives and questions. These included:
To perform a systematic review of the literature to investigate the natural history of acromial stress fracture and evaluate treatment options.
What is the incidence and epidemiology surrounding acromial stress fracture and can fracture risk factors be identified?
What classification systems for this fracture exist and how do they compare to each other?
What is the incidence of fracture in different prosthetic design and what are other significant surgical factors?
What are the clinical outcomes in conservative versus operative treatment of fracture patterns and can guidelines be developed to help surgeons in the management of each type of fracture?
What is the effect of fracture on validated outcomes scores in RTSA in both operative and non-operative groups?
Can guidance be provided to future publishers via a minimum data set to allow for further analysis and development of stronger recommendations for treatment?
Materials and methods
A systematic review of the English language literature was performed. The search included the EMBASE, Medline and NHS Evidence Information for Health databases, as well as the Cochrane Library in April 2017. A search strategy was carried out using the recommendations from the Cochrane Collaboration, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses and the Meta-Analysis of Observational Studies in Epidemiology.4 Search terms were shoulder, reverse, arthroplasty, prosthesis, fracture, insufficiency, stress, complications, acromial (and derivatives) and scapula. General search terms were employed to ensure maximum sensitivity of the search strategy. Cross matching of the references in all relevant studies was performed to include as many ‘relevant’ articles as possible.
Selection and exclusion bias
To ensure the maximum amount of homogeneity in our studies – which were all case series – a rigorous set of selection and exclusion criteria were employed. Inclusion criteria were any study specifically reporting on acromial fracture after RTSA. In the final selection, this included both papers which were case series of post-operative stress fracture as well as larger case series of RTSA in which fracture was one of any number of documented complications. We also included any study where acromial or scapula fracture (whether stress/insufficiency or traumatic) was noted as one of any number of complications post-RTSA. This review was restricted to the English language literature. Furthermore, only original research articles were included. Exclusion criteria included case reports, conference presentations, editorials, reviews and expert opinion.
Quality assessment
Two independent reviewers (SL and RL) assessed the articles to determine appropriateness for inclusion. Because quality scoring in systematic reviews and meta-analyses of observational studies can be controversial, each article was individually reviewed using the Strengthening the Reporting of Observational Studies in Epidemiology checklist.5 This was used to appraise the quality of included articles. Demographic data extracted included study design, level of evidence, number of fractures and incidence, patient demographics and the history and aetiology of acromial fracture. Intra-operative data included choice of prosthesis, surgical approach and if acromial osteosynthesis was performed. Post-operative functional outcome data were extracted including range of motion, overall post-surgical satisfaction, pain scores and functional outcomes scores such as the Simple Shoulder Test (SST) and American Shoulder and Elbow Society (ASES) scores. Any additional information such as radiological method of diagnosis and classification system used was also included in the study.
Statistical analysis
In this study, we employed both fixed- and random-effects models where there was sufficient data to perform meta-analyses. The fixed-effects model assumed the same treatment effects per study whereas it was assumed to fluctuate in random-effects models. Differences between studies was estimated using a Tau2 statistic, with values >50% considered significant heterogeneity. In this paper, we presented the results using a random-effects model to try and present the variations in patients and study methodology. A meta-regression analysis was also performed using implant type as a moderator to assess for variance in risk factors. Given the spectrum of search categories and challenges of investigating a complication of surgical intervention in the reported literature, we performed an Egger Assessment of bias and an inspection of funnel plot for asymmetry to examine for publication bias. The meta-analysis was performed using Meta-analysis v3 (Biostat Inc., Englewood, NJ) whilst STATA v15 (StataCorp, College Station, TX) was used for the meta-regression analysis.
Results
Question 1: literature review and search strategy
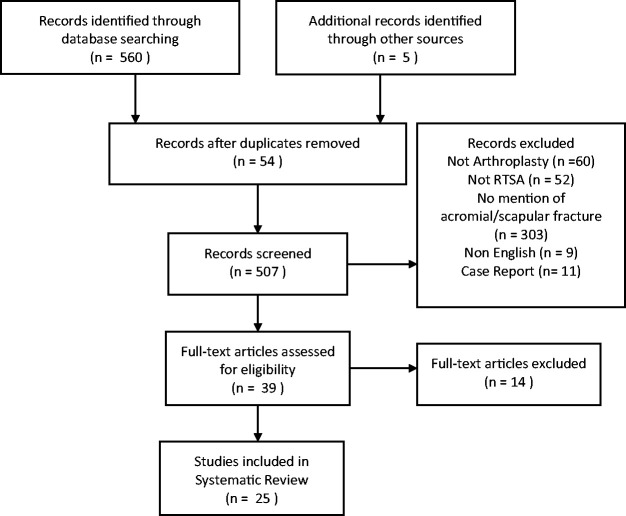
Our search strategy yielded 565 articles, of which 54 were removed as duplicate articles. This left a total cohort of 507 articles. The abstracts of each article were reviewed, and papers eliminated where they contained no relevance to acromial fracture after RTSA. Reasons included the absence of any arthroplasty (60), the absence of reverse shoulder arthroplasty (52), absence of acromial or scapular fracture (303), single case reports (9) and non-English articles (11). The remaining 39 articles were reviewed in full and a further 14 were eliminated based on the same criteria. Systematic reviews, biomechanical studies and basic sciences papers were also eliminated. This yielded a final cohort of 25 papers. Our search strategy is shown in Figure 1.
Figure 1.
Search strategy. RTSA: reverse total shoulder arthroplasty.
Question 2: incidence and epidemiology
Study design, level of evidence, number of cases and number of patients, timing of fracture, age and gender were recorded. In total, 208 acromial or scapular fractures were reported within 4456 RTSAs, which gives an overall incidence of 5%. Regarding aetiology, there were 73 cases of incidental, fatigue or stress fracture noted, and 14 as a result of direct trauma such as a fall, although in the remaining 124 cases (62%), no specific aetiology was reported. The 38% of fractures with specified aetiology were compared using random-effects analysis. This showed a point estimate of 0.038 (95% confidence interval (CI) 0.025–0.055) for stress fracture and 0.009 (95% CI 0.005–0.017) for traumatic fractures (p = 0.000), signifying that stress fractures were statistically more common than traumatic ones. The majority of fractures were seen in women with a mean age of 73.8 years at a mean time post-operatively of 12.7 months. These are summarised in Table 1.
