The Spanish flu, a virulent and previously unknown form of influenza, reared its ugly head in Canada in 1918 and remained a serious threat into 1920. Nearly 55,000 Canadians, most of them in the prime of their lives, were killed by the virus.1 As we experience the early months of the COVID-19 pandemic* and hear of pharmacists working on the front lines, it seems appropriate to step back in time and think about the pharmacists who went before us, the ones who ran the pharmacies during the Spanish influenza pandemic. What was it like to be a pharmacist back then? What were the pharmacies like? What drugs were used? What were pharmacists’ concerns and how did they cope? The following is a snapshot of some of our pharmacy history from just over 100 years ago.
Pharmacy practice in 1918
When Spanish influenza arrived, the majority of pharmacists in Canada were “retail druggists” practising in drugstores. These pharmacies were owned and operated by individual pharmacists (and, in some cases, physicians) registered and licensed through provincial pharmacy bodies and governed by Pharmacy Acts.2 It was not uncommon for a pharmacist to operate more than 1 drugstore in a community, with the additional locations known as branch stores. Chain drugstores, already in place in England and the United States, were on the verge of taking hold in Canada and were being observed with both interest and concern.3
The pharmacists of the day were a mix of those who had learned “the craft” through pharmacy apprenticeship alone and those who had the benefit of formal education along with apprenticeship.4 The first 3 institutions to offer formal pharmacy education in Canada were the Montreal College of Pharmacy (1868), the Ontario College of Pharmacy (1882) and the Manitoba College of Pharmacy (1889).5 Women began qualifying as pharmacists in noticeable numbers in the first years of the 20th century, and this increased during the war years of 1914 to 1918.6,7 Although they were in the minority, some pharmacies were managed by women.7 In Nova Scotia, pharmacist Carrie Kinley, who also had 3 brothers in the profession, was the manager of the Kinley family’s drugstore in Bridgewater in 1919.8
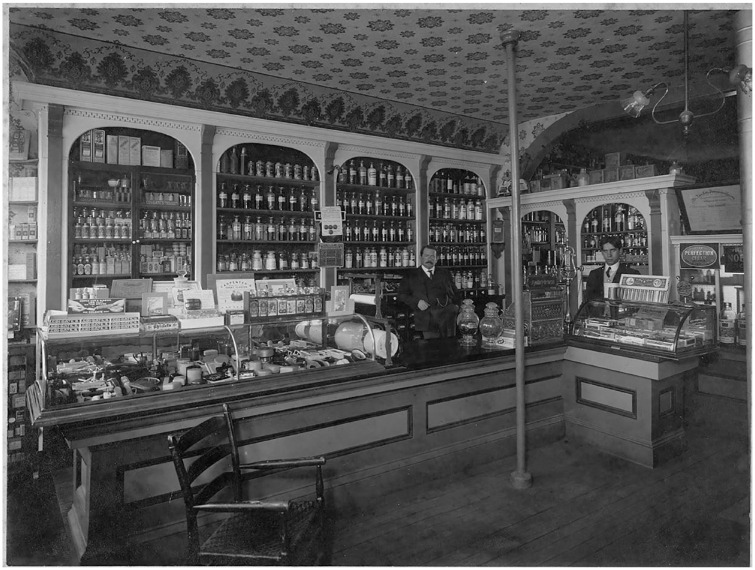
Prescriptions were written by physicians and brought to drugstores by customers, where they were compounded by pharmacists. The medicines compounded generally contained 3 or more ingredients and took considerable time and skill to prepare. The pharmacist did the compounding on a counter at the back of the store located behind decorative doors or a curtain, out of sight of the customer. This gave a degree of mystery to the medicine when the pharmacist emerged with the finished product. Pharmacists also stocked patent medicines and prepared proprietary preparations of their own for sale within their drugstores.2 These included a variety of items from cough syrup to household cleaners to toiletries such as shampoo and rose water. It was popular to arrange displays of seasonal items or special product lines in store windows to attract customers. Many pharmacists believed they could not rely on drug and prescription sales alone and included business sidelines such as photography, optometry, soda fountains, books and more. Drugstores featured decorative wooden shelving, oak counters, glass-stoppered medicine bottles and enclosed glass display cases (Figure 1).9
Figure 1.
