Abstract
BACKGROUND/OBJECTIVES
Frailty, loneliness, and social isolation are all associated with adverse outcomes in older adults, but little is known about their combined impact on mortality.
DESIGN
Prospective cohort study.
SETTING
The Longitudinal Aging Study Amsterdam.
PARTICIPANTS
Community‐dwelling older adults aged 65 and older (n = 1,427).
MEASUREMENTS
Frailty was measured with the frailty phenotype (Fried criteria). Loneliness was assessed with the De Jong Gierveld Loneliness Scale. Social isolation was operationalized using information on partner status, social support, and network size. Two categorical variables were created, for each possible combination regarding frailty and loneliness (FL) and frailty and social isolation (FS), respectively. Mortality was monitored over a period of 22 years (1995–2017). Survival curves and Cox proportional hazard models were used to study the effects of the FL and FS combinations on mortality. Analyses were adjusted for sociodemographic factors, depression, chronic diseases, and smoking.
RESULTS
Frailty prevalence was 13%, and 5.9% of the sample were frail and lonely, and 6.2% frail and socially isolated. In fully adjusted models, older adults who were only frail had a higher risk of mortality compared with people without any of the conditions (hazard ratio [HR] range = 1.40–1.48; P < .01). However, the highest risk of mortality was observed in people with a combined presence of frailty and loneliness or social isolation (HRFL = 1.83; 95% confidence interval [CI] = 1.42–2.37; HRFS = 1.77; 95% CI = 1.36–2.30). Sensitivity analyses using a frailty index based on the deficit accumulation approach instead of the frailty phenotype showed similar results, confirming the robustness of our findings.
CONCLUSION
Frail older adults are at increased risk of mortality, but this risk is even higher for those who are also lonely or socially isolated. To optimize well‐being and health outcomes in physically frail older adults, targeted interventions focusing on both subjective and objective social vulnerability are needed.
Keywords: physical frailty, loneliness, social isolation, longitudinal study, social vulnerability
Frailty in older adults is defined as a decline in reserve capacity in multiple physiological systems accompanied by an increased vulnerability to stressors. 1 Frailty is one of the most important predictors of adverse outcomes in later life, with major consequences for clinical practice and public health. 2 These adverse outcomes include events such as falls, functional decline, hospitalization, and mortality. 2
There is growing attention to loneliness and social isolation in later life. In the media, public debates, and scientific literature, the consequences of loneliness and social isolation are increasingly recognized. 3 , 4 , 5 , 6 , 7 , 8 Both have been linked to adverse outcomes such as incident depression, cardiovascular disease, and mortality. 7 , 9 , 10 , 11 , 12 Loneliness refers to subjectively perceived deficits in social support or social connections, whereas social isolation is a more objective measure of the lack of social contact. This important distinction means that loneliness and social isolation should be considered separately because they cover different aspects of social relationships. 13 For example, not all socially isolated people experience the feeling of loneliness.
Recently, studies have focused on associations between frailty and indicators of social connectedness, such as loneliness and social isolation. In general, older adults with frailty seem to have smaller social networks and higher rates of loneliness. 14 , 15 , 16 However, the direction of the association is not clear, and it was suggested that the associations are bidirectional. For instance, one study found that physical frailty was associated with an increase in loneliness over time. 14 At the same time, loneliness was identified as a risk factor for incident frailty. 17 It is therefore likely that frailty and loneliness or social isolation often exist simultaneously. This is supported by previous research in primary care that showed a large number of frail older adults living in the community report they receive insufficient care for their psychosocial needs including loneliness and lack of social contact. 18 , 19
One recent cross‐sectional study showed that the coexistence of physical frailty and social isolation is associated with falls in older adults. 20 However, it is unknown to what extent frailty and loneliness or social isolation jointly associate with adverse outcomes in older adults over time. By looking at the combined presence of frailty and loneliness or social isolation, it may be possible to identify groups that are highly vulnerable for adverse outcomes such as mortality. Identification of such groups is of major importance for health care and public health because it enables optimization of care pathways and intervention strategies. Therefore, the current study examined the combined impact of frailty and loneliness or social isolation on mortality in older adults, using data over a 22‐year period from the Longitudinal Aging Study Amsterdam (LASA). 21 , 22
METHODS
Study Population
Data came from LASA, an ongoing cohort study among older adults in the Netherlands. 21 , 22 LASA is a multidisciplinary study and includes measures on physical, emotional, cognitive, and social functioning. The study started in 1992 and enrolled 3,107 people aged 55 to 84 years. Follow‐up data are collected approximately every 3 years by trained interviewers who visit the respondents at home. This includes a main interview and a subsequent medical interview with additional questionnaires and clinical tests. More information on the LASA sample and data collection was published previously. 21 , 23 The LASA study was approved by the medical ethics committee of the VU University Medical Center. Written informed consent was obtained from all participants.
In the current study, data from the second LASA measurement wave (1995–1996) were used, because this was the first wave that included data on all the instruments to measure frailty. Of the 1,720 LASA participants aged 65 and older, 1,509 also participated in the medical interview (flowchart in Supplementary Figure S1). After excluding participants with missing data on frailty, loneliness, and covariates (n = 82), the final analytical sample for the combination of frailty and loneliness consisted of 1,427 participants. The final sample for the analyses on the combination of frailty and social isolation included 1,333 participants, due to some additional missing data on the social isolation variable (n = 94). Vital status of all participants was obtained from municipality registers. All deaths that occurred between baseline (1995) and the end of follow‐up (March 1, 2017) were recorded.