Table 1.
| First author | Year | Level of evidence | No. of fractures | No. of patients | Incidence (%) | Aetiology |
Timing of fracture (months) | Age | Gender |
||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Stress | Trauma | F | M | ||||||||
| Otto13 | 2013 | IV | 53 | 212 | 25 | NS | NS | 15.2 | 75 | 43 | 10 |
| Teusink10 | 2014 | IV | 25 | 1018 | 2.5 | NS | NS | 16 | 72.2 | 21 | 4 |
| Crosby6 | 2011 | IV | 22 | 400 | 5.5 | 17 | 5 | 10.7 | 71.1 | 16 | 6 |
| Levy8 | 2013 | IV | 16 | 157 | 10.2 | 16 | 0 | 3 | 77 | 13 | 3 |
| Dubrow14 | 2014 | IV | 14 | 125 | 11.2 | all | 0 | 5.1 | 72.1 | 12 | 2 |
| Kurowicki15 | 2016 | IV | 9 | 72 | 12.5 | NS | NS | NS | 76 | NS | NS |
| Kennon11 | 2017 | IV | 9 | 318 | 2.8 | NS | NS | 17 | 70 | 6 | 3 |
| Hattrup30 | 2010 | IV | 9 | 125 | 7.2 | 4 | 5 | 10 | 76 | 8 | 1 |
| Hamid7 | 2011 | IV | 8 | 173 | 4.6 | 6 | 2 | 34.4 | 76.3 | 8 | 0 |
| Wahlquist12 | 2011 | IV | 5 | 97 | 5.2 | 5 | 0 | 8.4 | 74.2 | 4 | 1 |
| Mollon17 | 2016 | IV | 5 | 297 | 1.7 | 5 | 0 | NS | NS | NS | NS |
| Mellano18 | 2017 | IV | 5 | 100 | 5 | NS | NS | NS | NS | NS | NS |
| Werner19 | 2005 | IV | 4 | 58 | 6.9 | 4 | 0 | NS | NS | NS | NS |
| Walch9 | 2009 | IV | 4 | 457 | 0.9 | 3 | 1 | 7 | 72.3 | NS | NS |
| Saltzman20 | 2014 | IV | 4 | 137 | 2.9 | 4 | 0 | NS | NS | NS | NS |
| Greiner16 | 2015 | I | 4 | 34 | 11.8 | NS | NS | NS | NS | NS | NS |
| Shafritz21 | 2012 | IV | 3 | 41 | 7.3 | 3 | 0 | NS | NS | NS | NS |
| Boileau22 | 2005 | IV | 2 | 45 | 4.4 | 2 | 0 | 3 | NS | NS | NS |
| von Engelhardt23 | 2015 | IV | 1 | 67 | 1.5 | NS | NS | NS | NS | NS | NS |
| Simovitch24 | 2015 | IV | 1 | 41 | 2.4 | 1 | 0 | 6 | NS | NS | NS |
| Kempton25 | 2011 | IV | 1 | 200 | 0.5 | 1 | 0 | NS | NS | NS | NS |
| Groh26 | 2014 | IV | 1 | 112 | 0.9 | NS | NS | 10 | 71 | 1 | 0 |
| Cuff27 | 2008 | IV | 1 | 96 | 1 | 0 | 1 | 3 | NS | NS | NS |
| Bufquin28 | 2007 | IV | 1 | 43 | 2.3 | 1 | 0 | 12 | NS | NS | NS |
| Atoun29 | 2014 | IV | 1 | 31 | 3.2 | 1 | 0 | 3 | NS | NS | NS |
| Total (mean) | NA | NA | 208 | 4456 | 4.7 | 73 | 14 | 12.7 | 73.8 | 132 | 30 |
F: female; M: male; NA: not applicable; NS: not specified.
Question 3: classification systems
Three classification systems were utilised in the literature to describe 151 acromial fractures. The remainder of our identified articles did not contain a description of the fracture or mention classification types, which accounted for 57 (28%) fractures.
The most popular was the classification system devised by Crosby et al. in 2011, which was used in six papers for a total of 113 stress fractures (75% of all classified fractures).6 No diagrams were provided by the original paper. Fractures were divided into three types based on their anatomical relationship with the acromioclavicular joint (ACJ) – with type I being fractures of the anterior acromion (near or at the footprint of the coracoacromial ligament). Type II fractures were those through the anterior acromion but posterior to the ACJ. Type III fractures involved the posterior acromion or scapular spine. The rationale behind this mechanism was the hypothesis that ACJ arthrosis contributed towards the propagation of type II fractures. Hamid et al. utilised a similar classification system to that of Crosby based on anatomical position at the base, mid-acromial or laterally without formally classifying this.7
The second most popular classification system was that of Levy et al. in 2013, which was utilised in two papers and 25 fractures.8 This was based around the involvement of the deltoid origin. Type I fractures involved bone that gives rise to the anterior and middle deltoid. Type II was associated with giving origin to the entire middle deltoid, whereas type III involved the entire middle and posterior deltoid origin. No papers compared these two classification systems, and neither has been validated in the literature.
Finally, Walch et al. qualified acromial and scapular spine fractures on the degree of inferior angulation of the lateral edge of the acromion on comparative pre- and post-operative anteroposterior radiographs.9 This method was the first classification to be described but only employed in two studies and 13 patients. The most recent paper using this classification was published in 2009.
Question 4: prosthetic design and surgical factors
A deltopectoral approach was utilised in all cases except one where an acromial or scapular spine fracture occurred. A Neviaser–MacKenzie (antero-superior) approach was used in the exception.
A variety of reverse shoulder prostheses were used, although the implant was not specified in 142 cases (68%). In many papers, a number of prostheses were co-reported but when complications occurred these were included without specification of the prosthesis itself. Papers exclusively reporting one implant self-selected and were therefore over-represented.
