The opioid problem
Canada is experiencing a public health crisis related to the alarming number of cases of opioid-induced respiratory depression (OIRD) due to prescription and illicit opioids.1
From January to September 2019, there were 3799 opioid-related deaths across Canada, with the highest rates (per 100,000 population) in British Columbia, Alberta and Ontario.2 In all of 2018, there were 4372 opioid-related deaths, with the number of deaths having increased from 4150 in 2017 and 3025 in 2016.
In 2019, there were 3663 hospitalizations for opioid-related poisoning across Canada, with 5349 hospitalizations reported in all of 2018.2
According to Statistics Canada, the number of deaths due to OIRD is so great it has affected overall life expectancy.3 For the first time in more than 40 years, life expectancy has not increased in Canada, with a decrease reported in British Columbia and Alberta from 2016 to 2017. Life expectancy decreased by 0.28 and 0.05 years in British Columbia and by 0.21 and 0.08 years in Alberta for men and women, respectively.
Prescription opioids such as codeine, morphine, oxycodone and hydromorphone are frequently used for treating pain, one of the most common reasons for seeking health care in Canada.4
Approximately 1 in 8 (~4.7 million) people in Canada were prescribed opioids in 2018, representing a large number of people at risk for opioid-related toxicities and OIRD.4
OIRD is characterized by sedation, hypotension and respiratory depression, potentially resulting in respiratory failure and death.5
The use of naloxone has been instrumental in preventing opioid-related deaths by counteracting depression of the central nervous and respiratory systems related to opioid toxicity.6
Currently, take-home naloxone (THN) kits are publicly funded across all Canadian provinces and territories.1
In most provinces (with the exception of British Columbia, Saskatchewan and Alberta), naloxone is classified as a Schedule II drug, thereby requiring pharmacist intervention for sale. In the other provinces and territories, it is classified as unscheduled.1
As frontline health care professionals, pharmacists are ideally and uniquely positioned to assess patients who are receiving opioid therapy, providing a critical point of care in the patient journey for distributing naloxone. However, Canadian guidelines to advise pharmacists in identifying the appropriate patients for naloxone distribution and education do not exist.
A steering committee of 8 pharmacists from relevant practice and professional settings across Canada was convened to develop guidelines to provide the first recommendations for pharmacists on the use and distribution of naloxone.
Effectiveness of naloxone distribution programs
- THN programs have been shown to effectively reduce opioid-related deaths.
- In a systematic review of 22 observational studies to assess the effectiveness of THN programs, a fatal outcome was reported in 1 out of 123 OIRD cases (0.8%; 95% confidence interval = 0.4, 1.2). This is in comparison to 1 fatal outcome for every 20 cases of OIRD that has been documented in populations without naloxone intervention.7
- In Canada specifically, a British Columbia THN program providing low-barrier access to naloxone kits at no cost greatly reduced the number of deaths due to OIRD during a time when there was an increase in the number of fentanyl-related toxicities.8-10
- This THN program, launched in 2012, originally provided naloxone through harm reduction sites and community organizations where there was a high prevalence of OIRD. In December 2017, the program incorporated selected community pharmacies to provide naloxone to other places and populations with limited access to THN kits.
- Distribution records from participating pharmacies indicated that 3523 kits were distributed by 562 pharmacies between January 1, 2018, and December 31, 2018. As of June 15, 2019, 656 community pharmacies were participating.
- Qualitative interviews were performed to determine key strengths and challenges of the program. Key strengths included standardized procedures, standardized THN kits across the province, a centralized distribution model, close-knit teams and adequate training and resources. Key challenges included complicated pharmacy structures, lack of remuneration for pharmacists, communication gaps and logistical challenges such as lag in data entry.
- Inclusion of community pharmacies had several benefits: providing an opportunity to address stigma, increasing access to THN, screening patients for naloxone and providing education and highlighting pharmacists as key providers in addressing the opioid crisis.