Frailty
Frailty was measured using the criteria of the frailty phenotype: weight loss, low grip strength, exhaustion, slow gait speed, and low physical activity. The criteria were either operationalized identically to those of Fried et al 24 or slightly modified. The latter applies to gait speed and physical activity, for which the lowest quintile approach was used. 25 The frailty phenotype was previously used and validated in LASA. 14 , 26 Weight loss was present if a participant lost 5% or more body weight since the previous LASA wave. The participant's weight was measured using a calibrated bathroom scale while wearing underclothing only. The sum of the highest values of two measurements on each hand with a handheld dynamometer was used to measure grip strength. Low grip strength was determined using the original cutoffs stratified by sex and body mass index. 24 Two items of the Center for Epidemiologic Studies Depression Scale (CES‐D) determined the presence of exhaustion: “In the last week I felt that everything I did was an effort” and “In the last week I could not get going.” 27 To measure gait speed, respondents were asked to walk 3 m, turn around, and walk 3 m back. The time was recorded, and the lowest quintile in gait speed stratified by sex and height was applied to indicate slow gait. Finally, physical activity was assessed using the LASA Physical Activity Questionnaire. 28 The lowest quintile of average time spent on physical activities per day during 2 weeks before the interview was applied to define low physical activity. Frailty was considered present when participants met at least three of five criteria. 24
For sensitivity analyses, we also operationalized a frailty index (FI) based on the deficit accumulation approach, another widely used frailty construct. 29 , 30 A 31‐item FI was used including health deficits from the physical, mental, and cognitive domain. Additional details of this FI and its validation were reported in previous studies. 31 , 32 For the purpose of the current study and to avoid overlap, the CES‐D item on loneliness was removed from the original 32‐item FI in LASA. 31 A cutoff of .25 or higher was applied to indicate frailty. 31 , 33
Loneliness and Social Isolation
Loneliness was assessed by the De Jong Gierveld Loneliness Scale. 34 Scores range from 0 to 11, with a score of 3 or higher indicating the presence of loneliness. 34 Because a standard instrument for measuring social isolation is not available, social isolation was operationalized by combining information on partner status, social support, and network size. Respondents were considered socially isolated if they met two of the following three criteria: no partner, no social support, and having a small network size. 35 , 36 Partner status was a good indicator for living arrangements because 97.1% of the people with a partner lived with someone in the same household. The size of the personal network was assessed by asking respondents to identify people (other than their partner) with whom they had frequent contact and who were important to them (score range = 0–75). This was done for various role types (eg, friends, family, and neighbors). 37 For the nine network members they had the most frequent contact with, information was collected on the intensity of the received emotional and instrumental support (range = 0–36). Respondents who scored 0 on both emotional and instrumental support were considered to receive no social support. A small network size was defined as belonging to the lowest quartile in the sample (eight or fewer network members).
Baseline Characteristics
Other variables included age, partner status (yes/no), sex, level of education, depression score, social participation, the presence of chronic diseases, and smoking. Three groups of education were distinguished: low (elementary school or less), medium (lower vocational or general intermediate education), and high (intermediate vocational education, general secondary school, higher vocational education, college or university). Depressive symptoms were measured using the CES‐D scale (score = 0–60). 27 Informal social participation was measured by participation in leisure activities, such as visiting a museum, going to the cinema, going to a restaurant, and shopping for pleasure. We counted the number of activities that participants engaged in at least every month (except for shopping that was included if participants did this at least once per week). Formal social participation was measured by number of memberships of community organizations (eg, church, political organization, sport organization, choir). To assess the presence of chronic diseases, respondents were asked whether they currently or previously had one of the following seven major chronic diseases: cardiac disease; arterial disease; diabetes mellitus; stroke; arthritis (rheumatoid arthritis or osteoarthritis); cancer; and chronic nonspecific lung disease (asthma or chronic obstructive pulmonary disease). Smoking was assessed with a question, whether respondents were currently smoking (yes/no).
Statistical Analysis
First, descriptive analyses were conducted to characterize the study sample. Differences in baseline characteristics by loneliness and social isolation status were determined using chi‐square tests for categorical variables and t tests for continuous variables. A Venn diagram was constructed to show the overlap between physical frailty, loneliness, and social isolation.
Before conducting survival analyses, participants were categorized into groups based on their frailty and loneliness status. Four groups were created for each possible combination: (1) people without frailty and without loneliness, (2) people with only loneliness, (3) people with only frailty, and (4) people with frailty and loneliness. The same was done for frailty and social isolation. This resulted in two categorical variables (frailty‐loneliness [FL] and frailty‐social isolation [FS] combinations, respectively) that were analyzed separately. Kaplan‐Meier curves were plotted to visualize the survival rate for each group. Survivors were censored at the end of follow‐up (March 1, 2017). Next, associations between the combined variables and mortality were studied using Cox proportional hazard models. Two models were fitted: a crude model and a model adjusted for covariates. The adjusted model included age, sex, education, partner status, depression, chronic diseases, and smoking as covariates. For the FS combinations, the adjusted model did not include partner status because this was already part of the social isolation variable. In sensitivity analyses, all models were repeated by using the FI as frailty indicator. The descriptive and Cox regression analyses were done in SPSS, v.24 (IBM Corp, Armonk, NY, USA). The Kaplan‐Meier survival curves were fitted using the “survminer” package in R (v.3.6.1).