The most common was the Reverse Shoulder Prosthesis (DJO Surgical, Austin, TX) with 59 cases of post-operative fracture. This equated to an incidence of 15% where the DJO prosthesis was employed – although 25 of these came from a single study.10 This was followed by the Grammont-style reversed implant (Tournier, Edina, MN) with 16 cases (25%), then the Equinoxe (Exactech, Gainesville, FL) with 15 cases (23%), the Delta III by DePuy (Warsaw, IN) with 5 cases (8%), the Aequalis (Tournier, Edina, MN) with 4 cases (6%), the TM Reverse (Zimmer, Warsaw, IN) with 3 cases and a single case each with the Total Evolve Shoulder System (Biomet, Warsaw, IN) and the Verso (Biomet, Warsaw, IN). A mixture of inlay and onlay humeral prostheses were employed, and onlay implants accounted for 72% of fractures. A meta-regression analysis investigating whether prosthetic choice was associated with timing of fracture, age or gender was not possible as insufficient raw data were reported in the 15 papers where prosthesis was specified.
Question 5: treatment options
The majority of acromial or scapular spine fractures were treated non-operatively with some form of sling immobilisation. There were a total of 115 fractures treated this way. There were also reports of bone stimulators being used to encourage bony union. The remainder had no treatment specified.
In total, there were 33 fractures which underwent surgery postacromial fracture. In 24 cases, this was via osteosynthesis – either with tension band wiring or plate and screw fixation or both. There were three documented cases of failed fixation and re-fixation surgery, which equates to a failed fixation rate of 13% when surgery was performed. Success or union rates were infrequently documented.
Nine revision arthroplasty procedures were performed after fracture. In seven instances, the indication was recurrent instability due to loss of deltoid tension from acromial displacement. In the other two, glenoid component loosening after scapular fracture and separately a glenoid component failure in a concurrent Crosby type 1 fracture were the documented indications. Five of the implants undergoing revision were the DJO prosthesis, and another the Exactech Equinoxe. A summary of the operative interventions can be seen in Table 2, and possible mechanisms of failure are included in the Discussion section of this paper.
Table 2.
| First author | Year | Treatment |
||
|---|---|---|---|---|
| Non- operative | TBW/ ORIF | Revision | ||
| Otto13 | 2013 | NS | NS | NS |
| Teusink10 | 2014 | 25 | 0 | 2 |
| Crosby6 | 2011 | 15 | 11 | 2 |
| Levy8 | 2013 | 16 | 0 | 2 |
| Dubrow14 | 2014 | 14 | 0 | 0 |
| Kurowicki15 | 2016 | NS | 0 | 1 |
| Kennon11 | 2017 | 3 | 5 | 1 |
| Hattrup30 | 2010 | 9 | 0 | 1 |
| Hamid7 | 2011 | 8 | 0 | 0 |
| Wahlquist12 | 2011 | 2 | 3 | 0 |
| Mollon17 | 2016 | NS | NS | NS |
| Mellano18 | 2017 | 4 | 1 | 0 |
| Werner19 | 2005 | 2 | 2 | 0 |
| Walch9 | 2009 | 3 | 1 | 0 |
| Saltzman20 | 2014 | NS | NS | NS |
| Greiner16 | 2015 | 4 | 0 | 0 |
| Shafritz21 | 2012 | 3 | 0 | 0 |
| Boileau22 | 2005 | 2 | 0 | 0 |
| von Engelhardt23 | 2015 | 0 | 1 | 0 |
| Simovitch24 | 2015 | 1 | 0 | 0 |
| Kempton25 | 2011 | NS | NS | NS |
| Groh26 | 2014 | 1 | 0 | 0 |
| Cuff27 | 2008 | 1 | 0 | 0 |
| Bufquin28 | 2007 | 1 | 0 | 0 |
| Atoun29 | 2014 | 1 | 0 | 0 |
| Total | 115 | 24 | 9 | |
NS: not specified; ORIF: Open Reduction Internal Fixation; TBW: Tension Band Wire.
Question 6: outcomes after fracture
Patients treated conservatively reported ASES of 64.8. In osteosynthesis patients, the ASES was 80.3. The significant limitations on these two numbers are described below.
The majority of studies included functional outcome score – such as the ASES or SST scores which were favoured by North American authors and the Constant–Murley Score (CMS) by European authors. In other instances, complications or pain post-operatively were the documented outcome. Bony union was rarely commented on. Functional outcomes after non-operative management were reported in depth in six papers. Of the 115 fractures treated non-operatively, only 34 patients had scores separately reported and at a variety of follow-up time periods. Only 6 of 115 non-operatively managed fractures had both their outcome score and fracture location specified. Table 3 summarises this heterogeneous reporting. The mean ASES of these fractures post-operatively was 64.8.
Table 3.
| Patient | Paper | Age | Sex | Pre-operative Dx | Prosthesis | Time to # (months) | Classification | Union? | Other treatment? | Final score | Time of final score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Teusink et al.10 | 79 | M | CTA | DJO | 10 | NS | NS | NS | ASES 48 | >12/12 from #, >24/12 from surgery |
| 2 | Teusink et al.10 | 77 | F | CTA | DJO | 4 | NS | Yes | NS | ASES 47 | >12/12 from #, >24/12 from surgery |
| 3 | Teusink et al.10 | 71 | F | Failed RCR | DJO | 31 | NS | NS | NS | ASES 80 | >12/12 from #, >24/12 from surgery |
| 4 | Teusink et al.10 | 75 | F | CTA | DJO | 3 | NS | Yes | NS | ASES 28 | >12/12 from #, >24/12 from surgery |
| 5 | Teusink et al.10 | 74 | F | CTA | DJO | 3 | NS | NS | NS | ASES 55 | >12/12 from #, >24/12 from surgery |
| 6 | Teusink et al.10 | 65 | M | CTA | DJO | 3 | NS | Yes | NS | ASES 90 | >12/12 from #, >24/12 from surgery |
| 7 | Teusink et al.10 | 70 | F | CTA | DJO | 35 | NS | NS | NS | NS | >12/12 from #, >24/12 from surgery |
| 8 | Teusink et al.10 | 74 | F | CTA | DJO | 3 | NS | NS | NS | ASES 63 | >12/12 from #, >24/12 from surgery |
| 9 | Teusink et al.10 | 81 | F | CTA | DJO | 2 | NS | Yes | NS | ASES 75 | >12/12 from #, >24/12 from surgery |
| 10 | Teusink et al.10 | 64 | M | CTA | DJO | 6 | NS | NS | NS | ASES 60 | >12/12 from #, >24/12 from surgery |
