Abstract
Background
Tension band wiring and plate fixation are common techniques used to stabilize simple olecranon fractures and osteotomies of the olecranon. All suture fixation is an alternative technique but has not been compared previously to these traditional methods. The aim of this study was to compare the clinical and radiographic outcomes of the three techniques.
Methods
One hundred and sixty-eight consecutive Mayo type 1 and 2 olecranon fractures (n = 138) and olecranon osteotomies (n = 30) with a minimum follow-up time of one year were compared. The primary outcome measure was the rate of re-operation. Secondary outcome measures were the incidence of complications, rate of radiographic union and incidence of radiographic reduction loss.
Results
Fixation was performed using tension band wiring in 89 patients, plating in 38 patients and suture fixation in 41 patients. There was no significant difference in the fracture type according to the Mayo classification between the groups. The re-operation rate was significantly higher in the tension band wiring group (36%) compared with both the plate group (11%, p = 0.03) and the suture group (2%, p = 0.002). There were two revision fixations in the tension band wiring group and one in the suture group. There was one asymptomatic non-union in the suture group. All other fractures and osteotomies achieved radiographic union.
Conclusion
Suture fixation of simple olecranon fractures and osteotomies was reliable in providing stable union and had a significantly lower re-operation rate when compared with tension band wiring.
Keywords: olecranon fracture, olecranon osteotomy, tension band wiring, internal fixation, suture fixation
Introduction
Olecranon fractures most commonly occur following a standing height fall with direct impact to the point of the elbow. Alternative mechanisms include avulsion fractures caused by eccentric triceps contraction and high-energy injuries such as falls from height or road traffic accidents.1 Seventy per cent of fractures are simple transverse fracture. More complex fracture patterns have varying degrees of articular comminution, ulnohumeral instability and associated osseo-ligamentous injuries.2
Although there is a role for non-operative management in undisplaced fractures or for displaced fractures in low demand patients,3 most displaced fractures in active patients are treated surgically.
The most common mode of fixation is to use tension band wiring (TBW), which is appropriate for transverse fractures with minimal articular comminution and no evidence of ulnohumeral instability. While this technique is associated with good outcomes related to fracture union, there is a high associated re-operation rate for removal of prominent wires. Various modifications of the technique have been employed to counteract this issue, including use of long intramedullary wires, wires placed into the anterior cortex of the ulna, threaded wires and cutting the wires without bending.4–6 Despite these measures, the rate of re-operation for wire removal is as high as 70% in the literature.1
Other common techniques such as plate fixation and intramedullary fixation mitigate the rate of wire migration but carry their own specific complications and use more costly implants than for TBW.7 In particular, dorsal plates can cause irritation when leaning on the elbow and wound healing problems, in slim patients or those with more fragile soft tissues.7,8 More novel techniques described include fragment excision and triceps advancement, fixation with an ‘olecranon sled’ and suture fixation.9–15
Several methods of suture fixation have been described, although the majority use either suture anchors, transosseous tunnels or suture in combination with Kirschner wires (K wires).11,13,15 A more recently described technique employs braided non-absorbable suture without use of tunnels, suture anchors or any metalwork for fixation of simple olecranon fractures and olecranon osteotomies, with good results reported.12,14
Although there are comparative data between TBW and plate fixation in the literature, there are no studies comparing the outcomes of these more traditional methods with a suture fixation technique.
The aim of this study was to compare the traditional techniques of TBW and plate fixation with a suture fixation technique for the treatment of simple olecranon fractures and olecranon osteotomies.
Methods
A two-centre (Brighton & Sussex University Hospitals, Wrightington, Wigan and Leigh Trust, UK) retrospective cohort study was performed.
Inclusion/exclusion criteria
All consecutive olecranon fractures treated surgically between June 2012 and June 2017 were retrospectively identified using a patient management database (Bluespier, Clanwilliam Group, Worcestershire, UK). Consecutive olecranon osteotomies used for treatment of distal humeral fractures were also identified using the same system.
Fractures were classified according to the Mayo system.1 Only Mayo type 1 and 2 fractures were included (displaced or undisplaced fractures with a simple fracture pattern and no evidence of ulnohumeral instability). Trans-olecranon fracture dislocations, oblique fractures, fractures extending beyond the coronoid and fractures with concomitant ligamentous or bony injuries were all excluded.
All osteotomies were distally based chevron osteotomies performed for access to distal humerus fracture fixation.