RESULTS
Baseline characteristics for both analytical samples are shown in Table 1. These results indicate that 519 of 1,427 people were lonely (36.4%) and that social isolation was present in 491 of 1,333 people (36.8%). Respondents who were lonely or socially isolated were older, more often had no partner, were more often female, had more depressive symptoms, had lower levels of social participation, had more chronic diseases, and had a higher frailty prevalence compared with respondents without loneliness or social isolation. Figure 1 shows the overlap between frailty (frailty phenotype ≥3), loneliness, and social isolation in the analytical sample of social isolation (n = 1,333). All three conditions (frailty, loneliness, and social isolation) were present in 3.6% of the sample. The combination of frailty and loneliness was observed in 5.9% of the respondents, and the combination of frailty and social isolation was present in 6.2% of the respondents. Loneliness and social isolation showed some overlap (3.6% and 15.4% = 19.0% of the sample), but the groups that were only lonely or only socially isolated were still substantial (>15% of the sample).
Table 1.
Baseline Characteristics of the Study Sample
| Baseline characteristics | Loneliness | Social isolation | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | Yes | No | Total | Yes | No | |||
| n = 1,427 | n = 519 | n = 908 | P a | n = 1,333 | n = 491 | n = 842 | P a | |
| Age, mean (SD) | 75.7 (6.6) | 76.9 (6.6) | 74.9 (6.5) | <.001 | 75.5 (6.5) | 77.5 (6.5) | 74.4 (6.3) | <.001 |
| Sex, % women | 51.5 | 56.5 | 48.7 | <.01 | 51.4 | 62.9 | 44.7 | <.001 |
| Partner status, % without partner | 41.9 | 59.0 | 32.2 | <.001 | 40.8 | 80.7 | 17.6 | <.001 |
| Educational level | ||||||||
| Low, % | 42.0 | 44.3 | 40.7 | .36 | 41.5 | 51.7 | 35.5 | <.001 |
| Medium, % | 30.3 | 28.3 | 31.4 | 30.5 | 25.9 | 33.3 | ||
| High, % | 27.7 | 27.4 | 27.9 | 28.1 | 22.4 | 31.4 | ||
| Depressive symptoms, CES‐D, mean (SD) | 8.2 (7.6) | 11.8 (8.5) | 6.1 (6.4) | <.001 | 8.2 (7.7) | 9.7 (8.0) | 7.3 (7.4) | <.001 |
| Social participation | ||||||||
| Leisure activities, mean (SD) | 1.7 (1.4) | 1.5 (1.3) | 1.7 (1.4) | <.01 | 1.7 (1.4) | 1.5 (1.3) | 1.8 (1.4) | <.001 |
| Memberships of organizations, mean (SD) | 1.8 (1.5) | 1.6 (1.5) | 1.9 (1.5) | <.001 | 1.8 (1.5) | 1.5 (1.4) | 1.9 (1.5) | <.001 |
| Chronic diseases,% | ||||||||
| Cardiac disease | 26.9 | 27.0 | 26.9 | .97 | 27.3 | 29.1 | 26.2 | .26 |
| Arterial disease | 12.8 | 15.4 | 11.2 | .02 | 12.8 | 16.1 | 10.9 | <.01 |
| Diabetes | 8.0 | 8.9 | 7.5 | .36 | 7.8 | 9.8 | 6.7 | .04 |
| Stroke | 7.8 | 7.9 | 7.7 | .90 | 7.8 | 10.0 | 6.5 | .02 |
| Arthritis | 47.4 | 52.6 | 44.4 | <.01 | 47.5 | 52.1 | 44.8 | <.01 |
| Cancer | 12.2 | 11.4 | 12.7 | .47 | 12.2 | 12.2 | 12.2 | 1.00 |
| Lung disease | 15.5 | 16.6 | 14.9 | .39 | 15.5 | 16.3 | 15.0 | .52 |
| No. of chronic diseases, 0–7, mean (SD) | 1.3 (1.1) | 1.4 (1.1) | 1.2 (1.1) | .02 | 1.3 (1.1) | 1.5 (1.2) | 1.2 (1.1) | <.001 |
| Smoking, % current smokers | 19.0 | 22.4 | 17.1 | .01 | 19.2 | 21.0 | 18.2 | .21 |
| Frailty | ||||||||
| Frailty phenotype, % frail (≥3) | 13.0 | 17.5 | 10.5 | <.001 | 12.5 | 16.9 | 9.9 | <.001 |
| Frailty index, % frail (≥.25) | 27.2 | 39.1 | 20.4 | <.001 | 26.8 | 36.3 | 21.3 | <.001 |
Abbreviations: CES‐D, Center for Epidemiologic Studies Depression Scale; SD, standard deviation.