Distribution of naloxone through community-based programs for substance users is associated with a decreased risk of OIRD at the community level.6 An observational time series analysis of opioid-related death and acute care utilization rates from 2002 to 2009 in 19 Massachusetts communities showed a reduction in death rates where opioid education and nasal naloxone distribution programs were implemented (adjusted death rate ratio: 0.54, 95% CI 0.39, 0.76 in high-implementation THN program areas).
Evaluations of THN programs have shown that they also encourage bystanders to take action when education is included.11 In a cross-sectional study of community support groups for family members of opioid users, attendees were highly motivated to receive training and use naloxone to rescue people when witnessing opioid-related toxicity.
Moreover, THN programs have been found to be cost-effective in the provision of naloxone to people using heroin.12
Therefore, increasing the availability and targeted distribution of naloxone is a critical component of continuing efforts to reduce OIRD deaths in Canada.
Pharmacists to the rescue: increasing naloxone distribution to those at risk
About one-quarter to one-third of opioid-related deaths in Ontario involve prescription opioids.13,14 In addition, approximately 80% of people assessed at an emergency department for opioid toxicity had received an opioid prescription in the previous 3 years.
The large population being prescribed opioids must therefore also be targeted with OIRD prevention strategies to reduce the risk of opioid-related deaths.
Pharmacists are uniquely positioned to distribute THN and educate people who are prescribed opioids.
- Despite the availability of these kits, naloxone dispensing by pharmacies is highly variable.
- A population-based study examining the uptake of THN in the Ontario Naloxone Program for Pharmacies in 2017 showed that only 55.6% of community pharmacies dispensed naloxone.13
- However, one-third (33.7%) of those THN kits were dispensed by the top 1% of naloxone-dispensing pharmacies.
- There was less uptake among prescription opioid recipients and those with past opioid exposure, regardless of their risk of OIRD.
- Over the 21-month study period, only 3918 of 55,000 (about 7%) of patients receiving high-dose opioids prescriptions (>90 mg morphine equivalents per day) were given THN in 2017.
Therefore, a need for pharmacists to increase the dispensing of THN kits to those prescribed opioids to prevent OIRD and possibly death is critical.
Patient selection for THN kits
Typically, patient selection guidelines for dispensing naloxone recommend using key risk factor criteria such as a history of OIRD or substance use disorder, higher opioid doses and concurrent benzodiazepine use15-18 (Appendix 1, available online at www.cpjournal.ca).
- However, risk factor information is not easy to acquire, as the stigma related to substance use disorders may prevent people from disclosing this information accurately.
- People may also use multiple pharmacies to acquire medications, making it difficult to determine whether they are taking benzodiazepines or other medications that increase their risk. They may also obtain these substances through the illicit market.
- In addition, the criteria do not consider the risk to other family members who live in the home.
- Many patients do not perceive their need for THN; therefore, a proactive, structured approach by pharmacists is needed.
- The benefit of having naloxone kits available in cases of emergency outweighs the drawbacks of dispensing those that end up not being used.
- Given the difficulties in assessing the potential risk of OIRD, naloxone kits should be distributed to anyone who is prescribed an opioid.
Recommendation.
All patients receiving an opioid should be dispensed take-home naloxone and counselled by a pharmacist.
Practice implementation tips
- Pharmacists must be proactive in addressing the need for naloxone.
- People may not feel comfortable asking for naloxone due to stigma, including feelings of shame around opioid use or addiction.
- Long-term opioid users may have a false sense of security.
- People may associate OIRD with illicit use only, not prescription opioids, and may not have considered the possibility of accidental or intentional ingestion of opioid medications by family members.
- People may not be aware that THN kits are available at no cost from community pharmacists, although a valid Health Card may be required in some provinces and territories.
- Pharmacists need to accept and feel confident in their role as educators on prevention of OIRD.
- It is important for pharmacists to take the lead by approaching those who may benefit from naloxone.
- Given the stigma associated with opioid use, pharmacists need to be sensitive when discussing the use of naloxone.