Outcome measures
The primary outcome measure was the rate of re-operation for any reason. Secondary outcome measures were complication rate, radiographic union rate and maintenance of anatomic reduction on post-operative radiographs. All complications were documented and included in the analysis. Re-operations and complications were identified from the medical notes and the hospital patient management database. Wound healing and adequacy of fixation were assessed on plain radiographs at two weeks post-operatively followed by X-rays to assess bony union between 6 and 12 weeks post-operatively. Further X-rays were repeated in the presence of ongoing symptoms or delayed union. Union was defined as the presence of bridging inter-fragmentary callus on a lateral radiograph, without evidence of fracture gapping or loss of fracture reduction. Radiographic assessment was carried out by three of the authors (AV, JP and JSP).
Patients
There were 168 fractures/osteotomies treated in 166 patients. Seventy-one patients were male and 95 were female. The mean age was 55 years (16–93 years). The minimum follow-up time was one year. Data were available for all patients with no loss to follow-up.
Fracture types and fixation techniques
There were 138 olecranon fractures and 30 chevron osteotomies. Ninety-five per cent (n = 131) of the fractures were displaced (Mayo type 2) and 5% (n = 7) were minimally displaced (Mayo type 1). Sixty-eight (52%) of the Mayo type 2 fractures were simple with no comminution (Mayo 2a) and 63 (48%) had some articular comminution (Mayo 2b).
Three methods of fixation were used: TBW in 89 cases (53%), plate fixation in 38 patients (23%), suture fixation in 41 patients (24%).
TBW was performed by passing two 1.6 mm or 2 mm longitudinal K wires across the fracture with an 18 or 20 gauge figure of eight steel wire looped around the wires and tightened using two knots. The size of the wires was determined by the operating surgeon depending on the patient size. The longitudinal K wires were placed intramedullary in 46/89 (52%) cases and trans-cortically in 43/89 (48%) cases.
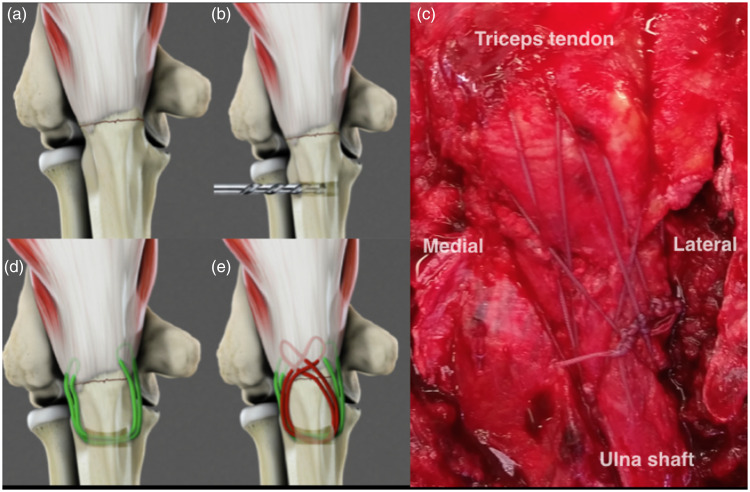
Suture fixation was performed using a number two braided, non-absorbable suture according to the technique described by Watts et al.12,14 without placement of any metalwork (Figure 1). In brief, after exposure of the fracture, anatomic reduction and inter-fragmentary compression are achieved using a large pointed reduction clamp. A transverse 2.5 mm drill hole is made distal to the fracture. Two sets of sutures are passed from lateral to medial through the transverse hole. The first suture is used to grasp the proximal fragment at the medial insertion of the triceps onto the fragment. It is then re-passed through the transverse hole from medial to lateral and used to grasp the proximal fragment on the lateral aspect in the same fashion. After tensioning of the sutures to remove slack, a knot is tied on the lateral aspect of the proximal ulna. A second suture is passed from lateral to medial through the transverse hole and is this time used to grasp the proximal fragment by passage through the posterolateral triceps attachment. The suture is then re-passed from medial to lateral through the transverse hole and then through the posteromedial triceps attachment to once more grasp the proximal fragment. After tensioning, this suture is also tied on the lateral aspect of the proximal ulna. Care is taken to tie the sutures with the elbow in a relatively extended position, so that the sutures tighten further in flexion adding compression to the construct but do not loosen in extension (Figure 2). Placing the knots laterally beneath anconeus minimizes the risk of knot irritation.
Figure 2.