Chi‐square test and t test.
Figure 1.
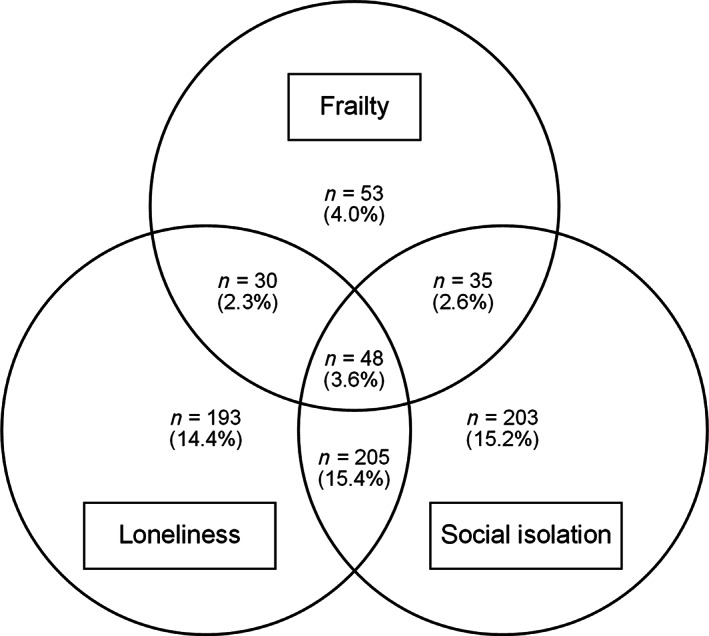
Venn diagram showing the overlap between frailty, loneliness, and social isolation. Note: There were also 566 respondents without any of the conditions (42.5% of the sample).
During 22 years of follow‐up, 1,217 of 1,427 people in the loneliness sample (85.3%) and 1,131 of 1,333 people in the social isolation sample (84.8%) died. Figure 2 displays the Kaplan‐Meier survival curves for the various FL and FS combinations. The survival curves clearly demonstrate a lower survival rate among those with frailty or those with combined presence of frailty and loneliness or frailty and social isolation. These results were confirmed in the Cox regression analyses (Table 2). In the crude model, people with loneliness (HRFL = 1.22; 95% confidence interval [CI] = 1.08–1.39), social isolation (HRFS = 1.27; 95% CI = 1.12–1.45), frailty (HRFL = 2.23; 95% CI = 1.80–2.79; HRFS = 2.14; 95% CI = 1.69–2.71), or a combination of both conditions (HRFL = 3.16; 95% CI = 2.52–3.95; HRFS = 3.33; 95% CI = 2.63–4.21) had a higher risk of mortality compared with older adults without any of the conditions. In fully adjusted models only people with frailty (HRFL = 1.40; 95% CI = 1.11–1.77; HRFS = 1.48; 95% CI = 1.15–1.91) and a combination of frailty and loneliness (HRFL = 1.83; 95% CI = 1.42–2.37) or frailty and social isolation (HRFS = 1.77; 95% CI = 1.36–2.30) had an increased risk of mortality.
Figure 2.
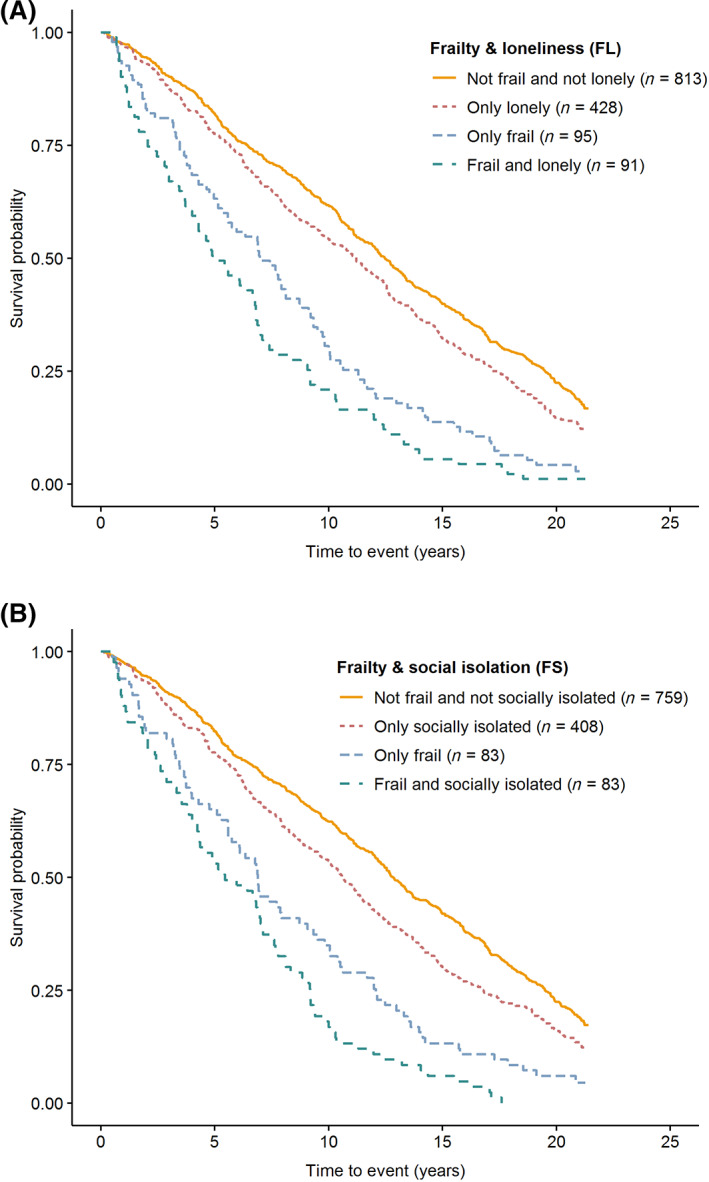
Kaplan‐Meier survival curves for groups based on the frailty phenotype (score ≥3) and loneliness (panel A) or social isolation (panel B).