- Use of language that reduces the stigma can help in increasing openness within discussions. For example, pharmacists can describe overdose in a technical way such as “opioid-induced respiratory depression,” which can be described as “slowed breathing” (an adverse effect that can occur in any person, regardless of the opioid used or the reason for use).
- Pharmacists can make it clear that they counsel all people who have an opioid prescription on the use of naloxone: “We give this to all patients using these medications.” This normalizes the dispensing of THN kits for patients using opioids.
- Strategically placed signage at prescription pick-up and drop-off can act as a conversation starter with patients and demystify stigma around age, gender, ethnicity and diversity.
- The discussion around naloxone can be built into the patient consultation on the adverse effects of opioids. For example, use of naloxone can be introduced when discussing that people cannot drive, may get constipation and may experience heavy sedation with opioid use.
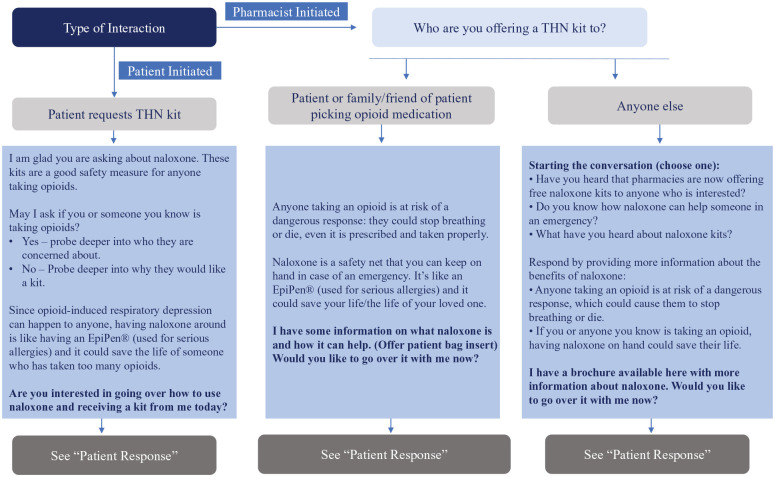
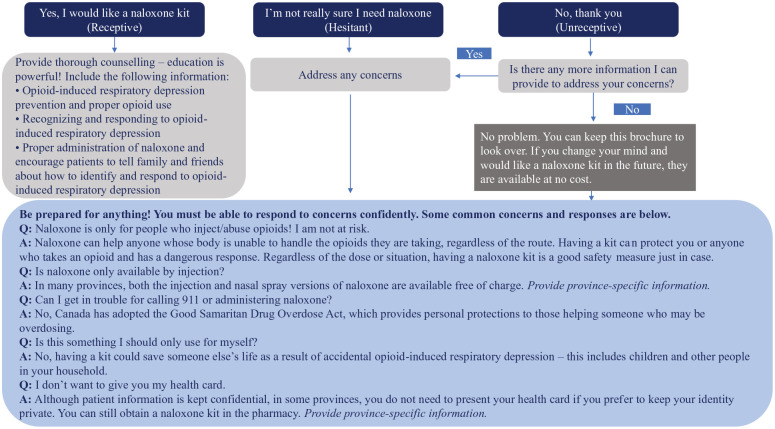
Following a script can be helpful in discussing the use of naloxone. See Figures 1 and 2 for step-by-step instructions that can aid in interactions with those who are eligible.
Figure 1.
Clinical tool: Pharmacist script based on type of interaction
THN, take home naloxone
Adapted with permission from the Ontario Pharmacists Association.16
Figure 2.
Clinical tool: Pharmacist script based on patient response
Adapted with permission from the Ontario Pharmacists Association.16
Patient follow-up
- It is important to follow up with patients to make sure naloxone kits have not expired.
- An alert could be set as a refill reminder to notify pharmacists to call patients. Note that replacement naloxone kits are also free to patients through THN programs in most provinces and territories.
- The follow-up communication points provide a critical opportunity to reinforce naloxone education.
If a naloxone kit has not been dispensed previously, changes in opioid prescriptions or the addition of a benzodiazepine, or other risk factor changes, are important opportunities to revisit offering a naloxone kit.