| 11 | Teusink et al.10 | 78 | F | CTA | DJO | 3 | NS | NS | NS | ASES 45 | >12/12 from #, >24/12 from surgery |
| 12 | Teusink et al.10 | 66 | F | Failed hemi | DJO | 4 | NS | NS | NS | ASES 57 | >12/12 from #, >24/12 from surgery |
| 13 | Teusink et al.10 | 56 | F | Failed TSA | DJO | 5 | NS | Yes | NS | ASES 35 | >12/12 from #, >24/12 from surgery |
| 14 | Teusink et al.10 | 62 | F | Failed hemi | DJO | 20 | NS | Yes | NS | ASES 55 | >12/12 from #, >24/12 from surgery |
| 15 | Teusink et al.10 | 83 | F | CTA | DJO | 7 | NS | Yes | NS | ASES 50 | >12/12 from #, >24/12 from surgery |
| 16 | Teusink et al.10 | 82 | F | CTA | DJO | 4 | NS | Yes | NS | ASES 82 | >12/12 from #, >24/12 from surgery |
| 17 | Teusink et al.10 | 65 | F | CTA | DJO | 1 | NS | Yes | NS | ASES 88 | >12/12 from #, >24/12 from surgery |
| 18 | Wahlquist et al.12 | 80 | F | Failed TSR | DePuy | 7 | ‘Base’ | NS | sling, bone stimulator | Neer 66 | 26 |
| 19 | Wahlquist et al.12 | 83 | F | Failed RCR | Zimmer TM | 10 | ‘Base’ | Yes | sling, bone stimulator | Neer 56 | 13 |
| 20 | Hamid et al.7 | 87 | F | NS | NS | 3 | ‘Midacromion’ | No | NS | ASES 98, DASH 20 | NS |
| 21 | Hamid et al.7 | 82 | F | NS | NS | 2 | ‘Midacromion’ | No | NS | ASES 28, DASH 65 | NS |
| 22 | Hamid et al.7 | 87 | F | NS | NS | 38 | ‘Base’ | No | NS | ASES 93, DASH 32 | NS |
| 23 | Hamid et al.7 | 91 | F | NS | NS | 5 | ‘Base’ | Yes (mal) | NS | ASES 24, DASH 77 | NS |
| 24 | Hamid et al.7 | 69 | F | NS | NS | 2 | ‘Base’ | No | NS | ASES 49, DASH 58 | NS |
| 25 | Hamid et al.7 | 63 | F | NS | NS | 48 | ‘Midacromion’ | No | NS | ASES 95, DASH 23 | NS |
| 26 | Hamid et al.7 | 63 | F | NS | NS | 13 | ‘Base’ | No | NS | ASES 73, DASH 58 | NS |
| 27 | Hamid et al.7 | 68 | F | NS | NS | 2 | ‘Lateral’ | No | NS | ASES 97, DASH 5 | NS |
| 28 | Boileau et al.22 | NS | NS | NS | NS | 3 | NS | NS | NS | CMS 69 | NS |
| 29 | Boileau et al.22 | NS | NS | NS | NS | 3 | NS | NS | NS | CMS 77 | NS |
| 30 | Kennon et al.11 | 78 | F | NS | Equinoxe, Exactech | 5 | Crosby III | NS | No | ASES 72, UCLA 28, SST 7, CMS 67 | 60 |
| 31 | Kennon et al.11 | 83 | M | NS | Equinoxe, Exactech | 6 | Crosby III | NS | No | ASES 78, UCLA 28, SST 10, CMS 47 | 48 |
| 32 | Walch et al.9 | NS | NS | Failed hemi | 3 | Walch | No | NS | CMS 15 | 36 | |
| 33 | Walch et al.9 | NS | NS | CTA | 3 | Walch 40° | Yes | NS | CMS 38 | 24 | |
| 34 | Walch et al.9 | CTA | 12 | Walch 55° | NS | NS | CMS 44 | 24 | |||
ASES: American Shoulder and Elbow Society; CMS: Constant–Murley Score; CTA: cuff tear arthropathy; DASH: Disabilities of Arm, Shoulder & Hand; F: female; M: male; NA: not applicable; NS: not specified; RCR: Rotator Cuff Repair; SST: Simple Shoulder Test; TSA: total shoulder arthroplasty; TSR: Total Shoulder Replacement; UCLA: University of California Los Angeles Shoulder Score. #fracture.
However, the summary statistics of ASES of 64.8 in non-operatively treated scapular fractures versus an ASES of 80.3 in operatively treated fractures is supported by only 12 patients from the total cohort of 208. Incomplete and inconsistent reporting made stronger meta-analysis impossible.
Of the 33 treated operatively, only 10 patients were reported with functional outcomes scores. These were patients from three studies, and patients sustained either a Crosby III or scapular ‘base’ fracture.11,12 Only one paper documented any change in functional outcome scores from pre- and post-operatively.11 The ASES was reported in six patients, with a mean score of 80.3. These are summarised in Table 4.
Table 4.
| Patient | Paper | Age | Sex | Pre-operative Dx | Prosthesis | Time to # (months) | Classification | Operative intervention | Time of surgery post-fracture (months) | Union? | Pre-operative score | Final score | Time of final score post-fracture (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Wahlquist et al.12 | 70 | F | Failed RCR | NS (DePuy) | 10 | ‘Base’ | ORIF | 1 | NS | NS | Neer 42 | 12 |
| 2 | Wahlquist et al.12 | 82 | F | CTA | DePuy Delta XTEND | 3 | ‘Base’ | TBW | 9 | NS | NS | Neer 76 | 12 |
| 3 | Wahlquist et al.12 | 65 | M | Failed RCR | Tournier RTSA | 12 | ‘Base’ | ORIF ×2 | 24/30 | Y | NS | Neer 77 | 7 |
| 4 | Kennon et al.11 | 77 | F | NS | Equinoxe, Exactech | 10 | Crosby III | ORIF | NS | NS | ASES 0, UCLA 7, SST 0, CMS 12 | ASES 67, UCLA 26, SST 7, CMS 53 | 36 |
| 5 | Kennon et al.11 | 71 | F | NS | Equinoxe, Exactech | 157 | Crosby III | ORIF | NS | NS | ASES 0, UCLA 6, SST 0, CMS 2 | ASES 95, UCLA 35, SST 11, CMS 94 | 48 |
| 6 | Kennon et al.11 | 69 | F | NS | Equinoxe, Exactech | 58 | Crosby III | ORIF | NS | NS | ASES 10, UCLA 6, SST 0, CMS 13 | ASES 70, UCLA 28, SST 9, CMS 68 | 36 |
| 7 | Kennon et al.11 | 61 | M | NS | Equinoxe, Exactech | 25 | Crosby III | Revision RTSA + ORIF | NS | NS | ASES 0, UCLA 8, SST 0, CMS 10 | ASES 77, UCLA 29, SST 7, CMS 72 | 36 |
| 8 | Kennon et al.11 | 70 | F | NS | Equinoxe, Exactech | 5 | Crosby III | ORIF | NS | NS | ASES 17, UCLA 9, SST 0, CMS 13 | ASES 78, UCLA 27, SST 8, CMS 65 | 36 |
| 9 | Kennon et al.11 | 70 | M | NS | Equinoxe, Exactech | 3 | Crosby III | ORIF | NS | NS | ASES 8, UCLA 10, SST 0, CMS 12 | ASES 95, UCLA 35, SST 11, CMS 86 | 48 |
| 10 | Walch et al.9 | NS | NS | CTA | 10 | Walch 25° | TBW | NS | No – hardware removed | NS | CMS 43 | NS |
ASES: American Shoulder and Elbow Society; CMS: Constant–Murley Score; CTA: cuff tear arthropathy; F: female; M: male; NS: not specified; ORIF: Open Reduction Internal Fixation; RCR: Rotator Cuff Repair; RTSA: reverse total shoulder arthroplasty; SST: Simple Shoulder Test; TBW: Tension Band Wire; UCLA: University of California Los Angeles Shoulder Score.