Table 2.
Cox Regression Analyses: Hazard Ratios for 22‐Year All‐Cause Mortality
| Crude model | Adjusted model b | ||||
|---|---|---|---|---|---|
| Groups a | n events/total N | HR (95% CI) | P | HR (95% CI) | P |
| Loneliness, FL | |||||
| Not frail and not lonely | 663/813 | 1.0 (ref.) | 1.0 (ref.) | ||
| Only lonely | 372/428 | 1.22 (1.08–1.39) | <.01 | 1.06 (.92–1.22) | .40 |
| Only frail | 92/95 | 2.23 (1.80–2.79) | <.001 | 1.40 (1.11–1.77) | <.01 |
| Frail and lonely | 90/91 | 3.16 (2.52–3.95) | <.001 | 1.83 (1.42–2.37) | <.001 |
| Crude model | Adjusted model c | ||||
|---|---|---|---|---|---|
| Groups a | n events/total N | HR (95% CI) | P | HR (95% CI) | P |
| Social isolation, FS | |||||
| Not frail and not socially isolated | 615/759 | 1.0 (ref.) | 1.0 (ref.) | ||
| Only socially isolated | 354/408 | 1.27 (1.12–1.45) | <.001 | 1.06 (.92–1.21) | .41 |
| Only frail | 79/83 | 2.14 (1.69–2.71) | <.001 | 1.48 (1.15–1.91) | <.01 |
| Frail and socially isolated | 83/83 | 3.33 (2.63–4.21) | <.001 | 1.77 (1.36–2.30) | <.001 |
Abbreviations: CI, confidence interval; FL, frailty and loneliness; FS, frailty and social isolation; HR, hazard ratio.
Frailty was measured with the frailty phenotype (score ≥3).
Adjusted for age, sex, education, partner status, depression score, number of chronic diseases, and smoking.
Adjusted for age, sex, education, depression score, number of chronic diseases, and smoking.
Results were the same when performing survival analyses with the FI as frailty indicator, even though the groups of older adults with frailty based on the FI were larger compared with frailty based on the frailty phenotype (Supplementary Figure S2). The sensitivity analyses with the FI showed that, in fully adjusted models, older adults who were frail and lonely (HRFL = 1.77; 95% CI = 1.49–2.11) or frail and socially isolated (HRFS = 1.80; 95% CI = 1.48–2.17) had the highest risk of mortality compared with older adults without any of the conditions (Supplementary Table S1).
DISCUSSION
Using data over a period of 22 years from a cohort of community‐dwelling older adults in the Netherlands, we examined the combined effects of frailty and loneliness or social isolation on mortality in later life. The results revealed a gradual increase in mortality risk: people with frailty were at higher risk of mortality compared with older adults without any of the conditions, but the highest risk was observed in those with a combined presence of frailty and loneliness or frailty and social isolation. These results indicate that both subjective and objective aspects of social vulnerability in older adults with frailty may have serious consequences in terms of premature death.
The results also showed that it did not matter whether the frailty phenotype or the FI was used as a frailty indicator: the results were similar, showing the robustness of our findings. At the same time, this is remarkable because the prevalence of frailty is much higher when using the FI instead of the frailty phenotype (27% vs 13%). Another noteworthy result is that the overlap between loneliness and social isolation was not that high. Only one‐third of the people with loneliness and/or social isolation presented with both conditions, showing that they should be regarded as distinct groups when targeting interventions. Furthermore, the group that had a combined presence of frailty with loneliness or social isolation was small (about 6% of the total sample), but their risk for mortality was generally higher compared with people with only one or without any of the conditions, even in models adjusted for various sociodemographic factors, comorbidity, and smoking.
The current study corroborates findings from previous work. Frailty, loneliness, and social isolation were all shown to be prospectively associated with adverse outcomes such as mortality in older adults. 2 , 9 Moreover, earlier research investigated the beneficial effects of psychosocial resources on frailty outcomes. 26 , 38 These studies found mixed results. In frail hospitalized older adults, psychosocial resources buffered against various adverse outcomes, 38 whereas in community‐dwelling older adults with frailty, protective effects of psychosocial resources were not observed. 26 However, none of these studies looked specifically at the lack of social resources, as measured subjectively by loneliness or objectively by social isolation. This is where the current study adds to previous work: we identified a new group at an increased risk of premature death, namely older adults with frailty who are also lonely or socially isolated.