Interior of Holdsworth’s Drug Store, Digby, NS, ca 1910
Courtesy Dr. J. Gordon Duff Pharmacy Museum, College of Pharmacy, Dalhousie University, Halifax, NS.
Drugstores were typically open 15 hours a day and 7 days a week. At the fourth convention of the Canadian Pharmaceutical Association in 1911, Halifax-based pharmacist, J. H. Angwin, presented a paper strongly encouraging limiting evening and Sunday hours to give pharmacists more time for family and recreation.10 This idea arose time and time again in the years that followed but, for the most part, did not take root.
Impact of Spanish influenza on pharmacies
The drugstores were overwhelmed. The National Drug News, written and distributed by the National Drug and Chemical Company of Canada, described the situation as follows:
Retail druggists throughout the country are alive to the situation; that they are using their knowledge and influence to help stamp out the disease goes without saying. Next to the physician they know better than anyone else the common sense methods of prevention.
The demand for certain drugs and preventative agents has been unprecedented. Rules of labour and hours of work have been swept aside and all from the messenger boy to the proprietor have turned in to do their bit. We believe this is true in every branch of the drug trade—wholesale, retail and manufacturing.11
Staffing in the drugstores was already at a premium before the flu hit. Many pharmacists and drug clerks had joined the war effort, either by choice or by conscription, and were serving overseas.12 Pharmacists and clerks at home had little choice but to roll up their sleeves and get to work. They dealt with the greatly increased prescription volume by closing the stores for a few hours during the day and working even later into the night. Pharmacy students, sent home when the colleges were closed due to the pandemic, were welcomed in the dispensaries.13,14 The Bulletin of Pharmacy provides valuable insight into how several American pharmacists coped with the increased workload in their drugstores.15 The main focus of their stores became filling prescriptions. The sale of toiletries was suspended except for those needed in the sickroom, as were other business aspects such as making creams and cosmetics and running the soda fountain.15 They recruited inexperienced staff to serve the public, to reply to questions that did not require professional attention and to answer the telephone.15 When wholesalers and manufacturers were unable to deliver on orders for chemicals, messengers were sent directly to their sites to obtain as much as was available.15 It was a stressful time, to say the least, made all the worse when pharmacists, their family members and staff also fell ill to the flu.16,17
The obituaries of well-loved Canadian pharmacists and store managers who died from the flu began appearing in the Canadian Pharmaceutical Journal (the former name of the Canadian Pharmacists Journal) in late 1918. One of these obituaries honours 25-year-old Edward G. Dann, who died December 4, 1918.17 Two years before, he had taken over the management of several pharmacies in London, Ontario, while Capt. Fred Taylor, founder of Taylor drugstores, went overseas. Dann, who was not a pharmacist, but “on the last lap of his pharmacy course,” put his formal education on hold to take on this responsibility. His untimely death was described as a recurrence of the flu. He was first stricken 5 weeks before he died. He “overcame it” and soon was back at work. The Wednesday before he died, he became ill again, soon felt better and returned to work. On Saturday, he was “taken to his bed,” grew worse and died that evening. The cause of death was “double pneumonia.”
Drugs for preventing and treating Spanish influenza
Preventatives
Experience gained through the influenza pandemic of 1889 to 1890 helped set in place principles for the prevention of Spanish flu.18 It was deemed important to keep away from those who were infected and to build up the “germ-resisting” defenses of the body by getting fresh air, having plenty of sleep and keeping well nourished.18 Great hope was placed on vaccines.19 Richard Pfeiffer first isolated and identified a bacillus in 1892 that was thought to be the causative agent of influenza infection.19 Connaught Antitoxin Laboratories in Toronto used strains of the Bacillus influenzae, also known as Pfeiffer’s bacillus, obtained in New York, to develop a vaccine. This vaccine was distributed free of charge to provincial health boards, hospitals and medical officers in October 1918.20 Looking back, physicians doubted that it did much good, blaming some of the problem on the arrival of the vaccine after Spanish influenza was dying out.21 Vaccines were developed in other parts of Canada, notably Winnipeg, where a lab made a “mixed-strain” vaccine similar to one prepared by Edward C. Rosenow at the Mayo Clinic, Rochester, Minnesota.20 This vaccine was prepared using strains of pneumococcus and streptococcus, along with Bacillus influenzae. Some thought that this vaccine was beneficial and helped protect patients from the deadly complication of pneumonia.22 The virus that caused the Spanish flu was not isolated until 1933.20 With this new knowledge, the vaccines produced during the pandemic of 1918 to 1920 are considered to have been of little use.