Discussion
Question 2: incidence, epidemiology and risk factors
This systematic review found an incidence of acromial or scapular spine fracture after RTSA of 5%. Previously, this has been documented between 0.8 to 10.2%.6,31,32 However, the true incidence – particularly of stress or fragility fracture – may be much higher given a tendency towards under-diagnosis. The majority of fractures were diagnosed via plain radiograph, and it is reasonable to wonder whether routine computed tomography (CT) or bone scan of all RTSA would diagnose a number of fractures which were either asymptomatic or not appreciated on plain radiograph. Indeed, Levy et al. found that plain radiographs were unreliable in detecting acromial fractures at the time of initial presentation of pain (K = −0.5) and at determining whether fracture union had occurred (K = 0.05).8
Mechanism of injury and risk factors
The causative factors leading to fatigue fracture can be divided into patient factors and sequelae of operative technique.
Osteoporosis
The most extensive article evaluating pre-operative patient factors was by Otto et al.13 They assessed 53 RTSAs with CTs performed on patients clinically presenting with fracture post-operatively and retrospectively identified osteoporosis as a significant risk factor for the development of fatigue fracture (odds ratio (OR) 1.97, 95% CI 1.00–3.91). Factors not associated with fracture included age, gender, body mass index, surgery on the dominant arm, previous surgery, endocrine disease, autoimmune disease, smoking, alcoholism and steroid use. Whilst their analysis fulfilled standard significance criteria (p = 0.049), the margin was small. There were no papers which investigated the role of bisphosphonates.
ACJ arthrosis
Although they did not investigate it, Crosby et al. offered a biomechanical hypothesis based on their classification system after RTSA.6 Type II fractures were posterior to the ACJ. Hypothetically, an arthritic or stiff ACJ would not allow for the dissipation of forces anteriorly thereby loading up the posterior acromion. Crosby’s type III fractures all occurred traumatically and were thought to be in relation to screw placement of the most superior metaglene screw (rather than pre-existing patient factors).
Conversely, in a retrospective review of 14 fatigue fractures, Dubrow et al. found that pre-existing ACJ arthritis was not predictive of fracture.14 Little evidence exists to support ACJ arthrosis as a risk factor of acromial fracture post-RTSA. The importance of anatomically classifying acromial fractures with reference to the ACJ remains unproven as does the utility of the Crosby classification system.
Pre-existing acromial pathology
A few studies investigated whether pre-existing acromial pathology or insufficiency was a risk factor of fatigue fracture after RTSA. Walch et al. had a series of 41 patients with pre-existing os acromiale, 17 with fatigue fracture pre-dating their primary RTSA operation and 1 with stress fracture non-union in a total cohort of 457 patients; 63% of these patients saw a progression of the inferior angulation of their distal acromion, but this was not associated with worse functional scores, active elevation or subjective satisfaction. They also had four fatigue fractures occur in patients with no evidence of pre-operative acromial pathology.9 However, there is no literature to support a correlation between these and acromial fracture post-RTSA at this time.
Question 3: classification
Currently, the classifications only comment on location of fracture, with no reference to fracture displacement. Whilst implicit in management decisions, explicit descriptions of displacement in future publications will foster stronger recommendations. Displacement less than 2 mm (type A), between 2 and 10 mm or resulting in >20° angulation (type B) or fractures with displacement exceeding these values (type C) might prove helpful. Other factors which could be accommodated include whether the fracture caused instability of the arthroplasty or resulted in loss of metaglene fixation.
Question 4: prosthesis and surgical factors
Screw positioning
Operative factors that were discussed included glenoid screw positioning. Otto et al. documented 11 of 16 scapular spine fractures (Crosby type III) occurring from the tip of the most posterior or superior screw, with a further 3 occurring from the tip of the centre screw. These positions were determined on CT. However, these were a subgroup of their total cohort of 53 fractures (as distinct to scapular spine only fractures), and statistical analysis failed to find any association between screw placement and stress fracture.13
Conversely, Crosby et al. modified their surgical technique after observing that a superiorly oriented screw acted as a stress riser in their type III acromial fractures.6 Evidence to further support this hypothesis from the same group of authors was provided by Kennon et al. who investigated both clinical and biomechanical stresses of a superior screw construct on the scapular spine. In a retrospective review of 318 patients, nine type III Crosby scapular fractures were identified in relation to a superior screw and none as a consequence of inferiorly placed screws.11
In the biomedical section of their paper, cadaveric specimens were divided into two groups – inferior glenoid screws alone and inferior screws with an additional superior screw directed into the glenoid neck and body, again using the Equinoxe RTSA by Exactech. These specimens were then loaded with a compressive force until failure – identified on both a load–displacement curve as well as visually with fracture propagation along the scapular spine. The superior screw group was found to have a failure threshold 45% lower than the inferior-only group. The superior screw group also had a decreased construct stiffness by 43%, where stiffness was defined as the slope of the load–displacement curve.11
Biomechanical studies have identified both the scapular spine and base of the coracoid as regions in the scapula with highest cortical thickness and thus potential bony corridors for superiorly orientated glenoid baseplate screws.33,34 Perhaps the orientation of the superior screw supero-posteriorly towards the scapular spine may predispose these constructs towards acromial base or Crosby III-style fracture post-RTSA. Conversely, supero-anteriorly orientated screws towards the coracoid may not have the same risks. There are no studies which have evaluated this in vivo.