(a)–(e). Depiction of suture fixation technique. The fracture is reduced (a) and a transverse drill hole is made in the ulna (b). Sutures are passed from lateral to medial with the first set grasping the proximal fragment in a longitudinal manner (c) and the second set creating a crisscross configuration (d). Intra-operative view of the technique used to fix a chevron olecranon osteotomy (e).
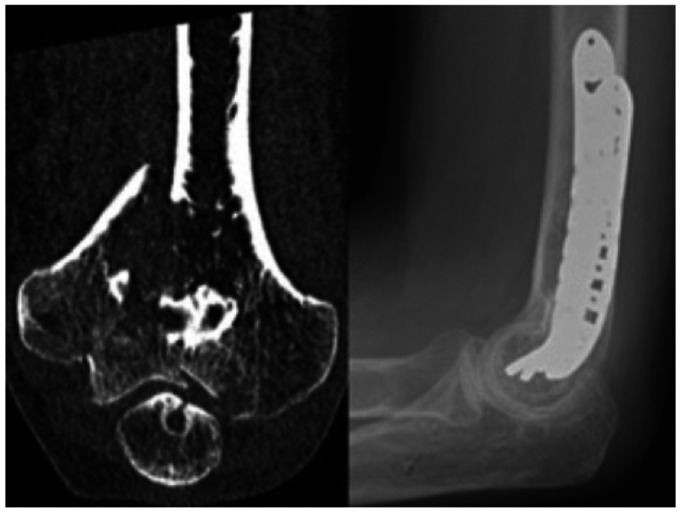
Figure 1.
Multi-fragmentary distal humeral fracture treated with internal fixation through an olecranon osteotomy approach. Fixation of the osteotomy with the all suture technique shows complete radiographic union at three months following surgery.
Plate fixation was performed using a dorsal pre-contoured peri-articular locking plate with a combination of 2.7 mm and 3.5 mm locking and cortical screws.
All operations were performed by or under the direct supervision of a consultant orthopaedic surgeon.
Statistical analysis
Categorical variables and baseline demographic data are described by frequencies and percentages. Continuous variables are presented as means. Non-parametric tests (Chi squared and Fisher's exact test) were used to test for differences between groups. The level of significance was set to a p value of <0.05.
Results
Fracture type and fixation method
In the TBW group, 81/89 (91%) cases were performed for fracture fixation and 8/89 (9%) were performed for osteotomy fixation. Of the fracture fixations, there were 5/81 (6%) Mayo type 1 and 76/81 (93%) Mayo type 2 fractures.
In the suture group, 24/41 (59%) cases were performed for fracture fixation and 17/41 (41%) were performed for osteotomy fixation. Of the fracture fixations, there were 2/24 (8%) Mayo type 1 and 22/24 (91%) Mayo type 2 fractures.
There was no difference in the proportion of Mayo type 1 and type 2 fractures between the TBW and suture groups.
In the plate group, 33/38 (87%) cases were performed for fracture fixation and 5/38 (13%) were performed for osteotomy fixation. All fractures (n = 33) in the plate group were Mayo type 2, although this was not significantly different to the proportion of Mayo type 1 and 2 fractures in either the TBW group or the suture group.
There were a significantly greater number of osteotomies in the suture group than in the TBW group (p≤0.001) and the plate group (p = 0.008).
Table 1 summarizes the number of patients in each group.
Table 1.
Patients categorized by fracture type and fixation technique.
| Fracture type | Surgical fixation technique |
Total | ||
|---|---|---|---|---|
| TBW | Suture | Plate | ||
| Osteotomy | 8 | 17 | 5 | 30 |
| Mayo type 1 | 5 | 2 | 0 | 7 |
| Mayo type 2 | 76 | 22 | 33 | 131 |
| Total | 89 | 41 | 38 | 168 |
TBW: tension band wiring.
Re-operations
The overall re-operation rate was 22% (37/168). No patient had more than one re-operation. The re-operation rate was 36% (32/89) in the TBW group; 2% (1/41) in the suture group and 11% (4/38) in the plate group. There was a significantly higher re-operation rate in the TBW group compared to both the suture group (p = 0.002) and the plate group (p = 0.03). There was no significant difference in the re-operation rate between the plate group and the suture group. In the TBW group, 20/46 (44%) cases, which used intramedullary wires and 12/43 (28%) cases, which used transcortical wires required re-operation for wire removal. This was not significantly different.