Pharmacist and educator Robert Fischelis published a series of articles in the Montreal Pharmaceutical Journal in 1919 encouraging “retail druggists” to become familiar with biologicals, such as vaccines, and to stock them in their drugstores.23,24 He suggested that physicians were hard-pressed to keep up with the rapid advances in bacteriology and immunology and that since they already were going to pharmacists for information on drug products that they would soon learn to do the same for vaccines, antitoxins and serums.23 I was unable to find any published evidence to demonstrate that Canadian pharmacists played a major role in the procurement and distribution of vaccines during the years of Spanish flu, but perhaps they did. O. F. Wolf, president of McKennan Pharmacy in Pittsburgh, Pennsylvania, described how difficult it was to obtain the influenza vaccine during the epidemic and how quickly the supply was depleted when they managed to get some in stock for physicians.15 They were able to “take care of a large volume of business” by limiting supply to the first inoculation, of what presumably was a 3-dose series, with the promise to deliver on the second and third inoculations when the time came.15
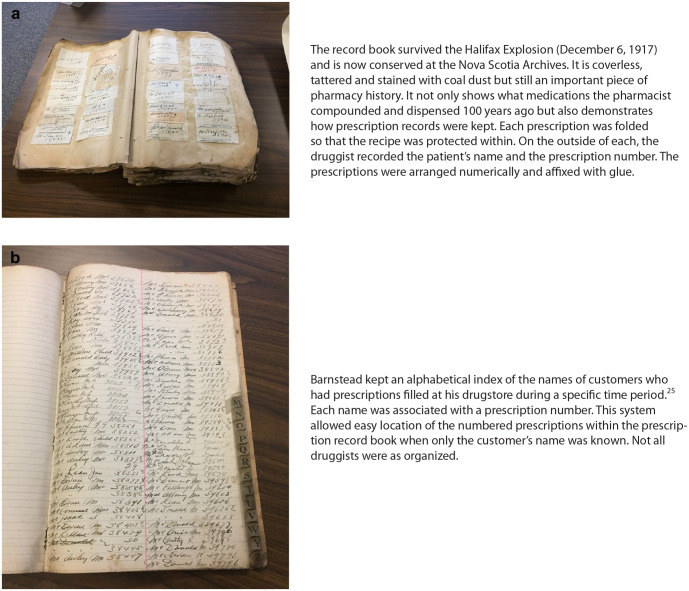
Another principle of prevention was to keep the mouth, throat and nose diligently protected through use of disinfecting washes and inhalations.18 The October 1918 prescription records of Charles A. Barnstead, a pharmacist who operated a drugstore on Granville Street in Halifax, show multiple scripts for preparations used to sanitize the nose and oral cavity (Figure 2).25 Examples of such prescriptions are 1) chloretone inhalant plus camphor and phenol, with the resulting solution to be used in an atomizer 3 or 4 times daily, and 2) a preparation mixing menthol, eucalyptus oil and carbolic acid, to be administered by adding it to hot water and inhaling the steam frequently. As well, prescriptions for the commercially available antiseptics Euthymol (used as a nasal spray), Borol (used as a nasal wash and gargle) and Listerine (used as a gargle) were also common.25 There are several unique prescriptions secured in the prescription book in early October, just when people were beginning to fall ill. These prescriptions are neither handwritten nor signed by a physician but appear to have been clipped from a newspaper. They are attributed to someone identified as “a medical well-wisher” and include advice as well as a recipe (Figure 3).25
Figure 2.
Charles A. Barnstead’s prescription record book for 1917 and 191825
Courtesy of the Nova Scotia Archives.
Figure 3.