Various mechanisms may explain the higher risk of mortality in older adults with frailty who also present with loneliness or social isolation. Further insights into these underlying mechanisms may enhance the development of new interventional approaches. First, well‐functioning social support networks are vital for maintaining autonomy and quality of life. This is highlighted in various care guidelines for older adults with frailty. 39 , 40 A lack of social connections may result in unfulfilled care needs and a higher chance of poor health outcomes. Second, frail older adults with loneliness or social isolation may also be those who have less favorable personality characteristics, such as low self‐esteem and low mastery. This makes them more vulnerable in coping with stressful situations and increases the risk of mortality. 35 Finally, loneliness or social isolation may also have more direct physiological effects in older adults, expressed by neuroendocrine and immune responses 41 and various medical conditions. Social isolation, for example, is associated with depression and cardiovascular disease that are both linked to mortality. 10 , 12
The results of our study have practical implications. They suggest a multidimensional and personalized approach to reduce frailty and its negative consequences. Social vulnerability should be considered when providing care to older adults with frailty or when designing frailty interventions, not only to prevent mortality but also to improve well‐being. Targeted interventions for social isolation and loneliness may be needed. These interventions should be tailored and match the cause of social isolation or loneliness. For social isolation, certain intervention strategies have proven to be effective, such as participation in group‐based social activities. 42 For loneliness, the evidence for effective interventions is fragmented. 4 Some approaches have the potential to diminish feelings of loneliness, such as friendship courses and psychological therapies. 42 However, more research is needed to show the extent to which various interventions are effective in expanding social networks and reducing loneliness in frail older populations.
The results of our study are also highly relevant in the light of the current COVID‐19 crisis. Frail older adults may be disproportionally affected by isolation measures that have been implemented in many countries. 43 Social distancing may prevent transmission of a virus, but it increases social isolation and feelings of loneliness that in turn may increase the long‐term risk of mortality in this group.
Strengths of this study include the large community‐based sample, the long‐term mortality follow‐up, the use of the two most widely used frailty indicators (ie, frailty phenotype and FI), and the use of both subjective and objective indicators of social connectedness. This enabled us to look at the effects of the combined presence of frailty and loneliness or social isolation on mortality, and to compare results between different frailty indicators, which has never been done before.
However, some limitations also have to be considered when interpreting the results of this study. First, we used validated instruments to measure frailty and loneliness, but for social isolation no standard measure is available. We constructed a social isolation variable similar to previous studies. 35 , 36 To be socially isolated, older adults had to meet two of three criteria: no partner, no social support, and having a small network size. It is noteworthy that a small network size in LASA, as defined by the lowest quartile, is higher than in other studies. This may be the result of the extensive network module that was used to ask about social connections in various domains, whereas other studies often use a single question to assess the number of network members. 36
Second, we only included baseline variables in the analyses. It is possible that during the long period of follow‐up there have been some shifts in frailty, loneliness, and social isolation status. Moreover, in the current design we cannot rule out reverse causation (ie, loneliness and social isolation may result from poor health). Future studies may therefore also look at time‐varying measurements. Third, we adjusted our analyses for the most important confounders. However, we acknowledge that there are other behavioral or clinical risk factors for mortality for which we could not control. For example, it would not be appropriate to control for physical activity because it is part of both frailty definitions.
Fourth, we were not able to consider potential cohort differences. Our baseline data come from 1995 to 1996, so it is possible that our findings do not apply to other generations of older adults. This may be investigated in the future when long‐term mortality data for refreshment cohorts in LASA (included in 2002–2003 and 2012–2013) become available. 22 Fifth, depression may be an important underlying condition of loneliness and social isolation in the studied population. Although we were able to show this using the CES‐D score of depressive symptoms, we did not have information available on depression diagnosis.
Finally, much more research is needed to understand how social resources contribute to resilience in older adults. 44 In the current study, we have only focused on loneliness and social isolation as indicators of social connectedness. It might be interesting to repeat this study with a broader index of social vulnerability, 45 , 46 to find out whether our findings are specific for loneliness and social isolation in frail older adults or also apply to other social determinants.
In conclusion, this study showed that older adults with frailty who are also lonely or socially isolated constitute a high‐risk group for mortality. This is important information for researchers and clinicians. To optimize well‐being and health outcomes in physically frail older adults, targeted interventions focusing on both subjective and objective social vulnerability are needed.
Supporting information
Supplementary Figure S1: Flowchart of the study population.
Supplementary Figure S2: Sensitivity analysis: Kaplan‐Meier survival curves for groups based on the frailty index (≥.25) and loneliness (panel A) or social isolation (panel B).
Supplementary Table S1: Sensitivity analysis with the frailty index as frailty indicator: Cox regression analyses, hazard ratios for 22‐year all‐cause mortality.
ACKNOWLEDGMENTS
Financial Disclosure
The Longitudinal Aging Study Amsterdam (LASA) is largely supported by a grant from the Netherlands Ministry of Health, Welfare and Sports, Directorate of Long‐Term Care. Emiel O. Hoogendijk was supported by an NWO/ZonMw Veni fellowship (Grant No. 91618067).
Conflict of Interest
The authors have declared no conflicts of interest for this article.