Thirty of 37 (81%) of all the re-operations were performed for removal of prominent metalwork without the presence of concurrent infection. Of these, 26/30 (87%) were in the TBW group and 4/30 (13%) were in the plate group. In the TBW group, 25/26 cases required removal of one or both longitudinal K wires because of back out and prominence. In 22/25 cases, the cerclage wire was also removed at the same time, and in three cases, the cerclage wire was retained, as wire removal was required before bony union of the fracture had occurred. In one case, the longitudinal wires were removed because of transcortical placement causing impingement against the radius with restricted forearm rotation.
There were no re-operations in the suture group for removal of sutures or to treat prominent knots.
Four of 37 (10.1%) of re-operations were for removal of metalwork in the presence of infection. These were all in the TBW group. All infections were treated successfully by wire removal, debridement and antibiotics. There were no infections in the plate or the suture groups.
Three of 37 (8%) of re-operations were performed to revise a failed fixation. Two of these were in the TBW group and one was in the suture group. Two cases (one TBW and one suture) were in patients who had displacement of an olecranon osteotomy repaired following fixation of a distal humeral fracture. The other was a Mayo type 2b fracture originally treated with TBW. All three cases were revised to fixation with a plate and all went on to bony union without further complications.
Table 2 summarizes the overall complications related to each group.
Table 2.
Summary of complications related to each group.
| Fixation technique | Number | Complications |
|||
|---|---|---|---|---|---|
| Implant removal | Re-fixation | Infections | Non-union | ||
| TBW | 89 | 32 (36%) | 2 (2%) | 4 (4%) | 0 |
| Plate | 38 | 4 (11%) | 0 | 0 | 0 |
| Suture | 41 | 1 (2%) | 1 (2%) | 0 | 1 (2%) |
TBW: tension band wiring.
Tables 3 and 4 show a sub-group analysis of complications according to fracture fixation or osteotomy fixation. There was a small trend towards higher complication rates across all types of fixation for osteotomy fixation compared to fracture fixation, although the numbers of complications were too small to warrant meaningful statistical evaluation.
Table 3.
Complications related to fracture fixation.
| Fixation technique | Number | Complications |
|||
|---|---|---|---|---|---|
| Implant removal | Re-fixation | Infections | Non-union | ||
| TBW | 81 | 29 (36%) | 1 (1%) | 4 (5%) | 0 |
| Plate | 33 | 3 (9%) | 0 | 0 | 0 |
| Suture | 24 | 0 | 0 | 0 | 0 |
Table 4.
Complications related to osteotomy fixation.
| Fixation technique | Number | Complications |
|||
|---|---|---|---|---|---|
| Implant removal | Re-fixation | Infections | Non-union | ||
| TBW | 8 | 3 (38%) | 1 (13%) | 0 | 0 |
| Plate | 5 | 1 (20%) | 0 | 0 | 0 |
| Suture | 17 | 0 | 1 (6%) | 0 | 1 (6%) |
TBW: tension band wiring.
Radiographic results
Initial radiographic anatomic reduction was achieved in all cases. In addition to the three cases of failed fixation already described, there was one case of non-union that was not treated with further surgery. This was a patient who underwent suture fixation of an olecranon osteotomy. At six weeks post-operatively, there was gapping of 4 mm and incomplete union at the osteotomy site. The gap was still present at three and six months post-operatively, although there was no increase in the size of the gap or further displacement of the proximal fragment on serial radiographs. The distal humeral fracture went on to satisfactory union and the patient had no pain, a 120° arc of motion and good resisted triceps power. Consequently, the patient elected not to have further intervention.
All other fractures and osteotomies achieved radiographic union between 6 and 16 weeks post-operatively without loss of reduction.
Discussion
This study demonstrated a significantly higher re-operation rate following TBW performed in simple olecranon fractures and osteotomies compared to both plate fixation and suture fixation. The majority of the re-operations in the TBW group were for removal of the longitudinal K wires, which is consistent with the existing literature that shows a re-operation rate of between 20 and 70% following TBW.1 Some authors have described modifications to the TBW technique such as placement of transcortical rather than intramedullary wires in an attempt to reduce the rate of re-operation; however, in both this study (28%) and others in the literature, there remains a high rate of wire removal despite this modification.4,16
In addition, long or inappropriately angled transcortical wires have been reported to cause impingement against the radius, radio-ulnar synostosis and anterior interosseous nerve palsy.17,18
Plate fixation has traditionally been the alternate surgical treatment to TBW, although it is usually employed for more complex fractures with ulnohumeral instability (Mayo type 3). As only Mayo type 1 and 2 fractures were included in this study, there were fewer patients in the plate fixation group. In a large comparative study of TBW and plate fixation for Mayo type 1 and 2 fractures, Claessen et al. reported a similar rate of re-operation for metalwork prominence in the two groups (22% and 26%, respectively).8 In contrast, in a randomized control trial of TBW versus plate fixation for simple and comminuted fractures, symptomatic hardware was significantly more common following TBW than plate fixation (42% vs. 5%), although there was no difference in functional outcome.19 Similarly, Schliemann et al. found no difference in the functional or radiographic outcome of plate fixation versus TBW for Mayo type 2 fractures, although the rate of implant removal was significantly higher in the TBW group (93% vs. 27%).5 The results of these studies reflect our findings when comparing TBW with plate fixation.