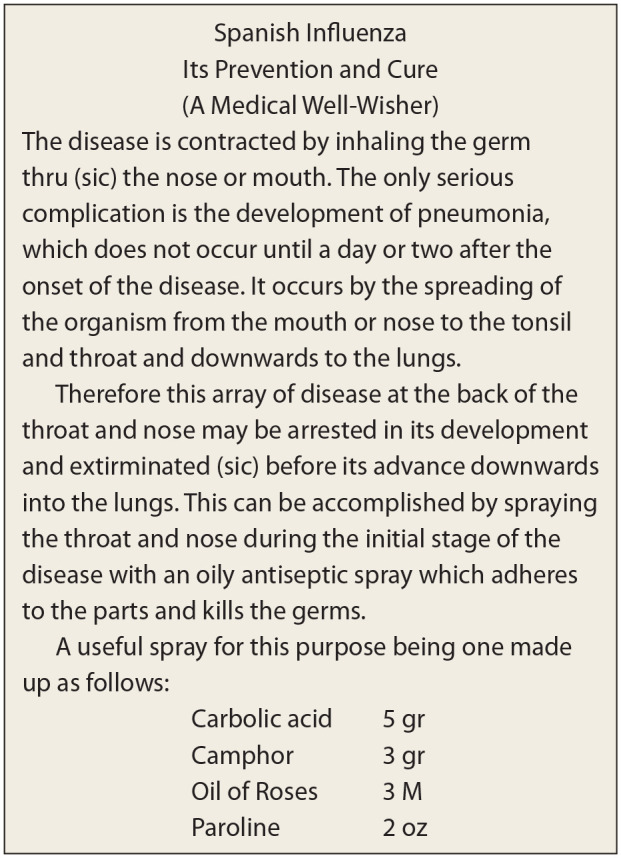
Copy of the unique prescription, clipped from a newspaper, which appeared several times in the prescription records of Charles A. Barnstead, Halifax, NS, October 191825
Courtesy of the Nova Scotia Archives.
Treatment
Physician F. H. Wetmore, from Hampton, NB, published a paper on the prophylaxis and treatment of influenza in the Canadian Medical Association Journal in 1919.22 He provided his colleagues with many details that give us a sense today of the treatments believed to be important at that time. For his “curative treatment,” he advocated a number of rules of general management: “absolute rest in bed from the first,” fresh air through an open window, good nursing care and a liquid diet of milk mixed with either limewater or raw eggs that was fed around the clock if the illness was serious. Medicines to be procured from a drugstore were Epsom salts, a vile-tasting and rapidly acting laxative, supplemented with a second laxative, calomel (mercury chloride), if the patient vomited the Epsom salts, acetylsalicylic acid for pains and a “moderate dose” of heroin (1/12 grain) for cough. It is possible that Wetmore’s cough preparation followed the recipe for Elixir of Terpin Hydrate and Heroin found in the Canadian Formulary of Unofficial Preparations from 1908. Each fluid dram (5 mL) of prepared elixir contained 1 grain terpin hydrate, a mucolytic and 1/24 grain heroin hydrochloride.26
Wetmore stressed the importance of having a good nurse present to make sure the patient followed orders, especially with regard to rest and nourishment and to ensure that enough laxative was used daily to clear the primae viae (digestive tract). Acidosis was to be prevented, and this was done by administering doses of sodium bicarbonate and citrate of potash alternatively every hour until no longer needed. In those cases where “vaso-motor paresis” occurred, adrenaline chloride was used. To treat circulatory failure accompanying pneumonia, digitalis tincture, with or without alcoholic stimulation (half-ounce doses), was the treatment. If the patient became dangerously toxemic, then the directive was to use alcoholic stimulation freely. Wetmore recognized that in a patient with pneumonia and high fever, the removal of serous fluid from a localized pleural effusion with a needle could sometimes be helpful for the patient’s recovery. (The first antibiotics, penicillin and streptomycin, would not be available for civilian patient use until the mid-1940s.27 It was the mid-to-late 1960s before amantadine was used as an antiviral for the prevention and treatment of influenza A.28)
A convalescing case was to remain in bed 3 to 10 days once the fever subsided. The following tonic was prescribed to be taken after meals: quinine hydrochloride 1/4 to 1/2 grain, dilute hydrochloric acid 10 Minims (M) and tincture nux vomica 5–10 M made up to 1 dram with essence of pepsin.22
Drugs in short supply