Deltoid overtensioning and prosthetic choice and design
Overtensioning of the deltoid by a lateralised implant was cited by almost all papers as a contributive factor in acromial or scapular spine stress fracturing. Biomechanically, RTSA medialises the centre of rotation, increasing the deltoid lever arm. Any lateralisation, bone or prosthesis derived, decreases the deltoid lever arm in comparison to other RTSA constructs and consequently increases the deltoid force necessary to generate an equal abduction moment. The change of vector orientation may also be important.
Wong et al. studied this in a biomechanical study of 10 cadaveric shoulders with increasing degrees of glenoid displacement inferiorly and laterally as well as humeral lateralisation.35They found that acromial stress was significantly reduced in an inferiorised glenosphere by 2.6% and that glenosphere lateralisation produced 17.2% greater acromial stress. In vivo, Kurowicki et al. also reported on the results of RTSA (DJO Reverse Shoulder Prosthesis) in patients with locked anterior dislocation and subsequent significant glenoid bone loss.15 They found post-operative acromial stress fractures in 21% of their locked group compared to only 9% of their control with a predominance of Crosby type III fractures. They argued that this could be secondary to additional acromial stress after lateralisation of a chronically medialised and contracted shoulder. Chronic dislocation may also lead to a disuse osteopaenia that may reduce the acromion’s ability to respond to the new deltoid force, size and direction.
Greiner et al. studied this clinically in a comparative study of lateralised versus non-lateralised RTSA in a prospective randomised trial using the Aequalis (Tournier) RTSA.16 This lateralisation was achieved using a 1 cm bony autograft (‘bony increased offset’ or ‘BIO-RSA’). Their results suggested no clinical difference in increased offset based on functional scores. They had four fatigue fractures in total with two each in the lateralised and non-lateralised groups out of a cohort of 34. This study was not powered to investigate this secondary outcome.
Our findings suggested that onlay humeral implant designs and the DJO prosthesis were more commonly associated with stress fracture. However, this finding is biased by under-reporting of prostheses. Furthermore, the degree of lateralisation achieved by the implants is not uniform and difficult to quantify retrospectively.
Despite being referred to in nearly every paper, there is still no clear in vivo evidence that deltoid overtensioning leads to fragility fractures of the acromion or scapular spine. The difficulty in confirming this theory may lie in the variability of measuring tension in RTSA by radiological markers. It is worth considering whether the vector of force on the acromion is more significant or whether scalar force matters more. The BIO-RSA ‘wraps’ the deltoid around the greater tuberosity, much like the patella does for the quadriceps. We had a small sample size when it comes to prosthesis design and choice with selection bias, making recommendations difficult. If lateralisation and deltoid overtensioning are to be confirmed as an aetiology of acromial stress fracturing, it needs to be investigated more rigorously.
Question 5 + 6: treatment and its effect on outcome
The results of non-operative management
Most acromial or scapular spine stress fractures were treated non-operatively with sling immobilisation. The majority of the literature reported inferior outcomes when acromial fracture was treated non-operatively (55%). Hamid et al. reported either non-union or mal union in all eight of their cases with concomitant reduction in active forward elevation and ASES scores.7 Walch et al. described four stress fractures with significantly inferior results with respect to range of motion, CMS and pain scores.9 Teusink et al. reported 32 post-operative scapular fractures with significantly inferior clinical outcome scores (ASES) of 58.0 compared to 74.2 in the non-fracture group (p < 0.001).10 Range of motion was also reduced with a mean gain of only 26° in the non-fracture group compared to 76° (p < 0.001). These results suggest a 26-point reduction in ASES after scapular spine fracture and thus that outcomes are measurably worse if fracture occurs.
There was one report of a ‘bone stimulator’ in acromial fracture after the patient refused operative intervention.12 At 13 months, radiological union was achieved, but a Neer Functional Outcome score of 66 out of 100 suggests an unsatisfactory result. There were no reports of low-intensity pulsed ultrasound being used. A Cochrane review identified its use in the radius and scaphoid.36 Its efficacy remains unknown.
Osteosynthesis
Where surgical fixation was attempted, a variety of constructs were used. Tension band wiring was employed in one instance in the study by Walquist et al.12 and once in that of Walch et al.9 In both cases, patient satisfaction with the overall result was low and in the case of Walch, removal of hardware required because of ongoing inferior acromial tilt and pain. The failure of this otherwise reliable technique may be because a tension band wire construct is ideal at neutralising forces parallel to the axis of its band but is unable to overcome the multiple vectors generated by the deltoid’s broad origin with multipennate orientations. Additionally, the tension band wire was not conceived to overcome a cantilever type moment of deformation.
Plate and screw osteosynthesis was also reported in Walquist’s study, although the initial operation failed with further fracture displacement and requiring revision.12 Post-operative satisfaction was poor in this case. Conversely, Crosby et al. advocated for plate and screw fixation of type III fractures and also reported on primary fixation of 3 of their 10 type II fractures – all of whom had no pain at their fracture site post-operatively. They also performed ACJ resection in three cases where the acromial fracture appeared stable at the time of operation. Of their type three fractures, one of the four required revision surgery for failure of fixation and one underwent eventual removal of metalware. All had good pain scores post-operatively.6 Similarly, Kennon et al. performed primary osteosynthesis in five instances and reported significant improvements in ASES, SST and CMS.11
Union rates generally were not specifically reported. In patients undergoing osteosynthesis of their acromial fracture, only two papers reported on union rates. Similarly, functional outcomes pre- and post-osteosynthesis surgery also had very limited documentation, which makes assessing the utility of surgery difficult.