In a study focused on financial cost, Amini et al. performed a comparison on 20 patients with an olecranon fracture (10 treated with TBW and 10 with locked plate fixation). They reported a 30-fold higher basic implant cost with locking plates and double the cost even in the hypothetical situation that all TBW were removed and no plates required re-operation.7 Although a cost analysis was not performed in our study, the much higher economic costs reported by other authors make the use of plates as an alternative to TBW difficult to justify. Suture fixation has been proposed in several small case series as a relatively low-cost alternative to TBW11,13–15 but has never been directly compared in other studies.
Although there were no re-operations for suture removal, there was one failure of fixation requiring revision and one non-union that was not revised. Both were in olecranon osteotomies. In the first case, there was propagation of the transverse ulnar tunnel through the dorsal cortex resulting in loss of suture tension. This was attributed to a technical error in placing the transverse tunnel too close to the dorsal cortex. In the second case, the reason for gapping and non-union was not established, as the patient was asymptomatic and no further intervention was performed. In both cases, intra-operative X-rays at the index procedure showed anatomic reduction of the osteotomy and no gapping under cyclic loading under direct vision. One possibility may be related to technique. The sutures were tied with the elbow extended to increase the tension of the construct and the inter-fragmentary compression during elbow flexion. The high tensile strength of the sutures and their increased tension during flexion may have led to ‘cheese wiring’ of the sutures through the bone. Another factor may be related to the fact that both cases occurred in olecranon osteotomies. Anecdotal experience suggests that osteotomies take longer to unite than an acute fracture. This could be related to several factors including: the more extensive soft tissue stripping performed to create a chevron osteotomy than to repair a fracture, heating of the bone and removal of a small amount of bone when creating an osteotomy and the lack of fracture haematoma and its biologic factors seen in an acute fracture. For these reasons and even though the results of osteotomy stabilization with sutures are satisfactory in this study, we recommend caution when performing the suture technique in osteotomies until experience is gained with simple fractures.
There are some limitations to this study. This was a retrospective analysis which has inherent limitations, one of which was the uneven numbers between the groups. Nevertheless, we feel the strict inclusion criteria (Mayo type 1 and 2 fractures only) and the relatively large number of patients in each group support the value of this study. Secondly, the follow-up times are different for the groups, which means there could have been complications related to the suture group with longer follow-up, although we feel that once bony union has occurred, it is unlikely that there will be any further reason for re-operation in the suture group, whereas in contrast, the need for wire removal or plate removal is likely to continue to increase over time. There may be bias in who performed the operations in each group. An attempt was made to control for this by including only consultant performed or supervised operations; however, only two surgeons (both specialist elbow surgeons) performed the suture fixations compared to six consultant trauma surgeons performing/supervising the TBW and plate fixations. However, there was only one failure of fixation in the TBW group, and the overall re-operation rate in the TBW and plate groups was comparable to the published literature, indicating that a sound technique was used for these cases.
A further possible limitation of the consultant-led nature of the surgery is whether the suture technique is reproducible by ‘non-specialist’ surgeons or surgeons in training. It is not possible to comment on this based on the results of this study; however, the technique is simple and does not require any additional skills to those used for TBW, so it is likely to have a relatively short learning curve for surgeons that are not familiar with it. Finally, patient-reported outcome measures were not collected as part of this study, as the focus was on re-operation rate, complications and radiographic union related to the three fixation methods.
Conclusion
All suture fixation had a significantly lower rate of re-operation compared to TBW and a lower but non-significant rate compared to plate fixation of Mayo type 1 and 2 olecranon fractures and osteotomies, without an increase in non-metal work related adverse events. The findings of this study suggest that suture fixation may be a viable alternative to the traditional methods of managing these fractures.