Camphor and quinine were 2 drugs in high demand and also hard for pharmacists to obtain. Camphor was extracted from trees (Cinnamonum camphora) grown in Japan and China, and it was in short supply due to restrictions around import brought on by World War I.29 Although clinical proof was lacking, there was belief that since camphor was useful in the treatment of colds and bronchitis, it should also be useful in the treatment of influenza.30 The effluvia from crystalized camphor (gum camphor), inhaled, 1 nostril at a time, was valued as a flu preventative. The fumes could be accentuated by burning the camphor in a metal pot or heating it on the stove.30 Another method of using camphor as a preventative was recommended by some doctors and renounced as a waste of time by others. It involved placing gum camphor in a muslin sack and wearing it around the neck to ward off germs!31 Alternatively, the little bag could be carried, one in an inside pocket, with a second conveniently placed in an outside pocket so it could readily be held near the nose when out in public.31 A writer with the Nelson BC Daily News casually referred to the small bag of camphor seen hanging from the necks of children as “the little white bag that says boo to the flu.”32
Quinine had a reputation as a useful preventative in previous epidemics and was in demand for the Spanish flu for its “anti-microbic” properties.18 It could be used as an antiseptic gargle (1 grain quinine sulphate mixed, but not dissolved, in a wineglassful of cold water) for sore throat.18 It was also purported to be a useful preventative taken internally, as determined in a study of cavalry squadrons in Europe. Squadron members who were administered daily doses of 7½ grains quinine in ½ ounce of whiskey for 3 weeks had only 4 cases of flu as compared to squadrons who received none that had 22 to 44 cases.18
Alcohol also presented problems for pharmacists. Prohibition was enacted at the start of World War I, and the use of intoxicating beverages was banned across Canada. One of the exceptions to Prohibition was alcohol for medicinal use, and it was due to this exception that pharmacists found themselves being gatekeepers of a much sought-after commodity. Alcohol could relieve the pains of flu in both body and mind and serve as a restorative or a stimulant. Alcohol supplies in drugstores were regularly depleted, and this was especially so at the time of Spanish influenza. Some of the demand was handled through the use of patent medicines with high alcohol content; sources of illicit alcohol were also common, and customers would also seek out their relief from these sources.33 How the control of alcohol for medicinal purposes was carried out in the provinces varied, but dispensing alcohol appears to have been a matter of some stress for pharmacists.34 A physician’s prescription was required, although at times of emergency, the need for a prescription could be ignored.34 The maximum quantity to be supplied, no matter the circumstances, was 6 ounces. The pharmacist was required to keep precise records. A case of a forged prescription for alcohol, filled by a clerk in Ontario, brought a fine of $300 to the pharmacist in charge in 1915. It was warned that a second infraction could lead to a 2-year cancellation of the pharmacist’s certificate to practise.34 The overall hassle plus the heavy fines and restrictions for noncompliance made some pharmacists grumble about being alcohol suppliers.