Revision arthroplasty
There were seven cases of recurrent instability post-RTSA in the setting of acromial fracture, and two of failure of the glenoid component. This led to nine revision arthroplasty operations (4%) after acromial fracture. Kurowicki et al. describes one patient who had a Levy type III acromial fracture who had two revision operations for instability.15 They hypothesised that the acromial fracture may have contributed towards this instability via loss of deltoid tensioning. Hattrup also described an instance of recurrent subluxation in the setting of acromial fracture which required the insertion of a thicker polyethylene liner two years after index surgery.30 Levy et al.’s study reported two revision arthroplasties in type III fractures. In both cases, recurrent instability was treated by revision arthroplasty surgery, although the fracture was managed non-operatively and the type of revision arthroplasty not specified.8 Kennon et al. also documented one case of recurrent instability where primary fixation and revision arthroplasty were performed at the same time.11 Crosby et al.’s series included revisions in two type I fractures: one for instability (with osteolysis) and another for failure of the glenoid component.6 Similarly, in Teusink et al.’s study, one revision was performed for glenoid loosening and another for recurrent instability two weeks after the initial fracture was identified.10
Given the variable treatments used for unstable RTSA after acromial fracture and the sporadic reporting of results, this analysis provides weak guidance. With instability, should the prosthesis be ‘lengthened’ to regain tension; should the fracture be operatively reduced to regain tension; or both?
Question 7: limitations, recommendations and proposal of a minimum data set
The collection of data surrounding acromial fracture after RTSA in the literature has been non-uniform and largely based on whichever factors various authors have been able to report.
Aside from a single level I study, the remainder of our studies were level IV. This restricts the external validity of our findings and recommendations. Furthermore, the majority of the studies had relatively small cohort sizes. Publication bias is a limitation in this systematic review. It is unknown how many fractures occur post-operatively, and the findings we have presented are a reflection of the under-reporting and publication bias that exists around complications post-surgical intervention. Relative heterogeneity and under-reporting of demographic, prosthetic and outcome data across our identified studies made meta-regression analysis under powered and conclusions weak. Finally, our search was limited to the English language. Accordingly, there are many papers published in other languages – particularly in French and relating to the Grammont-style prosthesis – which were not included in this study.
Despite these limitations, this is still the first paper to critically summarise and evaluate the existing literature relating to acromial fracture after RTSA and some weak suggestions are possible. These include:
Pain post-RTSA which occurs insidiously after a period of pain-free function should be investigated with plain radiographs ± CT as incidence of acromial stress fracture is 5%.
The natural history of acromial stress fracture after RTSA is for poorer function and more pain with an average reduction in ASES of 26 points.
In appropriate patients, internal fixation should be considered. Tension band wiring should not be chosen as a fixation construct.
Acromial fracture may predispose patients to instability or results in glenoid loosening. Revision surgery for instability may be directed at lengthening the prosthesis and fixing the fracture. The best method of revision has not been determined.
Recommendations for a minimum data set for future RTSA publication includes:
Anatomical classification (Crosby et al.6 and Otto et al.13) and further fracture factors like displacement and angulation, operative or non-operative intervention, rehabilitation protocols, time to union, rates of fracture union, need for further surgery such as revision arthroplasty or removal of metal and appropriate functional outcomes scores like the ASES, SST or CMS.
- Reporting of functional outcome scores should be at time points of:
- ° Prior to index RTSA
- ° At maximum time point prior to acromial fracture
- ° At 6, 12 and 24 months post-fracture or surgery
Incidence among entire cohorts, with specific numbers of each prosthesis and surgical approach used.
Conclusion
Acromial or scapular spine fracture after RTSA has an incidence of 4.7%, although this is probably under-representative as fractures may be underdiagnosed or not reach publication. The aetiology of stress fracture is yet to be fully described, although certain factors such as osteoporosis, superior glenoid baseplate screw stress risers and deltoid overtensioning have all been proposed. Treatment has predominantly been non-operative, but this tends to result in pain and a decrease in ASES of 26 points. When surgery is performed, results are varied and a high rate of revision osteosynthesis surgery is notable. Unfortunately, the sporadic reporting of union rates, description of fixation methods, rehabilitation protocols and post-fracture shoulder scores makes any recommendations weak and comparison highly subjective. A minimum data set for reporting has been recommended in our text; a standard we hope future publishers might apply.
Acknowledgements
This paper has previously been presented at the 2018 Victorian Australian Orthopaedic Association Annual Scientific Meeting in Lorne and the 2018 Australian Shoulder and Elbow Society Meeting in Perth. It has never otherwise been published in the written literature. The authors would like to thank Mr Nigel Broughton, Orthopaedic Surgeon and Director of Orthopaedic Research at Peninsula Health, and Dr Vicky Tobin, Research Co-ordinator, Peninsula Health, for their contributions to this manuscript.
Authors’ Contribution: SL wrote the first draft of the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Guarantor: RL.
Trial Registration: NA.
Ethical Review and Patient Consent
Ethical approval and patient consent were not sought for this article because a review of the literature (without patient contact) was all that was performed.