Footnotes
Contributorship: JP designed and wrote the study in conjunction with AW. TL, AV, JP and JW collected the data, performed data analysis.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical review and patient consent: Ethics committee application was deemed unnecessary by the local ethics board, as this was a service evaluation study without any patient contact outside normal treatment protocols. Patient consent was not requested for this study, as no new interventions or contact was made with the patients.
References
- 1.Brolin TJ, Throckmorton T. Olecranon fractures. Hand Clinics 2015; 31: 581–590. [DOI] [PubMed] [Google Scholar]
- 2.Duckworth AD, Clement ND, Aitken SA, et al. The epidemiology of fractures of the proximal ulna. Injury 2012; 43: 343–346. [DOI] [PubMed] [Google Scholar]
- 3.Duckworth AD, Bugler KE, Clement ND, et al. Nonoperative management of displaced olecranon fractures in low-demand elderly patients. J Bone Joint Surg Am 2014; 96: 67–72. [DOI] [PubMed] [Google Scholar]
- 4.Saeed ZM, Trickett RW, Yewlett AD, et al. Factors influencing K-wire migration in tension-band wiring of olecranon fractures. J Shoulder Elbow Surg 2014; 23: 1181–1186. [DOI] [PubMed] [Google Scholar]
- 5.Schliemann B, Raschke MJ, Groene P, et al. Comparison of tension band wiring and precontoured locking compression plate fixation in Mayo type IIA olecranon fractures. Acta Orthop Belg 2014; 80: 106–111. [PubMed] [Google Scholar]
- 6.Wilkerson JA, Rosenwasser MP. Surgical techniques of olecranon fractures. J Hand Surgery Am 2014; 39: 1606–1614. [DOI] [PubMed] [Google Scholar]
- 7.Amini MH, Azar FM, Wilson BR, et al. Comparison of outcomes and costs of tension-band and locking-plate osteosynthesis in transverse olecranon fractures: a matched-cohort study. Am J Orthop 2015; 44: E211–E215. [PubMed] [Google Scholar]
- 8.Claessen FMAP, Braun Y, Peters RM, et al. Factors Associated with reoperation after fixation of displaced olecranon fractures. Clin Orthop Relat Res 2016; 474: 193–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lovy AJ, Levy I, Keswani A, et al. Outcomes of displaced olecranon fractures treated with the olecranon sled. J Shoulder Elbow Surg 2018; 27: 393–397. [DOI] [PubMed] [Google Scholar]
- 10.Iannuzzi N, Dahners L. Excision and advancement in the treatment of comminuted olecranon fractures. J Orthop Trauma 2009; 23: 226–228. [DOI] [PubMed] [Google Scholar]
- 11.Ravenscroft MJ, Phillips N, Mulgrew E, et al. Suture anchor fixation of olecranon fractures: a case series. Shoulder Elbow 2013; 5: 116–119. [Google Scholar]
- 12.Phadnis J, Watts AC. Tension band suture fixation for olecranon fractures. Shoulder Elbow 2009; 9: 299–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nimura A, Nakagawa T, Wakabayashi Y, et al. Repair of olecranon fractures using fiberWire without metallic implants: report of two cases. J Orthop Surg Res 2010; 5: 73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Das AK, Jariwala A, Watts AC. Suture repair of simple transverse olecranon fractures and chevron olecranon osteotomy. Tech Hand Up Extrem Surg 2016; 20: 1–5. [DOI] [PubMed] [Google Scholar]
- 15.Bateman DK, Barlow JD, VanBeek C, et al. Suture anchor fixation of displaced olecranon fractures in the elderly: a case series and surgical technique. J Shoulder Elbow Surg 2015; 24: 1090–1097. [DOI] [PubMed] [Google Scholar]
- 16.van der Linden SC, van Kampen A, Jaarsma RL. K-wire position in tension-band wiring technique affects stability of wires and long-term outcome in surgical treatment of olecranon fractures. J Shoulder Elbow Surg 2012; 21: 405–411. [DOI] [PubMed] [Google Scholar]
- 17.Willinger L, Lucke M, Crönlein M, et al. Malpositioned olecranon fracture tension-band wiring results in proximal radioulnar synostosis. Eur J Med Res 2015; 20: 87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Parker JR, Conroy J, Campbell DA. Anterior interosseous nerve injury following tension band wiring of the olecranon. Injury 2005; 36: 1252–1253. [DOI] [PubMed] [Google Scholar]
- 19.Hume MC, Wiss DA. Olecranon fractures. A clinical and radiographic comparison of tension band wiring and plate fixation. Clin Orthop Relat Res 1992; 285: 229–235. [PubMed] [Google Scholar]