Author Contributions
Drafted the manuscript: Hoogendijk. Statistical analysis: Hoogendijk, Smit, and Schuster. Study design and concept: Hoogendijk, Smit, van Dam, Holwerda, and Andrew. Data interpretation, critical revision, and approval of final version: All authors.
Sponsor's Role
None.
REFERENCES
- 1. Clegg A, Young J, Iliffe S, Rikkert MO, Rockwood K. Frailty in elderly people. Lancet. 2013;381:752‐762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394:1365‐1375. [DOI] [PubMed] [Google Scholar]
- 3. Killeen C. Loneliness: an epidemic in modern society. J Adv Nurs. 1998;28:762‐770. [DOI] [PubMed] [Google Scholar]
- 4. Fried L, Prohaska T, Burholt V, et al. A unified approach to loneliness. Lancet. 2020;395:114. [DOI] [PubMed] [Google Scholar]
- 5. Cacioppo JT, Cacioppo S. The growing problem of loneliness. Lancet. 2018;391:426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Cacioppo S, Grippo AJ, London S, Goossens L, Cacioppo JT. Loneliness: clinical import and interventions. Perspect Psychol Sci. 2015;10:238‐249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Courtin E, Knapp M. Social isolation, loneliness and health in old age: a scoping review. Health Soc Care Community. 2017;25:799‐812. [DOI] [PubMed] [Google Scholar]
- 8. Shankar A, McMunn A, Demakakos P, Hamer M, Steptoe A. Social isolation and loneliness: prospective associations with functional status in older adults. Health Psychol. 2017;36:179‐187. [DOI] [PubMed] [Google Scholar]
- 9. Holt‐Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta‐analytic review. Perspect Psychol Sci. 2015;10:227‐237. [DOI] [PubMed] [Google Scholar]
- 10. Valtorta NK, Kanaan M, Gilbody S, Hanratty B. Loneliness, social isolation and risk of cardiovascular disease in the English longitudinal study of ageing. Eur J Prevent Cardiol. 2018;25:1387‐1396. [DOI] [PubMed] [Google Scholar]
- 11. Holwerda TJ, van Tilburg TG, Deeg DJ, et al. Impact of loneliness and depression on mortality: results from the Longitudinal Ageing Study Amsterdam. Br J Psychiatry. 2016;209:127‐134. [DOI] [PubMed] [Google Scholar]
- 12. Cacioppo JT, Hawkley LC, Thisted RA. Perceived social isolation makes me sad: 5‐year cross‐lagged analyses of loneliness and depressive symptomatology in the Chicago Health, Aging, and Social Relations Study. Psychol Aging. 2010;25:453‐463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Beller J, Wagner A. Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. 2018;37:808‐813. [DOI] [PubMed] [Google Scholar]
- 14. Hoogendijk EO, Suanet B, Dent E, Deeg DJ, Aartsen MJ. Adverse effects of frailty on social functioning in older adults: results from the Longitudinal Aging Study Amsterdam. Maturitas. 2016;83:45‐50. [DOI] [PubMed] [Google Scholar]
- 15. Jurschik P, Nunin C, Botigue T, Escobar MA, Lavedan A, Viladrosa M. Prevalence of frailty and factors associated with frailty in the elderly population of Lleida, Spain: the FRALLE survey. Arch Gerontol Geriatr. 2012;55:625‐631. [DOI] [PubMed] [Google Scholar]
- 16. Herrera‐Badilla A, Navarrete‐Reyes AP, Amieva H, Avila‐Funes JA. Loneliness is associated with frailty in community‐dwelling elderly adults. J Am Geriatr Soc. 2015;63:607‐609. [DOI] [PubMed] [Google Scholar]
- 17. Gale CR, Westbury L, Cooper C. Social isolation and loneliness as risk factors for the progression of frailty: the English Longitudinal Study of Ageing. Age Ageing. 2018;47:392‐397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Hoogendijk EO, Muntinga ME, van Leeuwen KM, et al. Self‐perceived met and unmet care needs of frail older adults in primary care. Arch Gerontol Geriatr. 2014;58:37‐42. [DOI] [PubMed] [Google Scholar]
- 19. Hermsen LAH, Hoogendijk EO, van der Wouden JC, et al. Self‐perceived care needs in older adults with joint pain and comorbidity. Aging Clin Exp Res. 2018;30:449‐455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hayashi T, Umegaki H, Makino T, et al. Combined impact of physical frailty and social isolation on rate of falls in older adults. J Nutr Health Aging. 2020;24:312‐318. [DOI] [PubMed] [Google Scholar]
- 21. Hoogendijk EO, Deeg DJ, Poppelaars J, et al. The Longitudinal Aging Study Amsterdam: cohort update 2016 and major findings. Eur J Epidemiol. 2016;31:927‐945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Hoogendijk EO, Deeg DJH, de Breij S, et al. The Longitudinal Aging Study Amsterdam: cohort update 2019 and additional data collections. Eur J Epidemiol. 2020;35:61‐74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Huisman M, Poppelaars J, van der Horst M, et al. Cohort profile: the Longitudinal Aging Study Amsterdam. Int J Epidemiol. 2011;40:868‐876. [DOI] [PubMed] [Google Scholar]
- 24. Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146‐M156. [DOI] [PubMed] [Google Scholar]