Recommendation.
Reminders should be set to follow up with people after 3 months and at 1 year after dispensing take-home naloxone. Ongoing yearly follow-up is recommended to ensure THN kits have not expired and reinforce overdose prevention education.
Conclusions
THN is a critical intervention to reduce opioid deaths; however, current distribution of the kits is insufficient to provide access to all those at risk.
Pharmacists are accessible and uniquely placed to screen patients and provide THN to prevent opioid-related deaths.
The federal and provincial/territorial governments have removed barriers to accessing naloxone by expanding pharmacist scope of practice, thereby promoting their ability to intervene effectively.
Patients prescribed opioids do not typically ask for naloxone and may be unaware of or fail to disclose the risk of OIRD for themselves and/or others in their household.
We therefore recommend that pharmacists provide naloxone proactively to all patients receiving opioids.
Follow-up with patients after 3 months and at 1 year after dispensing naloxone is recommended. Ongoing yearly follow-up is also recommended to ensure the kit has not expired and to reinforce OIRD prevention education.
Implementation strategies for initiating naloxone discussions with patients are suggested here but require further refinement and evaluation. ■
Supplemental Material
Supplemental material, sj-pdf-1-cph-10.1177_1715163520949973 for Canadian national consensus guidelines for naloxone prescribing by pharmacists by Ross T. Tsuyuki, Vinita Arora, Mark Barnes, Michael A. Beazely, Michael Boivin, Anna Christofides, Harsit Patel, Julie Laroche, Aaron Sihota and Randy So in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada
Supplemental material, sj-pdf-2-cph-10.1177_1715163520949973 for Canadian national consensus guidelines for naloxone prescribing by pharmacists by Ross T. Tsuyuki, Vinita Arora, Mark Barnes, Michael A. Beazely, Michael Boivin, Anna Christofides, Harsit Patel, Julie Laroche, Aaron Sihota and Randy So in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada
Footnotes
Author Contributions:R. Tsuyuki and A. Christofides wrote the initial draft of the article. All authors reviewed and revised the article. All authors approved the final version of the article.
Declaration of Conflicting Interests:With the exception of Mr. Barnes, all authors received consulting fees related to the preparation of this article. Dr. Tsuyuki has received consulting or speaking fees from Emergent BioSolutions, Sanofi and Shoppers Drug Mart. He has received investigator-initiated research grants from Merck and Sanofi in the past 5 years. He is the president of SMHEART CONSULTING, Inc. Mr. Barnes reports ownership of a community-based, ambulatory, addiction-focused pharmacy where naloxone is dispensed. He receives commercial terms and training fees for the professional dispensing of naloxone. The other authors declare no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding:Funding provided by Emergent BioSolutions for medical writing services through an unrestricted grant. Emergent BioSolutions has also paid the full cost of the open access fee.
ORCID iD:Anna Christofides  https://orcid.org/0000-0001-6421-8728
https://orcid.org/0000-0001-6421-8728
French guidelines are available at https://journals.sagepub.com/doi/suppl/10.1177/1715163520949973/suppl_file/sj-pdf-2-cph-10.1177_1715163520949973.pdf
References
- 1. Canadian Research Initiative in Substance Misuse. Environmental scan: naloxone access and distribution in Canada. June 2019. Available: https://crism.ca/2019/06/13/naloxone-distribution-environmental-scan/ (accessed Jul. 15, 2020).
- 2. Government of Canada. Opioid-related harms in Canada Available: https://health-infobase.canada.ca/substance-related-harms/opioids/maps?index=15 (accessed Apr. 10, 2020).
- 3. Statistics Canada. Changes in life expectancy by selected causes of death, 2017. Available: https://www150.statcan.gc.ca/n1/daily-quotidien/190530/dq190530d-eng.htm
- 4. Canadian Institute for Health Information. Opioid prescribing in Canada: how are practices changing? 2019. Available: https://www.cihi.ca/sites/default/files/document/opioid-prescribing-canada-trends-en-web.pdf (accessed Apr. 10, 2020).