Insight from a drug wholesaler
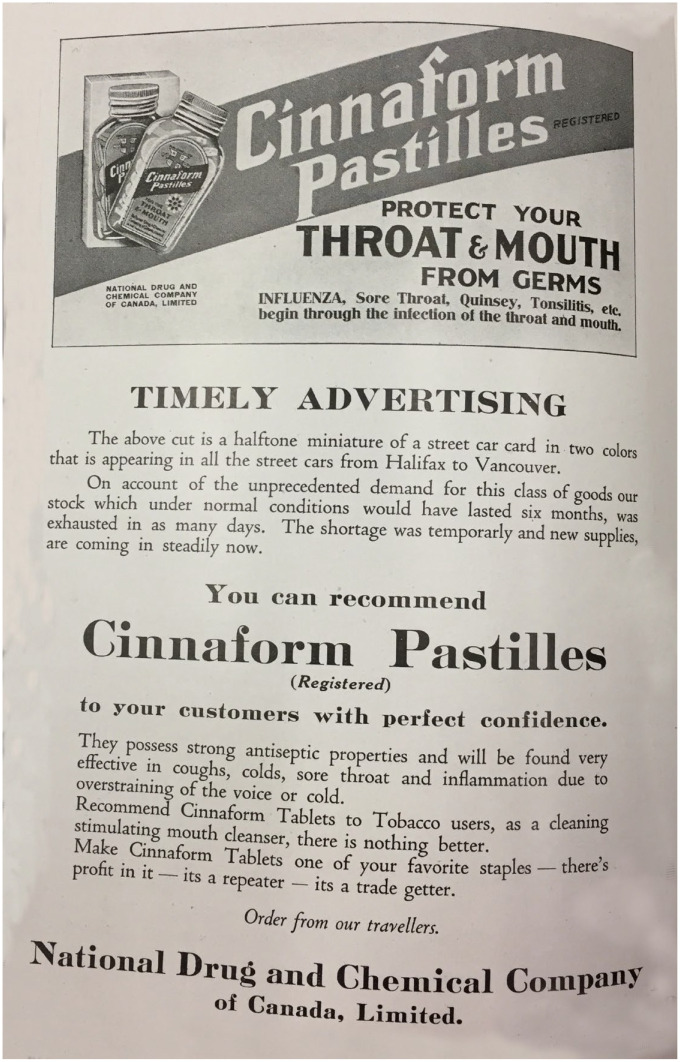
The National Drug and Chemical Company (Na-Dru-Co) became a national entity as a drug wholesaler in 1906 when it brought together, under one banner, many small drug wholesale companies operated by pharmacists.35 They maintained a strong tie with pharmacy and considered they were a branch of the profession. Their National Drug News, written for and distributed to pharmacists, sheds light on the products that were in high demand in pharmacies in October 1918. Unprecedented orders were received by Na-Dru-Co for the quinine product known as CBQ (Cascara Bromide Quinine).36 A pharmacist in Ontario who sold 23 dozen packages of CBQ between October 7 and 31 claimed that in 33 years of practice, he had never had a product sell so quickly.36 Supplies of Zycol, a saponified creosol disinfectant, were completely depleted in 2 weeks, despite the fact that Na-Dru-Co had sufficient stock on hand to last for 2 years in normal times.37 They also were “swept off their feet” with demands for Cinnaform Tablets.38 This oil of cinnamon and formaldehyde tablet benefitted from the endorsement of a doctor in Victoria, BC. It was said that if a person with influenza took Cinnaform within a few hours of onset of flu symptoms, that in all likelihood, the person could return to work within 48 hours.38
Na-Dru-Co was lavish in its praise for staff who worked nights, Sundays and holidays to try to fulfill the pharmacies’ orders, doing the extra work “without a murmur.” They lamented that they sometimes were not able to meet the requirements of the drugstores and had “shorts.” They claimed that they could have overcome the orders of unprecedented quantities had it not been for exasperating delays and red tape in place because of war measures.11
There were many advertisements for “National” products on the pages of their periodical. Some simply listed the names of products with the advice that they were all worthy of being recommended for influenza. One ad was a miniature of an advertisement for Cinnaform Pastilles, which was “appearing in street cars from Halifax to Vancouver.”39 Business-minded pharmacists would find it hard to ignore such a tempting “heads-up” (Figure 4).
Figure 4.
Example of high-pressure advertising for Cinnaform Pastilles, a product of the National Drug and Chemical Company
Published in National Drug News, November 1918.39
Reflection
While devastating to the community, it cannot be denied that the Spanish influenza was a boon to drug businesses.40 People flocked to pharmacies focused on procuring what was deemed necessary at the time to prevent being sick. For those dealing with the illness, the fear of dying was as great as the wish to return to good health. Pharmacists stayed where they were needed, compounding prescriptions and serving the community in need.
Historians tell us that history helps us understand people, changes and the societies in which we live.41 Certainly there are many differences in the preventatives and treatments used for infectious diseases since the time of Spanish influenza. These practices have changed and no doubt will change again over the next 100 years. Yet there are undeniable similarities between the Spanish influenza pandemic and the current COVID-19 pandemic. The lingering fear of an illness with no cure hangs over us; people want and need help from pharmacists at an alarming rate; pharmacists work long hours to meet the public’s medication needs; pharmacists continue to deal with a faltering drug supply.