References
- 1.Grammont P, Trouilloud R, Laffay J, et al. Etude de realisation d’une nouvelle prothèse d’épaule. Rheumatologie 1987; 39: 407–418. [Google Scholar]
- 2.Zumstein MA, Pinedo M, Old J, et al. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 2011; 20: 146–157. [DOI] [PubMed] [Google Scholar]
- 3.Farshad M, Gerber C. Reverse total shoulder arthroplasty-from the most to the least common complication. Int Orthop 2010; 34: 1075–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009; 6: e1000097–e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. Epidemiology 2007; 18: 805–835. [DOI] [PubMed] [Google Scholar]
- 6.Crosby LA, Hamilton A, Twiss T. Scapula fractures after reverse total shoulder arthroplasty: classification and treatment. Clin Orthop Relat Res 2011; 469: 2544–2549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hamid N, Connor PM, Fleischli JF, et al. Acromial fracture after reverse shoulder arthroplasty. Am J Orthop 2011; 40: E125–E129. [PubMed] [Google Scholar]
- 8.Levy JC, Anderson C, Samson A. Classification of postoperative acromial fractures following reverse shoulder arthroplasty. J Bone Joint Surg Am 2013; 95: e104–e104. [DOI] [PubMed] [Google Scholar]
- 9.Walch G, Mottier F, Wall B, et al. Acromial insufficiency in reverse shoulder arthroplasties. J Shoulder Elbow Surg 2009; 18: 495–502. [DOI] [PubMed] [Google Scholar]
- 10.Teusink MJ, Otto RJ, Cottrell BJ, et al. What is the effect of postoperative scapular fracture on outcomes of reverse shoulder arthroplasty? J Shoulder Elbow Surg 2014; 23: 782–790. [DOI] [PubMed] [Google Scholar]
- 11.Kennon JC, Lu C, McGee-Lawrence ME, et al. Scapula fracture incidence in reverse total shoulder arthroplasty using screws above or below metaglene central cage: clinical and biomechanical outcomes. J Shoulder Elbow Surg 2017; 26: 1023–1030. [DOI] [PubMed] [Google Scholar]
- 12.Wahlquist TC, Hunt AF, Braman JP. Acromial base fractures after reverse total shoulder arthroplasty: report of five cases. J Shoulder Elbow Surg 2011; 20: 1178–1183. [DOI] [PubMed] [Google Scholar]
- 13.Otto RJ, Virani NA, Levy JC, et al. Scapular fractures after reverse shoulder arthroplasty: evaluation of risk factors and the reliability of a proposed classification. J Shoulder Elbow Surg 2013; 22: 1514–1521. [DOI] [PubMed] [Google Scholar]
- 14.Dubrow S, Streit JJ, Muh S, et al. Acromial stress fractures: correlation with acromioclavicular osteoarthritis and acromiohumeral distance. Orthopedics 2014; 37: e1074–e1079. [DOI] [PubMed] [Google Scholar]
- 15.Kurowicki J, Triplet JJ, Momoh E, et al. Reverse shoulder prosthesis in the treatment of locked anterior shoulders: a comparison with classic reverse shoulder indications. J Shoulder Elbow Surg 2016; 25: 1954–1960. [DOI] [PubMed] [Google Scholar]
- 16.Greiner S, Schmidt C, Herrmann S, et al. Clinical performance of lateralized versus non-lateralized reverse shoulder arthroplasty: a prospective randomized study. J Shoulder Elbow Surg 2015; 24: 1397–1404. [DOI] [PubMed] [Google Scholar]
- 17.Mollon B, Mahure SA, Roche CP, et al. Impact of glenosphere size on clinical outcomes after reverse total shoulder arthroplasty: an analysis of 297 shoulders. J Shoulder Elbow Surg 2016; 25: 763–771. [DOI] [PubMed] [Google Scholar]
- 18.Mellano CR, Kupfer N, Thorsness R, et al. Functional results of bilateral reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2017; 26: 990–996. [DOI] [PubMed] [Google Scholar]
- 19.Werner CM, Steinmann PA, Gilbart M, et al. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am 2005; 87: 1476–1486. [DOI] [PubMed] [Google Scholar]
- 20.Saltzman BM, Chalmers PN, Gupta AK, et al. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: 1647–1654. [DOI] [PubMed] [Google Scholar]
- 21.Shafritz AB, Flieger S. Reverse total shoulder arthroplasty: early results of forty-one cases and a review of the literature. Hand Clin 2012; 28: 469–479. [DOI] [PubMed] [Google Scholar]
- 22.Boileau P, Watkinson DJ, Hatzidakis AM, et al. Grammont reverse prosthesis: design, rationale, and biomechanics. J Shoulder Elbow Surg 2005; 14: 147s–161s. [DOI] [PubMed] [Google Scholar]
- 23.von Engelhardt LV, Manzke M, Filler TJ, et al. Short-term results of the reverse Total Evolutive Shoulder System (TESS) in cuff tear arthropathy and revision arthroplasty cases. Arch Orthop Trauma Surg 2015; 135: 897–904. [DOI] [PubMed] [Google Scholar]
- 24.Simovitch RW, Gerard BK, Brees JA, et al. Outcomes of reverse total shoulder arthroplasty in a senior athletic population. J Shoulder Elbow Surg 2015; 24: 1481–1485. [DOI] [PubMed] [Google Scholar]
- 25.Kempton LB, Ankerson E, Wiater JM. A complication-based learning curve from 200 reverse shoulder arthroplasties. Clin Orthop Relat Res 2011; 469: 2496–2504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Groh GI, Groh GM. Complications rates, reoperation rates, and the learning curve in reverse shoulder arthroplasty. J Shoulder Elbow Surg 2014; 23: 388–394. [DOI] [PubMed] [Google Scholar]
- 27.Cuff D, Pupello D, Virani N, et al. Reverse shoulder arthroplasty for the treatment of rotator cuff deficiency. J Bone Joint Surg Am 2008; 90: 1244–1251. [DOI] [PubMed] [Google Scholar]
- 28.Bufquin T, Hersan A, Hubert L, et al. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br 2007; 89: 516–520. [DOI] [PubMed] [Google Scholar]
- 29.Atoun E, Van Tongel A, Hous N, et al. Reverse shoulder arthroplasty with a short metaphyseal humeral stem. Int Orthop 2014; 38: 1213–1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hattrup SJ. The influence of postoperative acromial and scapular spine fractures on the results of reverse shoulder arthroplasty. Orthopedics 2010; 33: 302–302. [DOI] [PubMed] [Google Scholar]
- 31.Stevens CG, Murphy MR, Stevens BD, et al. Bilateral scapular fractures after reverse shoulder arthroplasties. J Shoulder Elbow Surg 2015; 24: e50–e55. [DOI] [PubMed] [Google Scholar]
- 32.Zhou HS, Chung JS, Yi PH, et al. Management of complications after reverse shoulder arthroplasty. Curr Rev Musculoskelet Med 2015; 8: 92–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Karelse A, Kegels L, De Wilde L. The pillars of the scapula. Clin Anat 2007; 20: 392–399. [DOI] [PubMed] [Google Scholar]
- 34.DiStefano JG, Park AY, Nguyen TQ, et al. Optimal screw placement for base plate fixation in reverse total shoulder arthroplasty. J Shoulder Elbow Surg 2011; 20: 467–476. [DOI] [PubMed] [Google Scholar]
- 35.Wong MT, Langohr GD, Athwal GS, et al. Implant positioning in reverse shoulder arthroplasty has an impact on acromial stresses. J Shoulder Elbow Surg 2016; 25: 1889–1895. [DOI] [PubMed] [Google Scholar]
- 36.Griffin XL, Smith N, Parsons N, et al. Ultrasound and shockwave therapy for acute fractures in adults. Cochrane Database Syst Rev 2012; 15: Cd008579–Cd008579. [DOI] [PubMed] [Google Scholar]