- 5. Pattinson KT. Opioids and the control of respiration. Br J Anaesth. 2008;100(6):747-58. [DOI] [PubMed] [Google Scholar]
- 6. Walley AY, Xuan Z, Hackman HH, et al. Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. BMJ. 2013;346:f174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McDonald R, Strang J. Are take-home naloxone programmes effective? Systematic review utilizing application of the Bradford Hill criteria. Addiction. 2016;111(7):1177-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mamdani Z BJ. Evaluation of British Columbia’s take home naloxone program in community pharmacies. Vancouver: BC Centre for Disease Control; 2019. [Google Scholar]
- 9. Irvine MA, Buxton JA, Otterstatter M, et al. Distribution of take-home opioid antagonist kits during a synthetic opioid epidemic in British Columbia, Canada: a modelling study. Lancet Public Health. 2018;3(5):e218-e25. [DOI] [PubMed] [Google Scholar]
- 10. Young S, Williams S, Otterstatter M, Lee J, Buxton J. Lessons learned from ramping up a Canadian take home naloxone programme during a public health emergency: a mixed-methods study. BMJ Open. 2019;9(10):e030046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bagley SM, Peterson J, Cheng DM, et al. Overdose education and naloxone rescue kits for family members of individuals who use opioids: characteristics, motivations and naloxone use. Subst Abuse. 2015;36(2):149-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Langham S, Wright A, Kenworthy J, Grieve R, Dunlop WCN. Cost-effectiveness of take-home naloxone for the prevention of overdose fatalities among heroin users in the United Kingdom. Value Health. 2018;21(4):407-15. [DOI] [PubMed] [Google Scholar]
- 13. Choremis B, Campbell T, Tadrous M, Martins D, Antoniou T, Gomes T. The uptake of the pharmacy-dispensed naloxone kit program in Ontario: a population-based study. PloS One. 2019;14(10):e0223589-e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Gomes T, Khuu W, Martins D, et al. Contributions of prescribed and non-prescribed opioids to opioid related deaths: population based cohort study in Ontario, Canada. BMJ. 2018;362:k3207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Dowell DHT, Chou R. CDC guideline for prescribing opioids for chronic pain—United States. MMWR Recomm Rep. 2016;65(No. RR-1). [DOI] [PubMed] [Google Scholar]
- 16. Ontario Pharmacists Association. Pharmacist clinical tool. Available: https://www.opatoday.com/Media/Default/Tools%20and%20Forms%20-%20Naloxone/Naloxone%20Clinical%20Tool%20-%2020190918.pdf (accessed Apr. 10, 2020).
- 17. U.S. Department of Health & Human Services. U.S. surgeon general’s advisory on naloxone and opioid overdose. Available: https://www.hhs.gov/surgeongeneral/priorities/opioids-and-addiction/naloxone-advisory/index.html (accessed Apr. 10, 2020).
- 18. Government of Quebec. Risks of opioid overdose. Available: https://www.quebec.ca/en/health/advice-and-prevention/alcohol-drugs-gambling/risks-of-opioid-use/#c27022 (accessed Apr. 10, 2020).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-cph-10.1177_1715163520949973 for Canadian national consensus guidelines for naloxone prescribing by pharmacists by Ross T. Tsuyuki, Vinita Arora, Mark Barnes, Michael A. Beazely, Michael Boivin, Anna Christofides, Harsit Patel, Julie Laroche, Aaron Sihota and Randy So in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada
Supplemental material, sj-pdf-2-cph-10.1177_1715163520949973 for Canadian national consensus guidelines for naloxone prescribing by pharmacists by Ross T. Tsuyuki, Vinita Arora, Mark Barnes, Michael A. Beazely, Michael Boivin, Anna Christofides, Harsit Patel, Julie Laroche, Aaron Sihota and Randy So in Canadian Pharmacists Journal / Revue des Pharmaciens du Canada