Can we learn from this slice of pharmacy history? Pharmacists from 100 years ago made it through the challenges of Spanish flu. It was not easy; their mettle was tested. With determination and self-sacrifice, they helped others with their special skills and knowledge. It is hoped that learning what pharmacists did in the past will help instill pride in the profession and give strength and encouragement to pharmacists on the front lines today. ■
Declaration of Conflicting Interests:The author declares no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding:The author received no financial support for the research, authorship and/or publication of this article.
ORCID iD:Mary E. MacCara  https://orcid.org/0000-0003-3634-5863
https://orcid.org/0000-0003-3634-5863
The World Health Organization declared COVID-19 as a pandemic on March 11, 2020. This paper was written in May, 2020.
References
- 1. Parks Canada History and Culture. The Spanish flu in Canada (1918-1920). Available: https://www.pc.gc.ca/en/culture/clmhc-hsmbc/res/doc/information-backgrounder/espagnole-spanish (accessed May 11, 2020).
- 2. Rantucci M, editor. Evolution of pharmacy practice. In: Canadian Pharmacists Association 1907-2007: 100 years of leadership in pharmacy. Ottawa (ON): Canadian Pharmacists Association; 2007. p. 65-76. [Google Scholar]
- 3. Drefs CA. How the single drugstore can successfully compete with the chain stores. Can Druggist 1914;26(2):115-6. Available: https://archive.org/details/canadiandruggist26torouoft/page/114/mode/2up (accessed May 25, 2020). [Google Scholar]
- 4. Raison AV, editor. A brief history of pharmacy in Canada. Toronto: Canadian Pharmaceutical Association; 1968. [Google Scholar]
- 5. MacCara ME. Dispensing knowledge: one hundred years of the college of pharmacy. Tantallon, NS: Glen Margaret Publishing; 2012. [Google Scholar]
- 6. Women in pharmacy. Can Pharm J 1918; 51(11):484. [Google Scholar]
- 7. Stieb EW, Coulas GC, Ferguson JA, Clark RJ, Hornosty RW. Women in Ontario pharmacy, 1867-1927, in commemoration of the centenary of the first admission of women to the University of Toronto, 1984-85. Pharm Hist 1986; 28(3):125-34. [PubMed] [Google Scholar]
- 8. Index of pharmacists 1875-1930. J. Gordon Duff fonds. MS-13-82 Box 38. Dalhousie University Archives, Halifax, Nova Scotia, Canada. [Google Scholar]
- 9. Photograph Holdsworth’s Drugstore, Digby, Nova Scotia ca. 1910. Dr. J. Gordon Duff Pharmacy Museum, College of Pharmacy, Dalhousie University. [Google Scholar]
- 10. Angwin JH. Druggists’ hours. Can Druggist 1911;23(10):642-3. Available: https://archive.org/details/canadiandruggist23torouoft/page/642/mode/2up (accessed May 11, 2020). [Google Scholar]
- 11. The epidemic. Natl Drug News 1918;13(1-12):6-7. [Google Scholar]
- 12. MacCara ME. Dispensing aid: druggists and the Halifax explosion. Tantallon, NS: Glen Margaret Publishing; 2017. [Google Scholar]
- 13. Ontario College of Pharmacy. Pharm Era 1918;51(12):358. Available: https://archive.org/details/pharmaceuticaler51newyuoft/page/358/mode/2up (accessed May 13, 2020). [Google Scholar]
- 14. Steele JW. The University of Manitoba history of the faculty of pharmacy 1899-1999. Winnipeg, Canada: Faculty of Pharmacy, University of Manitoba; 1999. [Google Scholar]
- 15. When the influenza struck us—letters from druggists who give personal experiences. Bull Pharm 1918;32(pt 2):494-7. Available: https://babel.hathitrust.org/cgi/pt?id=hvd.hc4ed7&view=1up&seq=514 (accessed May 11, 2020). [Google Scholar]
- 16. Halifax & Nova Scotia news. Natl Drug News 1918;13(1-12):18. [Google Scholar]
- 17. Obituary Mr. E. Dann. Can Pharm J (Ott) 1918;52(5):236. [Google Scholar]
- 18. Montreal Pharm J 1918;29(10):192-3. [Google Scholar]