- 25. Saum KU, Muller H, Stegmaier C, Hauer K, Raum E, Brenner H. Development and evaluation of a modification of the fried frailty criteria using population‐independent cutpoints. J Am Geriatr Soc. 2012;60:2110‐2115. [DOI] [PubMed] [Google Scholar]
- 26. Hoogendijk EO, van Hout HP, van der Horst HE, et al. Do psychosocial resources modify the effects of frailty on functional decline and mortality? J Psychosom Res. 2014;77:547‐551. [DOI] [PubMed] [Google Scholar]
- 27. Radloff L. The CES‐D scale: a self‐report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385‐401. [Google Scholar]
- 28. Stel VS, Smit JH, Pluijm SM, Visser M, Deeg DJ, Lips P. Comparison of the LASA Physical Activity Questionnaire with a 7‐day diary and pedometer. J Clin Epidemiol. 2004;57:252‐258. [DOI] [PubMed] [Google Scholar]
- 29. Rockwood K, Mitnitski A. Frailty in relation to the accumulation of deficits. J Gerontol A Biol Sci Med Sci. 2007;62:722‐727. [DOI] [PubMed] [Google Scholar]
- 30. Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Hoogendijk EO, Theou O, Rockwood K, Onwuteaka‐Philipsen BD, Deeg DJH, Huisman M. Development and validation of a frailty index in the Longitudinal Aging Study Amsterdam. Aging Clin Exp Res. 2017;29:927‐933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Hoogendijk EO, Rockwood K, Theou O, et al. Tracking changes in frailty throughout later life: results from a 17‐year longitudinal study in the Netherlands. Age Ageing. 2018;47:727‐733. [DOI] [PubMed] [Google Scholar]
- 33. Song X, Mitnitski A, Rockwood K. Prevalence and 10‐year outcomes of frailty in older adults in relation to deficit accumulation. J Am Geriatr Soc. 2010;58:681‐687. [DOI] [PubMed] [Google Scholar]
- 34. De Jong‐Gierveld J, Kamphuls F. The development of a Rasch‐type loneliness scale. Appl Psychol Meas. 1985;9:289‐299. [Google Scholar]
- 35. Holwerda TJ, Beekman AT, Deeg DJ, et al. Increased risk of mortality associated with social isolation in older men: only when feeling lonely? Results from the Amsterdam Study of the Elderly (AMSTEL). Psychol Med. 2012;42:843‐853. [DOI] [PubMed] [Google Scholar]
- 36. Cornwell EY, Waite LJ. Measuring social isolation among older adults using multiple indicators from the NSHAP study. J Gerontol B Psychol Sci Soc Sci. 2009;64:i38‐i46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Broese van Groenou M, Hoogendijk EO, van Tilburg TG. Continued and new personal relationships in later life: differential effects of health. J Aging Health. 2013;25:274‐295. [DOI] [PubMed] [Google Scholar]
- 38. Dent E, Hoogendijk EO. Psychosocial factors modify the association of frailty with adverse outcomes: a prospective study of hospitalised older people. BMC Geriatr. 2014;14:108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Dent E, Morley JE, Cruz‐Jentoft AJ, et al. Physical frailty: ICFSR international clinical practice guidelines for identification and management. J Nutr Health Aging. 2019;23:771‐787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Dent E, Martin FC, Bergman H, Woo J, Romero‐Ortuno R, Walston JD. Management of frailty: opportunities, challenges, and future directions. Lancet. 2019;394:1376‐1386. [DOI] [PubMed] [Google Scholar]
- 41. Steptoe A, Owen N, Kunz‐Ebrecht SR, Brydon L. Loneliness and neuroendocrine, cardiovascular, and inflammatory stress responses in middle‐aged men and women. Psychoneuroendocrinology. 2004;29:593‐611. [DOI] [PubMed] [Google Scholar]
- 42. Gardiner C, Geldenhuys G, Gott M. Interventions to reduce social isolation and loneliness among older people: an integrative review. Health Soc Care Community. 2018;26:147‐157. [DOI] [PubMed] [Google Scholar]
- 43. Armitage R, Nellums LB. COVID‐19 and the consequences of isolating the elderly. Lancet Public Health. 2020;5(5):e256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gijzel SMW, Whitson HE, van de Leemput IA, et al. Resilience in clinical care: getting a grip on the recovery potential of older adults. J Am Geriatr Soc. 2019;67:2650‐2657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Andrew MK, Mitnitski AB, Rockwood K. Social vulnerability, frailty and mortality in elderly people. PLoS One. 2008;3:e2232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Armstrong JJ, Andrew MK, Mitnitski A, Launer LJ, White LR, Rockwood K. Social vulnerability and survival across levels of frailty in the Honolulu‐Asia Aging Study. Age Ageing. 2015;44:709‐712. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Figure S1: Flowchart of the study population.
Supplementary Figure S2: Sensitivity analysis: Kaplan‐Meier survival curves for groups based on the frailty index (≥.25) and loneliness (panel A) or social isolation (panel B).
Supplementary Table S1: Sensitivity analysis with the frailty index as frailty indicator: Cox regression analyses, hazard ratios for 22‐year all‐cause mortality.