- 19. Eyler JM. The state of science, microbiology and vaccines circa 1918. Public Health Rep 2010;125(suppl 3):27-36. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2862332/ (accessed May 5, 2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Defining Moments Canada. The Spanish flu and Canadian influenza vaccine initiatives. Available: https://definingmomentscanada.ca/wp-content/uploads/2018/12/Influenza_Vaccines.pdf (accessed May 14, 2020). [Google Scholar]
- 21. Howitt HO. Some observations in a recent epidemic. Public Health J 1919;10(11):508-10. Available: www.jstor.org/stable/45246164 (accessed May 3, 2020). [Google Scholar]
- 22. Wetmore FH. Treatment of influenza. Can Med Assoc J 1919;9(12):1075-80. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1523733/ (accessed May 11, 2020). [PMC free article] [PubMed] [Google Scholar]
- 23. Fischelis RP. Practical information on biological products for the retail druggists. Montreal Pharm J 1919;30(3):46-8. [Google Scholar]
- 24. Fischelis RP. Practical information on biological products for the retail druggists. Montreal Pharm J 1919;30(5):96-8. [Google Scholar]
- 25. Barnstead prescription book and index. Barnstead’s drugstore fonds. MG 3-Vols. 1748. & 1787. Nova Scotia Archives; Halifax, Nova Scotia, Canada. [Google Scholar]
- 26. Elixir of terpin hydrate and heroine. In: The Canadian formulary of unofficial preparations. Toronto: Ontario College of Pharmacy; 1908. Available: https://archive.org/details/canadianformular1908onta/page/16/mode/2up (accessed May 21, 2020). [Google Scholar]
- 27. Bush K. The coming of age of antibiotics: discovery and therapeutic value. Ann N Y Acad Sci 2010;1213(2010):1-4. Available: https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1111/j.1749-6632.2010.05872.x (accessed May 22, 2020). [DOI] [PubMed]
- 28. Stiver G. The treatment of influenza with antiviral drugs. CMAJ 2003;168(1):49-57. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC139319/ (accessed May 22, 2020). [PMC free article] [PubMed] [Google Scholar]
- 29. Camphor. Montreal Pharm J 1919;30(4):83-4. [Google Scholar]
- 30. Camphor in the treatment of influenza. Pharm Era 1918;51(11):314. Available: https://archive.org/details/pharmaceuticaler51newyuoft/page/314/mode/2up (accessed May 15, 2020). [Google Scholar]
- 31. Camphor as a disease preventative. Montreal Pharm J 1918;29(11):227-8. [Google Scholar]
- 32. Doctors believe no serious cases. Daily News. Available: https://open.library.ubc.ca/collections/bcnewspapers/ (accessed May 22, 2020).
- 33. Rutty C, Sullivan SC. This is public health: a Canadian history. Available: https://www.cpha.ca/sites/default/files/assets/history/book/history-book-print_all_e.pdf (accessed May 16, 2020).
- 34. Sale of alcohol by druggists in Ontario to the fore again. Retail Druggist Can 1915;2(12):28-9. Available: https://archive.org/details/retaildruggistof02torouoft/page/28/mode/2up (accessed May 16, 2020). [Google Scholar]
- 35. McKesson Canada. Our history. Available: https://www.mckesson.ca/our-history (accessed May 14, 2020).
- 36. A big seller. Natl Drug News 1918;13(1-12):11. [Google Scholar]
- 37. Shorts. Natl Drug News 1918;13(1-12):136. [Google Scholar]
- 38. Cinnamon for influenza. Natl Drug News 1918;13(1-12):5. [Google Scholar]
- 39. Cinnaform pastilles advertisement. Natl Drug News 1918;13(1-12):4. [Google Scholar]
- 40. Advocates developing drug and prescription end of business; time for careful stock-taking and analysis says G.A. Burbidge. Druggist Wkly 1923;4(4):17. Available: https://archive.org/details/drugmerch1923toro/page/n163/mode/2up (accessed May 14, 2020). [Google Scholar]
- 41. American Historical Association. Why study history. Available: https://www.historians.org/about-aha-and-membership/aha-history-and-archives/historical-archives/why-study-history-(1998) (accessed May 14, 2020).